Work Ability in Patients with Chronic Myeloid Leukemia: A Danish Nationwide Cohort Study
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Outcomes and Confounders
2.3. Statistical Analysis
3. Results
3.1. Patients and Matched Comparators
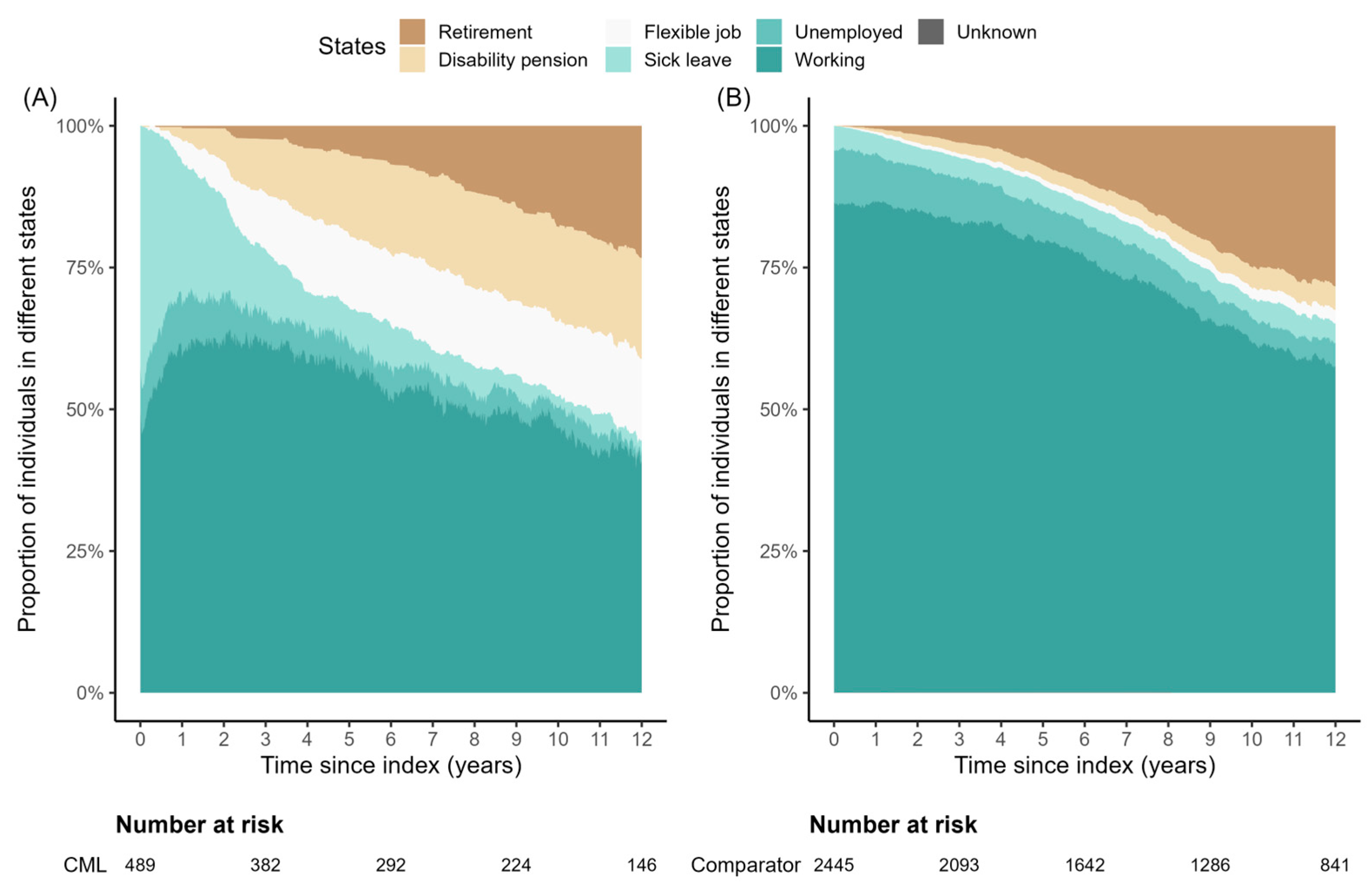
3.2. Work Ability
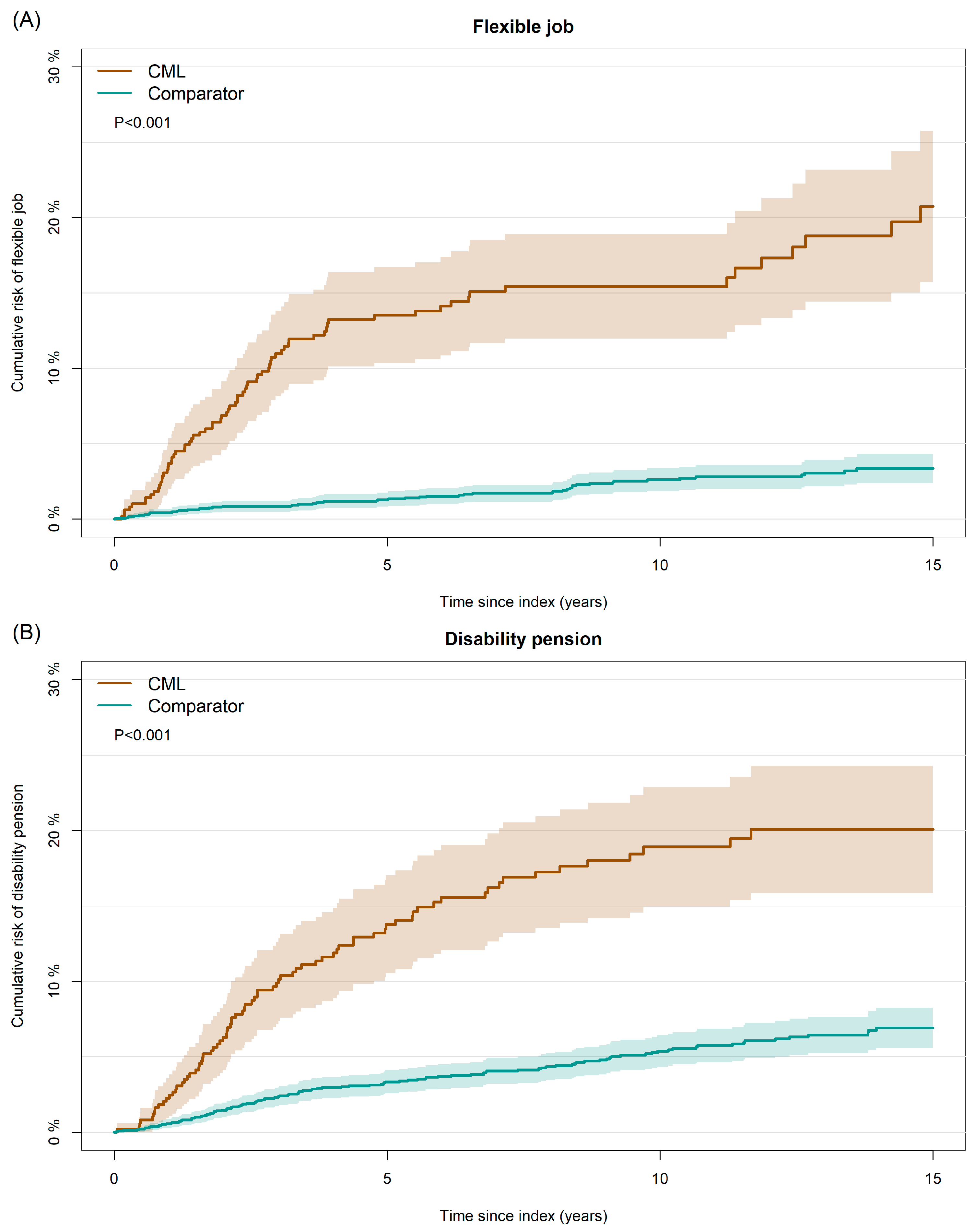
3.3. Risk of Flexible Job and Disability Pension
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CML | chronic myeloid leukemia |
| TKI | Tyrosine Kinase Inhibitor |
| IQR | Interquartile Range |
| CRS | The Danish Civil Registration System |
| CCI | Charlson comorbidity index |
| RD | Risk difference |
| MPN | Philadelphia-negative myeloproliferative neoplasm |
References
- Hochhaus, A.; Larson, R.A.; Guilhot, F.; Radich, J.P.; Branford, S.; Hughes, T.P.; Baccarani, M.; Deininger, M.W.; Cervantes, F.; Fujihara, S.; et al. Long-Term Outcomes of Imatinib Treatment for Chronic Myeloid Leukemia. N. Engl. J. Med. 2017, 376, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Hehlmann, R.; Lauseker, M.; Saußele, S.; Pfirrmann, M.; Krause, S.; Kolb, H.J.; Neubauer, A.; Hossfeld, D.K.; Nerl, C.; Gratwohl, A.; et al. Assessment of Imatinib as First-Line Treatment of Chronic Myeloid Leukemia: 10-Year Survival Results of the Randomized CML Study IV and Impact of Non-CML Determinants. Leukemia 2017, 31, 2398–2406. [Google Scholar] [CrossRef]
- Hamerschlak, N.; De Souza, C.; Cornacchioni, A.L.; Pasquini, R.; Tabak, D.; Spector, N.; Steagall, M. Quality of Life of Chronic Myeloid Leukemia Patients in Brazil: Ability to Work as a Key Factor. Support. Care Cancer 2014, 22, 2113–2118. [Google Scholar] [CrossRef]
- Horsboel, T.A.; Nielsen, C.V.; Nielsen, B.; Jensen, C.; Andersen, N.T.; de Thurah, A. Type of Hematological Malignancy Is Crucial for the Return to Work Prognosis: A Register-Based Cohort Study. J. Cancer Surviv. 2013, 7, 614–623. [Google Scholar] [CrossRef]
- Horsboel, T.A.; Nielsen, C.V.; Andersen, N.T.; Nielsen, B.; De Thurah, A. Risk of Disability Pension for Patients Diagnosed with Haematological Malignancies: A Register-Based Cohort Study. Acta Oncol. 2014, 53, 724–734. [Google Scholar] [CrossRef]
- Horsboel, T.A.; Nielsen, C.V.; Nielsen, B.; Andersen, N.T.; De Thurah, A. Wage-Subsidised Employment as a Result of Permanently Reduced Work Capacity in a Nationwide Cohort of Patients Diagnosed with Haematological Malignancies. Acta Oncol. 2015, 54, 743–749. [Google Scholar] [CrossRef] [PubMed]
- De Barros, S.; Vayr, F.; Despas, F.; Strumia, M.; Podevin, C.; Gauthier, M.; Delabesse, E.; Soulat, J.-M.; Laurent, G.; Huguet, F.; et al. The Impact of Chronic Myeloid Leukemia on Employment: The French Prospective Study. Ann. Hematol. 2019, 98, 615–623. [Google Scholar] [CrossRef]
- Conte, C.; Vayr, F.; Pajiep, M.C.; Despas, F.; Huguet, F.; Mestre, M.L.; Gauthier, M.; Herin, F. Impact of the Treatment of Chronic Myeloid Leukaemia by Tyrosine-Kinase Inhibitors on Sick Leaves Refund: A Nationwide Cohort Study. Support. Care Cancer 2022, 30, 5431–5440. [Google Scholar] [CrossRef] [PubMed]
- Erichsen, R.; Lash, T.L.; Hamilton-Dutoit, S.J.; Bjerregaard, B.; Vyberg, M.; Pedersen, L. Existing Data Sources for Clinical Epidemiology: The Danish National Pathology Registry and Data Bank. Clin. Epidemiol. 2010, 2, 51. [Google Scholar] [CrossRef]
- Bak, M.; Ibfelt, E.H.; Stauffer Larsen, T.; Rønnov-Jessen, D.; Pallisgaard, N.; Madelung, A.; Udby, L.; Hasselbalch, H.C.; Bjerrum, O.W.; Andersen, C.L. The Danish National Chronic Myeloid Neoplasia Registry. Clin. Epidemiol. 2016, 8, 567–572. [Google Scholar] [CrossRef]
- Pedersen, C.B.; Gøtzsche, H.; Møller, J.O.; Mortensen, P.B. The Danish Civil Registration System. A Cohort of Eight Million Persons. Dan. Med. Bull. 2006, 53, 441–449. [Google Scholar] [PubMed]
- Pedersen, C.B. The Danish Civil Registration System. Scand. J. Public Health 2011, 39, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Sundararajan, V.; Quan, H.; Halfan, P.; Fushimi, K.; Luthi, J.C.; Burnand, B.; Ghali, W.A. Cross-National Comparative Performance of Three Versions of the ICD-10 Charlson Index. Med. Care 2007, 45, 1210–1215. [Google Scholar] [CrossRef]
- Lynge, E.; Sandegaard, J.L.; Rebolj, M. The Danish National Patient Register. Scand. J. Public Health 2011, 39, 30–33. [Google Scholar] [CrossRef]
- Schmidt, M.; Schmidt, S.A.J.; Sandegaard, J.L.; Ehrenstein, V.; Pedersen, L.; Sørensen, H.T. The Danish National Patient Registry: A Review of Content, Data Quality, and Research Potential. Clin. Epidemiol. 2015, 7, 449. [Google Scholar] [CrossRef]
- Wallach Kildemoes, H.; Toft Sørensen, H.; Hallas, J. The Danish National Prescription Registry. Scand. J. Public Health 2011, 39, 38–41. [Google Scholar] [CrossRef]
- Pottegård, A.; Schmidt, S.A.J.; Wallach-Kildemoes, H.; Sørensen, H.T.; Hallas, J.; Schmidt, M. Data Resource Profile: The Danish National Prescription Registry. Int. J. Epidemiol. 2017, 46, 798–798f. [Google Scholar] [CrossRef]
- Mors, O.; Perto, G.P.; Mortensen, P.B. The Danish Psychiatric Central Research Register. Scand. J. Public Health 2011, 39, 54–57. [Google Scholar] [CrossRef]
- Hjollund, N.H.; Larsen, F.B.; Andersen, J.H. Register-Based Follow-up of Social Benefits and Other Transfer Payments: Accuracy and Degree of Completeness in a Danish Interdepartmental Administrative Database Compared with a Population-Based Survey. Scand. J. Public Health 2007, 35, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Jensen, V.M.; Rasmussen, A.W. Danish Education Registers. Scand. J. Public Health 2011, 39, 91–94. [Google Scholar] [CrossRef] [PubMed]
- UNESCO Institute for Statistics. International Standard Classification of Education, ISCED 2011; UNESCO Institute for Statistics: Montreal, QC, Canada, 2012. [Google Scholar]
- Baadsgaard, M.; Quitzau, J. Danish Registers on Personal Income and Transfer Payments. Scand. J. Public Health 2011, 39, 103–105. [Google Scholar] [CrossRef] [PubMed]
- OECD. What Are Equivalence Scales? OECD Projected Income Distribution Poverty [Internet]. 2011. Available online: http://www.oecd.org/els/soc/OECD-Note-EquivalenceScales.pdf (accessed on 23 March 2025).
- Maksten, E.F.; Jakobsen, L.H.; Kragholm, K.H.; Baech, J.; Andersen, M.P.; Madsen, J.; Jørgensen, J.M.; Clausen, M.R.; Pedersen, R.S.; Dessau-arp, A.; et al. Work Disability and Return to Work After Lymphoma: A Danish Nationwide Cohort Study. Clin. Epidemiol. 2023, 15, 337–348. [Google Scholar] [CrossRef]
- Putter, H.; Fiocco, M.; Geskus, R.B. Tutorial in Biostatistics: Competing Risks and Multi-State Models. Stat. Med. 2007, 26, 2389–2430. [Google Scholar] [CrossRef]
- Gray, R.J. A Class of K-Sample Tests for Comparing the Cumulative Incidence of a Competing Risk. Ann. Stat. 1988, 16, 1141–1154. [Google Scholar] [CrossRef]
- Svingel, L.S.; Christensen, S.F.; Kjærsgaard, A.; Stenling, A.; Paulsson, B.; Andersen, C.L.; Christiansen, C.F.; Stentoft, J.; Starklint, J.; Severinsen, M.T.; et al. Labor Market Affiliation of Patients with Myeloproliferative Neoplasms: A Population-Based Matched Cohort Study. Acta Oncol. 2023, 62, 1286–1294. [Google Scholar] [CrossRef]
- Del Rosario García, B.; Viña Romero, M.M.; González Rosa, V.; Alarcón Payer, C.; Oliva Oliva, L.; Merino Alonso, F.J.; Nazco Casariego, G.J.; Gutiérrez Nicolás, F. Risk Factors Determining Adherence to Tyrosine Kinase Inhibitors in Chronic Myeloid Leukaemia. J. Oncol. Pharm. Pract. 2024, 30, 902–906. [Google Scholar] [CrossRef]
- Efficace, F.; Baccarani, M.; Breccia, M.; Cottone, F.; Alimena, G.; Deliliers, G.L.; Baratè, C.; Specchia, G.; Di Lorenzo, R.; Luciano, L.; et al. Chronic Fatigue Is the Most Important Factor Limiting Health-Related Quality of Life of Chronic Myeloid Leukemia Patients Treated with Imatinib. Leukemia 2013, 27, 1511–1519. [Google Scholar] [CrossRef]
- Hehlmann, R. Chronic Myeloid Leukemia in 2020. HemaSphere 2020, 4, E468. [Google Scholar] [CrossRef] [PubMed]
- Maksten, E.; Jørgensen, R.; Pedersen, M.; Fonager, K.; Bech, R.; Mølle, I.; Ørskov, A.; Schöllkopf, C.; Overgaard, U.; Thomsen, G.; et al. Work Disability and Return to Work After Treatment for Acute Lymphoblastic Leukemia: A Danish Nationwide Cohort Study. Clin. Epidemiol. 2024, 16, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, P.; Aagesen, M.; Tang, L.H.; Bruun, N.H.; Zwisler, A.D.; Stapelfeldt, C.M. Risk of Being Granted Disability Pension among Incident Cancer Patients before and after a Structural Pension Reform: A Danish Population-Based, Matched Cohort Study. Scand. J. Work. Environ. Health 2020, 46, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Øvlisen, A.K.; Jakobsen, L.H.; Kragholm, K.H.; Nielsen, R.E.; de Nully Brown, P.; Dahl-Sørensen, R.B.; Frederiksen, H.; Mannering, N.; Josefsson, P.L.; Ludvigsen Al-Mashhadi, A.; et al. Mental Health among Patients with Non-Hodgkin Lymphoma: A Danish Nationwide Study of Psychotropic Drug Use in 8750 Patients and 43,750 Matched Comparators. Am. J. Hematol. 2022, 97, 749–761. [Google Scholar] [CrossRef] [PubMed]
- Krokstad, S.; Johnsen, R.; Westin, S. Social Determinants of Disability Pension: A 10-Year Follow-up of 62,000 People in a Norwegian County Population. Int. J. Epidemiol. 2002, 31, 1183–1191. [Google Scholar] [CrossRef]
| Patients with CML (n = 489) | Matched Comparators (n = 2445) | |
|---|---|---|
| Age, median (IQR) | 46 (39–54) | 46 (38–54) |
| Age group, n (%) | ||
| 25–36 years | 101 (20.7%) | 503 (20.6%) |
| 37–48 years | 181 (37.0%) | 902 (36.9%) |
| 49–60 years | 207 (42.3%) | 1040 (42.5%) |
| Sex, n (%) | ||
| Male | 291 (59.5%) | 1455 (59.5%) |
| Female | 198 (40.5%) | 990 (40.5%) |
| CCI prior to diagnosis, n (%) | ||
| 0 | 406 (83.0%) | 2030 (83.0%) |
| 1 | 50 (10.2%) | 250 (10.2%) |
| ≥2 | 33 (6.7%) | 165 (6.7%) |
| Cohabiting status, n (%) | ||
| Living alone | 118 (24.1%) | 677 (27.7%) |
| Living with partner | 366 (74.8%) | 1744 (71.3%) |
| Unknown | 5 (1.0%) | 24 (1.0%) |
| Education level (ISCED), n (%) | ||
| ISCED 0–2 | 98 (20.0%) | 436 (17.8%) |
| ISCED 3 | 232 (47.4%) | 1126 (46.1%) |
| ISCED 5–6 | 97 (19.8%) | 595 (24.3%) |
| ISCED 7–8 | 48 (9.8%) | 225 (9.2%) |
| Unknown | 14 (2.9%) | 63 (2.6%) |
| Equalized income, quartiles, n (%) | ||
| Lowest | 83 (17.0%) | 493 (20.2%) |
| Second lowest | 136 (27.8%) | 577 (23.6%) |
| Second highest | 127 (26.0%) | 683 (27.9%) |
| Highest | 138 (28.2%) | 668 (27.3%) |
| Unknown | 5 (1.0%) | 24 (1.0%) |
| Employment status 1, n (%) | ||
| Working | 410 (83.8%) | 2149 (87.9%) |
| Unemployed | 42 (8.6%) | 197 (8.1%) |
| Sick leave | 30 (6.1%) | 83 (3.4%) |
| Unclassified | 7 (1.4%) | 16 (0.7%) |
| Long-term sickness 2, n (%) | ||
| Yes | 59 (12.1%) | 198 (8.1%) |
| No | 430 (87.9%) | 2247 (91.9%) |
| Year of diagnosis, n (%) | ||
| 2002–2007 | 139 (28.4%) | - |
| 2008–2013 | 156 (31.9%) | - |
| 2014–2020 | 194 (39.7%) | - |
| Time Since Index (Years) | Working State | Patients with CML (%) | Matched Comparators (%) | p-Value |
|---|---|---|---|---|
| 0 | Working | 50.1 | 86.2 | <0.001 |
| Sick leave 1 | 42.3 | 4.3 | <0.001 | |
| Flexible job | 0 | 0 | - | |
| Disability pension | 0 | 0 | - | |
| 1 | Working | 59.2 | 86.5 | <0.001 |
| Sick leave 1 | 25.5 | 3.3 | <0.001 | |
| Flexible job | 3.9 | 0.4 | <0.001 | |
| Disability pension | 2.2 | 0.5 | 0.002 | |
| 3 | Working | 61.8 | 83.0 | <0.001 |
| Sick leave 1 | 11.3 | 3.3 | <0.001 | |
| Flexible job | 9.9 | 0.7 | <0.001 | |
| Disability pension | 9.4 | 1.9 | <0.001 | |
| 5 | Working | 56.8 | 79.3 | <0.001 |
| Sick leave 1 | 6.8 | 3.8 | 0.024 | |
| Flexible job | 12.7 | 1.0 | <0.001 | |
| Disability pension | 14.3 | 2.6 | <0.001 | |
| 10 | Working | 46.7 | 61.8 | <0.001 |
| Sick leave 1 | 2.0 | 3.4 | 0.505 | |
| Flexible job | 13.2 | 1.9 | <0.001 | |
| Disability pension | 16.8 | 3.7 | <0.001 |
| Flexible Job | Disability Pension | |||||
|---|---|---|---|---|---|---|
| Risk (%) | RD (Crude) | RD (Adjusted) 1 | Risk (%) | RD (Crude) | RD (Adjusted) 1 | |
| Sex | ||||||
| Male | 7.8 (4.6;11.1) | 0 | 9.7 (6.1;13.4) | 0 | ||
| Female | 21.9 (15.8;27.9) | 14.0 (7.2;20.9) * | 19.7 (13.9;25.5) | 10.0 (3.1;16.9) * | ||
| Age at diagnosis | ||||||
| 25–36 years | 13.9 (6.9;21.0) | 0 | 4.4 (0.2;8.7) | 0 | ||
| 37–48 years | 13.3 (8.2;18.4) | −0.7 (−9.6;8.2) | 12.9 (7.8;17.9) | 8.6 (1.7;15.4) * | ||
| 49–60 years | 13.6 (8.6;18.6) | −0.4 (−9.0;8.3) | 19.5 (13.6;25.4) | 14.9 (7.8;22.1) * | ||
| Year of diagnosis | ||||||
| 2002–2007 | 16.8 (10.5;23.0) | 0 | 0 | 17.5 (11.2;23.9) | 0 | 0 |
| 2008–2013 | 13.5 (8.1;18.8) | −3.0 (−11.9;5.8) | −3.1 (−11.7;5.5) | 12.8 (7.6;18.1) | −5.3 (−14.4;3.8) | −5.9 (−14.8;3.0) |
| 2014–2020 | 11.6 (6.2;17.1) | −5.2 (−13.1;2.7) | −5.4 (−13.2;2.4) | 12.5 (6.6;18.5) | −5.8 (−14.1;2.5) | −6.4 (−14.7;1.9) |
| Cohabiting status | ||||||
| Living alone | 8.8 (3.3;14.2) | 0 | 0 | 18.2 (10.7;25.6) | 0 | 0 |
| Living with partner | 14.9 (11.1;18.7) | 6.1 (−0.5;12.7) | 5.8 (−1.1;12.8) | 12.6 (9.0;16.1) | −5.5 (−13.7;2.7) | −8.3 (−16.4;−0.2) * |
| Education level | ||||||
| ISCED 0–2 | 17.0 (9.4;24.6) | 0 | 0 | 21.3 (12.7;29.8) | 0 | 0 |
| ISCED 3 | 13.3 (8.8;17.9) | −3.8 (−12.9;5.3) | −3.1 (−11.9;5.7) | 12.7 (8.2;17.2) | −8.8 (−18.7;1.2) | −8.1 (−17.9;1.7) |
| ISCED 5–6 | 12.9 (5.7;20.1) | −4.3 (−15.0;6.3) | −5.3 (−15.4;4.9) | 10.5 (4.0;17.0) | −10.9 (−21.9;0.1) | −12.1 (−22.8;−1.5) * |
| ISCED 7–8 | 7.2 (0.0;15.1) | −9.9 (−21.1;1.4) | −9.7 (−20.7;1.3) | 11.1 (1.9;20.4) | −10.3 (−23.2;2.7) | −8.8 (−21.5;3.9) |
| Equalized income | ||||||
| Lowest | 15.3 (7.3;23.3) | 0 | 0 | 24.6 (14.9;34.3) | 0 | 0 |
| Second lowest | 18.4 (11.5;25.2) | 3.0 (−7.8;13.8) | 3.2 (−7.6;14.0) | 18.6 (11.7;25.5) | −6.6 (−18.9;5.8) | −12.3 (−24.0;−0.7) * |
| Second highest | 12.4 (6.5;18.3) | −3.0 (−13.2;7.2) | −3.1 (−13.4;7.2) | 10.4 (4.8;16.1) | −14.7 (−26.4;−3.1) * | −18.6 (−29.3;−8.0) * |
| Highest | 8.1 (3.2;12.9) | −7.3 (−16.9;2.3) | −6.6 (−16.5;3.3) | 5.5 (1.5;9.6) | −19.6 (−30.6;−8.6) * | −22.1 (−32.4;−11.9) * |
| Long-term sickness 2 | ||||||
| No sick leave | 11.5 (8.3;14.6) | 0 | 0 | 11.7 (8.5;15.0) | 0 | 0 |
| Sick leave | 28.5 (16.6;40.3) | 16.9 (4.5;29.4) * | 15.4 (2.9;27.9) * | 28.6 (16.6;40.6) | 17.1 (4.6;29.5) * | 15.0 (2.7;27.4) * |
| CCI prior to diagnosis | ||||||
| 0 | 13.5 (10.0;17.0) | 0 | 0 | 12.1 (8.7;15.4) | 0 | 0 |
| 1 | 15.8 (5.0;26.6) | 2.2 (−8.8;13.1) | 2.5 (−8.9;13.9) | 22.7 (10.2;35.2) | 10.4 (−2.1;23.0) | 9.2 (−2.9;21.3) |
| ≥2 | 10.1 (0.0;21.1) | −3.1 (−14.5;8.3) | −3.4 (−15.4;8.7) | 24.2 (6.7;41.8) | 10.1 (−5.9;26.1) | 7.2 (−8.4;22.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maksten, E.F.; Jensen, J.F.; Thomsen, G.; Zenas, D.R.; Jørgensen, M.P.; Udby, L.; Fonager, K.; Severinsen, M.T. Work Ability in Patients with Chronic Myeloid Leukemia: A Danish Nationwide Cohort Study. Cancers 2025, 17, 1585. https://doi.org/10.3390/cancers17091585
Maksten EF, Jensen JF, Thomsen G, Zenas DR, Jørgensen MP, Udby L, Fonager K, Severinsen MT. Work Ability in Patients with Chronic Myeloid Leukemia: A Danish Nationwide Cohort Study. Cancers. 2025; 17(9):1585. https://doi.org/10.3390/cancers17091585
Chicago/Turabian StyleMaksten, Eva Futtrup, Jonas Faartoft Jensen, Gitte Thomsen, Ditte Rechter Zenas, Maren Poulsgaard Jørgensen, Lene Udby, Kirsten Fonager, and Marianne Tang Severinsen. 2025. "Work Ability in Patients with Chronic Myeloid Leukemia: A Danish Nationwide Cohort Study" Cancers 17, no. 9: 1585. https://doi.org/10.3390/cancers17091585
APA StyleMaksten, E. F., Jensen, J. F., Thomsen, G., Zenas, D. R., Jørgensen, M. P., Udby, L., Fonager, K., & Severinsen, M. T. (2025). Work Ability in Patients with Chronic Myeloid Leukemia: A Danish Nationwide Cohort Study. Cancers, 17(9), 1585. https://doi.org/10.3390/cancers17091585






