The Clinical Relevance of Distinguishing Between Simple and Complex Adnexal Cystic Structures by Ultrasound in Peri- and Postmenopause
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
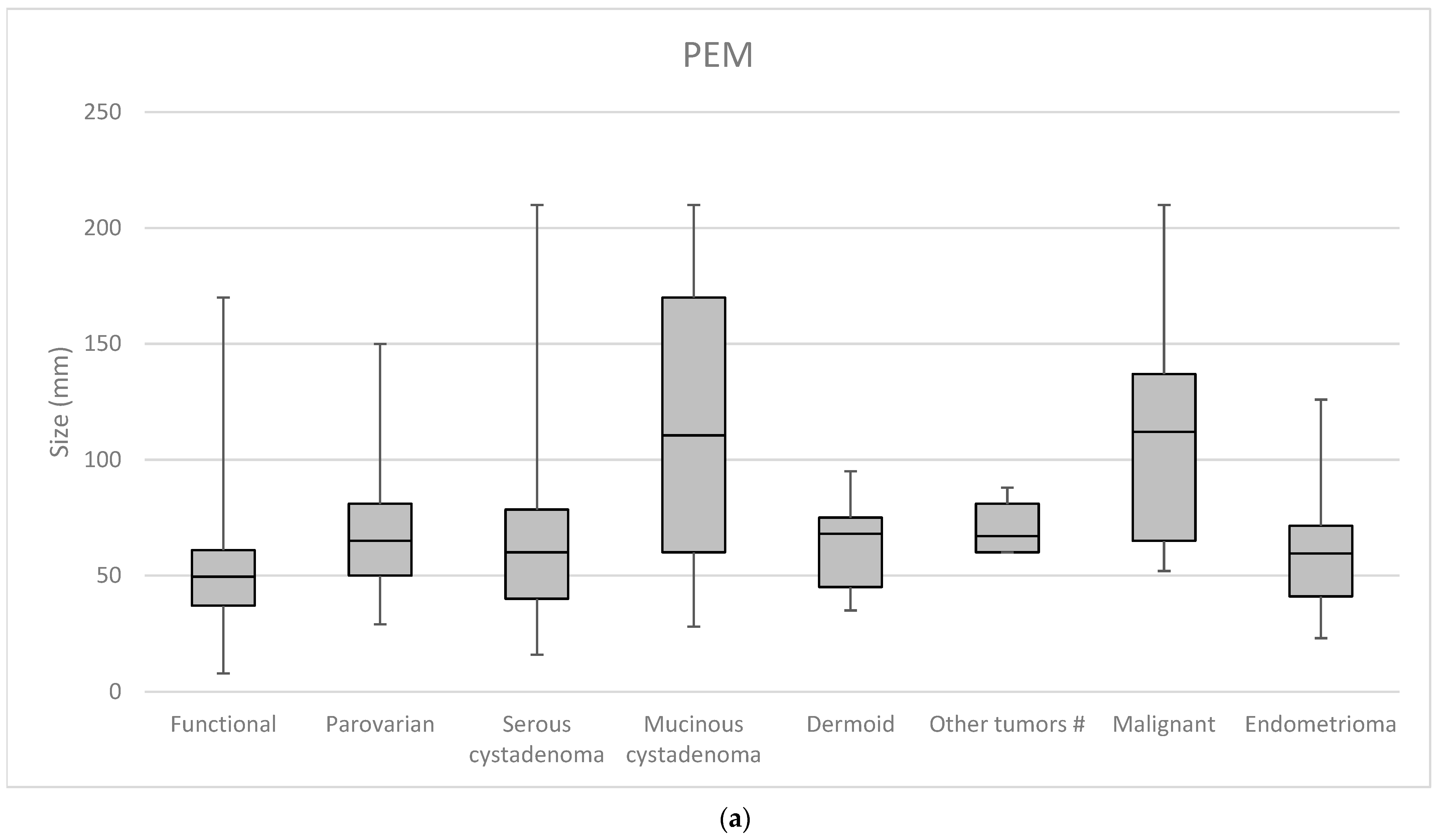
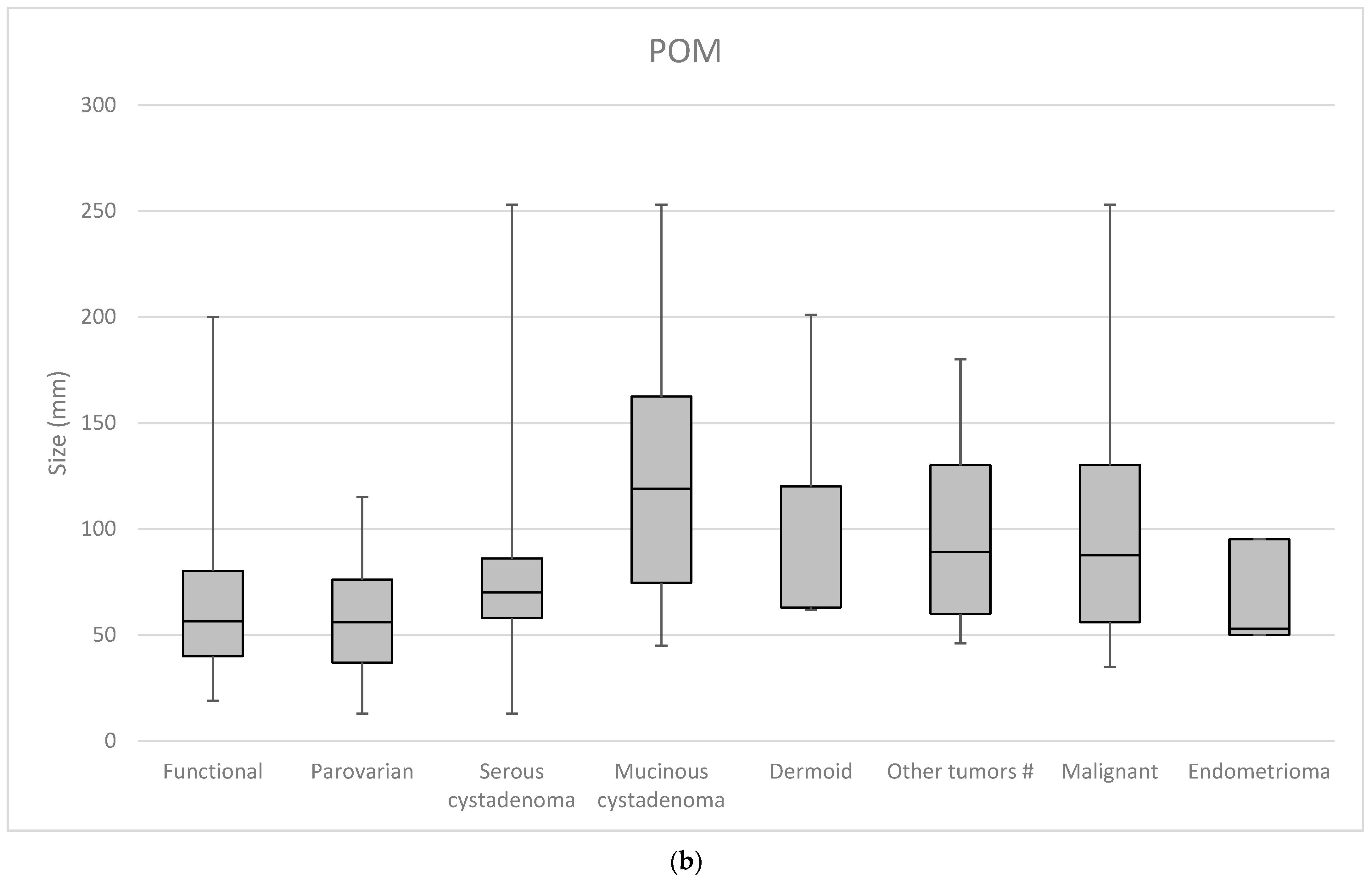
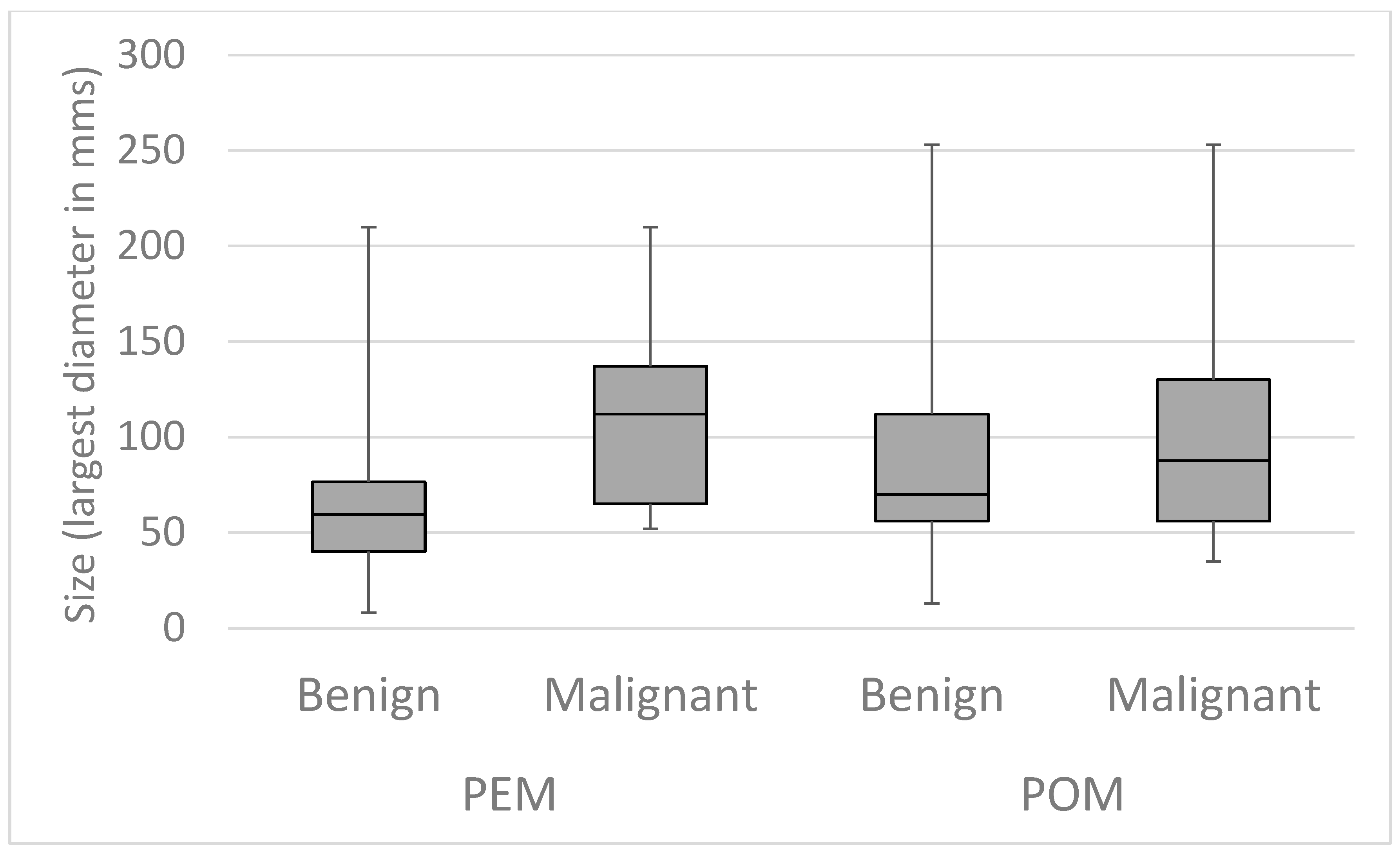
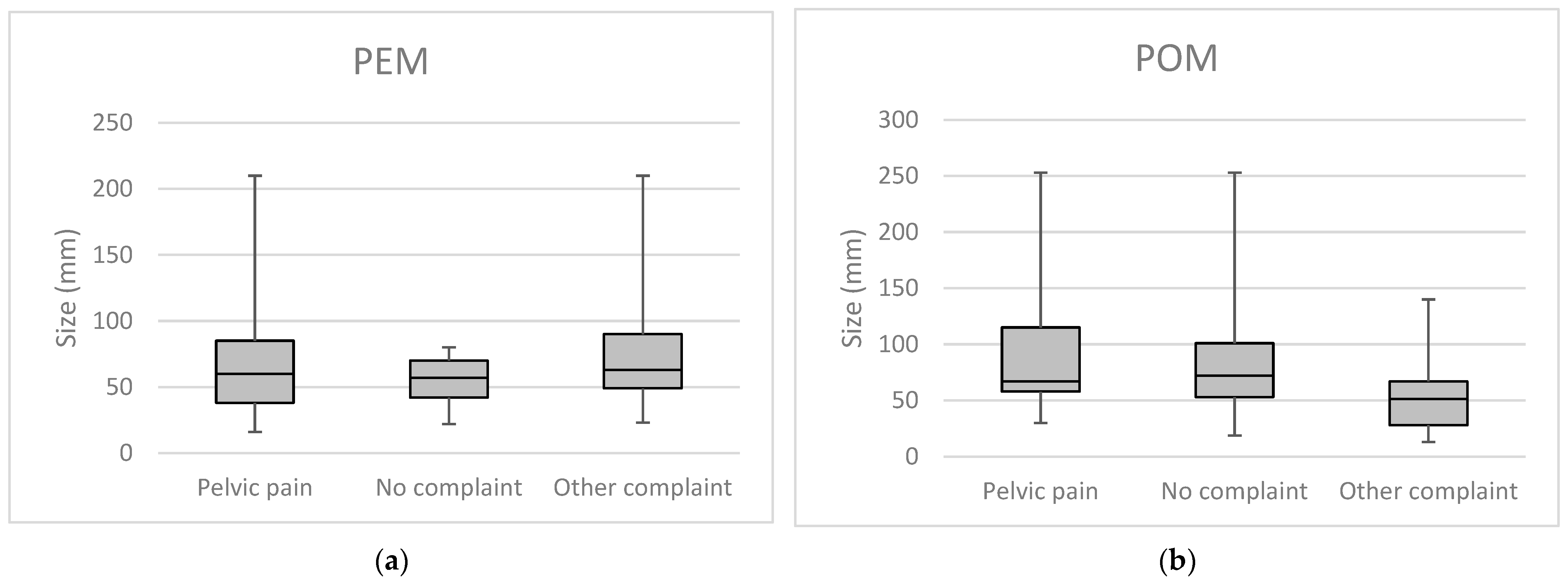
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Menon, U.; Gentry-Maharaj, A.; Hallett, R.; Ryan, A.; Burnell, M.; Sharma, A.; Lewis, S.; Davies, S.; Philpott, S.; Lopes, A.; et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: Results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncol. 2009, 10, 327–340. [Google Scholar] [CrossRef]
- Ekerhovd, E.; Wienerroith, H.; Staudach, A.; Granberg, S. Preoperative assessment of unilocular adnexal cysts by transvaginal ultrasonography: A comparison between ultrasonographic morphologic imaging and histopathologic diagnosis. Am. J. Obs. Gynecol. 2001, 184, 48–54. [Google Scholar] [CrossRef]
- Einhorn, N.; Sjovall, K.; Knapp, R.C.; Hall, P.; Scully, R.E.; Bast, R.C., Jr.; Zurawski, V.R., Jr. Prospective evaluation of serum CA 125 levels for early detection of ovarian cancer. Obs. Gynecol. 1992, 80, 14–18. [Google Scholar] [CrossRef]
- Jacobs, I.J.; Skates, S.J.; MacDonald, N.; Menon, U.; Rosenthal, A.N.; Davies, A.P.; Woolas, R.; Jeyarajah, A.R.; Sibley, K.; Lowe, D.G.; et al. Screening for ovarian cancer: A pilot randomised controlled trial. Lancet 1999, 353, 1207–1210. [Google Scholar] [CrossRef]
- Collins, W.P.; Bourne, T.H.; Campbell, S. Screening strategies for ovarian cancer. Curr. Opin. Obs. Gynecol. 1998, 10, 33–39. [Google Scholar] [CrossRef]
- Iatrakis, G.M.; Zervoudis, S.; Tsikouras, P.; Iatrakis, D.G.; Bothou, A.; Chardavelas, T.; Apostolakopoulos, P.; Ceausu, I.; Galazios, G. A new risk malignancy index to predict ovarian cancer: A bicentric preliminary study. J. Buon. 2018, 23, 1380–1383. [Google Scholar]
- Goldstein, S.R.; Subramanyam, B.; Snyder, J.R.; Beller, U.; Raghavendra, B.N.; Beckman, E.M. The postmenopausal cystic adnexal mass: The potential role of ultrasound in conservative management. Obs. Gynecol. 1989, 73, 8–10. [Google Scholar] [CrossRef]
- Sassone, A.M.; Timor-Tritsch, I.E.; Artner, A.; Westhoff, C.; Warren, W.B. Transvaginal sonographic characterization of ovarian disease: Evaluation of a new scoring system to predict ovarian malignancy. Obs. Gynecol. 1991, 78, 70–76. [Google Scholar]
- Ueland, F.R.; DePriest, P.D.; Pavlik, E.J.; Kryscio, R.J.; van Nagell, J.R., Jr. Preoperative differentiation of malignant from benign ovarian tumors: The efficacy of morphology indexing and Doppler flow sonography. Gynecol. Oncol. 2003, 91, 46–50. [Google Scholar] [CrossRef]
- Granberg, S.; Wikland, M.; Jansson, I. Macroscopic characterization of ovarian tumors and the relation to the histological diagnosis: Criteria to be used for ultrasound evaluation. Gynecol. Oncol. 1989, 35, 139–144. [Google Scholar] [CrossRef]
- Timmerman, D.; Ameye, L.; Fischerova, D.; Epstein, E.; Melis, G.B.; Guerriero, S.; Van Holsbeke, C.; Savelli, L.; Fruscio, R.; Lissoni, A.A.; et al. Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: Prospective validation by IOTA group. BMJ 2010, 341, c6839. [Google Scholar] [CrossRef] [PubMed]
- Tan, P.L.; Willatt, J.M.; Lindsell, D. The ability of ultrasound to detect gynaecological neoplasms and their ultrasound morphological features. Australas. Radiol. 2007, 51, 260–266. [Google Scholar] [CrossRef]
- Kurjak, A.; Prka, M.; Arenas, J.M.; Sparac, V.; Merce, L.T.; Corusic, A.; Ivancic-Kosuta, M. Three-dimensional ultrasonography and power Doppler in ovarian cancer screening of asymptomatic peri- and postmenopausal women. Croat. Med. J. 2005, 46, 757–764. [Google Scholar]
- Timor-Tritsch, I.E.; Goldstein, S.R. The complexity of a “complex mass” and the simplicity of a “simple cyst”. J. Ultrasound. Med. 2005, 24, 255–258. [Google Scholar] [CrossRef] [PubMed]
- Pavlik, E.J.; Ueland, F.R.; Miller, R.W.; Ubellacker, J.M.; DeSimone, C.P.; Elder, J.; Hoff, J.; Baldwin, L.; Kryscio, R.J.; van Nagell, J.R.J. Frequency and Disposition of Ovarian Abnormalities Followed With Serial Transvaginal Ultrasonography. Obstet. Gynecol. 2013, 122, 210–217. [Google Scholar] [CrossRef]
- Van Calster, B.; Timmerman, D.; Valentin, L.; McIndoe, A.; Ghaem-Maghami, S.; Testa, A.C.; Vergote, I.; Bourne, T. Triaging women with ovarian masses for surgery: Observational diagnostic study to compare RCOG guidelines with an International Ovarian Tumour Analysis (IOTA) group protocol. BJOG 2012, 119, 662–671. [Google Scholar] [CrossRef]
- Kaijser, J.; Bourne, T.; Valentin, L.; Sayasneh, A.; Van Holsbeke, C.; Vergote, I.; Testa, A.C.; Franchi, D.; Van Calster, B.; Timmerman, D. Improving strategies for diagnosing ovarian cancer: A summary of the International Ovarian Tumor Analysis (IOTA) studies. Ultrasound Obs. Gynecol. 2013, 41, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Van Calster, B.; Van Hoorde, K.; Valentin, L.; Testa, A.C.; Fischerova, D.; Van Holsbeke, C.; Savelli, L.; Franchi, D.; Epstein, E.; Kaijser, J.; et al. Evaluating the risk of ovarian cancer before surgery using the ADNEX model to differentiate between benign, borderline, early and advanced stage invasive, and secondary metastatic tumours: Prospective multicentre diagnostic study. BMJ 2014, 349, g5920. [Google Scholar] [CrossRef]
- Sayasneh, A.; Ferrara, L.; De Cock, B.; Saso, S.; Al-Memar, M.; Johnson, S.; Kaijser, J.; Carvalho, J.; Husicka, R.; Smith, A.; et al. Evaluating the risk of ovarian cancer before surgery using the ADNEX model: A multicentre external validation study. Br. J. Cancer 2016, 115, 542–548. [Google Scholar] [CrossRef]
- Meys, E.M.J.; Jeelof, L.S.; Achten, N.M.J.; Slangen, B.F.M.; Lambrechts, S.; Kruitwagen, R.; Van Gorp, T. Estimating risk of malignancy in adnexal masses: External validation of the ADNEX model and comparison with other frequently used ultrasound methods. Ultrasound Obs. Gynecol. 2017, 49, 784–792. [Google Scholar] [CrossRef]
- Padilla, L.A.; Radosevich, D.M.; Milad, M.P. Accuracy of the pelvic examination in detecting adnexal masses. Obs. Gynecol. 2000, 96, 593–598. [Google Scholar] [CrossRef]
- Hartge, P.; Hayes, R.; Reding, D.; Sherman, M.E.; Prorok, P.; Schiffman, M.; Buys, S. Complex ovarian cysts in postmenopausal women are not associated with ovarian cancer risk factors: Preliminary data from the prostate, lung, colon, and ovarian cancer screening trial. Am. J. Obs. Gynecol. 2000, 183, 1232–1237. [Google Scholar] [CrossRef]
- Bailey, C.L.; Ueland, F.R.; Land, G.L.; DePriest, P.D.; Gallion, H.H.; Kryscio, R.J.; van Nagell, J.R., Jr. The malignant potential of small cystic ovarian tumors in women over 50 years of age. Gynecol. Oncol. 1998, 69, 3–7. [Google Scholar] [CrossRef]
- Curtin, J.P. Management of the adnexal mass. Gynecol. Oncol. 1994, 55, S42–S46. [Google Scholar] [CrossRef]
- Reimer, T.; Gerber, B.; Muller, H.; Jeschke, U.; Krause, A.; Friese, K. Differential diagnosis of peri- and postmenopausal ovarian cysts. Maturitas 1999, 31, 123–132. [Google Scholar] [CrossRef]
- Owens, O.J.; Stewart, C.; Leake, R.E.; McNicol, A.M. A comparison of biochemical and immunohistochemical assessment of EGFR expression in ovarian cancer. Anticancer Res. 1992, 12, 1455–1458. [Google Scholar]
- Scambia, G.; Benedetti-Panici, P.; Ferrandina, G.; Distefano, M.; Salerno, G.; Romanini, M.E.; Fagotti, A.; Mancuso, S. Epidermal growth factor, oestrogen and progesterone receptor expression in primary ovarian cancer: Correlation with clinical outcome and response to chemotherapy. Br. J. Cancer 1995, 72, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, I.; Oram, D.; Fairbanks, J.; Turner, J.; Frost, C.; Grudzinskas, J.G. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br. J. Obs. Gynaecol. 1990, 97, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Koonings, P.P.; Campbell, K.; Mishell, D.R., Jr.; Grimes, D.A. Relative frequency of primary ovarian neoplasms: A 10-year review. Obs. Gynecol. 1989, 74, 921–926. [Google Scholar] [CrossRef]
- Modesitt, S.C.; Pavlik, E.J.; Ueland, F.R.; DePriest, P.D.; Kryscio, R.J.; van Nagell, J.R., Jr. Risk of malignancy in unilocular ovarian cystic tumors less than 10 centimeters in diameter. Obs. Gynecol. 2003, 102, 594–599. [Google Scholar] [CrossRef]
- Osmers, R.G.; Osmers, M.; von Maydell, B.; Wagner, B.; Kuhn, W. Evaluation of ovarian tumors in postmenopausal women by transvaginal sonography. Eur. J. Obs. Gynecol. Reprod. Biol. 1998, 77, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Auslender, R.; Atlas, I.; Lissak, A.; Bornstein, J.; Atad, J.; Abramovici, H. Follow-up of small, postmenopausal ovarian cysts using vaginal ultrasound and CA-125 antigen. J. Clin. Ultrasound 1996, 24, 175–178. [Google Scholar] [CrossRef]
- Di Legge, A.; Testa, A.C.; Ameye, L.; Van Calster, B.; Lissoni, A.A.; Leone, F.P.; Savelli, L.; Franchi, D.; Czekierdowski, A.; Trio, D.; et al. Lesion size affects diagnostic performance of IOTA logistic regression models, IOTA simple rules and risk of malignancy index in discriminating between benign and malignant adnexal masses. Ultrasound Obs. Gynecol. 2012, 40, 345–354. [Google Scholar] [CrossRef]
- Landolfo, C.; Bourne, T.; Froyman, W.; Van Calster, B.; Ceusters, J.; Testa, A.C.; Wynants, L.; Sladkevicius, P.; Van Holsbeke, C.; Domali, E.; et al. Benign descriptors and ADNEX in two-step strategy to estimate risk of malignancy in ovarian tumors: Retrospective validation in IOTA5 multicenter cohort. Ultrasound Obs. Gynecol. 2023, 61, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Osmers, R.G.; Osmers, M.; von Maydell, B.; Wagner, B.; Kuhn, W. Preoperative evaluation of ovarian tumors in the premenopause by transvaginosonography. Am. J. Obs. Gynecol. 1996, 175, 428–434. [Google Scholar] [CrossRef]
- Levine, D.; Brown, D.L.; Andreotti, R.F.; Benacerraf, B.; Benson, C.B.; Brewster, W.R.; Coleman, B.; Depriest, P.; Doubilet, P.M.; Goldstein, S.R.; et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology 2010, 256, 943–954. [Google Scholar] [CrossRef]
- Lasher, A.; Harris, L.E.; Solomon, A.L.; Harbin, L.M.; Raby, L.; Dietrich, C.S.; Kryscio, R.J.; van Nagell, J.R.; Pavlik, E.J. Variables Associated With Resolution and Persistence of Ovarian Cysts. Obstet. Gynecol. 2023, 142, 1293–1301. [Google Scholar] [CrossRef]
- Liu, Y.N.; Tan, X.; Xiong, W.; Dong, X.; Liu, J.; Wang, Z.L.; Chen, H.X. Natural history and malignant potential of simple ovarian cysts in postmenopausal women: A systematic review and meta-analysis. Menopause 2023, 30, 559–565. [Google Scholar] [CrossRef]
- Bast, R.C., Jr.; Klug, T.L.; St John, E.; Jenison, E.; Niloff, J.M.; Lazarus, H.; Berkowitz, R.S.; Leavitt, T.; Griffiths, C.T.; Parker, L.; et al. A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. N. Engl. J. Med. 1983, 309, 883–887. [Google Scholar] [CrossRef]
- Jacobs, I.; Bast, R.C., Jr. The CA 125 tumour-associated antigen: A review of the literature. Hum. Reprod. 1989, 4, 1–12. [Google Scholar] [CrossRef]
- Conway, C.; Zalud, I.; Dilena, M.; Maulik, D.; Schulman, H.; Haley, J.; Simonelli, K. Simple cyst in the postmenopausal patient: Detection and management. J. Ultrasound. Med. 1998, 17, 369–372, quiz 373–364. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, D.; Moerman, P.; Vergote, I. Meigs’ syndrome with elevated serum CA 125 levels: Two case reports and review of the literature. Gynecol. Oncol. 1995, 59, 405–408. [Google Scholar] [CrossRef]
- Kaijser, J.; Van Gorp, T.; Smet, M.E.; Van Holsbeke, C.; Sayasneh, A.; Epstein, E.; Bourne, T.; Vergote, I.; Van Calster, B.; Timmerman, D. Are serum HE4 or ROMA scores useful to experienced examiners for improving characterization of adnexal masses after transvaginal ultrasonography? Ultrasound Obs. Gynecol. 2014, 43, 89–97. [Google Scholar] [CrossRef]
- Montagnana, M.; Danese, E.; Ruzzenente, O.; Bresciani, V.; Nuzzo, T.; Gelati, M.; Salvagno, G.L.; Franchi, M.; Lippi, G.; Guidi, G.C. The ROMA (Risk of Ovarian Malignancy Algorithm) for estimating the risk of epithelial ovarian cancer in women presenting with pelvic mass: Is it really useful? Clin. Chem. Lab. Med. 2011, 49, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Kaijser, J.; Van Gorp, T.; Van Hoorde, K.; Van Holsbeke, C.; Sayasneh, A.; Vergote, I.; Bourne, T.; Timmerman, D.; Van Calster, B. A comparison between an ultrasound based prediction model (LR2) and the risk of ovarian malignancy algorithm (ROMA) to assess the risk of malignancy in women with an adnexal mass. Gynecol. Oncol. 2013, 129, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Valentin, L.; Jurkovic, D.; Van Calster, B.; Testa, A.; Van Holsbeke, C.; Bourne, T.; Vergote, I.; Van Huffel, S.; Timmerman, D. Adding a single CA 125 measurement to ultrasound imaging performed by an experienced examiner does not improve preoperative discrimination between benign and malignant adnexal masses. Ultrasound Obs. Gynecol. 2009, 34, 345–354. [Google Scholar] [CrossRef]
- Shen, L.; Sadowski, E.A.; Gupta, A.; Maturen, K.E.; Patel-Lippmann, K.K.; Zafar, H.M.; Kamaya, A.; Antil, N.; Guo, Y.; Barroilhet, L.M.; et al. The Ovarian-Adnexal Reporting and Data System (O-RADS) US Score Effect on Surgical Resection Rate. Radiology 2024, 313, e240044. [Google Scholar] [CrossRef]
- Suh-Burgmann, E.J.; Hung, Y.-Y.; Schmittdiel, J.A. Ovarian cancer risk among older patients with stable adnexal masses. Am. J. Obstet. Gynecol. 2024, 231, 440.e1–440.e7. [Google Scholar] [CrossRef]

| PEM Simplex | PEM Complex | POM Simplex | POM Complex | |||||
|---|---|---|---|---|---|---|---|---|
| <5 cm | ≥5 cm | <5 cm | ≥5 cm | <5 cm | ≥5 cm | <5 cm | ≥5 cm | |
| Functional cysts | ||||||||
| Corp. lut. cyst. hem. | 8 (25.00%) | 5 (12.20%) | 6 (20.69%) | 12 (12.90%) | 2 (13.33%) | 5 (4.17%) | ||
| Follicular cyst | 5 (15.63%) | 6 (14.63%) | 6 (20.69%) | 2 (2.15%) | 1 (11.11%) | 2 (1.67%) | ||
| Parovarian cysts | 1 (3.13%) | 11 (26.83%) | 3 (10.34%) | 3 (3.23%) | 2 (22.22%) | 5 (12.50%) | 3 (20.00%) | 5 (4.17%) |
| Benign | ||||||||
| Cystadenoma serosum | 16 (50.00%) | 16 (39.02%) | 3 (10.34%) | 21 (22.58%) | 5 (55.56%) | 27 (67.50%) | 4 (26.67%) | 34 (28.33%) |
| Cystadenoma mucinosum | 1 (3.13%) | 2 (4.88%) | 1 (3.45%) | 10 (10.75%) | 4 (10.00%) | 2 (13.33%) | 18 (15.00%) | |
| Dermoid | 4 (13.79%) | 10 (10.75%) | 5 (4.17%) | |||||
| Endometriosis | 1 (3.13%) | 1 (2.44%) | 6 (20.69%) | 12 (12.90%) | 3 (2.50%) | |||
| Fibroid | 3 (3.23%) | 2 (5.00%) | 1 (6.67%) | 7 (5.83%) | ||||
| Hydrosalpinx | 1 (11.11%) | 1 (2.50%) | 2 (1.67%) | |||||
| Struma ovarii | 1 (1.08%) | 1 (0.83%) | ||||||
| Brenner tu. | 3 (3.23%) | 2 (1.67%) | ||||||
| Malignant | 16 (17.20%) | 1 (2.50%) | 3 (20.00%) | 36 (30.00%) | ||||
| Risk Factors | PEM Simplex | PEM Complex | POM Simplex | POM Complex | Total (% of Total Cases) | ||||
|---|---|---|---|---|---|---|---|---|---|
| <5 cm | ≥5 cm | <5 cm | ≥5 cm | <5 cm | ≥5 cm | <5 cm | ≥5 cm | ||
| Parity | |||||||||
| Nulliparous | 2 (6%) | 10 (24%) | 6 (21%) | 14 (15%) | 1 (11%) | 1 (3%) | 3 (20%) | 20 (17%) | 57 (15.04%) |
| 1–2 children | 20 (63%) | 23 (56%) | 19 (66%) | 65 (70%) | 6 (67%) | 31 (78%) | 8 (53%) | 78 (65%) | 250 (65.96%) |
| 3–4 children | 10 (31%) | 8 (20%) | 3 (10%) | 13 (14%) | 2 (22%) | 7 (18%) | 4 (27%) | 20 (17%) | 67 (17.68%) |
| ≥5 children | 1 (3%) | 1 (1%) | 1 (3%) | 2 (2%) | 5 (1.32%) | ||||
| Family history of ovarian cancer | 2 (6%) | 1 (3%) | 1 (1%) | 4 (1.06%) | |||||
| Previous pelvic surgery | |||||||||
| Hysterectomy | 5 (16%) | 4 (10%) | 3 (10%) | 17 (18%) | 3 (33%) | 2 (5%) | 4 (27%) | 33 (28%) | 71 (18.73%) |
| Adnexectomy | 1 (3%) | 1 (2%) | 1 (3%) | 8 (9%) | 1 (7%) | 2 (2%) | 14 (3.69%) | ||
| Laparotomy | 1 (3%) | 4 (10%) | 1 (3%) | 10 (11%) | 1 (3%) | 5 (4%) | 22 (5.80%) | ||
| Punction | 3 (7%) | 1 (3%) | 1 (1%) | 1 (3%) | 1 (7%) | 7 (1.85%) | |||
| No previous surgery | 25 (78%) | 29 (71%) | 23 (79%) | 57 (61%) | 6 (67%) | 36 (90%) | 9 (60%) | 80 (67%) | 265 (69.92%) |
| Total (n) | 32 | 41 | 29 | 93 | 9 | 40 | 15 | 120 | 379 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erdodi, B.; Szollosi, G.J.; Toth, Z.; Krasznai, Z.T.; Jakab, A. The Clinical Relevance of Distinguishing Between Simple and Complex Adnexal Cystic Structures by Ultrasound in Peri- and Postmenopause. Cancers 2025, 17, 1370. https://doi.org/10.3390/cancers17081370
Erdodi B, Szollosi GJ, Toth Z, Krasznai ZT, Jakab A. The Clinical Relevance of Distinguishing Between Simple and Complex Adnexal Cystic Structures by Ultrasound in Peri- and Postmenopause. Cancers. 2025; 17(8):1370. https://doi.org/10.3390/cancers17081370
Chicago/Turabian StyleErdodi, Balazs, Gergo Jozsef Szollosi, Zoltan Toth, Zoard Tibor Krasznai, and Attila Jakab. 2025. "The Clinical Relevance of Distinguishing Between Simple and Complex Adnexal Cystic Structures by Ultrasound in Peri- and Postmenopause" Cancers 17, no. 8: 1370. https://doi.org/10.3390/cancers17081370
APA StyleErdodi, B., Szollosi, G. J., Toth, Z., Krasznai, Z. T., & Jakab, A. (2025). The Clinical Relevance of Distinguishing Between Simple and Complex Adnexal Cystic Structures by Ultrasound in Peri- and Postmenopause. Cancers, 17(8), 1370. https://doi.org/10.3390/cancers17081370







