Simple Summary
Bladder cancer is a common type of cancer, and in its metastatic form, it has a poor prognosis. Despite treatment options, a subset of patients with metastatic bladder cancer do not receive systemic oncological treatment. The aim of this study was to explore the reasons for abstaining from treatment. Patients were identified through a coding system, and patient data were retrieved from the electronic health records system. Among a total of 159 patients with metastatic bladder cancer, the most common reasons were poor general condition, patient preference, and decreased renal function. Furthermore, the study sought to investigate the characteristics of the patients who turned out to be long-term survivors despite the lack of treatment. The study can bring valuable information to the treatment decision and is underscoring the need for a nuanced approach and patient-tailored treatment strategies to improve the overall survival from metastatic bladder cancer.
Abstract
Background: A subset of patients with locally advanced or metastatic bladder cancer (la/mBC) do not receive systemic oncological treatment. The reasons for refraining from systemic treatment are poorly investigated, as are the characteristics of patients who turn out to be long-term survivors despite lack of treatment. Methods: This retrospective observational cohort study included patients with registration compatible with la/mBC who did not undergo systemic treatment. They were seen at a single tertiary university hospital covering one of 5 Danish regions in the study period from 1 January 2012 until 31 December 2022. Patients were identified through a coding system, and detailed patient information was obtained in the electronic medical records. Results: The initial study population consisted of 472 patients registered with la/mBC according to codes in the patient registries but with no registration of systemic oncological treatment. Out of the total cohort, 159 patients were registered correctly, while the rest of the population were excluded due to misclassification, as 10.8% did not have la/mBC and 55.5% had received oncological treatment. Among correctly registered patients, the median overall survival was 2.6 months (95% CI 0.26; 4.94) from being diagnosed with la/mBC. The most common reasons for lack of treatment were poor general condition (74.2%), patient preference (19.5%), and poor renal function (11.9%). Conclusions: Our study found that a significant amount of patients in a cohort of suspected la/mBC not undergoing treatment either received oncological treatment or did not have la/mBC, demonstrating a misclassification in the system. This should be taken into consideration when evaluating data about survival time for this patient group. The poorest survival of untreated la/mBC is associated with a high tumor burden and specifically liver metastasis.
1. Introduction
Bladder cancer is among the top ten most prevalent cancer diagnoses globally, with approximately 550,000 new cases annually [1,2]. In Denmark, about 2000 patients are diagnosed with bladder tumors each year, and around half of these have invasive tumors, whereas roughly half of them are muscle-invasive bladder cancer (MIBC) [3]. Up to 20% of patients present with metastatic or unresectable disease [4,5]. Moreover, approximately 50% of the patients who undergo curative, intended local radical treatment for MIBC will subsequently develop metastases [6,7]. Metastases originating from bladder cancer commonly manifest in lymph nodes, bones, lungs, and liver [8].
Patients with locally advanced or metastatic bladder cancer (la/mBC), including relapse after prior cystectomy or inoperable relapse after radiotherapy, are generally considered incurable. Theoretically, these patients are only candidates for palliative systemic oncological treatment [6,9].
Previous studies have found that more than 50% of patients diagnosed with la/mBC receive no systemic treatment [10,11,12,13]. The decision to not initiate treatment is often based on several factors like poor performance status, comorbidities, and patient preferences, but literature about the reasons for foregoing treatment is sparse. Additionally, the prevalence and characteristics of patients not undergoing treatment have previously only sparsely been described [14,15].
Interestingly, a proportion of patients with metastatic disease are found to have a fair overall survival even without relevant systemic treatment [16]. The underlying reasons for this unexpected survival trend remain inadequately investigated.
This retrospective single-center observational cohort study was conducted in order to investigate the prevalence, characteristics, and overall survival for patients with metastatic or locally advanced bladder cancer who refrained from receiving systemic oncological treatment. It raises questions about the found fair overall survival time. Additionally, the study sought to explore the reasons for why treatment was withheld and thereby provide valuable insights into the clinical landscape of untreated la/mBC patients.
2. Materials and Methods
2.1. Data Sources and Study Population
The patients in this study were diagnosed with bladder cancer and treated at the Department of Urology in Aarhus University Hospital between January 2012 and December 2022. Patients with suspected bladder cancer are referred to the Department of Urology, where the diagnostics are performed. Every patient with a disease suitable for surgery will be treated at the department, while patients who are considered not curable will be referred to the Department of Oncology for assessment. Aarhus University Hospital has approximately 81,000 annual admissions and serves as a regional center for the surgical treatment of bladder cancer, performing around 100 cystectomies each year.
In Denmark, each diagnosis and medical procedure is systematically cataloged within the electronic health records system. These entries are identified by a specific diagnosis code and procedure code, respectively. Furthermore, diagnoses derived from histopathological examinations are categorized by pathologists employing the Systematized Nomenclature of Medicine (SNOMED) and archived in Patobank, which constitutes an integral component of the Danish Pathology Register.
The diagnostic codes for bladder cancer or metastasis combined with a procedure code indicating the absence of treatment with chemotherapy or immunotherapy BWHA*, BOHJI9H*, or BOHJ19J* were used to identify the cohort. The specific diagnostic codes are seen in Table 1.

Table 1.
Distribution of the total of 472 patients found by different codes by the algorithms.
Danish Data Protection Agency approval was granted before data extraction (1-45-70-104-22). There were no direct patient interactions in relation to the project.
2.2. Outcome and Statistical Analysis
The reasoning that led to the decision to not initiate systemic oncological treatment for each patient was documented according to predefined categories. In addition, it was registered if the patient was assessed by an oncologist and if any palliative treatment, besides systemic treatment, was given.
Only patients who had a survival of 3 months or more from diagnosis of locally advanced or metastatic bladder cancer were registered with detailed information about gender, age, height, weight, ASA classification, serum creatinine, and comorbidity status. The date of initial la/mBC diagnosis and specific details regarding metastatic disease were listed. For patients with a known history of urothelial disease, data about their primary disease were recorded as well.
Descriptive analyses included medians and interquartile ranges (IQRs) or 95% confidence intervals (95% CIs) for continuous variables and sample sizes and frequencies for categorical variables.
The Kaplan–Meier method was used for survival analyses. Overall survival (OS) was calculated from the time of la/mBC diagnosis until death from any cause or, if the patient was still alive, the last time the electronic patient record was evaluated.
3. Results
A total of 472 patients were identified as the study population; see Table 1.
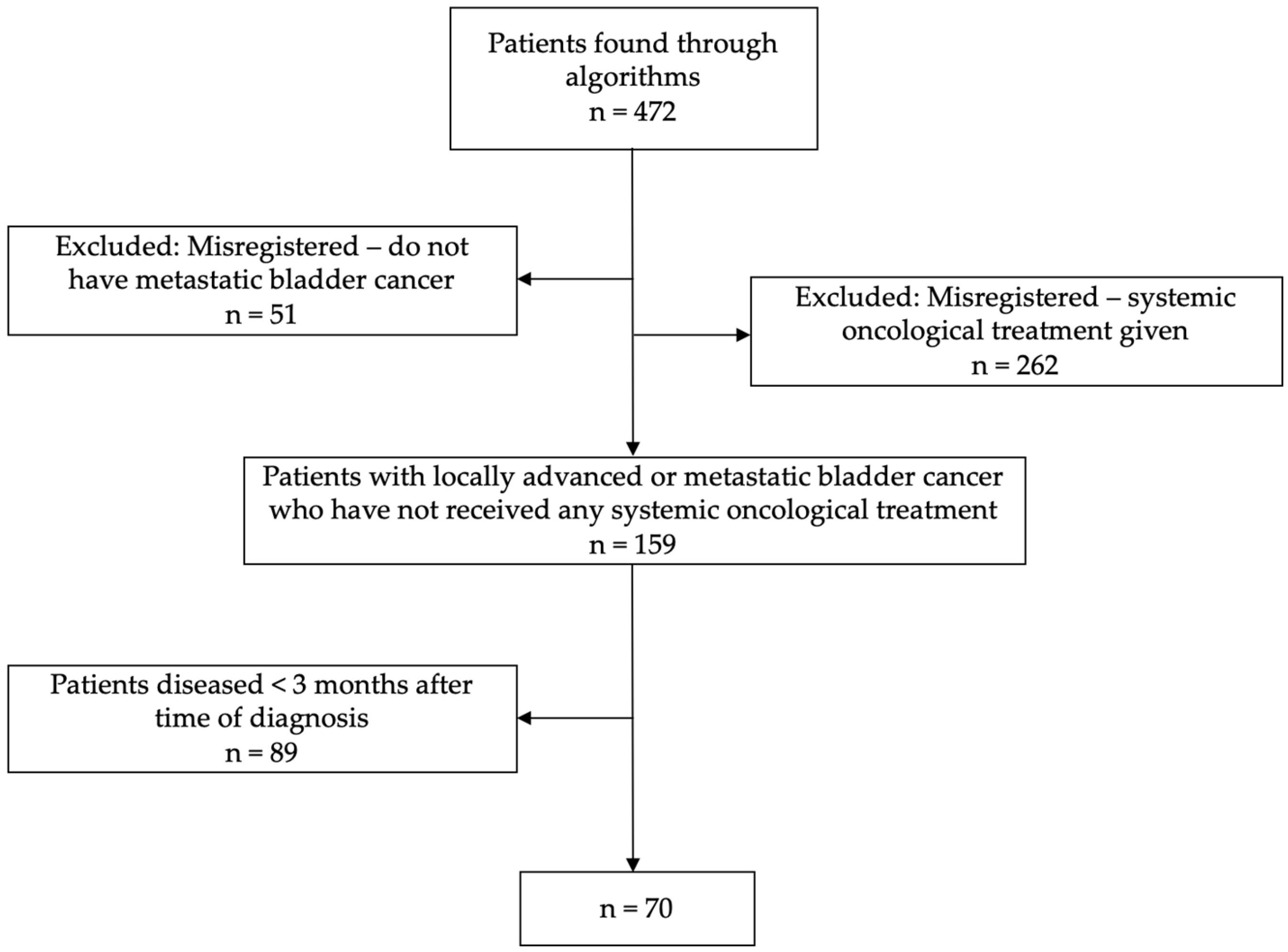
Despite their initial classification as not having undergone any form of systemic oncological treatment, 262 (55.5%) of these patients had received chemotherapy and/or immunotherapy subsequent to their date of diagnosis and were excluded from the cohort. Additionally, 51 (10.8%) out of the initial 472 patients were excluded as they did not have locally advanced or metastatic bladder cancer. These patients were predominantly patients with lymph node disease, who had undergone radical cystectomy or radiotherapy without disease relapse during the follow-up time; see the flowchart in Figure 1.
Figure 1.
Flowchart showing the population enrolled, reasons for exclusion, and final study population.
In the entire cohort of 472 patients, a total of 159 patients diagnosed with locally advanced or metastatic bladder cancer had not undergone any form of systemic oncological treatment.
Among the 159 patients, 66.7% were assessed for treatment eligibility by an oncologist, while for the remaining patients, the decision of lack of treatment was made by the urologist or/and the patient itself. Some patients received local palliative treatment, as 29.6% had palliative treatment targeted at metastases and 4.4% targeted the bladder.
The most common reasons for lack of treatment were poor general condition (74.2%), the patients’ personal preferences (19.5%), and poor renal function (11.9%), as outlined in Table 2. For 77% of the patients, one single reason was given, while the remaining 23% of patients had two or three reasons for not undergoing treatment. Among patients surviving less than three months (89 patients), 89.9% were seen in too poor general condition to initiate chemotherapy, and 13.3% had no wish to receive treatment either. The respective numbers for the group surviving for more than three months (70 patients) were 54.3% and 27.1%.

Table 2.
Reasons for lack of systemic oncological treatment in 159 patients with locally advanced or metastatic bladder cancer.
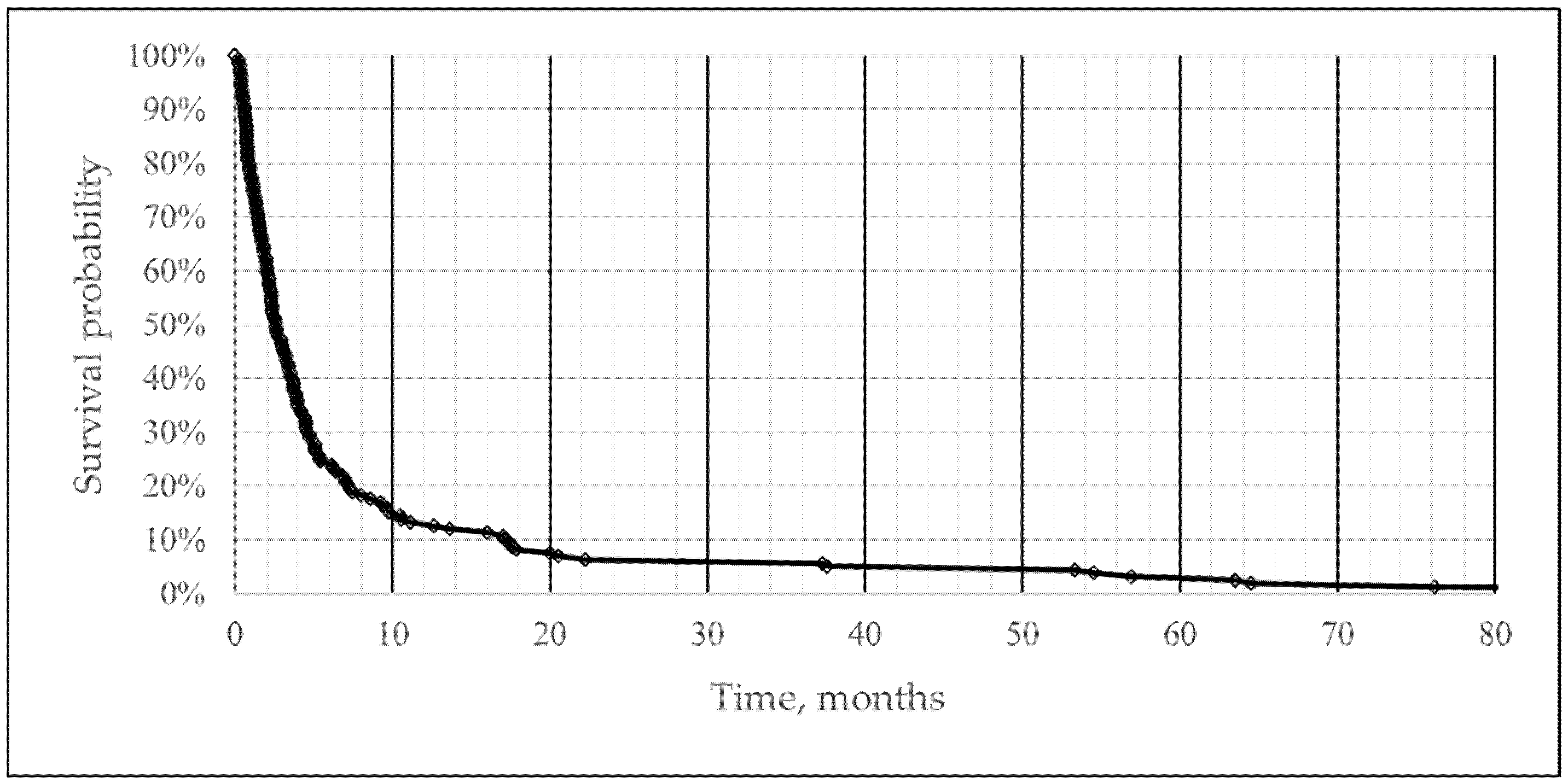
The median OS was 2.6 months (95% CI 0.26; 4.94) after being diagnosed with la/mBC. The 3-, 6-, and 12-month overall survival was 44%, 24%, and 13%. A total of five patients had not died by the end of the study follow-up time. The survival curve is graphically depicted in Figure 2.
Figure 2.
Survival curve illustrating survival from diagnosis of locally advanced bladder cancer or metastatic bladder cancer to death in 159 patients not receiving systemic oncological treatment.
From the 159 patients, a subset of 89 individuals died within the initial three months following their diagnosis. Consequently, a group of 70 patients represented patients diagnosed with locally advanced or metastatic bladder cancer who survived more than three months without undergoing any systemic oncological treatment. The characteristics of the patients are presented in Table 3. Among those patients, 54.3% had lymph node metastasis, 28.6% had lung metastases, 25.7% had bone metastases, and 20% had liver metastases.

Table 3.
Characteristics of the 70 patients with locally advanced or metastatic bladder cancer surviving for more than 3 months post diagnosis.
The majority of the 70 patients, 50 patients (71.4%), were initially diagnosed with local disease and subsequently underwent curatively intended treatment such as cystectomy (72%), radiotherapy (16%), or other forms of local tumor treatment (10%). Furthermore, 15.7% had received neoadjuvant chemotherapy before cystectomy. The metastatic pattern for disease relapse is seen in Table 4 as well as other characteristics of the patients.

Table 4.
Data for the 50 patients initially diagnosed with local disease.
4. Discussion
This retrospective study was a real-world, community-based investigation of patients diagnosed with la/mBC for an 11-year period. It can be assumed to reflect the general population of la/mBC nationally and in analogous countries globally, rendering the study data relevant and applicable on a larger scale.
Initially, 472 patients were identified in the register; however, 313 patients were misclassified either by diagnosis or by the administered treatment. Consequently, the final study population consisted of 159 patients. Prior to this study, data indicated that a large population of patients with la/mBC without oncological treatment were long-term survivors [16]. This study is questioning that observation, as the prolonged survival time might be caused by the misclassification.
The primary factor contributing to the lack of treatment in the 159 patients was a generally poor physical condition (74.4%). Notably, patients with a compromised general condition did often present with a larger tumor burden compared to those in better physical health. Omission of treatment was seldom exclusively due to comorbidities, except for cases involving decreased renal function, which aligns with existing literature [14,17]. In 19.5% of cases, patients expressed disinterest in systemic treatment, frequently coinciding with assessments of poor general condition rendering them unfit for treatment. The prevailing reasons for lack of treatment observed in this study closely align with findings from comparable research [15]. To our knowledge, no other study reports similar insights into the reasons for abstaining from treatment.
Examining the subgroup of long-term survivors, a notable increase in the proportion of cases where lack of treatment was attributed to the patient’s own wish and age was observed and less to poor general condition, compared to the overall study population.
The long-term survivors had a lower share of liver metastases, aligning with the established understanding that liver metastases serve as an adverse prognostic factor for overall survival [18]. Although the overall metastatic patterns were comparable, long-term survivors generally presented with fewer metastases, while patients with the shortest survival time often displayed severely disseminated disease. Furthermore, local directed treatments for metastases, such as radiotherapy or surgical resection, were more frequent among the patients who ended up with prolonged survival. This indicates the feasibility of local treatment of a single solitary metastasis, a strategy probably ineffective in cases of widespread metastatic disease.
The gender distribution observed in this study closely mirrored the overall la/mBC population in Denmark [19]. Interestingly, the median age at time of diagnosis was notably higher than that of patients initiating chemotherapy (77 vs. 69 years) [19]. The study shed light on the age-dependent increase in the proportion of untreated patients, a predictable observation considering the confluence of declining functional status and age-related comorbidities [12,14,20].
Age was registered only as a contributing factor (9%), suggesting that the decision to forego treatment may be influenced by age-related declines in general physical condition and renal function. While advanced age is conventionally deemed a relative contraindication for chemotherapy-based treatment, the existing evidence does not robustly support the routine exclusion of elderly patients based solely on age [17,21]. Additionally, age-related changes in patient preferences and concerns about treatment toxicity and the risk–benefit ratio of treatment may play a role.
That the median survival time is between 3 and 6 months for metastatic bladder cancer for patients not undergoing systemic oncological treatment but receiving best supportive care has previously been published [9,22,23]. Notably, this study illustrates the poor prognosis associated with la/mBC, highlighting a median survival time of 2.6 months (95% CI 0.26; 4.94) post-diagnosis for patients who do not receive treatment, aligning closely with findings from a comparable Danish study featuring a similar patient population [15]. Independent prognostic factors contributing to poor survival include a poor performance status and visceral metastases [24]. Patients with exclusively lymph node metastases exhibit a more favorable survival outcome [25].
A strength of this study is the real-world design, encapsulating an authentic patient population. The complete inclusion of patients, facilitated by pathology and diagnosis coding practices in Denmark and the utilization of the unique 10-digit personal identification number, emphasizes the robust foundation of this research [26].
The reliance on the electronic patient record system contributes another significant strength, affording detailed information and access to comprehensive patient data from electronic files. However, it is crucial to acknowledge that the electronic patient system, inherent to its retrospective nature, may be susceptible to errors and lack correct classification, potentially introducing a risk of underestimation in comorbidities. An ECOG performance status for every patient would also benefit our understanding of their functional status [21]. Nevertheless, this study is the first to map the long-term survivors after diagnosis of metastatic or locally advanced BC without systemic treatment and additionally the reason for wavering treatment.
5. Conclusions
This study found that a considerable number of patients registered with la/mBC and not having received systemic oncological treatment actually underwent treatment or did not have la/mBC, indicating a misclassification in the system. This misclassification might have contributed to the pre-study perception that a larger patient population turned out as long-term survivors.
The study found 159 patients who did forego treatment, which was often due to general poor physical condition, underscoring the need for effective and tolerable treatment. Median survival time was 2.6 months (95% CI 0.26; 4.94) post-diagnosis. Long-term survivors tend to have an overall lower tumor burden and were less likely to have liver metastasis.
This investigation is underscoring the need to advance patient care and tailor treatment strategies more effectively. This will potentially make more patients eligible for treatment and, by that, improve overall survival from la/mBC.
Author Contributions
Conceptualization, K.T. and J.B.J.; methodology, K.T., S.B.B. and J.B.J.; software, K.T. and S.B.B.; validation, K.T., S.B.B. and J.B.J.; formal analysis, K.T.; investigation, K.T., S.B.B. and J.B.J.; resources, J.B.J.; data curation, K.T.; writing—original draft preparation, K.T.; writing—review and editing, S.B.B. and J.B.J.; visualization, K.T.; supervision, S.B.B. and J.B.J.; project administration, J.B.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Danish Data Protection Agency approval was granted before data extraction (1-45-70-104-22).
Informed Consent Statement
Patient consent was waived as it was presumed that a significant proportion of the patients whose data are going to be analyzed may have already passed away at the time of data collection. A circumstance that had been officially approved by the Ethics Committee.
Data Availability Statement
Due to privacy and ethical considerations, the supporting data is not available, however, limited anonymous data can be shared upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Richters, A.; Aben, K.K.H.; Kiemeney, L.A.L.M. The global burden of urinary bladder cancer: An update. World J. Urol. 2020, 38, 1895–1904. [Google Scholar]
- Powles, T.; Bellmunt, J.; Comperat, E.; De Santis, M.; Huddart, R.; Loriot, Y.; Necchi, A.; Valderrama, B.P.; Ravaud, A.; Shariat, S.F.; et al. Bladder cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 33, 244–258. [Google Scholar] [PubMed]
- The Danish Bladder Cancer Group (DaBlaCa). Annual Report 2022. 2023. Available online: https://www.sundk.dk/media/bwaet3cf/a79647f3268f4da6bcce76d14a127b8d.pdf (accessed on 30 November 2023). (In Danish).
- Robert, S.; Svatek, A.S.-R.; Colin, P.; Dinney, M.D. Management of metastatic urothelial cancer: The role of surgery as an adjunct to chemotherapy. Can. Urol. Assoc. J. 2009, 3, 228–231. [Google Scholar]
- Stecca, C.; Abdeljalil, O.; Sridhar, S.S. Metastatic Urothelial Cancer: A Rapidly Changing Treatment Landscape. Ther. Adv. Med. Oncol. 2021, 13, 17588359211047352. [Google Scholar] [PubMed]
- Patel, V.G.; Oh, W.K.; Galsky, M.D. Treatment of muscle-invasive and advanced bladder cancer in 2020. CA Cancer J. Clin. 2020, 70, 404–423. [Google Scholar]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Comperat, E.M.; Cowan, N.C.; Gakis, G.; Hernandez, V.; Linares Espinos, E.; Lorch, A.; Neuzillet, Y.; et al. European Association of Urology Guidelines on Muscle-Invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur. Urol. 2021, 79, 82–104. [Google Scholar]
- Sengeløv, L.; Kamby, C.; von der Maase, H. Pattern of metastases in relation to characteristics of primary tumor and treatment in patients with disseminated urothelial carcinoma. J. Urol. 1996, 155, 111–114. [Google Scholar]
- The Danish Bladder Cancer Group (DaBlaCa). Clinical Guidelines for T4b and Metastatic Bladder Cancer. 2022. Available online: https://www.dmcg.dk/kliniske-retningslinjer/kliniske-retningslinjer-opdelt-paa-dmcg/cancer-i-urinvejene/blaerekraeft/ (accessed on 30 November 2023). (In Danish).
- Galsky, M.D.; Pal, S.K.; Lin, S.W.; Ogale, S.; Zivkovic, M.; Simpson, J.; Derleth, C.; Schiff, C.; Sonpavde, G. Real-World Effectiveness of Chemotherapy in Elderly Patients with Metastatic Bladder Cancer in the United States. Bladder Cancer 2018, 4, 227–238. [Google Scholar]
- Sonpavde, G.; Galsky, M.D.; Latini, D.; Chen, G.J. Cisplatin-ineligible and chemotherapy-ineligible patients should be the focus of new drug development in patients with advanced bladder cancer. Clin. Genitourin. Cancer 2014, 12, 71–73. [Google Scholar] [CrossRef]
- Porter, M.P.; Kerrigan, M.C.; Donato, B.M.; Ramsey, S.D. Patterns of use of systemic chemotherapy for Medicare beneficiaries with urothelial bladder cancer. Urol. Oncol. 2011, 29, 252–258. [Google Scholar] [CrossRef]
- Balar, A.V.; Castellano, D.; O’Donnell, P.H.; Grivas, P.; Vuky, J.; Powles, T.; Plimack, E.R.; Hahn, N.M.; de Wit, R.; Pang, L.; et al. First-line pembrolizumab in cisplatin-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): A multicentre, single-arm, phase 2 study. Lancet Oncol. 2017, 18, 1483–1492. [Google Scholar] [PubMed]
- Small, A.C.; Tsao, C.K.; Moshier, E.L.; Gartrell, B.A.; Wisnivesky, J.P.; Godbold, J.H.; Smith, C.B.; Sonpavde, G.; Oh, W.K.; Galsky, M.D. Prevalence and characteristics of patients with metastatic cancer who receive no anticancer therapy. Cancer 2012, 118, 5947–5954. [Google Scholar] [PubMed]
- Omland, L.H.; Joensen, U.N.; Toft, B.G.; Lund, C.M.; Lindberg, H.; Knudsen, M.B.; Tolver, A.; Suetta, C.; Pappot, H. Reasons for lack of treatment in patients with locally advanced, unresectable or metastatic urothelial carcinoma. Acta Oncol. 2022, 61, 1036–1042. [Google Scholar] [PubMed]
- Norgaard, M.; Mailhac, A.; Fagerlund, K.; Strunz-McKendry, T.; Agerbaek, M.; Jensen, J.B. Treatment patterns, survival, and healthcare utilisation and costs in patients with locally advanced and metastatic bladder cancer in Denmark 2015–2020. Acta Oncol. 2023, 62, 1784–1790. [Google Scholar]
- Galsky, M.D.; Hahn, N.M.; Rosenberg, J.; Sonpavde, G.; Hutson, T.; Oh, W.K.; Dreicer, R.; Vogelzang, N.; Sternberg, C.N.; Bajorin, D.F.; et al. Treatment of patients with metastatic urothelial cancer “unfit” for Cisplatin-based chemotherapy. J. Clin. Oncol. 2011, 29, 2432–2438. [Google Scholar] [CrossRef]
- Bellmunt, J.; Choueiri, T.K.; Fougeray, R.; Schutz, F.A.; Salhi, Y.; Winquist, E.; Culine, S.; von der Maase, H.; Vaughn, D.J.; Rosenberg, J.E. Prognostic factors in patients with advanced transitional cell carcinoma of the urothelial tract experiencing treatment failure with platinum-containing regimens. J. Clin. Oncol. 2010, 28, 1850–1855. [Google Scholar]
- Omland, L.H.; Lindberg, H.; Carus, A.; Als, A.B.; Jensen, N.V.; Taarnhoj, G.A.; Trepiakas, R.; Suetta, C.; Omland, L.H.; Pappot, H. Real-World Treatment Patterns and Overall Survival in Locally Advanced and Metastatic Urothelial Tract Cancer Patients Treated with Chemotherapy in Denmark in the Preimmunotherapy Era: A Nationwide, Population-Based Study. Eur. Urol. Open Sci. 2021, 24, 1–8. [Google Scholar]
- Bellmunt, J.; Mottet, N.; De Santis, M. Urothelial carcinoma management in elderly or unfit patients. Eur. J. Cancer Suppl. 2016, 14, 1–20. [Google Scholar]
- Stensland, K.D.; Galsky, M.D. Current Approaches to the Management of Bladder Cancer in Older Patients. Am. Soc. Clin. Oncol. Educ. Book 2014, 34, e250–e256. [Google Scholar]
- Nadal, R.; Bellmunt, J. Management of metastatic bladder cancer. Cancer Treat. Rev. 2019, 76, 10–21. [Google Scholar]
- Fisher, M.D.; Shenolikar, R.; Miller, P.J.; Fenton, M.; Walker, M.S. Treatment Patterns and Outcomes in Stage IV Bladder Cancer in a Community Oncology Setting: 2008–2015. Clin. Genitourin. Cancer 2018, 16, 1171–1179. [Google Scholar]
- Bajorin, D.F.; Dodd, P.M.; Mazumdar, M.; Fazzari, M.; McCaffrey, J.A.; Scher, H.I.; Herr, H.; Higgins, G.; Boyle, M.G. Long-term survival in metastatic transitional-cell carcinoma and prognostic factors predicting outcome of therapy. J. Clin. Oncol. 1999, 17, 3173–3181. [Google Scholar] [CrossRef] [PubMed]
- von der Maase, H.; Sengelov, L.; Roberts, J.T.; Ricci, S.; Dogliotti, L.; Oliver, T.; Moore, M.J.; Zimmermann, A.; Arning, M. Long-term survival results of a randomized trial comparing gemcitabine plus cisplatin, with methotrexate, vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J. Clin. Oncol. 2005, 23, 4602–4608. [Google Scholar] [PubMed]
- Schmidt, M.; Schmidt, S.A.J.; Adelborg, K.; Sundboll, J.; Laugesen, K.; Ehrenstein, V.; Sorensen, H.T. The Danish health care system and epidemiological research: From health care contacts to database records. J. Clin. Epidemiol. 2019, 11, 563–591. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).