Surgical Techniques for Radical Trachelectomy
Simple Summary
Abstract
1. Introduction
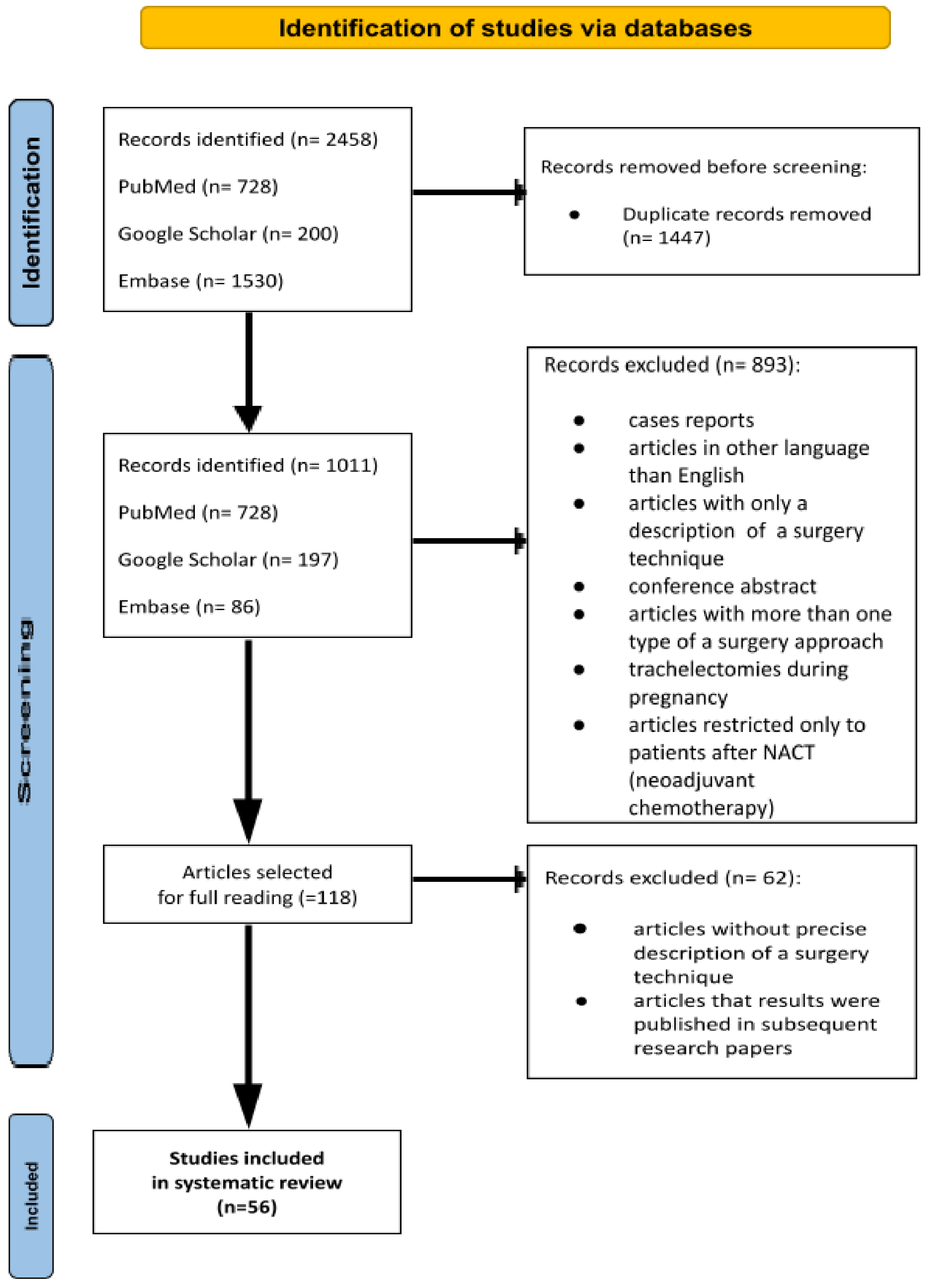
2. Materials and Methods
2.1. Literature Search
2.2. Data Extraction and Synthesis
2.3. Statistical Analysis
3. Results
3.1. Overview of the Studies
| Abdominal | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Number of Cases | FIGO | Tumor Types | Technique | Median Time to Pregnancy | IVF Rate (%) | Attempt for Pregnancy (%) | Pregnancy Rate/Attempt for Pregnancy (%) | Pregnancy Rate/Number of Patients Wit RT (%) | Live Birth Rate (%) | Preterm Delivery Rate (%) | Recurrence Rate (%) | ||||||||
| Uterine Artery Preservation | Nerve Sparing Surgery | Abdominal Cerclage | Type of Suture (Abdominal Cerclage) | Uterine Dilatation During Cerclage Placement | Prolongation of Uterine Catheterization | Type of Utero-Vaginal Anastomosis | Extended Antibiotic Prophylaxis | Suppression of Menstruation | ||||||||||||
| Kiss S.L. et al. [11]; 2021 | 18 | FIGO *: stage IA2 (6) to IB1 (4), IB2 (5), IB3 (4); >2 cm | SCC (15), AC (2) or ASC (1), | no | N/A | no | no | N/A | no | interrupted or a continuous absorbable suture | no | N/A | N/A | N/A | 7/18 (38.9%) | 3/7 (42.9%) | 3/18 (16.67%) | 5/5 (100%) | 0 (0%) | 2/18 (11.11%) |
| Wang Y. et al. [12]; 2020 | 31 | FIGO *: IA1 (1), IA2 (6), IB1 (24) | SCC (29) and AC (2) | yes | N/A | yes | polypropylene mesh | yes | Foley catheter (8 weeks) | N/A | N/A | no | N/A | 2/5 | 15/31 (48.4%) | 5/15 (33.3%) | 5/23 (21.7%) | 3/5 (60%) | 2/3 (66.67%) | 2/31 (9.7%) |
| Mabuchi S. et al. [13]; 2017 | 3 | FIGO *: IA2 (1), IB1 (2) | SCC (3), | yes | yes | yes | polyester suture size #0 | N/A | Foley catheter | N/A | no | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 0/3 0% |
| Li X. et al. [14]; 2016 | 107 | FIGO *: IB1 (46); IB2 (61) | SCC (91), AC (14), other (2); | no | no | yes | polyester Mersilene tape | N/A | T-IUD | interrupted, absorbable sutures | N/A | N/A | N/A | 2/7 (28.57%) | 38/107 (35.51%) | 7/38 (18.4%) | 7/107 (6.5%) | 6/7 (85.71%) | 1/6 (16.7%) | 2/107 (1.87%) |
| van Gent M.D. et al. [15]; 2014 | 28 | FIGO **: IA1 (3), IB1 (22), IB2 (3); ~1.73 cm | SCC (14), AC (11), other (3); | yes | yes | yes | N/A | yes | Foley catheter (7 days) | interrupted, absorbable sutures | yes | N/A | N/A | 2/26 (7.7,%) | 17/26 (65,4%) | 9/17 (52.9%) | 9/28 (3.21%) | 9/9 (100%) | 0/14 (0%) | 2/28 (7.14%) |
| Lintner B. et al. [16]; 2013 | 31 | FIGO **: IB2 (17), IB3 (14); 2–4 cm | SCC (17), AC (4), other (10); | no | no | yes | N/A | N/A | N/A | interrupted, absorbable sutures | N/A | N/A | N/A | N/A | 8/31 (25.8%) | 4/8 (50%) | 4/31 (12.9%) | 3/4 (75%) | 1/3 (33.33%) | 4/31 (12.9%) |
| Muraji M. et al. [9]; type III; 2012 | 8 | FIGO *: IB1 (8) | SCC (5) AC (3), | yes | no | N/A | N/A | N/A | N/A | 1-0 polydioxanone suture | N/A | N/A | N/A | 0 (0%) | N/A | 1 (not defined which group) | N/A | 1/1 (100%) | 1/1 (100%) | 0/8 (0%) |
| Muraji M. et al. [9], type II with nerve- sparing; 2012 | 15 | FIGO *: IB1 (2) IA2 (2) IB1 (11) | SCC (11), AC (3), other (1) | yes | yes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 1 (not defined which group) | N/A | N/A | N/A | 0/15 (0%) |
| Wethington S.L. et al. [17]; 2012 | 81 | FIGO **: IA1-3, IA2 (8,) IB1 (88), IB2 (1), IIA (1) | SCC (40), AC (54), ASC | no | N/A | yes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 38/70 (54.3%) | 28/38 (73.7%) | 28/81 (34.57%) | 16/25 (64%) | N/A | 4/81 (4.94%) |
| Karateke A. et al. [18]; 2012 | 8 | FIGO *: IB1 (2), IB2 (5), IIA (1) | SCC (4), AC (3), other (1), >2 cm (5) <2 cm (3) | no | N/A | no | N/A | no | N/A | interrupted, absorbable sutures | no | N/A | N/A | N/A | N/A | N/A | 3/8 (37.5%) | (2/3) 66.67% | 2/3 (66.67%) | 0/8 (0%) |
| Li J. et al. [19]; 2011 | 59 | FIGO *: IB1 (2), IB2 (5), IIA (1) | SCC (40) (4), AC (3), other (1), >2 cm (5) <2 cm (3) | yes | N/A | yes | polyester Mersilene tape | N/A | T-IUD | interrupted, absorbable sutures | N/A | N/A | N/A | N/A | 10/56 (17.86%) | 2/10 (20%) | N/A | N/A | N/A | 0/59 (0%) |
| Nishio H. et al. [20]; 2009 | 61 | FIGO *: IA1 (4), IA2 (8), IB1 (36), IB2 (13) | SCC (58), AC (2), ASC (1); | yes | N/A | yes |
nylon sutures (without size) | N/A | 1 (3–4 weeks) | interrupted, absorbable sutures | N/A | N/A | 13 months | 17/29 (58.62%) | 29/61 (47.54%) | 4/29 (13.79%) | 4/61 (6.56%) | 4/4 (100%) | 2/4 (50%) | 6/61 (9.84%) |
| Okugawa K. et al. [21]; 2019 | 182 | FIGO *: IA1 (3) IA2 (23) IB1 (94) IB2 (58) IIA1 (4) | SCC (125), AC (46), ASC (11) | yes | yes | yes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 26/182 (14.23%) | 20/36 (55.56%) | 12/34 (35.29%) | 3/182 (1.64%) |
| Kim C.H. et al. [22]; 2012 | 77 | FIGO *: IA1, IA2, IB1 | SCC (45), ASC (10), AC (50); | N/A | N/A | yes | polyester suture size #0 | N/A | N/A | N/A | N/A | N/A | 6 months | 11/23 (47.82%) | 35/77 (45.45%) | 23/35 (65.71%) | 23/77 (29.87%) | 20/23 (86.96%) | 7/20 (35%) | N/A |
| Cǎpîlna M.E. et al. [23]; 2014 | 26 | FIGO **: IA2 (11), IB1 (14), IB2 (1) | SCC (15), ASC (8), AC (3) | no | N/A | no | N/A | N/A | N/A | N/A | N/A | no | N/A | 0/3 (0%) | 7/26 (30.43%) | 3/7 (42.85%) | 3/26 (11.54%) | 1/3 (33.33%) | 0 (0%) | 1/26 (3.85%) |
| Li X. et al. [24]; 2019 | 333 | FIGO *: IA1 (50), IA2 (28) IB1 (255) | SCC (271), AC (51), ASC (11) | no | no | yes | polytetrafluoroethylene (ePTFE) GoreTex | N/A | T-IUD | interrupted, absorbable sutures | N/A | N/A | N/A | N/A | N/A | N/A | 22/333 (6.61%) | 15/22 (68.18%) | 3/15 (20%) | 11/333 (3.3%) |
| Nakajima T. et al. [25]; 2020 | 32 | FIGO *: IA1 (3), IB1 (29) | SCC (25), AC (5), other (2); | yes | yes | yes | polyester suture size #0 | yes | plastic tube (7 days) | U-shaped sutures | N/A | N/A | N/A | N/A | 9/32 (28.12%) | 6/9 (66.67%) | 6/32 (18.75%) | 6/6 (100%) | 2/6 (33.33%) | 0/32 0% |
| Li X. et al. [26]; 2020 | 360 | FIGO *: IA1 (50), IA2 (32), IB1 (268) | SCC (285), AC (51), other (24); | N/A | N/A | yes | polytetrafluoroethylene (ePTFE) GoreTex | N/A | N/A | N/A | N/A | N/A | N/A | 16/30 (53.33%) | 149/360 (41.39%) | 26/149 (17.45%) | 26/360 (7.22%) | 19/26 (73.11%) | 5/19 (26.32%) | N/A |
| Tamauchi S. et al. [27]; 2016 | 28 | FIGO **: IA2 (4), IB1 (24) | SCC (21), AC (5), other (2); | yes | yes | yes | N/A | N/A | N/A | N/A | N/A | no | N/A | 5/8 (62.5%) | 12/28 (42.85%) | 8/12 (66.67%) | 8/28 (28.57%) | 5/8 (62.5%) | 4/5 (80%) | 0/28 (0%) |
| Nishio H. et al. [28]; 2013 | 114 | FIGO **: IA1 (9), IA2 (12), IB1 (93) | SCC (99), AC (14), other (1) | yes | yes | yes | polyester suture size #0 | N/A | N/A | N/A | N/A | N/A | 32.6 +/− 22 months | 20/31 (64.52%) | 69/114 (60.53%) | 25/69 (36.23%) | 25/114 (2.,93%) | 21/25 (84%) | 17/21 (80.95%) | N/A |
| Tokunaga H. et al. [29]; 2014 | 42 | FIGO *: IA1 (1), IA2(4), IB1 (37), <2 cm | SCC (42); | N/A | yes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 9/18 (50%) | 18/42 (42.86%) | 5/18 (27.78%) | 5/42 (11.9%) | 3/5 (60%) | 2/3 (66.67%) | 3/42 (7.14%) |
| Wang Y. et al. [10]; 2021 | 68 | FIGO *: IA1 (6), IA2 (22), IB (40) | SCC (45), AC (14), other (9); | yes | no | yes | N/A | N/A | Foley catheter | N/A | N/A | N/A | 6 months | 2/22 (9.1%) | 52/68 (76.47%) | 11/52 (21.15%) | 11/68 (16.18%) | 9/11 (81.82%) | 3/9 (33.33%) | 11/68 (16.18%) |
| Endoscopic | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Number of Cases | FIGO | Tumor Types | Technique | Median Time to Pregnancy | IVF Rate (%) | Attempt for Pregnancy (%) | Pregnancy Rate/Attempt for Pregnancy (%) | Pregnancy Rate/Number of Patients Wit RT (%) | Live Birth Rate (%) | Preterm Delivery Rate (%) | Recurrence Rate (%) | ||||||||
| Uterine Artery Preservation | Nerve Sparing Surgery | Abdominal Cerclage | Type of Suture (Abdominal Cerclage) | Uterine Dilatation During Cerclage Placement | Prolongation of Uterine Catheterization | Type of Utero-Vaginal Anastomosis | Extended Antibiotic Prophylaxis | Suppression of Menstruation | ||||||||||||
| Johansen G. et al. [30]; 2016 | 48 | FIGO **: IA1-IA2 (16), IB1 (32) | SCC (25), ASC (5), AC (18) | no | N/A | yes | N/A | N/A | N/A | N/A | yes | N/A | 5.3 year | 1/3 (33.3) | 10/30 (33.3%) | 3/10 (30%) | 3/30 (10%) | 2/3 (66.6) | 0/2 (0%) | 3/30 (10%) |
| Ekdahl L. et al. [31]; 2021 | 149 | FIGO **: IA1 (8), IA2 (29), IB1 (111), IIA (1) | SCC (88), AC (61) | yes | no | yes | polypropylene sutures size #0, polytetrafluoroethylene (ePTFE) GoreTex | N/A | N/A | N/A | N/A | N/A | N/A | 17/88 (19.3) | 88/149 (59%) | 70/88 (79.5%) | 70/149 (47%) | 76/88 (86.4) | 18/76 (23.7%) | 11/149 (7.4%) |
| Xu M. et al. [32]; 2022 | 12 | FIGO *: IA2 (1) IB1 (9) IB2 (2); <2 cm (10) >2 cm (2) | SCC (10), ASC (2) | yes | yes | N/A | N/A | yes | 6 months | N/A | N/A | no | N/A | N/A | 3/12 (25%) | 2/3 (67%) | 2/12 (16.67%) | N/A | N/A | 0/12 (0%) |
| Xu M. et al. [33]; 2022 | 25 | FIGO *: IA2 (5), IB1 (16), IB2 (4) | SSC (21), ASC (4) | yes | yes | no | N/A | yes | modified IUD (6 months) | N/A | no | no | N/A | N/A | 8/25 (32.0%) | 4/8 (50%) | 4/25 (16%) | N/A | N/A | N/A |
| Kanao H. et al. [34]; 2021 | 35 | FIGO *: 1A2 (8), IB1 (29) 2A1 (3) | SCC (29), other (11) | yes | yes | yes | polypropylene sutures size #2 | N/A | N/A | N/A | N/A | N/A | N/A | 2/9 (22.2) | 9/35 (26%) | 7/9 (78%) | 7/35 (20%) | 8/9 (88.9) | 0/8 (0%) | 1/40 (2.5%) |
| Saadi J. et al. [35]; 2017 | 22 | FIGO *: IA2 (5), IB1 (16), IB2 (1); <2 cm (21), >3 cm (1) | SSC (17), AC (5) | yes | N/A | yes | polypropylene sutures, size #0 | yes | Foley catheter (7–10 days) | 2-0 Vicryl suture | N/A | N/A | N/A | N/A | N/A | N/A | 2/22 (9%) | 2 (100%) | 1/2 (50%) | 1/35 (2.9%) |
| Saadi J.M. et al. [36]; 2015 | 4 | FIGO **: IB1 (4) | SCC (2), AC (1), other (1) | yes | N/A | no | N/A | yes | Foley catheter (15 days) | 2-0 Vicryl suture | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Kim J. et al. [37]; 2010 | 27 | FIGO **: IIA (1), IB1 (26); | SSC (20), AC (6), ASC (1); | yes | N/A | yes | polyester Mersilene tape | N/A | N/A | N/A | N/A | N/A | N/A | 1/6 (16.7) | 6/27 (18.75%) | 3/6 (50%) | 3/27 (11.1%) | 1/3 (33.3) | 0/1 (0%) | 1/27 (3.7%) |
| Chen Y. et al. [38]; 2008 | 16 | FIGO ***: IA1 (3), IA2 (7), IB1 (6) | SSC (14), AC (2) | no | N/A | yes | polypropylene sutures size #1 | N/A | N/A | N/A | N/A | N/A | N/A | 1/16 (6.25) | N/A | N/A | 5/16 (31.3%) | 2/5 (40%) | 1/2 (50%) | 0/16 (0%) |
| Ekdahl L. et al. [39]; 2021 | 42 | FIGO *: IA1 (3), IA2 (12), IB1 (26), IIA (1) | SSC (16), AC (26) | yes | yes | yes | polypropylene sutures size #0 | N/A | N/A | N/A | N/A | N/A | N/A | 3/22 (14%) | 28/42 (67%) | 22/28 (79%) | 22/42 (52.4%) | 28/39 (71.8) | 4/39 (10.3%) | 0/42 (0%) |
| Park N. et al. [40]; 2009 | 4 | FIGO *: IA2 (1), IB1 (3) | SCC (4) | no | yes | no | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 1/4 (25%) |
| Ebisawa K. et al. [41]; 2013 | 56 | FIGO **: IA2 (4), IB1 (52) | SCC (42), AC (12), other (2) | yes | no | yes | polyester sutures size #2 | N/A | N/A | N/A | N/A | N/A | N/A | 7/21 (33%) | 25/56 (45%) | 13/25 (52%) | 13/56 (23.2%) | 13/21 (61.9) | 10/13 (76%) | 1/56 (1.8%) |
| Kucukmetin A. et al. [42]; 2014 | 11 | FIGO **: 1B1 (11) | SCC (5), AC (6) | no | yes | yes | polyester sutures size #1 | yes | 10 days | 2-0 Vicryl suture | N/A | yes | N/A | N/A | N/A | no pregnancies | N/A | N/A | N/A | 0/11 (0%) |
| Persson J. et al. [43]; 2012 | 12 | FIGO **: IA1 (4), IA2 (5), IB1 (3) | yes | yes | yes | polypropylene sutures size #0 | no | N/A | 2-0 Vicryl suture | no | N/A | N/A | N/A | 5/12 (42%) | 4/5 (80%) | 4/12 (33.3%) | 2/2 (100%) | 2/2 (100%) | 0/12 (0%) | |
| Vaginal | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Number of Cases | FIGO | Tumor Types | Technique | Median Time to Pregnancy | IVF Rate (%) | Attempt for Pregnancy (%) | Pregnancy Rate/Attempt for Pregnancy (%) | Pregnancy Rate/Number of Patients Wit RT (%) | Live Birth Rate (%) | Preterm Delivery Rate (%) | Recurrence Rate (%) | ||||||||
| Uterine Artery Preservation | Nerve Sparing Surgery | Abdominal Cerclage | Type of Suture (Abdominal Cerclage) | Uterine Dilatation During Cerclage Placement | Prolongation of Uterine Catheterization | Type of Utero-Vaginal Anastomosis | Extended Antibiotic Prophylaxis | Suppression of Menstruation | ||||||||||||
| Shinkai S. et al. [44]; 2022 | 10 | FIGO *: 1A2 (2), 1B1 (8) | SSC (6), AC and ASC (4) | yes | no | yes | nylon suture (without size) | no | no | neocervix was developed by the Sturmdorf technique | no | no | N/A | any | N/A | N/A | N/A | N/A | N/A | 0/10 (0%) |
| Plaikner A. et al. [45]; 2020 | 12 | FIGO *: IA1 (1), IA2 (1), IB1 (7), IB2 (2), IIA1 (1) | SSC (5), ASC (6), AC (1) | yes | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Meglic L. et al. [46]; 2017 | 15 | FIGO *: A1 (5), IA2 (8), IB1 (2) | N/A about type | N/A | N/A | yes | N/A | no | no | N/A | N/A | N/A | N/A | 1/15 (7.2%) | 4/15 (26.7%) | 3/15 (21.5%) | 3/15 (21.5%) | 3/3 100% | 0/3 (0%) | 0/15 (0%) |
| Takada S. et al. [47]; 2013 | 8 | FIGO *: IA1, IA2, IB1 | AC (2), SSC (6) | yes | N/A | yes | nylon suture (without size) | N/A | N/A | neocervix was developed by the Sturmdorf technique | N/A | N/A | 26 months | N/A | N/A | 8/7 (114)% | 8/8 (100%) | 8/8 (100%) | 8/8 (100%) | 0/8 0% |
| Hertel H. et al. [48]; 2006 | 108 | FIGO *: IA1 (18), IA2 (21), IB1 (69) | SCC (75), AC (33) | yes | N/A | yes | N/A | N/A | Foley catheter (5 days) | N/A | N/A | N/A | N/A | N/A | N/A | 18/108 (16.7%) | 18/108 (16.7%) | 15/18 (83.3%) | N/A | 3/108 (2.8%) |
| Speiser D. et al. [49]; 2011 | 212 | FIGO *: IA1 L1 (34), IA2 (47), IB1 (131) | SSC (154), AC (55), ASC (3) | yes | N/A | yes | N/A | N/A | Foley catheter (5 days) | N/A | N/A | N/A | N/A | 4/76 (5.3%) | 76/212 (35.8%) | 60/76 (75.6%) | 60/212 (28.3%) | 45/60 (7%) | 18/45 (40%) | 8/212 (3.7%) |
| Burnett A.F. et al. [50]; 2003 | 18 | FIGO **: IA2 (1), IB1 (20) | SSC (12), AC (9) | yes | N/A | yes | polypropylene-Prolene size 1.0; polyester Mersilene tape | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 3/18 (16.7%) | 3/18 (16.7%) | 2/3 (66.7%) | 1/2 (50%) | 0/18 (0%) |
| Dargent D. et al. [51]; 2000 | 47 | FIGO **: IA1 (5), IA2 (13), IB1 (22), IB2 (3), IIA (1), IIB(3) | SSC (39), AC (3), ASC (4), other (1) | N/A | N/A | yes | N/A | N/A | Foley catheter (2–6 days) | N/A | N/A | N/A | N/A | N/A | N/A | 25/47 (53.2%) | 24/47 (51%) | 13/25 (52%) | N/A | 2/47 (4.3%) |
| Roy M. et al. [52]; 1998 | 30 | FIGO **: IA1 (1), IA2 (7), IB1 (18), IB2 (2), IIA (2) | SSC (18), AC (12) | yes | N/A | yes | non- resorbable suture | N/A | 30 days | N/A | N/A | N/A | N/A | N/A | 6/30 (20%) | 6/6 (100%) | 6/30 (20%) | 4/6 (66.7%) | 2/4 (50%) | 1/30 (3.33%) |
| Hauerberg L. et al. [53]; 2015 | 120 | FIGO *: CIS (2), IA1 (7), IA2 (8), IB1 (96), IB2 (7) | AC (38), SSC (82) | no | N/A | yes | yes | N/A | Foley catheter (5 days) | N/A | N/A | N/A | N/A | 19/72 (26.4%) | 72/120 (60.0%) | 55/72 (76.3%) | 55/120 (45.8%) | 53/77 (68.8%) | 33/53 (62.3%) | 6/120 (5.1%) |
| van der Plas R.C.J. et al. [54]; 2021 | 34 | FIGO *: IB1 (30), IB2 (3), IB3 (1) | SSC (27), AC (6), ASC (1) | yes | N/A | yes | yes | N/A | Foley catheter (2 weeks) | N/A | N/A | N/A | N/A | 6/24 (25%) | 24/34 (70.6%) | 15/24 (62.5%) | 15/34 (44.1%) | 15/20 (75%) | 1/20 (5.0%) | 0/34 (0%) |
| Bernardini M. et al. [55]; 2003 | 80 | FIGO **: N/A | N/A | yes | N/A | yes | polyester Mersilene tape | N/A | Foley catheter (3 weeks) | N/A | N/A | N/A | 11 months | 3/18 (16.7%) | 39/80 (48.8%) | 18/39 (46.15%) | 18/80 (22.5%) | 18/22 (81.8%) | 6/22 (27.3%) | N/A |
| Wang A. et al. [56]; 2019 | 83 | FIGO *: IA1(26), IA2 | SSC (78), AC (5); (11), B1 (46) | yes | N/A | yes | N/A | N/A | N/A | N/A | N/A | N/A | 15 months | 0/69 (0%) | 69/83 (83.1%) | 54/69 (84.1%) | 54/83 (65.1%) | 50/58 (86.2%) | 8/50 (16%) | 1/83 (1.2%) |
| Brătilă E. et al. [57]; 2015 | 32 | FIGO **: IA1 (4), IA2 (13), IB1 (19) | SSC (34), AC (2); | yes | N/A | yes | polypropylene-Prolene size 1.0 | N/A | N/A | neocervix was developed by the Sturmdorf technique | N/A | yes | 2 years | 1/28 | 28/32 (87.5%) | 7/28 (25%) | 7/32 (21.9%) | 5/7 (71.4%) | 0 (0%) | 0/32 (0%) |
| Rizzuto I. et al. [58]; 2019 | 19 | FIGO *: IA2 (5), IB1 (14) | SSC (12), AC (7); | no | N/A | yes | nylon suture size 1.0 | yes | Foley catheter (2 days) | absorbable multifilament sutures | N/A | yes | N/A | 4/19 (21.05%) | 19/19 (100%) | 1/19 (5%) | 1/19 (5%) | N/A | N/A | 4/19 (21.05%) |
| Covens A. et al. [59]; 1999 | 32 | FIGO *: IB1 (31), IB2 (1) | SSC (19), AC (13) | yes | N/A | yes | polyester Mersilene tape | N/A | Foley catheter (3 weeks) | N/A | N/A | N/A | 13 months | N/A | 13/32 (41%) | 4/13 (31%) | 4/32 (12.5%) | 3/5 (60%) | 0/3 (0%) | 1/32 (3%) |
| Schlaerth J. et al. [60]; 2003 | 10 | FIGO *: IA2 (8), IB1 (2) | SSC (4), AC (5), ASC (1) | no | N/A | yes | polypropylene- Prolene size 1,0; polyester Mersilene tape | N/A | Foley catheter (few days) | N/A | N/A | N/A | N/A | N/A | N/A | 4/10 (40%) | 4/10 (40%) | 2/4 (50%) | 1/2 (50%) | 0/10 (0%) |
| Kim M. et al. [61]; 2014 | 36 | FIGO *: IA2 (1), IB1 (9) | SSC, AC (N/A about types) | no | N/A | yes | nylon suture (without size) | N/A | N/A | neocervix was developed by the Sturmdorf technique | N/A | no | 6–80 months | N/A | N/A | 9/36 (25%) | 9/36 (25%) | 9/10 (90%) | 7/10 (70%) | 0/36 (0%) |
| Alexander-Sefre F. et al. [62]; 2005 | 29 | FIGO **: N/A | N/A | no | N/A | yes | nylon suture size 1.0 | yes | Foley catheter (2–6 days) | absorbable multifilament sutures | N/A | N/A | 6 months | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Plante M. et al. [63]; 2010 | 125 | FIGO *: IA1 (7), IA2 (29), IB1 (73), IB2 (12), IB3 (2), IIA (2) | SSC (69), AC (48), ASC (8) | no | no | yes | polypropylene- Prolene size 1.0 | N/A | N/A | absorbable multifilament sutures | N/A | N/A | 6–12 months after surgery patients can try to conceive | N/A | N/A | 58/125 (46.4%) | 58/125 (46.4%) | 77/106 (72.6%) | 19/77 (24.6%) | 6/125 (4.8%) |
| Shepherd J. et al. [64]; 2001 | 30 | FIGO **: IB1 (3) | SSC (21), AC (8), other (1) | yes | N/A | yes | nylon suture size 1.0 | yes | N/A | N/A | N/A | yes | N/A | N/A | 13/30 (43.3%) | 14/13 (107.7%) | 14/30 (46.7%) | 9/14 (64.3%) | 7/9 (63%) | 0 (0%) |
| Wang Y. et al. [10]; 2021 | 68 | FIGO *: IA1 (4), IA2 (16), IB1 (48) | SSC (49), AC (11), other (8) | yes | no | yes | N/A | N/A | Foley catheter | N/A | N/A | N/A | 6 months | 3/22 (13.6%) | 57/68 (83.82%) | 22/57 (38.6%) | 22/68 (32.35%) | 20/22 (90.91%) | 6/20 (30%) | 7 (10.3%) |
3.2. Surgical Technique for Abdominal Radical Trachelectomy
3.3. Surgical Technique for Endoscopic Radical Trachelectomy
3.4. Surgical Technique for Vaginal Radical Trachelectomy
3.5. Surgical Techniques in Various Surgical Approaches for Radical Trachelectomy
3.6. The Relationship Between Surgical Techniques During RT and Oncological and Obstetrical Outcomes
3.7. Adverse Events
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Stelzle, D.; Tanaka, L.F.; Lee, K.K.; Khalil, A.I.; Baussano, I.; Shah, A.S.V.; McAllister, D.A.; Gottlieb, S.L.; Klug, S.J.; Winkler, A.S.; et al. Estimates of the Global Burden of Cervical Cancer Associated with HIV. Lancet Glob. Health 2021, 9, e161–e169. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of Incidence and Mortality of Cervical Cancer in 2018: A Worldwide Analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef]
- The Surveillance, Epidemiology, and End Results (SEER). Cancer Stat Facts: Cervical Cancer. National Cancer Institute. Available online: https://seer.cancer.gov/statfacts/html/cervix.html (accessed on 28 January 2025).
- Salman, L.; Covens, A. Fertility Preservation in Cervical Cancer—Treatment Strategies and Indications. Curr. Oncol. 2024, 31, 296–306. [Google Scholar] [CrossRef]
- Ronsini, C.; Solazzo, M.C.; Molitierno, R.; De Franciscis, P.; Pasanisi, F.; Cobellis, L.; Colacurci, N. Fertility-Sparing Treatment for Early-Stage Cervical Cancer ≥ 2 cm: Can One Still Effectively Become a Mother? A Systematic Review of Fertility Outcomes. Ann. Surg. Oncol. 2023, 30, 5587–5596. [Google Scholar] [CrossRef] [PubMed]
- Cervical Cancer. National Comprehensive Cancer Network Clinical (NCCN) Clinical Practice Guidelines in Oncology. Version 3.2025, Page CERV-2. Available online: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 11 March 2025).
- Li, X.; Jiang, Z.; Lu, J.; Chen, X.; Ge, H.; Wu, X.; Li, J. Neoadjuvant Chemotherapy Followed by Radical Trachelectomy versus Upfront Abdominal Radical Trachelectomy for Patients with FIGO 2018 Stage IB2 Cervical Cancer. Gynecol. Oncol. 2023, 169, 106–112. [Google Scholar] [CrossRef]
- Mereu, L.; Pecorino, B.; Ferrara, M.; Tomaselli, V.; Scibilia, G.; Scollo, P. Neoadjuvant Chemotherapy plus Radical Surgery in Locally Advanced Cervical Cancer: Retrospective Single-Center Study. Cancers 2023, 15, 5207. [Google Scholar] [CrossRef]
- Muraji, M.; Sudo, T.; Nakagawa, E.; Ueno, S.; Wakahashi, S.; Kanayama, S.; Yamada, T.; Yamaguchi, S.; Fujiwara, K.; Nishimura, R. Type II Versus Type III Fertility-Sparing Abdominal Radical Trachelectomy for Early-Stage Cervical Cancer: A Comparison of Feasibility of Surgical Outcomes. Int. J. Gynecol. Cancer 2012, 22, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, A.; Zhan, J.; Guo, T. Curative Effect of Laparoscopic-Assisted Vaginal Radical Trachelectomy Combined with Pelvic Lymph Node Dissection on Early-Stage Cervical Cancer. J. BUON 2021, 26, 684–690. [Google Scholar]
- Kiss, S.L.; Fandi, A.; Cozlea, A.L.; Gheorghe, M.; Stanca, M.; Bacalbașa, N.; Moldovan, A.A.; Căpîlna, M.E. Abdominal Radical Trachelectomy as Fertility-Sparing Management for Early Stages of Cervical Cancer: Our Experience in 18 Cases. Exp. Ther. Med. 2021, 22, 674. [Google Scholar] [CrossRef]
- Wang, Y.; Peng, Y.; Lin, Z.; Yao, T. The Safety and Effectiveness of Preserving the Ascending Uterine Artery in a Modified Fertility-Sparing Abdominal Radical Trachelectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 193–197. [Google Scholar] [CrossRef]
- Mabuchi, S.; Kimura, T. Extraperitoneal Radical Trachelectomy with Pelvic Lymphadenectomy. Int. J. Gynecol. Cancer 2017, 27, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, J.; Wen, H.; Ju, X.; Chen, X.; Xia, L.; Ke, G.; Tang, J.; Wu, X. The Survival Rate and Surgical Morbidity of Abdominal Radical Trachelectomy Versus Abdominal Radical Hysterectomy for Stage IB1 Cervical Cancer. Ann. Surg. Oncol. 2016, 23, 2953–2958. [Google Scholar] [CrossRef] [PubMed]
- van Gent, M.D.J.M.; van den Haak, L.W.; Gaarenstroom, K.N.; Peters, A.A.W.; van Poelgeest, M.I.E.; Trimbos, J.B.M.Z.; de Kroon, C.D. Nerve-Sparing Radical Abdominal Trachelectomy Versus Nerve-Sparing Radical Hysterectomy in Early-Stage (FIGO IA2-IB) Cervical Cancer: A Comparative Study on Feasibility and Outcome. Int. J. Gynecol. Cancer 2014, 24, 735–743. [Google Scholar] [CrossRef]
- Lintner, B.; Saso, S.; Tarnai, L.; Novak, Z.; Palfalvi, L.; Del Priore, G.; Smith, J.R.; Ungar, L. Use of Abdominal Radical Trachelectomy to Treat Cervical Cancer Greater Than 2 cm in Diameter. Int. J. Gynecol. Cancer 2013, 23, 1065–1070. [Google Scholar] [CrossRef]
- Wethington, S.L.; Cibula, D.; Duska, L.R.; Garrett, L.; Kim, C.H.; Chi, D.S.; Sonoda, Y.; Abu-Rustum, N.R. An International Series on Abdominal Radical Trachelectomy: 101 Patients and 28 Pregnancies. Int. J. Gynecol. Cancer 2012, 22, 1251–1257. [Google Scholar] [CrossRef]
- Karateke, A.; Kabaca, C. Radical Abdominal Trachelectomy Is a Safe and Fertility Preserving Option for Women with Early Stage Cervical Cancer. Eur. J. Gynaecol. Oncol. 2012, 33, 200–203. [Google Scholar]
- Li, J.; Li, Z.; Wang, H.; Zang, R.; Zhou, Y.; Ju, X.; Ke, G.; Wu, X. Radical Abdominal Trachelectomy for Cervical Malignancies: Surgical, Oncological and Fertility Outcomes in 62 Patients. Gynecol. Oncol. 2011, 121, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Nishio, H.; Fujii, T.; Kameyama, K.; Susumu, N.; Nakamura, M.; Iwata, T.; Aoki, D. Abdominal Radical Trachelectomy as a Fertility-Sparing Procedure in Women with Early-Stage Cervical Cancer in a Series of 61 Women. Gynecol. Oncol. 2009, 115, 51–55. [Google Scholar] [CrossRef]
- Okugawa, K.; Yahata, H.; Sonoda, K.; Ohgami, T.; Yasunaga, M.; Kaneki, E.; Kato, K. Safety Evaluation of Abdominal Trachelectomy in Patients with Cervical Tumors ≥ 2 cm: A Single-Institution, Retrospective Analysis. J. Gynecol. Oncol. 2020, 31, e41. [Google Scholar] [CrossRef]
- Kim, C.H.; Abu-Rustum, N.R.; Chi, D.S.; Gardner, G.J.; Leitao, M.M.; Carter, J.; Barakat, R.R.; Sonoda, Y. Reproductive Outcomes of Patients Undergoing Radical Trachelectomy for Early-Stage Cervical Cancer. Gynecol. Oncol. 2012, 125, 585–588. [Google Scholar] [CrossRef]
- Căpîlna, M.E.; Ioanid, N.; Scripcariu, V.; Gavrilescu, M.M.; Szabo, B. Abdominal Radical Trachelectomy: A Romanian Series. Int. J. Gynecol. Cancer 2014, 24, 615–619. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, J.; Jiang, Z.; Xia, L.; Ju, X.; Chen, X.; Wu, X. Oncological Results and Recurrent Risk Factors Following Abdominal Radical Trachelectomy: An Updated Series of 333 Patients. BJOG 2019, 126, 1169–1174. [Google Scholar] [CrossRef]
- Nakajima, T.; Kasuga, A.; Hara-Yamashita, A.; Ikeda, Y.; Asai-Sato, M.; Nakao, T.; Hayashi, C.; Takeya, C.; Adachi, K.; Tsuruga, T.; et al. Reconstructed Uterine Length Is Critical for the Prevention of Cervical Stenosis Following Abdominal Trachelectomy in Cervical Cancer Patients. J. Obstet. Gynaecol. Res. 2020, 46, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xia, L.; Li, J.; Chen, X.; Ju, X.; Wu, X. Reproductive and Obstetric Outcomes after Abdominal Radical Trachelectomy (ART) for Patients with Early-Stage Cervical Cancers in Fudan, China. Gynecol. Oncol. 2020, 157, 418–422. [Google Scholar] [CrossRef]
- Tamauchi, S.; Kajiyama, H.; Sakata, J.; Sekiya, R.; Suzuki, S.; Mizuno, M.; Utsumi, F.; Niimi, K.; Kotani, T.; Shibata, K.; et al. Oncologic and Obstetric Outcomes of Early Stage Cervical Cancer with Abdominal Radical Trachelectomy: Single-institution Experience. J. Obstet. Gynaecol. Res. 2016, 42, 1796–1801. [Google Scholar] [CrossRef]
- Nishio, H.; Fujii, T.; Sugiyama, J.; Kuji, N.; Tanaka, M.; Hamatani, T.; Miyakoshi, K.; Minegishi, K.; Tsuda, H.; Iwata, T.; et al. Reproductive and Obstetric Outcomes after Radical Abdominal Trachelectomy for Early-Stage Cervical Cancer in a Series of 31 Pregnancies. Human. Reprod. 2013, 28, 1793–1798. [Google Scholar] [CrossRef]
- Tokunaga, H.; Watanabe, Y.; Niikura, H.; Nagase, S.; Toyoshima, M.; Shiro, R.; Yokoyama, Y.; Mizunuma, H.; Ohta, T.; Nishiyama, H.; et al. Outcomes of Abdominal Radical Trachelectomy: Results of a Multicenter Prospective Cohort Study in a Tohoku Gynecologic Cancer Unit. Int. J. Clin. Oncol. 2015, 20, 776–780. [Google Scholar] [CrossRef]
- Johansen, G.; Lönnerfors, C.; Falconer, H.; Persson, J. Reproductive and Oncologic Outcome Following Robot-Assisted Laparoscopic Radical Trachelectomy for Early Stage Cervical Cancer. Gynecol. Oncol. 2016, 141, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Ekdahl, L.; Paraghamian, S.; Eoh, K.J.; Thumuluru, K.M.; Butler-Manuel, S.A.; Kim, Y.T.; Boggess, J.F.; Persson, J.; Falconer, H. Long Term Oncologic and Reproductive Outcomes after Robot-Assisted Radical Trachelectomy for Early-Stage Cervical Cancer. An International Multicenter Study. Gynecol. Oncol. 2022, 164, 529–534. [Google Scholar] [CrossRef]
- Xu, M.; Huo, C.; Huang, C.; Liu, Y.; Ling, X.; Xu, G.; Lin, Z.; Lu, H. Round Ligament Suspension and Vaginal Purse-String Suture: Newly Optimized Techniques to Prevent Tumor Spillage in Laparoscopic Radical Trachelectomy for Cervical Cancer. J. Obstet. Gynaecol. Res. 2022, 48, 1867–1875. [Google Scholar] [CrossRef]
- Xu, M.; Huo, C.; Huang, C.; Wu, B.; Liu, Y.; Li, J.; Ling, X.; Xu, G.; Lin, Z.; Lu, H. Feasibility of the “Cuff-Sleeve” Suture Method for Functional Neocervix Reconstruction in Laparoscopic Radical Trachelectomy: A Retrospective Analysis. J. Minim. Invasive Gynecol. 2022, 29, 673–682. [Google Scholar] [CrossRef]
- Kanao, H.; Aoki, Y.; Fusegi, A.; Omi, M.; Nomura, H.; Tanigawa, T.; Okamoto, S.; Kurita, T.; Netsu, S.; Omatsu, K.; et al. Feasibility and Outcomes of “No-Look No-Touch” Laparoscopic Radical Trachelectomy for Early-Stage Cervical Cancer. J. Clin. Med. 2021, 10, 4154. [Google Scholar] [CrossRef] [PubMed]
- Saadi, J.; Minig, L.; Noll, F.; Saraniti, G.; Cárdenas-Rebollo, J.M.; Perrotta, M. Four Surgical Approaches to Cervical Excision During Laparoscopic Radical Trachelectomy for Early Cervical Cancer. J. Minim. Invasive Gynecol. 2017, 24, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Saadi, J.M.; Perrotta, M.; Orti, R.; Salvo, G.; Giavedoni, M.E.; Gogorza, S.; Testa, R. Laparoscopic Radical Trachelectomy: Technique, Feasibility, and Outcomes. JSLS 2015, 19, e2013.00248. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, J.; Kim, D.; Kim, Y.; Kim, Y.; Nam, J. Fertility-sparing Laparoscopic Radical Trachelectomy for Young Women with Early Stage Cervical Cancer. BJOG 2010, 117, 340–347. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, H.; Zhang, Q.; Li, Y.; Wang, D.; Liang, Z. A Fertility-Preserving Option in Early Cervical Carcinoma: Laparoscopy-Assisted Vaginal Radical Trachelectomy and Pelvic Lymphadenectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 136, 90–93. [Google Scholar] [CrossRef]
- Ekdahl, L.; Crusensvärd, M.; Reynisson, P.; Lönnerfors, C.; Persson, J. Quality of Life and Long-Term Clinical Outcome Following Robot-Assisted Radical Trachelectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 267, 234–240. [Google Scholar] [CrossRef]
- Park, N.Y.; Chong, G.O.; Cho, Y.L.; Park, I.S.; Lee, Y.S. Total Laparoscopic Nerve-Sparing Radical Trachelectomy. J. Laparoendosc. Adv. Surg. Tech. 2009, 19, 53–58. [Google Scholar] [CrossRef]
- Ebisawa, K.; Takano, M.; Fukuda, M.; Fujiwara, K.; Hada, T.; Ota, Y.; Kurotsuchi, S.; Kanao, H.; Andou, M. Obstetric Outcomes of Patients Undergoing Total Laparoscopic Radical Trachelectomy for Early Stage Cervical Cancer. Gynecol. Oncol. 2013, 131, 83–86. [Google Scholar] [CrossRef]
- Kucukmetin, A.; Biliatis, I.; Ratnavelu, N.; Patel, A.; Cameron, I.; Ralte, A.; Naik, R. Laparoscopic Radical Trachelectomy Is an Alternative to Laparotomy with Improved Perioperative Outcomes in Patients With Early-Stage Cervical Cancer. Int. J. Gynecol. Cancer 2014, 24, 135–140. [Google Scholar] [CrossRef]
- Persson, J.; Imboden, S.; Reynisson, P.; Andersson, B.; Borgfeldt, C.; Bossmar, T. Reproducibility and Accuracy of Robot-Assisted Laparoscopic Fertility Sparing Radical Trachelectomy. Gynecol. Oncol. 2012, 127, 484–488. [Google Scholar] [CrossRef] [PubMed]
- Shinkai, S.; Ishioka, S.; Mariya, T.; Fujibe, Y.; Kim, M.; Someya, M.; Saito, T. Does Radical Trachelectomy (RT) during Pregnancy Have Higher Obstetrical and Oncological Risks than RT before Pregnancy? Arch. Gynecol. Obstet. 2022, 306, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Plaikner, A.; Jacob, A.; Siegler, K.; Schneider, A.; Ragosch, V.; Barinoff, J.; Kohler, C. Modification of Dargent’s Radical Vaginal Trachelectomy to Facilitate Ureteral Dissection: Description of Technique. Int. J. Gynecol. Cancer 2020, 30, 1210–1214. [Google Scholar] [CrossRef]
- Meglič, L.; Čavič, M.; Tomaževič, T.; Kobal, B.; Cvjetićanin, B.; Možina, A.; Barbič, M.; Smrkolj, Š. Laparoscopic Abdominal Cerclage after Radical Vaginal Trachelectomy. Clin. Exp. Obstet. Gynecol. 2017, 44, 343–346. [Google Scholar] [CrossRef]
- Takada, S.; Ishioka, S.I.; Endo, T.; Baba, T.; Morishita, M.; Akashi, Y.; Mizuuchi, M.; Adachi, H.; Kim, M.; Saito, T. Difficulty in the Management of Pregnancy after Vaginal Radical Trachelectomy. Int. J. Clin. Oncol. 2013, 18, 1085–1090. [Google Scholar] [CrossRef] [PubMed]
- Hertel, H.; Köhler, C.; Grund, D.; Hillemanns, P.; Possover, M.; Michels, W.; Schneider, A. Radical Vaginal Trachelectomy (RVT) Combined with Laparoscopic Pelvic Lymphadenectomy: Prospective Multicenter Study of 100 Patients with Early Cervical Cancer. Gynecol. Oncol. 2006, 103, 506–511. [Google Scholar] [CrossRef]
- Speiser, D.; Mangler, M.; Köhler, C.; Hasenbein, K.; Hertel, H.; Chiantera, V.; Gottschalk, E.; Lanowska, M. Fertility Outcome after Radical Vaginal Trachelectomy: A Prospective Study of 212 Patients. Int. J. Gynecol. Cancer 2011, 21, 1635–1639. [Google Scholar] [CrossRef]
- Burnett, A.F.; Roman, L.D.; O’Meara, A.T.; Morrow, C.P. Radical Vaginal Trachelectomy and Pelvic Lymphadenectomy for Preservation of Fertility in Early Cervical Carcinoma. Gynecol. Oncol. 2003, 88, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Dargent, D.; Martin, X.; Sacchetoni, A.; Mathevet, P. Laparoscopic Vaginal Radical Trachelectomy: A Treatment to Preserve the Fertility of Cervical Carcinoma Patients. Cancer 2000, 88, 1877–1882. [Google Scholar] [CrossRef]
- Roy, M.; Plante, M. Pregnancies after Radical Vaginal Trachelectomy for Early-Stage Cervical Cancer. Am. J. Obstet. Gynecol. 1998, 179, 1491–1496. [Google Scholar] [CrossRef]
- Hauerberg, L.; Høgdall, C.; Loft, A.; Ottosen, C.; Bjoern, S.F.; Mosgaard, B.J.; Nedergaard, L.; Lajer, H. Vaginal Radical Trachelectomy for Early Stage Cervical Cancer. Results of the Danish National Single Center Strategy. Gynecol. Oncol. 2015, 138, 304–310. [Google Scholar] [CrossRef]
- van der Plas, R.C.J.; Bos, A.M.E.; Jürgenliemk-Schulz, I.M.; Gerestein, C.G.; Zweemer, R.P. Fertility-Sparing Surgery and Fertility Preservation in Cervical Cancer: The Desire for Parenthood, Reproductive and Obstetric Outcomes. Gynecol. Oncol. 2021, 163, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Bernardini, M.; Barrett, J.; Seaward, G.; Covens, A. Pregnancy Outcomes in Patients after Radical Trachelectomy. Am. J. Obstet. Gynecol. 2003, 189, 1378–1382. [Google Scholar] [CrossRef]
- Wang, A.; Cui, G.; Jin, C.; Wang, Y.; Tian, X. Multicenter Research on Tumor and Pregnancy Outcomes in Patients with Early-Stage Cervical Cancer after Fertility-Sparing Surgery. J. Int. Med. Res. 2019, 47, 2881–2889. [Google Scholar] [CrossRef]
- Brătilă, E.; Brătilă, C.P.; Coroleuca, C.B. Radical Vaginal Trachelectomy with Laparoscopic Pelvic Lymphadenectomy for Fertility Preservation in Young Women with Early-Stage Cervical Cancer. Indian J. Surg. 2016, 78, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Rizzuto, I.; MacNab, W.; Nicholson, R.; Nalam, M.; Rufford, B. Less Radical Surgery for Women with Early Stage Cervical Cancer: Our Experience on Radical Vaginal Trachelectomy and Laparoscopic Pelvic Lymphadenectomy. Gynecol. Oncol. Rep. 2019, 28, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Covens, A.; Shaw, P.; Murphy, J.; DePetrillo, D.; Lickrish, G.; Laframboise, S.; Rosen, B. Is Radical Trachelectomy a Safe Alternative to Radical Hysterectomy for Patients with Stage IA-B Carcinoma of the Cervix? Cancer 1999, 86, 2273–2279. [Google Scholar] [CrossRef]
- Schlaerth, J.B.; Spirtos, N.M.; Schlaerth, A.C. Radical Trachelectomy and Pelvic Lymphadenectomy with Uterine Preservation in the Treatment of Cervical Cancer. Am. J. Obstet. Gynecol. 2003, 188, 29–34. [Google Scholar] [CrossRef]
- Kim, M.; Ishioka, S.; Endo, T.; Baba, T.; Akashi, Y.; Morishita, M.; Adachi, H.; Saito, T. Importance of Uterine Cervical Cerclage to Maintain a Successful Pregnancy for Patients Who Undergo Vaginal Radical Trachelectomy. Int. J. Clin. Oncol. 2014, 19, 906–911. [Google Scholar] [CrossRef]
- Alexander-Sefre, F.; Chee, N.; Spencer, C.; Menon, U.; Shepherd, J.H. Surgical Morbidity Associated with Radical Trachelectomy and Radical Hysterectomy. Gynecol. Oncol. 2006, 101, 450–454. [Google Scholar] [CrossRef]
- Plante, M.; Gregoire, J.; Renaud, M.C.; Roy, M. The Vaginal Radical Trachelectomy: An Update of a Series of 125 Cases and 106 Pregnancies. Gynecol. Oncol. 2011, 121, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.H.; Mould, T.; Oram, D.H. Radical Trachelectomy in Early Stage Carcinoma of the Cervix: Outcome as Judged by Recurrence and Fertility Rates. BJOG 2001, 108, 882–885. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef]
- Bentivegna, E.; Gouy, S.; Maulard, A.; Chargari, C.; Leary, A.; Morice, P. Oncological Outcomes after Fertility-Sparing Surgery for Cervical Cancer: A Systematic Review. Lancet Oncol. 2016, 17, e240–e253. [Google Scholar] [CrossRef]
- Lv, Z.; Wang, Y.; Wang, Y.; He, J.; Lan, W.; Peng, J.; Lin, Z.; Zhu, R.; Zhou, J.; Chen, Z. A Meta-Analysis of Treatment for Early-Stage Cervical Cancer: Open versus Minimally Invasive Radical Trachelectomy. BMC Pregnancy Childbirth 2023, 23, 727. [Google Scholar] [CrossRef]
- Morice, P.; Maulard, A.; Scherier, S.; Sanson, C.; Zarokian, J.; Zaccarini, F.; Espenel, S.; Pautier, P.; Leary, A.; Genestie, C. Oncologic Results of Fertility Sparing Surgery of Cervical Cancer: An Updated Systematic Review. Gynecol. Oncol. 2022, 165, 169–183. [Google Scholar] [CrossRef]
- Kuznicki, M.L.; Chambers, L.M.; Morton, M.; Son, J.; Horowitz, M.; Crean-Tate, K.K.; Hackett, L.; Rose, P.G. Fertility-Sparing Surgery for Early-Stage Cervical Cancer: A Systematic Review of the Literature. J. Minim. Invasive Gynecol. 2021, 28, 513–526. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Chen, Y.; Zheng, A.; Tan, X.; Chen, H. Minimally Invasive versus Abdominal Radical Trachelectomy for Early-Stage Cervical Cancer: A Systematic Review and Meta-Analysis. Am. J. Cancer Res. 2023, 13, 4466. [Google Scholar] [PubMed]
- Melamed, A.; Rauh-Hain, J.A.; Ramirez, P.T. Minimally Invasive Radical Hysterectomy for Cervical Cancer: When Adoption of a Novel Treatment Precedes Prospective, Randomized Evidence. J. Clin. Oncol. 2019, 37, 3069–3074. [Google Scholar] [CrossRef]
- Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Arévalo-Serrano, J.; Căpîlna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. SUCCOR Study: An International European Cohort Observational Study Comparing Minimally Invasive Surgery versus Open Abdominal Radical Hysterectomy in Patients with Stage IB1 Cervical Cancer. Int. J. Gynecol. Cancer 2020, 30, 1269–1277. [Google Scholar] [CrossRef]
- Bentivegna, E.; Maulard, A.; Pautier, P.; Chargari, C.; Gouy, S.; Morice, P. Fertility Results and Pregnancy Outcomes after Conservative Treatment of Cervical Cancer: A Systematic Review of the Literature. Fertil. Steril. 2016, 106, 1195–1211. [Google Scholar] [CrossRef] [PubMed]
- Kasuga, Y.; Nishio, H.; Miyakoshi, K.; Sato, S.; Sugiyama, J.; Matsumoto, T.; Tanaka, K.; Ochiai, D.; Minegishi, K.; Hamatani, T. Pregnancy Outcomes after Abdominal Radical Trachelectomy for Early-Stage Cervical Cancer: A 13-Year Experience in a Single Tertiary-Care Center. Int. J. Gynecol. Cancer 2016, 26, 163–168. [Google Scholar] [CrossRef]
- Kasuga, Y.; Miyakoshi, K.; Nishio, H.; Akiba, Y.; Otani, T.; Fukutake, M.; Ikenoue, S.; Ochiai, D.; Matsumoto, T.; Tanaka, K. Mid-trimester Residual Cervical Length and the Risk of Preterm Birth in Pregnancies after Abdominal Radical Trachelectomy: A Retrospective Analysis. BJOG 2017, 124, 1729–1735. [Google Scholar] [CrossRef] [PubMed]
- Pareja, R.; Rendón, G.J.; Sanz-Lomana, C.M.; Monzón, O.; Ramirez, P.T. Surgical, Oncological, and Obstetrical Outcomes after Abdominal Radical Trachelectomy—A Systematic Literature Review. Gynecol. Oncol. 2013, 131, 77–82. [Google Scholar] [CrossRef]
- Escobar, P.F.; Ramirez, P.T.; Garcia Ocasio, R.E.; Pareja, R.; Zimberg, S.; Sprague, M.; Frumovitz, M. Utility of Indocyanine Green (ICG) Intra-Operative Angiography to Determine Uterine Vascular Perfusion at the Time of Radical Trachelectomy. Gynecol. Oncol. 2016, 143, 357–361. [Google Scholar] [CrossRef]
- Hockel, M.; Horn, L.C.; Hentschel, B.; Hockel, S.; Naumann, G. Total Mesometrial Resection: High Resolution Nerve-Sparing Radical Hysterectomy Based on Developmentally Defined Surgical Anatomy. Int. J. Gynecol. Cancer 2003, 13, 791–803. [Google Scholar] [CrossRef]
- Lee, S.; Bae, J.; Han, M.; Cho, Y.; Park, J.; Oh, S.; Kim, S.; Choe, S.; Yun, J.; Lee, Y. Efficacy of Nerve-sparing Radical Hysterectomy vs. Conventional Radical Hysterectomy in Early-stage Cervical Cancer: A Systematic Review and Meta-analysis. Mol. Clin. Oncol. 2019, 12, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Bizzarri, N.; Querleu, D.; Dostálek, L.; van Lonkhuijzen, L.R.C.W.; Giannarelli, D.; Lopez, A.; Salehi, S.; Ayhan, A.; Kim, S.H.; Ortiz, D.I.; et al. Survival Associated with Extent of Radical Hysterectomy in Early-Stage Cervical Cancer: A Subanalysis of the Surveillance in Cervical CANcer (SCCAN) Collaborative Study. Am. J. Obstet. Gynecol. 2023, 229, e1–e428. [Google Scholar] [CrossRef]
- Kyo, S.; Mizumoto, Y.; Takakura, M.; Nakamura, M.; Sato, E.; Katagiri, H.; Ishikawa, M.; Nakayama, K.; Fujiwara, H. Nerve-Sparing Abdominal Radical Trachelectomy: A Novel Concept to Preserve Uterine Branches of Pelvic Nerves. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 193, 5–9. [Google Scholar] [CrossRef]
- Mathevet, P.; Laszlo de Kaszon, E.; Dargent, D. Fertility Preservation in Early Cervical Cancer. Gynecol. Obstet. Fertil. 2003, 31, 706–712. [Google Scholar] [CrossRef]
- Tusheva, O.A.; Cohen, S.L.; McElrath, T.F.; Einarsson, J.I. Laparoscopic Placement of Cervical Cerclage. Rev. Obstet. Gynecol. 2012, 5, e158–e165. [Google Scholar] [PubMed]
- Li, X.; Li, J.; Wu, X. Incidence, Risk Factors and Treatment of Cervical Stenosis after Radical Trachelectomy: A Systematic Review. Eur. J. Cancer 2015, 51, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Lake, A.G.; McPencow, A.M.; Dick-Biascoechea, M.A.; Martin, D.K.; Erekson, E.A. Surgical Site Infection after Hysterectomy. Am. J. Obstet. Gynecol. 2013, 209, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Einstein, M.H.; Park, K.J.; Sonoda, Y.; Carter, J.; Chi, D.S.; Barakat, R.R.; Abu-Rustum, N.R. Radical Vaginal versus Abdominal Trachelectomy for Stage IB1 Cervical Cancer: A Comparison of Surgical and Pathologic Outcomes. Gynecol. Oncol. 2009, 112, 73–77. [Google Scholar] [CrossRef]



| Nerve Sparing Technique | Traditional Surgery | p-Value | |
|---|---|---|---|
| FIGO stage | Abdominal approach | ||
| IA | 78 (100%) | 0 (0%) | <0.001 |
| IB | 130 (43.92%) | 166 (56.08%) | |
| Endoscopic approach | |||
| IA | 38 (88.37%) | 5 (11.63%) | 0.002 |
| IB | 100 (64.52%) | 55 (35.48%) | |
| Uterine Artery Preservation (No of Cases) | Uterine Artery Dissection (No of Cases) | p-Value | |
| Abdominal approach | |||
| IA | 112 (80%) | 28 (20%) | 0.210 |
| IB | 377 (70.86%) | 155 (29.14%) | |
| Endoscopic approach | |||
| IA | 47 (97.92%) | 1 (2.08%) | 0.201 |
| IB | 159 (91.91%) | 14 (8.09%) | |
| Vaginal approach | |||
| IA | 155 (84.24%) | 29 (15.76%) | <0.001 |
| IB | 388 (75.19%) | 128 (24.81%) | |
| Adverse Events | Abdominal Number of Events/ Number of Patients | Endoscopic Number of Events/ Number of Patients | Vaginal Number of Events/ Number of Patients | p-Value | |
|---|---|---|---|---|---|
| Cervical stenosis | Yes | 97/1103 | 35/399 | 53/480 | 0.355 |
| (8.79%) | (8.77%) | (11.04%) | |||
| No | 1006/1103 | 364/399 | 427/480 | ||
| (91.21%) | (91.23%) | (88.96%) | |||
| Infections complications | Yes | 55/494 | 19/331 | 25/441 | <0.001 |
| (11.13%) | (5.74%) | (5.67%) | |||
| No | 439/494 | 312/331 | 416/441 | ||
| (88.87%) | (94.26%) | (94.33%) | |||
| Lymphatic complications | Yes | 45/494 | 32/331 | 73/446 | <0.001 |
| (9.11%) | (9.67%) | (16.37%) | |||
| No | 449/494 | 229/331 | 373/446 | ||
| (90.89%) | (69.18%) | (83.63%) | |||
| Secondary infertility (fallopian tube obstruction, amenorrhea) | Yes | 38/854 | 26/331 | 5/326 | <0.001 |
| (4.45%) | (7.85%) | (1.53%) | |||
| No | 816/854 | 305/331 | 321/326 | ||
| (95.55%) | (92.15%) | (98.47%) | |||
| Urological adverse events | Yes | 35/494 | 12/331 | 21/409 | 0.09 |
| (7.09%) | (3.63%) | (5.13%) | |||
| No | 459/494 | 319/331 | 388/409 | ||
| (92.91%) | (96.37%) | (94.87%) | |||
| Vaginal bleeding | Yes | 5/494 | 8/331 | 31/326 | <0.001 |
| (1.01%) | (2.42%) | (9.51%) | |||
| No | 489/494 | 323/331 | 295/326 | ||
| (98.99%) | (97.58%) | (90.49%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szubert, S.; Nadolna, M.; Wawrzynowicz, P.; Horała, A.; Kołodziejczyk, J.; Koberling, Ł.; Caputa, P.; Zaborowski, M.P.; Nowak-Markwitz, E. Surgical Techniques for Radical Trachelectomy. Cancers 2025, 17, 985. https://doi.org/10.3390/cancers17060985
Szubert S, Nadolna M, Wawrzynowicz P, Horała A, Kołodziejczyk J, Koberling Ł, Caputa P, Zaborowski MP, Nowak-Markwitz E. Surgical Techniques for Radical Trachelectomy. Cancers. 2025; 17(6):985. https://doi.org/10.3390/cancers17060985
Chicago/Turabian StyleSzubert, Sebastian, Magdalena Nadolna, Paweł Wawrzynowicz, Agnieszka Horała, Julia Kołodziejczyk, Łukasz Koberling, Paweł Caputa, Mikołaj Piotr Zaborowski, and Ewa Nowak-Markwitz. 2025. "Surgical Techniques for Radical Trachelectomy" Cancers 17, no. 6: 985. https://doi.org/10.3390/cancers17060985
APA StyleSzubert, S., Nadolna, M., Wawrzynowicz, P., Horała, A., Kołodziejczyk, J., Koberling, Ł., Caputa, P., Zaborowski, M. P., & Nowak-Markwitz, E. (2025). Surgical Techniques for Radical Trachelectomy. Cancers, 17(6), 985. https://doi.org/10.3390/cancers17060985





