Association Between Suicidal Ideation and Cancer Screening Uptake: Results from Middle-Aged and Older Adults in Korea
Simple Summary
Abstract
1. Introduction
2. Methods
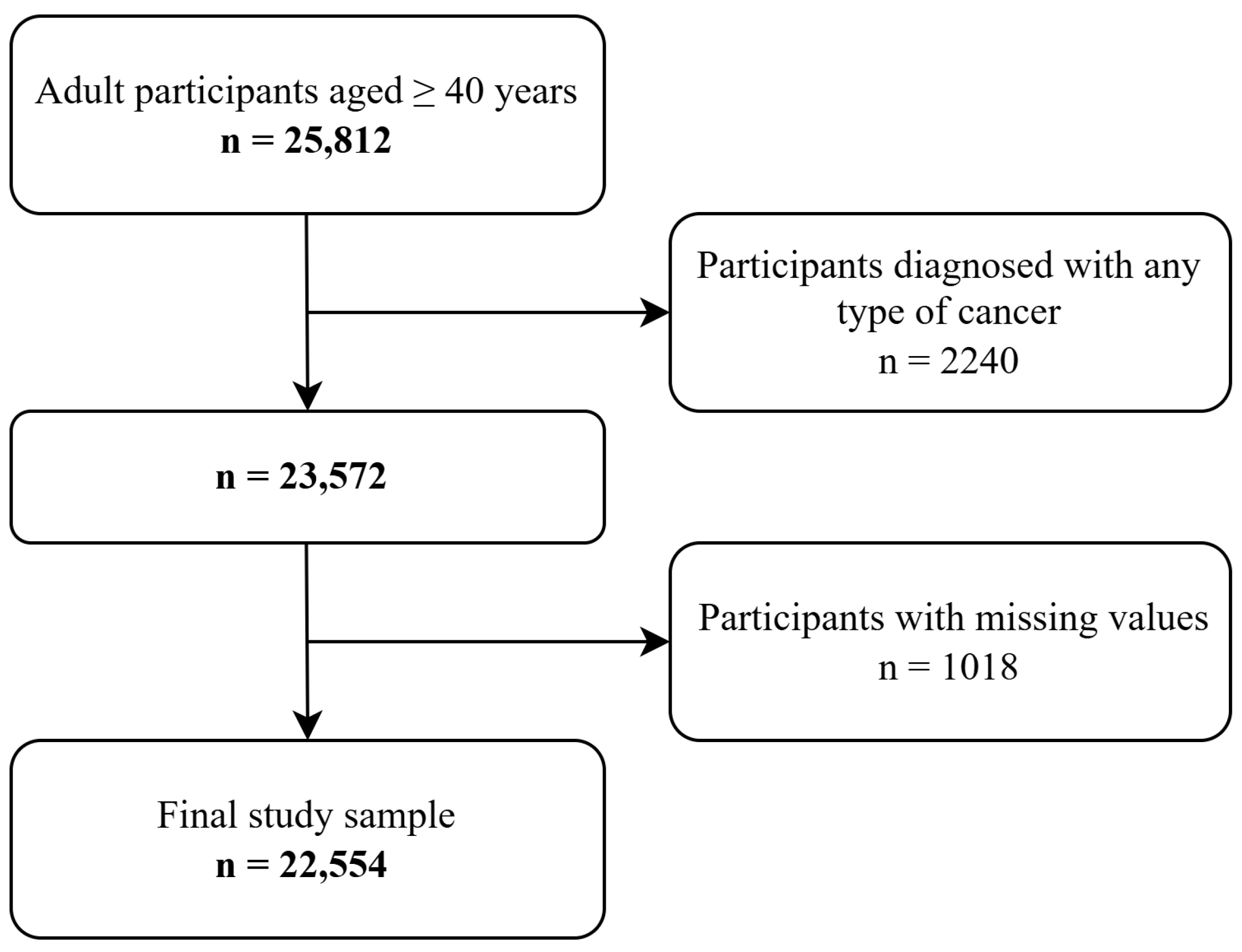
2.1. Study Population
2.2. Ethical Consideration and Data Availability Statement
2.3. Main Variables
2.4. Covariates
2.5. Analysis Strategy
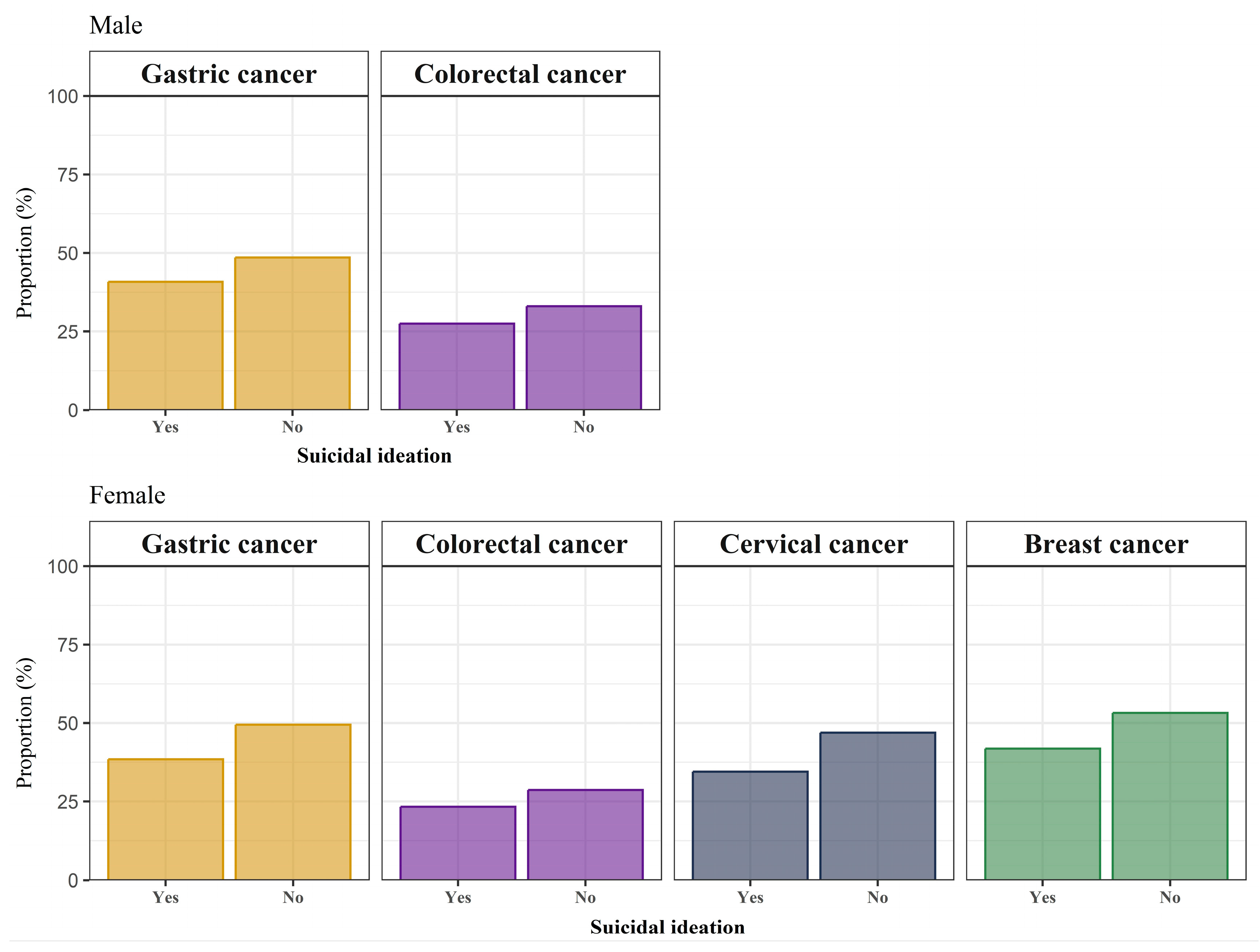
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD South Korea BoD Collaborators. Population health outcomes in South Korea 1990–2019, and projections up to 2040: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2023, 8, e639–e650. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Cho, J.; Park, J.H.; Cho, B. National General Health Screening Program in Korea: History, current status, and future direction. Precis. Future Med. 2022, 6, 9–31. [Google Scholar] [CrossRef]
- Kang, H.T. Current Status of the National Health Screening Programs in South Korea. Korean J. Fam. Med. 2022, 43, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Jun, J.K.; Choi, K.S.; Lee, H.Y.; Park, E.C. Overview of the National Cancer screening programme and the cancer screening status in Korea. Asian Pac. J. Cancer Prev. 2011, 12, 725–730. [Google Scholar]
- Park, B.; Her, E.Y.; Lee, K.; Nari, F.; Jun, J.K.; Choi, K.S.; Suh, M. Overview of the National Cancer Screening Program for Colorectal Cancer in Korea over 14 Years (2004–2017). Cancer Res. Treat. 2023, 55, 910–917. [Google Scholar] [CrossRef]
- Kang, E.; Choi, K.S.; Jun, J.K.; Kim, Y.; Lee, H.J.; Choi, C.K.; Kim, T.H.; Lee, S.H.; Suh, M. Trends in Cancer-Screening Rates in Korea: Findings from the National Cancer Screening Survey, 2004–2023. Cancer Res. Treat. 2025, 57, 28–38. [Google Scholar] [CrossRef]
- Hong, M.; Kim, H.; Park, C.H.K.; Lee, H.; Rhee, S.J.; Min, S.; Kim, M.J.; Yang, J.H.; Song, Y.; Son, K.; et al. Effect of community attitudes on suicide mortality in South Korea: A nationwide ecological study. Front. Psychiatry 2024, 15, 1423609. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Lee, W.Y. The prevalence of suicidal ideation and depression among primary care patients and current management in South Korea. Int. J. Ment. Health Syst. 2017, 11, 18. [Google Scholar] [CrossRef]
- Kim, E.; Kim, S. Spatially clustered patterns of suicide mortality rates in South Korea: A geographically weighted regression analysis. BMC Public. Health 2024, 24, 2380. [Google Scholar] [CrossRef]
- Musuuza, J.S.; Sherman, M.E.; Knudsen, K.J.; Sweeney, H.A.; Tyler, C.V.; Koroukian, S.M. Analyzing excess mortality from cancer among individuals with mental illness. Cancer 2013, 119, 2469–2476. [Google Scholar] [CrossRef]
- Gilham, K.; Gadermann, A.; Dummer, T.; Murphy, R.A. Mental health, cancer risk, and the mediating role of lifestyle factors in the CARTaGENE cohort study. PLoS ONE 2023, 18, e0281588. [Google Scholar] [CrossRef] [PubMed]
- Chierzi, F.; Stivanello, E.; Musti, M.A.; Perlangeli, V.; Marzaroli, P.; De Rossi, F.; Pandolfi, P.; Saponaro, A.; Grassi, L.; Belvederi Murri, M.; et al. Cancer mortality in Common Mental Disorders: A 10-year retrospective cohort study. Soc. Psychiatry Psychiatr. Epidemiol. 2023, 58, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Pan, K.Y.; van Tuijl, L.; Basten, M.; Rijnhart, J.J.M.; de Graeff, A.; Dekker, J.; Geerlings, M.I.; Hoogendoorn, A.; Ranchor, A.V.; Vermeulen, R.; et al. The mediating role of health behaviors in the association between depression, anxiety and cancer incidence: An individual participant data meta-analysis. Psychol. Med. 2024, 54, 2744–2757. [Google Scholar] [CrossRef] [PubMed]
- Kerrison, R.S.; Jones, A.; Peng, J.; Price, G.; Verne, J.; Barley, E.A.; Lugton, C. Inequalities in cancer screening participation between adults with and without severe mental illness: Results from a cross-sectional analysis of primary care data on English Screening Programmes. Br. J. Cancer 2023, 129, 81–93. [Google Scholar] [CrossRef]
- Kaida, A.; Colman, I.; Janssen, P.A. Recent Pap tests among Canadian women: Is depression a barrier to cervical cancer screening? J. Womens Health Larchmt. 2008, 17, 1175–1181. [Google Scholar] [CrossRef]
- Vigod, S.N.; Kurdyak, P.A.; Stewart, D.E.; Gnam, W.H.; Goering, P.N. Depressive symptoms as a determinant of breast and cervical cancer screening in women: A population-based study in Ontario, Canada. Arch. Womens Ment. Health 2011, 14, 159–168. [Google Scholar] [CrossRef]
- Burato, S.; D’Aietti, A.; Paci, A.; Pellegrini, L.; Di Salvo, G.; Sindici, C.; Dellach, C.; Negro, S.; Albert, U. Elevated mortality risks associated with late diagnosis of cancer in individuals with psychiatric disorders? J. Psychiatr. Res. 2025, 181, 547–552. [Google Scholar] [CrossRef]
- Kelsey, E.A.; West, C.P.; Cipriano, P.F.; Peterson, C.; Satele, D.; Shanafelt, T.; Dyrbye, L.N. Original Research: Suicidal Ideation and Attitudes Toward Help Seeking in U.S. Nurses Relative to the General Working Population. Am. J. Nurs. 2021, 121, 24–36. [Google Scholar] [CrossRef]
- Loas, G.; Lefebvre, G.; Rotsaert, M.; Englert, Y. Relationships between anhedonia, suicidal ideation and suicide attempts in a large sample of physicians. PLoS ONE 2018, 13, e0193619. [Google Scholar] [CrossRef]
- Ju, Y.J.; Park, E.C.; Han, K.T.; Choi, J.W.; Kim, J.L.; Cho, K.H.; Park, S. Low socioeconomic status and suicidal ideation among elderly individuals. Int. Psychogeriatr. 2016, 28, 2055–2066. [Google Scholar] [CrossRef]
- Jandial, R.; Subramanian, K.; Kumar, S.; Subramanian, E.; Balasundaram, S. Literacy and Attitude Toward Suicide Among Doctors and Nurses: A Cross-Sectional Comparative Study. Cureus 2024, 16, e64032. [Google Scholar] [CrossRef] [PubMed]
- Rimkeviciene, J.; Hawgood, J.; O’Gorman, J.; De Leo, D. Personal Stigma in Suicide Attempters. Death Stud. 2015, 39, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Ki, M.; Shim, H.Y.; Lim, J.; Hwang, M.; Kang, J.; Na, K.S. Preventive health behaviors among people with suicide ideation using nationwide cross-sectional data in South Korea. Sci. Rep. 2022, 12, 11615. [Google Scholar] [CrossRef]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Oh, K.; Kim, Y.; Kweon, S.; Kim, S.; Yun, S.; Park, S.; Lee, Y.K.; Kim, Y.; Park, O.; Jeong, E.K. Korea National Health and Nutrition Examination Survey, 20th anniversary: Accomplishments and future directions. Epidemiol. Health 2021, 43, e2021025. [Google Scholar] [CrossRef]
- Chuck, K.W.; Hwang, M.; Choi, K.S.; Suh, M.; Jun, J.K.; Park, B. Cancer screening rate in people with diabetes in the Korean population: Results from the Korea National Health and Nutrition Examination Survey 2007–2009. Epidemiol. Health 2017, 39, e2017036. [Google Scholar] [CrossRef]
- Kim, E.Y.; Shim, Y.S.; Kim, Y.S.; Lee, S.P.; Ko, K.D.; Choi, W.J. Adherence to general medical checkup and cancer screening guidelines according to self-reported smoking status: Korea National Health and Nutrition Examination Survey (KNHANES) 2010–2012. PLoS ONE 2019, 14, e0224224. [Google Scholar] [CrossRef]
- Kang, M.; Yoo, K.B.; Park, E.C.; Kwon, K.; Kim, G.; Kim, D.R.; Kwon, J.A. Factors associated with organized and opportunistic cancer screening: Results of the Korea National Health and Nutrition Examination Survey (KNHANES) 2007-2011. Asian Pac. J. Cancer Prev. 2014, 15, 3279–3286. [Google Scholar] [CrossRef]
- Myong, J.P.; Shin, J.Y.; Kim, S.J. Factors associated with participation in colorectal cancer screening in Korea: The Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV). Int. J. Color. Dis. 2012, 27, 1061–1069. [Google Scholar] [CrossRef]
- Kim, S.M.; Lee, G. Risk factors of suicide ideation in younger-old and older-old persons: Using data from the korea health panel survey. J. Korean Gerontol. Nurs. 2020, 22, 281–290. [Google Scholar] [CrossRef]
- Hwang, I.C.; Ahn, H.Y. Association between neighborhood environments and suicidal ideation among Korean adults. J. Affect. Disord. 2021, 295, 488–491. [Google Scholar] [CrossRef] [PubMed]
- Han, K.M.; Won, E.; Paik, J.W.; Lee, M.S.; Lee, H.W.; Ham, B.J. Mental health service use in adults with suicidal ideation within a nationally representative sample of the Korean population. J. Affect. Disord. 2016, 193, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Lee, D.W.; Kwon, J.; Yang, J.; Park, E.C.; Jang, S.I. Suicide related indicators and trends in Korea in 2019. Health Policy Manag. 2021, 31, 232–239. [Google Scholar]
- Lumley, T. Analysis of complex survey samples. J. Stat. Softw. 2004, 9, 1–19. [Google Scholar] [CrossRef]
- Solmi, M.; Firth, J.; Miola, A.; Fornaro, M.; Frison, E.; Fusar-Poli, P.; Dragioti, E.; Shin, J.I.; Carvalho, A.F.; Stubbs, B.; et al. Disparities in cancer screening in people with mental illness across the world versus the general population: Prevalence and comparative meta-analysis including 4 717 839 people. Lancet Psychiatry 2020, 7, 52–63. [Google Scholar] [CrossRef]
- Rano-Santamaria, O.; Fernandez-Merino, C.; Castano-Carou, A.I.; Lado-Baleato, O.; Fernandez-Dominguez, M.J.; Sanchez-Castro, J.J.; Gude, F. Health self-perception is associated with life-styles and comorbidities and its effect on mortality is confounded by age. A Popul. Based Study. Front. Med. Lausanne 2022, 9, 1015195. [Google Scholar] [CrossRef]
- Szanto, K.; Dombrovski, A.Y.; Sahakian, B.J.; Mulsant, B.H.; Houck, P.R.; Reynolds, C.F., 3rd; Clark, L. Social emotion recognition, social functioning, and attempted suicide in late-life depression. Am. J. Geriatr. Psychiatry 2012, 20, 257–265. [Google Scholar] [CrossRef]
- Sanchez-Carro, Y.; de la Torre-Luque, A.; Diaz-Marsa, M.; Aguayo-Estremera, R.; Andreo-Jover, J.; Ayad-Ahmed, W.; Bobes, J.; Bobes-Bascaran, T.; Bravo-Ortiz, M.F.; Canal-Rivero, M.; et al. Psychiatric profiles in suicidal attempters: Relationships with suicide behaviour features. Span. J. Psychiatry Ment. Health 2024. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Ma, X.; Park, S.K.; Lawson, K.A. Association of depression with adherence to breast cancer screening among women aged 50 to 74 years in the United States. J. Eval. Clin. Pract. 2020, 26, 1677–1688. [Google Scholar] [CrossRef]
- Yazgan, I.; Chagpar, A. The effect of emotional disorders on adherence to mammography screening guidelines. Breast Cancer Res. Treat. 2022, 192, 623–627. [Google Scholar] [CrossRef]
- Millner, A.J.; Lee, M.D.; Nock, M.K. Single-Item Measurement of Suicidal Behaviors: Validity and Consequences of Misclassification. PLoS ONE 2015, 10, e0141606. [Google Scholar] [CrossRef] [PubMed]
| Male | Female | |||
|---|---|---|---|---|
| Suicidal Ideation | Suicidal Ideation | |||
| Yes | No | Yes | No | |
| N = 1194 | N = 8473 | N = 2845 | N = 10,042 | |
| Region | ||||
| Urban | 799 (66.9) | 6098 (72.0) | 1899 (66.7) | 7344 (73.1) |
| Rural | 395 (33.1) | 2375 (28.0) | 946 (33.3) | 2698 (26.9) |
| Age | ||||
| Median (Q1, Q3) | 62.0 (51.0, 71.0) | 57.0 (48.0, 67.0) | 64.0 (52.0, 72.0) | 56.0 (48.0, 67.0) |
| Income level | ||||
| Highest | 199 (16.7) | 2412 (28.5) | 401 (14.1) | 2678 (26.7) |
| High | 213 (17.8) | 2197 (25.9) | 510 (17.9) | 2341 (23.3) |
| Low | 339 (28.4) | 2107 (24.9) | 737 (25.9) | 2493 (24.8) |
| Lowest | 443 (37.1) | 1757 (20.7) | 1197 (42.1) | 2530 (25.2) |
| Education level | ||||
| College or above | 194 (16.2) | 2280 (26.9) | 179 (6.3) | 1349 (13.4) |
| High school | 276 (23.1) | 2712 (32.0) | 477 (16.8) | 2789 (27.8) |
| Middle school or below | 724 (60.6) | 3481 (41.1) | 2189 (76.9) | 5904 (58.8) |
| Employment status | ||||
| Active | 720 (60.3) | 6359 (75.1) | 1154 (40.6) | 4832 (48.1) |
| Inactive | 474 (39.7) | 2114 (24.9) | 1691 (59.4) | 5210 (51.9) |
| Marital status | ||||
| Married | 993 (83.2) | 7842 (92.6) | 1754 (61.7) | 7478 (74.5) |
| Never married | 43 (3.6) | 150 (1.8) | 29 (1.0) | 91 (0.9) |
| Others | 158 (13.2) | 481 (5.7) | 1062 (37.3) | 2473 (24.6) |
| Personal medical insurance | ||||
| Yes | 553 (46.3) | 5405 (63.8) | 1352 (47.5) | 6607 (65.8) |
| No | 641 (53.7) | 3068 (36.2) | 1493 (52.5) | 3435 (34.2) |
| Chronic condition | ||||
| No | 861 (72.1) | 6910 (81.6) | 2173 (76.4) | 8656 (86.2) |
| Yes | 333 (27.9) | 1563 (18.4) | 672 (23.6) | 1386 (13.8) |
| Gastric Cancer | Colorectal Cancer | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Suicidal ideation | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.73 (0.62–0.87) | 0.83 (0.69–0.99) | 0.71 (0.58–0.86) | 0.82 (0.67–1.00) |
| Region | ||||
| Urban | Reference | Reference | ||
| Rural | 1.04 (0.91–1.18) | 0.90 (0.77–1.05) | ||
| Age | ||||
| Continuous scale | 1.03 (1.02–1.03) | 1.02 (1.01–1.03) | ||
| Income level | ||||
| Highest | Reference | Reference | ||
| High | 0.76 (0.66–0.86) | 0.87 (0.72–1.05) | ||
| Low | 0.74 (0.63–0.87) | 0.90 (0.74–1.09) | ||
| Lowest | 0.61 (0.51–0.73) | 0.62 (0.50–0.76) | ||
| Education level | ||||
| College or above | Reference | Reference | ||
| High school | 0.74 (0.65–0.84) | 0.85 (0.70–1.03) | ||
| Middle school or below | 0.75 (0.64–0.87) | 0.74 (0.61–0.90) | ||
| Employment status | ||||
| Active | Reference | Reference | ||
| Inactive | 0.89 (0.77–1.03) | 0.94 (0.80–1.09) | ||
| Marital status | ||||
| Married | Reference | Reference | ||
| Never married | 0.82 (0.57–1.17) | 0.86 (0.44–1.71) | ||
| Others | 0.67 (0.54–0.83) | 0.64 (0.49–0.84) | ||
| Personal medical insurance | ||||
| Yes | Reference | Reference | ||
| No | 0.61 (0.53–0.71) | 0.74 (0.64–0.87) | ||
| Chronic condition | ||||
| No | Reference | Reference | ||
| Yes | 1.00 (0.88–1.14) | 1.02 (0.89–1.18) | ||
| Gastric Cancer | Colorectal Cancer | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Suicidal ideation | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.64 (0.58–0.70) | 0.74 (0.67–0.82) | 0.60 (0.52–0.68) | 0.71 (0.62–0.81) |
| Region | ||||
| Urban | Reference | Reference | ||
| Rural | 1.06 (0.94–1.19) | 0.75 (0.64–0.89) | ||
| Age | ||||
| Continuous scale | 1.01 (1.00–1.02) | 0.99 (0.98–0.99) | ||
| Income level | ||||
| Highest | Reference | Reference | ||
| High | 0.83 (0.73–0.95) | 1.13 (0.95–1.34) | ||
| Low | 0.79 (0.69–0.90) | 1.07 (0.91–1.27) | ||
| Lowest | 0.75 (0.65–0.87) | 1.03 (0.87–1.21) | ||
| Education level | ||||
| College or above | Reference | Reference | ||
| High school | 0.95 (0.82–1.10) | 1.03 (0.80–1.34) | ||
| Middle school or below | 0.96 (0.82–1.13) | 0.94 (0.73–1.22) | ||
| Employment status | ||||
| Active | Reference | Reference | ||
| Inactive | 0.97 (0.88–1.07) | 1.02 (0.90–1.16) | ||
| Marital status | ||||
| Married | Reference | Reference | ||
| Never married | 0.75 (0.47–1.20) | 0.88 (0.46–1.70) | ||
| Others | 0.72 (0.64–0.80) | 0.81 (0.70–0.92) | ||
| Personal medical insurance | ||||
| Yes | Reference | Reference | ||
| No | 0.51 (0.45–0.58) | 0.61 (0.53–0.70) | ||
| Chronic condition | ||||
| No | Reference | Reference | ||
| Yes | 1.07 (0.95–1.21) | 1.07 (0.93–1.22) | ||
| Cervical Cancer | Breast Cancer | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Suicidal ideation | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.60 (0.53–0.66) | 0.75 (0.68–0.84) | 0.63 (0.57–0.70) | 0.76 (0.68–0.84) |
| Region | ||||
| Urban | Reference | Reference | ||
| Rural | 0.75 (0.66–0.85) | 1.06 (0.94–1.19) | ||
| Age | ||||
| Continuous scale | 0.98 (0.98–0.99) | 1.00 (0.99–1.01) | ||
| Income level | ||||
| Highest | Reference | Reference | ||
| High | 0.85 (0.74–0.96) | 0.85 (0.74–0.98) | ||
| Low | 0.90 (0.78–1.02) | 0.81 (0.70–0.93) | ||
| Lowest | 0.86 (0.75–1.00) | 0.86 (0.74–0.99) | ||
| Education level | ||||
| College or above | Reference | Reference | ||
| High school | 0.89 (0.76–1.04) | 0.91 (0.78–1.06) | ||
| Middle school or below | 0.89 (0.75–1.05) | 0.89 (0.76–1.04) | ||
| Employment status | ||||
| Active | Reference | Reference | ||
| Inactive | 1.00 (0.90–1.11) | 0.93 (0.84–1.03) | ||
| Marital status | ||||
| Married | Reference | Reference | ||
| Never married | 0.67 (0.41–1.08) | 0.60 (0.38–0.95) | ||
| Others | 0.79 (0.70–0.88) | 0.79 (0.71–0.88) | ||
| Personal medical insurance | ||||
| Yes | Reference | Reference | ||
| No | 0.55 (0.48–0.62) | 0.52 (0.46–0.58) | ||
| Chronic condition | ||||
| No | Reference | Reference | ||
| Yes | 0.94 (0.83–1.07) | 1.01 (0.89–1.14) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baek, S.-U.; Yoon, J.-H. Association Between Suicidal Ideation and Cancer Screening Uptake: Results from Middle-Aged and Older Adults in Korea. Cancers 2025, 17, 956. https://doi.org/10.3390/cancers17060956
Baek S-U, Yoon J-H. Association Between Suicidal Ideation and Cancer Screening Uptake: Results from Middle-Aged and Older Adults in Korea. Cancers. 2025; 17(6):956. https://doi.org/10.3390/cancers17060956
Chicago/Turabian StyleBaek, Seong-Uk, and Jin-Ha Yoon. 2025. "Association Between Suicidal Ideation and Cancer Screening Uptake: Results from Middle-Aged and Older Adults in Korea" Cancers 17, no. 6: 956. https://doi.org/10.3390/cancers17060956
APA StyleBaek, S.-U., & Yoon, J.-H. (2025). Association Between Suicidal Ideation and Cancer Screening Uptake: Results from Middle-Aged and Older Adults in Korea. Cancers, 17(6), 956. https://doi.org/10.3390/cancers17060956





