The Infectious Clue: Linking Bacterial Infections to Underlying Malignancies
Simple Summary
Abstract
1. Introduction
2. Infections Forecasting Cancer: What the Numbers Reveal
2.1. Gastrointestinal Cancers (Colorectal and Gastric)
2.2. Pancreaticobiliary Cancers
2.3. Lung Cancer and Pulmonary Infection Phenotypes
2.4. Genitourinary Cancers
2.5. Other Pathogens and Malignancies
| First Author, Year | Infection Phenotype | Study Design | Time Window | Effect Size/Absolute Risk |
|---|---|---|---|---|
| Colorectal and other gastrointestinal cancers | ||||
| Østergaard, 2025 [23] | Enterococcus faecalis bacteremia | Danish nationwide registries | First 6 months | CRC 0.45%, CRN 2.3%; CRC HR 3.7; CRN HR 4.6 |
| Ursi, 2021 [22] | Enterococcus spp. and S. gallolyticus IE | Single-center cohort | At time of IE work-up | In patients with colonoscopy: 71–83% intestinal disease; 13–15% CRC |
| Abe, 2024 [19] | Anaerobic bacteremia | Single-center cohort | Within 1 year | OR 3.44 for any GI cancer |
| Justesen, 2022 [46] | Anaerobic bacteremia | Population-based cohort | Within 1 year | C. septicum HR 76; Bacteroides HR 5.95; GPAC ~11; Fusobacterium ~8.5 |
| Kwong, 2018 [17] | Anaerobic bacteremia | Population-based cohort | Within 1 year | Pathogen-specific HRs: B. fragilis ~3.8; S. gallolyticus ~5.7; F. nucleatum ~6.9; C. septicum ~17 |
| Tsai, 2016 [21] | Streptococcus bovis bacteremia | Single-center cohort | No defined time window | CRC detected in 30.7% of patients with S. bovis bacteremia |
| Laupland, 2023 [14] | Community-onset bacteremia | Population-based surveillance cohort | Within 1 year | Overall IRR 16; RR C. septicum 25, B. ovatus 11.8, C. paraputrificum 11.4, S. infantarius 10.6, G. morbillorum 6.5 |
| Gaab, 2023 [18] | Colibactin-producing pks+ Escherichia coli | Systematic review and meta-analysis | No defined time window | Overall OR 2.3; Western countries OR 2.3; tissue-based studies OR 2.2 |
| Huang, 2012 [24] | Pyogenic liver abscess | Retrospective cohort | Highest risk within first 2 years | CRC 2.3%; SIR 4.00; Klebsiella spp. PLA SIR 5.8; aHR 2.7 |
| Suzuki, 2023 [25] | Pyogenic liver abscess | Retrospective cohort | Highest risk within 3 years after PLA | CRC 1.9% vs. 0.8%; time-dependent HRs: 3.6 (0.5 years), 2.5 (1 yr), 1.7 (2 yr), 1.4 (3 yr) |
| Hepatobiliary cancers (liver and gallbladder) | ||||
| Lin, 2011 [28] | Pyogenic liver abscess | Nationwide retrospective cohort | HCC diagnosed within 60 days of PLA | HCC in 2.1%; in liver cirrhosis (OR 5.1), HBV (OR 3.8), HCV (OR 3.5) |
| Koshiol, 2016 [29] | Chronic Salmonella Typhi carriage | Case–control studies/meta-analysis | No defined time window | High Vi antibody titer OR ≈ 4.0; meta-analysis summary RR 4.6–5.0 for S. Typhi and gallbladder cancer |
| Lung cancer | ||||
| Zhan, 2011 [31] | C. pneumoniae infection | Meta-analysis | No defined time window | Overall OR 1.5; prospective OR 1.2; retrospective OR 2.2; IgA ≥ 64 OR 2.4 |
| Shepshelovich, 2016 [16] | Pneumonia in smokers | Retrospective cohort | 1-year follow-up | 1-year lung cancer 8.1% (≈24% after upper-lobe pneumonia 76% located in same lobe) |
| Urinary tract cancers | ||||
| Sun, 2013 [32] | Urinary tract infection | Nationwide cohort | Risk highest in first 4 years | Any UTI HR 4.7; upper UTI HR 4.3 for renal pelvis/ureter cancer; lower UTI HR 5.7 for bladder cancer. |
| Vermeulen, 2015 [33] | Recurrent cystitis | Case–control study | No defined time window | Recurrent cystitis: OR 6.6 in men, OR 2.7 in women. Frequent recurrence (>10 episodes) in men: OR ~6 |
| Fan, 2017 [36] | Lower urinary tract infection | Nationwide population-based cohort | Follow-up for up to 14 yrs | Prostate cancer higher in cystitis aHR 1.5 and urethritis aHR 1.7 vs. no UTI; >5 LUTI visits/yr → aHR 9.3 |
| Zhu, 2016 [38] | Chlamydia trachomatis infection | Systematic review and meta-analysis | No defined time window | Overall OR ≈ 2.2 for cervical cancer; HPV + C. trachomatis OR ≈ 4.0 |
| Any cancer detection—multiple-site signal after severe infection | ||||
| Søgaard, 2020 [15] | Community-acquired Escherichia coli bacteremia (age ≥ 50) | Population-based cohort | Strongest association within 1 year | 1-year cancer incidence 3.0% (GI/hepatobiliary 1.9%, urinary 1.0%) SIR < 1 yr: GI/hepatobiliary 5.4; CRC 4.4; pancreas 7.2; kidney 10.5 SIR ≥ 1 yr: CRC 1.4; pancreas 2.3; overall 1.3 |
| Søgaard, 2017 [13] | First-time Gram-negative bacteremia | Nationwide cohort | 0–6 and 6–12 months after bacteremia | Overall SIR ≈ 1.4. Any cancer SIR ≈ 3.3 in first 6 months; particularly high SIRs (>4–10) for GI and GU cancers |
| Thomsen, 2013 [20] | Infective endocarditis | Retrospective cohort | Very high risk 0–3 months; persistent 3 months–5 yrs; modest > 5 yrs | Overall SIR 1.6: 0–3 months SIR 8; 3 months–5 yrs SIR 1.5; >5 yrs SIR 1.2 Site-specific SIR < 3 months: colon ~12, liver ~46, hematologic ~24 |
| Gotland, 2020 [8] | Staphylococcus aureus bacteremia | Nationwide matched cohort study | Within first year | 1-year IRR 1.65; highest site-specific IRRs: cervical 37.8, myeloma 6.3, leukemia 4.7, sarcoma 4.7, liver 3.6, pancreas 2.8, urinary 2.6. |
| McShane, 2014 [39] | Common community-acquired infections | Population-based case–control study | >13 months prior to diagnosis | ORs 1.1–1.4 for significant infections (strongest: pneumonia OR 1.3; sinusitis OR 1.15; bronchitis OR 1.14) Associations persist up to >72 months |
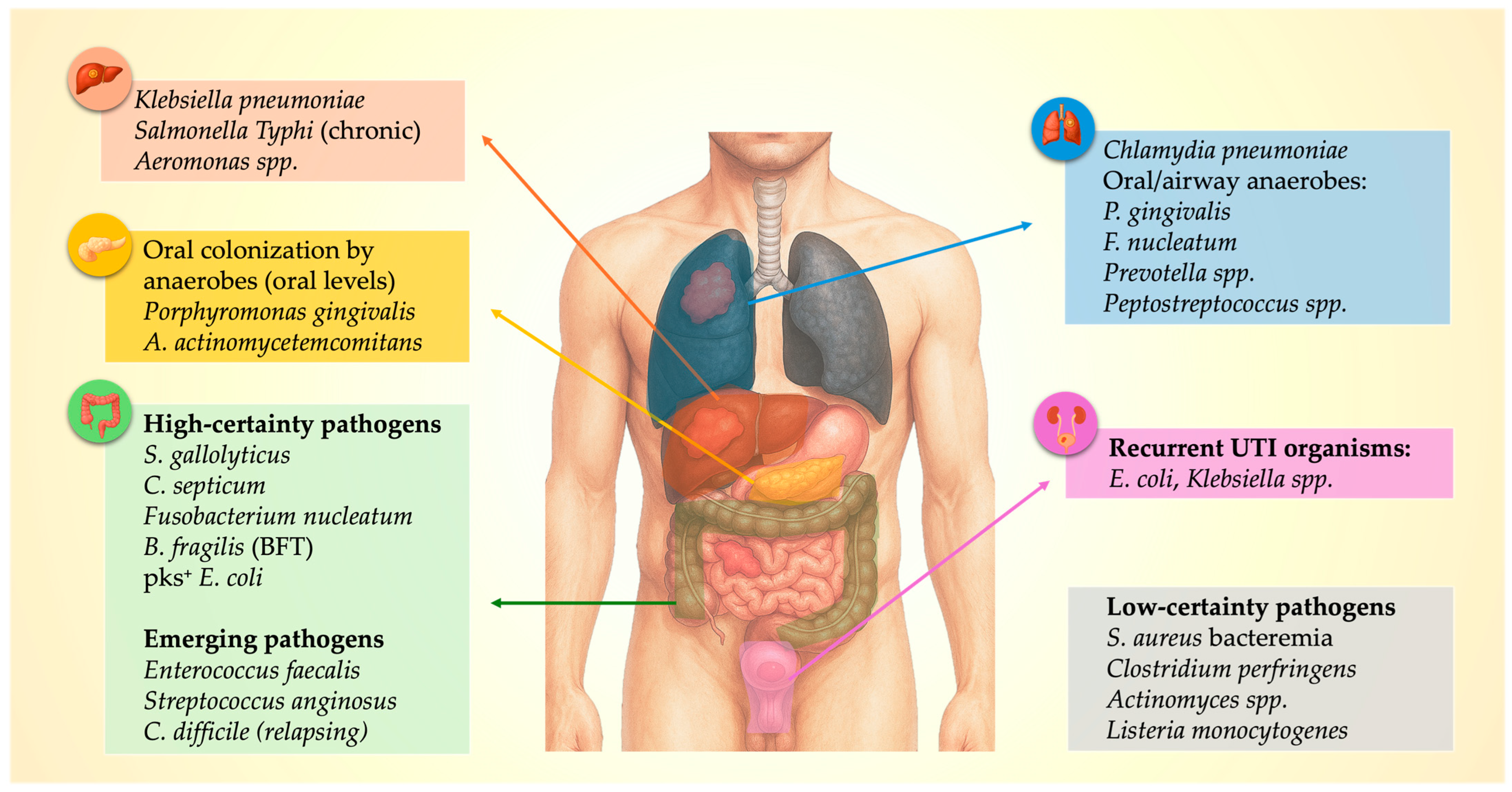
3. Infection-Cancer Nexus: A Pathogen Map
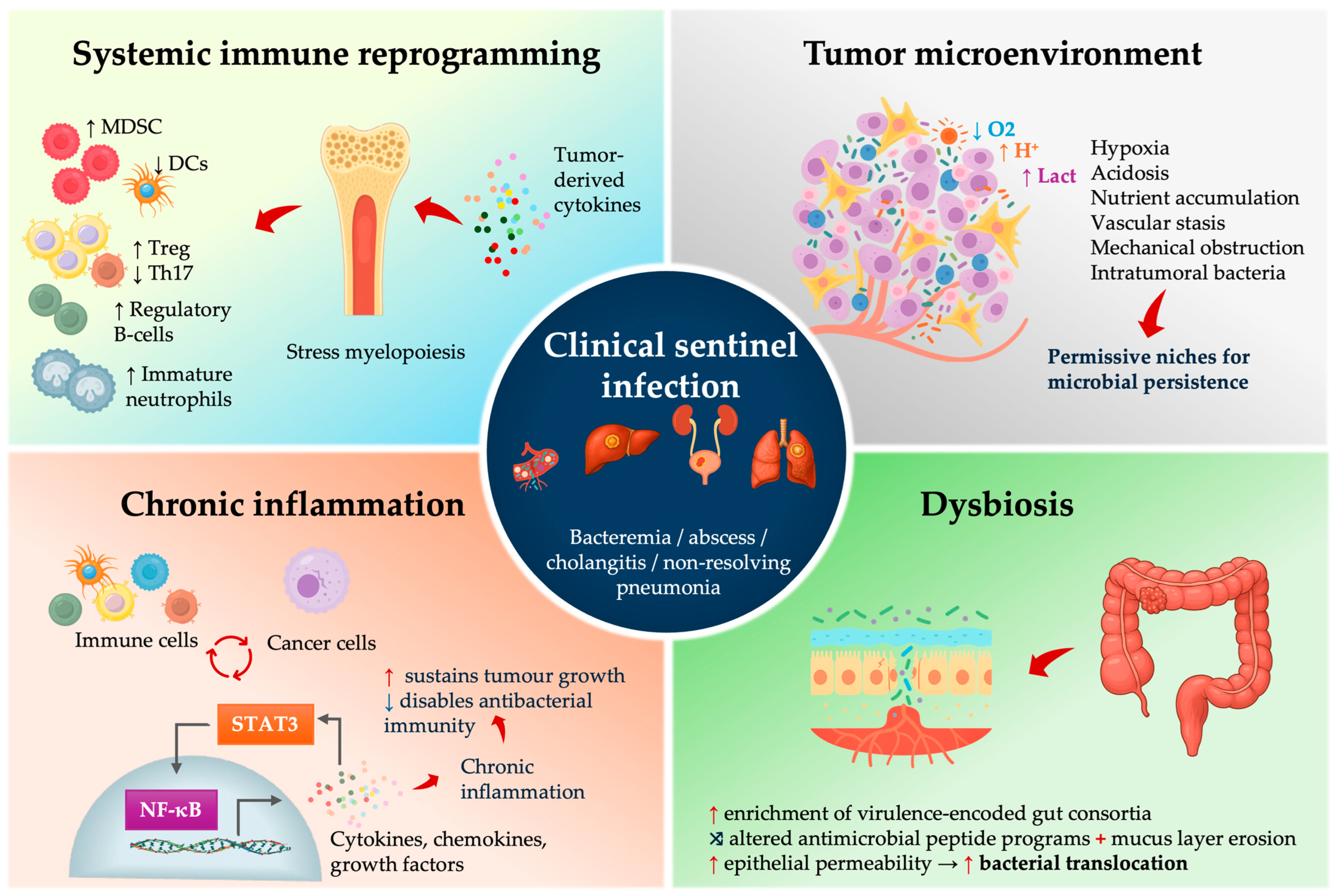
4. Mechanistic Insights: How Tumors Enable Infection
4.1. Early Systemic Immune Reprogramming in Cancer—Relevance for Infection Biology
4.2. The TME as a Microbial Incubator
4.3. Dysbiosis, Microbial Virulence Programs, and Translocation Risk
4.4. Chronic Inflammation as Integrator and Amplifier
5. Clinical Red Flags: Infection Signatures Suggesting Malignancy
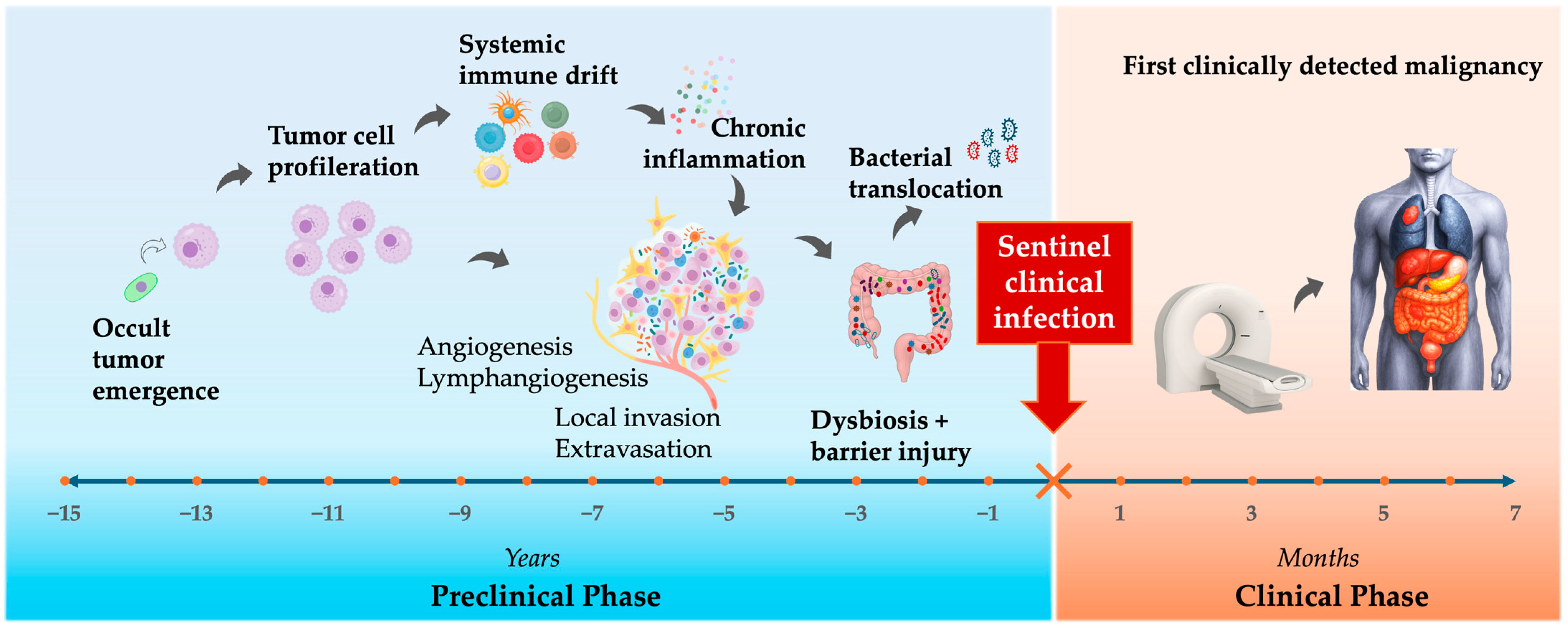
6. From Clue to Diagnosis—“Don’t Miss the Window”
7. Future Directions—From Sentinel Infections to Early Cancer Detection
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| aHR | Adjusted hazard ratio |
| CAP | Community-acquired pneumonia |
| CRC | Colorectal cancer |
| CRN | Colorectal neoplasia |
| CT | Computed tomography |
| CXCL | C-X-C motif chemokine ligand |
| FUO | Fever of unknown origin |
| GBC | Gallbladder cancer |
| GI | Gastrointestinal |
| GPAC | Gram-positive anaerobic cocci |
| GNR | Gram-negative rod |
| HBV | Hepatitis B virus |
| HCC | Hepatocellular carcinoma |
| HCV | Hepatitis C virus |
| HR | Hazard ratio |
| IFN-γ | Interferon gamma |
| IL | Interleukin |
| IRR | Incidence rate ratio |
| IV | Intravenous |
| LUTI | Lower urinary tract infection |
| MDSC | Myeloid-derived suppressor cells |
| MRCP | Magnetic resonance cholangiopancreatography |
| MRI | Magnetic resonance imaging |
| NNT | Number needed to test |
| OR | Odds ratio |
| PLA | Pyogenic liver abscess |
| ROS | Reactive oxygen species |
| RR | Relative risk |
| SARI | Severe acute respiratory infection |
| SIR | Standardized incidence ratio |
| STAT3 | Signal transducer and activator of transcription 3 |
| TGF-β | Transforming growth factor beta |
| Th17 | T-helper 17 cells |
| TNF-α | Tumor necrosis factor alpha |
| TME | Tumor microenvironment |
| UTI | Urinary tract infection |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Aktary, M.L.; Ghebrial, M.; Wang, Q.; Shack, L.; Robson, P.J.; Kopciuk, K.A. Health-Related and Behavioral Factors Associated with Lung Cancer Stage at Diagnosis: Observations from Alberta’s Tomorrow Project. Cancer Control 2022, 29, 10732748221091678. [Google Scholar] [CrossRef]
- Dantas, A.A.G.; de Oliveira, N.P.D.; Costa, G.A.B.; Martins, L.F.L.; dos Santos, J.E.M.; Migowski, A.; Cancela, M.d.C.; de Souza, D.L.B. Multilevel analysis of social determinants of advanced stage colorectal cancer diagnosis. Sci. Rep. 2024, 14, 9667. [Google Scholar] [CrossRef] [PubMed]
- Wassie, L.A.; Mekonnen, C.K.; Tiruneh, Y.M.; Melkam, M.; Belachew, E.A.; Zegeye, A.F. Advanced-stage presentation of cancer at the time of diagnosis and its associated factors among adult cancer patients at Northwest Amhara comprehensive specialized hospitals, Northwest Ethiopia 2022. BMC Cancer 2024, 24, 68. [Google Scholar] [CrossRef]
- Mc, C.W.; Mason, J.M., 3rd. Enterococcal endocarditis associated with carcinoma of the sigmoid; report of a case. J. Med. Assoc. State Ala. 1951, 21, 162–166. [Google Scholar]
- Klein, R.S.; Recco, R.A.; Catalano, M.T.; Edberg, S.C.; Casey, J.I.; Steigbigel, N.H. Association of Streptococcus bovis with Carcinoma of the Colon. N. Engl. J. Med. 1977, 297, 800–802. [Google Scholar] [CrossRef] [PubMed]
- Corredoira, J.; Grau, I.; Garcia-Rodriguez, J.F.; Alonso-Garcia, P.; Garcia-Pais, M.; Rabuñal, R.; Garcia-Garrote, F.; Ardanuy, C.; Coira, A.; Lopez-Alvarez, M.; et al. The clinical epidemiology and malignancies associated with Streptococcus bovis biotypes in 506 cases of bloodstream infections. J. Infect. 2015, 71, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Gotland, N.; Uhre, M.L.; Sandholdt, H.; Mejer, N.; Lundbo, L.F.; Petersen, A.; Larsen, A.R.; Benfield, T. Increased risk of incident primary cancer after Staphylococcus aureus bacteremia. Medicine 2020, 99, e19984. [Google Scholar] [CrossRef]
- Justesen, U.S.; Ellebæk, M.B.; Qvist, N.; Iachina, M.; Frimodt-Møller, N.; Søes, L.M.; Skovgaard, S.; Lemming, L.; Samulioniene, J.; Andersen, S.L.; et al. Colorectal cancer and association with anaerobic bacteraemia: A Danish nationwide population-based cohort study. J. Infect. 2024, 89, 106212. [Google Scholar] [CrossRef]
- Lai, H.; Lin, C.; Cheng, K.; Kao, J.; Chou, J.; Peng, C.; Lai, S.; Chen, P.; Sung, F. Increased Incidence of Gastrointestinal Cancers Among Patients with Pyogenic Liver Abscess: A Population-Based Cohort Study. Gastroenterology 2014, 146, 129–137.e1. [Google Scholar] [CrossRef]
- Mohan, B.P.; Aravamudan, V.M.; Khan, S.R.; Chandan, S.; Ponnada, S.; Asokkumar, R.; Navaneethan, U.; Adler, D.G. Prevalence of colorectal cancer in cryptogenic pyogenic liver abscess patients. Do they need screening colonoscopy? A systematic review and meta-analysis. Dig. Liver Dis. 2019, 51, 1641–1645. [Google Scholar] [CrossRef] [PubMed]
- Søgaard, K.K.; Farkas, D.K.; Pedersen, L.; Weiss, N.S.; Thomsen, R.W.; Sørensen, H. Pneumonia and the incidence of cancer: A Danish nationwide cohort study. J. Intern. Med. 2014, 277, 429–438. [Google Scholar] [CrossRef]
- Søgaard, K.K.; Farkas, D.K.; Søgaard, M.; Schønheyder, H.C.; Thomsen, R.W.; Sørensen, H.T. Gram-negative bacteremia as a clinical marker of occult malignancy. J. Infect. 2017, 74, 153–162. [Google Scholar] [CrossRef]
- Laupland, K.B.; Edwards, F.; Furuya-Kanamori, L.; Paterson, D.L.; Harris, P.N. Bloodstream Infection and Colorectal Cancer Risk in Queensland Australia, 2000–2019. Am. J. Med. 2023, 136, 896–901. [Google Scholar] [CrossRef]
- Søgaard, K.K.; Veres, K.; Vandenbroucke-Grauls, C.M.; Vandenbroucke, J.P.; Sørensen, H.T.; Schønheyder, H.C. Community-Acquired Escherichia coli Bacteremia after Age 50 and Subsequent Incidence of a Cancer Diagnosis: A Danish Population–Based Cohort Study. Cancer Epidemiol. Biomark. Prev. 2020, 29, 2626–2632. [Google Scholar] [CrossRef]
- Shepshelovich, D.; Barda, N.; Goldvaser, H.; Dagan, N.; Zer, A.; Diker-Cohen, T.; Balicer, R.; Gafter-Gvili, A. Incidence of lung cancer following pneumonia in smokers: A population-based study. QJM Int. J. Med. 2021, 115, 287–291. [Google Scholar] [CrossRef]
- Kwong, T.N.; Wang, X.; Nakatsu, G.; Chow, T.C.; Tipoe, T.; Dai, R.Z.; Tsoi, K.K.; Wong, M.C.; Tse, G.; Chan, M.T.; et al. Association Between Bacteremia from Specific Microbes and Subsequent Diagnosis of Colorectal Cancer. Gastroenterology 2018, 155, 383–390.e8. [Google Scholar] [CrossRef]
- Gaab, M.E.; Lozano, P.O.; Ibañez, D.; Manese, K.D.; Riego, F.M.; Tiongco, R.E.; Albano, P.M. A Meta-Analysis on the Association of Colibactin-Producing pks+ Escherichia coli with the Development of Colorectal Cancer. Lab. Med. 2022, 54, 75–82. [Google Scholar] [CrossRef]
- Abe, E.; Ishikawa, K.; Onishi, K.; Mori, N. Anaerobic gram-negative rod bacteremia as a marker of gastrointestinal cancer in Japanese patients: A single-center retrospective study. Chin. Clin. Oncol. 2024, 13, 2. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, R.W.; Farkas, D.K.; Friis, S.; Sværke, C.; Ording, A.G.; Nørgaard, M.; Sørensen, H.T. Endocarditis and Risk of Cancer: A Danish Nationwide Cohort Study. Am. J. Med. 2013, 126, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.; Chiu, C.; Rayner, C.K.; Wu, K.; Chiu, Y.; Hu, M.; Chuah, S.; Tai, W.; Liang, C.; Wang, H. Associated factors in Streptococcus bovis bacteremia and colorectal cancer. Kaohsiung J. Med. Sci. 2016, 32, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Ursi, M.P.; Bertolino, L.; Andini, R.; D’Amico, F.; Iossa, D.; Karruli, A.; D’Avenia, E.; Manduca, S.; Bernardo, M.; Zampino, R.; et al. Enterococcal infective endocarditis is a marker of current occult or future incident colorectal neoplasia. Eur. J. Intern. Med. 2021, 83, 68–73. [Google Scholar] [CrossRef]
- Østergaard, L.; Dahl, A.; Chamat-Hedemand, S.; Stahl, A.; Pries-Heje, M.; Moser, C.; Søgaard, K.; Agergaard, C.; Mortensen, K.; Iversen, K.; et al. Prevalence of colorectal cancer in patients with Enterococcus faecalis blood stream infection: A nationwide study. J. Infect. 2025, 91, 106644. [Google Scholar] [CrossRef]
- Huang, W.; Chang, J.W.; See, L.; Tu, H.; Chen, J.; Liaw, C.; Lin, Y.; Yang, T. Higher rate of colorectal cancer among patients with pyogenic liver abscess with Klebsiella pneumoniae than those without: An 11-year follow-up study. Color. Dis. 2012, 14, e794–e801. [Google Scholar] [CrossRef]
- Suzuki, H.; Kidder, I.; Tanaka, T.; Goto, M. Incidence of Colorectal Cancer in Patients Diagnosed with Pyogenic Liver Abscess. JAMA Netw. Open 2023, 6, e2348218. [Google Scholar] [CrossRef]
- Helicobacter and Cancer Collaborative Group. Gastric cancer and Helicobacter pylori: A combined analysis of 12 case control studies nested within prospective cohorts. Gut 2001, 49, 347–353. [Google Scholar] [CrossRef]
- Li, D.; Jiang, S.-F.; Lei, N.Y.; Shah, S.C.; Corley, D.A. Effect of Helicobacter pylori Eradication Therapy on the Incidence of Noncardia Gastric Adenocarcinoma in a Large Diverse Population in the United States. Gastroenterology 2023, 165, 391–401.e2. [Google Scholar] [CrossRef]
- Lin, Y.-T.; Liu, C.-J.; Chen, T.-J.; Chen, T.-L.; Yeh, Y.-C.; Wu, H.-S.; Tseng, C.-P.; Wang, F.-D.; Tzeng, C.-H.; Fung, C.-P. Pyogenic Liver Abscess as the Initial Manifestation of Underlying Hepatocellular Carcinoma. Am. J. Med. 2011, 124, 1158–1164. [Google Scholar] [CrossRef] [PubMed]
- Koshiol, J.; Wozniak, A.; Cook, P.; Adaniel, C.; Acevedo, J.; Azócar, L.; Hsing, A.W.; Roa, J.C.; Pasetti, M.F.; Miquel, J.F.; et al. Salmonella enterica serovar Typhi and gallbladder cancer: A case–control study and meta-analysis. Cancer Med. 2016, 5, 3310–3325. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Alekseyenko, A.V.; Wu, J.; Peters, B.A.; Jacobs, E.J.; Gapstur, S.M.; Purdue, M.P.; Abnet, C.C.; Stolzenberg-Solomon, R.; Miller, G.; et al. Human oral microbiome and prospective risk for pancreatic cancer: A population-based nested case-control study. Gut 2018, 67, 120–127. [Google Scholar] [CrossRef]
- Zhan, P.; Suo, L.-J.; Qian, Q.; Shen, X.-K.; Qiu, L.-X.; Yu, L.-K.; Song, Y. Chlamydia pneumoniae infection and lung cancer risk: A meta-analysis. Eur. J. Cancer 2011, 47, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Lin, C.; Liang, J.; Liu, S.; Sung, F.; Chang, Y.; Kao, C. Urinary tract infection increases subsequent urinary tract cancer risk: A population-based cohort study. Cancer Sci. 2013, 104, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, S.H.; Hanum, N.; Grotenhuis, A.J.; Castaño-Vinyals, G.; van der Heijden, A.G.; Aben, K.K.; Mysorekar, I.U.; Kiemeney, L.A. Recurrent urinary tract infection and risk of bladder cancer in the Nijmegen bladder cancer study. Br. J. Cancer 2014, 112, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Pelucchi, C.; Talamini, R.; Negri, E.; Franceschi, S.; La Vecchia, C. Genital and urinary tract diseases and prostate cancer risk. Eur. J. Cancer Prev. 2006, 15, 254–257. [Google Scholar] [CrossRef]
- Jansåker, F.; Li, X.; Sundquist, K. Acute cystitis and subsequent risk of urogenital cancer: A national cohort study from Sweden. BMJ Public Health 2025, 3, e002495. [Google Scholar] [CrossRef]
- Fan, C.-Y.; Huang, W.-Y.; Lin, K.-T.; Lin, C.-S.; Chao, H.-L.; Yang, J.-F.; Lin, C.-L.; Kao, C.-H. Lower Urinary Tract Infection and Subsequent Risk of Prostate Cancer: A Nationwide Population-Based Cohort Study. PLoS ONE 2017, 12, e0168254. [Google Scholar] [CrossRef]
- Caini, S.; Gandini, S.; Dudas, M.; Bremer, V.; Severi, E.; Gherasim, A. Sexually transmitted infections and prostate cancer risk: A systematic review and meta-analysis. Cancer Epidemiol. 2014, 38, 329–338. [Google Scholar] [CrossRef]
- Zhu, H.; Shen, Z.; Luo, H.; Zhang, W.; Zhu, X. Chlamydia Trachomatis Infection-Associated Risk of Cervical Cancer. Medicine 2016, 95, e3077. [Google Scholar] [CrossRef]
- McShane, C.M.; Murray, L.J.; Engels, E.A.; Landgren, O.; Anderson, L.A. Common community-acquired infections and subsequent risk of multiple myeloma: A population-based study. Int. J. Cancer 2013, 134, 1734–1740. [Google Scholar] [CrossRef]
- Rawla, P.; Vellipuram, A.R.; Bandaru, S.S.; Raj, J.P. Colon Carcinoma Presenting as Streptococcus anginosus Bacteremia and Liver Abscess. Gastroenterol. Res. 2017, 10, 376–379. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Su, S.-L.; Li, C.-W.; Tsai, C.-S.; Lo, C.-L.; Syue, L.-S.; Li, M.-C.; Lee, C.-C.; Lee, N.-Y.; Ko, W.-C.; et al. Pancreaticobiliary Cancers and Aeromonas Isolates Carrying Type III Secretion System Genes ascF-ascG Are Associated with Increased Mortality: An Analysis of 164 Aeromonas Infection Episodes in Southern Taiwan. Front. Cell. Infect. Microbiol. 2021, 11, 749269. [Google Scholar] [CrossRef]
- Melnick, S.; Nazir, S.; Chwiecko, B.; Lloyd, B. There may be more than meets the eye with Clostridium perfringens bacteremia. J. Community Hosp. Intern. Med. Perspect. 2017, 7, 134–135. [Google Scholar] [CrossRef] [PubMed]
- Suh, S.W.; Kim, Y.S.; Park, J.M.; Kim, M.K.; Park, Y.G.; Chi, K.C.; Lee, J.H.; Lim, H.M. Omental Actinomycosis Coexisting with Colon Cancer. J. Korean Surg. Soc. 2009, 77, S17–S21. [Google Scholar] [CrossRef]
- Snellings, R.; Matsuo, T.; Wurster, S.; Jiang, Y.; Tarrand, J.; Cho, S.-Y.; Kontoyiannis, D.P. P-2294. Listeriosis in cancer patients: Uncommon and protean. Open Forum Infect. Dis. 2025, 12, ofae631.2447. [Google Scholar] [CrossRef]
- Masood, U.; Sharma, A.; Lowe, D.; Khan, R.; Manocha, D. Colorectal Cancer Associated with Streptococcus anginosus Bacteremia and Liver Abscesses. Case Rep. Gastroenterol. 2016, 10, 769–774. [Google Scholar] [CrossRef]
- Justesen, U.S.; Nielsen, S.L.; Jensen, T.G.; Dessau, R.B.; Møller, J.K.; Coia, J.E.; Andersen, S.L.; Pedersen, C.; Gradel, K.O. Bacteremia with Anaerobic Bacteria and Association with Colorectal Cancer: A Population-based Cohort Study. Clin. Infect. Dis. 2022, 75, 1747–1753. [Google Scholar] [CrossRef]
- Wu, S.; Rhee, K.-J.; Zhang, M.; Franco, A.; Sears, C.L. Bacteroides fragilis toxin stimulates intestinal epithelial cell shedding and γ-secretase-dependent E-cadherin cleavage. J. Cell Sci. 2007, 120, 1944–1952. [Google Scholar] [CrossRef]
- Rubinstein, M.R.; Wang, X.; Liu, W.; Hao, Y.; Cai, G.; Han, Y.W. Fusobacterium nucleatum Promotes Colorectal Carcinogenesis by Modulating E-Cadherin/β-Catenin Signaling via its FadA Adhesin. Cell Host Microbe 2013, 14, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Littman, A.J.; White, E.; Jackson, L.A.; Thornquist, M.D.; Gaydos, C.A.; Goodman, G.E.; Vaughan, T.L. Chlamydia pneumoniae Infection and Risk of Lung Cancer. Cancer Epidemiol. Biomark. Prev. 2004, 13, 1624–1630. [Google Scholar] [CrossRef]
- Goto, T. Airway Microbiota as a Modulator of Lung Cancer. Int. J. Mol. Sci. 2020, 21, 3044. [Google Scholar] [CrossRef]
- Lee, S.H.; Sung, J.Y.; Yong, D.; Chun, J.; Kim, S.Y.; Song, J.H.; Chung, K.S.; Kim, E.Y.; Jung, J.Y.; Kang, Y.A.; et al. Characterization of microbiome in bronchoalveolar lavage fluid of patients with lung cancer comparing with benign mass like lesions. Lung Cancer 2016, 102, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zeng, H.; Liu, K.; Pan, H.; Wang, B.; Zhu, M.; Wang, J.; Wang, H.; Chen, H.; Shen, D.; et al. Microbiota profiles in the saliva, cancerous tissues and its companion paracancerous tissues among Chinese patients with lung cancer. BMC Microbiol. 2023, 23, 237. [Google Scholar] [CrossRef] [PubMed]
- Mook, P.; O’bRien, S.J.; Gillespie, I.A. Concurrent Conditions and Human Listeriosis, England, 1999–2009. Emerg. Infect. Dis. 2011, 17, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Zhang, P.; Jiao, G.; Lv, J.; Ma, C.; Song, X.; Zhang, J.; Wu, C.; Li, R.; Zhu, H. Mimicking uterine malignancy: Pelvic actinomycosis with giant uterine leiomyoma. IDCases 2021, 23, e00878. [Google Scholar] [CrossRef]
- Saramago, S.M.; Cominho, J.C.; Proença, S.S.M.; Conde, P.J.C.; Nunes, F.M.P. Pelvic Actinomycosis Mimicking Pelvic Malignancy. Rev. Bras. Hematol. Hemoter. 2019, 41, 463–466. [Google Scholar] [CrossRef]
- Čelešnik, H.; Potočnik, U. Peripheral Blood Transcriptome in Breast Cancer Patients as a Source of Less Invasive Immune Biomarkers for Personalized Medicine, and Implications for Triple Negative Breast Cancer. Cancers 2022, 14, 591. [Google Scholar] [CrossRef]
- Martinez-Usatorre, A.; Ciarloni, L.; Angelino, P.; Wosika, V.; Conforte, A.J.; Costa, S.S.F.; Durandau, E.; Monnier-Benoit, S.; Satizabal, H.F.; Despraz, J.; et al. Human blood cell transcriptomics unveils dynamic systemic immune modulation along colorectal cancer progression. J. Immunother. Cancer 2024, 12, e009888. [Google Scholar] [CrossRef]
- Qi, F.; Gao, F.; Cai, Y.; Han, X.; Qi, Y.; Ni, J.; Sun, J.; Huang, S.; Chen, S.; Wu, C.; et al. Complex Age- and Cancer-Related Changes in Human Blood Transcriptome—Implications for Pan-Cancer Diagnostics. Front. Genet. 2021, 12, 746879. [Google Scholar] [CrossRef]
- Marx, S.; Wilken, F.; Miebach, L.; Ispirjan, M.; Kinnen, F.; Paul, S.; Bien-Möller, S.; Freund, E.; Baldauf, J.; Fleck, S.; et al. Immunophenotyping of Circulating and Intratumoral Myeloid and T Cells in Glioblastoma Patients. Cancers 2022, 14, 5751. [Google Scholar] [CrossRef]
- Casbon, A.-J.; Reynaud, D.; Park, C.; Khuc, E.; Gan, D.D.; Schepers, K.; Passegué, E.; Werb, Z. Invasive breast cancer reprograms early myeloid differentiation in the bone marrow to generate immunosuppressive neutrophils. Proc. Natl. Acad. Sci. USA 2015, 112, E566–E575. [Google Scholar] [CrossRef]
- Li, K.; Shi, H.; Zhang, B.; Ou, X.; Ma, Q.; Chen, Y.; Shu, P.; Li, D.; Wang, Y. Myeloid-derived suppressor cells as immunosuppressive regulators and therapeutic targets in cancer. Signal Transduct. Target. Ther. 2021, 6, 362. [Google Scholar] [CrossRef]
- Gabrilovich, D.I.; Ostrand-Rosenberg, S.; Bronte, V. Coordinated regulation of myeloid cells by tumours. Nat. Rev. Immunol. 2012, 12, 253–268. [Google Scholar] [CrossRef]
- Wang, L.; Jia, B.; Claxton, D.F.; Ehmann, W.C.; Rybka, W.B.; Mineishi, S.; Naik, S.; Khawaja, M.R.; Sivik, J.; Han, J.; et al. VISTA is highly expressed on MDSCs and mediates an inhibition of T cell response in patients with AML. OncoImmunology 2018, 7, e1469594. [Google Scholar] [CrossRef]
- Gobert, M.; Treilleux, I.; Bendriss-Vermare, N.; Bachelot, T.; Goddard-Leon, S.; Arfi, V.; Biota, C.; Doffin, A.C.; Durand, I.; Olive, D.; et al. Regulatory T Cells Recruited through CCL22/CCR4 Are Selectively Activated in Lymphoid Infiltrates Surrounding Primary Breast Tumors and Lead to an Adverse Clinical Outcome. Cancer Res. 2009, 69, 2000–2009. [Google Scholar] [CrossRef]
- Mirlekar, B. Tumor promoting roles of IL-10, TGF-β, IL-4, and IL-35: Its implications in cancer immunotherapy. SAGE Open Med. 2022, 10. [Google Scholar] [CrossRef]
- Chaudhary, B.; Elkord, E. Regulatory T Cells in the Tumor Microenvironment and Cancer Progression: Role and Therapeutic Targeting. Vaccines 2016, 4, 28. [Google Scholar] [CrossRef] [PubMed]
- Blaschitz, C.; Raffatellu, M. Th17 Cytokines and the Gut Mucosal Barrier. J. Clin. Immunol. 2010, 30, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Pérez, M.M.; Martins, L.M.S.; Dias, M.S.; Pereira, C.A.; Leite, J.A.; Gonçalves, E.C.S.; de Almeida, P.Z.; de Freitas, E.N.; Tostes, R.C.; Ramos, S.G.; et al. Interleukin-17/interleukin-17 receptor axis elicits intestinal neutrophil migration, restrains gut dysbiosis and lipopolysaccharide translocation in high-fat diet-induced metabolic syndrome model. Immunology 2018, 156, 339–355. [Google Scholar] [CrossRef]
- Hiam-Galvez, K.J.; Allen, B.M.; Spitzer, M.H. Systemic immunity in cancer. Nat. Rev. Cancer 2021, 21, 345–359. [Google Scholar] [CrossRef]
- Meyer, M.A.; Baer, J.M.; Knolhoff, B.L.; Nywening, T.M.; Panni, R.Z.; Su, X.; Weilbaecher, K.N.; Hawkins, W.G.; Ma, C.; Fields, R.C.; et al. Breast and pancreatic cancer interrupt IRF8-dependent dendritic cell development to overcome immune surveillance. Nat. Commun. 2018, 9, 1250. [Google Scholar] [CrossRef] [PubMed]
- Giles, A.J.; Reid, C.M.; Evans, J.D.; Murgai, M.; Vicioso, Y.; Highfill, S.L.; Kasai, M.; Vahdat, L.; Mackall, C.L.; Lyden, D.; et al. Activation of Hematopoietic Stem/Progenitor Cells Promotes Immunosuppression Within the Pre–metastatic Niche. Cancer Res. 2016, 76, 1335–1347. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.-C.; Sun, H.-W.; Chen, H.-T.; Liang, J.; Yu, X.-J.; Wu, C.; Wang, Z.; Zheng, L. Circulating hematopoietic stem and progenitor cells are myeloid-biased in cancer patients. Proc. Natl. Acad. Sci. USA 2014, 111, 4221–4226. [Google Scholar] [CrossRef] [PubMed]
- Ciarloni, L.; Hosseinian, S.; Monnier-Benoit, S.; Imaizumi, N.; Dorta, G.; Ruegg, C. On behalf of the DGNP-COL-0310 Study Group. Discovery of a 29-Gene Panel in Peripheral Blood Mononuclear Cells for the Detection of Colorectal Cancer and Adenomas Using High Throughput Real-Time PCR. PLoS ONE 2015, 10, e0123904. [Google Scholar] [CrossRef]
- Khouzam, R.A.; Zaarour, R.F.; Brodaczewska, K.; Azakir, B.; Venkatesh, G.H.; Thiery, J.; Terry, S.; Chouaib, S. The Effect of Hypoxia and Hypoxia-Associated Pathways in the Regulation of Antitumor Response: Friends or Foes? Front. Immunol. 2022, 13, 828875. [Google Scholar] [CrossRef]
- Kelly, C.J.; Glover, L.E.; Campbell, E.L.; Kominsky, D.J.; Ehrentraut, S.F.; Bowers, B.E.; Bayless, A.J.; Saeedi, B.J.; Colgan, S.P. Fundamental role for HIF-1α in constitutive expression of human β defensin-1. Mucosal Immunol. 2013, 6, 1110–1118. [Google Scholar] [CrossRef]
- Saeedi, B.J.; Kao, D.J.; Kitzenberg, D.A.; Dobrinskikh, E.; Schwisow, K.D.; Masterson, J.C.; Kendrick, A.A.; Kelly, C.J.; Bayless, A.J.; Kominsky, D.J.; et al. HIF-dependent regulation of claudin-1 is central to intestinal epithelial tight junction integrity. Mol. Biol. Cell 2015, 26, 2252–2262. [Google Scholar] [CrossRef]
- Sagar, P.M.; MacFie, J.; Sedman, P.; May, J.; Mancey-Jones, B.; Johnstone, D. Intestinal obstruction promotes gut translocation of bacteria. Dis. Colon Rectum 1995, 38, 640–644. [Google Scholar] [CrossRef]
- Valvani, A.; Martin, A.; Devarajan, A.; Chandy, D. Postobstructive pneumonia in lung cancer. Ann. Transl. Med. 2019, 7, 357. [Google Scholar] [CrossRef]
- Ciernikova, S.; Novisedlakova, M.; Cholujova, D.; Stevurkova, V.; Mego, M. The Emerging Role of Microbiota and Microbiome in Pancreatic Ductal Adenocarcinoma. Biomedicines 2020, 8, 565. [Google Scholar] [CrossRef] [PubMed]
- Nejman, D.; Livyatan, I.; Fuks, G.; Gavert, N.; Zwang, Y.; Geller, L.T.; Rotter-Maskowitz, A.; Weiser, R.; Mallel, G.; Gigi, E.; et al. The human tumor microbiome is composed of tumor type–specific intracellular bacteria. Science 2020, 368, 973–980. [Google Scholar] [CrossRef]
- Nougayrède, J.-P.; Homburg, S.; Taieb, F.; Boury, M.; Brzuszkiewicz, E.; Gottschalk, G.; Buchrieser, C.; Hacker, J.; Dobrindt, U.; Oswald, E. Escherichia coli Induces DNA Double-Strand Breaks in Eukaryotic Cells. Science 2006, 313, 848–851. [Google Scholar] [CrossRef]
- Pleguezuelos-Manzano, C.; Puschhof, J.; Rosendahl Huber, A.; Van Hoeck, A.; Wood, H.M.; Nomburg, J.; Gurjao, C.; Manders, F.; Dalmasso, G.; Stege, P.B.; et al. Mutational signature in colorectal cancer caused by genotoxic pks+ E coli. Nature 2020, 580, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Chung, L.; Orberg, E.T.; Geis, A.L.; Chan, J.L.; Fu, K.; Shields, C.E.D.; Dejea, C.M.; Fathi, P.; Chen, J.; Finard, B.B.; et al. Bacteroides fragilis Toxin Coordinates a Pro-carcinogenic Inflammatory Cascade via Targeting of Colonic Epithelial Cells. Cell Host Microbe 2018, 23, 203–214.e5. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-G.; Hwang, S.; Gwon, S.-Y.; Park, C.; Jo, M.; Hong, J.-E.; Rhee, K.-J. Bacteroides fragilis Toxin Induces Intestinal Epithelial Cell Secretion of Interleukin-8 by the E-Cadherin/β-Catenin/NF-κB Dependent Pathway. Biomedicines 2022, 10, 827. [Google Scholar] [CrossRef] [PubMed]
- Gur, C.; Ibrahim, Y.; Isaacson, B.; Yamin, R.; Abed, J.; Gamliel, M.; Enk, J.; Bar-On, Y.; Stanietsky-Kaynan, N.; Coppenhagen-Glazer, S.; et al. Binding of the Fap2 Protein of Fusobacterium nucleatum to Human Inhibitory Receptor TIGIT Protects Tumors from Immune Cell Attack. Immunity 2015, 42, 344–355. [Google Scholar] [CrossRef]
- Yu, T.; Guo, F.; Yu, Y.; Sun, T.; Ma, D.; Han, J.; Qian, Y.; Kryczek, I.; Sun, D.; Nagarsheth, N.; et al. Fusobacterium nucleatum Promotes Chemoresistance to Colorectal Cancer by Modulating Autophagy. Cell 2017, 170, 548–563.e16. [Google Scholar] [CrossRef] [PubMed]
- Dupont, A.; Heinbockel, L.; Brandenburg, K.; Hornef, M.W. Antimicrobial peptides and the enteric mucus layer act in concert to protect the intestinal mucosa. Gut Microbes 2014, 5, 761–765. [Google Scholar] [CrossRef]
- Dougherty, M.W.; Jobin, C. Intestinal bacteria and colorectal cancer: Etiology and treatment. Gut Microbes 2023, 15, 2185028. [Google Scholar] [CrossRef]
- Grivennikov, S.I.; Karin, M. Dangerous liaisons: STAT3 and NF-κB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev. 2010, 21, 11–19. [Google Scholar] [CrossRef]
- Hirano, T. IL-6 in inflammation, autoimmunity and cancer. Int. Immunol. 2020, 33, 127–148. [Google Scholar] [CrossRef]
- Li, T.-T.; Ogino, S.; Qian, Z.R. Toll-like receptor signaling in colorectal cancer: Carcinogenesis to cancer therapy. World J. Gastroenterol. 2014, 20, 17699–17708. [Google Scholar] [CrossRef]
- Prasad, S.V.; Fiedoruk, K.; Daniluk, T.; Piktel, E.; Bucki, R. Expression and Function of Host Defense Peptides at Inflammation Sites. Int. J. Mol. Sci. 2019, 21, 104. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Luo, Y.; Lv, Y.; Huang, C.; Sheng, Q.; Zhao, P.; Ye, J.; Jiang, W.; Liu, L.; Song, X.; et al. Clostridium difficile colonization in preoperative colorectal cancer patients. Oncotarget 2017, 8, 11877–11886. [Google Scholar] [CrossRef] [PubMed]
- Goodman, A.L.; Packham, A.; Sharkey, A.R.; Cook, G.J. Advanced Imaging for Detection of Foci of Infection in Staphylococcus aureus Bacteremia- Can a Scan Save Lives? Semin. Nucl. Med. 2023, 53, 175–183. [Google Scholar] [CrossRef]
- Vos, F.J.; Bleeker-Rovers, C.P.; Sturm, P.D.; Krabbe, P.F.; van Dijk, A.P.; Cuijpers, M.L.; Adang, E.M.; Wanten, G.J.; Kullberg, B.-J.; Oyen, W.J. 18F-FDG PET/CT for Detection of Metastatic Infection in Gram-Positive Bacteremia. J. Nucl. Med. 2010, 51, 1234–1240. [Google Scholar] [CrossRef]
- Jeong, S.W.; Jang, J.Y.; Lee, T.H.; Kim, H.G.; Hong, S.W.; Park, S.H.; Kim, S.G.; Cheon, Y.K.; Kim, Y.S.; Cho, Y.D.; et al. Cryptogenic pyogenic liver abscess as the herald of colon cancer. J. Gastroenterol. Hepatol. 2012, 27, 248–255. [Google Scholar] [CrossRef]
- Heo, N.-Y.; Hong, Y.M.; Kim, T.O.; Moon, Y.S.; Yang, S.Y.; Park, S.H.; Park, J.; Choi, J.H.; Kim, S.-M.; Yoon, K.T.; et al. The Prevalence of Colonic Neoplasm in Cryptogenic Pyogenic Liver Abscess: A Prospectively Enrolled Cross-sectional Study. Korean J. Gastroenterol. 2016, 68, 195–201. [Google Scholar] [CrossRef]
- Abdulamir, A.S.; Hafidh, R.R.; Abu Bakar, F. The association of Streptococcus bovis/gallolyticus with colorectal tumors: The nature and the underlying mechanisms of its etiological role. J. Exp. Clin. Cancer Res. 2011, 30, 11. [Google Scholar] [CrossRef] [PubMed]
- Corredoira-Sanchez, J.; Garcia-Garrote, F.; Rabunal, R.; Lopez-Roses, L.; Garcia-Pais, M.J.; Castro, E.; Gonzalez-Soler, R.; Coira, A.; Pita, J.; Lopez-Alvarez, M.J.; et al. Association Between Bacteremia Due to Streptococcus gallolyticus subsp. gallolyticus (Streptococcus bovis I) and Colorectal Neoplasia: A Case-Control Study. Clin. Infect. Dis. 2012, 55, 491–496. [Google Scholar] [CrossRef]
- Chaudhuri, A.D.; Mukherjee, S.; Nandi, S.; Bhuniya, S.; Tapadar, S.R.; Saha, M. A study on non-resolving pneumonia with special reference to role of fiberoptic bronchoscopy. Lung India 2013, 30, 27–32. [Google Scholar] [CrossRef]
- Lai, H.-C.; Lin, H.-C. Cryptogenic pyogenic liver abscess as a sign of colorectal cancer: A population-based 5-year follow-up study. Liver Int. 2010, 30, 1387–1393. [Google Scholar] [CrossRef]
- Bodilsen, J.; Søgaard, K.K.; Nielsen, H.; Omland, L.H. Brain Abscess and Risk of Cancer. Neurology 2022, 99, E835–E842. [Google Scholar] [CrossRef] [PubMed]
- You, M.S.; Lee, S.H.; Kang, J.; Choi, Y.H.; Choi, J.H.; Shin, B.-S.; Huh, G.; Paik, W.H.; Ryu, J.K.; Kim, Y.-T.; et al. Natural Course and Risk of Cholangiocarcinoma in Patients with Recurrent Pyogenic Cholangitis: A Retrospective Cohort Study. Gut Liver 2019, 13, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Arab, T.; Malekzadegan, M.R.; Morante, J.; Cervellione, K.L.; Fein, A.M. Nonresolving pneumonia in the setting of malignancy. Curr. Opin. Pulm. Med. 2019, 25, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Raj, A.; Venugopal, K.P.P.; Musthafa, S.; Narayan, K.V. Characterising aetiologies and clinical-radiological factors of non-resolving pneumonia in a tertiary care centre. Egypt. J. Bronchol. 2024, 18, 61. [Google Scholar] [CrossRef]
- Søgaard, K.K.; Farkas, D.K.; Leisner, M.Z.; Schmidt, S.A.J.; Lash, T.L.; Sørensen, H.T. Fever of Unknown Origin and Incidence of Cancer. Clin. Infect. Dis. 2022, 75, 968–974. [Google Scholar] [CrossRef]
- Naito, T.; Tanei, M.; Ikeda, N.; Ishii, T.; Suzuki, T.; Morita, H.; Yamasaki, S.; Tamura, J.; Akazawa, K.; Yamamoto, K.; et al. Key diagnostic characteristics of fever of unknown origin in Japanese patients: A prospective multicentre study. BMJ Open 2019, 9, e032059. [Google Scholar] [CrossRef] [PubMed]
- Nagaraja, V.; Eslick, G.D. Systematic review with meta-analysis: The relationship between chronic Salmonella typhi carrier status and gall-bladder cancer. Aliment. Pharmacol. Ther. 2014, 39, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Wu, F.; Kwak, S.; Wang, C.; Usyk, M.; Freedman, N.D.; Huang, W.-Y.; Um, C.Y.; Gonda, T.A.; Oberstein, P.E.; et al. Oral Bacterial and Fungal Microbiome and Subsequent Risk for Pancreatic Cancer. JAMA Oncol. 2025, 11, 1331. [Google Scholar] [CrossRef] [PubMed]
- Kwak, S.; Wang, C.; Usyk, M.; Wu, F.; Freedman, N.D.; Huang, W.-Y.; McCullough, M.L.; Um, C.Y.; Shrubsole, M.J.; Cai, Q.; et al. Oral Microbiome and Subsequent Risk of Head and Neck Squamous Cell Cancer. JAMA Oncol. 2024, 10, 1537–1547. [Google Scholar] [CrossRef]
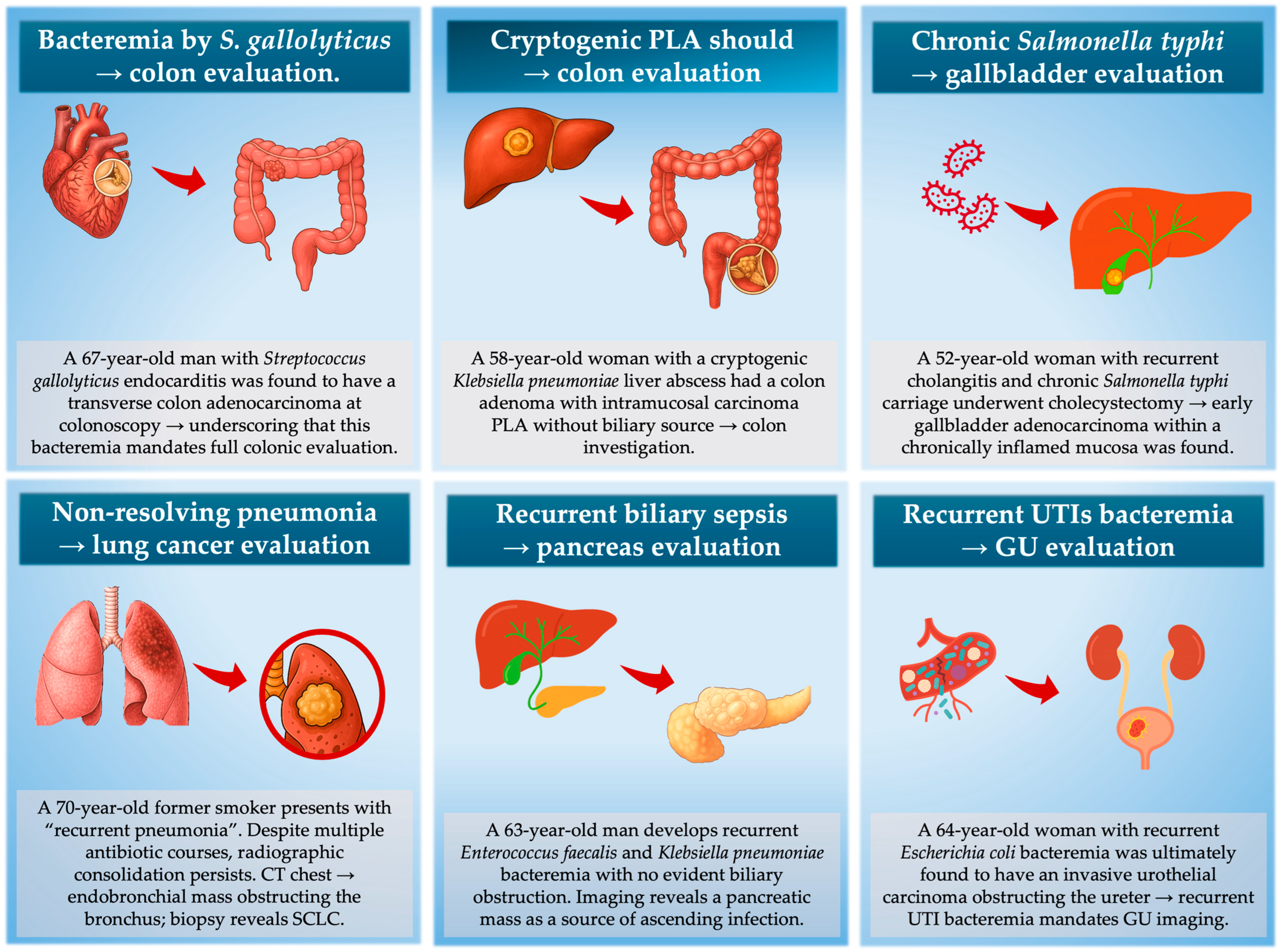
| Infection Phenotype | Immediate Targeted Cancer Evaluation |
|---|---|
| Anaerobic bacteremia (no abscess/perforation) | Colonoscopy (even if 3–5 years prior was normal) ± CT chest–abdomen–pelvis |
| Cryptogenic pyogenic liver abscess | Colonoscopy + CT chest–abdomen–pelvis ± MRCP if cholestatic enzymes |
| Recurrent cholangitis without stones/strictures | MRCP or pancreas-protocol MRI (±EUS based on ductal findings) |
| Non-resolving pneumonia with segmental/lobar collapse | Contrast CT chest (±FDG-PET/CT if available) + diagnostic bronchoscopy |
| Recurrent bacteremic UTI in older adult (no stones, no instrumentation) | Cystoscopy ± prostate MRI (men) + CT chest–abdomen–pelvis |
| Organ Domain | Sentinel Infection Phenotype | Typical Organisms | Short-Term Cancer Detection Yield */Implied NNT † | Key Sources |
|---|---|---|---|---|
| Colon | Anaerobic bacteremia (no abscess/perforation) | Bacteroides, Clostridium, Fusobacterium; pks+ E. coli | ~5–10% (≤6–12 mo) → NNT 10–20 | [9,46] |
| Cryptogenic pyogenic liver abscess | K. pneumoniae ± anaerobes | West: ~5–10% → NNT 10–20; East Asia: ~15–30% → NNT 3–7 | [10,11,25,101] | |
| Fusobacterium nucleatum brain abscess (no ear–nose–throat or sinus focus of infection) | F. nucleatum | case series signal | [102] | |
| Clostridium septicum bacteremia/gas gangrene | C. septicum | very high co-occurrence | [46] | |
| Pancreas/biliary | Recurrent cholangitis without stones/strictures | Enterobacterales (esp. Klebsiella) | ~10% over 5–10 years → NNT ~10 | [103] |
| Liver | Pyogenic liver abscess without risk factors | Klebsiella, Enterobacterales | ~2% → NNT ~50 | [28] |
| Lung | Non-resolving pneumonia > 4–6 wks despite adequate therapy (lobar collapse/mucus plug) | mixed community-acquired flora; anaerobes in obstruction | ~20–30% → NNT 3–5 | [104,105] |
| Urinary | Recurrent bacteremic UTI in older adult (esp. male or post-menopausal; no stones/instrumentation) | E. coli, Klebsiella | OR ~2–7; not well quantified | [33,35] |
| Systemic | Cryptogenic Gram-negative bacteremia (overall) | E. coli, Klebsiella, others | ~3% (≤6 mo) → NNT ≈ 33 | [13,15] |
| Fever of unknown origin | ≥50 y with persistent inflammatory signature | — | ~10–20% → NNT 5–10 | [106,107] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Močibob, L.; Gjurašin, B.; Papić, N. The Infectious Clue: Linking Bacterial Infections to Underlying Malignancies. Cancers 2025, 17, 3958. https://doi.org/10.3390/cancers17243958
Močibob L, Gjurašin B, Papić N. The Infectious Clue: Linking Bacterial Infections to Underlying Malignancies. Cancers. 2025; 17(24):3958. https://doi.org/10.3390/cancers17243958
Chicago/Turabian StyleMočibob, Loris, Branimir Gjurašin, and Neven Papić. 2025. "The Infectious Clue: Linking Bacterial Infections to Underlying Malignancies" Cancers 17, no. 24: 3958. https://doi.org/10.3390/cancers17243958
APA StyleMočibob, L., Gjurašin, B., & Papić, N. (2025). The Infectious Clue: Linking Bacterial Infections to Underlying Malignancies. Cancers, 17(24), 3958. https://doi.org/10.3390/cancers17243958







