Accuracy and Clinical Significance of Intraoperative Gross Extrathyroidal Extension (T3b) Assessment in Differentiated Thyroid Carcinoma
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
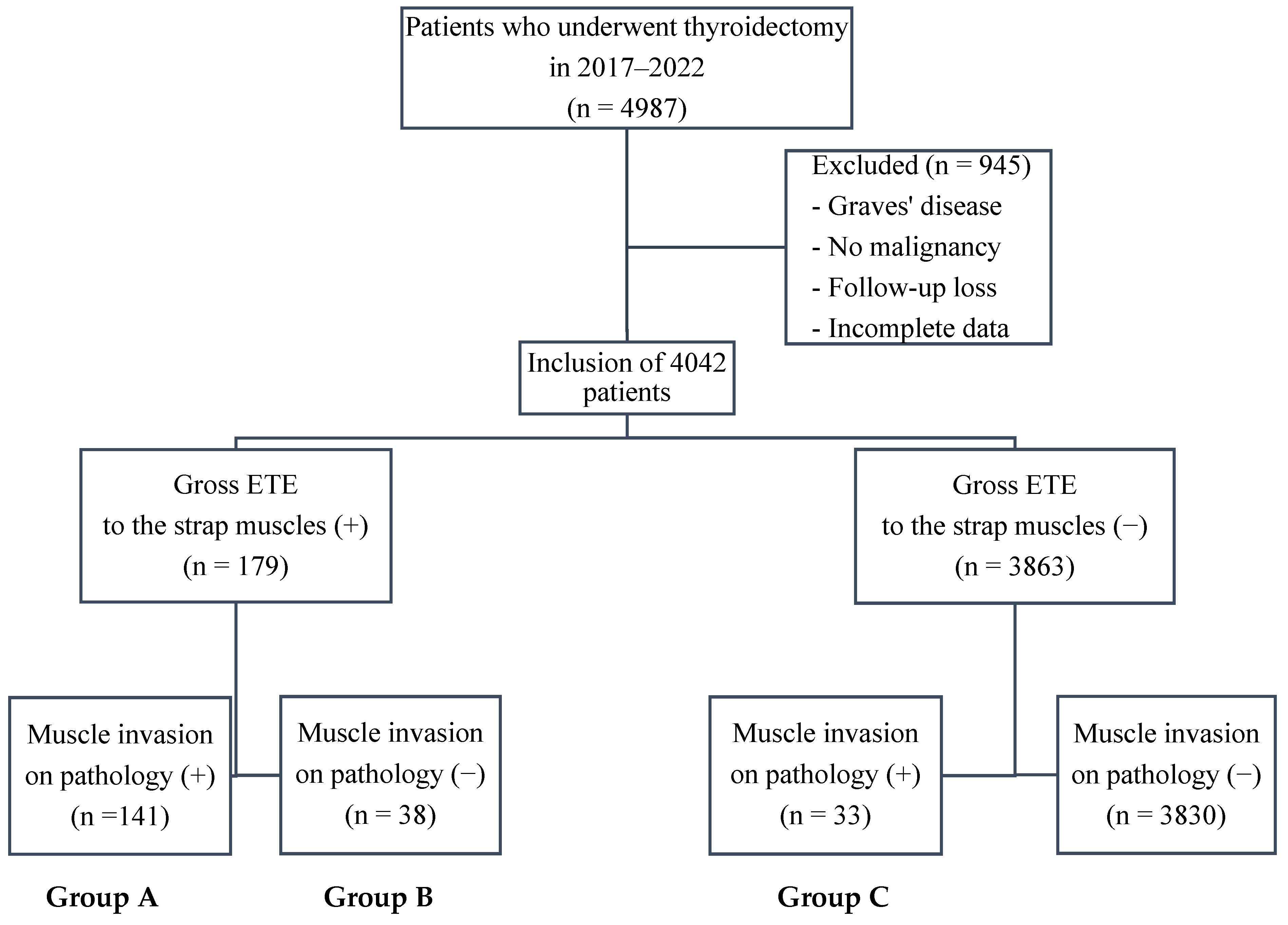
2.1. Patients
2.2. Statistical Analysis
3. Results
3.1. Comparison of Baseline Clinicopathological Characteristics
3.2. Analyses of Clinical Factors Influencing the Misjudgment of ETE
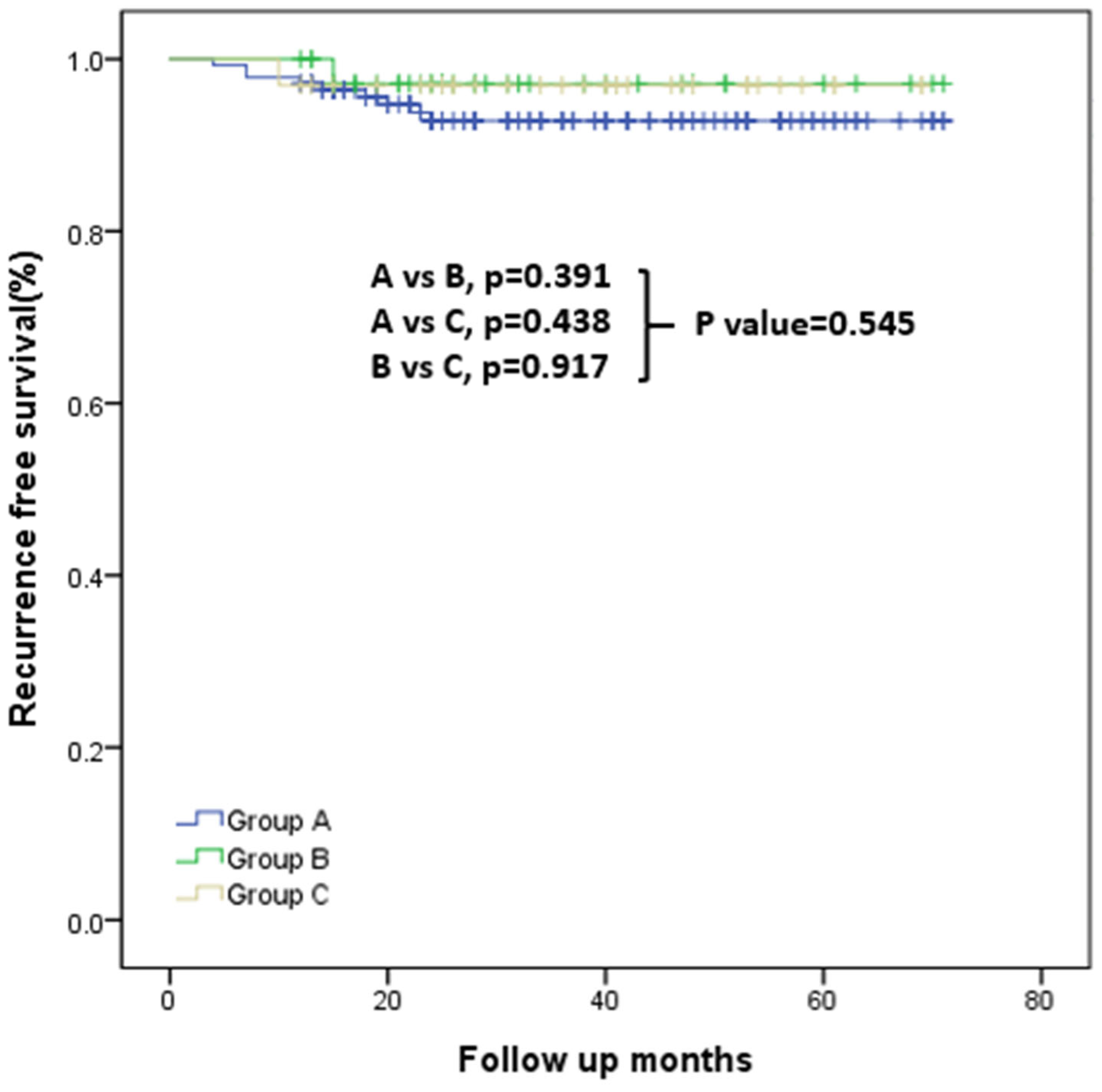
3.3. Analysis of RFS and Recurrence Events
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, J.; An, S.; Bae, J.S.; Kim, K.; Kim, J.S. Impact of tumor size on prognosis in differentiated thyroid cancer with gross extrathyroidal extension to strap muscles: Redefining T3b. Cancers 2024, 16, 2577. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; Su, Y.; Wei, W.; Gong, Y.; Huang, Y.; Zeng, J.; Li, L.; Shi, H.; Chen, S. Extra-thyroid extension prediction by ultrasound quantitative method based on thyroid capsule response evaluation. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2021, 27, e929408. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.-Y.; Yang, P.-S.; Chien, M.-N.; Cheng, S.-P. Preoperative factors associated with extrathyroidal extension in papillary thyroid cancer. Eur. Thyroid. J. 2020, 9, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Megwalu, U.C.; Moon, P.K. Thyroid cancer incidence and mortality trends in the United States: 2000–2018. Thyroid 2022, 32, 560–570. [Google Scholar] [CrossRef]
- Jeon, M.J.; Kim, H.K.; Kim, E.H.; Kim, E.S.; Yi, H.-S.; Kim, T.Y.; Kang, H.-C.; Shong, Y.K.; Kim, W.B.; Kim, B.H.; et al. Decreasing disease-specific mortality of differentiated thyroid cancer in Korea: A multicenter cohort study. Thyroid 2018, 28, 1121–1127. [Google Scholar] [CrossRef]
- Xu, M.; Xi, Z.; Zhao, Q.; Yang, W.; Tan, J.; Yi, P.; Zhou, J.; Huang, T. Causal inference between aggressive extrathyroidal extension and survival in papillary thyroid cancer: A propensity score matching and weighting analysis. Front. Endocrinol. 2023, 14, 1149826. [Google Scholar] [CrossRef]
- Lu, Y.; Jiang, L.; Chen, C.; Chen, H.; Yao, Q. Clinicopathologic characteristics and outcomes of papillary thyroid carcinoma in younger patients. Medicine 2020, 99, e19795. [Google Scholar] [CrossRef]
- Nam, S.H.; Bae, M.R.; Roh, J.-L.; Gong, G.; Cho, K.-J.; Choi, S.-H.; Nam, S.Y.; Kim, S.Y. A comparison of the 7th and 8th editions of the AJCC staging system in terms of predicting recurrence and survival in patients with papillary thyroid carcinoma. Oral Oncol. 2018, 87, 158–164. [Google Scholar] [CrossRef]
- Yoon, J.K.; Lee, J.; Kim, E.-K.; Yoon, J.H.; Park, V.Y.; Han, K.; Kwak, J.Y. Strap muscle invasion in differentiated thyroid cancer does not impact disease-specific survival: A population-based study. Sci. Rep. 2020, 10, 18248. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B.; Greene, F.L.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; Jessup, J.M.; et al. AJCC Cancer Staging Manual, 8th ed.; Springer: New York, NY, USA, 2017. [Google Scholar]
- Ito, Y.; Miyauchi, A.; Hirokawa, M.; Yamamoto, M.; Oda, H.; Masuoka, H.; Sasai, H.; Fukushima, M.; Higashiyama, T.; Kihara, M.; et al. Prognostic value of the 8th edition of the tumor-node-metastasis classification for patients with papillary thyroid carcinoma: A single-institution study at a high-volume center in Japan. Endocr. J. 2018, 65, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Allo, Y.J.M.; Bosio, L.; Morejón, A.; Parisi, C.; Faingold, M.C.; Ilera, V.; Gauna, A.; Brenta, G. Comparison of the prognostic value of AJCC cancer staging system 7th and 8th editions for differentiated thyroid cancer. BMC Endocr. Disord. 2022, 22, 146. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Liu, J.; Wang, P.; Xue, S.; Li, J.; Chen, G. Impact of gross strap muscle invasion on outcome of differentiated thyroid cancer: Systematic review and meta-analysis. Front. Oncol. 2020, 10, 1687. [Google Scholar] [CrossRef] [PubMed]
- Won, H.-R.; Kim, J.W.; Son, H.-O.; Yi, S.; Chang, J.W.; Koo, B.S. Clinical significance of gross extrathyroidal extension to only the strap muscle according to tumor size in differentiated thyroid cancer: A systematic review and meta-analysis. Clin. Exp. Otorhinolaryngol. 2024, 17, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Al-Qurayshi, Z.; Shama, M.A.; Randolph, G.W.; Kandil, E. Minimal extrathyroidal extension does not affect survival of well-differentiated thyroid cancer. Endocr.-Relat. Cancer 2017, 24, 221–226. [Google Scholar] [CrossRef]
- Woo, C.G.; Sung, C.O.; Choi, Y.M.; Kim, W.G.; Kim, T.Y.; Shong, Y.K.; Kim, W.B.; Hong, S.J.; Song, D.E. Clinicopathological significance of minimal extrathyroid extension in solitary papillary thyroid carcinomas. Ann. Surg. Oncol. 2015, 22, 728–733. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, Y.-S.; Bae, J.S.; Kim, J.S.; Kim, K. Is gross extrathyroidal extension to strap muscles (T3b) only a risk factor for recurrence in papillary thyroid carcinoma? A propensity score matching study. Cancers 2022, 14, 2370. [Google Scholar] [CrossRef]
- Jung, S.P.; Kim, M.; Choe, J.-H.; Kim, J.S.; Nam, S.J.; Kim, J.-H. Clinical implication of cancer adhesion in papillary thyroid carcinoma: Clinicopathologic characteristics and prognosis analyzed with degree of extrathyroidal extension. World J. Surg. 2013, 37, 1606–1613. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, S.; Tan, M.; Xu, X. Impact of thyroid nodule location on the risk of papillary thyroid carcinoma. Postgrad. Med. J. 2025, qgaf119. [Google Scholar] [CrossRef]
- Li, G.; Li, R.; Song, L.; Chen, W.; Jiang, K.; Tang, H.; Wei, T.; Li, Z.; Gong, R.; Lei, J.; et al. Implications of extrathyroidal extension invading only the strap muscles in papillary thyroid carcinomas. Thyroid 2020, 30, 57–64. [Google Scholar] [CrossRef]
- Amit, M.; Boonsripitayanon, M.; Goepfert, R.P.; Tam, S.; Busaidy, N.L.; Cabanillas, M.E.; Dadu, R.; Varghese, J.; Waguespack, S.G.; Gross, N.D.; et al. Extrathyroidal extension: Does strap muscle invasion alone influence recurrence and survival in patients with differentiated thyroid cancer? Ann. Surg. Oncol. 2018, 25, 3380–3388. [Google Scholar] [CrossRef]
- Bortz, M.D.; Kuchta, K.; Winchester, D.J.; Prinz, R.A.; Moo-Young, T.A. Extrathyroidal extension predicts negative clinical outcomes in papillary thyroid cancer. Surgery 2021, 169, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Jang, A.; Jin, M.; Kim, W.W.; Jeon, M.J.; Sung, T.Y.; Song, D.E.; Kim, T.Y.; Chung, K.W.; Kim, W.B.; Shong, Y.K.; et al. Prognosis of patients with 1–4 cm papillary thyroid cancer who underwent lobectomy: Focus on gross extrathyroidal extension invading only the strap muscles. Ann. Surg. Oncol. 2022, 29, 7835–7842. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- World Medical Association. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects; World Medical Association: Ferney-Voltaire, France, 2013. [Google Scholar]
- Xiang, J.; Wang, Z.; Sun, W.; Zhang, H. The new T3b category has clinical significance? SEER-based study. Clin. Endocrinol. 2020, 94, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Chang, J.W.; Liu, L.; Jung, S.-N.; Koo, B.S. Clinical implications of microscopic extrathyroidal extension in patients with papillary thyroid carcinoma. Oral Oncol. 2017, 72, 183–187. [Google Scholar] [CrossRef]
- Youngwirth, L.M.; Adam, M.A.; Scheri, R.P.; Roman, S.A.; Sosa, J.A. Extrathyroidal extension is associated with compromised survival in patients with thyroid cancer. Thyroid 2017, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Wang, M.; Dong, L.; Li, F.; He, X.; Li, X.; Sun, D.; Zheng, X.; Jia, Q.; Tan, J.; et al. Extrathyroidal extension or tumor size of primary lesion influences thyroid cancer outcomes. Nucl. Med. Commun. 2023, 44, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Sahin, C.; Inan, M.A.; Bilezikci, B.; Bostanci, H.; Taneri, F.; Kozan, R. Interstitial fibrosis as a common counterpart of histopathological risk factors in papillary thyroid microcarcinoma: A retrospective analysis. Diagnostics 2024, 14, 1624. [Google Scholar] [CrossRef] [PubMed]
- Jasim, S.; Baranski, T.J.; Teefey, S.A.; Middleton, W.D. Investigating the effect of thyroid nodule location on the risk of thyroid cancer. Thyroid 2020, 30, 401–407. [Google Scholar] [CrossRef]
- Zhang, F.; Russell, Y.X.; Guber, H.A. Transverse and longitudinal ultrasound location of thyroid nodules and risk of thyroid cancer. Endocr. Pract. 2021, 27, 682–690. [Google Scholar] [CrossRef]
- Zhang, F.; Oluwo, O.; Castillo, F.B.; Gangula, P.; Castillo, M.; Farag, F.; Zakaria, S.; Zahedi, T. Thyroid nodule location on ultrasonography as a predictor of malignancy. Endocr. Pract. 2019, 25, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Li, H.; Lu, S.; Li, X. Thyroid-associated ophthalmopathy: The role of oxidative stress. Front. Endocrinol. 2024, 15, 1400869. [Google Scholar] [CrossRef] [PubMed]
- Shen, T.; Wu, Y.; Wang, X.; Wang, Z.; Li, E.; Zhou, C.; Yue, C.; Jiang, Z.; Wei, G.; Lian, J.; et al. Activating SIRT3 in peritoneal mesothelial cells alleviates postsurgical peritoneal adhesion formation by decreasing oxidative stress and inhibiting the NLRP3 inflammasome. Exp. Mol. Med. 2022, 54, 1486–1501. [Google Scholar] [CrossRef] [PubMed]
- El-Anwar, M.W.; Abdelaal, T.M.; Khazbak, A.O. Stepwise approach to preserve the external branch of superior laryngeal nerve during thyroidectomy. Egypt. J. Otolaryngol. 2022, 38, 50. [Google Scholar] [CrossRef]
- Gan, X.; Feng, J.; Deng, X.; Shen, F.; Lu, J.; Liu, Q.; Cai, W.; Chen, Z.; Guo, M.; Xu, B. The significance of Hashimoto’s thyroiditis for postoperative complications of thyroid surgery: A systematic review and meta-analysis. Ann. R. Coll. Surg. Engl. 2021, 103, 223–230. [Google Scholar] [CrossRef]
- Polyzos, S.A.; Patsiaoura, K.; Zachou, K. Histological alterations following thyroid fine needle biopsy: A systematic review. Diagn. Cytopathol. 2009, 37, 455–465. [Google Scholar] [CrossRef] [PubMed]
| Group A (n = 141) | Group B (n = 38) | p-Value | |
|---|---|---|---|
| Age (years) | 52.2 ± 14.9 (range, 17–84) | 47.4 ± 14.5 (range, 20–81) | 0.760 |
| Male | 38 (27.0%) | 9 (23.7%) | 0.685 |
| Palpation | 34 (24.1%) | 7 (18.4%) | 0.459 |
| Extent of surgery | |||
| Total | 86 (61.0%) | 20 (52.6%) | 0.352 |
| Less than total | 55 (39.0%) | 18 (47.4%) | |
| CLND | 141 (100%) | 37 (97.4%) | 0.212 |
| LND | 40 (28.4%) | 8 (21.1%) | 0.366 |
| Thyroiditis | 53 (37.6%) | 14 (36.8%) | 0.933 |
| Pathology | |||
| PTC | 138 (97.9%) | 38 (100%) | 1 |
| PDTC | 3 (2.1%) | 0 | |
| Tumor location | |||
| Upper | 8 (5.7%) | 9 (23.7%) | 0.222 |
| Mid | 113 (80.1%) | 21 (55.3%) | |
| Lower | 20 (14.2%) | 8 (21.0%) | |
| Tumor size (cm) | 2.0 ± 1.0 (range, 0.4–5.8) | 1.4 ± 1.0 (range, 0.3–5.8) | 0.005 |
| Multifocality | |||
| Unilateral | 24 (17.0%) | 11 (28.9%) | 0.863 |
| Bilateral | 18 (12.8%) | 3 (7.9%) | |
| Vascular invasion | 12 (8.5%) | 0 | 0.073 |
| Lymphatic invasion | 98 (69.5%) | 18 (47.4%) | 0.011 |
| Perineural invasion | 8 (5.7%) | 0 | 0.206 |
| Harvested LNs | 25.9 ± 31.2 (range, 0–164) | 20.3 ± 20.5 (range, 1–80) | 0.186 |
| Positive LNs | 6.2 ± 7.7 (range, 0–33) | 5.3 ± 7.1 (range, 0–25) | 0.553 |
| N stage | |||
| N0 | 40 (28.4%) | 13 (34.2%) | 0.385 |
| N1a | 66 (46.8%) | 18 (47.4%) | |
| N1b | 35 (24.8%) | 7 (18.4%) | |
| RAI ablation | 62 (44.0%) | 14 (36.8%) | 0.430 |
| RAI mean dose (mCi) | 111.3 ± 46.5 | 104.2 ± 28.5 | 0.590 |
| Recurrence | 9 (6.4%) | 1 (2.6%) | 0.691 |
| Group B (n = 38) | Group C (n = 33) | p-Value | |
|---|---|---|---|
| Age (years) | 47.4 ± 14.5 (range, 20–81) | 49.4 ± 14.9 (range, 18–76) | 0.562 |
| Male | 9 (23.7%) | 7 (21.2%) | 0.804 |
| Palpation | 7 (18.4%) | 5 (15.2%) | 0.714 |
| Extent of surgery | |||
| Total | 20 (52.6%) | 19 (57.6%) | 0.676 |
| Less than total | 18 (47.4%) | 14 (42.4%) | |
| CLND | 37 (97.4%) | 32 (97.0%) | 1 |
| LND | 8 (21.1%) | 9 (27.3%) | 0.540 |
| Thyroiditis | 14 (36.8%) | 10 (30.3%) | 0.561 |
| Pathology | |||
| PTC | 38 (100%) | 32 (97.0%) | 0.465 |
| PDTC | 0 | 1 (3.0%) | |
| Tumor location | |||
| Upper | 9 (23.7%) | 3 (9.1%) | 0.157 |
| Mid | 21 (55.3%) | 25 (75.8%) | |
| Lower | 8 (21.0%) | 5 (15.2%) | |
| Tumor size (cm) | 1.4 ± 1.0 (range, 0.3–5.8) | 2.2 ± 1.5 (range, 0.5–6.0) | 0.016 |
| Multifocality | |||
| Unilateral | 11 (28.9%) | 7 (21.2%) | 0.255 |
| Bilateral | 3 (7.9%) | 7 (21.2%) | |
| Vascular invasion | 0 | 4 (12.1%) | 0.042 |
| Lymphatic invasion | 18 (47.4%) | 24 (72.7%) | 0.030 |
| Perineural invasion | 0 | 1 (3.0%) | 0.465 |
| Harvested LNs | 20.3 ± 20.5 (range, 1–80) | 25.7 ± 30.4 (range, 0–108) | 0.384 |
| Positive LNs | 5.3 ± 7.1 (range, 0–25) | 6.0 ± 6.2 (range, 0–22) | 0.692 |
| N stage | |||
| N0 | 13 (34.2%) | 15 (45.5%) | 0.564 |
| N1a | 18 (47.4%) | 10 (30.3%) | |
| N1b | 7 (18.4%) | 8 (24.2%) | |
| RAI ablation | 14 (36.8%) | 17 (51.5%) | 0.214 |
| RAI mean dose (mCi) | 104.3 ± 28.5 | 117.6 ± 52.9 | 0.403 |
| Recurrence | 1 (2.6%) | 1 (3.0%) | 1 |
| Group A (n = 141) | Group C (n = 33) | p-Value | |
|---|---|---|---|
| Age (years) | 52.2 ± 14.9 (range, 17–84) | 49.4 ± 14.9 (range, 18–76) | 0.334 |
| Male | 38 (27.0%) | 7 (21.2%) | 0.498 |
| Palpation | 34 (24.1%) | 5 (15.2%) | 0.266 |
| Extent of surgery | 0.718 | ||
| Total | 86 (61.0%) | 19 (57.6%) | |
| Less than total | 55 (39.0%) | 14 (42.4%) | |
| CLND | 141 (100%) | 32 (97.0%) | 0.190 |
| LND | 40 (28.4%) | 9 (27.3%) | 0.900 |
| Thyroiditis | 53 (37.6%) | 10 (30.3%) | 0.433 |
| Pathology | 0.572 | ||
| PTC | 138 (97.9%) | 32 (97.0%) | |
| PDTC | 3 (2.1%) | 1 (3.0%) | |
| Tumor location | 0.778 | ||
| Upper | 8 (5.7%) | 3 (9.1%) | |
| Mid | 113 (80.1%) | 25 (75.8%) | |
| Lower | 20 (14.2%) | 5 (15.2%) | |
| Tumor size (cm) | 2.0 ± 1.0 (range, 0.4–5.8) | 2.2 ± 1.5 (range, 0.5–6.0) | 0.476 |
| Multifocality | 0.138 | ||
| Unilateral | 24 (17.0%) | 7 (21.2%) | |
| Bilateral | 18 (12.8%) | 7 (21.2%) | |
| Vascular invasion | 12 (8.5%) | 4 (12.1%) | 0.509 |
| Lymphatic invasion | 98 (69.5%) | 24 (72.7%) | 0.716 |
| Perineural invasion | 8 (5.7%) | 1 (3.0%) | 1 |
| Harvested LNs | 25.9 ± 31.2 (range, 0–164) | 25.7 ± 30.4 (range, 0–108) | 0.978 |
| Positive LNs | 6.2 ± 7.7 (range, 0–33) | 6.0 ± 6.2 (range, 0–22) | 0.895 |
| N stage | 0.125 | ||
| N0 | 40 (28.4%) | 15 (45.5%) | |
| N1a | 66 (46.8%) | 10 (30.3%) | |
| N1b | 35 (24.8%) | 8 (24.2%) | |
| RAI ablation | 62 (44.0%) | 17 (51.5%) | 0.433 |
| RAI mean dose (mCi) | 111.3 ± 46.5 | 117.6 ± 52.9 | 0.872 |
| Recurrence | 9 (6.4%) | 1 (3.0%) | 0.690 |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR (CI) | p-Value | OR (CI) | p-Value | |
| Age (years) | 0.978 (0.955–1.002) | 0.078 | 0.961 (0.932–0.990) | 0.009 |
| Male | 0.841 (0.365–1.939) | 0.685 | ||
| Palpation | 0.711 (0.287–1.759) | 0.460 | ||
| LND | 0.673 (0.284–1.594) | 0.368 | ||
| Thyroiditis | 0.969 (0.461–2.034) | 0.933 | ||
| Tumor location | ||||
| Upper | Ref. | Ref. | ||
| Mid | 0.165 (0.057–0.477) | 0.001 | 0.182 (0.056–0.591) | 0.005 |
| Lower | 0.356 (0.101–1.249) | 0.107 | 0.337 (0.085–1.329) | 0.120 |
| Tumor size (cm) | 0.532 (0.338–0.837) | 0.006 | 0.647 (0.393–1.065) | 0.087 |
| Multifocality | ||||
| Unilateral | 1.891 (0.815–4.386) | 0.138 | ||
| Bilateral | 0.688 (0.187–2.525) | 0.572 | ||
| Lymphatic invasion | 0.395 (0.190–0.820) | 0.013 | 0.292 (0.118–0.719) | 0.007 |
| Harvested LNs | 0.992 (0.978–1.007) | 0.296 | ||
| Positive LNs | 0.985 (0.936–1.036) | 0.551 | ||
| N stage | ||||
| N0 | Ref. | |||
| N1a | 0.839 (0.372–1.895) | 0.673 | ||
| N1b | 0.615 (0.221–1.715) | 0.353 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
An, S.; Park, J.; Kim, K.; Bae, J.S. Accuracy and Clinical Significance of Intraoperative Gross Extrathyroidal Extension (T3b) Assessment in Differentiated Thyroid Carcinoma. Cancers 2025, 17, 3914. https://doi.org/10.3390/cancers17243914
An S, Park J, Kim K, Bae JS. Accuracy and Clinical Significance of Intraoperative Gross Extrathyroidal Extension (T3b) Assessment in Differentiated Thyroid Carcinoma. Cancers. 2025; 17(24):3914. https://doi.org/10.3390/cancers17243914
Chicago/Turabian StyleAn, Solji, Joonseon Park, Kwangsoon Kim, and Ja Seong Bae. 2025. "Accuracy and Clinical Significance of Intraoperative Gross Extrathyroidal Extension (T3b) Assessment in Differentiated Thyroid Carcinoma" Cancers 17, no. 24: 3914. https://doi.org/10.3390/cancers17243914
APA StyleAn, S., Park, J., Kim, K., & Bae, J. S. (2025). Accuracy and Clinical Significance of Intraoperative Gross Extrathyroidal Extension (T3b) Assessment in Differentiated Thyroid Carcinoma. Cancers, 17(24), 3914. https://doi.org/10.3390/cancers17243914







