Simple Summary
Cancer treatment can be improved by using tiny particles, called nanoparticles, to deliver drugs directly to cancer cells. To understand how these drug-loaded nanoparticles work in the body, researchers create mathematical models that predict their behavior. These models help us understand how different factors—like the size and makeup of nanoparticles, the characteristics of tumors, and the body’s own responses—affect the treatment’s success. However, current models sometimes make assumptions that may not match what happens in real-life scenarios, causing us to overestimate the treatment’s effectiveness. This research aims to refine these mathematical models by incorporating more realistic data and advanced artificial intelligence techniques. These improvements may lead to more accurate predictions and ultimately make nanoparticle-based cancer treatments more successful in clinical settings, benefiting patients and advancing the field of cancer therapy.
Abstract
Mathematical models are crucial for predicting the behavior of drug conjugate nanoparticles and optimizing drug delivery systems in cancer therapy. These models simulate interactions among nanoparticle properties, tumor characteristics, and physiological conditions, including drug resistance and targeting specificity. However, they often rely on assumptions that may not accurately reflect in vivo conditions. In vitro studies, while useful, may not fully capture the complexities of the in vivo environment, leading to an overestimation of nanoparticle-based therapy effectiveness. Advancements in mathematical modeling, supported by preclinical data and artificial intelligence, are vital for refining nanoparticle-based therapies and improving their translation into effective clinical treatments.
Keywords:
cancer; nanoparticles; in vitro; in vivo; therapy; drug resistance; preclinical; overestimation 1. Introduction
Drug delivery is crucial in cancer therapy, influencing both the efficacy and safety of treatments [1,2,3,4]. Traditional methods, such as systemic chemotherapy, distribute therapeutic agents throughout the body, targeting both cancerous and healthy cells, often resulting in significant side effects due to the lack of specificity [5,6,7]. Advanced delivery systems, such as nanoparticles (NPs) and targeted therapies, aim to improve this by offering more precise and controlled delivery, reducing systemic toxicity, and enhancing treatment effectiveness [2,7,8].
Despite their potential, NP-mediated cancer therapies have only seen moderate clinical success, primarily due to low tumor delivery efficiency [9,10,11]. Although NPs can exploit the enhanced permeability and retention (EPR) effect and actively target cancer cells via surface functionalization, only about 0.7% of the injected dose accumulates in tumors [12,13]. Enhanced permeability and retention (EPR) refers to the tendency of nanoparticles or drugs to accumulate more in tumor tissues than in normal tissues due to the leaky blood vessels and poor lymphatic drainage in tumors [14]. EPR efficiency measures the effectiveness of this phenomenon in delivering therapeutic agents to tumor sites, with higher efficiency indicating better accumulation and retention of the drug in the tumor [15]. Inefficiency is largely due to rapid clearance by the mononuclear phagocytic system (MPS) and kidneys, which is influenced by NP size, charge, and the physiological characteristics of these organs [5,16,17]. Understanding and manipulating these factors are crucial to improving NP delivery to tumors and enhancing therapy success.
To better navigate these challenges, mathematical and computational models have emerged as powerful tools for predicting NP behavior, guiding experimental design, and refining therapeutic strategies. These models integrate principles from physics, chemistry, and biology to simulate NP transport, distribution, and interactions at various levels—ranging from molecular events at the cell membrane to systemic factors like blood flow and organ clearance. By incorporating experimental data, such as NP physicochemical characteristics, preclinical animal studies, and patient-derived tumor parameters, mathematical models can provide insights into how altering NP properties or administering specific dosing regimens might enhance tumor accumulation and improve drug delivery efficiency. Such models also help identify critical variables that influence treatment outcomes, enabling researchers to focus on optimizing key parameters like NP size, shape, and surface functionalization. Furthermore, advancements in computational techniques, including machine learning and multiscale modeling, allow for more accurate, patient-specific predictions, potentially accelerating the translation of NP-based therapies from the laboratory to clinical practice.
Conversely, the inefficiencies of NP-mediated therapies, such as poor targeting accuracy, inadequate drug release, and limited tissue penetration, stem from the complex interactions between NPs and biological systems, which current mathematical models fail to fully capture [2,18]. These models often oversimplify biological environments, neglecting factors like tissue heterogeneity, immune responses, and patient variability, which limits their predictive power. As a result, NP designs cannot be optimized effectively, leading to suboptimal therapeutic outcomes and hindering clinical translation [19,20]. To improve NP-based therapies, more sophisticated, multiscale, and personalized mathematical models are needed to better simulate NP behavior and address these inefficiencies.
2. Challenges in In Vivo and In Vitro Nano-Based Cancer Drug Delivery
Challenges such as drug resistance, targeting specificity, and the tumor microenvironment significantly hinder the effectiveness of nano-based cancer therapies [1,2,4,21]. Drug resistance occurs when cancer cells adapt to evade the effects of treatment, often through genetic mutations or by activating alternative survival pathways, making it difficult to achieve long-term remission [21,22,23,24]. Targeting specificity is another critical challenge, as ensuring that drug delivery systems accurately distinguish between cancerous and healthy cells is essential to minimize side effects and enhance therapeutic efficacy [25,26,27,28]. The tumor microenvironment, characterized by abnormal vasculature, high interstitial pressure, and a dense extracellular matrix, further complicates treatment by impeding drug penetration and distribution within the tumor [29,30,31]. Addressing these challenges requires innovative strategies that can overcome biological barriers, enhance targeting precision, and counteract resistance mechanisms to improve cancer treatment outcomes. Furthermore, developing dynamic models that consider time-dependent changes in tumor microenvironments and physiological conditions can offer more realistic simulations of nanoparticle behavior throughout treatment [32,33]. These models would better reflect the complexities of how tumors evolve and how the body responds over time, leading to more accurate predictions and optimized treatment strategies [34,35]. By incorporating these dynamic factors, the models can enhance the precision of drug delivery systems and improve their effectiveness in cancer therapy.
The human body is far more complex than controlled lab conditions, where in vitro studies are typically conducted in simplified environments that do not fully replicate the intricate interactions within a living organism, such as the immune system, blood flow dynamics, and the presence of various cell types and tissues [36,37]. In vivo, NPs must navigate various biological barriers, including the MPS, blood–brain barrier, and the complex tumor microenvironment, which can significantly reduce the efficiency of NP delivery to the target site (Figure 1) [38]. Additionally, NPs in vivo are often rapidly cleared from the bloodstream by organs like the liver and spleen, reducing their availability to target tumors [12]. The distribution of NPs throughout the body (biodistribution) can also be unpredictable, leading to off-target effects and reduced efficacy at the tumor site [12,38]. Furthermore, tumors in vivo have highly heterogeneous microenvironments that vary greatly from patient to patient and even within different regions of the same tumor, affecting how NPs interact with the tumor and leading to inconsistent drug delivery and therapeutic outcomes [12,31,38]. Finally, the immune system in vivo can recognize and eliminate NPs before they reach the tumor, a factor that in vitro studies typically do not account for, leading to an overestimation of NP efficacy [36]. Several assumptions in drug delivery systems have led to the overestimation of efficacy in real-life applications. For example, the assumption that smaller nanoparticles penetrate tumors more effectively has been challenged by tumor heterogeneity and blood vessel permeability, which limit nanoparticle penetration [39,40]. Similarly, the EPR effect, often relied upon for targeted drug delivery, fails in tumors with well-organized blood vessels, reducing nanoparticle accumulation. Additionally, the assumptions of stable, controlled drug release can be disrupted by factors like pH changes and enzymatic activity, leading to premature drug release. Lastly, surface modifications, such as targeting ligands, are not always effective due to receptor expression variability and immune system interactions [41,42]. These cases highlight the need for more realistic models to address the complexities of drug delivery systems. Incorporating comprehensive preclinical data into mathematical models can significantly improve their accuracy and predictive power [43,44]. This data, derived from various animal models, help capture the diversity of tumor types and treatment responses, providing a more robust understanding of how nanoparticles behave in different scenarios. By including this broad range of preclinical insights, models can better simulate real-world conditions, leading to more effective predictions and optimized drug delivery strategies for cancer therapy [45]. Furthermore, regulatory hurdles, scalability factors, and patient-specific factors impact the efficacy of NP-based drug delivery. Strict regulatory standards can delay adoption, while scaling production for clinical use may affect consistency and cost-effectiveness [46,47]. Additionally, individual patient factors (genetics, health conditions, and immune responses) can influence how NPS are absorbed and metabolized, further complicating treatment effectiveness [48].
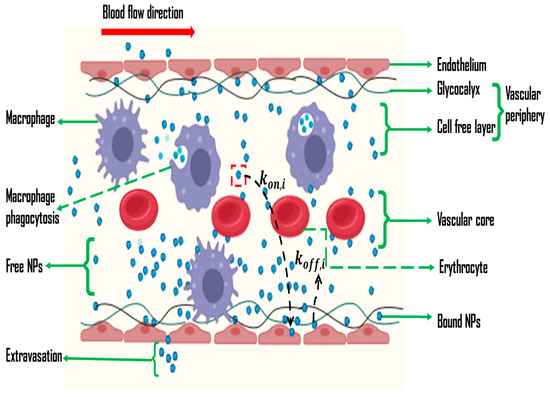
Figure 1.
Schematic diagram showing the NP adsorption and dislodgement during the delivery process.
In addition to the complexities encountered in vivo, the in vitro evaluation of nanoparticle-based therapies also presents inherent challenges. These include the use of simplified, two-dimensional cell culture systems that fail to mimic the three-dimensional architecture, extracellular matrix composition, and dynamic fluid flows of tumor tissues, potentially leading to inaccurate assessments of nanoparticle penetration and uptake [49]. Moreover, standard in vitro assays often lack critical components such as immune cells, stromal cells, and vascular networks, thereby overlooking key biological interactions and responses that influence nanoparticle behavior in patients [50]. These limitations can result in the overestimation of therapeutic efficacy, as in vitro conditions do not capture the immune clearance, metabolic variability, and heterogeneous microenvironments that NPs encounter in vivo. Consequently, more complex in vitro models, including three-dimensional spheroid or organoid cultures and microfluidic “tumor-on-a-chip” devices, are being explored to improve the predictive power of preclinical studies and better inform the design of effective nanoparticle-based cancer therapies [51].
Figure 1 illustrates a model applied in both in vivo and in vitro cancer drug delivery systems, focusing on the vascular wall and the influence of NP properties on drug delivery dynamics [16,38]. It demonstrates how the size, shape, and surface chemistry of NPs significantly affect the rates of NP adsorption () and dislodgement () during the delivery process [52,53]. This visualization underscores the importance of NP design in optimizing drug delivery efficacy and overcoming the challenges associated with both in vivo and in vitro systems [54,55]. Smaller NPs typically have higher diffusion rates, which can increase their ability to approach and bind to the endothelial wall, potentially enhancing [53]. Conversely, larger NPs might face greater resistance in diffusing through the glycocalyx and therefore could exhibit reduced and [56].
The shape of NPs also affects their interaction with the endothelial surface, with shapes that align better with the wall geometry possibly enhancing the binding and affecting the dislodgement rate [55]. Surface chemistry, including functional groups and charge, influences the binding affinity and stability of NPs on the endothelial wall, altering both and [53]. Surface modifications can enhance specific interactions or promote repulsion, thus impacting how readily NPs adhere to or dislodge from the endothelial surface [57]. These factors collectively influence the efficiency and effectiveness of NP-mediated drug delivery in vitro systems.
Mathematical models are key to predicting the behavior of drug conjugate nanoparticles and optimizing drug delivery systems in cancer therapy. While challenges such as the assumptions and limitations of in vitro studies exist, advancements in mathematical modeling, particularly when combined with preclinical data and AI, show great potential for improving nanoparticle-based therapies [44]. AI has been integrated into both in vitro and in vivo nanoparticle drug delivery models, improving drug targeting and delivery accuracy [58]. In vitro, AI analyzes experimental data to optimize nanoparticle design for better cellular uptake and drug release. Machine learning, including deep learning, helps predict cell responses and nanoparticle interactions, enabling personalized delivery strategies [59]. In vivo, AI simulates complex biological systems, accounting for tumor heterogeneity and immune responses to predict nanoparticle behavior [60]. Overall, AI bridges the gap between theoretical models and clinical applications, enhancing the efficacy of nanoparticle-based therapies in cancer treatment. These models can enhance prediction accuracy and aid in translating research into clinical treatments, advancing cancer therapy and patient outcomes. To address these challenges, a comprehensive understanding of NP behavior within systemic pharmacokinetics and the tumor microenvironment is essential [12,38,52]. Preclinical studies have highlighted various physicochemical and physiological factors, but a holistic approach using mathematical models is needed to simulate the complex interactions between NP properties, tumor characteristics, and physiological conditions [61,62]. Existing models have provided valuable insights but are often limited in scope or lack tumor-specific compartments [62,63]. Advancing mathematical models for NP-based drug delivery can improve the design, predict behavior, and enhance therapeutic efficacy, leading to more effective and targeted cancer treatments [61].
In conclusion, this review delves into the complexities and potential advancements in the mathematical modeling of nanomedicine, providing a comprehensive examination of how the biophysicochemical properties of nanoparticles influence drug delivery effectiveness. By analyzing the interplay between these properties and various biological conditions, both in vivo and in vitro, this review aims to highlight the current challenges and prospects in refining nanoparticle-based therapies. Through a detailed exploration of model limitations and advancements, including the integration of preclinical data and artificial intelligence, this review seeks to offer valuable insights into optimizing drug delivery systems and enhancing their clinical translation. Furthermore, there is a significant need for multi-scale modeling approaches that link molecular interactions to cellular and tissue-level responses. These models may offer a more comprehensive understanding of how drug conjugate nanoparticles behave in complex biological systems, improving the design and effectiveness of drug delivery systems in cancer therapy by capturing the full spectrum of nanoparticle behavior.
3. Nanoparticle-Based Cancer Drug Delivery Models
This section explores the common modeling approaches used to describe and predict the behavior of nanoparticle-based drug delivery systems in cancer therapy. Figure 2 illustrates the complex interaction between nanoparticles and cell membranes by highlighting the dynamic interplay of four key factors. Physical and chemical barriers at the cell membrane level, such as lipid and protein composition [16], membrane charge, and local molecular environment [53], can impede or facilitate nanoparticle penetration. Internalization forces, including endocytosis [64,65] and membrane disruption [65,66] also influence how effectively nanoparticles move from the bloodstream into target cells and tissues. When considering the movement of nanoparticles within the vasculature, factors such as nanoparticle size, shape, surface charge, and ligand chemistry, as well as fluid dynamics and red blood cell (RBC)-induced shear forces, collectively govern their radial migration from the vessel core toward the vessel walls. For instance, nanoparticle margination—the tendency of nanoparticles to drift toward the periphery of the blood vessel—depends on their physicochemical properties [54,65,66] and their interactions with flowing blood components [55,61,67]. This margination process is further influenced by the endothelial glycocalyx [55,61], which can either facilitate or hinder nanoparticle adhesion depending on nanoparticle surface characteristics and the local vascular environment. Ultimately, these biophysicochemical factors and their interplay determine how nanoparticles are distributed, deposited, and ultimately taken up by cells, thus impacting their therapeutic efficacy [54,65,66].
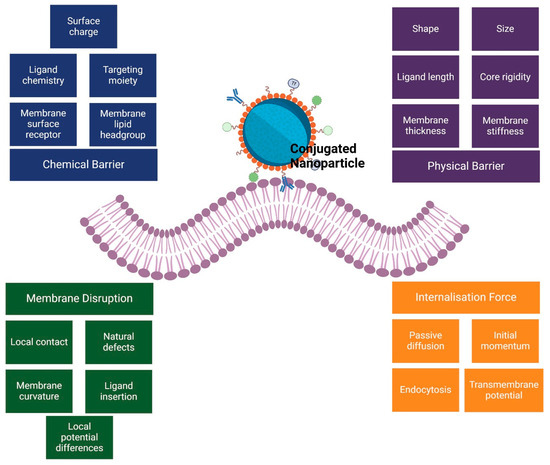
Figure 2.
The mechanisms of nanoparticle interaction with cell membranes: a framework of chemical and physical barriers.
Nanoparticles within the microvascular space often exhibit a non-uniform radial distribution, showing a propensity to move from the vascular core to the periphery [55]. This distribution is influenced by Brownian motion, shear-induced diffusion due to erythrocytes, and sedimentation [61,67]. Once at the periphery, interactions with the endothelial glycocalyx and vessel wall determine whether the nanoparticles remain free-flowing or adhere to the surface. This adhesion process is a critical step that directs nanoparticles closer to target tissues. The overall deposition of nanoparticles on the microvascular wall is thus governed by complex interactions among nanoparticle characteristics, hemorheological parameters, and hemodynamic conditions which collectively influence nanoparticle migration, distribution, and kinetics at the organ level [55,67,68].
Assuming the nanoparticle motion from the core toward the vessel wall is governed by gravitational and buoyant forces (Figure 1), the terminal sedimentation velocity of a nanoparticle with radius can be derived using Stoke’s law. This simplified calculation focuses solely on sedimentation by disregarding longitudinal blood flow and RBC presence, providing a baseline understanding of nanoparticle behavior before incorporating additional complexities of the blood microenvironment [55,61]. Stoke’s law (Equation (1)) provides the terminal velocity of a spherical NP settling in a fluid due to gravity:
where: is the terminal sedimentation velocity, is the radius of the nanoparticle, is the density of the nanoparticle, is the density of the fluid (blood plasma), is the gravitational acceleration constant, and is the dynamic viscosity of the fluid. The equation calculates the sedimentation rate of a NP under gravitational forces, considering the NP’s size and the fluid properties, and assumes the NP operates in a low Reynolds number regime, where viscous forces dominate over inertial forces [69].
However, in the presence of blood flow and erythrocytes, the sedimentation velocity of NPs is adjusted by dividing the original equation (Equation (1)) by the characteristic length of sedimentation (the radius of the microvessel, R) and the Peclet number [70]. The Peclet number is calculated using the average blood flow velocity and the effective diffusivity of NPs, which includes contributions from both Brownian motion () derived from the Stokes-Einstein equation and shear-induced diffusion () based on an analytical expression by Xu et al. [71].
where k is the Boltzmann’s constant (1.38 × 10−23 J K−1), T is the absolute temperature in K, is the dynamic viscosity of fluid, r is the nanoparticle radius, Cc is a slip correction factor, β is the radius of the erythrocytes, γ̇ is the shear rate, and H is the hematocrit: the volume fraction of red blood cells in the blood.
Subsequently, the final adjustment results in the parameter (), which characterizes the rate of deposition of the NPs on the microvascular wall, as depicted by Equation (3).
NPs marginated towards the microvascular wall are either endocytosed by macrophages or remain non-specifically bound to the endothelial wall [61]. However, NPs can re-enter the vessel lumen and continue their transport if they diffuse back through the endothelial glycocalyx’s characteristic diffusion length (lg), with the rate of dislodging determined by their ability to traverse this glycocalyx layer, as highlighted by Equation (4) [55,72].
Although NP dislodgement from the endothelial wall can be influenced by specific interactions between NP surface ligands and endothelial cell receptors (Figure 2), many studies simplify this by assuming that the relative tendency of NPs to approach and diffuse away from the wall is governed by and , respectively [12,53,55,67].
When nanoparticles approach a cell membrane, they may adsorb, penetrate, or be internalized via endocytosis, depending on their surface characteristics and the membrane’s composition [54,65,66]. Basic models developed to study these interactions often focus on electrostatic forces, van der Waals forces, and hydrophobic interactions, which govern the adsorption and adhesion of nanoparticles to the cell membrane [62,73,74,75]. Additionally, molecular dynamics simulations and continuum models have been employed to predict the behavior of nanoparticles at the nanoscale, providing insights into how factors like nanoparticle rigidity and ligand–receptor binding can influence cellular uptake [75,76,77]. These models help in understanding the initial stages of nanoparticle–membrane interaction and are essential for optimizing drug delivery efficiency and minimizing off-target effects [78,79].
Figure 3 depicts the interactions of nanoparticles with porous membranes, which are a focal point in various theoretical studies including drug delivery mathematical models [16,55]. These interactions are crucial for understanding how NPs navigate and permeate biological barriers, influencing their effectiveness in drug delivery systems.

Figure 3.
Conjugated nanoparticle–membrane interactions.
Various models have been developed to simulate how conjugated nanoparticles interact with cellular membranes, especially focusing on their behavior as they encounter and interact with membrane pores [62,73,80,81]. These models help in understanding and predicting the efficiency and mechanisms of nanoparticle delivery into cells. Goldberg et al. conducted a comprehensive review of the models used to describe nanoparticle transport in saturated porous media, evaluating their ability to predict flow [82]. The models were categorized according to key transport phenomena, including flow equations, deposition terms, remobilization, and blocking effects [82]. Notably, the study suggested that increased model complexity does not necessarily correlate with improved predictive accuracy for nanoparticle behavior.
Ju and Fan developed a mathematical model for nanoparticle transport in porous media with several key assumptions: (1) the flow is one-dimensional and isothermal with incompressible fluids; (2) the porous medium is heterogeneous; (3) both drug and nanoparticle colloid flow follow Darcy’s law, with gravity effects ignored; (4) nanoparticles are divided into discrete intervals; and (5) fluid viscosity and density are constant, and the medium behaves as a Newtonian fluid [83]. The model employs Darcy’s law to describe fluid flow in porous media, represented by Equation (5):
where x is the distance of the particle in the reservoir, t is time, ϕ is the porosity of the reservoir medium, Kl is the effective permeability, and Sl, μl, and Pl are the saturation, viscosity, and porosity of phase l (media), respectively. Ju and colleagues developed models to describe the changes in porosity and the permeability of porous media following the injection of cancer drug-conjugated nanoparticles [84]. These changes are mathematically represented by Equations (6) and (7), which quantify how nanoparticle injection alters the structural and flow properties of the porous media, respectively:
The permeability of the porous medium, after the injection of cancer drug-conjugated nanoparticles, can be calculated using Equation (7):
The model, solved using the implicit pressure explicit saturation (IMPES) method, accurately predicts nanoparticle movement in porous media [85]. As one of the pioneering models for evaluating nanoparticle transport, it has been widely utilized and referenced in subsequent research advancements [86,87,88]. Most NP-based drug delivery mathematical models rely on the conceptual framework depicted in Figure 1 and Equations (1)–(7), with minor modifications to address specific target niches. However, these equations often necessitate cumbersome and continuous optimization to account for the complex differences between in vivo and in vitro scenarios, reflecting the challenges in achieving accurate and universal modeling for diverse nanoparticle physicochemical properties and biological environments. Furthermore, while nanoparticle-based cancer drug delivery models complement each other and provide valuable insights, their predictive power for in vivo efficacy remains limited. This gap highlights the need for continued refinement and the integration of experimental data to enhance model accuracy and better translate laboratory successes into effective clinical outcomes.
4. Future Prospects
While mathematical models are excellent at predicting nanoparticle-based cancer drug delivery, they are often built on assumptions that may not be feasible in vivo. These models typically simplify the complexities of the human body, such as the variability in biological environments, the dynamic interactions between nanoparticles and biological systems, and the impact of the immune response [89,90]. A critical challenge in developing these models is their validation against experimental data. Ensuring that models accurately reflect biological realities is essential for their utility in clinical applications. As a result, the predictions made by these models may not fully capture the challenges encountered during actual in vivo drug delivery.
Moreover, mathematical modeling plays a crucial role in the design and development of next-generation drug delivery systems by allowing researchers to explore a wide range of scenarios and predict outcomes before conducting expensive and time-consuming experiments [91,92]. However, future improvements lie in the integration of diverse data sources and advanced computational techniques to increase the fidelity of these models. By incorporating high-resolution imaging data, multi-omic datasets (genomic, transcriptomic, proteomic, and metabolomic), patient-specific tumor characteristics, and real-time clinical feedback, models can begin to approximate the complexities of the tumor microenvironment and systemic circulation more accurately. Such data-rich models can better capture dynamic processes, including tumor evolution, metastasis, and the interplay between cancer cells, immune cells, and the vasculature. Additionally, advances in artificial intelligence (AI) and machine learning are poised to further enhance the predictive power of mathematical models in nanoparticle-based delivery [93,94,95]. AI-driven approaches can help identify patterns and relationships that are difficult to discern through traditional modeling methods, leading to improved parameter estimation, model calibration, and uncertainty quantification. This can facilitate the rapid adaptation of models as new data become available, making it possible to tailor therapies in a patient-specific manner and improve treatment outcomes. The development of hybrid models that combine mechanistic understanding with data-driven insights holds particular promise in refining dosing strategies, selecting the most effective nanoparticle formulations, and predicting therapeutic responses more accurately [96].
On the engineering side, emerging fabrication techniques, such as microfluidic templating and bioprinting, can produce nanoparticles with more precise control over size, shape, and surface chemistry. These advancements enable researchers to systematically test and validate model predictions, bridging the gap between theoretical optimization and experimental realization. The integration of organ-on-a-chip platforms and patient-derived organoids can also provide biologically relevant validation environments for next-generation models, enabling iterative improvements based on direct feedback from physiologically representative systems [97].
Looking ahead, the field would benefit from a greater emphasis on personalized medicine, where models incorporate patient-specific parameters to guide therapy selection and dosing. As models become more complex and computational methods advance, there is potential for real-time clinical decision support, where healthcare providers can leverage predictive simulations to adjust treatment plans dynamically. These developments, coupled with ongoing innovations in nanoparticle design and functionalization (e.g., stimuli-responsive, immunomodulatory, or multi-drug loaded nanoparticles), are set to expand the toolbox for improving drug targeting, increasing therapeutic efficacy, and minimizing off-target effects.
In summary, the future of nanoparticle-based cancer drug delivery and associated mathematical modeling is poised to become increasingly data-driven, patient-centric, and integrative. By embracing these emerging technologies and methodologies, the field can advance toward more robust, accurate, and clinically meaningful predictions—ultimately improving outcomes and reducing the burden of cancer therapy on patients.
5. Conclusions
Mathematical modeling plays a critical role in advancing nanoparticle-based cancer drug delivery by improving the understanding and prediction of drug behavior. However, to move beyond current limitations, researchers should prioritize a few key strategies. First, integrating comprehensive, high-quality datasets from diverse sources—including multi-omic profiles, advanced imaging modalities, and patient-derived tissues—can provide richer inputs for models. Collaborations with experimentalists can ensure ongoing feedback loops that refine parameter estimates and validate model predictions. Second, adopting multi-scale modeling frameworks that span molecular interactions, cellular uptake, and whole-organism pharmacokinetics will capture the full complexity of nanoparticle dynamics. Third, employing AI-driven simulations and machine learning tools can enable adaptive models that incorporate evolving datasets and patient-specific parameters, improving both accuracy and personalization. Finally, establishing standardized protocols and shared databases can facilitate model comparison, reproducibility, and community-driven improvements. By taking these concrete steps, the research community can enhance the predictive power and clinical relevance of mathematical models, ultimately guiding the design of more effective and personalized nanoparticle-based cancer therapies.
Author Contributions
Conceptualization, T.A.M.; writing—original draft preparation, T.A.M.; writing—review and editing, T.A.M. and A.C.; visualization, T.A.M. and A.C.; supervision, A.C.; funding acquisition, A.C. All authors have read and agreed to the published version of the manuscript.
Funding
The authors are funded by the National Research Foundation of South Africa Thuthuka Instrument, grant number TTK2205035996; the Department of Science and Innovation (DSI)-funded African Laser Centre (ALC), grant number HLHA23X task ALC-R007; the University Research Council, grant number 2022URC00513; the Department of Science and Technology’s South African Research Chairs Initiative (DST-NRF/SARChI), grant number 98337; and the University Research Council and Faculty of Health Sciences at the University of Johannesburg.
Acknowledgments
The authors would like to acknowledge the University of Johannesburg for their facilities.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of this study; in the collection, analyses, or interpretation of the data; in the writing of the manuscript; or in the decision to publish the results.
References
- Elumalai, K.; Srinivasan, S.; Shanmugam, A. Review of the efficacy of nanoparticle-based drug delivery systems for cancer treatment. Biomed. Technol. 2024, 5, 109–122. [Google Scholar] [CrossRef]
- Chehelgerdi, M.; Chehelgerdi, M.; Allela, O.Q.B.; Pecho, R.D.C.; Jayasankar, N.; Rao, D.P.; Thamaraikani, T.; Vasanthan, M.; Viktor, P.; Lakshmaiya, N.; et al. Progressing nanotechnology to improve targeted cancer treatment: Overcoming hurdles in its clinical implementation. Mol. Cancer 2023, 22, 169. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Yang, L.; Chen, G.; Xu, F.; Yang, F.; Yu, H.; Li, L.; Dong, X.; Han, J.; Cao, C.; et al. A Review on Drug Delivery System for Tumor Therapy. Front. Pharmacol. 2021, 12, 735446. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Zhou, Y.; Liu, L.; Xu, Y.; Chen, Q.; Wang, Y.; Wu, S.; Deng, Y.; Zhang, J.; Shao, A. Nanoparticle-Based Drug Delivery in Cancer Therapy and Its Role in Overcoming Drug Resistance. Front. Mol. Biosci. 2020, 7, 193. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Sun, M.; Huang, H.; Jin, W.-L. Drug repurposing for cancer therapy. Signal Transduct. Target. Ther. 2024, 9, 92. [Google Scholar] [CrossRef]
- Billaut, J.C.; André, V.; Kergosien, Y.; Tournamille, J.F. Optimization Issues in Chemotherapy Delivery. In Health Efficiency; Sarazin, M., Ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 91–118. [Google Scholar]
- Debela, D.T.; Muzazu, S.G.; Heraro, K.D.; Ndalama, M.T.; Mesele, B.W.; Haile, D.C.; Kitui, S.K.; Manyazewal, T. New approaches and procedures for cancer treatment: Current perspectives. SAGE Open Med. 2021, 9, 20503121211034366. [Google Scholar] [CrossRef]
- Ding, L.; Agrawal, P.; Singh, S.K.; Chhonker, Y.S.; Sun, J.; Murry, D.J. Polymer-Based Drug Delivery Systems for Cancer Therapeutics. Polymers 2024, 16, 843. [Google Scholar] [CrossRef]
- Cheng, Z.; Li, M.; Dey, R.; Chen, Y. Nanomaterials for cancer therapy: Current progress and perspectives. J. Hematol. Oncol. 2021, 14, 85. [Google Scholar] [CrossRef]
- Giri, P.M.; Banerjee, A.; Layek, B. A Recent Review on Cancer Nanomedicine. Cancers 2023, 15, 2256. [Google Scholar] [CrossRef]
- Bravo, M.; Fortuni, B.; Mulvaney, P.; Hofkens, J.; Uji-I, H.; Rocha, S.; Hutchison, J. Nanoparticle-mediated thermal Cancer therapies: Strategies to improve clinical translatability. J. Control. Release 2024, 372, 751–777. [Google Scholar] [CrossRef]
- Milligan, J.J.; Saha, S. A Nanoparticle’s Journey to the Tumor: Strategies to Overcome First-Pass Metabolism and Their Limitations. Cancers 2022, 14, 1741. [Google Scholar] [CrossRef] [PubMed]
- Horejs, C. It all comes down to the dose. Nat. Rev. Mater. 2020, 5, 728. [Google Scholar] [CrossRef]
- Tan, A.; Jeyaraj, R.; De Lacey, S.F. Chapter 7—Nanotechnology in neurosurgical oncology. In Nanotechnology in Cancer; Mathur, A.B., Ed.; William Andrew Publishing: Norwich, NY, USA, 2017; pp. 139–170. [Google Scholar]
- Subhan, M.A.; Yalamarty, S.S.K.; Filipczak, N.; Parveen, F.; Torchilin, V.P. Recent Advances in Tumor Targeting via EPR Effect for Cancer Treatment. J. Pers. Med. 2021, 11, 571. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Miao, L.; Zhong, G.; Lin, C.-H.; Dargazangy, R.; Alexander-Katz, A. Understanding the synergistic effect of physicochemical properties of nanoparticles and their cellular entry pathways. Commun. Biol. 2020, 3, 205. [Google Scholar] [CrossRef]
- Panigrahi, L.L.; Samal, P.; Sahoo, S.R.; Sahoo, B.; Pradhan, A.K.; Mahanta, S.; Rath, S.K.; Arakha, M. Nanoparticle-mediated diagnosis, treatment, and prevention of breast cancer. Nanoscale Adv. 2024, 6, 3699–3713. [Google Scholar] [CrossRef]
- Tiwari, H.; Rai, N.; Singh, S.; Gupta, P.; Verma, A.; Singh, A.K.; Kajal; Salvi, P.; Singh, S.K.; Gautam, V. Recent Advances in Nanomaterials-Based Targeted Drug Delivery for Preclinical Cancer Diagnosis and Therapeutics. Bioengineering 2023, 10, 760. [Google Scholar] [CrossRef]
- Waheed, S.; Li, Z.; Zhang, F.; Chiarini, A.; Armato, U.; Wu, J. Engineering nano-drug biointerface to overcome biological barriers toward precision drug delivery. J. Nanobiotechnol. 2022, 20, 395. [Google Scholar] [CrossRef]
- Deshmukh, R.; Sethi, P.; Singh, B.; Shiekmydeen, J.; Salave, S.; Patel, R.J.; Ali, N.; Rashid, S.; Elossaily, G.M.; Kumar, A. Recent Review on Biological Barriers and Host–Material Interfaces in Precision Drug Delivery: Advancement in Biomaterial Engineering for Better Treatment Therapies. Pharmaceutics 2024, 16, 1076. [Google Scholar] [CrossRef]
- Bukhari, S.N.A. Emerging Nanotherapeutic Approaches to Overcome Drug Resistance in Cancers with Update on Clinical Trials. Pharmaceutics 2022, 14, 866. [Google Scholar] [CrossRef]
- Vasan, N.; Baselga, J.; Hyman, D.M. A view on drug resistance in cancer. Nature 2019, 575, 299–309. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, Y.; Lai, Y.; Xu, W.; Lei, S.; Chen, G.; Wang, Z. A computer-aided, heterodimer-based “triadic” carrier-free drug delivery platform to mitigate multidrug resistance in lung cancer and enhance efficiency. J. Colloid Interface Sci. 2025, 677 Pt B, 523–540. [Google Scholar] [CrossRef]
- Chatterjee, N.; Bivona, T.G. Polytherapy and Targeted Cancer Drug Resistance. Trends Cancer 2019, 5, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Ezike, T.C.; Okpala, U.S.; Onoja, U.L.; Nwike, C.P.; Ezeako, E.C.; Okpara, O.J.; Okoroafor, C.C.; Eze, S.C.; Kalu, O.L.; Odoh, E.C.; et al. Advances in drug delivery systems, challenges and future directions. Heliyon 2023, 9, e17488. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, Q.; Xia, G.; Adilijiang, N.; Li, Y.; Hou, Z.; Fan, Z.; Li, J. Recent Advances in Targeted Drug Delivery Strategy for Enhancing Oncotherapy. Pharmaceutics 2023, 15, 2233. [Google Scholar] [CrossRef]
- Baracos, V.E. On the cusp of targeted therapy for cancer cachexia—What clinical benefits might we promise our patients? Nat. Rev. Clin. Oncol. 2024, 22, 8–9. [Google Scholar] [CrossRef]
- van Winkel, C.A.J.; Pierik, F.R.; Brouwers, A.H.; de Groot, D.J.A.; de Vries, E.G.; Lub-de Hooge, M.N. Molecular imaging supports the development of multispecific cancer antibodies. Nat. Rev. Clin. Oncol. 2024, 21, 852–866. [Google Scholar] [CrossRef]
- Wang, Q.; Shao, X.; Zhang, Y.; Zhu, M.; Wang, F.X.C.; Mu, J.; Li, J.; Yao, H.; Chen, K. Role of tumor microenvironment in cancer progression and therapeutic strategy. Cancer Med. 2023, 12, 11149–11165. [Google Scholar] [CrossRef]
- Miao, L.; Huang, L. Exploring the tumor microenvironment with nanoparticles. Cancer Treat. Res. 2015, 166, 193–226. [Google Scholar]
- Liu, Y.; Zhou, J.; Li, Q.; Li, L.; Jia, Y.; Geng, F.; Zhou, J.; Yin, T. Tumor microenvironment remodeling-based penetration strategies to amplify nanodrug accessibility to tumor parenchyma. Adv. Drug Deliv. Rev. 2021, 172, 80–103. [Google Scholar] [CrossRef]
- Joseph, J.F.; Gronbach, L.; García-Miller, J.; Cruz, L.M.; Wuest, B.; Keilholz, U.; Zoschke, C.; Parr, M.K. Automated Real-Time Tumor Pharmacokinetic Profiling in 3D Models: A Novel Approach for Personalized Medicine. Pharmaceutics 2020, 12, 413. [Google Scholar] [CrossRef]
- Gutmann, D.H.; Boehm, J.S.; Karlsson, E.K.; Padron, E.; Seshadri, M.; Wallis, D.; Snyder, J.C. Precision preclinical modeling to advance cancer treatment. J. Natl. Cancer Inst. 2024, djae249. [Google Scholar] [CrossRef] [PubMed]
- Andrade, E.L.; Bento, A.F.; Cavalli, J.; Oliveira, S.K.; Schwanke, R.C.; Siqueira, J.M.; Freitas, C.S.; Marcon, R.; Calixto, J.B. Non-clinical studies in the process of new drug development—Part II: Good laboratory practice, metabolism, pharmacokinetics, safety and dose translation to clinical studies. Braz. J. Med. Biol. Res. 2016, 49, e5646. [Google Scholar] [CrossRef] [PubMed]
- Nie, L.; Rubin, E.H.; Mehrotra, N.; Pinheiro, J.; Fernandes, L.L.; Roy, A.; Bailey, S.; de Alwis, D.P. Rendering the 3 + 3 Design to Rest: More Efficient Approaches to Oncology Dose-Finding Trials in the Era of Targeted Therapy. Clin. Cancer Res. 2016, 22, 2623–2629. [Google Scholar] [CrossRef] [PubMed]
- Shi, D.; Mi, G.; Wang, M.; Webster, T.J. In vitro and ex vivo systems at the forefront of infection modeling and drug discovery. Biomaterials 2019, 198, 228–249. [Google Scholar] [CrossRef] [PubMed]
- Liston, A.; Humblet-Baron, S.; Duffy, D.; Goris, A. Human immune diversity: From evolution to modernity. Nat. Immunol. 2021, 22, 1479–1489. [Google Scholar] [CrossRef]
- Nguyen, L.N.M.; Ngo, W.; Lin, Z.P.; Sindhwani, S.; MacMillan, P.; Mladjenovic, S.M.; Chan, W.C.W. The mechanisms of nanoparticle delivery to solid tumours. Nat. Rev. Bioeng. 2024, 2, 201–213. [Google Scholar] [CrossRef]
- Egwu, C.O.; Aloke, C.; Onwe, K.T.; Umoke, C.I.; Nwafor, J.; Eyo, R.A.; Chukwu, J.A.; Ufebe, G.O.; Ladokun, J.; Audu, D.T.; et al. Nanomaterials in Drug Delivery: Strengths and Opportunities in Medicine. Molecules 2024, 29, 2584. [Google Scholar] [CrossRef]
- Sultana, A.; Zare, M.; Thomas, V.; Kumar, T.S.; Ramakrishna, S. Nano-based drug delivery systems: Conventional drug delivery routes, recent developments and future prospects. Med. Drug Discov. 2022, 15, 100134. [Google Scholar] [CrossRef]
- Ly, P.-D.; Ly, K.-N.; Phan, H.-L.; Nguyen, H.H.T.; Duong, V.-A. Recent advances in surface decoration of nanoparticles in drug delivery. Front. Nanotechnol. 2024, 6, 1456939. [Google Scholar] [CrossRef]
- Mujtaba, M.; Negi, A.; King, A.W.; Zare, M.; Kuncova-Kallio, J. Surface modifications of nanocellulose for drug delivery applications: A critical review. Curr. Opin. Biomed. Eng. 2023, 28, 100475. [Google Scholar] [CrossRef]
- Sun, X.; Hu, B. Mathematical modeling and computational prediction of cancer drug resistance. Brief. Bioinform. 2017, 19, 1382–1399. [Google Scholar] [CrossRef] [PubMed]
- Hassan, J.; Saeed, S.M.; Deka, L.; Uddin, J.; Das, D.B. Applications of Machine Learning (ML) and Mathematical Modeling (MM) in Healthcare with Special Focus on Cancer Prognosis and Anticancer Therapy: Current Status and Challenges. Pharmaceutics 2024, 16, 260. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, L.; Agarwal, S.; Tanner, K. Preclinical models for drug discovery for metastatic disease. Cell 2023, 186, 1792–1813. [Google Scholar] [CrossRef] [PubMed]
- De Jong, W.H.; Geertsma, R.E.; Borchard, G. Regulatory safety evaluation of nanomedical products: Key issues to refine. Drug Deliv. Transl. Res. 2022, 12, 2042–2047. [Google Scholar] [CrossRef]
- Oualikene-Gonin, W.; Sautou, V.; Ezan, E.; Bastos, H.; Bellissant, E.; Belgodère, L.; Maison, P.; Ankri, J.; Scientific Advisory Board of the ANSM. Regulatory assessment of nano-enabled health products in public health interest. Position of the scientific advisory board of the French National Agency for the Safety of Medicines and Health Products. Front. Public Health 2023, 11, 1125577. [Google Scholar] [CrossRef]
- Bertram-Ralph, E.; Amare, M. Factors affecting drug absorption and distribution. Anaesth. Intensive Care Med. 2023, 24, 221–227. [Google Scholar] [CrossRef]
- Abolhassani, H.; Eskandari, A.; Poor, A.S.; Zarrabi, A.; Khodadadi, B.; Karimifard, S.; Sahrayi, H.; Bourbour, M.; Yaraki, M.T. Nanobiotechnological approaches for breast cancer Management: Drug delivery systems and 3D In-Vitro models. Coord. Chem. Rev. 2024, 508, 215754. [Google Scholar] [CrossRef]
- Khalil, A.S.; Jaenisch, R.; Mooney, D.J. Engineered tissues and strategies to overcome challenges in drug development. Adv. Drug Deliv. Rev. 2020, 158, 116–139. [Google Scholar] [CrossRef]
- Katt, M.E.; Placone, A.L.; Wong, A.D.; Xu, Z.S.; Searson, P.C. In Vitro Tumor Models: Advantages, Disadvantages, Variables, and Selecting the Right Platform. Front. Bioeng. Biotechnol. 2016, 4, 12. [Google Scholar] [CrossRef]
- Wilhelm, S.; Tavares, A.J.; Dai, Q.; Ohta, S.; Audet, J.; Dvorak, H.F.; Chan, W.C.W. Analysis of nanoparticle delivery to tumours. Nat. Rev. Mater. 2016, 1, 16014. [Google Scholar] [CrossRef]
- Sabourian, P.; Yazdani, G.; Ashraf, S.S.; Frounchi, M.; Mashayekhan, S.; Kiani, S.; Kakkar, A. Effect of Physico-Chemical Properties of Nanoparticles on Their Intracellular Uptake. Int. J. Mol. Sci. 2020, 21, 8019. [Google Scholar] [CrossRef] [PubMed]
- Barua, S.; Mitragotri, S. Challenges associated with penetration of nanoparticles across cell and tissue barriers: A review of current status and future prospects. Nano Today 2014, 9, 223–243. [Google Scholar] [CrossRef] [PubMed]
- Dogra, P.; Butner, J.D.; Ramírez, J.R.; Chuang, Y.-L.; Noureddine, A.; Brinker, C.J.; Cristini, V.; Wang, Z. A mathematical model to predict nanomedicine pharmacokinetics and tumor delivery. Comput. Struct. Biotechnol. J. 2020, 18, 518–531. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Gao, S.; Yang, D.; Fang, Y.; Lin, X.; Jin, X.; Liu, Y.; Liu, X.; Su, K.; Shi, K. Influencing factors and strategies of enhancing nanoparticles into tumors in vivo. Acta Pharm. Sin. B 2021, 11, 2265–2285. [Google Scholar] [CrossRef]
- Yue, Z.-G.; Wei, W.; Lv, P.-P.; Yue, H.; Wang, L.-Y.; Su, Z.-G.; Ma, G.-H. Surface Charge Affects Cellular Uptake and Intracellular Trafficking of Chitosan-Based Nanoparticles. Biomacromolecules 2011, 12, 2440–2446. [Google Scholar] [CrossRef]
- Rehman, A.U.; Li, M.; Wu, B.; Ali, Y.; Rasheed, S.; Shaheen, S.; Liu, X.; Luo, R.; Zhang, J. Role of Artificial Intelligence in Revolutionizing Drug Discovery. Fundam. Res. 2024. [Google Scholar] [CrossRef]
- Hassanzadeh, P.; Atyabi, F.; Dinarvand, R. The significance of artificial intelligence in drug delivery system design. Adv. Drug Deliv. Rev. 2019, 151–152, 169–190. [Google Scholar] [CrossRef]
- Druedahl, L.C.; Price, W.N.; Minssen, T.; Sarpatwari, A. Use of Artificial Intelligence in Drug Development. JAMA Netw. Open 2024, 7, e2414139. [Google Scholar] [CrossRef]
- Dogra, P.; Butner, J.D.; Chuang, Y.-L.; Caserta, S.; Goel, S.; Brinker, C.J.; Cristini, V.; Wang, Z. Mathematical modeling in cancer nanomedicine: A review. Biomed. Microdevices 2019, 21, 40. [Google Scholar] [CrossRef]
- Salahshoori, I.; Golriz, M.; Nobre, M.A.; Mahdavi, S.; Malekshah, R.E.; Javdani-Mallak, A.; Jorabchi, M.N.; Khonakdar, H.A.; Wang, Q.; Mohammadi, A.H.; et al. Simulation-based approaches for drug delivery systems: Navigating advancements, opportunities, and challenges. J. Mol. Liq. 2024, 395, 123888. [Google Scholar] [CrossRef]
- Dai, X.; Chen, Y. Computational Biomaterials: Computational Simulations for Biomedicine. Adv. Mater. 2023, 35, e2204798. [Google Scholar] [CrossRef] [PubMed]
- Mazumdar, S.; Chitkara, D.; Mittal, A. Exploration and insights into the cellular internalization and intracellular fate of amphiphilic polymeric nanocarriers. Acta Pharm. Sin. B 2021, 11, 903–924. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R.; Hasan, A.; Primavera, R.; Wilson, R.J.; Thakor, A.S.; Kevadiya, B.D. Cellular uptake and retention of nanoparticles: Insights on particle properties and interaction with cellular components. Mater. Today Commun. 2020, 25, 101692. [Google Scholar] [CrossRef]
- Behzadi, S.; Serpooshan, V.; Tao, W.; Hamaly, M.A.; Alkawareek, M.Y.; Dreaden, E.C.; Brown, D.; Alkilany, A.M.; Farokhzad, O.C.; Mahmoudi, M. Cellular uptake of nanoparticles: Journey inside the cell. Chem. Soc. Rev. 2017, 46, 4218–4244. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Clausen, J.R.; Rao, R.R.; Aidun, C.K. Nanoparticle diffusion in sheared cellular blood flow. J. Fluid Mech. 2019, 871, 636–667. [Google Scholar] [CrossRef]
- Lee, T.-R.; Choi, M.; Kopacz, A.M.; Yun, S.-H.; Liu, W.K.; Decuzzi, P. On the near-wall accumulation of injectable particles in the microcirculation: Smaller is not better. Sci. Rep. 2013, 3, 2079. [Google Scholar] [CrossRef]
- Peng, W.; Minli, B.; Jizu, L.; Chengzhi, H.; Yuyan, W. Numerical Investigation on the Turbulent Flow Characteristic of Nanofluids in a Horizontal Circular Tube. Numer. Heat Transf. Part A Appl. 2014, 66, 646–668. [Google Scholar] [CrossRef]
- Ahumada-Lazo, J.A.; Chen, R.H. Effects of nanoparticle concentration and peclet number on nanofluid droplet evaporation behavior. Int. J. Therm. Sci. 2022, 178, 107582. [Google Scholar] [CrossRef]
- Xu, Z.; Kleinstreuer, C. Direct nanodrug delivery for tumor targeting subject to shear-augmented diffusion in blood flow. Med. Biol. Eng. Comput. 2018, 56, 1949–1958. [Google Scholar] [CrossRef]
- Lin, C.; Kaper, H.J.; Li, W.; Splinter, R.; Sharma, P.K. Role of endothelial glycocalyx in sliding friction at the catheter-blood vessel interface. Sci. Rep. 2020, 10, 11855. [Google Scholar] [CrossRef]
- Kosmidis, K.; Dassios, G. Monte Carlo simulations in drug release. J. Pharmacokinet. Pharmacodyn. 2019, 46, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.H.; Zhang, X.P.; Zhao, Z.Q.; Guo, X.D. Dissipative Particle Dynamics Aided Design of Drug Delivery Systems: A Review. Mol. Pharm. 2020, 17, 1778–1799. [Google Scholar] [CrossRef]
- Galdi, I.; Lamberti, G. Drug release from matrix systems: Analysis by finite element methods. Heat Mass Transf. 2012, 48, 519–528. [Google Scholar] [CrossRef]
- Casalini, T.; Limongelli, V.; Schmutz, M.; Som, C.; Jordan, O.; Wick, P.; Borchard, G.; Perale, G. Molecular Modeling for Nanomaterial-Biology Interactions: Opportunities, Challenges, and Perspectives. Front. Bioeng. Biotechnol. 2019, 7, 268. [Google Scholar] [CrossRef]
- Borówko, M.; Staszewski, T. Molecular Dynamics Simulations of Different Nanoparticles at Substrates. Int. J. Mol. Sci. 2024, 25, 4550. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Zhang, P.; Sun, H.; Dai, Y.; Liang, S.; Bai, X.; Feng, L. Optimization of Nanoparticles for Smart Drug Delivery: A Review. Nanomaterials 2021, 11, 2790. [Google Scholar] [CrossRef] [PubMed]
- Ekhator, C.; Qureshi, M.Q.; Zuberi, A.W.; Hussain, M.; Sangroula, N.; Yerra, S.; Devi, M.; Naseem, M.A.; Bellegarde, S.B.; Pendyala, P.R.; et al. Advances and Opportunities in Nanoparticle Drug Delivery for Central Nervous System Disorders: A Review of Current Advances. Cureus 2023, 15, e44302. [Google Scholar] [CrossRef]
- Mollazadeh, S.; Sahebkar, A.; Shahlaei, M.; Moradi, S. Nano drug delivery systems: Molecular dynamic simulation. J. Mol. Liq. 2021, 332, 115823. [Google Scholar] [CrossRef]
- Akalin, A.A.; Dedekargınoğlu, B.; Choi, S.R.; Han, B.; Ozcelikkale, A. Predictive Design and Analysis of Drug Transport by Multiscale Computational Models Under Uncertainty. Pharm. Res. 2023, 40, 501–523. [Google Scholar] [CrossRef]
- Goldberg, E.; Scheringer, M.; Bucheli, T.D.; Hungerbühler, K. Critical Assessment of Models for Transport of Engineered Nanoparticles in Saturated Porous Media. Environ. Sci. Technol. 2014, 48, 12732–12741. [Google Scholar] [CrossRef]
- Ju, B.; Fan, T. Experimental study and mathematical model of nanoparticle transport in porous media. Powder Technol. 2009, 192, 195–202. [Google Scholar] [CrossRef]
- Ju, B.; Dai, S.; Luan, Z.; Zhu, T.; Su, X.; Qiu, X. A study of wettability and permeability change caused by adsorption of nanometer structured polysilicon on the surface of porous media. In Proceedings of the SPE Asia Pacific Oil and Gas Conference and Exhibition, Melbourne, Australia, 8–10 October 2002. [Google Scholar] [CrossRef]
- Irfan, S.A.; Shafie, A.; Yahya, N.; Zainuddin, N. Mathematical Modeling and Simulation of Nanoparticle-Assisted Enhanced Oil Recovery—A Review. Energies 2019, 12, 1575. [Google Scholar] [CrossRef]
- Kashkooli, F.M.; Soltani, M.; Momeni, M.M.; Rahmim, A. Enhanced Drug Delivery to Solid Tumors via Drug-Loaded Nanocarriers: An Image-Based Computational Framework. Front. Oncol. 2021, 11, 655781. [Google Scholar] [CrossRef]
- Mircioiu, C.; Voicu, V.; Anuta, V.; Tudose, A.; Celia, C.; Paolino, D.; Fresta, M.; Sandulovici, R.; Mircioiu, I. Mathematical Modeling of Release Kinetics from Supramolecular Drug Delivery Systems. Pharmaceutics 2019, 11, 140. [Google Scholar] [CrossRef]
- Lux, J.; Anguy, Y. A Study of the Behavior of Implicit Pressure Explicit Saturation (IMPES) Schedules for Two-phase Flow in Dynamic Pore Network Models. Transp. Porous Media 2012, 93, 203–221. [Google Scholar] [CrossRef]
- Hofer, S.; Hofstätter, N.; Punz, B.; Hasenkopf, I.; Johnson, L.; Himly, M. Immunotoxicity of nanomaterials in health and disease: Current challenges and emerging approaches for identifying immune modifiers in susceptible populations. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2022, 14, e1804. [Google Scholar] [CrossRef]
- Li, J.; Gao, X.; Wang, Y.; Xia, T.; Zhao, Y.; Meng, H. Precision design of engineered nanomaterials to guide immune systems for disease treatment. Matter 2022, 5, 1162–1191. [Google Scholar] [CrossRef]
- Hasan, M.R.; Alsaiari, A.A.; Fakhurji, B.Z.; Molla, M.H.R.; Asseri, A.H.; Sumon, M.A.A.; Park, M.N.; Ahammad, F.; Kim, B. Application of Mathematical Modeling and Computational Tools in the Modern Drug Design and Development Process. Molecules 2022, 27, 4169. [Google Scholar] [CrossRef]
- Ashwini, T.; Narayan, R.; Shenoy, P.A.; Nayak, U.Y. Computational modeling for the design and development of nano based drug delivery systems. J. Mol. Liq. 2022, 368, 120596. [Google Scholar]
- Askin, S.; Burkhalter, D.; Calado, G.; El Dakrouni, S. Artificial Intelligence Applied to clinical trials: Opportunities and challenges. Heal. Technol. 2023, 13, 203–213. [Google Scholar] [CrossRef]
- Weissler, E.H.; Naumann, T.; Andersson, T.; Ranganath, R.; Elemento, O.; Luo, Y.; Freitag, D.F.; Benoit, J.; Hughes, M.C.; Khan, F.; et al. The role of machine learning in clinical research: Transforming the future of evidence generation. Trials 2021, 22, 537. [Google Scholar]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- Elahi, M.; Afolaranmi, S.O.; Lastra, J.L.M.; Garcia, J.A.P. A comprehensive literature review of the applications of AI techniques through the lifecycle of industrial equipment. Discov. Artif. Intell. 2023, 3, 43. [Google Scholar] [CrossRef]
- De Spirito, M.; Palmieri, V.; Perini, G.; Papi, M. Bridging the Gap: Integrating 3D Bioprinting and Microfluidics for Advanced Multi-Organ Models in Biomedical Research. Bioengineering 2024, 11, 664. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).