Benign and Malignant Tumors of the Hand: Patterns, Pathology, and Surgical Outcomes in a Large Retrospective Cohort
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
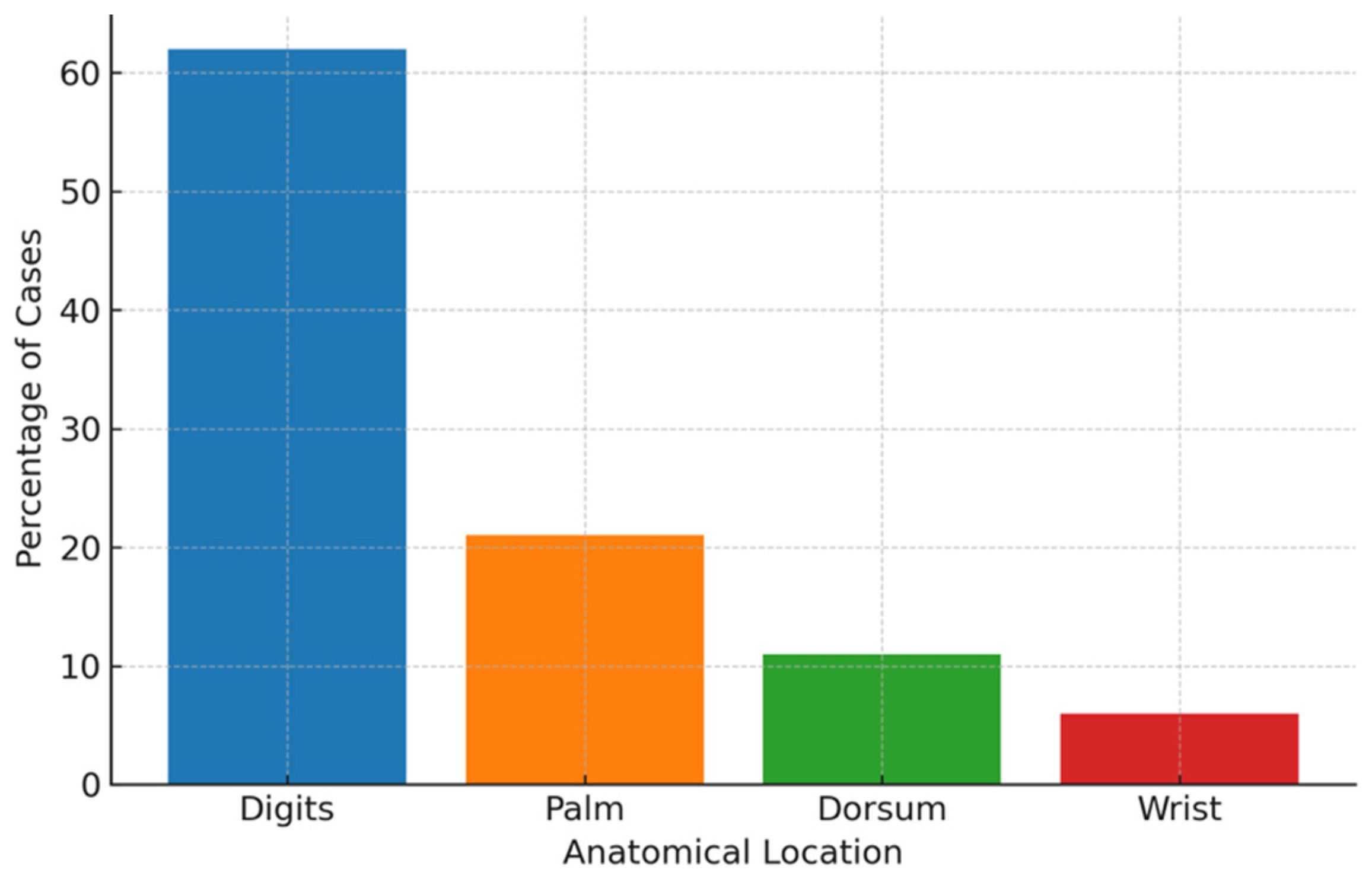
3. Results
3.1. Tumor-like Lesions
3.2. Benign Neoplasms
3.3. Malignant Tumors
3.4. Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BCC | Basal cell carcinoma |
| CT | Computed tomography |
| CSF1R | Colony-Stimulating Factor 1 Receptor |
| EDTA | Ethylenediaminetetraacetic Acid |
| GCTTS | Giant Cell Tumor of the Tendon Sheath |
| H&E | Hematoxylin and Eosin |
| MRI | Magnetic Resonance Imaging |
| SCC | Squamous Cell Carcinoma |
References
- AbuMoussa, S.; Roshan, M.P.; Souza, F.F.; Daley, D.; Rosenberg, A.; Pretell, J.; Fullerton, N.; Subhawong, T. Soft Tissue Masses of the Hand: A Review of Clinical Presentation and Imaging Features. Curr. Oncol. 2023, 30, 2032–2048. [Google Scholar] [CrossRef]
- Fujibuchi, T.; Imai, H.; Miyawaki, J.; Kidani, T.; Kiyomatsu, H.; Miura, H. Miura Hand tumors: A review of 186 patients at a single institute. J. Orthop. Surg. 2021, 29, 2309499021993994. [Google Scholar] [CrossRef]
- Marty, F.L.; Marteau, E.; Rosset, P.; Faizon, G. A retrospective study of hand and wrist tumors in adults. Chir. Main 2010, 29, 183–187. [Google Scholar] [CrossRef]
- Lans, J.; Yue, K.-L.C.; Castelein, R.M.; Suster, D.I.; Nielsen, G.P.; Chen, N.C.; Lozano-Calderon, S.A. Benign Hand Tumors (Part II): Soft Tissue Tumors. Hand 2020, 17, 519–528. [Google Scholar] [CrossRef]
- Yue, K.-L.C.; Lans, J.; Castelein, R.M.; Suster, D.I.; Nielsen, G.P.; Chen, N.C.; Lozano-Calderón, S.A. Benign Hand Tumors (Part I): Cartilaginous and Bone Tumors. Hand 2020, 17, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.J.; Pogoda, P.; Hövelborn, F.; Krause, M.; Zustin, J.; Amling, M.; Barvencik, F. Incidence, histopathologic analysis and distribution of tumours of the hand. BMC Musculoskelet. Disord. 2014, 15, 182. [Google Scholar] [CrossRef]
- Cavit, A.; Ozcanli, H.; Sancmis, M.; Ocak, G.A.; Gurer, E.I. Tumorous conditions of the hand: A retrospective review of 402 cases. Turk. J. Pathol. 2017, 34, 66–72. [Google Scholar] [CrossRef] [PubMed]
- De Vitis, R.; Vitiello, R.; Perna, A.; Passiatore, M.; Cipolloni, V.; Pripp, C.; Taccardo, G. Hand’s aneurysmal bone cyst: A rare localization. case report and systematic literature review. Orthop. Rev. 2020, 12, 23–28. [Google Scholar] [CrossRef]
- De Vitis, R.; D’ORio, M.; Fiorentino, V.; Passiatore, M. Primary lymphoma of the medial cutaneous nerve of the forearm: The first case in a pure sensory nerve of the upper limb. BMJ Case Rep. 2022, 15, e248597. [Google Scholar] [CrossRef] [PubMed]
- De Vitis, R.; Passiatore, M.; Barchetti, G.; Ceravolo, I.; Larocca, L.; Starnoni, M.; Federico, F.; Castri, F.; Taccardo, G. Pattern of a Primary B-Cell Lymphoma in Ulnar Nerve: Intraneural or Extraneural. Georgian Med. News 2023, 335, 99–103. [Google Scholar] [PubMed]
- Pertea, M.; Grosu, O.M.; Filip, A.; Moraru, D.C.; Luca, S.; Fotea, M.-C.; Lunca, S.; Olinici, D.; Poroch, V.; Carp, C.; et al. Rare Benign Tumors and Tumor-Like Lesions of the Hand Without Skin Damage—Clinical, Imagistic and Histopathological Diagnosis, Retrospective Study. Diagnostics 2023, 13, 1204. [Google Scholar] [CrossRef]
- Sureen, S.K.; Singhal, V.K.; Alaswad, F.D.; Bilal, H.Y.; Mohammed, O.E.A. Frequency of Painful Benign Tumors of Hand: HULS Report. J. Orthop. Sports Med. 2025, 7, 287–291. [Google Scholar] [CrossRef]
- Chong, P.Q.Y.; Choudhury, M.M.; Chung, S.R.; Yap, R.T.J.; Chia, D.S.Y.; Jiang, J.K.H.; Chin, A.Y.H.; McGrouther, D.A. A multivariate analysis on characteristics of hand and wrist tumours: A multiethnic study. Singap. Med. J. 2024; epub ahead of print. [Google Scholar] [CrossRef]
- Zaidi, Z.; Acha, D.V.; Wahid, M.; McCranie, A.; Kargel, J.; Sajjad, S.A. Malignant and Bony Tumors of the Pediatric Hand: A Review of Diagnosis and Treatment Strategies. Cureus 2025, 17, e86907. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, H.; Heydari, S.; Hushmandi, K.; Daneshi, S.; Raesi, R. Raesi Bone tumors: A systematic review of prevalence, risk determinants, and survival patterns. BMC Cancer 2025, 25, 321. [Google Scholar] [CrossRef]
- Amer, K.; Otero, K.; Smith, B.; Datiashvili, R. Hand Tumors: An Individual Surgeon’s Retrospective Review. Eplasty 2022, 22, e1. [Google Scholar] [PubMed Central]
- Jerome, J.T.J.; Karunanithi, D. Giant cell tumor of the tendon sheath: A critical review of current diagnostic and therapeutic approaches with treatment recommendations for hand and foot lesions. J. Musculoskelet. Surg. Res. 2024, 9, 28–41. [Google Scholar] [CrossRef]
- Albanese, K.M.; Lynch, C.P.; Eswaran, S.P.; Damron, T.A. Benign Bone Tumors of the Hand: Beyond Enchondromas. J. Am. Acad. Orthop. Surg. 2024, 33, e1000–e1016. [Google Scholar] [CrossRef]
- Park, H.Y.; Joo, M.W.; Choi, Y.-H.; Chung, Y.-G.; Park, C.J. Park Simple curettage and allogeneic cancellous bone chip impaction grafting in solitary enchondroma of the short tubular bones of the hand. Sci. Rep. 2023, 13, 2081. [Google Scholar] [CrossRef]
- Fang, L.; Abdullah, S.; Tadrousse, K.; Sapuan, J.; Hami, R.B.; Moni, A.S.B. Outcome predictors of clinically diagnosed benign upper extremity soft tissue masses: A retrospective study. J. Orthop. Rep. 2025, 4, 100607. [Google Scholar] [CrossRef]
- Alexander, L. Epithelioid Sarcoma of Upper Extremity: Diagnostic Dilemma with Therapeutic Challenges. Cureus 2021, 13, e14156. [Google Scholar] [CrossRef]
- Sobanko, J.F.; Meijer, L.; Nigra, T.P. Epithelioid Sarcoma: A Review and Update. J. Clin. Aesthetic Dermatol. 2009, 2, 49–54. [Google Scholar]
- Gounder, M.; Schöffski, P.; Jones, R.L.; Agulnik, M.; Cote, G.M.; Villalobos, V.M.; Attia, S.; Chugh, R.; Chen, T.W.-W.; Jahan, T.; et al. Tazemetostat in advanced epithelioid sarcoma with loss of INI1/SMARCB1: An international, open-label, phase 2 basket study. Lancet Oncol. 2020, 21, 1423–1432. [Google Scholar] [CrossRef]
- Komurcugil, I.; Arslan, Z.; Bal, Z.I.; Aydogan, M.; Ciman, Y. Cutaneous metastases different clinical presentations: Case series and review of the literature. Dermatol. Rep. 2022, 15, 9553. [Google Scholar] [CrossRef]
- Fones, L.; Schroeder, J.T.; Beredjiklian, P.K.; Gallant, G.G. Acral Metastasis to the Hand as the Primary Presentation of Malignancy. J. Hand Surg. Glob. Online 2024, 6, 593–596. [Google Scholar] [CrossRef]
- Umana, G.E.; Scalia, G.; Palmisciano, P.; Passanisi, M.; Da Ros, V.; Pompili, G.; Barone, F.; Amico, P.; Tomasi, S.O.; Graziano, F.; et al. Acrometastases to the hand: A systematic review. Medicina 2021, 57, 950. [Google Scholar] [CrossRef]
- Lazerges, C.; Degeorge, B.; Coulet, B.; Chammas, M. Diagnosis and treatment of hand tumors. Orthop. Traumatol. Surg. Res. 2021, 108, 103153. [Google Scholar] [CrossRef]
- Cengiz, T.; Şimşek, Ş.A.; Bayar, E.; Erdoğan, F.; Yurtbay, A.; Coşkun, H.S.; Pişkin, A.; Dabak, N. Tenosynovial Giant Cell Tumors of the Hand: Analysis of Risk Factors for Surgical Margin and Recurrence. Medicina 2025, 61, 949. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Panagopoulos, G.N.; Angelini, A.; Lesenský, J.; Vottis, C.; Megaloikonomos, P.D.; Kokkalis, Z.T.; Kontogeorgakos, V.; Ruggieri, P.; Papagelopoulos, P.J. Tumors of the hand. Eur. J. Orthop. Traumatol. 2017, 27, 747–762. [Google Scholar] [CrossRef]
- Muramatsu, K.; Ihara, K.; Yoshida, K.; Tominaga, Y.; Hashimoto, T.; Taguchi, T. Musculoskeletal sarcomas in the forearm and hand: Standard treatment and microsurgical reconstruction for limb salvage. Anticancer. Res. 2013, 33, 4175–4182. [Google Scholar]
- Bocchino, G.; Capece, G.; Pietramala, S.; Rovere, G.; Rocchi, L.; Farsetti, P.; Maccauro, G.; Fulchignoni, C. Myoepithelioma of the Hand: A Systematic Review. Appl. Sci. 2024, 14, 9149. [Google Scholar] [CrossRef]
| Lesion Type | Total (n) | Male (n) | Female (n) | Age Range (yrs) |
|---|---|---|---|---|
| Mucous cyst | 24 | 6 | 18 | 19–84 |
| Foreign body granuloma | 24 | 13 | 11 | 19–73 |
| Pyogenic granuloma | 18 | 7 | 11 | 23–85 |
| Epidermoid cyst | 11 | 10 | 1 | 32–61 |
| Viral wart | 10 | 8 | 2 | 24–76 |
| Neuroma | 5 | 5 | 3 | 22–49 |
| Total | 94 | 49 | 46 |
| Tumor Type | Total (n) | Male (n) | Female (n) | Age Range (yrs) |
|---|---|---|---|---|
| Giant cell tumor of the tendon sheath (GCTTS) | 39 | 14 | 26 | 14–81 |
| Hemangioma | 15 | 6 | 9 | 25–58 |
| Lipoma | 13 | 6 | 7 | 24–81 |
| Glomus tumor | 12 | 4 | 8 | 23–62 |
| Fibroma | 11 | 8 | 3 | 20–65 |
| Keratoacanthoma | 11 | 2 | 9 | 70–92 |
| Osteochondroma | 7 | 2 | 5 | 23–71 |
| Schwannoma | 5 | 3 | 2 | 73–75 |
| Neurofibroma | 4 | 1 | 3 | 32–70 |
| Other benign tumors * | 6 | 5 | 1 | 16–45 |
| Total | 123 | 51 | 72 |
| Tumor Type | Total (n) | Male (n) | Female (n) | Age Range (yrs) |
|---|---|---|---|---|
| Squamous cell carcinoma | 10 | 7 | 3 | 47–87 |
| Basal cell carcinoma | 8 | 7 | 1 | 51–80 |
| Melanoma | 5 | 3 | 2 | 45–90 |
| Epithelioid hemangioendothelioma | 1 | 0 | 1 | 33 |
| Liposarcoma | 1 | 1 | 0 | 46 |
| Spino-basocellular carcinoma | 1 | 1 | 0 | 84 |
| Total | 26 | 19 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Battaglia, F.; Giuffrida, R.; Pagano, M.; Troisi, L.; Delia, G. Benign and Malignant Tumors of the Hand: Patterns, Pathology, and Surgical Outcomes in a Large Retrospective Cohort. Cancers 2025, 17, 3079. https://doi.org/10.3390/cancers17183079
Battaglia F, Giuffrida R, Pagano M, Troisi L, Delia G. Benign and Malignant Tumors of the Hand: Patterns, Pathology, and Surgical Outcomes in a Large Retrospective Cohort. Cancers. 2025; 17(18):3079. https://doi.org/10.3390/cancers17183079
Chicago/Turabian StyleBattaglia, Fabiana, Roberta Giuffrida, Marco Pagano, Luigi Troisi, and Gabriele Delia. 2025. "Benign and Malignant Tumors of the Hand: Patterns, Pathology, and Surgical Outcomes in a Large Retrospective Cohort" Cancers 17, no. 18: 3079. https://doi.org/10.3390/cancers17183079
APA StyleBattaglia, F., Giuffrida, R., Pagano, M., Troisi, L., & Delia, G. (2025). Benign and Malignant Tumors of the Hand: Patterns, Pathology, and Surgical Outcomes in a Large Retrospective Cohort. Cancers, 17(18), 3079. https://doi.org/10.3390/cancers17183079






