Clinicopathological Factors Affecting Prognosis in Patients with Advanced Cervical Cancer Undergoing Concurrent Chemoradiation Therapy
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Selection
2.2. Clinicopathological Data Collection
2.3. Definitive Concurrent Chemoradiotherapy Procedure
2.4. Follow-Up
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Kang, S.; Wu, J.; Li, J.; Hou, Q.; Tang, B. Prognostic significance of clinicopathological factors influencing overall survival and event-free survival of patients with cervical cancer: A systematic review and meta-analysis. Med. Sci. Monit. 2022, 28, e934588. [Google Scholar] [CrossRef]
- Walboomers, J.M.; Jacobs, M.V.; Manos, M.M.; Bosch, F.X.; Kummer, J.A.; Shah, K.V.; Snijders, P.J.; Peto, J.; Meijer, C.J.; Muñoz, N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 1999, 189, 12–19. [Google Scholar] [CrossRef]
- Kweon, S.S. Updates on cancer epidemiology in Korea, 2018. Chonnam Med. J. 2018, 54, 90–100. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bhatla, N.; Aoki, D.; Sharma, D.N.; Sankaranarayanan, R. Cancer of the cervix uteri. Int. J. Gynaecol. Obstet. 2018, 143, 22–36. [Google Scholar] [CrossRef]
- Cohen, P.A.; Jhingran, A.; Oaknin, A.; Denny, L. Cervical cancer. Lancet 2019, 393, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Peters, W.A., 3rd; Liu, P.Y.; Barrett, R.J., 2nd; Stock, R.J.; Monk, B.J.; Berek, J.S.; Souhami, L.; Grigsby, P.; Gordon, W.; Alberts, D.S. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J. Clin. Oncol. 2000, 18, 1606–1613. [Google Scholar] [CrossRef]
- Whitney, C.W.; Sause, W.; Bundy, B.N.; Malfetano, J.H.; Hannigan, E.V.; Fowler, W.C.; Clarke-Pearson, D.L.; Liao, S.Y. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: A gynecologic oncology group and Southwest oncology group study. J. Clin. Oncol. 1999, 17, 1339–1348. [Google Scholar] [CrossRef]
- Liu, J.; Tang, G.; Zhou, Q.; Kuang, W. Outcomes and prognostic factors in patients with locally advanced cervical cancer treated with concurrent chemoradiotherapy. Radiat. Oncol. 2022, 17, 142. [Google Scholar] [CrossRef]
- Marchetti, C.; Fagotti, A.; Tombolini, V.; Scambia, G.; De Felice, F. Survival and toxicity in neoadjuvant chemotherapy plus surgery versus definitive chemoradiotherapy for cervical cancer: A systematic review and meta-analysis. Cancer Treat. Rev. 2020, 83, 101945. [Google Scholar] [CrossRef]
- Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: A systematic review and meta-analysis of individual patient data from 18 randomized trials. J. Clin. Oncol. 2008, 26, 5802–5812. [Google Scholar] [CrossRef]
- Chen, C.C.; Wang, L.; Lin, J.C.; Jan, J.S. The prognostic factors for locally advanced cervical cancer patients treated by intensity-modulated radiation therapy with concurrent chemotherapy. J. Formos. Med. Assoc. 2015, 114, 231–237. [Google Scholar] [CrossRef][Green Version]
- Endo, D.; Todo, Y.; Okamoto, K.; Minobe, S.; Kato, H.; Nishiyama, N. Prognostic factors for patients with cervical cancer treated with concurrent chemoradiotherapy: A retrospective analysis in a Japanese cohort. J. Gynecol. Oncol. 2015, 26, 12–18. [Google Scholar] [CrossRef]
- Phung, H.T.; Truong, M.C.; Nguyen, L.T.; Dang, A.T.V.; Vu, T.H.; Nguyen, H.T. Treatment outcome and prognosis factors of FIGO 2018 Stage III cervical cancer patients treated with definitive concurrent chemoradiation in Vietnam. Asian Pac. J. Cancer Prev. 2021, 22, 853–859. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, L.H.; Litière, S.; de Vries, E.; Ford, R.; Gwyther, S.; Mandrekar, S.; Shankar, L.; Bogaerts, J.; Chen, A.; Dancey, J.; et al. RECIST 1.1-Update and clarification: From the RECIST committee. Eur. J. Cancer 2016, 62, 132–137. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI classification percentile and cut off points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Miccò, M.; Lupinelli, M.; Mangialardi, M.; Gui, B.; Manfredi, R. Patterns of recurrent disease in cervical cancer. J. Pers. Med. 2022, 12, 755. [Google Scholar] [CrossRef] [PubMed]
- Medici, F.; Ferioli, M.; Cammelli, S.; Forlani, L.; Laghi, V.; Ma, J.; Cilla, S.; Buwenge, M.; Macchia, G.; Deodato, F.; et al. Sarcopenic obesity in cervical carcinoma: A strong and independent prognostic factor beyond the conventional predictors (Esther study-AFRAID project). Cancers 2024, 16, 929. [Google Scholar] [CrossRef]
- Grigsby, P.W.; Massad, L.S.; Mutch, D.G.; Powell, M.A.; Thaker, P.H.; McCourt, C.; Hagemann, A.; Fuh, K.; Kuroki, L.; Schwarz, J.K.; et al. FIGO 2018 staging criteria for cervical cancer: Impact on stage migration and survival. Gynecol. Oncol. 2020, 157, 639–643. [Google Scholar] [CrossRef]
- Song, S.; Kim, J.Y.; Kim, Y.J.; Yoo, H.J.; Kim, S.H.; Kim, S.K.; Lim, M.C.; Kang, S.; Seo, S.S.; Park, S.Y. The size of the metastatic lymph node is an independent prognostic factor for the patients with cervical cancer treated by definitive radiotherapy. Radiother. Oncol. 2013, 108, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.C.; Lin, L.C.; Kuo, Y.T.; Lin, Y.W. Radiographic number of positive pelvic lymph nodes as a prognostic factor in cervical cancer treated with definitive concurrent chemoradiotherapy or intensity-modulated radiotherapy. Front. Oncol. 2018, 8, 546. [Google Scholar] [CrossRef]
- Pedone Anchora, L.; Carbone, V.; Gallotta, V.; Fanfani, F.; Cosentino, F.; Turco, L.C.; Fedele, C.; Bizzarri, N.; Scambia, G.; Ferrandina, G. Should the number of metastatic pelvic lymph nodes be integrated into the 2018 figo staging classification of early stage cervical cancer? Cancers 2020, 12, 1552. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Yun, B.S.; Kim, J.H.; Jeon, S.; Eom, K.Y.; Roh, J.W. Therapeutic effects of surgical debulking of metastatic lymph nodes in cervical cancer stage IIICr: A phase III, randomized controlled clinical trial (KGOG 1047/DEBULK Trial). Int. J. Gynecol. Cancer 2024, 34, A560–A561. [Google Scholar] [CrossRef]
- Jethwa, K.R.; Jang, S.; Gonuguntla, K.; Evans, J.; Block, M.S.; Kumar, A.; Langstraat, C.; Whitaker, T.; Day, C.; Deufel, C.; et al. Lymph node-directed simultaneous integrated boost in patients with clinically lymph node-positive cervical cancer treated with definitive chemoradiation: Clinical outcomes and toxicity. Int. J. Radiat. Oncol. 2018, 102, e625–e626. [Google Scholar] [CrossRef]
- McCormack, M.; Rincón, D.G.; Eminowicz, G.; Diez, P.; Farrelly, L.; Kent, C.; Hudson, E.; Panades, M.; Mathews, T.; Anand, A.; et al. LBA8 A randomised phase III trial of induction chemotherapy followed by chemoradiation compared with chemoradiation alone in locally advanced cervical cancer: The GCIG INTERLACE trial. Ann. Oncol. 2023, 34, S1276. [Google Scholar] [CrossRef]
- Grau-Bejar, J.F.; Garcia-Duran, C.; Garcia-Illescas, D.; Mirallas, O.; Oaknin, A. Advances in immunotherapy for cervical cancer. Ther. Adv. Med. Oncol. 2023, 15, 17588359231163836. [Google Scholar] [CrossRef]
- Lorusso, D.; Xiang, Y.; Hasegawa, K.; Scambia, G.; Leiva, M.; Ramos-Elias, P.; Acevedo, A.; Sukhin, V.; Cloven, N.; Pereira de Santana Gomes, A.J.; et al. Pembrolizumab or placebo with chemoradiotherapy followed by pembrolizumab or placebo for newly diagnosed, high-risk, locally advanced cervical cancer (ENGOT-cx11/GOG-3047/KEYNOTE-A18): A randomised, double-blind, phase 3 clinical trial. Lancet 2024, 403, 1341–1350. [Google Scholar] [CrossRef] [PubMed]
- Pötter, R.; Tanderup, K.; Kirisits, C.; de Leeuw, A.; Kirchheiner, K.; Nout, R.; Tan, L.T.; Haie-Meder, C.; Mahantshetty, U.; Segedin, B.; et al. The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin. Transl. Radiat. Oncol. 2018, 9, 48–60. [Google Scholar] [CrossRef]
- Gnade, C.M.; Hill, E.K.; Botkin, H.E.; Hefel, A.R.; Hansen, H.E.; Sheets, K.A.; Mott, S.L.; Hardy-Fairbanks, A.J.; Stockdale, C.K. Effect of obesity on cervical cancer screening and outcomes. J. Low. Genit. Tract. Dis. 2020, 24, 358–362. [Google Scholar] [CrossRef]
- Clark, L.H.; Jackson, A.L.; Soo, A.E.; Orrey, D.C.; Gehrig, P.A.; Kim, K.H. Extremes in body mass index affect overall survival in women with cervical cancer. Gynecol. Oncol. 2016, 141, 497–500. [Google Scholar] [CrossRef]
- Xiao, M.; Wang, L.; Tang, Q.; Yang, X.; Zhu, G. Postoperative tumor treatment strategies: From basic research to clinical therapy. VIEW 2024, 5, 20230117. [Google Scholar] [CrossRef]
- Volgger, B.; Aspisirengil, C.; Genser-Krimbacher, E.; Ciresa-Koenig, A.; Daxenbichler, G.; Fuchs, D.; Windbichler, G.; Marth, C. Prognostic significance of TPA versus SCC-Ag, CEA and neopterin in carcinoma of the uterine cervix. Cancer Lett. 2008, 262, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Dattoli, M.J.; Gretz, H.F., 3rd; Beller, U.; Lerch, I.A.; Demopoulos, R.I.; Beckman, E.M.; Fried, P.R. Analysis of multiple prognostic factors in patients with stage IB cervical cancer: Age as a major determinant. Int. J. Radiat. Oncol. Biol. Phys. 1989, 17, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Sturdza, A.E.; Pötter, R.; Kossmeier, M.; Kirchheiner, K.; Mahantshetty, U.; Haie-Meder, C.; Lindegaard, J.C.; Jurgenliemk-Schulz, I.; Tan, L.T.; Hoskin, P.; et al. Nomogram predicting overall survival in patients with locally advanced cervical cancer treated with radiochemotherapy including image-guided brachytherapy: A retro-EMBRACE study. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 168–177. [Google Scholar] [CrossRef] [PubMed]




| Variables | No. of Patients (n = 128) | Value (%) |
|---|---|---|
| Age | ||
| Median | 59 (32–87) | |
| <50 | 27 | 21.1 |
| ≥50 | 101 | 78.9 |
| Body mass index (kg/m2) | ||
| Mean | 24.0 ± 3.9 | |
| <25 | 87 | 68.0 |
| ≥25 | 41 | 32.0 |
| FIGO stage (2018) | ||
| IB2 | 1 | 0.8 |
| IIA2 | 1 | 0.8 |
| IIB | 33 | 25.8 |
| IIIB | 6 | 4.7 |
| IIIC1r | 60 | 46.9 |
| IIIC2r | 22 | 17.2 |
| IVA | 5 | 3.9 |
| Histology | ||
| Non-SCC | 14 | 10.9 |
| SCC | 114 | 89.1 |
| Tumor size (cm) | Mean = 4.9 ± 1.4 | |
| <4 | 28 | 21.9 |
| ≥4 | 100 | 78.1 |
| HPV infection | ||
| Negative | 5 | 3.9 |
| Positive | 123 | 96.1 |
| Lymph node metastasis | ||
| Negative | 40 | 31.3 |
| PLN or PALN | 88 | 68.8 |
| PALN metastasis | ||
| No | 104 | 81.3 |
| Yes | 24 | 18.8 |
| Parametrial invasion | ||
| No | 6 | 4.7 |
| Yes | 122 | 95.3 |
| SCC Ag | ||
| <2 | 39 | 31.7 |
| ≥2 | 84 | 68.3 |
| Recurrence | ||
| No | 93 | 72.7 |
| Yes | 35 | 27.3 |
| Response to CCRT (n = 128) | Percent (%) |
|---|---|
| CR 107 | 83.6 |
| PR 16 | 12.5 |
| SD 4 | 3.1 |
| PD 1 | 0.8 |
| Recurrence Pattern (n = 35) | Number of patients |
| Local | 2 |
| Regional | 4 |
| Distant | 29 |
| Sites of Recurrence | Number of patients |
| Intrapelvic space (including pelvic lymph nodes) | 14 |
| Para-aortic Lymph nodes | 11 |
| Lung | 9 |
| Mediastinum | 3 |
| Liver | 3 |
| Bone | 4 |
| Other distant (SCN/Inguinal nodes/Axillary nodes/Psoas muscle) | 14 |
| Variables | Recur | OR | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Age | <50 | 20 | 7 | 0.994 | 0.345–2.868 | 0.991 |
| ≥50 | 73 | 28 | ||||
| BMI (kg/m2) | <25 | 67 | 20 | 2.737 | 1.093–6.855 | 0.032 |
| ≥25 | 26 | 15 | ||||
| Tumor size (cm) | <4 | 22 | 6 | 2.394 | 0.720–7.694 | 0.154 |
| ≥4 | 71 | 29 | ||||
| PLN or PALN metastasis | No | 34 | 6 | 1.584 | 0.537–4.673 | 0.405 |
| Yes | 59 | 29 | ||||
| PALN metastasis | No | 83 | 21 | 5.892 | 2.030–17.097 | 0.001 |
| Yes | 10 | 14 | ||||
| Parametrial invasion | No | 4 | 2 | 0.742 | 0.130–4.241 | 0.737 |
| Yes | 89 | 33 | ||||
| SCC Ag | <2 | 28 | 11 | 0.848 | 0.361–1.994 | 0.706 |
| ≥2 | 63 | 21 | ||||
| Variables | Beta | SE | OR | 95% CI | p-Value | |
| BMI ≥ 25 kg/m2) | 0.992 | 0.464 | 2.697 | 1.087–6.692 | 0.032 | |
| Tumor size (≥4 cm) | 0.946 | 0.594 | 2.574 | 0.804–8.239 | 0.111 | |
| PALN metastasis | 1.939 | 0.512 | 6.931 | 2.540–18.916 | <0.001 | |
| Variables | PFS | TFI | OS | |||
|---|---|---|---|---|---|---|
| H.R (95% CI) | p Value | H.R (95% CI) | p Value | H.R (95% CI) | p Value | |
| Age (≥50 vs. <50) | 0.8841 (0.2265–3.4511) | 0.8592 | ||||
| BMI | 1.1273 (1.0306–1.2331) | 0.0089 | 1.1265 (1.0299–1.2320) | 0.0092 | 1.1032 (0.9948–1.2234) | 0.0628 |
| Tumor size (cm) | 0.9577 (0.744–1.2333) | 0.7379 | 0.9534 (0.7403–1.2279) | 0.7117 | 0.7697 (0.5383–1.1006) | 0.1514 |
| PLN or PALN (pos vs. neg) | 2.2967 (0.8143–6.4774) | 0.1160 | 2.2934 (0.8128–6.4714) | 0.1168 | 1.6624 (0.4415–6.2586) | 0.4524 |
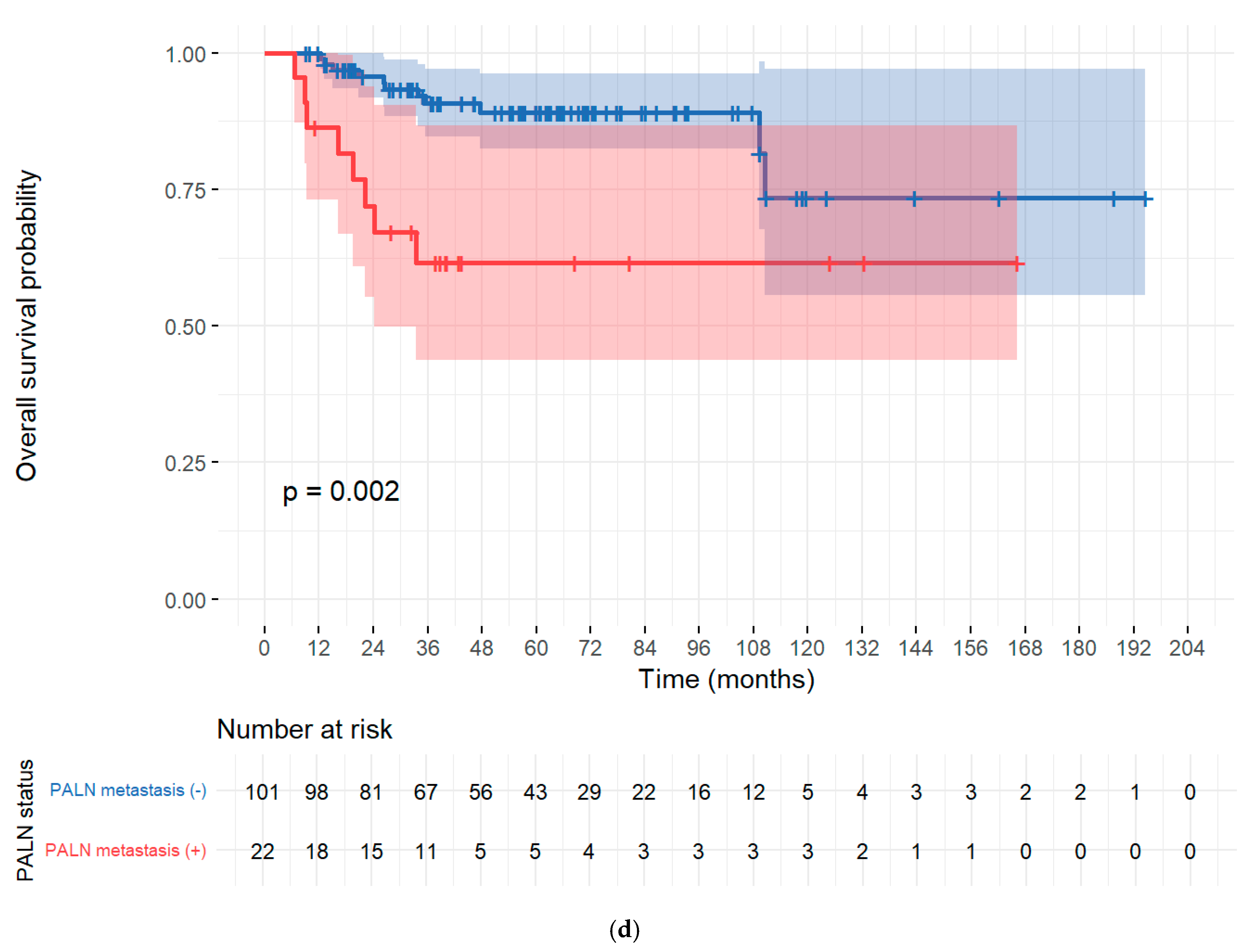
| PALN (pos vs. neg) | 3.5948 (1.6288–7.9339) | 0.0015 | 3.6127 (1.6376–7.9699) | 0.0015 | 3.7172 (1.3036–10.5994) | 0.0141 |
| SCC Ag | 1.0056 (0.9962–1.0152) | 0.2424 | 1.0058 (0.9963–1.0153) | 0.2320 | 1.0107 (1.0005–1.0211) | 0.0398 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parulekar, M.; Kim, M.K.; Noh, J.J.; Suh, D.H.; Kim, K.; Kim, Y.B.; No, J.H. Clinicopathological Factors Affecting Prognosis in Patients with Advanced Cervical Cancer Undergoing Concurrent Chemoradiation Therapy. Cancers 2025, 17, 3042. https://doi.org/10.3390/cancers17183042
Parulekar M, Kim MK, Noh JJ, Suh DH, Kim K, Kim YB, No JH. Clinicopathological Factors Affecting Prognosis in Patients with Advanced Cervical Cancer Undergoing Concurrent Chemoradiation Therapy. Cancers. 2025; 17(18):3042. https://doi.org/10.3390/cancers17183042
Chicago/Turabian StyleParulekar, Maitreyee, Min Kyung Kim, Joseph J. Noh, Dong Hoon Suh, Kidong Kim, Yong Beom Kim, and Jae Hong No. 2025. "Clinicopathological Factors Affecting Prognosis in Patients with Advanced Cervical Cancer Undergoing Concurrent Chemoradiation Therapy" Cancers 17, no. 18: 3042. https://doi.org/10.3390/cancers17183042
APA StyleParulekar, M., Kim, M. K., Noh, J. J., Suh, D. H., Kim, K., Kim, Y. B., & No, J. H. (2025). Clinicopathological Factors Affecting Prognosis in Patients with Advanced Cervical Cancer Undergoing Concurrent Chemoradiation Therapy. Cancers, 17(18), 3042. https://doi.org/10.3390/cancers17183042






