Safety and Efficacy of Transvaginal Natural Orifice Transluminal Endoscopic (vNOTES) Right Colectomy: A Systematic Review
Simple Summary
Abstract
1. Introduction
1.1. Rationale
1.2. Aim
2. Materials and Methods
2.1. Study Protocol
2.2. Search Strategy
2.3. Endpoints
2.4. Eligibility and Exclusion Criteria
2.5. Quality Assessment
2.6. Study Selection and Data Collection
2.7. Statistical Analysis
3. Results
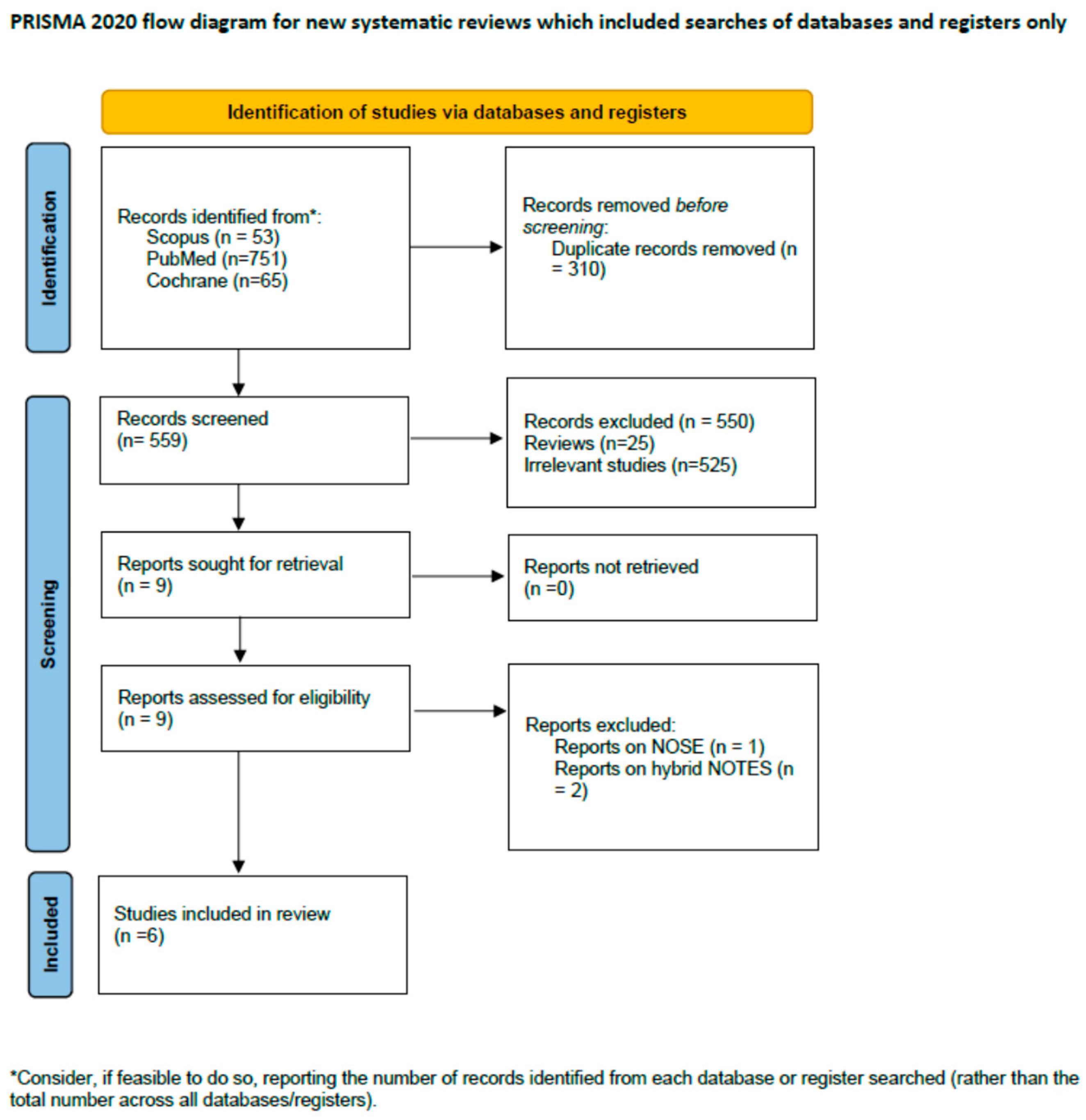
3.1. Search Results
3.2. Study Characteristics
3.3. Quality Assessment
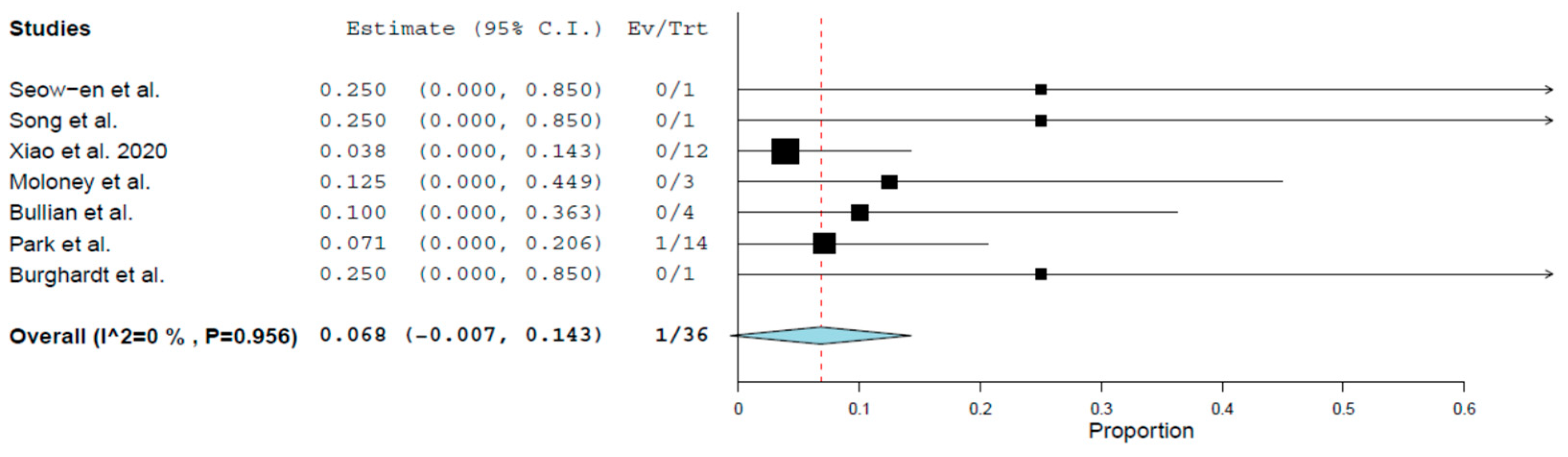
3.4. Primary Outcomes
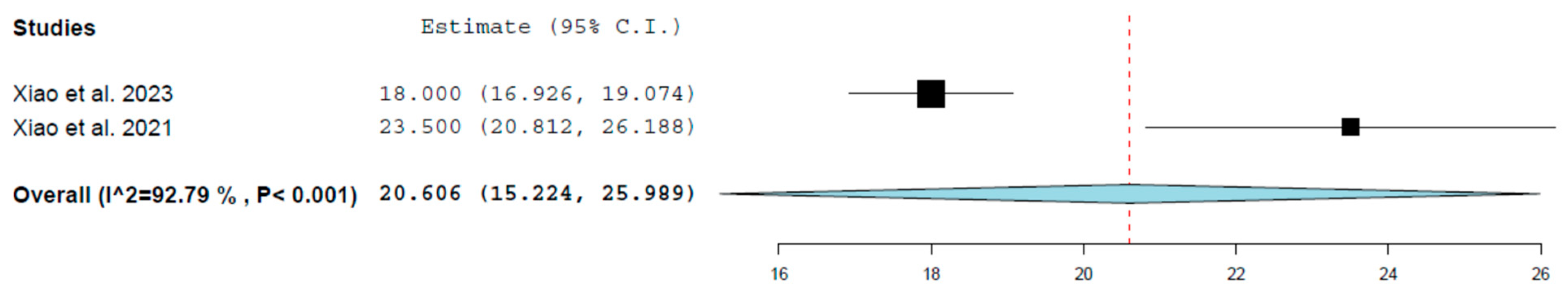
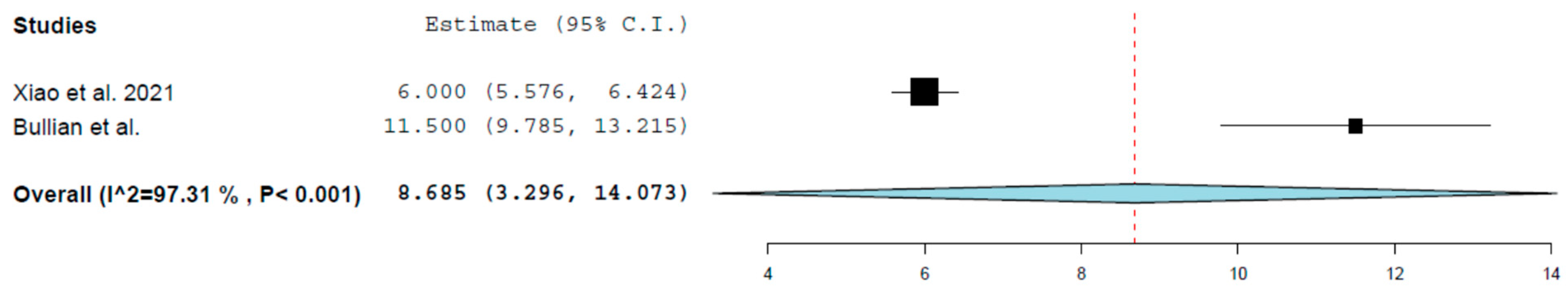
3.5. Secondary Outcomes
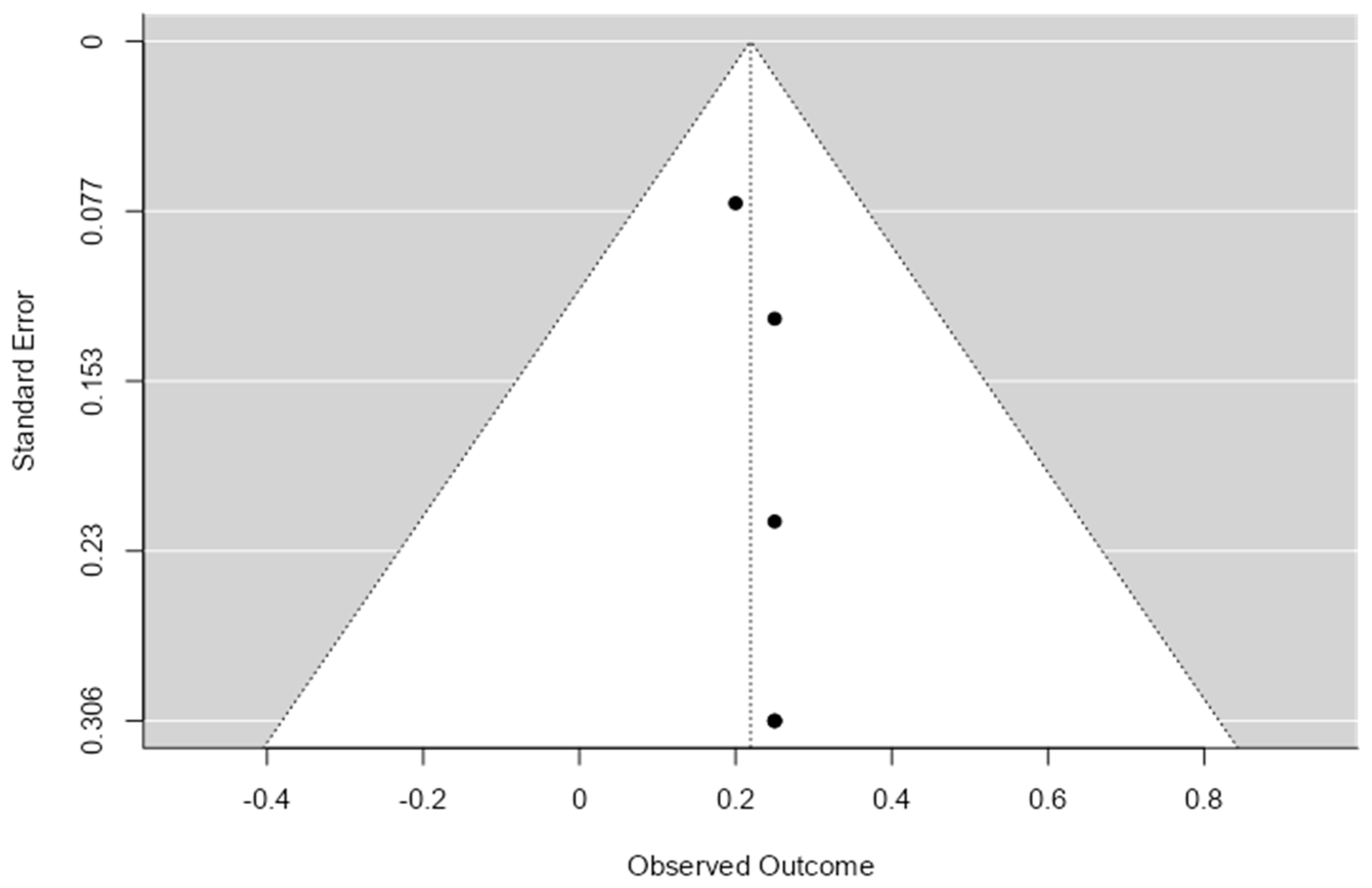
3.6. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| NOTES | Natural Orifice Translumenal Endoscopic Surgery |
| TaTME | Trans-Anal Total Mesorectal Excision |
| NOSE | Natural Orifice Specimen Extraction |
| vNOTES | Transvaginal NOTES |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| NHLBI | National Heart, Lung, And Blood Institute |
| SD | Standard Deviation |
| IQR | Interquartile Range |
| 95% CI | 95% Confidence Interval |
| RP | Raw Proportion |
| RE | Random Effects |
| FE | Fixed-Effect |
| CF-E | Continuous Fixed-Effect |
| CR-E | Continuous Random-Effect |
| BF-E | Binary Fixed-Effect |
| n/a | Not Applicable |
| BMI | Body Mass Index |
| ASA | American Society of Anesthesiologists |
| TNM | Tumor Node Metastasis |
Appendix A
| First Author | Previous Abdominal Operations | ASA | T | N | M | Tumour Location | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | Tis | 1 | 2 | 3 | 4 | 0 | 1 | 2 | 0 | Cecum/Ascending | Hepatic Flexure/ Transverse | Tumor Size (cm) | ||
| Seow-en et al. | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 3 | ||||
| Xiao et al. | n/a | n/a | n/a | n/a | n/a | n/a | ||||||||||
| Song et al. | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 2.5 (0) | |||
| Xiao et al. | n/a | 10 | 2 | 0 | 1 | 2 | 1 | 2 | 3 | 8 | 4 | 0 | 5 | n/a | n/a | 6.75 (1.5) |
| Bullian et al. | n/a | 1 | 1 | 2 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Burghardt et al. | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | n/a | |||||
| First Author | Bowel Preparation | Position | Pneumoperitoneum (mmHg) | Access | Laparoscopic/Robotic | Trocar | Anastomosis | Approach | Number of Surgeons | Access Closure | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdominal | Vaginal | ||||||||||
| Seow-en et al. | no | lithotomy & trendelenburg | 12 | wound protector & glove | lap | 1 | 4 | intracorporeal antiperistaltic stapled side-to-side | inferior to superior | direct suture | |
| Xiao et al. | n/a | lithotomy | 14 | Single Port Access System HTKD Medical™ | lap | 0 | 5 | intracorporeal stapled antiperistaltic side-to-side | caudal | n/a | n/a |
| Song et al. | mechanical & oral antibiotics | lithotomy & trendelenburg | n/a | StarPort™ | lap | 0 | 3 | extracorporeal stapled end-to-side | caudal | n/a | direct suture |
| Xiao et al. | n/a | lithotomy | 14 | Single Port Access System HTKD Medical™ | lap | 0 | 5 | intracorporeal stapled antiperistaltic side-to-side | caudal | n/a | n/a |
| Bullian et al. | n/a | n/a | n/a | n/a | lap | n/a | n/a | n/a | n/a | n/a | direct suture |
| Burghardt et al. | n/a | lithotomy | n/a | 12mm trocar | lap | 2 | 1 | intracorporeal stapled side-to-side | n/a | n/a | n/a |
| Seow-en et al. (2024) | Song et al. (2021) | Burghardt et al. (2008) | |
|---|---|---|---|
| Q1. Were the patient’s demographic characteristics clearly described? | YES | NO | NO |
| Q2. Was the patient’s history clearly described and presented as a timeline? | YES | YES | YES |
| Q3. Was the current clinical condition of the patient clearly described? | YES | YES | YES |
| Q4. Were diagnostic tests or assessment methods and the results clearly described? | YES | YES | YES |
| Q5. Was the intervention(s) or treatment procedure(s) clearly described? | YES | YES | YES |
| Q6. Was the post-intervention clinical condition clearly described? | YES | YES | YES |
| Q7. Were adverse events (harms) or unanticipated events identified and described? | YES | YES | YES |
| Q8. Does the case report provide takeaway lessons? | YES | YES | YES |
| Xiao et al. (2023) | Xiao et al. (2020) | Bullian et al. (2014) | |
|---|---|---|---|
| 1. Was the research question or objective in this paper clearly stated? | YES | YES | YES |
| 2. Was the study population clearly specified and defined? | YES | YES | YES |
| 3. Was the participation rate of eligible people at least 50%? | YES | YES | YES |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | YES | YES | NO |
| 5. Was sample size justification, power description, or variance and effect estimates provided? | YES | YES | NO |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | YES | YES | YES |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | YES | YES | YES |
| 8. For exposures that can vary in amount or level, did the study examine different levels of exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? | YES | YES | YES |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | YES | YES | YES |
| 10. Was the exposure(s) assessed more than once over time? | NO | NO | NO |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | YES | YES | YES |
| 12. Were the outcome assessors blinded to the exposure status of participants? | YES | YES | NO |
| 13. Was loss to follow-up after baseline 20% or less? | NO | NO | NO |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | YES | YES | YES |
| Study | Study Type | Total Items Assessed | Items Answered “Yes” | Quality Score (%) |
|---|---|---|---|---|
| Seow-en et al. (2024) | Case Report | 8 | 8 | 100 |
| Song et al. (2021) | Case Report | 8 | 7 | 87.5 |
| Burghardt et al. (2008) | Case Report | 8 | 7 | 87.5 |
| Xiao et al. (2020) | Cohort | 14 | 12 | 85.7 |
| Xiao et al. (2023) | Cohort | 14 | 12 | 85.7 |
| Bullian et al. (2014) | Cohort | 14 | 11 | 78.6 |




References
- Kim, H.S.; Noh, G.T.; Chung, S.S.; Lee, R.A. Long-Term Oncological Outcomes of Robotic versus Laparoscopic Approaches for Right Colon Cancer: A Systematic Review and Meta-Analysis. Tech. Coloproctol. 2023, 27, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Kossenas, K.; Moutzouri, O.; Georgopoulos, F. Comparison of Short-Term Outcomes of Robotic versus Laparoscopic Right Colectomy for Patients ≥ 65 Years of Age: A Systematic Review and Meta-Analysis of Prospective Studies. J. Robot. Surg. 2025, 19, 60. [Google Scholar] [CrossRef]
- Rausa, E.; Bianco, F.; Kelly, M.E.; Aiolfi, A.; Petrelli, F.; Bonitta, G.; Sgroi, G. Systemic Review and Network Meta-Analysis Comparing Minimal Surgical Techniques for Rectal Cancer: Quality of Total Mesorectum Excision, Pathological, Surgical, and Oncological Outcomes. J. Surg. Oncol. 2019, 119, 987–998. [Google Scholar] [CrossRef]
- Mostafa, O.E.S.; Zaman, S.; Beedham, W.; Kakaniaris, G.; Husain, N.; Kumar, L.; Akingboye, A.; Waterland, P. Systematic Review and Meta-Analysis Comparing Outcomes of Multi-Port versus Single-Incision Laparoscopic Surgery (SILS) in Hartmann’s Reversal. Int. J. Colorectal Dis. 2024, 39, 190. [Google Scholar] [CrossRef] [PubMed]
- Brucchi, F.; Montroni, I.; Cirocchi, R.; Taffurelli, G.; Vitellaro, M.; Mascianà, G.; Sandri, G.B.L.; Dionigi, G.; Lauricella, S. A Systematic Review of the Da Vinci® Single-Port System (DVSP) in the Context of Colorectal Surgery. Int. J. Colorectal Dis. 2025, 40, 83. [Google Scholar] [CrossRef]
- Pompeu, B.F.; Guerra, L.S.; de Guedes, L.S.S.P.; Brunini, J.H.; Delgado, L.M.; Poli de Figueiredo, S.M.; Formiga, F.B. Natural Orifice Extraction Techniques (Natural Orifice Specimen Extraction and Natural Orifice Transluminal Endoscopic Surgery) for Left-Sided Colorectal Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Laparoendosc. Adv. Surg. Tech. A 2025, 35, 379–387. [Google Scholar] [CrossRef]
- Lee, G.C.; Sylla, P. Shifting Paradigms in Minimally Invasive Surgery: Applications of Transanal Natural Orifice Transluminal Endoscopic Surgery in Colorectal Surgery. Clin. Colon. Rectal Surg. 2015, 28, 181–193. [Google Scholar] [CrossRef]
- Fuchs, K.H.; Meining, A.; Von Renteln, D.; Fernandez-Esparrach, G.; Breithaupt, W.; Zornig, C.; Lacy, A. Euro-NOTES Status Paper: From the Concept to Clinical Practice. Surg. Endosc. 2013, 27, 1456–1467. [Google Scholar] [CrossRef]
- Bulian, D.R.; Runkel, N.; Burghardt, J.; Lamade, W.; Butters, M.; Utech, M.; Thon, K.P.; Lefering, R.; Heiss, M.M.; Buhr, H.J.; et al. Natural Orifice Transluminal Endoscopic Surgery (NOTES) for Colon Resections—Analysis of the First 139 Patients of the German NOTES Registry (GNR). Int. J. Colorectal Dis. 2014, 29, 853–861. [Google Scholar] [CrossRef]
- Marks, J.H.; Montenegro, G.A.; Salem, J.F.; Shields, M.V.; Marks, G.J. Transanal TATA/TME: A Case-Matched Study of TaTME versus Laparoscopic TME Surgery for Rectal Cancer. Tech. Coloproctol. 2016, 20, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Stipa, F.; Burza, A.; Curinga, R.; Santini, E.; Delle Site, P.; Avantifiori, R.; Picchio, M. Laparoscopic Colon and Rectal Resections with Intracorporeal Anastomosis and Trans-Vaginal Specimen Extraction for Colorectal Cancer. A Case Series and Systematic Literature Review. Int. J. Colorectal Dis. 2015, 30, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Efetov, S.K.; Cao, Y.; Panova, P.D.; Khlusov, D.I.; Shulutko, A.M. Reduced-Port Laparoscopic Right Colonic Resection with D3 Lymph Node Dissection and Transvaginal Specimen Extraction (NOSES VIIIa) for Right Colon Cancer: Clinical Features. Tech. Coloproctol. 2024, 29, 34. [Google Scholar] [CrossRef] [PubMed]
- Moloney, J.M.; Gan, P.S.L. Hybrid Transvaginal NOTES and Mini-Laparoscopic Colectomy: Benefit Through Synergy. JSLS 2016, 20, e2016.00062. [Google Scholar] [CrossRef]
- Park, J.S.; Choi, G.S.; Lim, K.H.; Jang, Y.S.; Kim, H.J.; Park, S.Y.; Jun, S.H. Clinical Outcome of Laparoscopic Right Hemicolectomy with Transvaginal Resection, Anastomosis, and Retrieval of Specimen. Dis. Colon. Rectum 2010, 53, 1473–1479. [Google Scholar] [CrossRef]
- Xiao, Y.; Lin, C.; Lu, J.Y.; Xu, L.; Hou, W.Y.; Sun, R.; Chang, G.J.; Zhang, J.J. Short-Term Outcomes of Pure Transvaginal Laparoscopic Right Colectomy: A Novel Surgery Approach Based on an Idea, Development, Exploration, Assessment, Long-Term Framework Stage IIa Study. J. Surg. Oncol. 2021, 123 (Suppl. 1), S36–S42. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.5 (Updated August 2024); Cochrane: London, UK, 2024; Available online: www.cochrane.org/handbook (accessed on 16 August 2025).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Sun, Z.; Sun, R.; Hou, W.; Xu, L.; Lu, J. Safety and Feasibility of Right Colectomy via a Transvaginal Approach: Early Experience from a Single Center. Zhonghua Wei Chang Wai Ke Za Zhi 2023, 26, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Burghardt, J.; Federlein, M.; Müller, V.; Benhidjeb, T.; Elling, D.; Gellert, K. Minimal Invasive Transvaginal Right Hemicolectomy: Report of the First Complex NOS (Natural Orifice Surgery) Bowels Operation Using a Hybrid Approach. Zentralbl Chir. 2008, 133, 574–576. [Google Scholar] [CrossRef]
- Song, Z.J.; Shi, Y.Q.; Jiang, Y.M.; Liu, K.; Li, Y.; Wang, C.G.; Zhao, R. Pure Transvaginal Natural Orifice Transluminal Endoscopic Surgery Right Hemicolectomy for Colon Cancer: A Case Report. World J. Clin. Cases 2021, 9, 1714–1719. [Google Scholar] [CrossRef]
- Seow-En, I.; Villanueva, M.E.; Seah, A.W.M.; Tan, E.J.K.W.; Ang, J.X. Vaginal Natural Orifice Transluminal Endoscopic Surgery (VNOTES) Right Hemicolectomy with Intracorporeal Anastomosis for Cecal Cancer. Tech. Coloproctol. 2024, 28, 108. [Google Scholar] [CrossRef]
- Gu, C.; Wu, Q.; Zhang, X.; Wei, M.; Wang, Z. Single-Incision versus Conventional Multiport Laparoscopic Surgery for Colorectal Cancer: A Meta-Analysis of Randomized Controlled Trials and Propensity-Score Matched Studies. Int. J. Colorectal Dis. 2021, 36, 1407–1419. [Google Scholar] [CrossRef] [PubMed]
- Li, C.B.; Hua, K.Q. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (VNOTES) in Gynecologic Surgeries: A Systematic Review. Asian J. Surg. 2020, 43, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Zhou, C.; Hua, Q.; Yang, L.; Zhao, W.; Xu, P. Impact of Operation Duration on Short-Term and Long-Term Prognosis in Patients Undergoing Radical Colorectal Surgery. J. Cancer 2022, 13, 1160. [Google Scholar] [CrossRef]
- Rausa, E.; Kelly, M.E.; Asti, E.; Aiolfi, A.; Bonitta, G.; Bonavina, L. Right Hemicolectomy: A Network Meta-Analysis Comparing Open, Laparoscopic-Assisted, Total Laparoscopic, and Robotic Approach. Surg. Endosc. 2019, 33, 1020–1032. [Google Scholar] [CrossRef]
- Liu, X.; Yang, W.H.; Jiao, Z.G.; Zhang, J.F.; Zhang, R. Systematic Review of Comparing Single-Incision versus Conventional Laparoscopic Right Hemicolectomy for Right Colon Cancer. World J. Surg. Oncol. 2019, 17, 179. [Google Scholar] [CrossRef]
- Migliore, M.; Giuffrida, M.C.; Marano, A.; Pellegrino, L.; Giraudo, G.; Barili, F.; Borghi, F. Robotic versus Laparoscopic Right Colectomy within a Systematic ERAS Protocol: A Propensity-Weighted Analysis. Updates Surg. 2021, 73, 1057–1064. [Google Scholar] [CrossRef]
- Solaini, L.; Bazzocchi, F.; Cavaliere, D.; Avanzolini, A.; Cucchetti, A.; Ercolani, G. Robotic versus Laparoscopic Right Colectomy: An Updated Systematic Review and Meta-Analysis. Surg. Endosc. 2018, 32, 1104–1110. [Google Scholar] [CrossRef]
- Apostolou, K.G.; Orfanos, S.V.; Papalois, A.E.; Felekouras, E.S.; Zografos, G.C.; Liakakos, T. Single-Incision Laparoscopic Right Hemi-Colectomy: A Systematic Review. Indian J. Surg. 2015, 77, 301–312. [Google Scholar] [CrossRef]
- Chang, J.H.E.; Xu, H.; Zhao, Y.; Wee, I.J.Y.; Ang, J.X.; Tan, E.K.W.; Seow-En, I. Transvaginal versus Transabdominal Specimen Extraction in Minimally Invasive Surgery: A Systematic Review and Meta-Analysis. Langenbecks Arch. Surg. 2024, 409, 172. [Google Scholar] [CrossRef] [PubMed]
- Tsai, P.L.; Chen, J.S.; Lin, C.H.; Hsu, T.C.; Lin, Y.W.; Chen, M.J. Abdominal Wound Length Influences the Postoperative Serum Level of Interleukin-6 and Recovery of Flatus Passage among Patients with Colorectal Cancer. Front. Surg. 2024, 11, 1400264. [Google Scholar] [CrossRef]
- Bartels, S.A.L.; Vlug, M.S.; Ubbink, D.T.; Bemelman, W.A. Quality of Life after Laparoscopic and Open Colorectal Surgery: A Systematic Review. World J. Gastroenterol. 2010, 16, 5035–5041. [Google Scholar] [CrossRef]
- Nakamura, T.; Takayama, Y.; Sato, T.; Watanabe, M. Risk Factors for Wound Infection After Laparoscopic Surgery for Colon Cancer. Surg. Laparosc. Endosc. Percutan Tech. 2020, 30, 45–48. [Google Scholar] [CrossRef]
- Leung, A.L.H.; Cheung, H.Y.S.; Fok, B.K.L.; Chung, C.C.C.; Li, M.K.W.; Tang, C.N. Prospective Randomized Trial of Hybrid NOTES Colectomy Versus Conventional Laparoscopic Colectomy for Left-Sided Colonic Tumors. World J. Surg. 2013, 37, 2678–2682. [Google Scholar] [CrossRef]
- He, J.; Hu, J.F.; Shao, S.X.; Yao, H.B.; Zhang, X.F.; Yang, G.G.; Shen, Z. The Comparison of Laparoscopic Colorectal Resection with Natural Orifice Specimen Extraction versus Mini-Laparotomy Specimen Extraction for Colorectal Tumours: A Systematic Review and Meta-Analysis of Short-Term Outcomes. J. Oncol. 2020, 2020, 6204264. [Google Scholar] [CrossRef]
- Kapurubandara, S.; Lowenstein, L.; Salvay, H.; Herijgers, A.; King, J.; Baekelandt, J. Consensus on Safe Implementation of Vaginal Natural Orifice Transluminal Endoscopic Surgery (VNOTES). Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 263, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.; Sodergren, M.; Noonan, D.; Darzi, A.; Yang, G.Z. The Natural Orifice Simulated Surgical Environment (NOSsE): Exploring the Challenges of NOTES without the Animal Model. J. Laparoendosc. Adv. Surg. Tech. A 2009, 19, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Gillen, S.; Gröne, J.; Knödgen, F.; Wolf, P.; Meyer, M.; Friess, H.; Buhr, H.-J.; Ritz, J.-P.; Feussner, H.; Lehmann, K.S. Educational and Training Aspects of New Surgical Techniques: Experience with the Endoscopic–Laparoscopic Interdisciplinary Training Entity (ELITE) Model in Training for a Natural Orifice Translumenal Endoscopic Surgery (NOTES) Approach to Appendectomy. Surg. Endosc. 2012, 26, 2376–2382. [Google Scholar] [CrossRef]
- Wang, C.J.; Go, J.; Huang, H.Y.; Wu, K.Y.; Huang, Y.T.; Liu, Y.C.; Weng, C.H. Learning Curve Analysis of Transvaginal Natural Orifice Transluminal Endoscopic Hysterectomy. BMC Surg. 2019, 19, 88. [Google Scholar] [CrossRef] [PubMed]
- Korzeniowski, P.; Barrow, A.; Sodergren, M.H.; Hald, N.; Bello, F. NOViSE: A Virtual Natural Orifice Transluminal Endoscopic Surgery Simulator. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 2303–2315. [Google Scholar] [CrossRef]
- Lau, S.Y.C.; Choy, K.T.; Yang, T.W.W.; Heriot, A.; Warrier, S.K.; Guest, G.D.; Kong, J.C. Defining the Learning Curve of Transanal Total Mesorectal Excision: A Systematic Review and Meta-Analysis. ANZ J. Surg. 2022, 92, 355–364. [Google Scholar] [CrossRef] [PubMed]

| First Author | Publication Date | Type of Study | Country | Single-/Multi-Center | Study Period | Number of Patients | BMI | Age | Follow Up (Months) |
|---|---|---|---|---|---|---|---|---|---|
| Seow-en et al. | 2024 | case report | Singapore | single | 2024 | 1 | 32 (0) | 59 (0) | 60 (0) |
| Xiao et al. | 2023 | retrospective | China | single | 2019–2022 | 30 | 22 (3.1) | n/a | n/a |
| Song et al. | 2021 | case report | China | single | 2021 | 1 | 18.4 (0) | 65 (0) | 1 (0) |
| Xiao et al. | 2021 | prospective | China | single | 2018–2020 | 12 | n/a | 70 (7.5) | 30 (0) |
| Bullian et al. | 2014 | prospective | Germany | multi | 2008–2013 | 4 | 26 (2.75) | 63.5 (5.5) | n/a |
| Burghardt et al. | 2008 | case report | Germany | single | 2008 | 1 | 22 (0) | 66 (0) | n/a |
| Model | Metric | Estimate | Lower Bound | Upper Bound | Std. Error | p-Value | Tau2 | Q | Het. p-Value | I2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary outcome | |||||||||||
| Overall Complications | BF-E | Proportion | 0.219 | 0.107 | 0.332 | 0.05 | <0.001 | 0 | 0.18 | 0.99 | 0 |
| Secondary outcome | |||||||||||
| Intraoperative Complications | BF-E | Proportion | 0.199 | 0.094 | 0.303 | 0.053 | <0.001 | 0 | 3.19 | 0.67 | 0 |
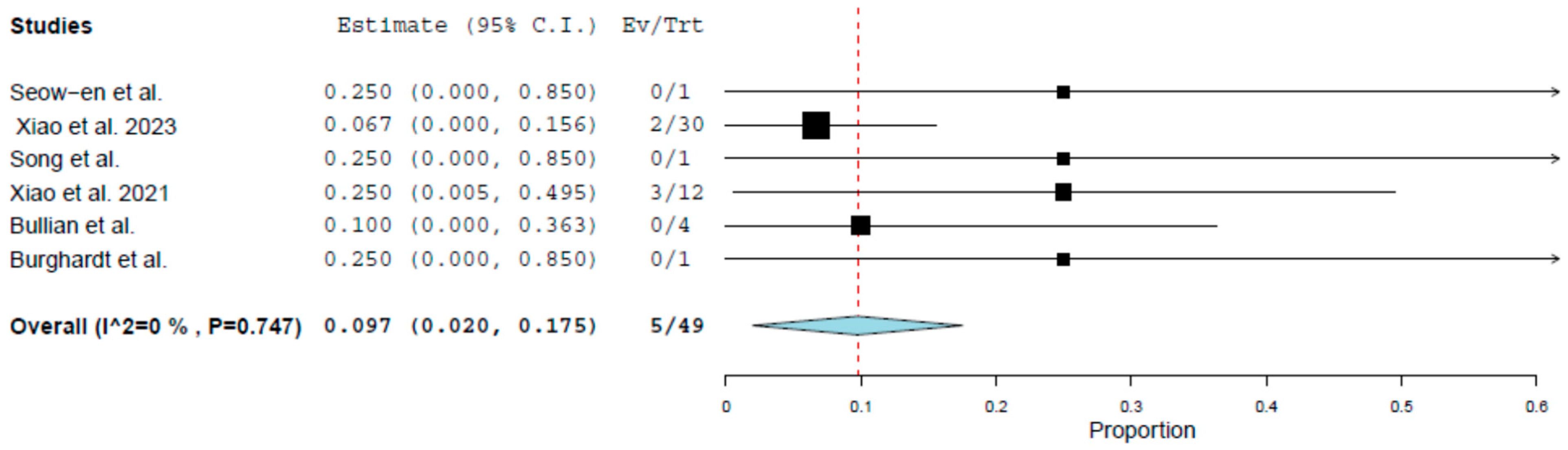
| Intraoperative Hemorrhage | BF-E | Proportion | 0.097 | 0.02 | 0.175 | 0.04 | 0.014 | 0 | 2.691 | 0.747 | 0 |
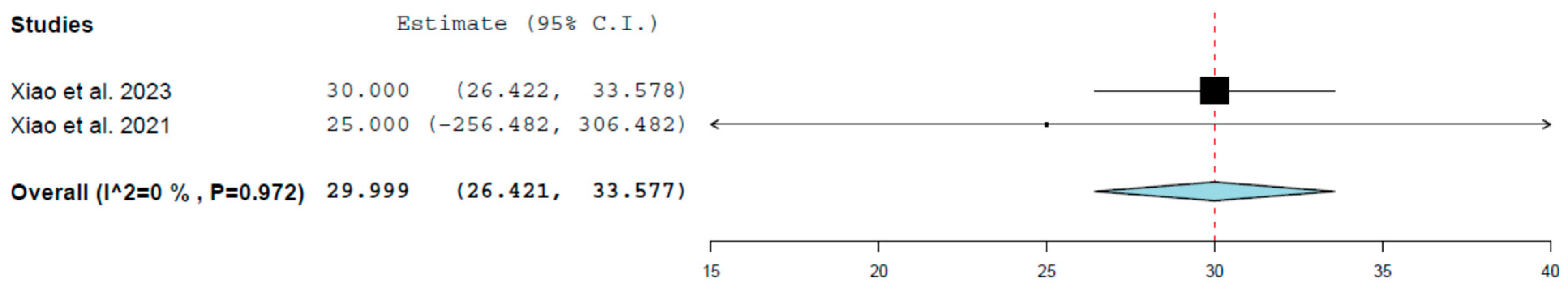
| Intraoperative Blood Loss (mL) | CF-E | Mean | 29.9 | 26.42 | 33.57 | 1.826 | <0.001 | 0 | 0.001 | 0.972 | 0 |
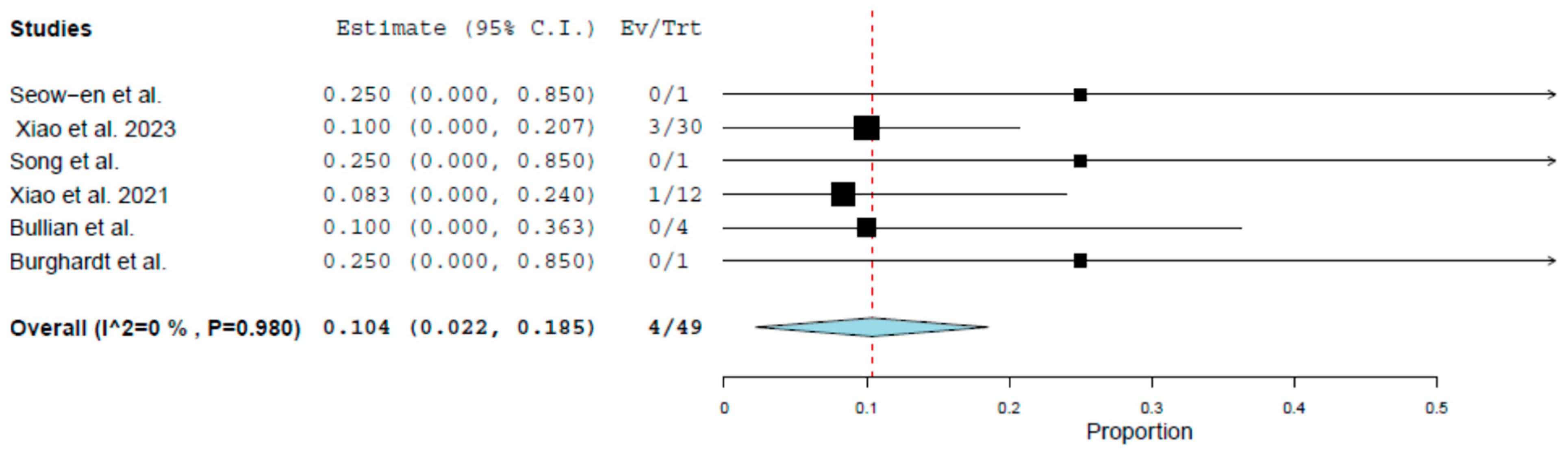
| Intraoperative Bladder Injury | BF-E | Proportion | 0.104 | 0.022 | 0.185 | 0.042 | 0.013 | 0 | 0.755 | 0.98 | 0 |
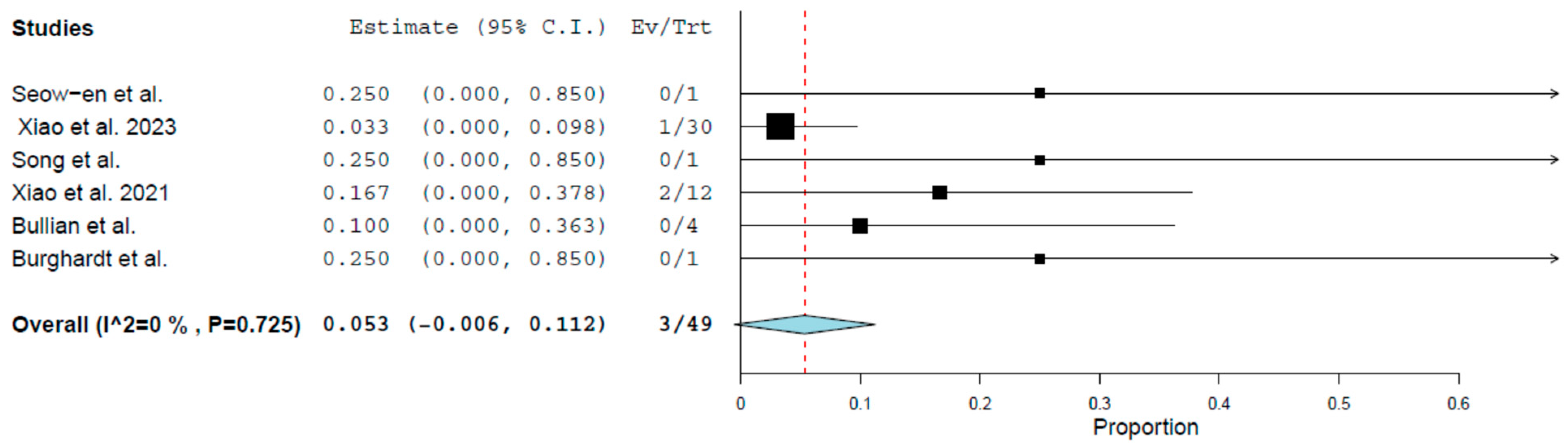
| Conversion | BF-E | Proportion | 0.053 | −0.006 | 0.112 | 0.03 | 0.076 | 0 | 2.841 | 0.725 | 0 |
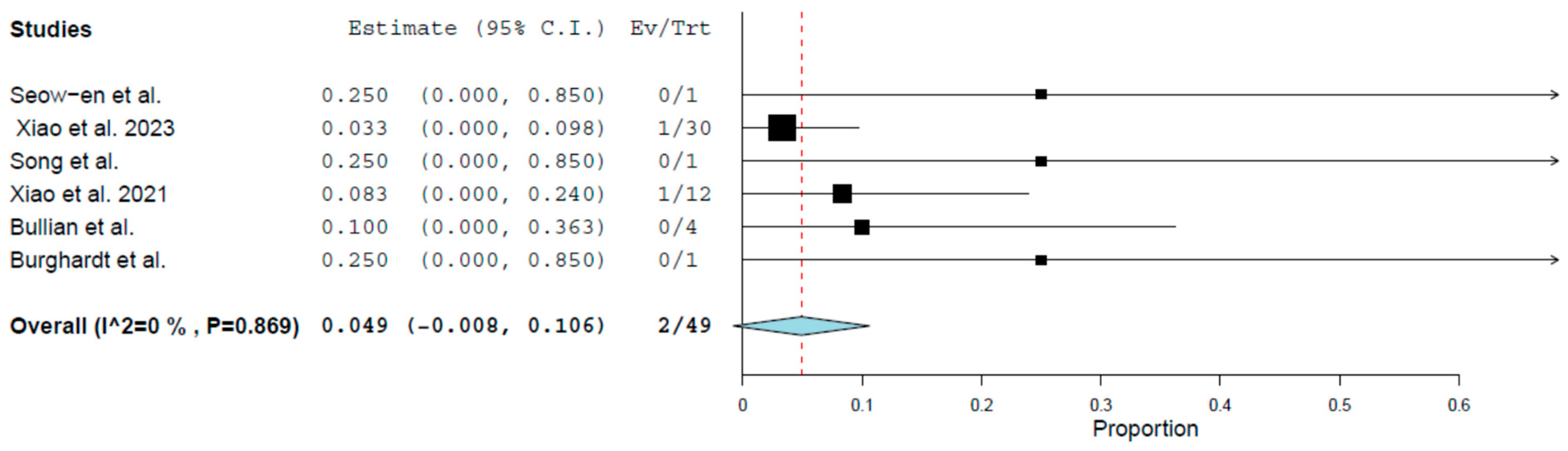
| Hematoma | BF-E | Proportion | 0.049 | −0.008 | 0.106 | 0.029 | 0.093 | 0 | 1.851 | 0.869 | 0 |
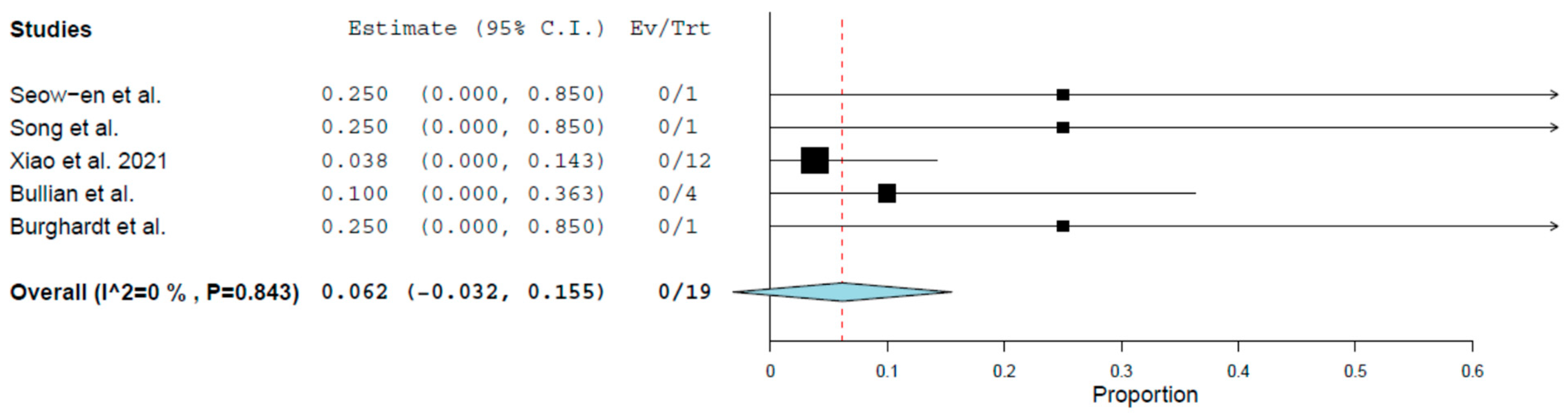
| Ileus | BF-E | Proportion | 0.062 | −0.032 | 0.155 | 0.048 | 0.196 | 0 | 1.406 | 0.843 | 0 |
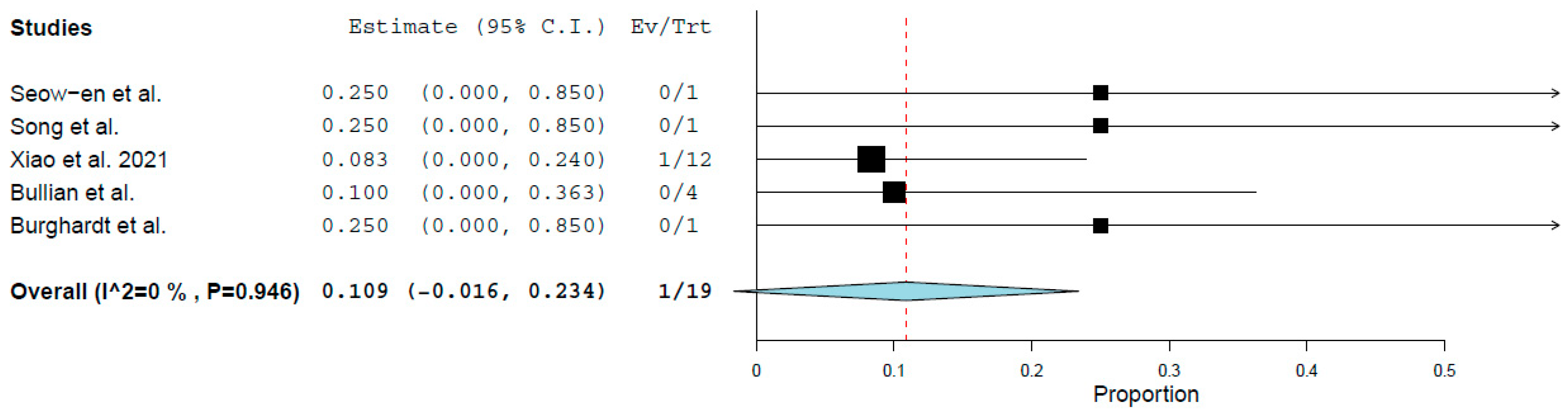
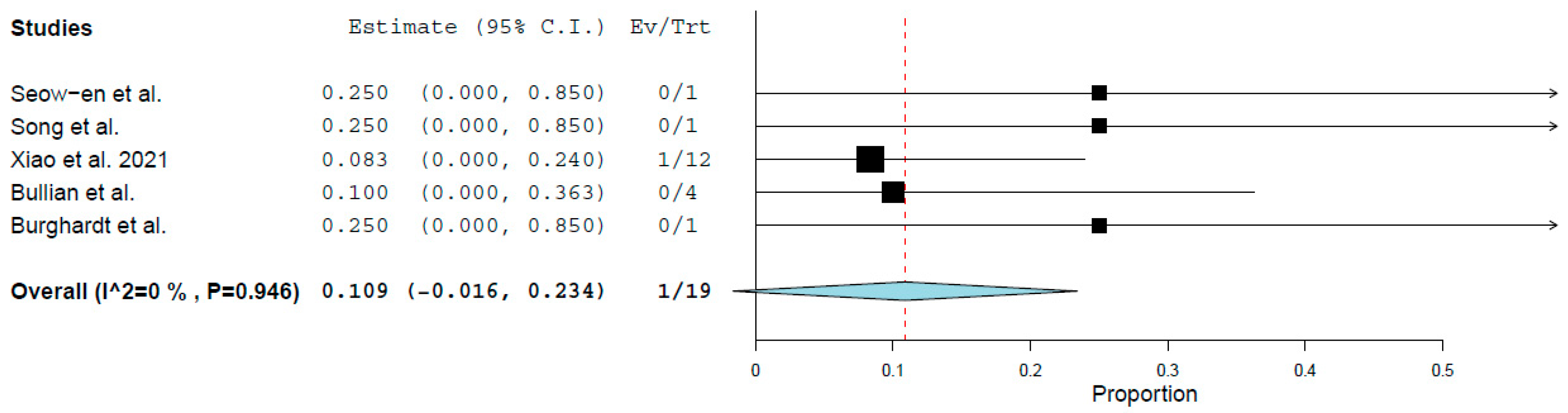
| Vaginal Infection | BF-E | Proportion | 0.109 | −0.016 | 0.234 | 0.064 | 0.088 | 0 | 0.744 | 0.946 | 0 |
| Bacteremia | BF-E | Proportion | 0.109 | −0.016 | 0.234 | 0.064 | 0.088 | 0 | 0.744 | 0.946 | 0 |
| Anastomotic Bleeding | BF-E | Proportion | 0.062 | −0.032 | 0.155 | 0.048 | 0.196 | 0 | 1.406 | 0.843 | 0 |
| Recurrence | BF-E | Proportion | 0.062 | −0.032 | 0.155 | 0.048 | 0.196 | 0 | 1.406 | 0.843 | 0 |
| Operation Duration (minutes) | CF-E | Mean | 176.42 | 170.76 | 182.08 | 2.88 | <0.001 | 0 | 1.348 | 0.510 | 0 |
| Length of Hospital Stay (days) | CR-E | Mean | 8.68 | 3.29 | 14.07 | 2.74 | 0.002 | 14.7 | 37.2 | <0.001 | 97.3 |
| Lymph Node Yield | CR-E | Mean | 20.6 | 15.2 | 25.9 | 2.74 | <0.001 | 14 | 13.8 | <0.001 | 92.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimopoulou, G.; Perivoliotis, K.; Lolis, E.; Symeonidis, D.; Tepetes, K.; Baloyiannis, I. Safety and Efficacy of Transvaginal Natural Orifice Transluminal Endoscopic (vNOTES) Right Colectomy: A Systematic Review. Cancers 2025, 17, 2699. https://doi.org/10.3390/cancers17162699
Dimopoulou G, Perivoliotis K, Lolis E, Symeonidis D, Tepetes K, Baloyiannis I. Safety and Efficacy of Transvaginal Natural Orifice Transluminal Endoscopic (vNOTES) Right Colectomy: A Systematic Review. Cancers. 2025; 17(16):2699. https://doi.org/10.3390/cancers17162699
Chicago/Turabian StyleDimopoulou, Georgia, Konstantinos Perivoliotis, Evangelos Lolis, Dimitrios Symeonidis, Konstantinos Tepetes, and Ioannis Baloyiannis. 2025. "Safety and Efficacy of Transvaginal Natural Orifice Transluminal Endoscopic (vNOTES) Right Colectomy: A Systematic Review" Cancers 17, no. 16: 2699. https://doi.org/10.3390/cancers17162699
APA StyleDimopoulou, G., Perivoliotis, K., Lolis, E., Symeonidis, D., Tepetes, K., & Baloyiannis, I. (2025). Safety and Efficacy of Transvaginal Natural Orifice Transluminal Endoscopic (vNOTES) Right Colectomy: A Systematic Review. Cancers, 17(16), 2699. https://doi.org/10.3390/cancers17162699






