Prognostic Factors in Colorectal Liver Metastases: An Exhaustive Review of the Literature and Future Prospectives
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
- Evidence-based treatment modalities for CRLM (surgery, chemotherapy, local therapies);
- Guideline recommendations for resectability and sequencing of therapies;
- Role of molecular markers (e.g., KRAS, NRAS, BRAF, MSI) in clinical decision-making;
- Use of decision-support tools or AI in managing CRLM;
- Barriers to standardized care in real-world settings.
- Consistency or conflict among guidelines;
- Gaps in integrating molecular and imaging data into treatment algorithms;
- Emerging evidence on the role of AI or predictive tools;
- Implications for future clinical pathways and research.
3. Results
3.1. Clinical Prognostic Factors
- Patient demographic characteristics
- b.
- Number and size of liver metastases
- c.
- Anatomic distribution (unilateral/bilateral)
- d.
- Extrahepatic metastases
- e.
- Characteristics of primary tumor
- f.
- Timing of onset (synchronous vs. metachronous)
- g.
- Resectability criteria and strategies to optimize surgical eligibility in CRLM
- Portal vein embolization (PVE): This is the standard method to induce hypertrophy of the future liver remnant. It achieves 10–20% FLR growth within 3–8 weeks. Morbidity is low (~2–5%), and the dropout rate for resection is about 20%. Two-stage hepatectomy (TSH) offers 35–45% 5-year survival rates when completed, though up to 20–30% of patients may experience progression and dropout between stages [128].
- Liver venous deprivation (LVD): This combines the embolization of the portal vein and the hepatic vein of the liver to be resected. This leads to more rapid and greater hypertrophy (~40–50% FLR increase within 2–4 weeks) compared to PVE alone. Early data suggest a comparable safety profile [129].
- Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): ALPPS, which induces rapid hypertrophy (~70–80% in 7–10 days), carries a 5–10% mortality risk but offers faster liver regeneration. Minimally invasive resections have reduced morbidity by up to 40%, improving recovery times and patient outcomes. It is indicated mainly in highly selected patients with insufficient FLR and good performance status [130].
3.2. Biological Prognostic Factors
- Pre- and postoperative CEA levels
- b.
- Inflammatory markers: Neutrophil–Lymphocyte Ratio and PLR The Platelet–Lymphocyte Ratio
- c.
- Nutritional and functional reserve: the role of albumin, sarcopenia and nutritional status
- d.
- Pharmacological sensibility
3.3. Molecular and Histopathological Prognostic Factors
- KRAS, NRAS and BRAF mutations
- b.
- MSI-H Status
- c.
- HER2/neu Alterations
- d.
- POLE, POLD1 and PD-L1
- e.
- Tumor budding, lymphovascular and perineural invasion
- f.
- Histological growth patterns of liver metastases (pushing vs. replacement patterns)
- Desmoplastic Growth Pattern (dHGP) characterized by a fibrous rim separating tumor cells from the liver parenchyma, often accompanied by dense immune cell infiltration. This pattern is associated with better OS and DFS. For instance, a study reported a median DFS of 22 months in patients with dHGP [207],
- Replacement Growth Pattern (rHGP): Tumor cells infiltrate and replace hepatocytes with minimal desmoplastic reaction and inflammatory cell infiltration. This pattern is associated with poorer prognosis, with a hazard ratio for OS of 2.15 compared to dHGP [208]. Patients with rHGP exhibit significantly poorer OS compared to those with pHGP. A study involving 217 patients reported a median OS of 22.8 months for rHGP, compared to 44.2 months for pHGP. Cox regression analysis indicated that the hazard ratio (HR) for death in rHGP patients was approximately 2.5 times higher than in pHGP patients (HR: 0.41, 95% CI: 0.22–0.75, p = 0.004). Regarding RFS, rHGP is also associated with worse outcomes. In a cohort of 110 patients undergoing liver resection for CRLM, the DFS rate was significantly lower in patients with rHGP compared to those with pHGP (20.2% vs. 40.5%, p = 0.05) [209].
3.4. Emerging Prognostic Factors from Precision Medicine
- Circulating tumor DNA (ctDNA): detection of minimal residual disease, early recurrence prediction
- b.
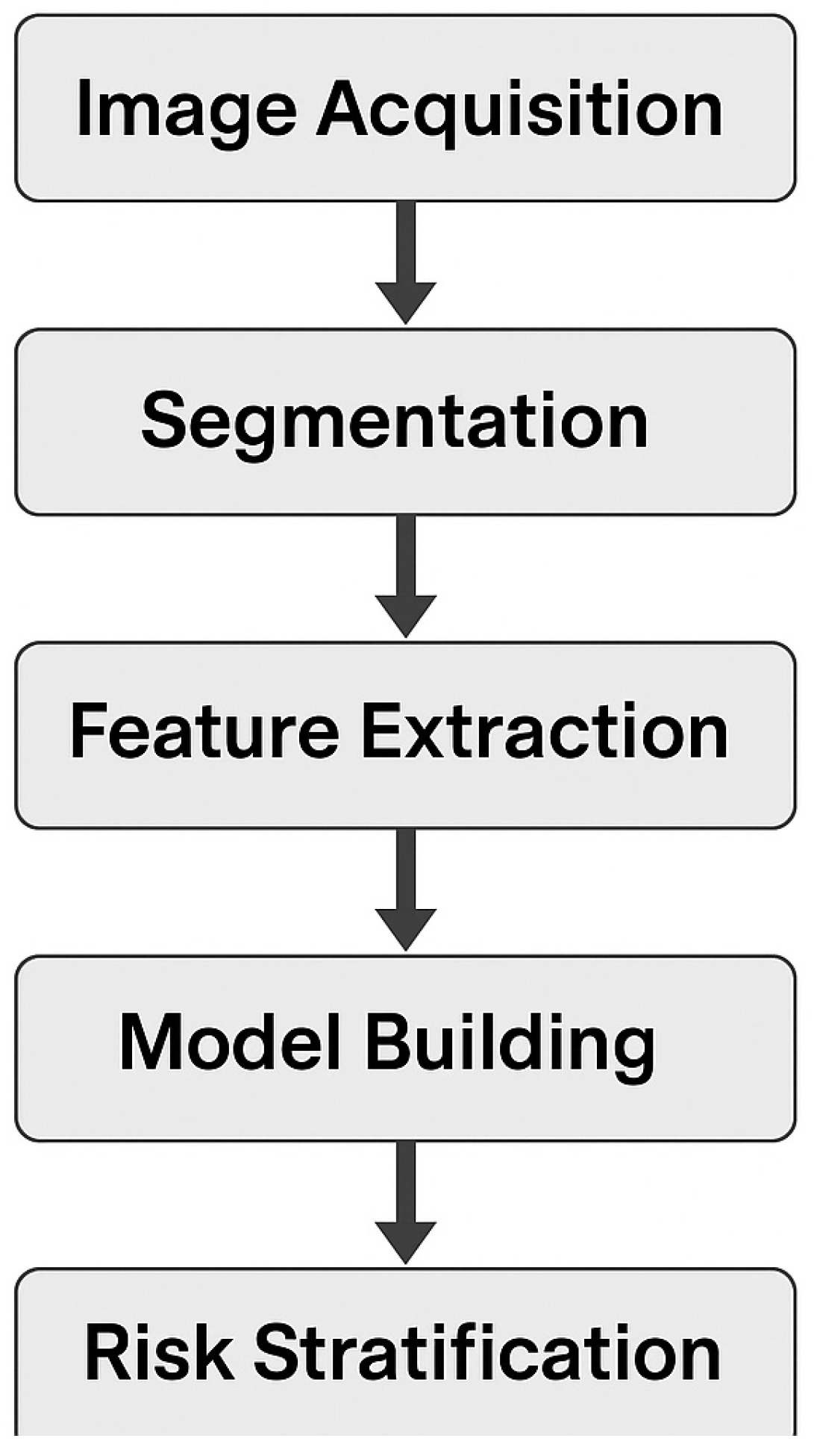
- Radiomics: role of quantitative imaging analysis in risk prediction
- c.
- Gut microbiome: influence on immune response and tumor progression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Colorectal Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/colorectal-cancer (accessed on 30 March 2025).
- Engstrand, J.; Nilsson, H.; Strömberg, C.; Jonas, E.; Freedman, J. Colorectal cancer liver metastases—A population-based study on incidence, management and survival. BMC Cancer 2018, 18, 78. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; Avisar, E.; Ariche, A.; Giachetti, S.; Azoulay, D.; Castaing, D.; Kunstlinger, F.; Levi, F.; Bismuth, F. Resection of non-resectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. J. Clin. Oncol. 2001, 19, 857–864. [Google Scholar] [CrossRef]
- Kanas, G.P.; Taylor, A.; Primrose, J.N.; Langeberg, W.J.; Kelsh, M.A.; Mowat, F.S.; Alexander, D.D.; Choti, M.A.; Poston, G. Survival after liver resection in metastatic colorectal cancer: Review and meta-analysis of prognostic factors. Clin. Epidemiol. 2012, 4, 283–301. [Google Scholar] [CrossRef] [PubMed]
- Shindoh, J.; Vauthey, J.N.; Zimmitti, G.; Curley, S.A.; Aloia, T.A.; Conrad, C. Strategies for patients with initially unresectable colorectal liver metastases: From hepatic resection to liver transplantation. Oncology 2013, 85, 111–121. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Cervantes, A.; Adam, R.; Sobrero, A.; Van Krieken, J.H.; Aderka, D.; Aguilar, E.A.; Bardelli, A.; Benson, A.; Bodoky, G.; et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 2016, 27, 1386–1422. [Google Scholar] [CrossRef]
- Reboux, N.; Jooste, V.; Goungounga, J.; Robaszkiewicz, M.; Nousbaum, J.B.; Bouvier, A.M. Incidence and Survival in Synchronous and Metachronous Liver Metastases From Colorectal Cancer. JAMA Netw. Open 2022, 5, e2236666. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lam, V.W.T.; Laurence, J.M.; Hollands, M.J.; Pleass, H.C.; Richardson, A.J. Defining resection criteria for colorectal liver metastases: An international expert consensus statement. HPB 2017, 19, 673–680. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef]
- Smith, J.J.; Ng, S.C.; Garcia-Aguilar, J. Sex disparities in the surgical treatment and outcomes of colorectal liver metastases: A comprehensive review. J. Surg. Oncol. 2023, 127, 567–575. [Google Scholar]
- Miller, K.; Green, J.; Patel, R. Postoperative outcomes in female versus male patients undergoing liver resection for colorectal metastases. Br. J. Surg. 2023, 110, 1123–1130. [Google Scholar]
- Jones, R.D.; Sutton, P.A.; Evans, J.P. The impact of sex on chemotherapy toxicity and efficacy in colorectal liver metastases: A systematic review. Eur. J. Cancer 2022, 160, 123–134. [Google Scholar]
- Taylor, C.; Lee, Y.J.; Ma, W. Influence of sex on tumor biology and survival in patients undergoing resection for colorectal liver metastases. Ann. Surg. Oncol. 2023, 30, 2550–2560. [Google Scholar]
- Williams, T.; Harrison, B.; Ahmed, S. Sex-based differences in response to targeted therapies for colorectal liver metastases: A meta-analysis. World J. Gastroenterol. 2023, 29, 2784–2799. [Google Scholar]
- Chen, X.Y.; Zhao, Y.; Wang, J. The role of estrogen in colorectal cancer: Implications for sex differences in treatment outcomes. Oncol. Lett. 2022, 24, 301–310. [Google Scholar]
- Kenis, C.; Decoster, L.; Van Puyvelde, K.; De Groof, I.; Foca, C.; Cornélis, F.; Verschaeve, V.; Bachmann, C.; Bron, D.; Luce, S.; et al. Performance of two geriatric screening tools in older patients with cancer. J. Clin. Oncol. 2014, 32, 19–26. [Google Scholar] [CrossRef]
- Booth, C.M.; Nanji, S.; Wei, X.; Mackillop, W.J. Management and outcome of colorectal cancer liver metastases in elderly patients: A population-based study. JAMA Oncol. 2015, 1, 1111–1119. [Google Scholar] [CrossRef]
- Jin, K.-M.; Wang, K.; Bao, Q.; Wang, H.-W.; Xing, B.-C. Liver resection for colorectal liver-limited metastases in elderly patients: A propensity score matching analysis. World J. Surg. Oncol. 2020, 18, 275. [Google Scholar] [CrossRef]
- Mann, C.D.; Neal, C.P.; Pattenden, C.J.; Metcalfe, M.S.; Garcea, G.; Dennison, A.R.; Berry, D.P. Major resection of hepatic colorectal liver metastases in elderly patients—An aggressive approach is justified. Eur. J. Surg. Oncol. 2008, 34, 428–432. [Google Scholar] [CrossRef]
- Rees, M.; Tekkis, P.P.; Welsh, F.K.; O’Rourke, T.; John, T.G. Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: A multifactorial model of 929 patients. Ann. Surg. 2008, 247, 125–135. [Google Scholar] [CrossRef]
- Nardo, B.; Serafini, S.; Ruggiero, M.; Grande, R.; Fugetto, F.; Zullo, A.; Novello, M.; Rizzuto, A.; Bonaiuto, E.; Vaccarisi, S.; et al. Liver resection for metastases from colorectal cancer in very elderly patients: New surgical horizons. Int. J. Surg. 2016, 33 (Suppl. 1), S135–S141. [Google Scholar] [CrossRef]
- Folprecht, G.; Seymour, M.T.; Saltz, L.; Douillard, J.Y.; Hecker, H.; Stephens, R.J.; Maughan, T.S.; Van Cutsem, E.; Rougier, P.; Mitry, E.; et al. Irinotecan/fluorouracil combination in first-line therapy of older and younger patients with metastatic colorectal cancer: Combined analysis of 2,691 patients in randomized controlled trials. J. Clin. Oncol. 2008, 26, 1443–1451. [Google Scholar] [CrossRef] [PubMed]
- van Amerongen, M.J.; Jenniskens, S.F.M.; van den Boezem, P.B.; Fütterer, J.J.; de Wilt, J.H.W. Radiofrequency ablation compared to surgical resection for curative treatment of patients with colorectal liver metastases - a meta-analysis. HPB 2017, 19, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Cervantes, A.; Adam, R.; Roselló, S.; Arnold, D.; Normanno, N.; Taïeb, J.; Seligmann, J.; De Baere, T.; Osterlund, P.; Yoshino, T.; et al. Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2023, 34, 10–32. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology: Colon Cancer. Version 3.2023. Available online: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf (accessed on 30 March 2025).
- Mohile, S.G.; Dale, W.; Somerfield, M.R.; Schonberg, M.A.; Boyd, C.M.; Burhenn, P.S.; Canin, B.; Cohen, H.J.; Holmes, H.M.; Hopkins, J.O.; et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J. Clin. Oncol. 2018, 36, 2326–2347. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists. ASA Physical Status Classification System. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-asa-physical-status-classification-system (accessed on 30 March 2025).
- Fretland, Å.A.; Dagenborg, V.J.; Bjørnelv, G.M.; Kazaryan, A.M.; Kristiansen, R.; Fagerland, M.W.; Hausken, J.; Tønnessen, T.I.; Abildgaard, A.; Barkhatov, L.; et al. Laparoscopic versus open resection for colorectal liver metastases: The OSLO-COMET randomised controlled trial. Ann. Surg. 2018, 267, 199–207. [Google Scholar] [CrossRef]
- Adam, R.; Kitano, Y. Multidisciplinary approach of liver metastases from colorectal cancer: Evolving role of surgery. J. Clin. Oncol. 2016, 34, 2357–2365. [Google Scholar]
- Aloia, T.A.; Vauthey, J.N. Conservation liver surgery for colorectal liver metastases. J. Gastrointest. Surg. 2011, 15, 379–389. [Google Scholar]
- De Baere, T.; Tselikas, L.; Depla, A.; Roux, C.; Varin, E.; Kobe, A.; Yevich, S.; Deschamps, F. Thermal ablation in the management of oligometastatic colorectal cancer. Int. J. Hyperth. 2022, 39, 627–632. [Google Scholar] [CrossRef]
- Vogl, T.J.; Zangos, S.; Balzer, J.O.; Thalhammer, A.; Mack, M.G. Transarterial chemoembolization in the treatment of liver metastases: Current status and future perspectives. Rofo 2010, 182, 396–405. [Google Scholar]
- European Society for Medical Oncology (ESMO). Metastatic colorectal cancer: ESMO Clinical Practice Guidelines. Ann. Oncol. 2022, 33, 802–820. [Google Scholar]
- Pawlik, T.M.; Abdalla, E.K.; Ishizawa, T. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann. Surg. 2005, 241, 715–722. [Google Scholar] [CrossRef]
- Cloyd, J.M.; Chun, Y.S.; Ikoma. Association of preoperative comorbid conditions with perioperative outcomes after hepatic resection for colorectal liver metastases. JAMA Surg. 2019, 154, 256–263. [Google Scholar]
- Michiel Zeeuw, J.; Wesdorp, N.J.; Ali, M.; Bakker, A.J.J.; Voigt, K.R.; Starmans, M.P.A.; Roor, J.; Kemna, R.; van Waesberghe, J.H.T.M.; van den Bergh, J.E.; et al. Prognostic value of total tumor volume in patients with colorectal liver metastases: A secondary analysis of the randomized CAIRO5 trial with external cohort validation. Eur. J. Cancer 2024, 207, 114185. [Google Scholar] [CrossRef] [PubMed]
- Folprecht, G.; Gruenberger, T.; Bechstein, W.O.; Raab, H.R.; Lordick, F.; Hartmann, J.T.; Lang, H.; Frilling, A.; Stoehlmacher, J.; Weitz, J.; et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: The CELIM randomised phase 2 trial. Lancet Oncol. 2010, 11, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Poultsides, G.A.; Schulick, R.D.; Pawlik, T.M. Hepatic resection for colorectal metastases: The impact of surgical margin status on outcome. HPB 2010, 12, 43–49. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gervais, D.A.; Arellano, R.S.; Hahn, P.F. Laparoscopic hepatic resection for colorectal liver metastases: A multi-institutional analysis. J. Vasc. Interv. Radiol. 2010, 21, 1241–1247. [Google Scholar] [CrossRef]
- Adam, R.; Miller, R.; Pitombo, M.; Wicherts, D.A.; de Haas, R.J.; Bitsakou, G.; Aloia, T. Two-stage hepatectomy approach for initially unresectable colorectal hepatic metastases. Surg. Oncol. Clin. N. Am. 2007, 16, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Schadde, E.; Schnitzbauer, A.A.; Tschuor, C.; Raptis, D.A.; Bechstein, W.O.; Clavien, P.A. Systematic review and meta-analysis of feasibility, safety, and efficacy of a novel procedure: Associating liver partition and portal vein ligation for staged hepatectomy. Ann. Surg. Oncol. 2015, 22, 3109–3120. [Google Scholar] [CrossRef] [PubMed]
- Łapiński, T.W.; Łapińska, M. Nutritional status in patients with liver cirrhosis. Clin. Exp. Hepatol. 2019, 5, 30–34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morris-Janzen, D.; Jatana, S.; Verhoeff, K.; Shapiro, A.M.J.; Bigam, D.L.; Dajani, K.; Anderson, B. Impact of Hypoalbuminemia on Outcomes Following Hepatic Resection: A NSQIP Retrospective Cohort Analysis of 26,394 Patients. Livers 2024, 4, 507–520. [Google Scholar] [CrossRef]
- Wagner, D.; Wienerroither, V.; Scherrer, M.; Thalhammer, M.; Faschinger, F.; Lederer, A.; Hau, H.M.; Sucher, R.; Kornprat, P. Value of sarcopenia in the resection of colorectal liver metastases-a systematic review and meta-analysis. Front. Oncol. 2023, 13, 1241561. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giakoustidis, A.; Papakonstantinou, M.; Chatzikomnitsa, P.; Gkaitatzi, A.D.; Bangeas, P.; Loufopoulos, P.D.; Louri, E.; Myriskou, A.; Moschos, I.; Antoniadis, D.; et al. The Effects of Sarcopenia on Overall Survival and Postoperative Complications of Patients Undergoing Hepatic Resection for Primary or Metastatic Liver Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 3869. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Haruki, K.; Shiba, H.; Horiuchi, T.; Sakamoto, T.; Gocho, T.; Fujiwara, Y.; Furukawa, K.; Misawa, T.; Yanaga, K. Impact of the C-reactive protein to albumin ratio on long-term outcomes after hepatic resection for colorectal liver metastases. Am. J. Surg. 2017, 214, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Gradel, K.O. Interpretations of the Role of Plasma Albumin in Prognostic Indices: A Literature Review. J. Clin. Med. 2023, 12, 6132. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kobayashi, T.; MTeruya; Kishiki, T.; Endo, D.; Takenaka, Y.; Miki, K.; Kobayashi, K.; Morita, K. Elevated C-Reactive Protein and Hypoalbuminemia Measured before Resection of Colorectal Liver Metastases Predict Postoperative Survival. Dig. Surg. 2010, 27, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Lodewick, T.M.; van Nijnatten, T.J.; van Dam, R.M.; van Mierlo, K.; Dello, S.A.; Neumann, U.P.; Olde Damink, S.W.; Dejong, C.H. Are sarcopenia, obesity and sarcopenic obesity predictive of outcome in patients with colorectal liver metastases? HPB 2015, 17, 438–446. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gupta, D.; Lis, C.G. Pretreatment serum albumin as a predictor of cancer survival: A systematic review of the epidemiological literature. Nutr. J. 2010, 9, 69. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fong, Y.; Fortner, J.; Sun, R.L.; Brennan, M.F.; Blumgart, L.H. Clinical score to predict recurrence after hepatic resection for metastatic colorectal cancer: Analysis of 1001 consecutive cases. Ann. Surg. 1999, 230, 309–318. [Google Scholar] [CrossRef]
- Kuhlmann, A.D.; Spies, C.; Schulte, E.; Jara, M.; von Haefen, C.; Mertens, M.; Süß, L.A.; Winkler, N.; Lachmann, G.; Lachmann, C. Preoperative hypoalbuminaemia in liver surgery: An observational study at a university medical centre. BMJ Open 2023, 13, e068405. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meriggi, F.; Bertocchi, P.; Zaniboni, A. Management of potentially resectable colorectal cancer liver metastases. World J. Gastrointest. Surg. 2013, 5, 138–145. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brouquet, A.; Abdalla, E.K.; Kopetz, S. High survival rate after two-stage resection of advanced colorectal liver metastases: Response-based selection and complete resection define outcome. J. Clin. Oncol. 2011, 29, 1083–1090. [Google Scholar] [CrossRef] [PubMed]
- Shindoh, J.; Vauthey, J.N.; Zimmitti, G.; Curley, S.A.; Huang, S.Y.; Mahvash, A.; Gupta, S.; Wallace, M.J.; Aloia, T.A. Analysis of the efficacy of portal vein embolization for patients with extensive liver malignancy and very low future liver remnant volume, including a comparison with the associating liver partition with portal vein ligation for staged hepatectomy approach. J. Am. Coll. Surg. 2013, 217, 126–133. [Google Scholar] [CrossRef]
- Glinka, M.; Bachellier, P.; Farges, O.; de Santibañes, E.; de Santibañes, M. The role of associating liver partition and portal vein ligation for staged hepatectomy in the management of patients with colorectal liver metastasis. Hepatobiliary Surg. Nutr. 2019, 8, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Nasti, G.; Piccirillo, M.C.; Izzo, F.; Ottaiano, A.; Albino, V.; Delrio, P.; Romano, C.; Giordano, P.; Lastoria, S.; Caracò, C.; et al. Neoadjuvant FOLFIRI+bevacizumab in patients with resectable liver metastases from colorectal cancer: A phase 2 trial. Br. J. Cancer 2013, 108, 1566–1570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, Y.; Zheng, Y.; Wu, J.; Ye, R.; Jia, H.; Zhou, Z.; Chen, W.; Xu, L.; Zhang, Y.; Zheng, M. Neoadjuvant chemotherapy combined with bevacizumab for resectable colorectal liver metastasis with risk factors for recurrence: A multicenter real-world study. Ther. Adv. Med. Oncol. 2025, 17, 17588359251328457. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, Y.C.; Huang, C.W.; Li, C.C.; Chang, T.K.; Su, W.C.; Chen, P.J.; Yeh, Y.S.; Chang, Y.T.; Tsai, H.L.; Shih, M.P.; et al. Efficacy of transarterial chemoembolization with drug-eluting beads combined with systemic chemotherapy and targeted therapy in colorectal cancer liver metastasis. World J. Surg. Oncol. 2023, 21, 378. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- van Hazel, G.A.; Heinemann, V.; Sharma, N.K.; Findlay, M.P.; Ricke, J.; Peeters, M.; Perez, D.; Robinson, B.A.; Strickland, A.H.; Ferguson, T.; et al. SIRFLOX: Randomized Phase III Trial Comparing First-Line mFOLFOX6 (Plus or Minus Bevacizumab) Versus mFOLFOX6 (Plus or Minus Bevacizumab) Plus Selective Internal Radiation Therapy in Patients With Metastatic Colorectal Cancer. J. Clin. Oncol. 2016, 34, 1723–1731, Erratum in J. Clin. Oncol. 2016, 34, 4059. https://doi.org/10.1200/JCO.2016.70.8982. [Google Scholar] [CrossRef] [PubMed]
- Nordlinger, B.; Sorbye, H.; Glimelius, B.; Poston, G.J.; Schlag, P.M.; Rougier, P.; Bechstein, W.O.; Primrose, J.N.; Walpole, E.T.; Finch-Jones, M.; et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): A randomised controlled trial. Lancet 2008, 371, 1007–1016. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cucchetti, A.; Ercolani, G.; Cescon, M.; Di Gioia, P.; Peri, E.; Brandi, G.; Pellegrini, S.; Pinna, A.D. Safety of hepatic resection for colorectal metastases in the era of neo-adjuvant chemotherapy. Langenbecks Arch. Surg. 2012, 397, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Tönnies, S.; Tönnies, M.; Kollmeier, J.; Bauer, T.T.; Förster, G.J.; Kaiser, D.; Wernecke, K.D.; Pfannschmidt, J. Impact of preoperative 18F-FDG PET/CT on survival of resected mono-metastatic non-small cell lung cancer. Lung Cancer 2016, 93, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Pfannschmidt, J.; Klode, J.; Muley, T.; Dienemann, H.; Hoffmann, H. Nodal involvement at the time of pulmonary metastasectomy: Experiences in 245 patients. Ann. Thorac. Surg. 2006, 81, 448–454. [Google Scholar] [CrossRef]
- Pfannschmidt, J.; Bischoff, M.; Muley, T. Diagnosis of pulmonary metastases with helical CT: The effect of imaging techniques. Thorac. Cardiovasc. Surg. 2008, 56, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Tatsuta, K.; Sakata, M.; Kojima, T. Updated insights into the impact of adjuvant chemotherapy on recurrence and survival after curative resection of liver or lung metastases in colorectal cancer: A rapid review and meta-analysis. World J. Surg. Oncol. 2025, 23, 56. [Google Scholar] [CrossRef]
- Reece, M.; Saluja, H.; Hollington, P.; Karapetis, C.S.; Vatandoust, S.; Young, G.P.; Symonds, E.L. The Use of Circulating Tumor DNA to Monitor and Predict Response to Treatment in Colorectal Cancer. Front. Genet. 2019, 10, 1118. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Colon Cancer. Version 2.2024. Available online: https://www.nccn.org/guidelines/guidelines-detail?id=1428 (accessed on 30 March 2025).
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Rectal Cancer. Version 2.2024. Available online: https://www.nccn.org/guidelines/guidelines-detail?id=1461 (accessed on 30 March 2025).
- Verwaal, V.J.; Boot, H.; Aleman, B.M.P.; van Tinteren, H.; Zoetmulder, F.A.N. Recurrences after peritoneal carcinomatosis of colorectal origin treated by cytoreduction and hyperthermic intraperitoneal chemotherapy: Location, treatment, and outcome. Ann. Surg. Oncol. 2004, 11, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Kianmanesh, R.; Scaringi, S.; Sabate, J.M.; Castel, B.; Pons-Kerjean, N.; Coffin, B.; Hay, J.M.; Flamant, Y.; Msika, S. Iterative cytoreductive surgery associated with hyperthermic intraperitoneal chemotherapy for treatment of peritoneal carcinomatosis of colorectal origin with or without liver metastases. Ann. Surg. 2007, 245, 597–603. [Google Scholar] [CrossRef]
- Elias, D.; Gilly, F.; Boutitie, F.; Quenet, F.; Bereder, J.M.; Mansvelt, B.; Lorimier, G.; Dube, P.; Glehen, O. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: Retrospective analysis of 523 patients from a multicentric French study. J. Clin. Oncol. 2010, 28, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Quenet, F.; Goéré, D.; Mehta, S.S.; Roca, L.; Dumont, F.; Hessissen, M.; Saint-Aubert, B.; Elias, D. Results of two bi-institutional prospective studies using intraperitoneal oxaliplatin with or without irinotecan during HIPEC after cytoreductive surgery for colorectal carcinomatosis. Ann. Surg. 2011, 254, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Franko, J.; Shi, Q.; Goldman, C.D.; Pockaj, B.A.; Nelson, G.D.; Goldberg, R.M.; Pitot, H.C.; Grothey, A.; Alberts, S.R. Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy: A pooled analysis of North Central Cancer Treatment Group phase III trials N9741 and N9841. J. Clin. Oncol. 2012, 30, 263–267. [Google Scholar] [CrossRef]
- Sugarbaker, P.H. Surgical management of peritoneal carcinomatosis: Long-term results of a prospective study in 51 patients. Ann. Surg. 1995, 221, 29–36. [Google Scholar] [CrossRef]
- Sprave, T.; Verma, V.; Förster, R.; Schlampp, I.; Bruckner, T.; Bostel, T.; Welte, S.E.; Tonndorf-Martini, E.; Nicolay, N.H.; Debus, J.; et al. Randomized phase II trial evaluating pain response in patients with spinal metastases following stereotactic body radiotherapy versus three-dimensional conformal radiotherapy. Radiother. Oncol. 2018, 128, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Chimutengwende-Gordon, M.; Coomber, R.; Peat, F.; Tarazi, N.; Chou, D.; Carrothers, A. The Harrington plus reconstruction for pelvic and acetabular metastases. J. Bone Oncol. 2022, 33, 100414. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mirels, H. The classic: Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin. Orthop. Relat. Res. 2003, 415, S4–S13. [Google Scholar] [CrossRef]
- Van Poznak, C.; Somerfield, M.R.; Barlow, W.E.; Biermann, J.S.; Bosserman, L.D.; Clemons, M.J.; Dhesy-Thind, S.K.; Dillmon, M.S.; Eisen, A.; Frank, E.S.; et al. Role of Bone-Modifying Agents in Metastatic Breast Cancer: An American Society of Clinical Oncology-Cancer Care Ontario Focused Guideline Update. J. Clin. Oncol. 2017, 35, 3978–3986. [Google Scholar] [CrossRef] [PubMed]
- Van der Velden, J.M.; Versteeg, A.L.; van der Linden, Y.M. Efficacy and safety of stereotactic body radiation therapy for spinal metastases: A systematic review. Radiother. Oncol. 2021, 160, 274–283. [Google Scholar]
- Coleman, R.E.; Lipton, A.; Roodman, G.D.; Guise, T.A.; Boyce, B.F.; Brufsky, A.M.; Clézardin, P.; Croucher, P.I.; Gralow, J.R.; Hadji, P.; et al. Metastasis and bone loss: Advancing treatment and prevention. Cancer Treat. Rev. 2010, 36, 615–620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sperduto, P.W.; Chao, S.T.; Sneed, P.K.; Luo, X.; Suh, J.; Roberge, D.; Bhatt, A.; Jensen, A.W.; Brown, P.D.; Shih, H.; et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: A multi-institutional analysis of 4,259 patients. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.; Soffietti, R.; Abacioglu, U.; Villà, S.; Fauchon, F.; Baumert, B.G.; Fariselli, L.; Tzuk-Shina, T.; Kortmann, R.D.; Carrie, C.; et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: Results of the EORTC 22952-26001 study. J. Clin. Oncol. 2011, 29, 134–141. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aoyama, H.; Shirato, H.; Tago, M.; Nakagawa, K.; Toyoda, T.; Hatano, K.; Kenjyo, M.; Oya, N.; Hirota, S.; Shioura, H.; et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: A randomized controlled trial. JAMA 2006, 295, 2483–2491. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Jaeckle, K.; Ballman, K.V.; Farace, E.; Cerhan, J.H.; Anderson, S.K.; Carrero, X.W.; Barker, F.G., 2nd; Deming, R.; Burri, S.H.; et al. Effect of Radiosurgery Alone vs Radiosurgery with Whole Brain Radiation Therapy on Cognitive Function in Patients With 1 to 3 Brain Metastases: A Randomized Clinical Trial. JAMA 2016, 316, 401–409, Erratum in JAMA 2018, 320, 510. https://doi.org/10.1001/jama.2018.9890. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grothey, A.; Van Cutsem, E.; Sobrero, A.; Siena, S.; Falcone, A.; Ychou, M.; Humblet, Y.; Bouché, O.; Mineur, L.; Barone, C.; et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): An international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013, 381, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Serizawa, T.; Shuto, T.; Akabane, A.; Higuchi, Y.; Kawagishi, J.; Yamanaka, K.; Sato, Y.; Jokura, H.; Yomo, S.; et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi-institutional prospective observational study. Lancet Oncol. 2014, 15, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Del Carpio Huerta, L.; Virgili Manrique, A.C.; Szafranska, J.; Martin-Richard, M.; Paez Lopez-Bravo, D.; Sebio Garcia, A.; Espinosa Mariscal, I.; Gomila Pons, P.; Andres Granyo, M.; Barba Joaquin, A.; et al. Brain metastases in colorectal cancer: Prognostic factors and survival analysis. Int. J. Color. Dis. 2018, 33, 1517–1523. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Wang, H.W.; Wang, K.; Xing, B.C. The primary tumor location impacts survival outcome of colorectal liver metastases after hepatic resection: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2019, 45, 1349–1356. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, M.S.; McCall, J.L. Surgery for colorectal liver metastases with hepatic lymph node involvement: A systematic review. Br. J. Surg. 2000, 87, 1142–1155, Erratum in Br. J. Surg. 2001, 88, 472. [Google Scholar] [CrossRef] [PubMed]
- Laurent, C.; Sa Cunha, A.; Rullier, E.; Smith, D.; Rullier, A.; Saric, J. Impact of microscopic hepatic lymph node involvement on survival after resection of colorectal liver metastasis. J. Am. Coll. Surg. 2004, 198, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Turner, K.M.; Delman, A.M.; Wima, K.; Quillin, R.C.; Shah, S.A.; Ahmad, S.A.; Patel, S.H.; Wilson, G.C. Microsatellite instability is associated with worse overall survival in resectable colorectal liver metastases. Am. J. Surg. 2023, 225, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Vauthey, J.N.; Zimmitti, G.; Kopetz, S.E.; Shindoh, J.; Chen, S.S.; Andreou, A.; Curley, S.A.; Aloia, T.A.; Maru, D.M. RAS mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg. 2013, 258, 619–626; discussion 626–627. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kawakami, H.; Zaanan, A.; Sinicrope, F.A. Microsatellite instability testing and its role in the management of colorectal cancer. Curr. Treat. Options Oncol. 2015, 16, 30. [Google Scholar] [CrossRef]
- Takamizawa, Y.; Shida, D.; Horie, T.; Tsukamoto, S.; Esaki, M.; Shimada, K.; Kondo, T.; Kanemitsu, Y. Prognostic Role for Primary Tumor Location in Patients With Colorectal Liver Metastases: A Comparison of Right-Sided Colon, Left-Sided Colon, and Rectum. Dis. Colon. Rectum. 2023, 66, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Hokuto, D.; Koyama, F.; Matsuo, Y.; Nomi, T.; Yoshikawa, T.; Kamitani, N.; Sadamitsu, T.; Takei, T.; Matsumoto, Y.; et al. The Prognosis and Recurrence Pattern of Right- and Left-Sided Colon Cancer in Stage II, Stage III, and Liver Metastasis After Curative Resection. Ann. Coloproctol. 2021, 37, 326–336. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, J.H.; Lin, W.L.; Chen, W.S.; Jiang, J.K.; Yang, S.H.; Wang, H.S.; Chang, S.C.; Lan, Y.T.; Lin, C.C.; Lin, H.H.; et al. The survival outcome differs between left-sided colon cancer and middle/low rectal cancer after colorectal hepatic metastasectomy. J. Gastrointest. Surg. 2024, 28, 1250–1258. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; Heng, Y.; Deng, S.; Gu, J.; Mao, F.; Xue, Y.; Jiang, Z.; Wang, J.; Cheng, D.; Wu, K.; et al. Perineural invasion affects prognosis of patients undergoing colorectal cancer surgery: A propensity score matching analysis. BMC Cancer 2023, 23, 452. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Holch, J.W.; Ricard, I.; Stintzing, S.; Modest, D.P.; Heinemann, V. The relevance of primary tumour location in patients with metastatic colorectal cancer: A meta-analysis of first-line clinical trials. Eur. J. Cancer 2017, 70, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Valdimarsson, V.T.; Syk, I.; Lindell, G.; Norén, A.; Isaksson, B.; Sandström, P.; Rizell, M.; Ardnor, B.; Sturesson, C. Outcomes of liver-first strategy and classical strategy for synchronous colorectal liver metastases in Sweden. HPB 2018, 20, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Lillemoe, H.A.; Vauthey, J.N. Surgical approach to synchronous colorectal liver metastases: Staged, combined, or reverse strategy. Hepatobiliary Surg. Nutr. 2020, 9, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Zeyara, A.; Torén, W.; Søreide, K.; Andersson, R. The liver-first approach for synchronous colorectal liver metastases: A systematic review and meta-analysis of completion rates and effects on survival. Scand. J. Gastroenterol. 2022, 111, 14574969211030131. [Google Scholar] [CrossRef]
- Mesheryakova, M.Y.; Trifanov, V.S.; Chernichenko, M.A.; Moshurov, R.I. Liver-first approach in surgical treatment of colorectal cancer with synchronous liver metastases: Results of a single-center study. Russ. J. Oncol. 2024, 28, 159–169. [Google Scholar] [CrossRef]
- Nordlinger, B.; Sorbye, H.; Glimelius, B.; Poston, G.J.; Schlag, P.M.; Rougier, P.; Bechstein, W.O.; Primrose, J.N.; Walpole, E.T.; Finch-Jones, M.; et al. Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): Long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol. 2013, 14, 1208–1215. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, P.J.; van Etten, B.; Hospers, G.A.; Påhlman, L.; van de Velde, C.J.; Beets-Tan, R.G.; Blomqvist, L.; Beukema, J.C.; Kapiteijn, E.; Marijnen, C.A.; et al. Short-course radiotherapy followed by neo-adjuvant chemotherapy in locally advanced rectal cancer--the RAPIDO trial. BMC Cancer 2013, 13, 279. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bahadoer, R.R.; Dijkstra, E.A.; van Etten, B.; Marijnen, C.A.M.; Putter, H.; Kranenbarg, E.M.; Roodvoets, A.G.H.; Nagtegaal, I.D.; Beets-Tan, R.G.H.; Blomqvist, L.K.; et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): A randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 29–42, Erratum in Lancet Oncol. 2021, 22, e42. https://doi.org/10.1016/S1470-2045(20)30781-6. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Li, Q.; Wang, C.; Zhu, H.; Shi, Y.; Zhao, G. Simultaneous vs. staged resection for synchronous colorectal liver metastases: A metaanalysis. Int. J. Color. Dis. 2011, 26, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Chua, T.C.; Saxena, A.; Chu, F. Hepatectomy for colorectal liver metastases: A 10-year experience from a single institution. ANZ J. Surg. 2010, 80, 277–282. [Google Scholar] [CrossRef]
- Gollins, S.; West, N.; Sebag-Montefiore, D.; Susnerwala, S.; Falk, S.; Brown, N.; Saunders, M.; Quirke, P.; Ray, R.; Parsons, P.; et al. A prospective phase II study of pre-operative chemotherapy then short-course radiotherapy for high risk rectal cancer: COPERNICUS. Br. J. Cancer. 2018, 119, 697–706. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karam, E.; Bucur, P.; Gil, C.; Sindayigaya, R.; Tabchouri, N.; Barbier, L.; Pabst-Giger, U.; Bourlier, P.; Lecomte, T.; Moussata, D.; et al. Simultaneous or staged resection for synchronous liver metastasis and primary rectal cancer: A propensity score matching analysis. BMC Gastroenterol. 2022, 22, 201. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abbas, S.; Lam, V.; Hollands, M. Ten-year survival after liver resection for colorectal metastases: Systematic review and meta-analysis. ISRN Oncol. 2011, 2011, 763245. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Giuliante, F.; Viganò, L.; De Rose, A.M.; Mirza, D.F.; Lapointe, R.; Kaiser, G.; Barroso, E.; Ferrero, A.; Isoniemi, H.; Lopez-Ben, S.; et al. Liver-First Approach for Synchronous Colorectal Metastases: Analysis of 7360 Patients from the LiverMetSurvey Registry. Ann. Surg. Oncol. 2021, 28, 8198–8208. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Jong, M.C.; Beckers, R.C.J.; van Woerden, V.; Sijmons, J.M.L.; Bemelmans, M.H.A.; van Dam, R.M.; Dejong, C.H.C. The liver-first approach for synchronous colorectal liver metastases: More than a decade of experience in a single centre. HPB 2018, 20, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, E.K.; Bauer, T.W.; Chun, Y.S.; D’Angelica, M.; Kooby, D.A.; Jarnagin, W.R. Locoregional surgical and interventional therapies for advanced colorectal cancer liver metastases: Expert consensus statements. HPB 2013, 15, 119–130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Del Basso, C.; Usai, S.; Sandri, G.B.L. Laparoscopic hepatic resections for colorectal cancer metastases: A narrative review. Laparosc. Surg. 2023, 7, 13. [Google Scholar] [CrossRef]
- Bulisani, B.M.; Leite, M.A.O.; Waisberg, J. Liver-first approach to the treatment of patients with synchronous colorectal liver metastases: A systematic review and meta-analysis. Einstein (Sao Paulo). 2024, 22, eRW0596. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scheele, J.; Stang, R.; Altendorf-Hofmann, A.; Paul, M. Resection of colorectal liver metastases. World J. Surg. 1995, 19, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Boudjema, K.; Locher, C.; Sabbagh, C.; Ortega-Deballon, P.; Heyd, B.; Bachellier, P.; Métairie, S.; Paye, F.; Bourlier, P.; Adam, R.; et al. Simultaneous Versus Delayed Resection for Initially Resectable Synchronous Colorectal Cancer Liver Metastases: A Prospective, Open-label, Randomized, Controlled Trial. Ann. Surg. 2021, 273, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Siriwardena, A.K.; Serrablo, A.; Fretland, Å.A.; Wigmore, S.J.; Ramia-Angel, J.M.; Malik, H.Z.; Stättner, S.; Søreide, K.; Zmora, O.; Meijerink, M.; et al. Multisocietal European consensus on the terminology, diagnosis, and management of patients with synchronous colorectal cancer and liver metastases: An E-AHPBA consensus in partnership with ESSO, ESCP, ESGAR, and CIRSE. Br. J. Surg. 2023, 110, 1161–1170. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ihnát, P.; Vávra, P.; Zonča, P. Treatment strategies for colorectal carcinoma with synchronous liver metastases: Which way to go? World. J. Gastroenterol. 2015, 21, 7014–7021. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adam, R.; Delvart, V.; Pascal, G.; Valeanu, A.; Castaing, D.; Azoulay, D.; Giacchetti, S.; Paule, B.; Kunstlinger, F.; Ghémard, O.; et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: A model to predict long-term survival. Ann. Surg. 2004, 240, 644–657; discussion 657–658. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Accardo, C.; Vella, I.; di Francesco, F.; Rizzo, S.; Calamia, S.; Tropea, A.; Bonsignore, P.; Li Petri, S.; Gruttadauria, S. Multimodal treatment of colorectal liver metastases: Where are we? Current strategies and future perspectives. Biosci. Trends 2025. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Welsh, F.K.; Tekkis, P.P.; John, T.G.; Rees, M. Predictive models in colorectal liver metastases--can we personalize treatment and outcome? Dig. Surg. 2008, 25, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Worni, M.; Shah, K.N.; Clary, B.M. Colorectal cancer with potentially resectable hepatic metastases: Optimizing treatment. Curr. Oncol. Rep. 2014, 16, 407. [Google Scholar] [CrossRef] [PubMed]
- Huiskens, J.; Bolhuis, K.; Engelbrecht, M.R.; De Jong, K.P.; Kazemier, G.; Liem, M.S.; Verhoef, C.; de Wilt, J.H.; Punt, C.J.; van Gulik, T.M.; et al. Outcomes of resectability assessment of the Dutch Colorectal Cancer Group Liver Metastases Expert Panel. J. Am. Coll. Surg. 2019, 229, 523–532.e2. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; De Gramont, A.; Figueras, J.; Guthrie, A.; Kokudo, N.; Kunstlinger, F.; Loyer, E.; Poston, G.; Rougier, P.; Rubbia-Brandt, L.; et al. The oncosurgery approach to managing liver metastases from colorectal cancer: A multidisciplinary international consensus. Oncologist 2012, 17, 1225–1239. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mohammad, W.M.; Martel, G.; Mimeault, R.; Fairfull-Smith, R.J.; Auer, R.C.; Balaa, F.K. Evaluating agreement regarding the resectability of colorectal liver metastases: A national case-based survey of hepatic surgeons. HPB 2012, 14, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Mattar, R.E.; Al-Alem, F.; Simoneau, E.; Hassanain, M. Preoperative selection of patients with colorectal cancer liver metastasis for hepatic resection. World J. Gastroenterol. 2016, 22, 567–581. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giuliante, F.; Ardito, F.; Ferrero, A.; Aldrighetti, L.; Ercolani, G.; Grande, G.; Ratti, F.; Giovannini, I.; Federico, B.; Pinna, A.D.; et al. Tumor progression during preoperative chemotherapy predicts failure to complete 2-stage hepatectomy for colorectal liver metastases: Results of an Italian multicenter analysis of 130 patients. J. Am. Coll. Surg. 2014, 219, 285–294. [Google Scholar] [CrossRef]
- Lau, W.Y.; Lai, E.C.; Lau, S.H. Associating liver partition and portal vein ligation for staged hepatectomy: The current role and development. Hepatobiliary Pancreat. Dis. Int. 2017, 16, 17–26. [Google Scholar] [CrossRef]
- Chen, F.L.; Wang, Y.Y.; Liu, W.; Xing, B.C. Neoadjuvant chemotherapy improves overall survival in resectable colorectal liver metastases patients with high clinical risk scores—A retrospective, propensity score matching analysis. Front. Oncol. 2022, 12, 973418. [Google Scholar] [CrossRef]
- Adam, R.; Avisar, E.; Ariche, A.; Giachetti, S.; Azoulay, D.; Castaing, D.; Kunstlinger, F.; Levi, F.; Bismuth, F. Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal. Ann. Surg. Oncol. 2001, 8, 347–353. [Google Scholar] [CrossRef]
- Araujo, R.L.; Gönen, M.; Allen, P.J.; DeMatteo, R.; Kingham, P.; Jarnagin, W.; D’Angelica, M.; Fong, Y. Positive postoperative CEA is a strong predictor of recurrence for patients after resection for colorectal liver metastases. Ann. Surg. Oncol. 2015, 22, 3087–3093. [Google Scholar] [CrossRef][Green Version]
- He, Y.; Ma, X.; Chen, K.; Liu, F.; Cai, S.; Han-Zhang, H.; Hou, T.; Xiang, J.; Peng, J. Perioperative circulating tumor DNA in colorectal liver metastases: Concordance with metastatic tissue and predictive value for tumor burden and prognosis. J. Clin. Oncol. 2020, 38 (Suppl. 15), e16020. [Google Scholar] [CrossRef] [PubMed]
- Mao, R.; Zhao, J.J.; Bi, X.Y.; Zhang, Y.F.; Li, Z.Y.; Zhou, J.G.; Wu, X.L.; Xiao, C.; Zhao, H.; Cai, J.Q. A postoperative scoring system for post-hepatectomy early recurrence of colorectal liver metastases. Oncotarget 2017, 8, 102531–102539. [Google Scholar] [CrossRef][Green Version]
- Nevola, R.; Ruocco, R.; Criscuolo, L.; Villani, A.; Alfano, M.; Beccia, D.; Imbriani, S.; Claar, E.; Cozzolino, D.; Sasso, F.C.; et al. Predictors of early and late hepatocellular carcinoma recurrence. World J. Gastroenterol. 2023, 29, 1243–1260. [Google Scholar] [CrossRef]
- Park, J.K.; Lee, Y.J.; Lee, J.H. Prognostic significance of tissue and serum CEA expression after resection of colorectal liver metastases. J. Surg. Oncol. 2010, 102, 274–280. [Google Scholar] [CrossRef]
- Tan, M.C.B.; Castaldo, E.T.; Gao, F.; Chari, R.S.; Linehan, D.C.; Wright, J.K.; Hawkins, W.G.; Siegel, B.A.; Delbeke, D.; Pinson, C.W.; et al. A prognostic system applicable to patients with resectable liver metastasis from colorectal carcinoma staged by positron emission tomography with [18F]fluoro-2-deoxy-D-glucose: Role of primary tumor variables. J. Am. Coll. Surg. 2008, 206, 857–868. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Wang, J.; Li, Z.; Yang, Y.; Yang, L.; Zhang, Y.; Shi, Y.; Cao, Y.; Zhou, J.; Wang, Z.; et al. Risk factors and outcomes of early relapse after curative resection of intrahepatic cholangiocarcinoma. Front. Oncol. 2019, 9, 854. [Google Scholar] [CrossRef] [PubMed]
- Papakonstantinou, M.; Fiflis, S.; Christodoulidis, G.; Giglio, M.C.; Louri, E.; Mavromatidis, S.; Giakoustidis, D.; Papadopoulos, V.N.; Giakoustidis, A. Neutrophil-to-lymphocyte ratio as a prognostic factor for survival in patients with colorectal liver metastases: A systematic review. World J. Clin. Oncol. 2022, 13, 822–834. [Google Scholar] [CrossRef] [PubMed]
- Guo, G.; Hu, X.; Gao, T.; Zhou, H.; Li, B.; Zhou, C.; Yu, B.; Wang, G. Potential impact of platelet-to-lymphocyte ratio on prognosis in patients with colorectal cancer: A systematic review and meta-analysis. Front. Surg. 2023, 10, 1139503. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, H.Y.; Li, J.; Shao, X.Y.; Zhang, C.X. The elevated NLR, PLR and PLT may predict the prognosis of patients with colorectal cancer: A systematic review and meta-analysis. Oncotarget 2017, 8, 68837–68846. [Google Scholar] [CrossRef]
- Wang, J.; Li, J.; Wei, S. The ratio of platelets to lymphocytes predicts the prognosis of metastatic colorectal cancer: A review and meta-analysis. Front. Oncol. 2021, 11, 5877. [Google Scholar] [CrossRef]
- Chen, Q.; Li, G.L.; Zhu, H.Q.; Yu, J.D.; Chen, Z.P.; Wu, J.Y.; Lin, Z.Y.; Wan, Y.L. The neutrophil-to-lymphocyte ratio and lactate dehydrogenase combined in predicting liver metastasis and prognosis of colorectal cancer. Front. Med. 2023, 10, 1205897. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kawada, K.; Obama, K. Inflammation-related biomarkers for the prediction of prognosis in colorectal cancer patients. Int. J. Mol. Sci. 2021, 22, 8002. [Google Scholar] [CrossRef]
- Lu, C.; Gao, P.; Yang, Y.; Chen, X.; Wang, L.; Yu, D.; Song, Y.; Xu, Q.; Wang, Z. Prognostic evaluation of platelet to lymphocyte ratio in patients with colorectal cancer. Oncotarget 2017, 8, 86287–86295. [Google Scholar] [CrossRef]
- Bhattacharjee, D.; Quirke, P. What is the role of the neutrophil: Lymphocyte ratio in colorectal cancer? Turk. J. Color. Dis. 2021, 31, 1–12. [Google Scholar] [CrossRef]
- Polk, N.; Budai, B.; Hitre, E.; Patócs, A.; Mersich, T. High neutrophil-to-lymphocyte ratio (NLR) and systemic immune-inflammation index (SII) are markers of longer survival after metastasectomy of patients with liver-only metastasis of rectal cancer. Pathol. Oncol. Res. 2022, 28, 1610315. [Google Scholar] [CrossRef]
- Amini, N.; Spolverato, G.; Gupta, R.; Margonis, G.A.; Kim, Y.; Wagner, D. Defining the impact of preoperative hypoalbuminemia on outcomes of patients undergoing hepatic resection for colorectal liver metastases. HPB 2016, 18, 124–131. [Google Scholar]
- Liu, Y.W.; Lu, C.C.; Chang, C.D.; Lee, K.C.; Chen, H.H.; Yeh, W.S.; Hu, W.H.; Tsai, K.L.; Yeh, C.H.; Wee, S.Y.; et al. Prognostic value of sarcopenia in patients with colorectal liver metastases undergoing hepatic resection. Sci. Rep. 2020, 10, 6459. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peng, P.D.; van Vledder, M.G.; Tsai, S.; de Jong, M.C.; Makary, M.; Ng, J.; Edil, B.H.; Wolfgang, C.L.; Schulick, R.D.; Choti, M.A.; et al. Sarcopenia negatively impacts short-term outcomes in patients undergoing hepatic resection for colorectal liver metastasis. HPB 2011, 13, 439–446. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hübner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.; et al. ESPEN guideline: Clinical nutrition in surgery. Clin. Nutr. 2017, 36, 623–650. [Google Scholar] [CrossRef]
- Joglekar, S.; Asghar, A.; Mott, S.L.; Johlin, F.C.; Ehlers, A.P.; Mezhir, J.J. Sarcopenia is an independent predictor of complications following pancreatectomy for adenocarcinoma. J. Surg. Oncol. 2015, 111, 771–775. [Google Scholar] [CrossRef]
- Parmar, C.; Dadar, M.; Marignol, L.; McDonough, M.; Sheikh, K.; O’Reilly, D. Prognostic value of sarcopenia in patients with liver metastases from colorectal cancer. Cancer Imaging 2021, 21, 55. [Google Scholar]
- Dolan, R.D.; Almasaudi, A.S.; Dieu, L.B.; Horgan, P.G.; McMillan, D.C. The relationship between nutritional status, systemic inflammation, and survival in patients with colorectal liver metastases. Ann. Surg. Oncol. 2021, 28, 1909–1916. [Google Scholar]
- Bo, Z.; Chen, Z.; Chen, B.; Yang, J.; Zhao, Z.; Yang, Y.; Ma, J.; He, Q.; Yu, H.; Zheng, C.; et al. Development of sarcopenia-based nomograms predicting postoperative complications of benign liver diseases undergoing hepatectomy: A multicenter cohort study. Front. Nutr. 2023, 10, 1040297. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Song, X.; Long, S.R.; Barber, B.; Kassed, C.A.; Healey, M.; Jones, C.; Zhao, Z. Systematic review on infusion reactions associated with chemotherapies and monoclonal antibodies for metastatic colorectal cancer. Curr. Clin. Pharmacol. 2012, 7, 56–65. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Seymour, M.T.; Maughan, T.S.; Ledermann, J.A.; Topham, C.; James, R.; Gwyther, S.J.; Smith, D.B.; Shepherd, S.; Maraveyas, A.; Ferry, D.R.; et al. Different strategies of sequential and combination chemotherapy for patients with poor prognosis advanced colorectal cancer (MRC FOCUS): A randomised controlled trial. Lancet 2007, 370, 143–152. [Google Scholar] [CrossRef]
- Van Kuilenburg, A.B.; Meinsma, R.; Zoetekouw, L.; Van Gennip, A.H. High prevalence of the IVS14 + 1G>A mutation in the dihydropyrimidine dehydrogenase gene of patients with severe 5-fluorouracil-associated toxicity. Pharmacogenetics 2002, 12, 555–558. [Google Scholar] [CrossRef]
- Lenz, H.J.; Van Cutsem, E.; Khambata-Ford, S.; Mayer, R.J.; Gold, P.; Stella, P.; Mirtsching, B.; Cohn, A.L.; Pippas, A.W.; Azarnia, N. Multicenter phase II and translational study of cetuximab in metastatic colorectal carcinoma refractory to irinotecan, oxaliplatin, and fluoropyrimidines. J. Clin. Oncol. 2006, 24, 4914–4921. [Google Scholar] [CrossRef]
- Hurwitz, H.; Fehrenbacher, L.; Novotny, W.; Cartwright, T.; Hainsworth, J.; Heim, W.; Berlin, J.; Baron, A.; Griffing, S.; Holmgren, E.; et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N. Engl. J. Med. 2004, 350, 2335–2342. [Google Scholar] [CrossRef]
- Ruzzo, A.; Graziano, F.; Loupakis, F.; Rulli, E.; Canestrari, E.; Santini, D.; Catalano, V.; Ficarelli, R.; Maltese, P.; Bisonni, R.; et al. Pharmacogenetic profiling in patients with advanced colorectal cancer treated with first-line FOLFOX-4 chemotherapy. J. Clin. Oncol. 2007, 25, 1247–1254. [Google Scholar] [CrossRef]
- Hu, Z.Y.; Yu, Q.; Pei, Q.; Guo, C. Dose-dependent association between UGT1A1*28 genotype and irinotecan-induced neutropenia: Low doses also increase risk. Clin. Cancer Res. 2010, 16, 3832–3842. [Google Scholar] [CrossRef] [PubMed]
- Lecomte, T.; Ferraz, J.M.; Zinzindohoué, F.; Loriot, M.A.; Tregouet, D.A.; Landi, B.; Berger, A.; Cugnenc, P.H.; Jian, R.; Beaune, P.; et al. Thymidylate synthase gene polymorphism predicts toxicity in colorectal cancer patients receiving 5-fluorouracil-based chemotherapy. Clin. Cancer Res. 2004, 10, 5880–5888. [Google Scholar] [CrossRef] [PubMed]
- Levin-Sparenberg, E.; Bylsma, L.C.; Lowe, K.; Sangare, L.; Fryzek, J.P.; Alexander, D.D. A systematic literature review and meta-analysis describing the prevalence of KRAS, NRAS, and BRAF gene mutations in metastatic colorectal cancer. J. Gastrointest. Oncol. 2020, 11, 1234–1245. [Google Scholar] [CrossRef] [PubMed]
- Margonis, G.A.; Buettner, S.; Andreatos, N.; Kim, Y.; Wagner, D.; Sasaki, K.; Beer, A.; Schwarz, C.; Løes, I.M.; Smolle, M.; et al. Association of BRAF mutations with survival and recurrence in surgically treated patients with metastatic colorectal liver cancer. JAMA Surg. 2018, 153, e180996. [Google Scholar] [CrossRef]
- Søreide, K.; Sandvik, O.M.; Søreide, J.A. KRAS mutation in patients undergoing hepatic resection for colorectal liver metastasis: A biomarker of cancer biology or a byproduct of patient selection? Cancer 2014, 120, 3862–3865. [Google Scholar] [CrossRef][Green Version]
- Rhaiem, R.; Rached, L.; Tashkandi, A.; Bouché, O.; Kianmanesh, R. Implications of RAS Mutations on Oncological Outcomes of Surgical Resection and Thermal Ablation Techniques in the Treatment of Colorectal Liver Metastases. Cancers 2022, 14, 816. [Google Scholar] [CrossRef]
- Yaeger, R.; Cercek, A.; Chou, J.F.; Sylvester, B.E.; Kemeny, N.E.; Hechtman, J.F.; Ladanyi, M.; Rosen, N.; Weiser, M.R.; Capanu, M.; et al. BRAF mutation predicts for poor outcomes after metastasectomy in patients with metastatic colorectal cancer. Cancer 2014, 120, 2316–2324. [Google Scholar] [CrossRef]
- Saravani, K.; Salarzaei, M.; Parooie, F. Effect of KRAS and BRAF mutations in metastatic colorectal cancer patients: A systematic review and meta-analysis based on tumor sidedness and KRAS subtypes. Hum. Antibodies 2021, 29, 275–284. [Google Scholar] [CrossRef]
- Javed, S.; Benoist, S.; Devos, P.; Truant, S.; Guimbaud, R.; Lièvre, A.; Sefrioui, D.; Cohen, R.; Artru, P.; Dupré, A.; et al. Prognostic factors of BRAF V600E colorectal cancer with liver metastases: A retrospective multicentric study. World J. Surg. Oncol. 2022, 20, 131. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gong, J.; Cho, M.; Fakih, M. RAS and BRAF in metastatic colorectal cancer management. J. Gastrointest. Oncol. 2016, 7, 687–704. [Google Scholar] [CrossRef]
- Clarke, C.N.; Kopetz, E.S. BRAF mutant colorectal cancer as a distinct subset of colorectal cancer: Clinical characteristics, clinical behavior, and response to targeted therapies. J. Gastrointest. Oncol. 2016, 7, 604–617. [Google Scholar]
- Niu, C.G.; Zhang, J.; Rao, A.V.; Joshi, U.; Okolo, P. Comparative effectiveness of immunotherapy and chemotherapy in patients with metastatic colorectal cancer stratified by microsatellite instability status. World J. Gastroenterol. 2024, 15, 540–548. [Google Scholar] [CrossRef]
- Le, D.T.; Diaz Jr, L.A.; Kim, T.W.; Van Cutsem, E.; Geva, R.; Jäger, D.; Hara, H.; Burge, M.; O’Neil, B.H.; Kavan, P.; et al. Pembrolizumab for previously treated, microsatellite instability-high/mismatch repair-deficient advanced colorectal cancer: Final analysis of KEYNOTE-164. J. Clin. Oncol. 2023, 41, 1234–1242. [Google Scholar] [CrossRef]
- Greco, L.; Rubbino, F.; Dal Buono, A.; Laghi, L. Microsatellite Instability and Immune Response: From Microenvironment Features to Therapeutic Actionability-Lessons from Colorectal Cancer. Genes 2023, 14, 1169. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Overman, M.J.; McDermott, R.; Leach, J.L.; Lonardi, S.; Lenz, H.J.; Morse, M.A.; Desai, J.; Hill, A.; Axelson, M.; Moss, R.A.; et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): An open-label, multicentre, phase 2 study. Lancet Oncol. 2017, 18, 1182–1191, Erratum in Lancet Oncol. 2017, 18, 510. https://doi.org/10.1016/S1470-2045(17)30638-1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bullock, A.J.; Schlechter, B.L.; Fakih, M.G.; Tsimberidou, A.M.; Grossman, J.E.; Gordon, M.S.; Wilky, B.A.; Pimentel, A.; Mahadevan, D.; Balmanoukian, A.S.; et al. Botensilimab plus balstilimab in relapsed/refractory microsatellite stable metastatic colorectal cancer: A phase 1 trial. Nat. Med. 2024, 30, 2558–2567. [Google Scholar] [CrossRef]
- Barzi, A.; Azad, N.S.; Yang, Y.; Tsao-Wei, D.; Rehman, R.; Fakih, M.; Iqbal, S.; El-Khoueiry, A.B.; Millstein, J.; Jayachandran, P.; et al. Phase I/II study of regorafenib (rego) and pembrolizumab (pembro) in refractory microsatellite stable colorectal cancer (MSSCRC). JCO 2022, 40, 15. [Google Scholar] [CrossRef]
- Andre, T.; Elez, E.; Van Cutsem, E.; Jensen, L.H.; Bennouna, J.; Mendez, G.; Schenker, M.; de la Fouchardiere, C.; Limon, M.L.; Yoshino, T.; et al. Nivolumab plus Ipilimumab in Microsatellite-Instability-High Metastatic Colorectal Cancer. N. Engl. J. Med. 2024, 391, 2014–2026. [Google Scholar] [CrossRef] [PubMed]
- Shao, B.; Yin, Y.S.; Wei, Y.N.; Dong, P.; Ning, H.F.; Wang, G.Z. Combining with immunotherapy is an emerging trend for local treatment of colorectal cancer liver metastases: A bibliometric analysis. Front. Oncol. 2025, 15, 1490570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Siena, S.; Di Bartolomeo, M.; Raghav, K.; Masuishi, T.; Loupakis, F.; Kawakami, H.; Yamaguchi, K.; Nishina, T.; Fakih, M.; Elez, E.; et al. Trastuzumab deruxtecan (DS-8201) in patients with HER2-expressing metastatic colorectal cancer (DESTINY-CRC01): A multicentre, open-label, phase 2 trial. Lancet Oncol. 2021, 22, 779–789. [Google Scholar] [CrossRef]
- Raghav, K.; Loree, J.M.; Morris, J.S.; Overman, M.J.; Yu, R.; Meric-Bernstam, F.; Menter, D.; Korphaisarn, K.; Kee, B.; Muranyi, A.; et al. Validation of HER2 amplification as a predictive biomarker for anti–epidermal growth factor receptor antibody therapy in metastatic colorectal cancer. JCO Precis. Oncol. 2019, 3, 1–13. [Google Scholar] [CrossRef]
- Sawada, K.; Nakamura, Y.; Yamanaka, T.; Kuboki, Y.; Yamaguchi, D.; Yuki, S.; Yoshino, T.; Komatsu, Y.; Sakamoto, N.; Okamoto, W.; et al. Prognostic and predictive value of HER2 amplification in patients with metastatic colorectal cancer. Clin. Color. Cancer. 2018, 17, 198–205. [Google Scholar] [CrossRef]
- Strickler, J.H.; Cercek, A.; Siena, S.; André, T.; Ng, K.; Van Cutsem, E.; Wu, C.; Paulson, A.S.; Hubbard, J.M.; Coveler, A.L.; et al. Tucatinib plus trastuzumab for chemotherapy-refractory, HER2-positive, RAS wild-type unresectable or metastatic colorectal cancer (MOUNTAINEER): A multicentre, open-label, phase 2 study. Lancet Oncol. 2023, 24, 496–508. [Google Scholar] [CrossRef]
- Sart Sartore-Bianchi, A.; Trusolino, L.; Martino, C.; Bencardino, K.; Lonardi, S.; Bergamo, F.; Zagonel, V.; Leone, F.; Depetris, I.; Martinelli, E.; et al. Dual-targeted therapy with trastuzumab and lapatinib in treatment-refractory, KRAS codon 12/13 wild-type, HER2-positive metastatic colorectal cancer (HERACLES): A proof-of-concept, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016, 17, 738–746. [Google Scholar] [CrossRef]
- Chen, P.C.; Yeh, Y.M.; Chu, C.T.; Su, P.F.; Chiu, P.H.; Lin, B.W.; Chen, S.H.; Lin, P.C.; Lee, C.T.; Chen, H.H.W.; et al. HER2 amplification in colorectal cancer with brain metastasis: A propensity score matching study. Eur. J. Cancer 2023, 181, 62–69. [Google Scholar] [CrossRef]
- Chang, J.; Xu, M.; Wang, C.; Huang, D.; Zhang, Z.; Chen, Z.; Zhu, X.; Li, W. Dual HER2 targeted therapy with pyrotinib and trastuzumab in refractory HER2 positive metastatic colorectal cancer: A result from HER2-FUSCC-G study. Nat. Commun. 2023, 14, 3332. [Google Scholar] [CrossRef]
- Zumwalt, T.J.; Goel, A. Immunotherapy of Metastatic Colorectal Cancer: Prevailing Challenges and New Perspectives. Curr. Color. Cancer Rep. 2015, 11, 125–140. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wei, X.L.; Luo, X.; Sheng, H.; Wang, Y.; Chen, D.L.; Li, J.N.; Wang, F.H.; Xu, R.H. PD-L1 expression in liver metastasis: Its clinical significance and discordance with primary tumor in colorectal cancer. J. Transl. Med. 2020, 18, 475. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, J.; Dang, F.; Ren, J.; Wei, W. Role of stromal PD-L1 expression in colorectal liver metastasis. BMC Cancer 2023, 23, 1–9. [Google Scholar]
- Gorzo, A.; Galos, D.; Volovat, S.R.; Lungulescu, C.V.; Burz, C.; Sur, D. Landscape of Immunotherapy Options for Colorectal Cancer: Current Knowledge and Future Perspectives beyond Immune Checkpoint Blockade. Life 2022, 12, 229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cohen, R.; Hain, E.; Buhard, O.; Guilloux, A.; Bardier, A.; Kaci, R.; Bertheau, P.; Renaud, F.; Bibeau, F.; Fléjou, J.F.; et al. Association of Polymerase e Mutations with Exceptional Response to PD-1 Inhibition in Microsatellite Stable Metastatic Colorectal Cancer. JAMA Oncol. 2020, 6, 927–932. [Google Scholar]
- Mandal, R.; Samstein, R.M.; Lee, K.W.; Havel, J.J.; Wang, H.; Krishna, C.; Sabio, E.Y.; Makarov, V.; Kuo, F.; Blecua, P.; et al. Genetic diversity of tumors with mismatch repair deficiency influences anti–PD-1 immunotherapy response. Science 2019, 364, 485–491. [Google Scholar] [CrossRef]
- Chang, L.; Chang, M.; Chang, H.M.; Chang, F. Microsatellite Instability: A Predictive Biomarker for Cancer Immunotherapy. Appl. Immunohistochem. Mol. Morphol. 2018, 26, e15–e21. [Google Scholar] [CrossRef]
- Briggs, S.; Tomlinson, I. Germline and somatic polymerase ε and δ mutations define a new class of hypermutated colorectal and endometrial cancers. J. Pathol. 2013, 230, 148–153. [Google Scholar] [CrossRef]
- Luchini, C.; Bibeau, F.; Ligtenberg, M.J.L.; Singh, N.; Nottegar, A.; Bosse, T.; Miller, R.; Riaz, N.; Douillard, J.Y.; Andre, F.; et al. ESMO recommendations on microsatellite instability testing for immunotherapy in cancer, and its relationship with PD-1/PD-L1 expression and tumor mutational burden: A systematic review-based approach. Ann. Oncol. 2019, 30, 1232–1243. [Google Scholar] [CrossRef]
- Schrock, A.B.; Ouyang, C.; Sandhu, J.; Sokol, E.; Jin, D.; Ross, J.S.; Miller, V.A.; Lim, D.; Amanam, I.; Chao, J.; et al. Tumor mutational burden is predictive of response to immune checkpoint inhibitors in MSI-high metastatic colorectal cancer. Ann. Oncol. 2019, 30, 1096–1103. [Google Scholar] [CrossRef]
- Stenzinger, A.; Allen, J.D.; Maas, J.; Stewart, M.D.; Merino, D.M.; Wempe, M.M.; Dietel, M. Tumor mutational burden standardization initiatives: Recommendations for consistent tumor mutational burden assessment in clinical samples to guide immunotherapy treatment decisions. Genes Chromosomes Cancer 2019, 58, 578–588. [Google Scholar] [CrossRef]
- Mitrovic, B.; Schaeffer, D.F.; Riddell, R.H.; Kirsch, R. Tumor budding in colorectal carcinoma: Time to take notice. Mod. Pathol. 2012, 25, 1315–1325. [Google Scholar] [CrossRef]
- Yuan, H.; Dong, Q.; Zheng, B.; Hu, X.; Xu, J.B.; Tu, S. Lymphovascular invasion is a high risk factor for stage I/II colorectal cancer: A systematic review and meta-analysis. Oncotarget 2017, 8, 46565–46579. [Google Scholar] [CrossRef]
- Knijn, N.; Mogk, S.C.; Teerenstra, S.; Simmer, F.; Nagtegaal, I.D. Perineural Invasion is a Strong Prognostic Factor in Colorectal Cancer: A Systematic Review. Am. J. Surg. Pathol. 2016, 40, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Li, L.; Hu, K. Clinical implications of perineural invasion in patients with colorectal cancer. Medicine 2020, 99, e19525. [Google Scholar] [CrossRef]
- Yang, Y.; Huang, X.; Sun, J.; Gao, P.; Song, Y.; Chen, X.; Zhao, J.; Wang, Z. Prognostic value of perineural invasion in colorectal cancer: A meta-analysis. J. Gastrointest. Surg. 2015, 19, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Kaya, T.; Dursun, A. Can lymphovascular and perineural invasion be additional staging criteria in colorectal cancer? J. Coll. Physicians Surg. Pak. 2021, 30, 657–662. [Google Scholar] [CrossRef]
- Huh, J.W.; Lee, W.Y.; Shin, J.K.; Park, Y.A.; Cho, Y.B.; Kim, H.C.; Yun, S.H. A novel histologic grading system based on lymphovascular invasion, perineural invasion, and tumor budding in colorectal cancer. J. Cancer Res. Clin. Oncol. 2019, 145, 471–477. [Google Scholar] [CrossRef]
- Nielsen, K.; Rolff, H.C.; Eefsen, R.L.; Vainer, B. The morphological growth patterns of colorectal liver metastases are prognostic for overall survival. Mod. Pathol. 2014, 27, 1641–1648. [Google Scholar] [CrossRef] [PubMed]
- Latacz, E.; Höppener, D.; Bohlok, A.; Leduc, S.; Tabariès, S.; Fernández Moro, C.; Lugassy, C.; Nyström, H.; Bozóky, B.; Floris, G.; et al. Histopathological growth patterns of liver metastasis: Updated consensus guidelines for pattern scoring, perspectives and recent mechanistic insights. Br. J. Cancer 2022, 127, 988–1013. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zaharia, C.; Veen, T.; Lea, D.; Kanani, A.; Alexeeva, M.; Søreide, K. Histopathological growth pattern in colorectal liver metastasis and the tumor immune microenvironment. Cancers 2023, 15, 181. [Google Scholar] [CrossRef]
- Van den Eynden, G.G.; Bird, N.C.; Majeed, A.W.; Van Laere, S.; Dirix, L.Y.; Vermeulen, P.B. The histological growth pattern of colorectal cancer liver metastases has prognostic value. Clin. Exp. Metastasis 2012, 29, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Eefsen, R.L.; Vermeulen, P.B.; Christensen, I.J.; Laerum, O.D.; Mogensen, M.B.; Rolff, H.C.; Van den Eynden, G.G.; Høyer-Hansen, G.; Osterlind, K.; Vainer, B.; et al. Growth pattern of colorectal liver metastasis as a marker of recurrence risk. Clin. Exp. Metastasis 2015, 32, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Reinert, T.; Petersen, L.M.S.; Henriksen, T.V.; Larsen, M.Ø.; Rasmussen, M.H.; Johansen, A.F.B.; Øgaard, N.; Knudsen, M.; Nordentoft, I.; Vang, S.; et al. Circulating tumor DNA for prognosis assessment and postoperative management in colorectal cancer patients with liver metastases undergoing local treatment. Cancer 2022, 128, 1106–1118. [Google Scholar]
- Tie, J.; Cohen, J.D.; Lahouel, K.; Lo, S.N.; Wang, Y.; Kosmider, S.; Wong, R.; Shapiro, J.; Lee, M.; Harris, S.; et al. Circulating tumor DNA analysis guiding adjuvant therapy in stage II colon cancer. N. Engl. J. Med. 2022, 386, 2261–2272. [Google Scholar] [CrossRef]
- NCCN Updates ctDNA Stance in Colon, Rectal, and MCC Guidelines. OncLive. Published March 2024. Available online: https://www.onclive.com/view/nccn-updates-ctdna-stance-in-colon-rectal-and-mcc-guidelines (accessed on 30 March 2025).
- Kou, M.; Deng, Y. Circulating tumor DNA as a predictive biomarker for treatment response and survival in metastatic colorectal cancer. Int. J. Color. Dis. 2024, 39, 203. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- NCCN Strengthens Guidance on ctDNA in Colon Cancer, Rectal Cancer, and Merkel Cell Carcinoma. Published March 2024. Available online: https://www.natera.com/company/news/nccn-strengthens-guidance-on-ctdna-in-colon-cancer-rectal-cancer-and-merkel-cell-carcinoma/ (accessed on 30 March 2025).
- Bartolomucci, A.; Nobrega, M.; Ferrier, T.; Dickinson, K.; Kaorey, N.; Nadeau, A.; Castillo, A.; Burnier, J.V. Circulating tumor DNA to monitor treatment response in solid tumors and advance precision oncology. NPJ Precis. Oncol. 2025, 9, 84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marmorino, F.; Prisciandaro, M.; Giordano, M.; Ortolan, E.; Crucitta, S.; Manca, P.; Antoniotti, C.; Valenti, M.M.; Danesi, R.; Conca, V.; et al. Circulating Tumor DNA as a Marker of Minimal Residual Disease After Radical Resection of Colorectal Liver Metastases. JCO Precis. Oncol. 2022, 6, e2200244. [Google Scholar] [CrossRef] [PubMed]
- Peoples, J.J.; Hamghalam, M.; James, I.; Wasim, M.; Gangai, N.; Kang, H.C.; Rong, X.J.; Chun, Y.S.; Do, R.K.G.; Simpson, A.L. Finding reproducible and prognostic radiomic features in variable slice thickness contrast-enhanced CT of colorectal liver metastases. arXiv 2025, arXiv:2501.11221. [Google Scholar] [CrossRef]
- Hu, H.; Chi, J.C.; Zhai, B.; Guo, J.H. CT-based radiomics analysis to predict local progression of recurrent colorectal liver metastases after microwave ablation. Medicine 2023, 102, e36586. [Google Scholar] [CrossRef]
- Zhang, G.; Liu, P.; Wang, G.; He, X.; Xu, L.; Wang, Y.; Li, W.; Peng, W. Local Tumor Progression Predictive Model Based on MRI for Colorectal Cancer Liver Metastases after Radiofrequency Ablation. Discov. Med. 2024, 36, 765–777. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ma, L.Y.; Yin, X.P.; Gao, B.L. Radiomics and Radiogenomics in Evaluation of Colorectal Cancer Liver Metastasis. Front. Oncol. 2022, 11, 689509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de la Pinta, C.; Castillo, M.E.; Collado, M.; Galindo-Pumariño, C.; Peña, C. Radiogenomics: Hunting Down Liver Metastasis in Colorectal Cancer Patients. Cancers 2021, 13, 5547. [Google Scholar] [CrossRef]
- Wang, X.; Fang, Y.; Liang, W.; Wong, C.C.; Qin, H.; Gao, Y.; Liang, M.; Song, L.; Zhang, Y.; Fan, M.; et al. Fusobacterium nucleatum facilitates anti-PD-1 therapy in microsatellite stable colorectal cancer. Cancer Cell 2025, 43, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Mima, K.; Sukawa, Y.; Nishihara, R.; Qian, Z.R.; Yamauchi, M.; Inamura, K.; Kim, S.A.; Masuda, A.; Nowak, J.A.; Nosho, K.; et al. Fusobacterium nucleatum and T cells in colorectal carcinoma. JAMA Oncol. 2015, 1, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Ting, N.L.; Wong, C.C.; Huang, P.; Jiang, L.; Liu, C.; Lin, Y.; Li, S.; Liu, Y.; Xie, M.; et al. Bacteroides fragilis promotes chemoresistance in colorectal cancer, and its elimination by phage VA7 restores chemosensitivity. Cell Host Microbe 2025, 33, 941–956.e10. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, Y.; Mima, K.; Ishimoto, T.; Ogata, Y.; Imai, K.; Miyamoto, Y.; Akiyama, T.; Daitoku, N.; Hiyoshi, Y.; Iwatsuki, M.; et al. Fusobacterium nucleatum in colorectal cancer liver metastases. J. Hepatobiliary Pancreat. Sci. 2024, 31, 345–352. [Google Scholar] [CrossRef]
- Sivan, A.; Corrales, L.; Hubert, N.; Williams, J.B.; Aquino-Michaels, K.; Earley, Z.M.; Benyamin, F.W.; Lei, Y.M.; Jabri, B.; Alegre, M.L.; et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science 2015, 350, 1084–1089. [Google Scholar] [CrossRef]
- Marmorino, F.; Faggioni, L.; Rossini, D.; Gabelloni, M.; Goddi, A.; Ferrer, L.; Conca, V.; Vargas, J.; Biagiarelli, F.; Daniel, F.; et al. The prognostic value of radiomic features in liver-limited metastatic colorectal cancer patients from the TRIBE2 study. Future Oncol. 2023, 19, 1601–1611. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; De Muzio, F.; Cutolo, C.; Setola, S.V.; Grassi, R.; Grassi, F.; Ottaiano, A.; Nasti, G.; Tatangelo, F.; et al. Radiomics textural features by MR imaging to assess clinical outcomes following liver resection in colorectal liver metastases. La Radiol. Medica 2022, 127, 461–470. [Google Scholar] [CrossRef]
- Hao, M.; Wang, K.; Ding, Y.; Li, H.; Liu, Y.; Ding, L. Which patients are prone to suffer liver metastasis? A review of risk factors of metachronous liver metastasis of colorectal cancer. Eur. J. Med. Res. 2022, 27, 130. [Google Scholar] [CrossRef] [PubMed]
- Karami, P.; Elahi, R. Radiomics-based artificial intelligence (AI) models in colorectal cancer (CRC) diagnosis, metastasis detection, prognosis, and treatment response. arXiv 2024, arXiv:2406.12467. [Google Scholar] [CrossRef]
- Jing, H.H.; Hao, D.; Liu, X.J.; Cui, M.J.; Xue, K.J.; Wang, D.S.; Zhang, J.H.; Lu, Y.; Tian, G.Y.; Liu, S.L. Development and validation of a radiopathomics model for predicting liver metastases of colorectal cancer. Eur. Radiol. 2025, 35, 3409–3417. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hu, H.; Chi, J.C.; Zhai, B.; Guo, J.H. A CT-based radiomics tumor quality and quantity model to predict early recurrence after radical surgery for colorectal liver metastases. Clin. Transl. Oncol. 2023, 25, 4553. [Google Scholar] [CrossRef]
- Saber, R.; Henault, D.; Rebolledo, R.; Turcotte, S.; Kadoury, S. Prediction of a T-cell/MHC-I-based immune profile for colorectal liver metastases from CT images using ensemble learning. arXiv 2023, arXiv:2303.04149. [Google Scholar] [CrossRef]
- Li, X.; Xiao, H.; Weng, W.; Xu, X.; Shi, Y. MPBD-LSTM: A Predictive Model for Colorectal Liver Metastases Using Time Series Multi-phase Contrast-Enhanced CT Scans. arXiv 2024, arXiv:2412.01973. [Google Scholar]
- Elforaici, M.E.; Montagnon, E.; Perdigon Romero, F.; Le, W.T.; Azzi, F.; Trudel, D.; Nguyen, B.; Turcotte, S.; Tang, A.; Kadoury, S. Semi-supervised ViT knowledge distillation network with style transfer normalization for colorectal liver metastases survival prediction. arXiv 2023, arXiv:2311.10305. [Google Scholar] [CrossRef]
- Bodalal, Z.; Bogveradze, N.; Ter Beek, L.C.; van den Berg, J.G.; Sanders, J.; Hofland, I.; Trebeschi, S.; Groot Lipman, K.B.W.; Storck, K.; Hong, E.K.; et al. Radiomic signatures from T2W and DWI MRI are predictive of tumour hypoxia in colorectal liver metastases. Insights Into Imaging 2023, 14, 133. [Google Scholar] [CrossRef]
- Taghavi, M.; Trebeschi, S.; Simões, R.; Meek, D.B.; Beckers, R.C.J.; Lambregts, D.M.J.; Verhoef, C.; Houwers, J.B.; van der Heide, U.A.; Beets-Tan, R.G.H.; et al. Machine learning-based analysis of CT radiomics model for prediction of colorectal metachronous liver metastases. Abdom. Radiol. 2021, 46, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wei, H.; Fu, F.; Wei, W.; Wu, Y.; Bai, Y.; Li, Q.; Wang, M. Preoperative prediction of lymphovascular invasion of colorectal cancer by radiomics based on 18F-FDG PET-CT and clinical factors. Front. Radiol. 2023, 3, 1212382. [Google Scholar] [CrossRef] [PubMed]
- Dercle, L.; Lu, L.; Schwartz, L.H.; Qian, M.; Tejpar, S.; Eggleton, P.; Zhao, B.; Piessevaux, H. Radiomics response signature for identification of metastatic colorectal cancer sensitive to therapies targeting EGFR pathway. J. Natl. Cancer Inst. 2020, 112, 902–912. [Google Scholar] [CrossRef]
- Bera, K.; Braman, N.; Gupta, A.; Velcheti, V.; Madabhushi, A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat. Rev. Clin. Oncol. 2022, 19, 132–146. [Google Scholar] [CrossRef]
- Rompianesi, G.; Pegoraro, F.; Ceresa, C.D.; Montalti, R.; Troisi, R.I. Artificial intelligence in the diagnosis and management of colorectal cancer liver metastases. World J. Gastroenterol. 2022, 28, 108–122. [Google Scholar] [CrossRef]
- Moaven, O.; Tavolara, T.E.; Valenzuela, C.D.; Corvera, C.U.; Cha, C.H.; Stauffer, J.A.; Niazi, M.K.K. Machine learning models for predicting the outcomes of surgical treatment of colorectal liver metastases. J. Am. Coll. Surg. 2023, 367, 884–893. [Google Scholar] [CrossRef]
- Rieser, C.J.; Hoehn, R.S.; Zenati, M.; Hall, L.B.; Kang, E.; Zureikat, A.H.; Lee, A.; Ongchin, M.; Holtzman, M.P.; Pingpank, J.F.; et al. Impact of Socioeconomic Status on Presentation and Outcomes in Colorectal Peritoneal Metastases Following Cytoreduction and Chemoperfusion: Persistent Inequalities in Outcomes at a High-Volume Center. Ann. Surg. Oncol. 2021, 28, 3522–3531, Erratum in Ann. Surg. Oncol. 2021, 28 (Suppl. 3), 875. https://doi.org/10.1245/s10434-021-10045-7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sell, N.M.; Shafique, N.; Lee, H.; Lee, G.C.; Tanabe, K.K.; Ferrone, C.R.; Blaszkowsky, L.S.; Hong, T.S.; Wo, J.; Qadan, M. Socioeconomic determinants of the surgical treatment of colorectal liver metastases. Am. J. Surg. 2020, 220, 952–957. [Google Scholar] [CrossRef] [PubMed]
- Vallance, A.E.; van der Meulen, J.; Kuryba, A.; Braun, M.; Jayne, D.G.; Hill, J.; Cameron, I.C.; Walker, K. Socioeconomic differences in selection for liver resection in metastatic colorectal cancer and the impact on survival. Eur. J. Surg. Oncol. 2018, 44, 1588–1594. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, X.; Wang, M.; Gu, J.; Guo, H.; Yang, Y.; Liu, J.; Li, Q. Effect of comorbidity assessed by the Charlson Comorbidity Index on the length of stay, costs, and mortality among colorectal cancer patients undergoing colorectal surgery. Curr. Med. Res. Opin. 2022, 39, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.S.N.; Bharwani, A.A.; Chan, E.H.Y.; Chan, V.H.Y.; Au, H.L.H.; Ho, M.K.; Rashed, S.; Kwong, B.M.H.; Fang, W.; Ma, K.W.; et al. A machine learning model for colorectal liver metastasis post-hepatectomy prognostications. Hepatobiliary Surg. Nutr. 2023, 12, 495–506. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| FACTOR | IMPACT ON PROGNOSIS | MANAGEMENT IMPLICATIONS | KEY REFERENCES |
|---|---|---|---|
| GENDER | Women: 23% less likely to undergo surgery; better OS (40–60 vs. 35–50 months in men) | Consider hormonal factors and tailored chemotherapy dosing (e.g., oxaliplatin adjustments). | [10,11,12,13,14,15] |
| AGE | Elderly (≥65): OS 30–50 months vs. 40–60 months in younger patients | Use geriatric assessments (G8, CGA) to guide treatment intensity. | [16,17,18,19,20] |
| ASA SCORE ≥3 | Higher perioperative complications; OS drops to 36 months with major vascular invasion | Prehabilitation, minimally invasive surgery, and ERAS protocols recommended. | [27,28,29,30,31,32] |
| NUMBER OF METASTASES | 1–3 lesions: 5-year OS 50–60%; ≥4 lesions: DFS drops to 2.5 months | Neoadjuvant chemotherapy (FOLFOX/FOLFIRI ± biologics) to downsize tumors. | [36,37,38,39,40,41] |
| SIZE OF METASTASES | <5 cm: OS 60 months; ≥5 cm: OS 40 months | Two-stage hepatectomy or ALPPS for large lesions. | [46,47,48,49,50] |
| ANATOMIC DISTRIBUTION | Unilateral: 5-year OS > 50%; bilateral: higher recurrence risk | Portal vein embolization or ALPPS for bilobar disease. | [54,55,56,57,58,59] |
| EXTRAHEPATIC METS | Lung (solitary: 5-year OS 71%; multiple: 48%); Peritoneal (PCI < 10: 5-year OS 53%) | Aggressive local therapy (resection/SBRT) for oligometastatic disease. | [63,64,65,66,67,68,69,70,71,72,73,74,75] |
| STRATEGY | DESCRIPTION | OUTCOMES | KEY CONSIDERATIONS |
|---|---|---|---|
| PORTAL VEIN EMBOLIZATION | Induces FLR hypertrophy (10–20% growth in 3–8 weeks). | 5-year OS 35–45%; 20–30% dropout due to progression. | Low morbidity (2–5%). |
| ALPPS | Rapid FLR growth (70–80% in 7–10 days). | Higher morbidity (40%); mortality 5–10%. | Reserved for selected patients. |
| NEOADJUVANT CHEMOTHERAPY | FOLFOX/FOLFIRI ± biologics; resectability in 30–40% of initially unresectable. | Bevacizumab requires 6-week washout; anti-EGFR for RAS WT. | Monitor for liver injury (sinusoidal obstruction). |
| BIOMARKER | PREVALENCE | PROGNOSTIC IMPACT | THERAPEUTIC IMPLICATIONS | KEY REFERENCES |
|---|---|---|---|---|
| RAS MUTATIONS | 35–45% | Median OS 55.3 months; resistance to anti-EGFR therapies | Bevacizumab preferred over cetuximab. | [165,166,167,168,169] |
| BRAF V600E | 1–6.1% | Median OS 16.2 months; aggressive biology | BRAF/MEK inhibitors (e.g., encorafenib + binimetinib). | [167,168,169,170,171,172,173] |
| MSI-H | 5–15% | Favorable with immunotherapy (HR 0.57 for OS vs. chemotherapy) | Pembrolizumab/nivolumab in first-line. | [174,175,176,177,178,179,180,181] |
| HER2 AMPLIFICATION | 3–5% (KRAS WT) | Resistance to anti-EGFR; response to trastuzumab + pertuzumab (30–50% response rate) | Dual HER2 blockade or trastuzumab deruxtecan. | [182,183,184,185,186,187,188,189] |
| POLE/POLD1 | 1–2% | Hypermutated phenotype; favorable response to immunotherapy | Checkpoint inhibitors (even in MSS tumors). | [190,191,192,193,194,195,196,197] |
| TOOL | APPLICATION | CLINICAL UTILITY | LIMITATIONS | KEY REFERENCES |
|---|---|---|---|---|
| CTDNA | Detects minimal residual disease; predicts recurrence (50–60% relapse if +postop) | Guides adjuvant therapy decisions; early intervention for high-risk patients. | Standardization and cost. | [212,213,214,215,216,217,218] |
| RADIOMICS | Quantifies tumor heterogeneity (e.g., sphericity, entropy) | Predicts local progression post-ablation (AUC 0.89–0.91). | Reproducibility across imaging protocols. | [219,220,221,222,223] |
| GUT MICROBIOME | Fusobacterium nucleatum linked to PD-L1 expression; B. fragilis worsens DFS | Potential for microbiome modulation (e.g., probiotics) to enhance immunotherapy. | Causality not established. | [224,225,226,227,228] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conticchio, M.; Uldry, E.; Hübner, M.; Digklia, A.; Fraga, M.; Sempoux, C.; Raisaro, J.L.; Fuks, D. Prognostic Factors in Colorectal Liver Metastases: An Exhaustive Review of the Literature and Future Prospectives. Cancers 2025, 17, 2539. https://doi.org/10.3390/cancers17152539
Conticchio M, Uldry E, Hübner M, Digklia A, Fraga M, Sempoux C, Raisaro JL, Fuks D. Prognostic Factors in Colorectal Liver Metastases: An Exhaustive Review of the Literature and Future Prospectives. Cancers. 2025; 17(15):2539. https://doi.org/10.3390/cancers17152539
Chicago/Turabian StyleConticchio, Maria, Emilie Uldry, Martin Hübner, Antonia Digklia, Montserrat Fraga, Christine Sempoux, Jean Louis Raisaro, and David Fuks. 2025. "Prognostic Factors in Colorectal Liver Metastases: An Exhaustive Review of the Literature and Future Prospectives" Cancers 17, no. 15: 2539. https://doi.org/10.3390/cancers17152539
APA StyleConticchio, M., Uldry, E., Hübner, M., Digklia, A., Fraga, M., Sempoux, C., Raisaro, J. L., & Fuks, D. (2025). Prognostic Factors in Colorectal Liver Metastases: An Exhaustive Review of the Literature and Future Prospectives. Cancers, 17(15), 2539. https://doi.org/10.3390/cancers17152539






