Correction: Lin et al. Incidental Findings in Lung Cancer Screening. Cancers 2024, 16, 2600
Corrected Affiliation
Error in Figure and Figure Legend
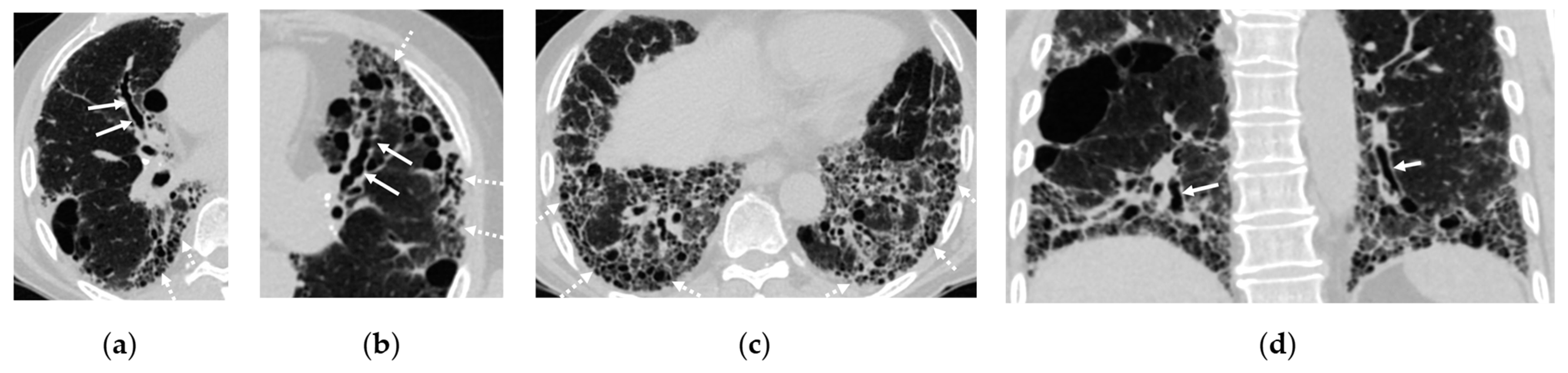
- Figure 2: The original figure intended to illustrate interstitial lung disease (ILD) but inadequately highlighted bronchiectasis in Figure 2a. Additionally, Figure 2b,c presented confusing representations with the consolidation in the right lower lobe. The revised figure now accurately showcases the full spectrum of ILD findings, including traction bronchiectasis, reticulations, cystic changes, and honeycombing. Furthermore, the citation for Figure 2 has been corrected to ensure relevance to the surrounding text.
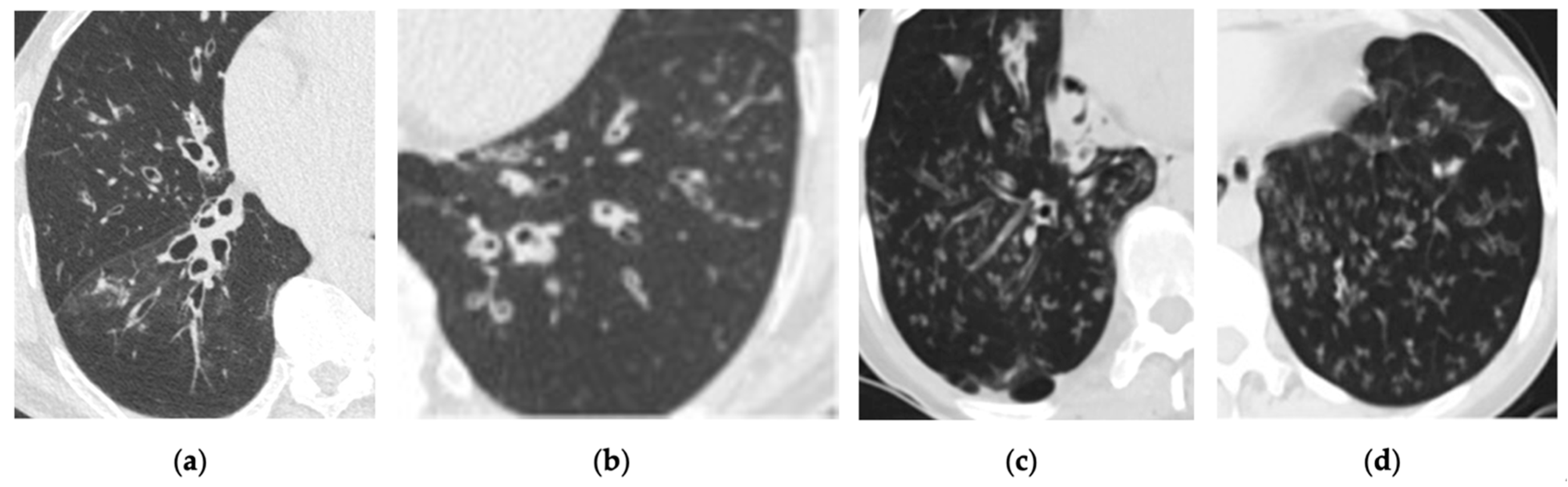
- Figure 4: The replacement figure provides a clearer and more focused depiction of bronchiectasis and infectious bronchiolitis.
Text Correction
Reference
- Lin, Y.; Khurelsukh, K.; Li, I.-G.; Wu, C.-T.; Wu, Y.-M.; Lin, G.; Toh, C.-H.; Wan, Y.-L. Incidental Findings in Lung Cancer Screening. Cancers 2024, 16, 2600. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Y.; Khurelsukh, K.; Li, I.-G.; Wu, C.-T.; Wu, Y.-M.; Lin, G.; Toh, C.-H.; Wan, Y.-L. Correction: Lin et al. Incidental Findings in Lung Cancer Screening. Cancers 2024, 16, 2600. Cancers 2025, 17, 41. https://doi.org/10.3390/cancers17010041
Lin Y, Khurelsukh K, Li I-G, Wu C-T, Wu Y-M, Lin G, Toh C-H, Wan Y-L. Correction: Lin et al. Incidental Findings in Lung Cancer Screening. Cancers 2024, 16, 2600. Cancers. 2025; 17(1):41. https://doi.org/10.3390/cancers17010041
Chicago/Turabian StyleLin, Yenpo, Khulan Khurelsukh, I-Gung Li, Chen-Te Wu, Yi-Ming Wu, Gigin Lin, Cheng-Hong Toh, and Yung-Liang Wan. 2025. "Correction: Lin et al. Incidental Findings in Lung Cancer Screening. Cancers 2024, 16, 2600" Cancers 17, no. 1: 41. https://doi.org/10.3390/cancers17010041
APA StyleLin, Y., Khurelsukh, K., Li, I.-G., Wu, C.-T., Wu, Y.-M., Lin, G., Toh, C.-H., & Wan, Y.-L. (2025). Correction: Lin et al. Incidental Findings in Lung Cancer Screening. Cancers 2024, 16, 2600. Cancers, 17(1), 41. https://doi.org/10.3390/cancers17010041





