Implementation and Evaluation of a Breast Cancer Disease Model Using Real-World Claims Data in Germany from 2010 to 2020
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Robert-Koch-Institut. Krebs in Deutschland 2017/2018; Robert Koch-Institut: Berlin, Germany, 2021. [Google Scholar]
- Jemal, A.; Center, M.M.; DeSantis, C.; Ward, E.M. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1893–1907. [Google Scholar] [CrossRef]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up †. Ann. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef] [PubMed]
- Park-Simon, T.W.; Müller, V.; Jackisch, C.; Albert, U.S.; Banys-Paluchowski, M.; Bauerfeind, I.; Blohmer, J.U.; Budach, W.; Dall, P.; Ditsch, N.; et al. Arbeitsgemeinschaft Gynäkologische Onkologie Recommendations for the Diagnosis and Treatment of Patients with Early Breast Cancer: Update 2023. Breast Care 2023, 18, 289–305. [Google Scholar] [CrossRef]
- Dannehl, D.; Engler, T.; Volmer, L.L.; Staebler, A.; Fischer, A.K.; Weiss, M.; Hahn, M.; Walter, C.B.; Grischke, E.M.; Fend, F.; et al. Recurrence Score(®) Result Impacts Treatment Decisions in Hormone Receptor-Positive, HER2−Negative Patients with Early Breast Cancer in a Real-World Setting-Results of the IRMA Trial. Cancers 2022, 14, 5365. [Google Scholar] [CrossRef] [PubMed]
- Dannehl, D.; Engler, T.; Volmer, L.L.; Tegeler, C.M.; Fusshoeller, J.; Gabrysch, E.; Eissler, K.; Seller, A.; Grischke, E.M.; Hahn, M.; et al. Which Patients Do We Need to Test for BRCA1/2 Mutation? Feasibility of Adjuvant Olaparib Treatment in Early Breast Cancer-Real-World Data from Two Large German Breast Centers. Cancers 2023, 15, 3847. [Google Scholar] [CrossRef] [PubMed]
- Dannehl, D.; Volmer, L.L.; Weiss, M.; Matovina, S.; Grischke, E.M.; Oberlechner, E.; Seller, A.; Walter, C.B.; Hahn, M.; Engler, T.; et al. Feasibility of Adjuvant Treatment with Abemaciclib-Real-World Data from a Large German Breast Center. J. Pers. Med. 2022, 12, 382. [Google Scholar] [CrossRef] [PubMed]
- Katalinic, A.; Halber, M.; Meyer, M.; Pflüger, M.; Eberle, A.; Nennecke, A.; Kim-Wanner, S.Z.; Hartz, T.; Weitmann, K.; Stang, A.; et al. Population-Based Clinical Cancer Registration in Germany. Cancers 2023, 15, 3934. [Google Scholar] [CrossRef] [PubMed]
- Fasching, P.A.; Brucker, S.Y.; Fehm, T.N.; Overkamp, F.; Janni, W.; Wallwiener, M.; Hadji, P.; Belleville, E.; Häberle, L.; Taran, F.A.; et al. Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network. Geburtshilfe Frauenheilkd. 2015, 75, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Schäffler, H.; Mergel, F.; Pfister, K.; Lukac, S.; Fink, A.; Veselinovic, K.; Rack, B.; Fink, V.; Leinert, E.; Dimpfl, M. The Clinical Relevance of the NATALEE Study: Application of the NATALEE Criteria to a Real-World Cohort from Two Large German Breast Cancer Centers. Int. J. Mol. Sci. 2023, 24, 16366. [Google Scholar] [CrossRef]
- Langner, I.; Ohlmeier, C.; Haug, U.; Hense, H.W.; Czwikla, J.; Zeeb, H. Implementation of an algorithm for the identification of breast cancer deaths in German health insurance claims data: A validation study based on a record linkage with administrative mortality data. BMJ Open 2019, 9, e026834. [Google Scholar] [CrossRef]
- Heinig, M.; Heinze, F.; Schwarz, S.; Haug, U. Initial and ten-year treatment patterns among 11,000 breast cancer patients undergoing breast surgery-an analysis of German claims data. BMC Cancer 2022, 22, 130. [Google Scholar] [CrossRef] [PubMed]
- Kawai, M.; Takada, M.; Nakayama, T.; Masuda, N.; Shiheido, H.; Cai, Z.; Huang, Y.J.; Kawaguchi, T.; Tanizawa, Y. Patient characteristics, treatment patterns, and outcomes of hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer patients prescribed cyclin-dependent kinase 4 and 6 inhibitors: Large-scale data analysis using a Japanese claims database. Breast Cancer Res. Treat. 2023, 197, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Kreis, K.; Plöthner, M.; Schmidt, T.; Seufert, R.; Schreeb, K.; Jahndel, V.; Maas, S.; Kuhlmann, A.; Zeidler, J.; Schramm, A. Healthcare costs associated with breast cancer in Germany: A claims data analysis. Eur. J. Health Econ. 2020, 21, 451–464. [Google Scholar] [CrossRef] [PubMed]
- Luyendijk, M.; Vernooij, R.W.M.; Blommestein, H.M.; Siesling, S.; Uyl-de Groot, C.A. Assessment of Studies Evaluating Incremental Costs, Effectiveness, or Cost-Effectiveness of Systemic Therapies in Breast Cancer Based on Claims Data: A Systematic Review. Value Health 2020, 23, 1497–1508. [Google Scholar] [CrossRef] [PubMed]
- Krankenkassen, S.d.G. Spitzenverband der Gesetzlichen Krankenkassen. 2023. Available online: https://www.gkv-spitzenverband.de/gkv_spitzenverband/gkv_spitzenverband.jsp (accessed on 12 April 2024).
- Krankenkassen, S.d.P. Spitzenverband der Privaten Krankenkassen. 2023. Available online: https://www.pkv.de/wissen/private-krankenversicherung/ (accessed on 12 April 2024).
- Baden-Wuerttemberg, A.O.A. Krankenkasseninfo. 2023. Available online: https://www.krankenkasseninfo.de/zahlen-fakten/mitgliederzahlen/ (accessed on 12 April 2024).
- (KKG), B.f.A.u.M.B.i.A.d.B.f.G.B.u.B.d.A.I.d.K.f.F.d.K.i.G. ICD-10-GM Version 2021, Systematisches Verzeichnis, Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme, 10. Revision, Stand: 18. September 2020. 2020.
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Medizinprodukte, B.f.A.u. Operationen und Prozedurenschlüssel (OPS) 2022. 2021. Operationen- und Prozedurenschlüssel Version 2024; Bundesinstitut für Arzneimittel und Medizinprodukte. Available online: https://klassifikationen.bfarm.de/ops/kode-suche/htmlops2024/index.htm (accessed on 12 April 2024).
- Medizinprodukte, B.f.A.u. Anatomic Therapeutic Chemical (ATC) classification. 2023. ATC Klassifikation Version 2024; Bundesinstitut für Arzneimittel und Medizinprodukte. Available online: https://www.bfarm.de/DE/Kodiersysteme/Klassifikationen/ATC/_node.html (accessed on 12 April 2024).
- Rosenbaum, P.R. Combining planned and discovered comparisons in observational studies. Biostatistics 2020, 21, 384–399. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.B.; Klopfer, S.O. Optimal Full Matching and Related Designs via Network Flows. J. Comput. Graph. Stat. 2006, 15, 609–627. [Google Scholar] [CrossRef]
- Geyer, C.E., Jr.; Garber, J.E.; Gelber, R.D.; Yothers, G.; Taboada, M.; Ross, L.; Rastogi, P.; Cui, K.; Arahmani, A.; Aktan, G.; et al. Overall survival in the OlympiA phase III trial of adjuvant olaparib in patients with germline pathogenic variants in BRCA1/2 and high-risk, early breast cancer. Ann. Oncol. 2022, 33, 1250–1268. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Tarruella, S.; Echavarria, I.; Jerez, Y.; Herrero, B.; Gamez, S.; Martin, M. How we treat HR−positive, HER2−negative early breast cancer. Future Oncol. 2022, 18, 1003–1022. [Google Scholar] [CrossRef]
- Johnston, S.R.D.; Toi, M.; O’Shaughnessy, J.; Rastogi, P.; Campone, M.; Neven, P.; Huang, C.S.; Huober, J.; Jaliffe, G.G.; Cicin, I.; et al. Abemaciclib plus endocrine therapy for hormone receptor-positive, HER2−negative, node-positive, high-risk early breast cancer (monarchE): Results from a preplanned interim analysis of a randomised, open-label, phase 3 trial. Lancet Oncol. 2023, 24, 77–90. [Google Scholar] [CrossRef]
- Sledge, G.W., Jr.; Toi, M.; Neven, P.; Sohn, J.; Inoue, K.; Pivot, X.; Burdaeva, O.; Okera, M.; Masuda, N.; Kaufman, P.A.; et al. The Effect of Abemaciclib Plus Fulvestrant on Overall Survival in Hormone Receptor-Positive, ERBB2-Negative Breast Cancer That Progressed on Endocrine Therapy-MONARCH 2: A Randomized Clinical Trial. JAMA Oncol. 2020, 6, 116–124. [Google Scholar] [CrossRef]
- Swain, S.M.; Baselga, J.; Kim, S.B.; Ro, J.; Semiglazov, V.; Campone, M.; Ciruelos, E.; Ferrero, J.M.; Schneeweiss, A.; Heeson, S.; et al. Pertuzumab, trastuzumab, and docetaxel in HER2−positive metastatic breast cancer. N. Engl. J. Med. 2015, 372, 724–734. [Google Scholar] [CrossRef] [PubMed]
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Increasing the dose intensity of chemotherapy by more frequent administration or sequential scheduling: A patient-level meta-analysis of 37 298 women with early breast cancer in 26 randomised trials. Lancet 2019, 393, 1440–1452. [Google Scholar] [CrossRef] [PubMed]
- Piccart, M.; Procter, M.; Fumagalli, D.; de Azambuja, E.; Clark, E.; Ewer, M.S.; Restuccia, E.; Jerusalem, G.; Dent, S.; Reaby, L.; et al. Adjuvant Pertuzumab and Trastuzumab in Early HER2−Positive Breast Cancer in the APHINITY Trial: 6 Years’ Follow-Up. J. Clin. Oncol. 2021, 39, 1448–1457. [Google Scholar] [CrossRef]
- Robson, M.E.; Tung, N.; Conte, P.; Im, S.A.; Senkus, E.; Xu, B.; Masuda, N.; Delaloge, S.; Li, W.; Armstrong, A.; et al. OlympiAD final overall survival and tolerability results: Olaparib versus chemotherapy treatment of physician’s choice in patients with a germline BRCA mutation and HER2−negative metastatic breast cancer. Ann. Oncol. 2019, 30, 558–566. [Google Scholar] [CrossRef]
- Müller, V.; Ruhnke, M.; Hoffmann, O.; Grafe, A.; Tomé, O.; Fett, W.; Bruch, H.R.; Sommer-Joos, A.K.; Schneeweiss, A. First-line bevacizumab-containing therapy for HER2−negative locally advanced/metastatic breast cancer: Real-world experience from >2000 patients treated in the multicentre AVANTI study. Breast 2021, 60, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Ryu, K.J.; Kim, M.S.; Lee, J.Y.; Nam, S.; Jeong, H.G.; Kim, T.; Park, H. Risk of Endometrial Polyps, Hyperplasia, Carcinoma, and Uterine Cancer After Tamoxifen Treatment in Premenopausal Women with Breast Cancer. JAMA Netw. Open 2022, 5, e2243951. [Google Scholar] [CrossRef]
- Grady, I.; Grady, S.; Chanisheva, N. Long-term cost of breast cancer treatment to the United States Medicare Program by stage at diagnosis. Eur. J. Health Econ. 2021, 22, 1365–1370. [Google Scholar] [CrossRef]
- Rubió-Casadevall, J.; Hernandez-Pujol, A.M.; Ferreira-Santos, M.C.; Morey-Esteve, G.; Vilardell, L.; Osca-Gelis, G.; Vilar-Coromina, N.; Marcos-Gragera, R. Trends in incidence and survival analysis in non-melanoma skin cancer from 1994 to 2012 in Girona, Spain: A population-based study. Cancer Epidemiol. 2016, 45, 6–10. [Google Scholar] [CrossRef]
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. Biomed. Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef]
- Tutt, A.N.J.; Garber, J.E.; Kaufman, B.; Viale, G.; Fumagalli, D.; Rastogi, P.; Gelber, R.D.; de Azambuja, E.; Fielding, A.; Balmaña, J.; et al. Adjuvant Olaparib for Patients with BRCA1- or BRCA2-Mutated Breast Cancer. N. Engl. J. Med. 2021, 384, 2394–2405. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.R.D.; Harbeck, N.; Hegg, R.; Toi, M.; Martin, M.; Shao, Z.M.; Zhang, Q.Y.; Martinez Rodriguez, J.L.; Campone, M.; Hamilton, E.; et al. Abemaciclib Combined with Endocrine Therapy for the Adjuvant Treatment of HR+, HER2−, Node-Positive, High-Risk, Early Breast Cancer (monarchE). J. Clin. Oncol. 2020, 38, 3987–3998. [Google Scholar] [CrossRef] [PubMed]
- Cristofanilli, M.; Turner, N.C.; Bondarenko, I.; Ro, J.; Im, S.A.; Masuda, N.; Colleoni, M.; DeMichele, A.; Loi, S.; Verma, S.; et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2−negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): Final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016, 17, 425–439. [Google Scholar] [CrossRef] [PubMed]
- Slamon, D.J.; Neven, P.; Chia, S.; Fasching, P.A.; De Laurentiis, M.; Im, S.A.; Petrakova, K.; Bianchi, G.V.; Esteva, F.J.; Martín, M.; et al. Phase III Randomized Study of Ribociclib and Fulvestrant in Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: MONALEESA-3. J. Clin. Oncol. 2018, 36, 2465–2472. [Google Scholar] [CrossRef] [PubMed]
- Tonellotto, F.; Bergmann, A.; de Souza Abrahão, K.; de Aguiar, S.S.; Bello, M.A.; Thuler, L.C.S. Impact of Number of Positive Lymph Nodes and Lymph Node Ratio on Survival of Women with Node-Positive Breast Cancer. Eur. J. Breast Health 2019, 15, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.; Chavez-MacGregor, M.; Lichtensztajn, D.Y.; Yi, M.; Tadros, A.; Hortobagyi, G.N.; Giordano, S.H.; Hunt, K.K.; Mittendorf, E.A. Validation Study of the American Joint Committee on Cancer Eighth Edition Prognostic Stage Compared with the Anatomic Stage in Breast Cancer. JAMA Oncol. 2018, 4, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Mittendorf, E.A.; Jeruss, J.S.; Tucker, S.L.; Kolli, A.; Newman, L.A.; Gonzalez-Angulo, A.M.; Buchholz, T.A.; Sahin, A.A.; Cormier, J.N.; Buzdar, A.U.; et al. Validation of a novel staging system for disease-specific survival in patients with breast cancer treated with neoadjuvant chemotherapy. J. Clin. Oncol. 2011, 29, 1956–1962. [Google Scholar] [CrossRef] [PubMed]
- Goldhirsch, A.; Winer, E.P.; Coates, A.S.; Gelber, R.D.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.J. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann. Oncol. 2013, 24, 2206–2223. [Google Scholar] [CrossRef] [PubMed]
- Tinterri, C.; Gentile, D.; Gatzemeier, W.; Sagona, A.; Barbieri, E.; Testori, A.; Errico, V.; Bottini, A.; Marrazzo, E.; Dani, C.; et al. Preservation of Axillary Lymph Nodes Compared with Complete Dissection in T1-2 Breast Cancer Patients Presenting One or Two Metastatic Sentinel Lymph Nodes: The SINODAR-ONE Multicenter Randomized Clinical Trial. Ann. Surg. Oncol. 2022, 29, 5732–5744. [Google Scholar] [CrossRef]
- de Boniface, J.; Frisell, J.; Andersson, Y.; Bergkvist, L.; Ahlgren, J.; Rydén, L.; Olofsson Bagge, R.; Sund, M.; Johansson, H.; Lundstedt, D. Survival and axillary recurrence following sentinel node-positive breast cancer without completion axillary lymph node dissection: The randomized controlled SENOMAC trial. BMC Cancer 2017, 17, 379. [Google Scholar] [CrossRef]
- Giuliano, A.E.; McCall, L.; Beitsch, P.; Whitworth, P.W.; Blumencranz, P.; Leitch, A.M.; Saha, S.; Hunt, K.K.; Morrow, M.; Ballman, K. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: The American College of Surgeons Oncology Group Z0011 randomized trial. Ann. Surg. 2010, 252, 426–432; discussion 432–433. [Google Scholar] [CrossRef] [PubMed]
- Elston, D.M. Survivorship bias. J. Am. Acad. Dermatol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Jensen, E.T.; Cook, S.F.; Allen, J.K.; Logie, J.; Brookhart, M.A.; Kappelman, M.D.; Dellon, E.S. Enrollment factors and bias of disease prevalence estimates in administrative claims data. Ann. Epidemiol. 2015, 25, 519–525.e2. [Google Scholar] [CrossRef] [PubMed]
- Chubak, J.; Pocobelli, G.; Weiss, N.S. Tradeoffs between accuracy measures for electronic health care data algorithms. J. Clin. Epidemiol. 2012, 65, 343–349.e2. [Google Scholar] [CrossRef] [PubMed]
- Groenwold, R.H.; Van Deursen, A.M.; Hoes, A.W.; Hak, E. Poor quality of reporting confounding bias in observational intervention studies: A systematic review. Ann. Epidemiol. 2008, 18, 746–751. [Google Scholar] [CrossRef] [PubMed]
- Kümpel, C.; Schneider, U. Additional reimbursement for outpatient physicians treating nursing home residents reduces avoidable hospital admissions: Results of a reimbursement change in Germany. Health Policy 2020, 124, 470–477. [Google Scholar] [CrossRef]
- Dahlen, A.; Charu, V. Analysis of Sampling Bias in Large Health Care Claims Databases. JAMA Netw. Open 2023, 6, e2249804. [Google Scholar] [CrossRef]

| Breast Cancer | Control | |||
|---|---|---|---|---|
| N | % | N | % | |
| Total | 97,121 | 100 | 94,809 | 100 |
| Excluded unreliable C50 | 50,098 | 51.6 | 0 | 0 |
| Excluded diagnoses outside the time window | 7069 | 7.3 | 0 | 0 |
| Excluded secondary neoplasia | 9640 | 9.9 | 10,964 | 11.6 |
| Excluded metastases | 1487 | 1.5 | 3017 | 3.2 |
| Excluded insured too short | 652 | 0.7 | 2594 | 2.7 |
| Excluded death before diagnosis | 91 | 0.1 | 0 | 0 |
| Excluded male gender | 215 | 0.2 | 1138 | 1.2 |
| Excluded due to matching | 0 | 0 | 21,358 | 22.5 |
| Included | 27,869 | 28.7 | 55,738 | 58.8 |
| Breast Cancer | Control | |||
|---|---|---|---|---|
| N | % | N | % | |
| age at breast cancer diagnosis (years) | ||||
| <50 | 4467 | 16.0 | 8934 | 16.0 |
| 50ies | 5975 | 21.4 | 11,950 | 21.4 |
| 60ies | 6331 | 22.7 | 12,662 | 22.7 |
| 70ies | 6321 | 22.7 | 12,642 | 22.7 |
| >80 | 4775 | 17.1 | 9550 | 17.1 |
| urban density level | ||||
| rural | 7133 | 25.6 | 14,139 | 25.4 |
| suburban | 8928 | 32.0 | 17,609 | 31.6 |
| urban | 11,792 | 42.3 | 23,831 | 42.8 |
| missing | 16 | 0.1 | 159 | 0.3 |
| N | % | |
|---|---|---|
| Estimated receptor expression | ||
| HR+ | 21,697 | 77.9 |
| HR− | 6172 | 22.1 |
| HER2+ | 2747 | 9.9 |
| HER2− | 25,122 | 90.1 |
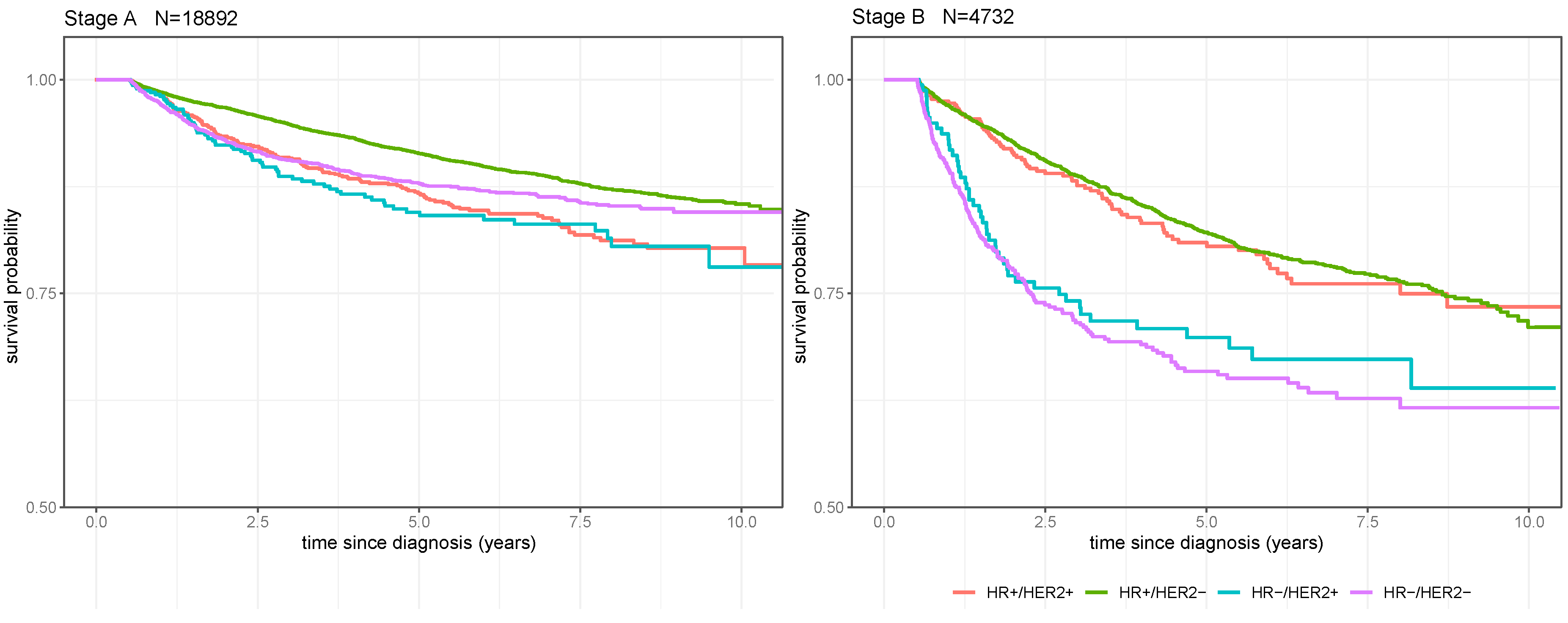
| Estimated biologic subtype | ||
| HR+/HER2+ | 1930 | 6.9 |
| HR+/HER2− | 19,767 | 70.9 |
| HR−/HER2+ | 817 | 2.9 |
| HR−/HER2− | 5355 | 19.2 |
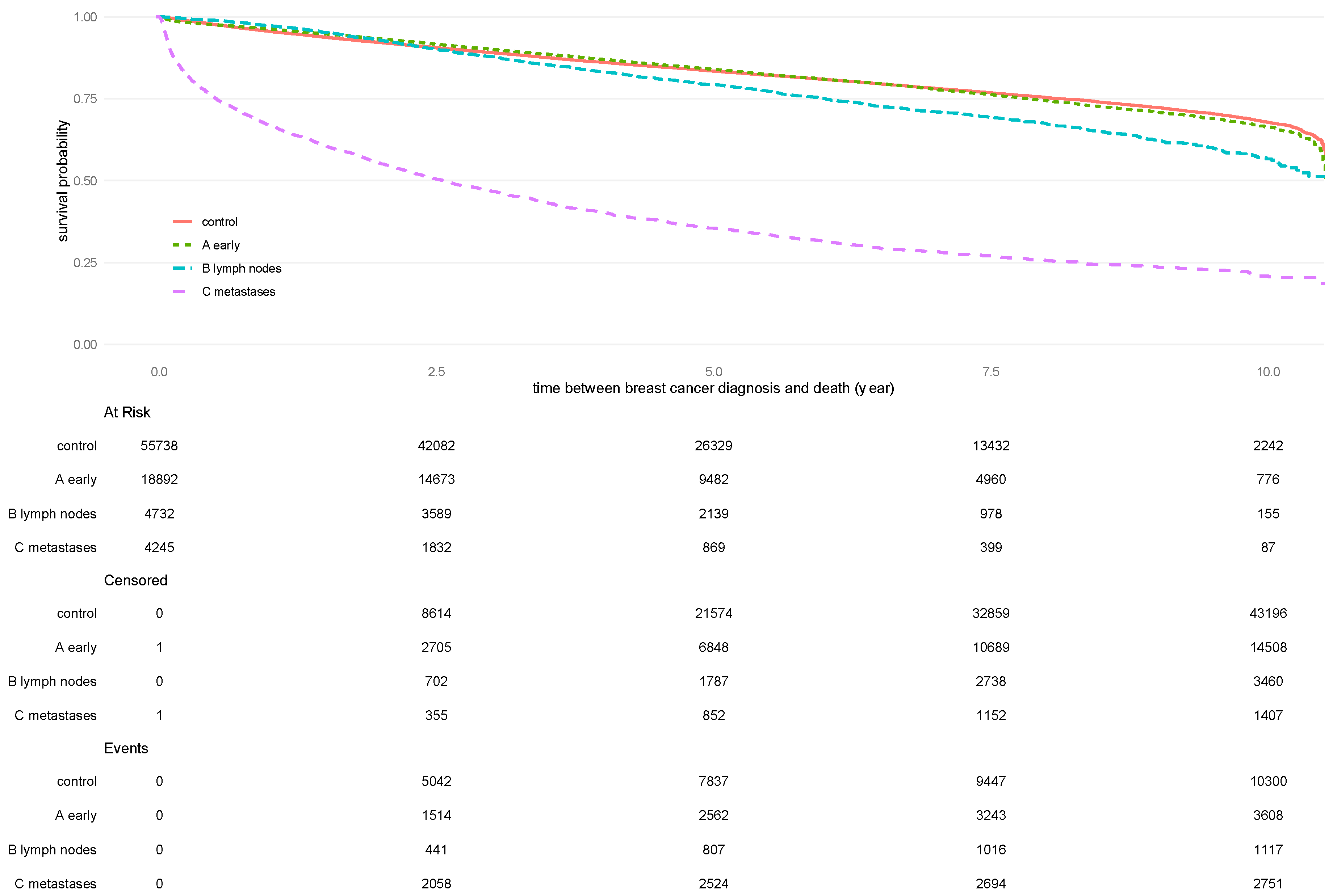
| Stage | ||
| A | 18,892 | 67.8 |
| B | 4732 | 17.0 |
| C | 4245 | 15.2 |
| Breast surgery | ||
| yes | 22,337 | 80.1 |
| no | 5532 | 19.9 |
| Radiation therapy | ||
| yes | 16,425 | 58.9 |
| no | 11,444 | 41.1 |
| Systemic therapy | ||
| yes | 9182 | 32.9 |
| no | 18,687 | 67.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dannehl, D.; von Au, A.; Engler, T.; Volmer, L.L.; Gutsfeld, R.; Englisch, J.F.; Hahn, M.; Hawighorst-Knapstein, S.; Chaudhuri, A.; Bauer, A.; et al. Implementation and Evaluation of a Breast Cancer Disease Model Using Real-World Claims Data in Germany from 2010 to 2020. Cancers 2024, 16, 1490. https://doi.org/10.3390/cancers16081490
Dannehl D, von Au A, Engler T, Volmer LL, Gutsfeld R, Englisch JF, Hahn M, Hawighorst-Knapstein S, Chaudhuri A, Bauer A, et al. Implementation and Evaluation of a Breast Cancer Disease Model Using Real-World Claims Data in Germany from 2010 to 2020. Cancers. 2024; 16(8):1490. https://doi.org/10.3390/cancers16081490
Chicago/Turabian StyleDannehl, Dominik, Alexandra von Au, Tobias Engler, Léa Louise Volmer, Raphael Gutsfeld, Johannes Felix Englisch, Markus Hahn, Sabine Hawighorst-Knapstein, Ariane Chaudhuri, Armin Bauer, and et al. 2024. "Implementation and Evaluation of a Breast Cancer Disease Model Using Real-World Claims Data in Germany from 2010 to 2020" Cancers 16, no. 8: 1490. https://doi.org/10.3390/cancers16081490
APA StyleDannehl, D., von Au, A., Engler, T., Volmer, L. L., Gutsfeld, R., Englisch, J. F., Hahn, M., Hawighorst-Knapstein, S., Chaudhuri, A., Bauer, A., Wallwiener, M., Taran, F.-A., Wallwiener, D., Brucker, S. Y., Wallwiener, S., Hartkopf, A. D., & Dijkstra, T. M. H. (2024). Implementation and Evaluation of a Breast Cancer Disease Model Using Real-World Claims Data in Germany from 2010 to 2020. Cancers, 16(8), 1490. https://doi.org/10.3390/cancers16081490







