Posterior and Para-Aortic (D2plus) Lymphadenectomy after Neoadjuvant/Conversion Therapy for Locally Advanced/Oligometastatic Gastric Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Preoperative Work-up and Chemotherapy
2.3. Surgical Treatment
2.4. Lymph Node Mapping and Pathological Classifications
2.5. Additional Treatments and Follow-Up
2.6. Statistical Analysis
3. Results
3.1. Clinicopathological Characteristics and Preoperative Chemotherapy
3.2. Surgical Treatment and Lymphadenectomy
3.3. Metastases to Posterior and Para-Aortic Lymph Nodes
3.4. Early Postoperative Outcomes
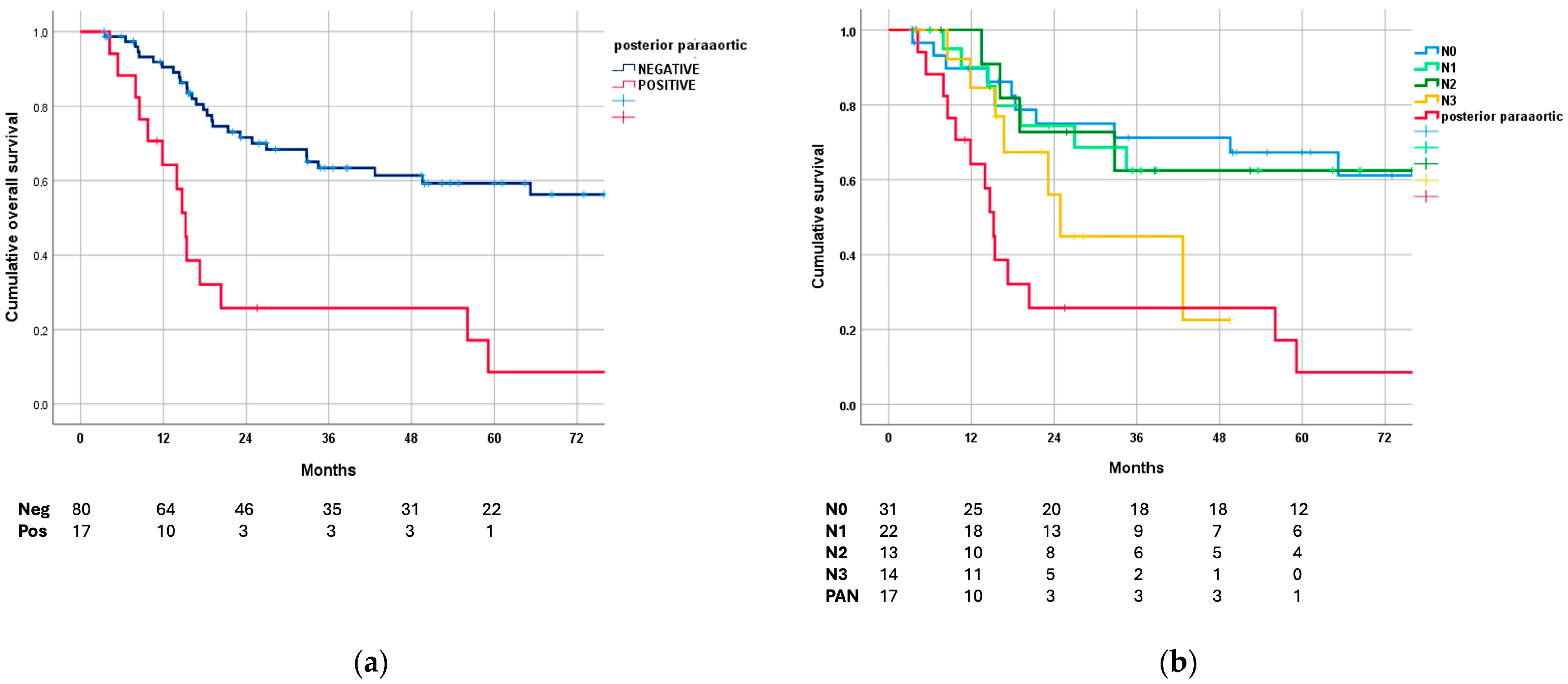
3.5. Long-Term Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Manzoni, G.; Marrelli, D.; Baiocchi, G.L.; Morgagni, P.; Saragoni, L.; Degiuli, M.; Donini, A.; Fumagalli, U.; Mazzei, M.A.; Pacelli, F.; et al. The Italian Research Group for Gastric Cancer (GIRCG) Guidelines for Gastric Cancer Staging and Treatment: 2015. Gastric Cancer 2017, 20, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Japanese Gastric Cancer Association. Japanese Gastric Cancer Treatment Guidelines 2021, 6th ed.; In Gastric Cancer; Springer: Berlin/Heidelberg, Germany, 2023; Volume 26, pp. 1–25. [Google Scholar] [CrossRef]
- Lordick, F.; Carneiro, F.; Cascinu, S.; Fleitas, T.; Haustermans, K.; Piessen, G.; Vogel, A.; Smyth, E.C. Gastric Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2022, 33, 1005–1020. [Google Scholar] [CrossRef] [PubMed]
- Sasako, M.; Sano, T.; Yamamoto, S.; Kurokawa, Y.; Nashimoto, A.; Kurita, A.; Hiratsuka, M.; Tsujinaka, T.; Kinoshita, T.; Arai, K.; et al. D2 Lymphadenectomy Alone or with Para-Aortic Nodal Dissection for Gastric Cancer. N. Engl. J. Med. 2008, 359, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Tokunaga, M.; Ohyama, S.; Hiki, N.; Fukunaga, T.; Aikou, S.; Yamaguchi, T. Can Superextended Lymph Node Dissection Be Justified for Gastric Cancer with Pathologically Positive Para-Aortic Lymph Nodes? Ann. Surg. Oncol. 2010, 17, 2031–2036. [Google Scholar] [CrossRef] [PubMed]
- Morita, S.; Fukagawa, T.; Fujiwara, H.; Katai, H. The Clinical Significance of Para-Aortic Nodal Dissection for Advanced Gastric Cancer. Eur. J. Surg. Oncol. 2016, 42, 1448–1454. [Google Scholar] [CrossRef]
- Marrelli, D.; Ferrara, F.; Giacopuzzi, S.; Morgagni, P.; Di Leo, A.; De Franco, L.; Pedrazzani, C.; Saragoni, L.; De Manzoni, G.; Roviello, F. Incidence and Prognostic Value of Metastases to “Posterior” and Para-Aortic Lymph Nodes in Resectable Gastric Cancer. Ann. Surg. Oncol. 2017, 24, 2273–2280. [Google Scholar] [CrossRef] [PubMed]
- Shen, D.-F.; Chen, D.-W.; Quan, Z.-W.; Dong, P.; Wang, X.-F.; Xy, H.-Z.; Zhao, M.-L.; Chen, L. Dissection of No. 13 Lymph Node in Radical Gastrectomy for Gastric Carcinoma. World J. Gastroenterol. 2008, 14, 936. [Google Scholar] [CrossRef][Green Version]
- Ji, X.; Bu, Z.-D.; Yan, Y.; Li, Z.-Y.; Wu, A.-W.; Zhang, L.-H.; Zhang, J.; Wu, X.-J.; Zong, X.-L.; Li, S.-X.; et al. The 8th Edition of the American Joint Committee on Cancer Tumor-Node-Metastasis Staging System for Gastric Cancer Is Superior to the 7th Edition: Results from a Chinese Mono-Institutional Study of 1663 Patients. Gastric Cancer 2018, 21, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Han, D.-S.; Suh, Y.-S.; Kong, S.-H.; Lee, H.-J.; Choi, Y.; Aikou, S.; Sano, T.; Park, B.-J.; Kim, W.-H.; Yang, H.-K. Nomogram Predicting Long-Term Survival After D2 Gastrectomy for Gastric Cancer. J. Clin. Oncol. 2012, 30, 3834–3840. [Google Scholar] [CrossRef]
- In, H.; Solsky, I.; Palis, B.; Langdon-Embry, M.; Ajani, J.; Sano, T. Validation of the 8th Edition of the AJCC TNM Staging System for Gastric Cancer Using the National Cancer Database. Ann. Surg. Oncol. 2017, 24, 3683–3691. [Google Scholar] [CrossRef]
- Yoshida, K.; Yasufuku, I.; Terashima, M.; Young Rha, S.; Moon Bae, J.; Li, G.; Katai, H.; Watanabe, M.; Seto, Y.; Hoon Noh, S.; et al. International Retrospective Cohort Study of Conversion Therapy for Stage IV Gastric Cancer 1 (CONVO-GC-1). Ann. Gastroenterol. Surg. 2022, 6, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, J.; Yamaguchi, T.; Moriyama, H.; Fushida, S. Current Status of Conversion Surgery for Stage IV Gastric Cancer. Surg. Today 2021, 51, 1736–1754. [Google Scholar] [CrossRef] [PubMed]
- Chevallay, M.; Wassmer, C.-H.; Iranmanesh, P.; Jung, M.K.; Mönig, S.P. Multimodal Treatment in Oligometastatic Gastric Cancer. World J. Gastrointest. Oncol. 2022, 14, 434–449. [Google Scholar] [CrossRef] [PubMed]
- Hojo, Y.; Ishida, Y.; Tomita, T.; Kurahashi, Y.; Nakamura, T.; Kitayama, Y.; Nakao, E.; Kohno, S.; Murakami, M.; Takeuchi, J.; et al. Treatment Strategy for Successful Conversion Surgery in Clinical Stage IVB Gastric Cancer. Eur. J. Surg. Oncol. 2024, 50, 107314. [Google Scholar] [CrossRef] [PubMed]
- Tsuburaya, A.; Mizusawa, J.; Tanaka, Y.; Fukushima, N.; Nashimoto, A.; Sasako, M. Neoadjuvant Chemotherapy with S-1 and Cisplatin Followed by D2 Gastrectomy with Para-Aortic Lymph Node Dissection for Gastric Cancer with Extensive Lymph Node Metastasis. Br. J. Surg. 2014, 101, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Takahari, D.; Ito, S.; Mizusawa, J.; Katayama, H.; Terashima, M.; Sasako, M.; Morita, S.; Nomura, T.; Yamada, M.; Fujiwara, Y.; et al. Long-Term Outcomes of Preoperative Docetaxel with Cisplatin plus S-1 Therapy for Gastric Cancer with Extensive Nodal Metastasis (JCOG1002). Gastric Cancer 2020, 23, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Ri, M.; Ohashi, M.; Eto, K.; Ishizuka, N.; Atsumi, S.; Makuuchi, R.; Ida, S.; Kumagai, K.; Sano, T.; Nunobe, S. Favorable Outcomes of Neoadjuvant Chemotherapy and Limited Para-Aortic Lymph Node Dissection for Advanced Gastric Cancer with Para-aortic Lymph Node Metastasis. World J. Surg. 2021, 45, 2849–2859. [Google Scholar] [CrossRef] [PubMed]
- Hara, K.; Cho, H.; Onodera, A.; Endo, K.; Maezawa, Y.; Aoyama, T.; Yamada, T.; Oshima, T.; Rino, Y. Long-term Treatment Outcomes in Gastric Cancer with Oligometastasis. Ann. Gastroenterol. Surg. 2024, 8, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Hikage, M.; Fujiya, K.; Kamiya, S.; Tanizawa, Y.; Bando, E.; Notsu, A.; Terashima, M. Prognostic Factors in Patients Who Received Paraaortic Lymph Node Dissection for Locally Advanced Gastric Cancer with Extensive Lymph Node Metastasis. Langenbeck’s Arch. Surg. 2022, 407, 1027–1037. [Google Scholar] [CrossRef]
- Kurokawa, Y.; Doki, Y.; Kitabayashi, R.; Yoshikawa, T.; Nomura, T.; Tsuji, K.; Goto, M.; Cho, H.; Hihara, J.; Hiki, N.; et al. Short-Term Outcomes of Preoperative Chemotherapy with Docetaxel, Oxaliplatin, and S-1 for Gastric Cancer with Extensive Lymph Node Metastasis (JCOG1704). In Gastric Cancer; Springer: Berlin/Heidelberg, Germany, 2024. [Google Scholar] [CrossRef]
- Marrelli, D.; Pedrazzani, C.; Neri, A.; Corso, G.; De Stefano, A.; Pinto, E.; Roviello, F. Complications after Extended (D2) and Superextended (D3) Lymphadenectomy for Gastric Cancer: Analysis of Potential Risk Factors. Ann. Surg. Oncol. 2007, 14, 25–33. [Google Scholar] [CrossRef]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A. The 2019 WHO Classification of Tumours of the Digestive System. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Marrelli, D.; Polom, K.; Pascale, V.; Vindigni, C.; Piagnerelli, R.; De Franco, L.; Ferrara, F.; Roviello, G.; Garosi, L.; Petrioli, R.; et al. Strong Prognostic Value of Microsatellite Instability in Intestinal Type Non-Cardia Gastric Cancer. Ann. Surg. Oncol. 2016, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; Van de Velde, C.J.H.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative Chemotherapy versus Surgery Alone for Resectable Gastroesophageal Cancer. N. Engl. J. Med. 2006, 355, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Al-Batran, S.-E.; Homann, N.; Pauligk, C.; Goetze, T.O.; Meiler, J.; Kasper, S.; Kopp, H.-G.; Mayer, F.; Haag, G.M.; Luley, K.; et al. Perioperative Chemotherapy with Fluorouracil plus Leucovorin, Oxaliplatin, and Docetaxel versus Fluorouracil or Capecitabine plus Cisplatin and Epirubicin for Locally Advanced, Resectable Gastric or Gastro-Oesophageal Junction Adenocarcinoma (FLOT4): A Randomised, Phase 2/3 Trial. Lancet 2019, 393, 1948–1957. [Google Scholar] [CrossRef] [PubMed]
- Siewert, J.R.; Böttcher, K.; Stein, H.J.; Roder, J.D. Relevant Prognostic Factors in Gastric Cancer. Ann. Surg. 1998, 228, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q. Effects of Extended Lymphadenectomy and Postoperative Chemotherapy on Node-Negative Gastric Cancer. World J. Gastroenterol. 2013, 19, 5551. [Google Scholar] [CrossRef]
- Songun, I.; Putter, H.; Kranenbarg, E.M.-K.; Sasako, M.; van de Velde, C.J. Surgical Treatment of Gastric Cancer: 15-Year Follow-up Results of the Randomised Nationwide Dutch D1D2 Trial. Lancet Oncol. 2010, 11, 439–449. [Google Scholar] [CrossRef] [PubMed]
- Degiuli, M.; Reddavid, R.; Tomatis, M.; Ponti, A.; Morino, M.; Sasako, M.; Rebecchi, F.; Garino, M.; Vigano, L.; Scaglione, D.; et al. D2 Dissection Improves Disease-Specific Survival in Advanced Gastric Cancer Patients: 15-Year Follow-up Results of the Italian Gastric Cancer Study Group D1 versus D2 Randomised Controlled Trial. Eur. J. Cancer 2021, 150, 10–22. [Google Scholar] [CrossRef]
- Claassen, Y.H.M.; Hartgrink, H.H.; Dikken, J.L.; de Steur, W.O.; van Sandick, J.W.; van Grieken, N.C.T.; Cats, A.; Trip, A.K.; Jansen, E.P.M.; Meershoek-Klein Kranenbarg, W.M.; et al. Surgical Morbidity and Mortality after Neoadjuvant Chemotherapy in the CRITICS Gastric Cancer Trial. Eur. J. Surg. Oncol. 2018, 44, 613–619. [Google Scholar] [CrossRef]
- Bracale, U.; Corcione, F.; Pignata, G.; Andreuccetti, J.; Dolce, P.; Boni, L.; Cassinotti, E.; Olmi, S.; Uccelli, M.; Gualtierotti, M.; et al. Impact of Neoadjuvant Therapy Followed by Laparoscopic Radical Gastrectomy with D2 Lymph Node Dissection in Western Population: A Multi-institutional Propensity Score-matched Study. J. Surg. Oncol. 2021, 124, 1338–1346. [Google Scholar] [CrossRef]
- Marano, L.; Carbone, L.; Poto, G.E.; Restaino, V.; Piccioni, S.A.; Verre, L.; Roviello, F.; Marrelli, D. Extended Lymphadenectomy for Gastric Cancer in the Neoadjuvant Era: Current Status, Clinical Implications and Contentious Issues. Curr. Oncol. 2023, 30, 875–896. [Google Scholar] [CrossRef]
- Monti, M.; Morgagni, P.; Nanni, O.; Framarini, M.; Saragoni, L.; Marrelli, D.; Roviello, F.; Petrioli, R.; Fumagalli Romario, U.; Rimassa, L.; et al. Preoperative or Perioperative Docetaxel, Oxaliplatin, and Capecitabine (GASTRODOC Regimen) in Patients with Locally-Advanced Resectable Gastric Cancer: A Randomized Phase-II Trial. Cancers 2020, 12, 2790. [Google Scholar] [CrossRef] [PubMed]
- Kroese, T.E.; Christ, S.M.; van Rossum, P.S.N.; Burger, M.D.L.; Buijs, G.S.; Mühlematter, U.; Andratschke, N.; Ruurda, J.P.; Hüllner, M.; Gutschow, C.A.; et al. Incidence and Survival of Patients with Oligometastatic Esophagogastric Cancer: A Multicenter Cohort Study. Radiother Oncol. 2022, 173, 269–276. [Google Scholar] [CrossRef]
- Bencivenga, M.; Treppiedi, E.; Dal Cero, M.; Torroni, L.; Verlato, G.; Iglesias, M.; Renaud, F.; Tomezzoli, A.; Castelli, C.; Piessen, G.; et al. The Amount of Signet Ring Cells Is Significantly Associated with Tumour Stage and Survival in Gastric Poorly Cohesive Tumours. J. Surg. Oncol. 2020, 121, 1084–1089. [Google Scholar] [CrossRef] [PubMed]
- Blumenthaler, A.N.; Newhook, T.E.; Ikoma, N.; Estrella, J.S.; Blum Murphy, M.; Das, P.; Minsky, B.D.; Ajani, J.A.; Mansfield, P.F.; Badgwell, B.D. Concurrent Lymphovascular and Perineural Invasion after Preoperative Therapy for Gastric Adenocarcinoma Is Associated with Decreased Survival. J. Surg. Oncol. 2021, 123, 911–922. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, K.; Hatakeyama, K.; Terashima, M.; Nagashima, T.; Urakami, K.; Ohshima, K.; Notsu, A.; Sugino, T.; Yagi, T.; Fujiya, K.; et al. Molecular Classification of Gastric Cancer Predicts Survival in Patients Undergoing Radical Gastrectomy Based on Project HOPE. Gastric Cancer 2022, 25, 138–148. [Google Scholar] [CrossRef]
- Marrelli, D.; Marano, L.; Ambrosio, M.R.; Carbone, L.; Spagnoli, L.; Petrioli, R.; Ongaro, A.; Piccioni, S.; Fusario, D.; Roviello, F. Immunohistochemical Markers of the Epithelial-to-Mesenchymal Transition (EMT) Are Related to Extensive Lymph Nodal Spread, Peritoneal Dissemination, and Poor Prognosis in the Microsatellite-Stable Diffuse Histotype of Gastric Cancer. Cancers 2022, 14, 6023. [Google Scholar] [CrossRef]

| Characteristics | No. (%) |
|---|---|
| Age [IQR] | 65 (26–83) |
| Gender | |
| Male | 64 (66) |
| Female | 33 (34) |
| Location | |
| Upper | 23 (23.7) |
| Middle | 23 (23.7) |
| Lower | 43 (44.3) |
| Linitis | 8 (8.3) |
| Clinical Stage | |
| II | 14 (14.4) |
| III | 48 (49.5) |
| IV | 35 (36.1) |
| Lauren Classification | |
| Intestinal | 45 (46.4) |
| Diffuse/mixed | 47 (48.5) |
| NC | 5 (5.1) |
| WHO Classification | |
| Mucinous | 5 (5.2) |
| Tubular/papillary | 40 (41.2) |
| Poorly cohesive-non SRC | 13 (13.4) |
| Poorly cohesive-SRC | 34 (35.1) |
| NC | 5 (5.1) |
| Her2 Status | |
| Neg | 87 (89.7) |
| Pos | 9 (9.3) |
| NA | 1 (1.0) |
| Microsatellite Status | |
| MSS | 90 (92.8) |
| MSI | 5 (5.1) |
| NA | 2 (2.1) |
| Chemotherapy | |
| DOX/FLOT | 63 (64.9) |
| ECF/EOX | 19 (19.6) |
| FOLFOX | 6 (6.2) |
| Others | 9 (9.3) |
| No. Chemotherapy cycles | |
| 2–4 | 77 (79.4) |
| 5–8 | 14 (14.4) |
| >8 | 6 (6.2) |
| Clinical Restaging | |
| CR | 4 (4.1) |
| PR | 52 (53.6) |
| SD | 37 (38.2) |
| PD | 4 (4.1) |
| Gastrectomy | |
| Total | 52 (53.6) |
| Subtotal | 45 (46.4) |
| Extended organ Resection | |
| Performed | 12 (12.4) |
| Not performed | 85 (86.6) |
| UICC R | |
| R0 | 66 (68) |
| R1 | 20 (20.6) |
| R2 | 11 (11.4) |
| Lymphovascular Invasion | |
| Present | 56 (57.7) |
| Absent | 41 (42.3) |
| Perineural Invasion | |
| Present | 49 (50.5) |
| Absent | 48 (49.5) |
| Pathological Stage | |
| 0 | 7 (7.2) |
| I | 12 (12.4) |
| II | 25 (25.8) |
| III | 23 (23.7) |
| IV | 30 (30.9) |
| ypT | |
| 0 | 9 (9.3) |
| 1 | 4 (4.1) |
| 2 | 13 (13.4) |
| 3 | 22 (22.7) |
| 4 | 49 (50.5) |
| ypN | |
| 0 | 31 (32.0) |
| 1 | 22 (22.7) |
| 2 | 16 (16.5) |
| 3a | 15 (15.4) |
| 3b | 13 (13.4) |
| yM | |
| 0 | 67 (69.2) |
| M1 (cy+, peritoneal) | 16 (16.4) |
| M1 (hematogenous) | 5 (5.1) |
| M1 (extra-regional nodes) | 9 1 (9.3) |
| Becker Regression Grade | |
| 1 | 17 (17.5) |
| 2 | 23 (23.8) |
| 3 | 49 (50.5) |
| NA | 8 (8.2) |
| Characteristics | Posterior/Para-Aortic Lymph Node Metastasis Negative (No. = 80) No. (%) | Posterior/Para-Aortic Lymph Node Metastasis Positive (No. = 17) No. (%) | p |
|---|---|---|---|
| Age | 0.965 | ||
| <55 | 17 (85) | 3 (15) | |
| 55–64 | 22 (81.5) | 5 (18.5) | |
| 65–74 | 30 (83.3) | 6 (16.7) | |
| 75–84 | 11 (78.6) | 3 (21.4) | |
| Gender | 0.903 | ||
| Male | 53 (82.8) | 11 (17.2) | |
| Female | 27 (81.8) | 6 (18.2) | |
| Location | 0.882 | ||
| Upper | 19 (82.6) | 4 (17.4) | |
| Middle | 20 (87) | 3 (13) | |
| Lower | 35 (81.4) | 8 (18.6) | |
| Linitis | 6 (75) | 2 (25) | |
| Clinical Stage | <0.001 | ||
| II | 14 (100) | 0 (0) | |
| III | 46 (95.8) | 2 (4.2) | |
| IV | 20 (57.1) | 15 (42.9) | |
| Lauren Classification | 0.255 | ||
| Intestinal | 39 (86.7) | 6 (13.3) | |
| Diffuse/mixed | 36 (76.6) | 11 (23.4) | |
| NC | 5 (100) | 0 (0) | |
| WHO Classification | 0.489 | ||
| Mucinous | 5 (100) | 0 (0) | |
| Tubular/papillary | 34 (85) | 6 (15) | |
| Poorly cohesive-non SRC | 10 (76.9) | 3 (23.1) | |
| Poorly cohesive-SRC | 26 (76.5) | 8 (23.5) | |
| NC | 5 (100) | 0 (0) | |
| Her-2 Status | 0.873 | ||
| Neg | 72 (82.8) | 15 (17.2) | |
| Pos | 7 (77.8) | 2 (22.2) | |
| NA | 1 (100) | 0 (0) | |
| Microsatellite Status | 0.178 | ||
| MSS | 76 (84.4) | 14 (15.6) | |
| MSI | 3 (60) | 2 (40) | |
| NA | 1 (50) | 1 (50) | |
| Lymphovascular Invasion | 0.005 | ||
| Present | 41 (73.2) | 15 (26.8) | |
| Absent | 39 (92.1) | 2 (4.9) | |
| Perineural Invasion | 0.018 | ||
| Present | 36 (73.5) | 13 (26.5) | |
| Absent | 44 (91.7) | 4 (8.3) | |
| ypT | 0.322 | ||
| 0 | 9 (100) | 0 (0) | |
| 1 | 4 (100) | 0 (0) | |
| 2 | 11 (84.6) | 2 (15.4) | |
| 3 | 19 (86.4) | 3 (13.6) | |
| 4 | 37 (75.5) | 12 (24.5) | |
| ypN | <0.001 | ||
| 0 | 31 (100) | 0 (0) | |
| 1 | 22 (100) | 0 (0) | |
| 2 | 13 (81.25) | 3 (18.75) | |
| 3a | 8 (53.3) | 7 (46.7) | |
| 3b | 6 (46.2) | 7 (53.8) | |
| Becker | 0.236 | ||
| 1 | 16 (94.1) | 1 (5.9) | |
| 2 | 19 (82.6) | 4 (17.4) | |
| 3 | 37 (75.5) | 12 (24.5) | |
| NA | 8 (100) | 0 (0) |
| Complications | No. (%) | Grade II 1 | Grades III–IV 1 | Treatment |
|---|---|---|---|---|
| SURGICAL | 10 (10.3) | 6 | 4 | |
| Anastomotic leakage | 7 (7.2) | 3 | 4 | Medical (4), surgery (2), other intervention (1) |
| Abdominal abscess | 2 (2.1) | 2 | 0 | Conservative (2) |
| Lymphocele | 1 (1.0) | 1 | 0 | Conservative (2) |
| MEDICAL | 11 (11.3) | 3 | 5 | |
| Pleuro-pulmonary | 7 (7.2) | 3 | 4 | Pharmacological (7) |
| Cardiovascular | 2 (2.1) | 1 | 1 ** | Pharmacological (1), death (1) |
| Acute renal failure | 2 (2.1) | 2 | 0 | Pharmacological (2) |
| 90-day morbidity | 21 (21.6) | 12 | 9 | |
| 30-day mortality | 1 (1.0) | |||
| Hospital stay (days) 2 | 15 ± 2 * |
| Characteristics | No. | Median Survival (Months, 95% CI) | 5-Year Survival Rate (% ± SE) | p |
|---|---|---|---|---|
| Age | 0.580 | |||
| <65 | 50 | 34 (21–62) | 46 ± 8 | |
| >65 | 47 | 65 (26–104) | 54 ± 9 | |
| Gender | 0.894 | |||
| Male | 33 | 56 (20–88) | 47 ± 10 | |
| Female | 64 | 65 (9–120) | 50 ± 7 | |
| Location | <0.001 | |||
| Upper | 23 | 19 (16–22) | 33 ± 10 | |
| Middle | 23 | NR | 58 ± 12 | |
| Lower | 43 | NR | 66 ± 9 | |
| Linitis | 8 | 15 (13–18) | 0 | |
| Clinical Stage | 0.006 | |||
| II | 14 | NR | 70 ± 15 | |
| III | 48 | NR | 61 ± 8 | |
| IV | 35 | 19 (12–26) | 23 ± 10 | |
| Lauren Classification 1 | 0.273 | |||
| Intestinal | 45 | 85 (39–120) | 55 ± 8 | |
| Diffuse/Mixed | 47 | 43 (10–75) | 42 ± 9 | |
| WHO Classification 1 | 0.738 | |||
| Tubular/papillary | 40 | 65 (23–108) | 52 ± 9 | |
| Poorly cohesive-non SRC | 13 | 35 (0–69) | 31 ± 16 | |
| Poorly cohesive-SRC | 34 | 43 (15–89) | 47 ± 10 | |
| Chemotherapy Schedule | 0.557 | |||
| DOX-FLOT | 63 | 84 (40–110) | 54 ± 7 | |
| ECF-EOX | 19 | 30 (10–43) | 32 ± 11 | |
| Others | 15 | NR | 61 ± 15 | |
| Clinical Restaging | 0.106 | |||
| CR+PR | 56 | 85 (40–105) | 56 ± 8 | |
| SD+PD | 41 | 25 (3–47) | 40 ± 9 | |
| Gastrectomy | 0.030 | |||
| Total | 52 | 27 (11–43) | 41 ± 7 | |
| Subtotal | 45 | NR | 60 ± 9 | |
| UICC R | <0.001 | |||
| 0 | 69 | NR | 60 ± 7 | |
| 1 | 18 | 23 (6–40) | 31 ± 13 | |
| 2 | 10 | 14 (8–20) | 0 | |
| Lymphovascular Invasion | 0.040 | |||
| Present | 56 | 27 (5–49) | 37 ± 8 | |
| Absent | 41 | NR | 63 ± 8 | |
| Perineural Invasion | 0.004 | |||
| Present | 49 | 21 (12–30) | 31 ± 8 | |
| Absent | 48 | NR | 57 ± 9 | |
| ypT | 0.025 | |||
| 0 | 9 | NR | 67 ± 16 | |
| 1–2 | 17 | NR | 80 ± 13 | |
| 3 | 22 | NR | 52 ± 13 | |
| 4 | 49 | 25 (10–40) | 34 ± 8 | |
| ypN | <0.001 | |||
| 0 | 31 | NR | 67 ± 9 | |
| 1 | 22 | 85 (40–110) | 62 ± 11 | |
| 2 | 16 | NR | 53 ± 14 | |
| 3 | 28 | 17 (11–22) | 0 | |
| Becker 1 | 0.306 | |||
| 1 | 17 | NR | 62 ± 15 | |
| 2 | 23 | 65 (10–120) | 48 ± 12 | |
| 3 | 49 | 34 (3–68) | 12 ± 8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marrelli, D.; Piccioni, S.A.; Carbone, L.; Petrioli, R.; Costantini, M.; Malagnino, V.; Bagnacci, G.; Rizzoli, G.; Calomino, N.; Piagnerelli, R.; et al. Posterior and Para-Aortic (D2plus) Lymphadenectomy after Neoadjuvant/Conversion Therapy for Locally Advanced/Oligometastatic Gastric Cancer. Cancers 2024, 16, 1376. https://doi.org/10.3390/cancers16071376
Marrelli D, Piccioni SA, Carbone L, Petrioli R, Costantini M, Malagnino V, Bagnacci G, Rizzoli G, Calomino N, Piagnerelli R, et al. Posterior and Para-Aortic (D2plus) Lymphadenectomy after Neoadjuvant/Conversion Therapy for Locally Advanced/Oligometastatic Gastric Cancer. Cancers. 2024; 16(7):1376. https://doi.org/10.3390/cancers16071376
Chicago/Turabian StyleMarrelli, Daniele, Stefania Angela Piccioni, Ludovico Carbone, Roberto Petrioli, Maurizio Costantini, Valeria Malagnino, Giulio Bagnacci, Gabriele Rizzoli, Natale Calomino, Riccardo Piagnerelli, and et al. 2024. "Posterior and Para-Aortic (D2plus) Lymphadenectomy after Neoadjuvant/Conversion Therapy for Locally Advanced/Oligometastatic Gastric Cancer" Cancers 16, no. 7: 1376. https://doi.org/10.3390/cancers16071376
APA StyleMarrelli, D., Piccioni, S. A., Carbone, L., Petrioli, R., Costantini, M., Malagnino, V., Bagnacci, G., Rizzoli, G., Calomino, N., Piagnerelli, R., Mazzei, M. A., & Roviello, F. (2024). Posterior and Para-Aortic (D2plus) Lymphadenectomy after Neoadjuvant/Conversion Therapy for Locally Advanced/Oligometastatic Gastric Cancer. Cancers, 16(7), 1376. https://doi.org/10.3390/cancers16071376









