Optimising Patient Outcomes in Tongue Cancer: A Multidisciplinary Approach
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Assembly of Multidisciplinary Expert Panel
2.2. Multidisciplinary Discussions and Literature Review
2.3. Development of Online Lectures
2.4. Synthesis of Findings
3. Results
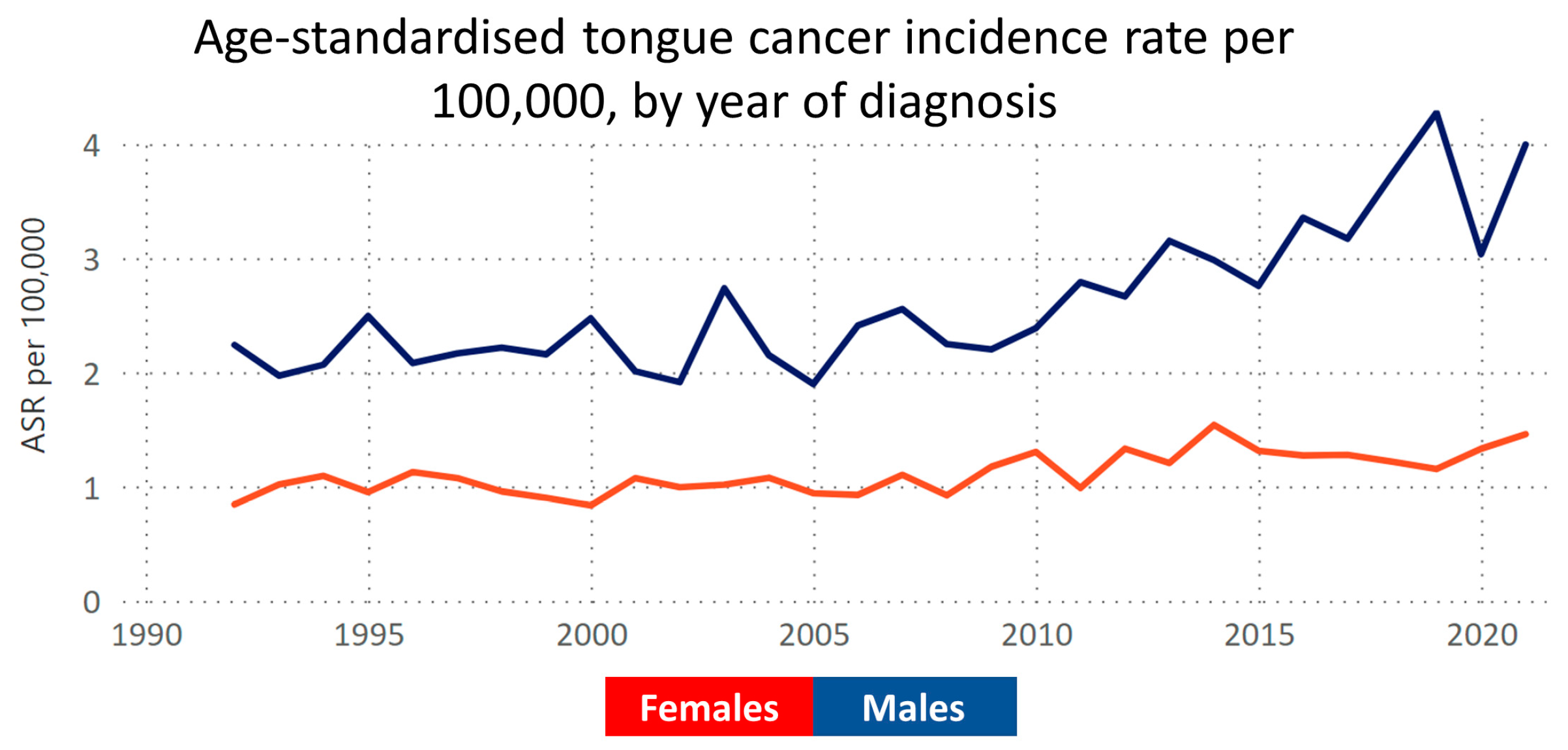
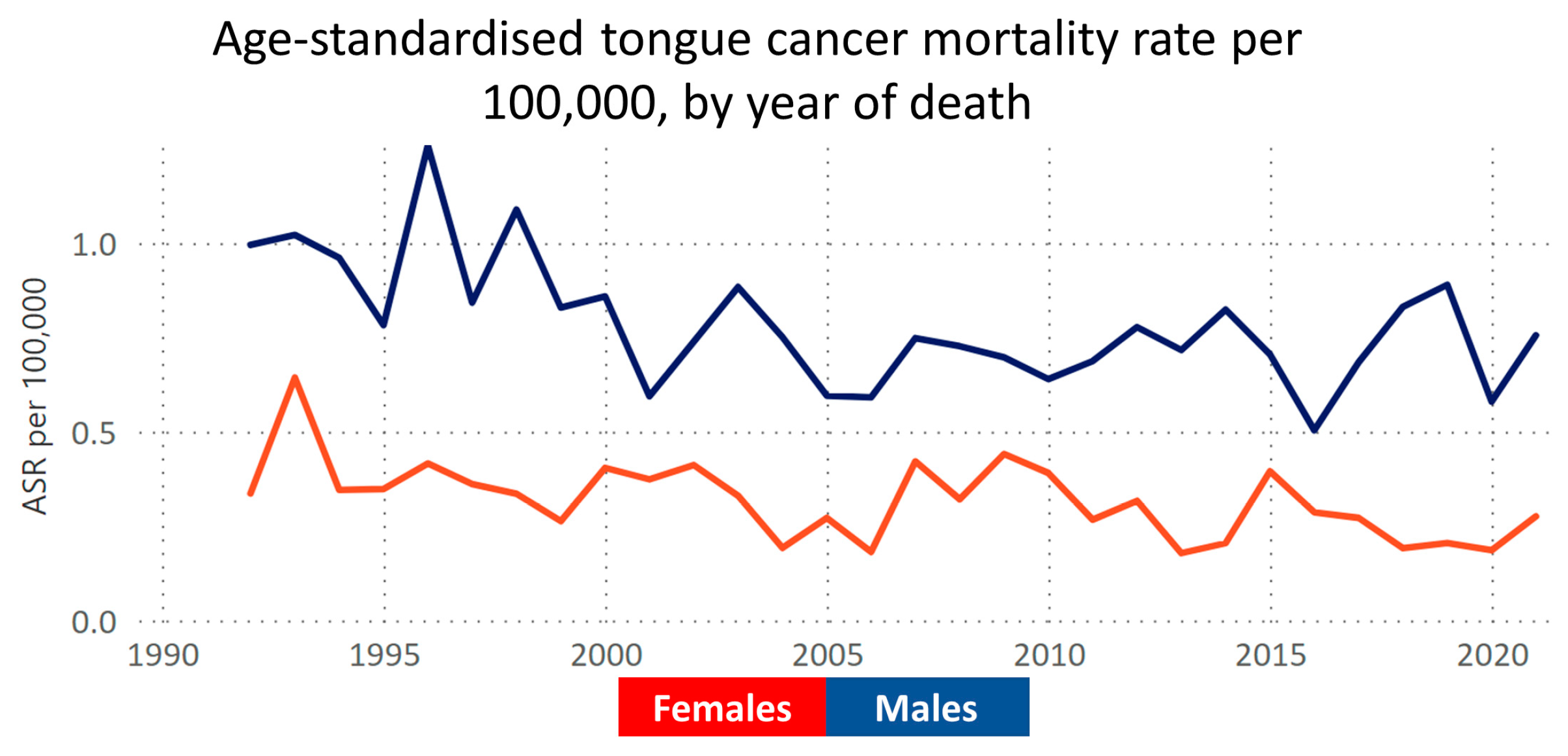
3.1. Epidemiology and Aetiology of Tongue Cancer
3.2. Applying the Optimal Care Pathway to Tongue Cancer
3.3. Disease Presentation, Referral Patterns, and COVID-19
3.4. Diagnosis, Staging, and Treatment Planning
3.5. Multidisciplinary Meetings
3.6. Preparing the Patient for Surgery
3.7. Supportive Care
3.8. Surgical Principles
3.9. Management of the Primary and Neck Nodes
3.10. Management of the Neck
3.11. Dealing with Treatment Failure
3.12. Reconstruction Techniques
3.13. Post-Surgical Recovery, Rehabilitation and Functional Outcomes
3.14. Systemic Therapies in Tongue Cancer
3.15. Radiation Oncology in Oral Tongue Cancer Treatment
3.16. Supportive Care and Survivorship
3.17. Support Groups
3.18. Managing Recurrent, Residual, or Metastatic Disease and Palliative Care
3.19. Future Research Outlook
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dew, K.; Stubbe, M.; Signal, L.; Stairmand, J.; Dennett, E.; Koea, J.; Simpson, A.; Sarfati, D.; Cunningham, C.; Batten, L.; et al. Cancer care decision making in multidisciplinary meetings. Qual. Health Res. 2015, 25, 397–407. [Google Scholar] [CrossRef] [PubMed]
- AIHW. Cancer in Australia. Available online: https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/cancer-summary-data-visualisation (accessed on 19 April 2023).
- Irani, S. New Insights into Oral Cancer-Risk Factors and Prevention: A Review of Literature. Int. J. Prev. Med. 2020, 11, 202. [Google Scholar] [CrossRef]
- CCA. VCR Data Explorer. Available online: https://www.cancervic.org.au/research/vcr (accessed on 19 April 2023).
- Centers for Disease, C. Smoking and cancer. MMWR Morb. Mortal. Wkly. Rep. 1982, 31, 77–80. [Google Scholar]
- Satgunaseelan, L.; Allanson, B.M.; Asher, R.; Reddy, R.; Low, H.T.H.; Veness, M.; Gopal Iyer, N.; Smee, R.I.; Palme, C.E.; Gupta, R.; et al. The incidence of squamous cell carcinoma of the oral tongue is rising in young non-smoking women: An international multi-institutional analysis. Oral. Oncol. 2020, 110, 104875. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, L.M.; Antonsson, A.; Garvey, G.; Ju, X.; Smith, M.; Logan, R.M.; Johnson, N.W.; Hedges, J.; Sethi, S.; Dunbar, T.; et al. Prevalence of Oral Human Papillomavirus Infection Among Australian Indigenous Adults. JAMA Netw. Open 2020, 3, e204951. [Google Scholar] [CrossRef] [PubMed]
- Cancer Council Victoria. Optimal Care Pathway for People with Head and Neck Cancer, 2nd ed.; Cancer Council Victoria: Melbourne, Australia, 2021. [Google Scholar]
- Bouaoud, J.; Bossi, P.; Elkabets, M.; Schmitz, S.; van Kempen, L.C.; Martinez, P.; Jagadeeshan, S.; Breuskin, I.; Puppels, G.J.; Hoffmann, C.; et al. Unmet Needs and Perspectives in Oral Cancer Prevention. Cancers 2022, 14, 1815. [Google Scholar] [CrossRef] [PubMed]
- Cancer Council Victoria. Cancer in Victoria 2022 Annual Report. Available online: https://www.cancervic.org.au/downloads/cec/cancer-in-vic/Cancer-in-Victoria-statistics-and-trends-2022.pdf?V=2 (accessed on 12 January 2024).
- Linz, C.; Brands, R.C.; Herterich, T.; Hartmann, S.; Muller-Richter, U.; Kubler, A.C.; Haug, L.; Kertels, O.; Bley, T.A.; Dierks, A.; et al. Accuracy of 18-F Fluorodeoxyglucose Positron Emission Tomographic/Computed Tomographic Imaging in Primary Staging of Squamous Cell Carcinoma of the Oral Cavity. JAMA Netw. Open 2021, 4, e217083. [Google Scholar] [CrossRef]
- Toh, H.J.; Low, J.A.; Lim, Z.Y.; Lim, Y.; Siddiqui, S.; Tan, L. Jonsen’s Four Topics Approach as a Framework for Clinical Ethics Consultation. Asian Bioeth. Rev. 2018, 10, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Clark, P.G.; Cott, C.; Drinka, T.J. Theory and practice in interprofessional ethics: A framework for understanding ethical issues in health care teams. J. Interprof. Care 2007, 21, 591–603. [Google Scholar] [CrossRef]
- Fitch, M.I. Supportive care framework. Can. Oncol. Nurs. J. 2008, 18, 6–24. [Google Scholar] [CrossRef]
- Cancer Council Australia. Evidence-Based Practice Guidelines for the Nutritional Management of Adult Patients with Head and Neck Cancer. Available online: https://wiki.cancer.org.au/australia/COSA:Head_and_neck_cancer_nutrition_guidelines (accessed on 12 January 2024).
- Megee, F.; Gough, K.; Frowen, J.; Dixon, B.; Magarey, M.; Wiesenfeld, D.; Ramakrishnan, A. Predictors of distress associated with altered appearance and function in people treated surgically for oral cancers: A cross-sectional study. Int. J. Oral Maxillofac. Surg. 2023, 52, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Daniell, J.; Udovicich, C.; Rowe, D.; McDowell, L.; Vital, D.; Bressel, M.; Magarey, M.J.R.; Iseli, T.A.; Wong, T.; Lekgabe, E.; et al. Impact of histological Oral Tongue Cancer margins on locoregional recurrence: A multi-centre retrospective analysis. Oral Oncol. 2020, 111, 105004. [Google Scholar] [CrossRef] [PubMed]
- D’Cruz, A.K.; Vaish, R.; Kapre, N.; Dandekar, M.; Gupta, S.; Hawaldar, R.; Agarwal, J.P.; Pantvaidya, G.; Chaukar, D.; Deshmukh, A.; et al. Elective versus Therapeutic Neck Dissection in Node-Negative Oral Cancer. N. Engl. J. Med. 2015, 373, 521–529. [Google Scholar] [CrossRef] [PubMed]
- DeAngelis, A.; Breik, O.; Koo, K.; Iseli, T.; Nastri, A.; Fua, T.; Rischin, D.; McCullough, M.; Wiesenfeld, D. Non-smoking, non-drinking elderly females, a 5 year follow-up of a clinically distinct cohort of oral squamous cell carcinoma patients. Oral Oncol. 2018, 86, 113–120. [Google Scholar] [CrossRef]
- Daniell, J.R.; Dolja-Gore, X.; McDowell, L.; Udovicich, C.; Rowe, D.; Iseli, T.A.; Wong, T.; Magarey, M.J.R.; Wiesenfeld, D. The impact of travel distance to treatment centre on oral tongue squamous cell carcinoma survival and recurrence. Int. J. Oral Maxillofac. Surg. 2022, 51, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.J.; Guiney, A.; Iseli, C.E.; Buchanan, M.; Iseli, T.A. Prophylactic neck dissection in early oral tongue squamous cell carcinoma 2.1 to 4.0 mm depth. Otolaryngol. Head Neck Surg. 2011, 144, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Russo, E.; Alessandri-Bonetti, M.; Costantino, A.; Festa, B.M.; Egro, F.M.; Giannitto, C.; Spriano, G.; De Virgilio, A. Functional outcomes and complications of total glossectomy with laryngeal preservation and flap reconstruction: A systematic review and meta-analysis. Oral Oncol. 2023, 141, 106415. [Google Scholar] [CrossRef]
- Halczy-Kowalik, L.; Wiktor, A.; Rzewuska, A.; Kowalczyk, R.; Wysocki, R.; Posio, V. Compensatory Mechanisms in Patients After a Partial or Total Glossectomy due to Oral Cancer. Dysphagia 2015, 30, 738–750. [Google Scholar] [CrossRef]
- Lam, L.; Samman, N. Speech and swallowing following tongue cancer surgery and free flap reconstruction—A systematic review. Oral Oncol. 2013, 49, 507–524. [Google Scholar] [CrossRef]
- Philiponis, G.; Kagan, S.H. Speaking legibly: Qualitative perceptions of altered voice among oral tongue cancer survivors. Asia Pac. J. Oncol. Nurs. 2015, 2, 250–256. [Google Scholar] [CrossRef]
- Dzioba, A.; Aalto, D.; Papadopoulos-Nydam, G.; Seikaly, H.; Rieger, J.; Wolfaardt, J.; Osswald, M.; Harris, J.R.; O’Connell, D.A.; Lazarus, C.; et al. Functional and quality of life outcomes after partial glossectomy: A multi-institutional longitudinal study of the head and neck research network. J. Otolaryngol. Head Neck Surg. 2017, 46, 56. [Google Scholar] [CrossRef]
- Gane, E.M.; Michaleff, Z.A.; Cottrell, M.A.; McPhail, S.M.; Hatton, A.L.; Panizza, B.J.; O’Leary, S.P. Prevalence, incidence, and risk factors for shoulder and neck dysfunction after neck dissection: A systematic review. Eur. J. Surg. Oncol. 2017, 43, 1199–1218. [Google Scholar] [CrossRef]
- McGarvey, A.C.; Osmotherly, P.G.; Hoffman, G.R.; Chiarelli, P.E. Lymphoedema following treatment for head and neck cancer: Impact on patients, and beliefs of health professionals. Eur. J. Cancer Care 2014, 23, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Dort, J.C.; Farwell, D.G.; Findlay, M.; Huber, G.F.; Kerr, P.; Shea-Budgell, M.A.; Simon, C.; Uppington, J.; Zygun, D.; Ljungqvist, O.; et al. Optimal Perioperative Care in Major Head and Neck Cancer Surgery With Free Flap Reconstruction: A Consensus Review and Recommendations From the Enhanced Recovery After Surgery Society. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 292–303. [Google Scholar] [CrossRef] [PubMed]
- Shaw, L.M.; Iseli, T.A.; Wiesenfeld, D.; Ramakrishnan, A.; Granger, C.L. Postoperative pulmonary complications following major head and neck cancer surgery. Int. J. Oral Maxillofac. Surg. 2021, 50, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Pigott, A.; Nixon, J.; Fleming, J.; Porceddu, S. Head and neck lymphedema management: Evaluation of a therapy program. Head Neck 2018, 40, 1131–1137. [Google Scholar] [CrossRef]
- Ferris, R.L.; Blumenschein, G., Jr.; Fayette, J.; Guigay, J.; Colevas, A.D.; Licitra, L.; Harrington, K.; Kasper, S.; Vokes, E.E.; Even, C.; et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N. Engl. J. Med. 2016, 375, 1856–1867. [Google Scholar] [CrossRef]
- Burtness, B.; Rischin, D.; Greil, R.; Soulieres, D.; Tahara, M.; de Castro, G., Jr.; Psyrri, A.; Brana, I.; Baste, N.; Neupane, P.; et al. Pembrolizumab Alone or With Chemotherapy for Recurrent/Metastatic Head and Neck Squamous Cell Carcinoma in KEYNOTE-048: Subgroup Analysis by Programmed Death Ligand-1 Combined Positive Score. J. Clin. Oncol. 2022, 40, 2321–2332. [Google Scholar] [CrossRef]
- Machiels, J.P.; Tao, Y.; Burtness, B.; Tahara, M.; Rischin, D.; Alves, G.V.; Lima, I.P.F.; Hughes, B.G.M.; Pointreau, Y.; Aksoy, S.; et al. Primary results of the phase III KEYNOTE-412 study: Pembrolizumab (pembro) with chemoradiation therapy (CRT) vs placebo plus CRT for locally advanced (LA) head and neck squamous cell carcinoma (HNSCC). Ann. Oncol. 2022, 33, S1399. [Google Scholar] [CrossRef]
- Lee, N.Y.; Ferris, R.L.; Psyrri, A.; Haddad, R.I.; Tahara, M.; Bourhis, J.; Harrington, K.; Chang, P.M.; Lin, J.C.; Razaq, M.A.; et al. Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: A randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol. 2021, 22, 450–462. [Google Scholar] [CrossRef]
- Nenclares, P.; Rullan, A.; Tam, K.; Dunn, L.A.; St John, M.; Harrington, K.J. Introducing Checkpoint Inhibitors Into the Curative Setting of Head and Neck Cancers: Lessons Learned, Future Considerations. Am. Soc. Clin. Oncol. Educ. Book 2022, 42, 511–526. [Google Scholar] [CrossRef]
- Peters, L.J.; Goepfert, H.; Ang, K.K.; Byers, R.M.; Maor, M.H.; Guillamondegui, O.; Morrison, W.H.; Weber, R.S.; Garden, A.S.; Frankenthaler, R.A.; et al. Evaluation of the dose for postoperative radiation therapy of head and neck cancer: First report of a prospective randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 1993, 26, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Bernier, J.; Cooper, J.S.; Pajak, T.F.; van Glabbeke, M.; Bourhis, J.; Forastiere, A.; Ozsahin, E.M.; Jacobs, J.R.; Jassem, J.; Ang, K.K.; et al. Defining risk levels in locally advanced head and neck cancers: A comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head Neck 2005, 27, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Machiels, J.-P.; Leemans, C.R.; Golusinski, W.; Grau, C.; Licitra, L.; Gregoire, V. Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1462–1475. [Google Scholar] [CrossRef] [PubMed]
- Koyfman, S.A.; Ismaila, N.; Crook, D.; D’Cruz, A.; Rodriguez, C.P.; Sher, D.J.; Silbermins, D.; Sturgis, E.M.; Tsue, T.T.; Weiss, J.; et al. Management of the Neck in Squamous Cell Carcinoma of the Oral Cavity and Oropharynx: ASCO Clinical Practice Guideline. J. Clin. Oncol. 2019, 37, 1753–1774. [Google Scholar] [CrossRef] [PubMed]
- Ganly, I.; Goldstein, D.; Carlson, D.L.; Patel, S.G.; O’Sullivan, B.; Lee, N.; Gullane, P.; Shah, J.P. Long-term regional control and survival in patients with “low-risk”, early stage oral tongue cancer managed by partial glossectomy and neck dissection without postoperative radiation: The importance of tumor thickness. Cancer 2013, 119, 1168–1176. [Google Scholar] [CrossRef]
- McLaughlin, T.M.; Broadhurst, J.J.; Harris, C.J.; McGarry, S.; Keesing, S.L. A randomized pilot study on self-management in head and neck lymphedema. Laryngoscope Investig. Otolaryngol. 2020, 5, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.C.; Huang, B.S.; Hung, T.M.; Chang, Y.L.; Lin, C.Y.; Chung, C.Y.; Wu, S.C. Swallowing ability and its impact on dysphagia-specific health-related QOL in oral cavity cancer patients post-treatment. Eur. J. Oncol. Nurs. 2018, 36, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Nallani, R.; Smith, J.B.; Penn, J.P.; Bur, A.M.; Kakarala, K.; Shnayder, Y.; Villwock, M.R.; Sykes, K.J. Decision regret 3 and 6 months after treatment for head and neck cancer: Observational study of associations with clinicodemographics, anxiety, and quality of life. Head Neck 2022, 44, 59–70. [Google Scholar] [CrossRef]
- CCV. Building Effective Cancer Support Groups: Report to the Department of Health and Ageing; Cancer Council Australia: Sydney, NSW, Australia, 2005. [Google Scholar]
- Yap, T.; Tan, I.; Ramani, R.S.; Bhatia, N.; Demetrio de Souza Franca, P.; Angel, C.; Moore, C.; Reiner, T.; Bussau, L.; McCullough, M.J. Acquisition and annotation in high resolution in vivo digital biopsy by confocal microscopy for diagnosis in oral precancer and cancer. Front. Oncol. 2023, 13, 1209261. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Boer, J.; Barnett, R.; Cardin, A.; Cimoli, M.; Davies, L.; Delany, C.; Dixon, B.J.; Evans, S.M.; Findlay, M.W.; Fox, C.; et al. Optimising Patient Outcomes in Tongue Cancer: A Multidisciplinary Approach. Cancers 2024, 16, 1277. https://doi.org/10.3390/cancers16071277
de Boer J, Barnett R, Cardin A, Cimoli M, Davies L, Delany C, Dixon BJ, Evans SM, Findlay MW, Fox C, et al. Optimising Patient Outcomes in Tongue Cancer: A Multidisciplinary Approach. Cancers. 2024; 16(7):1277. https://doi.org/10.3390/cancers16071277
Chicago/Turabian Stylede Boer, Jasper, Rebecca Barnett, Anthony Cardin, Michelle Cimoli, Lauren Davies, Clare Delany, Benjamin J. Dixon, Sue M. Evans, Michael W. Findlay, Carly Fox, and et al. 2024. "Optimising Patient Outcomes in Tongue Cancer: A Multidisciplinary Approach" Cancers 16, no. 7: 1277. https://doi.org/10.3390/cancers16071277
APA Stylede Boer, J., Barnett, R., Cardin, A., Cimoli, M., Davies, L., Delany, C., Dixon, B. J., Evans, S. M., Findlay, M. W., Fox, C., Ftanou, M., Hart, C. D., Howard, M., Iseli, T. A., Jackson, A., Kranz, S., Le, B. H., Lekgabe, E., Lennox, R., ... Wiesenfeld, D. (2024). Optimising Patient Outcomes in Tongue Cancer: A Multidisciplinary Approach. Cancers, 16(7), 1277. https://doi.org/10.3390/cancers16071277







