Multimodal, Technology-Assisted Intervention for the Management of Menopause after Cancer Improves Cancer-Related Quality of Life—Results from the Menopause after Cancer (Mac) Study
Abstract
Simple Summary
Abstract
1. Introduction
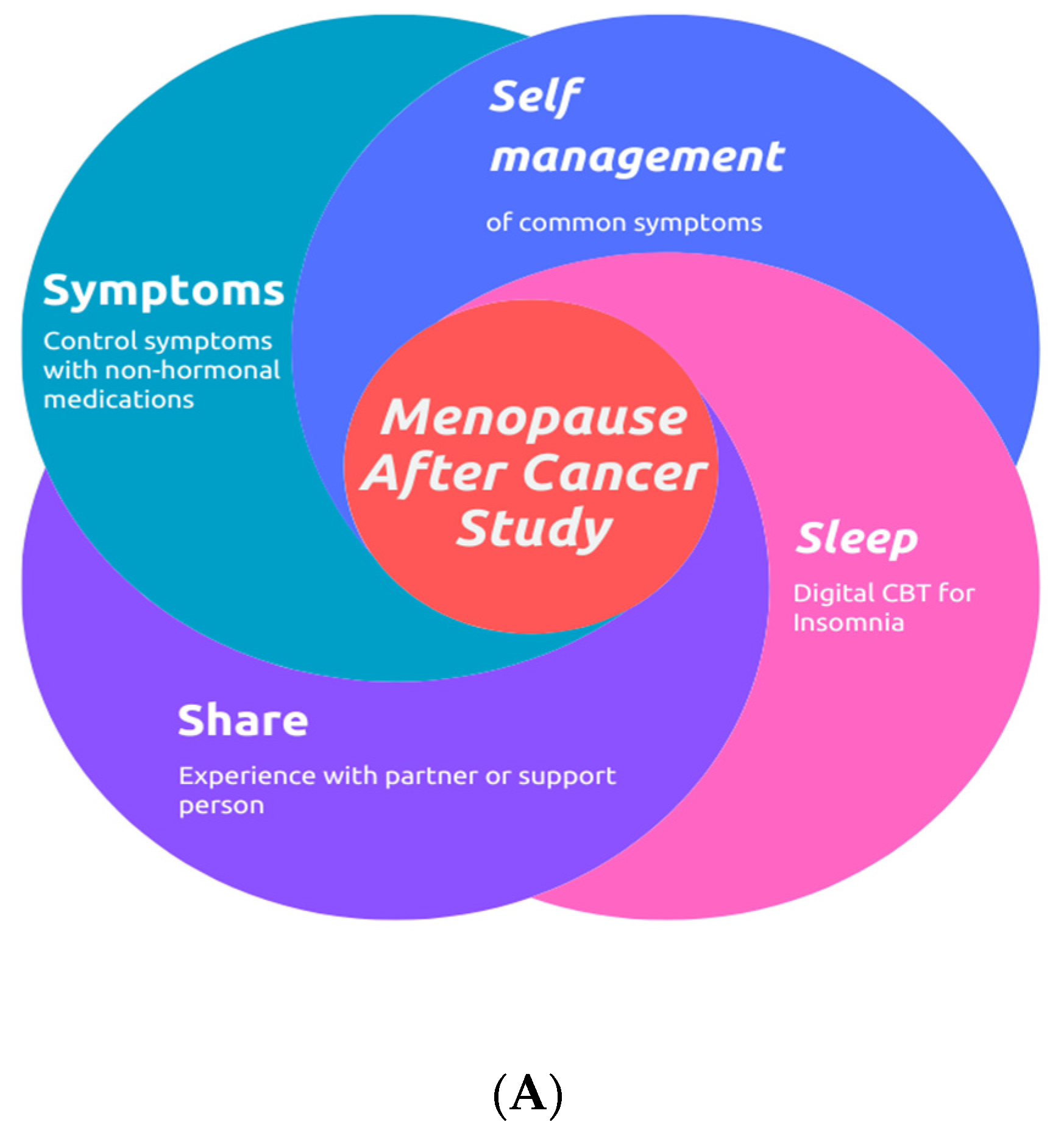
2. Materials and Methods
- Female aged 18 or over;
- At least five VMS episodes in an average 24 h period;
- Moderate degree of bother from these symptoms defined as a score of 5.3 or higher on HFRS [43];
- A prior or current history of cancer;
- A contraindication to standard MHT;
- Confident use of a smartphone.
- Eastern Cooperative Oncology Group (ECOG) performance status of 3 or higher;
- Use of study medications to manage VMS in the preceding six months;
- Use of CBT-I in the preceding six months;
- Any contraindication to study medications;
- Limited spoken or written English;
- No internet access or not confident with smartphone use.
2.1. Non-Hormonal Pharmacotherapy
2.2. Outcomes
2.3. Sample Size Calculation
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Compliance
3.2. The Impact of the Composite MAC Intervention on Global Health Status
3.3. Baseline Quality of Life Was the Main Predictor of Benefit from the MAC Intervention
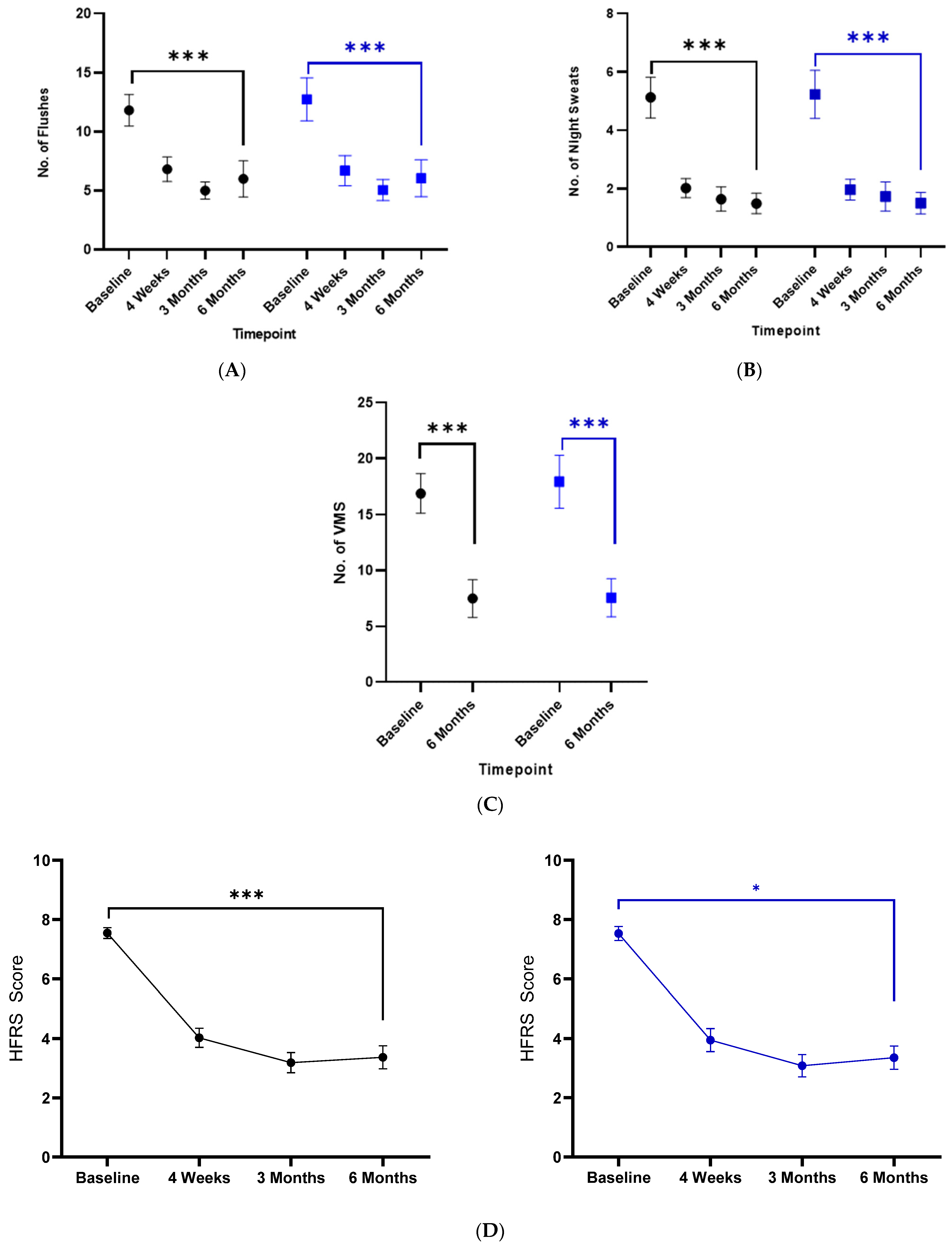
3.4. Menopause Outcomes
3.5. Sleep Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Digital CBT-I
Appendix A.2. myPatient Space
Appendix A.3. Support Person
Appendix B

References
- Tauchmanovà, L.; Selleri, C.; De Rosa, G.; Sammartino, A.; Di Carlo, C.; Musella, T.; Martorelli, C.; Lombardi, G.; Rotoli, B.; Nappi, C.; et al. Estrogen-progestin therapy in women after stem cell transplant: Our experience and literature review. Menopause 2007, 14, 320–330. [Google Scholar] [CrossRef]
- Mahase, E. Colorectal cancer: Screening may need to change given rising incidence in under 50s. Br. Med. J. 2019, 365, l2249. [Google Scholar] [CrossRef]
- Faubion, S.S.; Crandall, C.J.; Davis, L.; El Khoudary, S.R.; Hodis, H.N.; Lobo, R.A.; Maki, P.M.; Manson, J.E.; Pinkerton, J.V.; Santoro, N.F.; et al. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause 2022, 29, 767–794. [Google Scholar]
- Sarri, G.; Pedder, H.; Dias, S.; Guo, Y.; Lumsden, M.A. Vasomotor symptoms resulting from natural menopause: A systematic review and network meta-analysis of treatment effects from the National Institute for Health and Care Excellence guideline on menopause. BJOg 2017, 124, 1514–1523. [Google Scholar] [CrossRef]
- Holmberg, L.; Iversen, O.E.; Rudenstam, C.M.; Hammar, M.; Kumpulainen, E.; Jaskiewicz, J.; Jassem, J.; Dobaczewska, D.; Fjosne, H.E.; Peralta, O.; et al. Increased risk of recurrence after hormone replacement therapy in breast cancer survivors. J. Natl. Cancer Inst. 2008, 100, 475–482. [Google Scholar] [CrossRef]
- von Schoultz, E.; Rutqvist, L.E.; Stockholm Breast Cancer Study Group. Menopausal hormone therapy after breast cancer: The Stockholm randomized trial. J. Natl. Cancer Inst. 2005, 97, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Fahlén, M.; Fornander, T.; Johansson, H.; Johansson, U.; Rutqvist, L.E.; Wilking, N.; von Schoultz, E. Hormone replacement therapy after breast cancer: 10 year follow up of the Stockholm randomised trial. Eur. J. Cancer 2013, 49, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Hickey, M.; Szabo, R.A.; Hunter, M.S. Non-hormonal treatments for menopausal symptoms. Br. Med. J. (Clin. Res. Ed.) 2017, 359, j5101. [Google Scholar] [CrossRef] [PubMed]
- Boekhout, A.H.; Vincent, A.D.; Dalesio, O.B.; van den Bosch, J.; Foekema-Töns, J.H.; Adriaansz, S.; Sprangers, S.; Nuijen, B.; Beijnen, J.H.; Schellens, J.H.M. Management of hot flashes in patients who have breast cancer with venlafaxine and clonidine: A randomized, double-blind, placebo-controlled trial. J. Clin. Oncol. 2011, 29, 3862–3868. [Google Scholar] [CrossRef] [PubMed]
- Bordeleau, L.; Pritchard, K.I.; Loprinzi, C.L.; Ennis, M.; Jugovic, O.; Warr, D.; Haq, R.; Goodwin, P.J. Multicenter, randomized, cross-over clinical trial of venlafaxine versus gabapentin for the management of hot flashes in breast cancer survivors. J. Clin. Oncol. 2010, 28, 5147–5152. [Google Scholar] [CrossRef] [PubMed]
- Loibl, S.; Schwedler, K.; von Minckwitz, G.; Strohmeier, R.; Mehta, K.M.; Kaufmann, M. Venlafaxine is superior to clonidine as treatment of hot flashes in breast cancer patients--a double-blind, randomized study. Ann. Oncol. 2007, 18, 689–693. [Google Scholar] [CrossRef]
- Carpenter, J.S.; Storniolo, A.M.; Johns, S.; Monahan, P.O.; Azzouz, F.; Elam, J.L.; Johnson, C.S.; Shelton, R.C. Randomized, double-blind, placebo-controlled crossover trials of venlafaxine for hot flashes after breast cancer. Oncologist 2007, 12, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, C.L.; Kugler, J.W.; Sloan, J.A.; Mailliard, J.A.; LaVasseur, B.I.; Barton, D.L.; Novotny, P.J.; Dakhil, S.R.; Rodger, K.; Rummans, T.A.; et al. Venlafaxine in management of hot flashes in survivors of breast cancer: A randomised controlled trial. Lancet 2000, 356, 2059–2063. [Google Scholar] [CrossRef] [PubMed]
- Buijs, C.; Mom, C.H.; Willemse, P.H.B.; Marike Boezen, H.; Maurer, J.M.; Wymenga, A.N.M.; de Jong, R.S.; Nieboer, P.; de Vries, E.G.E.; Mourits, M.J.E. Venlafaxine versus clonidine for the treatment of hot flashes in breast cancer patients: A double-blind, randomized cross-over study. Breast Cancer Res. Treat. 2009, 115, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Barton, D.L.; LaVasseur, B.I.; Sloan, J.A.; Stawis, A.N.; Flynn, K.A.; Dyar, M.; Johnson, D.B.; Atherton, P.J.; Diekmann, B.; Loprinzi, C.L. Phase III, placebo-controlled trial of three doses of citalopram for the treatment of hot flashes: NCCTG trial N05C9. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 3278–3283. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kimmick, G.G.; Lovato, J.; McQuellon, R.; Robinson, E.; Muss, H.B. Randomized, double-blind, placebo-controlled, crossover study of sertraline (Zoloft) for the treatment of hot flashes in women with early stage breast cancer taking tamoxifen. Breast J. 2006, 12, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.F.; Hilsenbeck, S.G.; Tham, Y.L.; Kramer, R.; Elledge, R.M.; Chang, J.C.; Friedman, L.C. The efficacy of sertraline for controlling hot flashes in women with or at high risk of developing breast cancer. Breast Cancer Res. Treat. 2009, 118, 369–375. [Google Scholar] [CrossRef]
- Loprinzi, C.L.; Sloan, J.A.; Perez, E.A.; Quella, S.K.; Stella, P.J.; Mailliard, J.A.; Halyard, M.Y.; Pruthi, S.; Novotny, P.J.; Rummans, T.A. Phase III evaluation of fluoxetine for treatment of hot flashes. J. Clin. Oncol. 2002, 20, 1578–1583. [Google Scholar] [CrossRef] [PubMed]
- Biglia, N.; Bounous, V.E.; Susini, T.; Pecchio, S.; Sgro, L.G.; Tuninetti, V.; Torta, R. Duloxetine and escitalopram for hot flushes: Efficacy and compliance in breast cancer survivors. Eur. J. Cancer Care 2018, 27, e12484. [Google Scholar] [CrossRef]
- Leon-Ferre, R.A.; Novotny, P.J.; Wolfe, E.G.; Faubion, S.S.; Ruddy, K.J.; Flora, D.; Dakhil, C.S.R.; Rowland, K.M.; Graham, M.L.; Le-Lindqwister, N.; et al. Oxybutynin vs Placebo for Hot Flashes in Women With or Without Breast Cancer: A Randomized, Double-Blind Clinical Trial (ACCRU SC-1603). JNCI Cancer Spectr. 2020, 4, pkz088. [Google Scholar] [CrossRef]
- Loprinzi, C.L.; Kugler, J.W.; Barton, D.L.; Dueck, A.C.; Tschetter, L.K.; Nelimark, R.A.; Balcueva, E.P.; Burger, K.N.; Novotny, P.J.; Carlson, M.D.; et al. Phase III Trial of Gabapentin Alone or in Conjunction With an Antidepressant in the Management of Hot Flashes in Women Who Have Inadequate Control With an Antidepressant Alone: NCCTG N03C5. J. Clin. Oncol. 2007, 25, 308–312. [Google Scholar] [CrossRef]
- Pandya, K.J.; Morrow, G.R.; Roscoe, J.A.; Zhao, H.; Hickok, J.T.; Pajon, E.; Sweeney, T.J.; Banerjee, T.K.; Flynn, P.J. Gabapentin for hot flashes in 420 women with breast cancer: A randomised double-blind placebo-controlled trial. Lancet 2005, 366, 818–824. [Google Scholar] [CrossRef]
- Loprinzi, C.L.; Qin, R.; Balcueva, E.P.; Flynn, K.A.; Rowland, K.M.; Graham, D.L.; Erwin, N.K.; Dakhil, S.R.; Jurgens, D.J.; Burger, K.N. Phase III, randomized, double-blind, placebo-controlled evaluation of pregabalin for alleviating hot flashes, N07C1. J. Clin. Oncol. 2010, 28, 641–647. [Google Scholar] [CrossRef]
- Australasian Menopause Society. NonHormonal Treatments for Menopausal Symptoms—Australasian Menopause Society. 2016. Available online: https://www.menopause.org.au/hp/information-sheets/600-nonhormonal-treatments-for-menopausal-symptoms (accessed on 17 January 2024).
- Carpenter, J.; Gass, M.L.; Maki, P.M.; Newton, K.M.; Pinkerton, J.V.; Taylor, M.; Utian, W.H.; Schnatz, P.F.; Kaunitz, A.M.; Shapiro, M.; et al. Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The North American Menopause Society. Menopause 2015, 22, 1155–1172. [Google Scholar]
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 141: Management of menopausal symptoms. Obstet. Gynecol. 2014, 123, 202–216. [Google Scholar] [CrossRef]
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.L.; Edge, S.B.; Jacobs, L.A.; et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J. Clin. 2016, 66, 43–73. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.; Oliver, T.K.; Keller-Olaman, S.; Davidson, J.R.; Garland, S.; Samuels, C.; Savard, J.; Harris, C.; Aubin, M.; Olson, K.; et al. Sleep disturbance in adults with cancer: A systematic review of evidence for best practices in assessment and management for clinical practice. Ann. Oncol. 2014, 25, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Ancoli-Israel, S. Recognition and treatment of sleep disturbances in cancer. J. Clin. Oncol. 2009, 27, 5864–5866. [Google Scholar] [CrossRef] [PubMed]
- Arndt, V.; Merx, H.; Stegmaier, C.; Ziegler, H.; Brenner, H. Persistence of restrictions in quality of life from the first to the third year after diagnosis in women with breast cancer. J. Clin. Oncol. 2005, 23, 4945–4953. [Google Scholar] [CrossRef] [PubMed]
- Jean-Pierre, P.; Grandner, M.A.; Garland, S.N.; Henry, E.; Jean-Louis, G.; Burish, T.G. Self-reported memory problems in adult-onset cancer survivors: Effects of cardiovascular disease and insomnia. Sleep Med. 2015, 16, 845–849. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Innominato, P.F.; Focan, C.; Gorlia, T.; Moreau, T.; Garufi, C.; Waterhouse, J.; Giacchetti, S.; Coudert, B.; Iacobelli, S.; Genet, D.; et al. Circadian Rhythm in Rest and Activity: A Biological Correlate of Quality of Life and a Predictor of Survival in Patients with Metastatic Colorectal Cancer. Cancer Res. 2009, 69, 4700–4707. [Google Scholar] [CrossRef] [PubMed]
- Cash, E.; Sephton, S.E.; Chagpar, A.B.; Spiegel, D.; Rebholz, W.N.; Zimmaro, L.A.; Tillie, J.M.; Dhabhar, F.S. Circadian disruption and biomarkers of tumor progression in breast cancer patients awaiting surgery. Brain Behav. Immun. 2015, 48, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Filipski, E.; Li, X.M.; Lévi, F. Disruption of circadian coordination and malignant growth. Cancer Causes Control 2006, 17, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Kansagara, D.; Forciea, M.A.; Cooke, M.; Denberg, T.D.; Clinical Guidelines Committee of the American College of Physicians. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians. Ann. Intern. Med. 2016, 165, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Baglioni, C.; Bassetti, C.; Bjorvatn, B.; Dolenc Groselj, L.; Ellis, J.G.; Espie, C.A.; Garcia-Borreguero, D.; Gjerstad, M.; Gonçalves, M.; et al. European guideline for the diagnosis and treatment of insomnia. J. Sleep Res. 2017, 26, 675–700. [Google Scholar] [CrossRef] [PubMed]
- Edinger, J.D.; Arnedt, J.T.; Bertisch, S.M.; Carney, C.E.; Harrington, J.J.; Lichstein, K.L.; Sateia, M.J.; Troxel, W.M.; Zhou, E.S.; Kazmi, U.; et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: An American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 2021, 17, 255–262. [Google Scholar] [CrossRef]
- Morin, C.M. Cognitive-behavioral Therapy of Insomnia. Sleep Med. Clin. 2006, 1, 375–386. [Google Scholar] [CrossRef]
- Johnson, J.A.; Rash, J.A.; Campbell, T.S.; Savard, J.; Gehrman, P.R.; Perlis, M.; Carlson, L.E.; Garland, S.N. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med. Rev. 2016, 27, 20–28. [Google Scholar] [CrossRef]
- Guthrie, K.A.; Larson, J.C.; Ensrud, K.E.; Anderson, G.L.; Carpenter, J.S.; Freeman, E.W.; Joffe, H.; LaCroix, A.Z.; Manson, J.E.; Morin, C.M.; et al. Effects of Pharmacologic and Nonpharmacologic Interventions on Insomnia Symptoms and Self-reported Sleep Quality in Women With Hot Flashes: A Pooled Analysis of Individual Participant Data From Four MsFLASH Trials. Sleep 2018, 41, zsx190. [Google Scholar] [CrossRef]
- Sleepio to Treat Insomnia and Insomnia Symptoms|Guidance|NICE. NICE. 2022. Available online: https://www.nice.org.uk/guidance/mtg70/chapter/1-Recommendations (accessed on 17 January 2024).
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Hunter, M.S.; Liao, K.L.M. A psychological analysis of menopausal hot flushes. Br. J. Clin. Psychol. 1995, 34, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Espie, C.A.; Kyle, S.D.; Hames, P.; Gardani, M.; Fleming, L.; Cape, J. The Sleep Condition Indicator: A clinical screening tool to evaluate insomnia disorder. BMJ Open 2014, 4, e004183. [Google Scholar] [CrossRef]
- Espie, C.A.; Fleming, L.; Cassidy, J.; Samuel, L.; Taylor, L.M.; White, C.A.; Douglas, N.J.; Engleman, H.M.; Kelly, H.L.; Paul, J. Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J. Clin. Oncol. 2008, 26, 4651–4658. [Google Scholar] [CrossRef]
- Donohoe, F.; O’Meara, Y.; Roberts, A.; Comerford, L.; Kelly, C.M.; Walshe, J.M.; Peate, M.; Hickey, M.; Brennan, D.J. The menopause after cancer study (MACS)—A multimodal technology assisted intervention for the management of menopausal symptoms after cancer—Trial protocol of a phase II study. Contemp. Clin. Trials Commun. 2021, 24, 100865. [Google Scholar] [CrossRef] [PubMed]
- Freeman, E.W.; Guthrie, K.A.; Caan, B.; Sternfeld, B.; Cohen, L.S.; Joffe, H.; Carpenter, J.S.; Anderson, G.L.; Larson, J.C.; Ensrud, K.E.; et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: A randomized controlled trial. J. Am. Med. Assoc. 2011, 305, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, C.L.; Barton, D.L.; Sloan, J.A.; Novotny, P.J.; Dakhil, S.R.; Verdirame, J.D.; Knutson, W.H.; Kelaghan, J.; Christensen, B. Mayo Clinic and North Central Cancer Treatment Group hot flash studies: A 20-year experience. Menopause 2008, 15, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.D.; Vesco, K.K.; Haney, E.; Fu, R.; Nedrow, A.; Miller, J.; Nicolaidis, C.; Walker, M.; Humphrey, L. Nonhormonal therapies for menopausal hot flashes: Systematic review and meta-analysis. J. Am. Med. Assoc. 2006, 295, 2057–2071. [Google Scholar] [CrossRef]
- Loprinzi, C.L.; Sloan, J.; Stearns, V.; Slack, R.; Iyengar, M.; Diekmann, B.; Kimmick, G.; Lovato, J.; Gordon, P.; Pandya, K.; et al. Newer antidepressants and gabapentin for hot flashes: An individual patient pooled analysis. J. Clin. Oncol. 2009, 27, 2831–2837. [Google Scholar] [CrossRef]
- Hunter, M.S.; Nuttall, J.; Fenlon, D. A comparison of three outcome measures of the impact of vasomotor symptoms on women’s lives. Climacteric 2019, 22, 419–423. [Google Scholar] [CrossRef]
- Espie, C.A.; Farias Machado, P.; Carl, J.R.; Kyle, S.D.; Cape, J.; Siriwardena, A.N.; Luik, A.I. The Sleep Condition Indicator: Reference values derived from a sample of 200,000 adults. J. Sleep Res. 2018, 27, e12643. [Google Scholar] [CrossRef]
- Cocks, K.; King, M.T.; Velikova, G.; de Castro, G.; Martyn St-James, M.; Fayers, P.M.; Brown, J.M. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur. J. Cancer 2012, 48, 1713–1721. [Google Scholar] [CrossRef] [PubMed]
- Mackey, J.R.; Pieńkowski, T.; Crown, J.; Sadeghi, S.; Martin, M.; Chan, A.; Saleh, M.; Sehdev, S.; Provencher, L.; Semiglazov, V.; et al. Long-term outcomes after adjuvant treatment of sequential versus combination docetaxel with doxorubicin and cyclophosphamide in node-positive breast cancer: BCIRG-005 randomized trial. Ann. Oncol. 2016, 27, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Intravenous RPR109881 in Male or Female Patients With Advanced Breast Cancer Who no Longer Respond to Anthracycline, Taxane and Capecitabine Treatment—Full Text View—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT00087958 (accessed on 24 August 2023).
- Stearns, V.; Slack, R.; Greep, N.; Henry-Tilman, R.; Osborne, M.; Bunnell, C.; Ullmer, L.; Gallagher, A.; Cullen, J.; Gehan, E.; et al. Paroxetine is an effective treatment for hot flashes: Results from a prospective randomized clinical trial. J. Clin. Oncol. 2005, 23, 6919–6930. [Google Scholar] [CrossRef] [PubMed]
- Avis, N.E.; Smith, K.W.; Link, C.L.; Hortobagyi, G.N.; Rivera, E. Factors associated with participation in breast cancer treatment clinical trials. J. Clin. Oncol. 2006, 24, 1860–1867. [Google Scholar] [CrossRef] [PubMed]
- Legge, F.; Eaton, D.; Molife, R.; Ferrandina, G.; Judson, I.; de Bono, J.; Kaye, S. Participation of patients with gynecological cancer in phase I clinical trials: Two years experience in a major cancer center. Gynecol. Oncol. 2007, 104, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.J.; Tan, T.; Li, S.Q.; Meghani, S.H.; Glanz, K.; Bruner, D. Attitudes and barriers towards participation in an acupuncture trial among breast cancer patients: A survey study. BMC Complement Altern Med. 2014, 14, 7. [Google Scholar] [CrossRef] [PubMed]
- Espie, C.A.; Emsley, R.; Kyle, S.D.; Gordon, C.; Drake, C.L.; Siriwardena, A.N.; Cape, J.; Ong, J.C.; Sheaves, B.; Foster, R.; et al. Effect of Digital Cognitive Behavioral Therapy for Insomnia on Health, Psychological Well-being, and Sleep-Related Quality of Life: A Randomized Clinical Trial. JAMA Psychiatry 2019, 76, 21–30. [Google Scholar] [CrossRef]
- Smejka, T.; Henry, A.L.; Wheatley, C.; Espie, C.A.; Johansen-Berg, H.; Fleming, M.K. A qualitative examination of the usability of a digital cognitive behavioral therapy for insomnia program after stroke. Brain Inj. 2022, 36, 271–278. [Google Scholar] [CrossRef]
- Treacy, T.; O’Meara, Y.; Henry, A.L.; Lensen, S.F.; Higgins, M.J.; Hickey, M.; Brennan, D.J. The Sleepio after cancer (SAC) study. Digital cognitive behavioural therapy for insomnia (dCBT-I) in women cancer patients—Trial protocol of a randomised controlled trial. Contemp. Clin. Trials 2023, 136, 107337. [Google Scholar] [CrossRef]
- Guttuso, T.; Kurlan, R.; McDermott, M.P.; Kieburtz, K. Gabapentin’s effects on hot flashes in postmenopausal women: A randomized controlled trial. Obstet. Gynecol. 2003, 101, 337–345. [Google Scholar] [CrossRef]
- Pistilli, B.; Paci, A.; Ferreira, A.R.; Di Meglio, A.; Poinsignon, V.; Bardet, A.; Menvielle, G.; Dumas, A.; Pinto, S.; Dauchy, S.; et al. Serum Detection of Nonadherence to Adjuvant Tamoxifen and Breast Cancer Recurrence Risk. J. Clin. Oncol. 2020, 38, 2762–2772. [Google Scholar] [CrossRef]
- Francis, P.A.; Pagani, O.; Fleming, G.F.; Walley, B.A.; Colleoni, M.; Láng, I.; Gómez, H.L.; Tondini, C.; Ciruelos, E.; Burstein, H.J.; et al. SOFT and TEXT Investigators and the International Breast Cancer Study Group. Tailoring Adjuvant Endocrine Therapy for Premenopausal Breast Cancer. N. Engl. J. Med. 2018, 379, 122–137. [Google Scholar] [CrossRef]
- Barnes, C.M.; Miller, J.A.; Bostock, S. Helping employees sleep well: Effects of cognitive behavioral therapy for insomnia on work outcomes. J. Appl. Psychol. 2017, 102, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Bostock, S.; Luik, A.I.; Espie, C.A. Sleep and Productivity Benefits of Digital Cognitive Behavioral Therapy for Insomnia: A Randomized Controlled Trial Conducted in the Workplace Environment. J. Occup. Environ. Med. 2016, 58, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Luik, A.I.; Fellman-Couture, C.; Peterson, E.; Joseph, C.L.M.; Tallent, G.; Tran, K.M.; Ahmedani, B.K.; Roehrs, T.; Roth, T.; et al. Efficacy of digital CBT for insomnia to reduce depression across demographic groups: A randomized trial. Psychol. Med. 2019, 49, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Espie, C.A.; Kyle, S.D.; Williams, C.; Ong, J.C.; Douglas, N.J.; Hames, P.; Brown, J.S.L. A Randomized, Placebo-Controlled Trial of Online Cognitive Behavioral Therapy for Chronic Insomnia Disorder Delivered via an Automated Media-Rich Web Application. Sleep 2012, 35, 769–781. [Google Scholar] [CrossRef]
- Denis, D.; Eley, T.C.; Rijsdijk, F.; Zavos, H.M.S.; Keers, R.; Espie, C.A.; Luik, A.I.; Badini, I.; Derveeuw, S.; Hodsoll, J.; et al. Is digital cognitive behavioural therapy for insomnia effective in treating sub-threshold insomnia: A pilot RCT. Sleep Med. 2020, 66, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Felder, J.N.; Epel, E.S.; Neuhaus, J.; Krystal, A.D.; Prather, A.A. Efficacy of Digital Cognitive Behavioral Therapy for the Treatment of Insomnia Symptoms Among Pregnant Women: A Randomized Clinical Trial. JAMA Psychiatry 2020, 77, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Sheaves, B.; Goodwin, G.M.; Yu, L.M.; Nickless, A.; Harrison, P.J.; Emsley, R.; Luik, A.I.; Foster, R.G.; Wadekar, V.; et al. The effects of improving sleep on mental health (OASIS): A randomised controlled trial with mediation analysis. Lancet Psychiatry 2017, 4, 49–58. [Google Scholar] [CrossRef]
- Kalmbach, D.A.; Cheng, P.; O’Brien, L.M.; Swanson, L.M.; Sangha, R.; Sen, S.; Guille, C.; Cuamatzi-Castelan, A.; Henry, A.L.; Roth, T.; et al. A randomized controlled trial of digital cognitive behavioral therapy for insomnia in pregnant women. Sleep Med. 2020, 72, 82–92. [Google Scholar] [CrossRef]
- Kyle, S.D.; Hurry, M.E.D.; Emsley, R.; Marsden, A.; Omlin, X.; Juss, A.; Spiegelhalder, K.; Bisdounis, L.; Luik, A.I.; Espie, C.A.; et al. The effects of digital cognitive behavioral therapy for insomnia on cognitive function: A randomized controlled trial. Sleep 2020, 43, zsaa034. [Google Scholar] [CrossRef] [PubMed]
- McGrath, E.R.; Espie, C.A.; Power, A.; Murphy, A.W.; Newell, J.; Kelly, C.; Duffy, N.; Gunning, P.; Gibson, I.; Bostock, S.; et al. Sleep to Lower Elevated Blood Pressure: A Randomized Controlled Trial (SLEPT). Am. J. Hypertens. 2017, 30, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Pillai, V.; Anderson, J.R.; Cheng, P.; Bazan, L.; Bostock, S.; Espie, C.; Roth, T.; Drake, C. The Anxiolytic Effects of Cognitive Behavior Therapy for Insomnia: Preliminary Results from a Web-delivered Protocol. J. Sleep Med. Disord. 2015, 2, 1017. [Google Scholar] [PubMed]
- Fleming, M.K.; Smejka, T.; Macey, E.; Luengo-Fernandez, R.; Henry, A.L.; Robinson, B.; Kyle, S.D.; Espie, C.A.; Johansen-Berg, H. Improving sleep after stroke: A randomised controlled trial of digital cognitive behavioural therapy for insomnia. J. Sleep Res. 2023, e13971. [Google Scholar] [CrossRef]
- Ho, K.K.N.; Simic, M.; Pinheiro, M.B.; Miller, C.B.; Ferreira, M.L.; Grunstein, R.R.; Hopper, J.L.; Ordoñana, J.R.; Ferreira, P.H. Efficacy of a digital cognitive behavioral therapy for insomnia in people with low back pain: A feasibility randomized co-twin and singleton-controlled trial. Pilot Feasibility Stud. 2022, 8, 125. [Google Scholar] [CrossRef]




| ITT (n = 204) | PP (n = 120) | ||
|---|---|---|---|
| Median Age (Range, IQR) | 49 (28–66, 45–53) | 50 (28–66, 46–53) | |
| Ethnicity | White | 202 (99) | 118 (98.3) |
| Asian/Asian Irish | 2 (1) | 2 (1.7) | |
| Educational level | Primary | 1 (0.5) | 1 (0.8) |
| Secondary | 29 (14.2) | 16 (13.3) | |
| Third level | 138 (67.6) | 87 (72.5) | |
| Third level > 4 years | 36 (17.6) | 16 (13.3) | |
| Smoking status | Current smoker | 12 (5.9) | 7 (5.8) |
| Ex smoker | 71 (34.8) | 42 (35) | |
| Non-smoker | 121 (59.3) | 71 (59.2) | |
| Alcohol consumption | Non-drinkers | 52 (25.4) | 33 (27.5) |
| 1–5 units/week | 109 (53.4) | 65 (54.2) | |
| 6–10 units/week | 36 (17.6) | 19 (15.8) | |
| >10 units/week | 7 (3.4) | 3 (2.5) | |
| Exercise frequency (active for >30 min) | 5–7 times/week | 112 (54.9) | 72 (60) |
| 1–5 times/week | 69 (33.8) | 35 (29.2) | |
| Stopped | 21 (10.3) | 12 (10.8) | |
| Never | 2 (1) | 0 | |
| Diagnosis | Breast cancer | 167 (81.9) | 102 (85) |
| Ovarian cancer | 18 (8.8) | 7 (5.8) | |
| Endometrial cancer | 12 (5.9) | 7 (5.8) | |
| Other | 7 (3.4) | 4 (3.3) | |
| Stage at diagnosis | Stage 1 | 58 (28.4) | 32 (26.7) |
| Stage 2 | 70 (34.3) | 41 (34.2) | |
| Stage 3 | 44 (21.6) | 25 (20.8) | |
| Stage 4 | 11 (5.4) | 7 (5.8) | |
| Stage unknown | 21 (10.3) | 15 (12.5) | |
| Treatment—Breast cancer | Surgery alone | 42 (25.1) | 30 (29.4) |
| ITT (n = 167) | Surgery + chemotherapy | 21 (12.6) | 10 (9.8) |
| PP (n = 102) | Surgery + chemotherapy + radiotherapy | 102 (61.1) | 60 (58.8) |
| Chemotherapy alone | |||
| 2 (1.2) | 2 (1.9) | ||
| Current anti-endocrine therapy * | |||
| 120 (71.9) | 72 (70.6) | ||
| Treatment—Ovarian cancer | Surgery alone | 4 (22.2) | 2 (28.6) |
| ITT (n = 18) | Surgery + chemotherapy | 14 (77.8) | 5 (71.4) |
| PP (n = 7) | |||
| Current anti-endocrine therapy * | 4 (22.2) | 2 (28.6) | |
| Treatment—Endometrial cancer | Surgery alone | 11 (91.7) | 6 (85.7) |
| ITT (n = 12) | Surgery + chemotherapy | 1 (8.3) | 1 (14.3) |
| PP (n = 7) | |||
| Current status | No evidence of disease | 191 (93.6) | 112 (93.3) |
| Recurrent/metastatic disease | 13 (6.4) | 8 (6.7) | |
| Characteristic | Not Substantially Improved (n = 99) | Improvement ≥ 5 (n = 90) | Total (n = 189) | p Value |
|---|---|---|---|---|
| Baseline global health status | <0.001 | |||
| Median (Q1, Q3) | 67.0 (58.0, 83.0) | 50.0 (42.0, 67.0) | 67.0 (50.0,75.0) | |
| Started Sleepio | 0.428 | |||
| No | 18 (18.2%) | 12 (13.3%) | 30 (15.9%) | |
| Yes | 81 (81.8%) | 78 (86.7%) | 159 (84.1%) | |
| Completed Sleepio | 0.008 | |||
| No | 76 (76.8%) | 52 (57.8%) | 128 (67.7%) | |
| Yes | 23 (23.2%) | 38 (42.2%) | 61 (32.3%) | |
| Medications at six months | <0.001 | |||
| Stopped | 42 (42.4%) | 17 (18.9%) | 59 (31.2%) | |
| Not stopped | 41 (41.4%) | 60 (66.7%) | 101 (53.4%) | |
| Unknown | 16 (16.2%) | 13 (14.4%) | 29 (15.3%) | |
| Third level education | 1 | |||
| No | 14 (14.1%) | 13 (14.4%) | 27 (14.3%) | |
| Yes | 85 (85.9%) | 77 (85.6%) | 162 (85.7%) | |
| Never smoked | 0.655 | |||
| No | 37 (37.4%) | 37 (41.1%) | 74 (39.2%) | |
| Yes | 62 (62.6%) | 53 (58.9%) | 115 (60.8%) | |
| Units of alcohol | 0.86 | |||
| N-Miss | 0 | 1 | 1 | |
| Median (Q1, Q3) | 2.0 (0.5, 5.0) | 2.0 (0.0, 5.0) | 2.0 (0.0, 5.0) | |
| Exercise ≥ 5 days/w | 0.243 | |||
| No | 50 (50.5%) | 37 (41.1%) | 87 (46.0%) | |
| Yes | 49 (49.5%) | 53 (58.9%) | 102 (54.0%) | |
| Breast cancer diagnosis | 0.052 | |||
| No | 22 (22.2%) | 10 (11.1%) | 32 (16.9%) | |
| Yes | 77 (77.8%) | 80 (88.9%) | 157 (83.1%) | |
| VMS same or worse at night | 0.714 | |||
| No | 20 (20.2%) | 16 (17.8%) | 36 (19.0%) | |
| Yes | 79 (79.8%) | 74 (82.2%) | 153 (81.0%) | |
| VMS worst at night | 0.382 | |||
| No | 48 (48.5%) | 50 (55.6%) | 98 (51.9%) | |
| Yes | 51 (51.5%) | 40 (44.4%) | 91 (48.1%) | |
| Cognitive symptoms | 0.75 | |||
| No | 69 (69.7%) | 65 (72.2%) | 134 (70.9%) | |
| Yes | 30 (30.3%) | 25 (27.8%) | 55 (29.1%) | |
| Psychological symptoms | 0.869 | |||
| No | 72 (72.7%) | 67 (74.4%) | 139 (73.5%) | |
| Yes | 27 (27.3%) | 23 (25.6%) | 50 (26.5%) | |
| Sexual symptoms | 0.843 | |||
| No | 84 (84.8%) | 75 (83.3%) | 159 (84.1%) | |
| Yes | 15 (15.2%) | 15 (16.7%) | 30 (15.9%) | |
| Musculoskeletal symptoms | 0.882 | |||
| N-Miss | 0 | 1 | 1 | |
| No | 58 (58.6%) | 54 (60.7%) | 112 (59.6%) | |
| Yes | 41 (41.4%) | 35 (39.3%) | 76 (40.4%) | |
| Sleep symptoms | 0.366 | |||
| No | 40 (40.4%) | 30 (33.3%) | 70 (37.0%) | |
| Yes | 59 (59.6%) | 60 (66.7%) | 119 (63.0%) | |
| Current anti endocrine therapy | 0.655 | |||
| No | 40 (40.4%) | 33 (36.7%) | 73 (38.6%) | |
| Yes | 59 (59.6%) | 57 (63.3%) | 116 (61.4%) |
| n | SCI at Baseline (SEM) | Prescribed Gabapentin (n) | SCI at 6 Months (SEM) | Continued Gabapentin (n) | |
|---|---|---|---|---|---|
| Sleepio completers | 62 | 7.5 (0.4) | 50 | 17.4 (0.8) | 41 |
| At least 1 session of Sleepio | 161 | 8.3 (0.4) | 134 | 17.1 (0.5) | 74 |
| No Sleepio | 43 | 9.5 (1.2) | 35 | 18.4 (1.6) | 11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donohoe, F.; O’Meara, Y.; Roberts, A.; Comerford, L.; Valcheva, I.; Kearns, U.; Galligan, M.; Higgins, M.J.; Henry, A.L.; Kelly, C.M.; et al. Multimodal, Technology-Assisted Intervention for the Management of Menopause after Cancer Improves Cancer-Related Quality of Life—Results from the Menopause after Cancer (Mac) Study. Cancers 2024, 16, 1127. https://doi.org/10.3390/cancers16061127
Donohoe F, O’Meara Y, Roberts A, Comerford L, Valcheva I, Kearns U, Galligan M, Higgins MJ, Henry AL, Kelly CM, et al. Multimodal, Technology-Assisted Intervention for the Management of Menopause after Cancer Improves Cancer-Related Quality of Life—Results from the Menopause after Cancer (Mac) Study. Cancers. 2024; 16(6):1127. https://doi.org/10.3390/cancers16061127
Chicago/Turabian StyleDonohoe, Fionán, Yvonne O’Meara, Aidin Roberts, Louise Comerford, Ivaila Valcheva, Una Kearns, Marie Galligan, Michaela J. Higgins, Alasdair L. Henry, Catherine M. Kelly, and et al. 2024. "Multimodal, Technology-Assisted Intervention for the Management of Menopause after Cancer Improves Cancer-Related Quality of Life—Results from the Menopause after Cancer (Mac) Study" Cancers 16, no. 6: 1127. https://doi.org/10.3390/cancers16061127
APA StyleDonohoe, F., O’Meara, Y., Roberts, A., Comerford, L., Valcheva, I., Kearns, U., Galligan, M., Higgins, M. J., Henry, A. L., Kelly, C. M., Walshe, J. M., Hickey, M., & Brennan, D. J. (2024). Multimodal, Technology-Assisted Intervention for the Management of Menopause after Cancer Improves Cancer-Related Quality of Life—Results from the Menopause after Cancer (Mac) Study. Cancers, 16(6), 1127. https://doi.org/10.3390/cancers16061127






