Socioeconomic Burden of Psychiatric Cancer Patients: A Narrative Review
Abstract
Simple Summary
Abstract
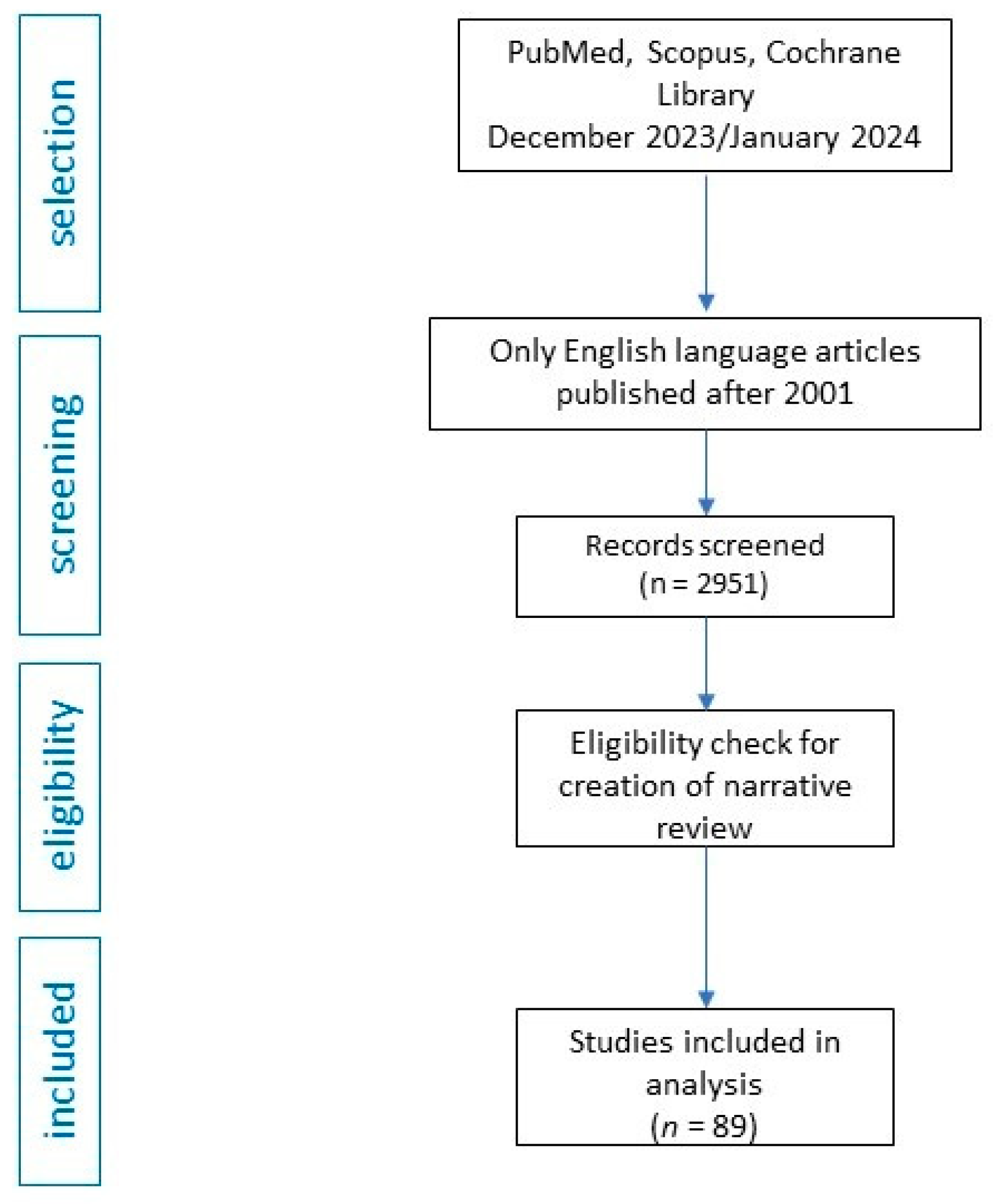
1. Introduction
2. Socioeconomic Associations between Psychiatric Illness and Cancer
2.1. Affective Disorders
2.2. Psychotic Disorders (e.g., Schizophrenia)
2.3. Addictions
2.4. Anxiety Disorders
2.5. Post-Traumatic Stress Disorder (PTSD)
2.6. Somatic Symptom Disorder
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, K.; Liu, Q.; László, K.D.; Wei, D.; Yang, F.; Fall, K.; Adami, H.-O.; Ye, W.; Valdimarsdóttir, U.A.; Li, J.; et al. Risk of Psychiatric Disorders Among Spouses of Patients with Cancer in Denmark and Sweden. JAMA Netw. Open 2023, 6, e2249560. [Google Scholar] [CrossRef]
- Günther, M.P.; Riemann, P.M.; von Känel, R.; Euler, S.; Ben Schulze, J. Steriod-associated psychiatric burden in cancer patients. Basic Clin. Pharmacol. Toxicol. 2023, 132, 501–509. [Google Scholar] [CrossRef]
- Kim, Y.A.; Lee, Y.-R.; Park, J.; Oh, I.-H.; Kim, H.; Yoon, S.-J.; Park, K. Socioeconomic Burden of Cancer in Korea from 2011 to 2015. Cancer Res. Treat. 2020, 52, 896–906. [Google Scholar] [CrossRef]
- Caruso, R.; Breitbart, W. Mental health care in oncology. Contemporary perspective on the psychosocial burden of cancer and evidence-based interventions. Epidemiol. Psychiatr. Sci. 2020, 29, e86. [Google Scholar] [CrossRef]
- Klügel, S.; Lücke, C.; Meta, A.; Schild-Suhren, M.; Malik, E.; Philipsen, A.; Müller, H.H. Concomitant psychiatric symptoms and impaired quality of life in women with cervical cancer: A critical review. Int. J. Womens Health 2017, 9, 795–805. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G. Current Cancer Epidemiology. J. Epidemiol. Glob. Health 2019, 9, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Ampalam, P.; Gunturu, S.; Padma, V. A comparative study of caregiver burden in psychiatric illness and chronic medical illness. Indian J. Psychiatry 2012, 54, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.H.; Lai, A.G. Cumulative burden of psychiatric disorders and self-harm across 26 adult cancers. Nat. Med. 2022, 28, 860–870. [Google Scholar] [CrossRef] [PubMed]
- Nasrabadi, A.N.; Sharif, S.P.; Allen, K.A.; Naghavi, N.; Nia, H.S.; Salisu, W.J.; Yaghoobzadeh, A. The role of socioeconomic status in the relationship between social support and burden among cancer caregivers. Eur. J. Cancer Prev. 2022, 31, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Lai, A.G.; Chang, W.H. There is no health without mental health: Challenges ignored and lessons learned. Clin. Transl. Med. 2022, 12, e897. [Google Scholar] [CrossRef] [PubMed]
- Dinker, N.L.; Kumar, P.; Naidu, S. Psychiatric morbidity in cancer patients. Int. J. Contemp. Med. Res. 2019, 6, F1–F8. [Google Scholar] [CrossRef]
- García-Torres, F.; Jabłoński, M.J.; Solís, G.; Jaén-Moreno, M.J.; Gálvez-Lara, M.; Moriana, J.A.; Moreno-Díaz, M.J.; Aranda, E. Caregiver Burden Domains and Their Relationship with Anxiety and Depression in the First Six Months of Cancer Diagnosis. Int. J. Environ. Res. Public Health 2020, 17, 4101. [Google Scholar] [CrossRef] [PubMed]
- Vadher, S.; Desai, R.; Panchal, B.; Vala, A.; Ratnani, I.J.; Rupani, M.P.; Vasava, K. Burden of care in caregivers of patients with alcohol use disorder and schizophrenia and its association with anxiety, depression and quality of life. Gen. Psychiatr. 2020, 33, e100215. [Google Scholar] [CrossRef] [PubMed]
- Alhelali, A.; Almheiri, E.; Abdelnaim, M.; Weber, F.C.; Langguth, B.; Schecklmann, M.; Hebel, T. Effectiveness of Repetitive Transcranial Magnetic Stimulation in the Treatment of Bipolar Disorder in Comparison to the Treatment of Unipolar Depression in a Naturalistic Setting. Brain Sci. 2022, 12, 298. [Google Scholar] [CrossRef] [PubMed]
- Esaki, Y.; Obayashi, K.; Saeki, K.; Fujita, K.; Iwata, N.; Kitajima, T. Preventive effect of morning light exposure on relapse into depressive episode in bipolar disorder. Acta Psychiatr. Scand. 2021, 143, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Yasuma, N.; Imamura, K.; Watanabe, K.; Iida, M.; Takano, A. Adolescent cannabis use and the later onset of bipolar disorder: Protocol for a systematic review and meta-analysis of prospective cohort studies. Neuropsychopharmacol. Rep. 2022, 42, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Tanna, K.J. Evaluation of burden felt by caregivers of patients with schizophrenia and bipolar disorder. Ind. Psychiatry J. 2021, 30, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Bauer, R.; Gottfriedsen, G.; Binder, H.; Dobmeier, M.; Cording, C.; Hajak, G.; Spiessl, H. Burden of caregivers of patients with bipolar affective disorders. Am. J. Orthopsychiatry 2011, 81, 139–148. [Google Scholar] [CrossRef]
- Reinares, M.; Vieta, E.; Colom, F.; Martínez-Arán, A.; Torrent, C.; Comes, M.; Goikolea, J.; Benabarre, A.; Sánchez-Moreno, J. Impact of a psychoeducational family intervention on caregivers of stabilized bipolar patients. Psychother. Psychosom. 2004, 73, 312–319. [Google Scholar] [CrossRef]
- Chen, M.; Tsai, S.; Su, T.; Li, C.; Lin, W.; Cheng, C.; Chen, T.; Bai, Y. Cancer risk in patients with bipolar disorder and unaffected siblings of such patients: A nationwide population-based study. Int. J. Cancer 2022, 150, 1579–1586. [Google Scholar] [CrossRef]
- Crespo-Facorro, B.; Such, P.; Nylander, A.-G.; Madera, J.; Resemann, H.K.; Worthington, E.; O’connor, M.; Drane, E.; Steeves, S.; Newton, R. The burden of disease in early schizophrenia—A systematic literature review. Curr. Med. Res. Opin. 2021, 37, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Kozloff, N.; Mulsant, B.H.; Stergiopoulos, V.; Voineskos, A.N. The COVID-19 Global Pandemic: Implications for People with Schizophrenia and Related Disorders. Schizophr. Bull. 2020, 46, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Bang, M. Anti-inflammatory Strategies for Schizophrenia: A Review of Evidence for Therapeutic Applications and Drug Repurposing. Clin. Psychopharmacol. Neurosci. 2020, 18, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Adeosun, I.I. Correlates of Caregiver Burden among Family Members of Patients with Schizophrenia in Lagos, Nigeria. Schizophr. Res. Treatment 2013, 2013, 353809. [Google Scholar] [CrossRef] [PubMed]
- Chou, F.H.; Tsai, K.; Wu, H.; Shen, S. Cancer in patients with schizophrenia: What is the next step? Psychiatry Clin. Neurosci. 2016, 70, 473–488. [Google Scholar] [CrossRef] [PubMed]
- Koujalgi, S.R.; Patil, S.R. Family burden in patient with schizophrenia and depressive disorder: A comparative study. Indian J. Psychol. Med. 2013, 35, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Saad, S.; Bshawri, J.A.; Alsaedi, S.M.; Radi, R.E.; Ghonim, R.M.; Nasraldain, H.M.; Gadeer, A.A. Social stigma among health-care providers toward patients with schizophrenia and obsessive-compulsive disorders at tertiary hospital in Makkah, Saudi Arabia. Ment. Health Rev. J. 2022, 27, 281–294. [Google Scholar] [CrossRef]
- van Zelst, C. Stigmatization as an environmental risk in schizophrenia: A user perspective. Schizophr. Bull. 2009, 35, 293–296. [Google Scholar] [CrossRef][Green Version]
- Lin, C.-Y.; Chang, C.-C.; Wu, T.-H.; Wang, J.-D. Dynamic changes of self-stigma, quality of life, somatic complaints, and depression among people with schizophrenia: A pilot study applying kernel smoothers. Stigma Health 2016, 1, 29–43. [Google Scholar] [CrossRef]
- Świtaj, P.; Chrostek, A.; Grygiel, P.; Wciórka, J.; Anczewska, M. Exploring Factors Associated with the Psychosocial Impact of Stigma Among People with Schizophrenia or Affective Disorders. Community Ment. Health J. 2016, 52, 370–378. [Google Scholar] [CrossRef][Green Version]
- Sevinik, H.; Ceylan, B. Internalized stigma and social functioning in people with schizophrenia. In Proceedings of the 4th Business & Management Conference, Istanbul, Turkey, 12–14 October 2016. [Google Scholar] [CrossRef][Green Version]
- Vidović, D.; Brečić, P.; Vilibić, M.; Jukić, V. Insight and Self-Stigma in Patients with Schizophrenia. Acta Clin. Croat. 2016, 55, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.-H.; Kao, M.-Y.; Goh, K.K.; Lu, C.-Y.; Lu, M.-L. Renaming Schizophrenia and Stigma Reduction: A Cross-Sectional Study of Nursing Students in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 3563. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Azman, N.; Eyu, H.T.; Jaafar, N.R.N.; Sahimi, H.M.S.; Yunus, M.R.M.; Shariff, N.M.; Hami, R.; Mansor, N.S.; Lu, P.; et al. Validation of the Malay Version of the Shame and Stigma Scale among Cancer Patients in Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 14266. [Google Scholar] [CrossRef] [PubMed]
- Warner, E.T.; Park, E.R.; Luberto, C.M.; Rabin, J.; Perez, G.K.; Ostroff, J.S. Internalized stigma among cancer patients enrolled in a smoking cessation trial: The role of cancer type and associations with psychological distress. Psychooncology 2022, 31, 753–760. [Google Scholar] [CrossRef]
- Ernst, J.; Mehnert, A.; Dietz, A.; Hornemann, B.; Esser, P. Perceived stigmatization and its impact on quality of life—Results from a large register-based study including breast, colon, prostate and lung cancer patients. BMC Cancer 2017, 17, 741. [Google Scholar] [CrossRef]
- Chambers, S.K.; Baade, P.; Youl, P.; Aitken, J.; Occhipinti, S.; Vinod, S.; Valery, P.C.; Garvey, G.; Fong, K.M.; Ball, D.; et al. Psychological distress and quality of life in lung cancer: The role of health-related stigma, illness appraisals and social constraints. Psychooncology 2015, 24, 1569–1577. [Google Scholar] [CrossRef]
- Marlow, L.A.; Wardle, J. Development of a scale to assess cancer stigma in the non-patient population. BMC Cancer 2014, 14, 285. [Google Scholar] [CrossRef]
- Williamson, T.J.; Rawl, S.M.; Kale, M.S.; Carter-Harris, L. Lung Cancer Screening and Stigma: Do Smoking-related Differences in Perceived Lung Cancer Stigma Emerge Prior to Diagnosis? Stigma Health 2023, 8, 497–500. [Google Scholar] [CrossRef]
- Hamann, H.A.; Ostroff, J.S.; Marks, E.G.; Gerber, D.E.; Schiller, J.H.; Lee, S.J.C. Stigma among patients with lung cancer: A patient-reported measurement model. Psychooncology 2014, 23, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Homberg, J.R.; De Boer, S.F.; Raasø, H.S.; Olivier, J.D.A.; Verheul, M.; Ronken, E.; Cools, A.R.; Ellenbroek, B.A.; Schoffelmeer, A.N.M.; Vanderschuren, L.J.M.J.; et al. Adaptations in pre- and postsynaptic 5-HT1A receptor function and cocaine supersensitivity in serotonin transporter knockout rats. Psychopharmacology 2008, 200, 367–380. [Google Scholar] [CrossRef] [PubMed]
- Winkelman, T.N.A.; Admon, L.K.; Jennings, L.; Shippee, N.D.; Richardson, C.R.; Bart, G. Evaluation of Amphetamine-Related Hospitalizations and Associated Clinical Outcomes and Costs in the United States. JAMA Netw. Open 2018, 1, e183758. [Google Scholar] [CrossRef]
- Chiappini, S.; Guirguis, A.; John, A.; Corkery, J.M.; Schifano, F. COVID-19: The Hidden Impact on Mental Health and Drug Addiction. Front. Psychiatry 2020, 11, 767. [Google Scholar] [CrossRef]
- Lichtenstein, M.B.; Nielsen, R.O.; Gudex, C.; Hinze, C.J.; Jørgensen, U. Exercise addiction is associated with emotional distress in injured and non-injured regular exercisers. Addict. Behav. Rep. 2018, 8, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Frost, E.A.M.; Gist, R.S.; Adriano, E. Drugs, alcohol, pregnancy, and the fetal alcohol syndrome. Int. Anesthesiol. Clin. 2011, 49, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. Factors Associated with Smartphone Addiction Tendency in Korean Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 11668. [Google Scholar] [CrossRef]
- Wang, Y.; Teng, H.; Sapozhnikov, D.M.; Du, Q.; Zhao, M. Transcriptome Sequencing Reveals Candidate NF-κB Target Genes Involved in Repeated Cocaine Administration. Int. J. Neuropsychopharmacol. 2018, 21, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Parés-Bayerri, A.; Calvo, F.; Font-Mayolas, S.; Panadero, S.; Vázquez, J.J. Differences in Drug Use among Persons Experiencing Homelessness According to Gender and Nationality. Int. J. Environ. Res. Public Health 2023, 20, 4007. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, C.; Browne, M.; Hing, N.; Rockloff, M.; Hilbrecht, M. Trajectories of wellbeing in people who live with gamblers experiencing a gambling problem: An 18-year longitudinal analysis of the Household, Income and Labour Dynamics in Australia (HILDA) survey. PLoS ONE 2023, 18, e0281099. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.E.; Aliabadi, M.; Golmohammadi, R.; Shafiee, M.S. Experimental study of the sound emission pattern based on acoustic characteristics in typical industrial manufactories in Hamadan, Iran. J. Occup. Hyg. Eng. 2023, 10, 1–8. [Google Scholar] [CrossRef]
- Atroszko, P.A.; Sawicki, A.; Kamble, S. Cross-cultural pilot study on the relationship between study addiction and narcissism among undergraduate students in Poland and India. Health Psychol. Rep. 2019, 7, 325–333. [Google Scholar] [CrossRef]
- Akintola, A.I.; Ada, J.A.; Angioha, P.U.; Ibioro, F.E.; Igwe-Okomiso, J.B.; Bisong, K.B.; Ogunsola, O.V. Illicit Drug Addiction and Efficacy of Employees in the Hospitality Industry. ARRUS J. Social Sci. Humanit. 2021, 2, 1–12. [Google Scholar] [CrossRef]
- Kassew, T.; Tarekegn, G.E.; Alamneh, T.S.; Kassa, S.F.; Liyew, B.; Terefe, B. The prevalence and determinant factors of substance use among the youth in Ethiopia: A multilevel analysis of Ethiopian Demographic and Health Survey. Front. Psychiatry 2023, 14, 1096863. [Google Scholar] [CrossRef]
- Hughes, D.; Colvin, E.; Bartkowiak-Théron, I. Police and Vulnerability in Bail Decisions. Int. J. Crime. Justice Soc. Democracy 2022, 11, 122–138. [Google Scholar] [CrossRef]
- Bell, J.A.H.; Kelly, M.T.; Gelmon, K.; Chi, K.; Ho, A.; Rodney, P.; Balneaves, L.G. Gatekeeping in cancer clinical trials in Canada: The ethics of recruiting the “ideal” patient. Cancer Med. 2020, 9, 4107–4113. [Google Scholar] [CrossRef]
- Cagle, J.G.; Carr, D.C.; Hong, S.; Zimmerman, S. Financial burden among US households affected by cancer at the end of life. Psychooncology 2016, 25, 919–926. [Google Scholar] [CrossRef]
- Hastert, T.A.; Young, G.S.; Pennell, M.L.; Padamsee, T.; Zafar, S.Y.; DeGraffinreid, C.; Naughton, M.; Simon, M.; Paskett, E.D. Financial burden among older, long-term cancer survivors: Results from the LILAC study. Cancer Med. 2018, 7, 4261–4272. [Google Scholar] [CrossRef]
- Danhauer, S.C.; Canzona, M.; Tucker-Seeley, R.D.; Reeve, B.B.; Nightingale, C.L.; Howard, D.S.; Puccinelli-Ortega, N.; Little-Greene, D.; Salsman, J.M. Stakeholder-informed conceptual framework for financial burden among adolescents and young adults with cancer. Psychooncology 2022, 31, 597–605. [Google Scholar] [CrossRef] [PubMed]
- McCaffrey, N.; Engel, L. Protocol for a systematic review of the financial burden experienced by people affected by head and neck cancer. BMJ Open 2022, 12, e055213. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, C.L.; Canzona, M.R.; Danhauer, S.C.; Reeve, B.B.; Howard, D.S.; Tucker-Seeley, R.D.; Golden, S.L.S.; Little-Greene, D.; Roth, M.E.; Victorson, D.E.; et al. Financial burden for caregivers of adolescents and young adults with cancer. Psychooncology 2022, 31, 1354–1364. [Google Scholar] [CrossRef] [PubMed]
- Sedgewick, F.; Leppanen, J.; Tchanturia, K. Gender differences in mental health prevalence in autism. Adv. Autism. 2021, 7, 208–224. [Google Scholar] [CrossRef]
- Browne, M.A.O.; Wells, J.E.; Scott, K.M.; Mcgee, M.A. New Zealand Mental Health Survey Research Team. Lifetime prevalence and projected lifetime risk of DSM-IV disorders in Te Rau Hinengaro: The New Zealand Mental Health Survey. Aust. N. Z. J. Psychiatry 2006, 40, 865–874. [Google Scholar] [CrossRef]
- Elnahas, W.; Hadidy, E.; Hegazy, M.A.; Hafez, M.T.; Refky, B.; Wahab, A. Psychiatric morbidity among Egyptian breast cancer patients and their partners and its impact on surgical decision-making. Breast Cancer 2012, 4, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.; Kalia, S.; Itrat, A.; Khan, A.; Kamal, M.; A Khan, M.; Khalid, R.; Khalid, S.; Javed, S.; Umer, A.; et al. Prevalence and demographics of anxiety disorders: A snapshot from a community health centre in Pakistan. Ann. Gen. Psychiatry 2007, 6, 30. [Google Scholar] [CrossRef] [PubMed]
- Etindele-Sosso, F.A. Insomnia, excessive daytime sleepiness, anxiety, depression and socioeconomic status among customer service employees in Canada. Sleep Sci. 2020, 13, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Menon, S.B.; Jayan, C. An assessment of the mental health of mastectomized women in South India. Psychol. Community Health 2016, 5, 214–228. [Google Scholar] [CrossRef]
- Lépine, J.P.; Pélissolo, A. Why take social anxiety disorder seriously? Depress. Anxiety 2000, 11, 87–92. [Google Scholar] [CrossRef]
- Shafi, S.; Sshah, M.; Shafi, J.; Shah, M.; Khan, A.W. Psychological impact of cancer on patients in a tertiary care centre: A prospective study. Int. J. Res. Med. Sci. 2019, 7, 2116–2120. [Google Scholar] [CrossRef]
- Davis, L.L.; Schein, J.; Cloutier, M.; Gagnon-Sanschagrin, P.; Maitland, J.; Urganus, A.; Guerin, A.; Lefebvre, P.; Houle, C.R. The Economic Burden of Posttraumatic Stress Disorder in the United States from a Societal Perspective. J. Clin. Psychiatry 2022, 83, 21m14116. [Google Scholar] [CrossRef]
- Brenner, L.; Köllner, V.; Bachem, R. Symptom burden and work-related impairment among patients with PTSD and complex PTSD. Eur. J. Psychotraumatol. 2019, 10, 1694766. [Google Scholar] [CrossRef]
- Nipp, R.D.; El-Jawahri, A.; D’Arpino, S.M.; Chan, A.; Fuh, C.; Johnson, P.C.; Lage, D.E.; Wong, R.L.; Pirl, W.F.; Traeger, L.; et al. Symptoms of posttraumatic stress disorder among hospitalized patients with cancer. Cancer 2018, 124, 3445–3453. [Google Scholar] [CrossRef]
- El-Jawahri, A.; Traeger, L.; Greer, J.A.; VanDusen, H.; Fishman, S.R.; LeBlanc, T.W.; Pirl, W.; Jackson, V.A.; Telles, J.; Rhodes, A.; et al. Effect of Inpatient Palliative Care During Hematopoietic Stem-Cell Transplant on Psychological Distress 6 Months After Transplant: Results of a Randomized Clinical Trial. J. Clin. Oncol. 2017, 35, 3714–3721. [Google Scholar] [CrossRef]
- Al Jadili, M.; Thabet, A.A. The Relationship Between Post-Traumatic Stress Disorder and Coping Strategies among Patients with Cancer in Gaza Strip. J. Nurs. Health Stud. 2017, 2, 1. [Google Scholar] [CrossRef]
- Calhoun, P.S.; Beckham, J.C.; Bosworth, H.B. Caregiver burden and psychological distress in partners of veterans with chronic posttraumatic stress disorder. J. Trauma. Stress 2002, 15, 205–212. [Google Scholar] [CrossRef]
- Wolcott, D.L.; Jacobsen, P.B.; Loscalzo, M.J. Supportive Oncology: New Models for the Role of Psychiatry in Cancer Care. J. Lifelong Learn. Psychiatry 2013, 11, 471. [Google Scholar] [CrossRef]
- Holmes, S.C.; Callinan, L.; Facemire, V.C.; Williams, M.T.; Ciarleglio, M.M.; Smith, M.V. Material hardship is associated with posttraumatic stress disorder symptoms among low-income Black women. J. Trauma. Stress 2021, 34, 905–916. [Google Scholar] [CrossRef]
- Citero, V.d.A.; Nogueira-Martins, L.A.; Lourenço, M.T.; Andreoli, S.B. Clinical and demographic profile of cancer patients in a consultation-liaison psychiatric service. Sao Paulo Med. J. 2003, 121, 111–116. [Google Scholar] [CrossRef]
- Mayer, S.; Teufel, M.; Schaeffeler, N.; Keim, U.; Garbe, C.; Eigentler, T.K.; Zipfel, S.; Forschner, A. The need for psycho-oncological support for melanoma patients: Central role of patients’ self-evaluation. Medicine 2017, 96, e7987. [Google Scholar] [CrossRef]
- Segal, E.M.; Bates, J.; Fleszar, S.L.; Holle, L.M.; Kennerly-Shah, J.; Rockey, M.; Jeffers, K.D. Demonstrating the value of the oncology pharmacist within the healthcare team. J. Oncol. Pharm. Pract. 2019, 25, 1945–1967. [Google Scholar] [CrossRef] [PubMed]
- Broom, A.; Wong, W.K.T.; Kirby, E.; Sibbritt, D.; Karikios, D.; Harrup, R.; Lwin, Z. A Qualitative Study of Medical Oncologists’ Experiences of Their Profession and Workforce Sustainability. PLoS ONE 2016, 11, e0166302. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chierzi, F.; Stivanello, E.; Musti, M.A.; Perlangeli, V.; Marzaroli, P.; De Rossi, F.; Pandolfi, P.; Saponaro, A.; Grassi, L.; Murri, M.B.; et al. Cancer mortality in Common Mental Disorders: A 10-year retrospective cohort study. Soc. Psychiatry Psychiatr. Epidemiol. 2023, 58, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Mattes, M.D.; Patel, K.R.; Burt, L.M.; Hirsch, A.E. A Nationwide Medical Student Assessment of Oncology Education. J. Cancer Educ. 2016, 31, 679–686. [Google Scholar] [CrossRef]
- Kline, N.; Thom, B. The Lived Experience of Grief, Loss, and Coping Among Pediatric Oncology Nurses. J. Pain Symptom Manag. 2011, 41, 292. [Google Scholar] [CrossRef]
- Holle, L.M.; Harris, C.S.; Chan, A.; Fahrenbruch, R.J.; Labdi, B.A.; Mohs, J.E.; Norris, L.B.; Perkins, J.; Vela, C.M. Pharmacists’ roles in oncology pharmacy services: Results of a global survey. J. Oncol. Pharm. Pract. 2017, 23, 185–194. [Google Scholar] [CrossRef]
- Brunner, M.; Krautz, C.; Kersting, S.; Weber, G.F.; Stinner, B.; Benz, S.R.; Grützmann, R. Oncological colorectal surgery during the COVID-19pandemic-a national survey. Int. J. Color. Dis. 2020, 35, 2219–2225. [Google Scholar] [CrossRef]
- Mehnert, A.; Koch, U. Psychosocial care of cancer patients—International differences in definition, healthcare structures, and therapeutic approaches. Support. Care Cancer 2005, 13, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Williamson, T.S. The shift of oncology inpatient care to outpatient care: The challenge of retaining expert oncology nurses. Clin. J. Oncol. Nurs. 2008, 12, 186–189. [Google Scholar] [CrossRef]
- Morrison, E.J.; Novotny, P.J.; Sloan, J.A.; Yang, P.; Patten, C.A.; Ruddy, K.J.; Clark, M.M. Emotional Problems, Quality of Life, and Symptom Burden in Patients with Lung Cancer. Clin. Lung Cancer 2017, 18, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Paice, J.A. Cancer pain management and the opioid crisis in America: How to preserve hard-earned gains in improving the quality of cancer pain management. Cancer 2018, 124, 2491–2497. [Google Scholar] [CrossRef] [PubMed]
| Factor | Explanation |
|---|---|
| Individualized approach | Tailor treatment plans to the specific combination of mental disorder and cancer, taking into account individual needs, preferences, and values. |
| Collaborative care | Facilitate communication between oncology and mental health professionals to ensure comprehensive and coordinated support. |
| Clear and empathetic communication | Ensure a sensitive communication style and that information is conveyed clearly and sensitively to reduce anxiety. |
| Mental health stability assessment | Assess the stability of a patient’s mental health before starting cancer treatment, working with mental health professionals. |
| Regular mental health check-ups | Conduct routine mental health check-ups during medical appointments to address concerns immediately and provide ongoing sup-port. |
| Support coping mechanisms | Identify and encourage the integration of adaptive coping mechanisms for managing mental health throughout cancer treatment. |
| Informed consent and shared decision making | Facilitate informed decision making by discussing the potential impact of cancer treatment on mental health and involving those affected in shared decision making. |
| Managing stigma and fears | Acknowledge and address the stigma associated with mental health and cancer by encouraging open discussions and providing accurate information. |
| Family and social support | Recognize the importance of a support network and involve family and friends to actively participate in emotional care and support. |
| Survivorship planning | Discuss survivorship planning issues early, including concerns about cancer recurrence and long-term side effects, and emphasize ongoing mental health support. |
| Planning for end-of-life and palliative care | Approach end-of-life conversations sensitively and work with palliative care teams to address emotional needs in advanced stages of cancer. |
| Accessible mental health resources | Ensure access to mental health resources and provide information about support groups, counseling services, and crisis intervention throughout the cancer journey. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Więckiewicz, G.; Weber, S.; Florczyk, I.; Gorczyca, P. Socioeconomic Burden of Psychiatric Cancer Patients: A Narrative Review. Cancers 2024, 16, 1108. https://doi.org/10.3390/cancers16061108
Więckiewicz G, Weber S, Florczyk I, Gorczyca P. Socioeconomic Burden of Psychiatric Cancer Patients: A Narrative Review. Cancers. 2024; 16(6):1108. https://doi.org/10.3390/cancers16061108
Chicago/Turabian StyleWięckiewicz, Gniewko, Sophie Weber, Iga Florczyk, and Piotr Gorczyca. 2024. "Socioeconomic Burden of Psychiatric Cancer Patients: A Narrative Review" Cancers 16, no. 6: 1108. https://doi.org/10.3390/cancers16061108
APA StyleWięckiewicz, G., Weber, S., Florczyk, I., & Gorczyca, P. (2024). Socioeconomic Burden of Psychiatric Cancer Patients: A Narrative Review. Cancers, 16(6), 1108. https://doi.org/10.3390/cancers16061108







