CPX-351 Pharmacokinetics and Safety in Adults with Hematologic Malignancies and Renal Function Impairment: Phase 1 Trial
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Treatment
2.3. Endpoints
2.4. Statistical Analysis
3. Results
3.1. Patients
3.2. Exposure
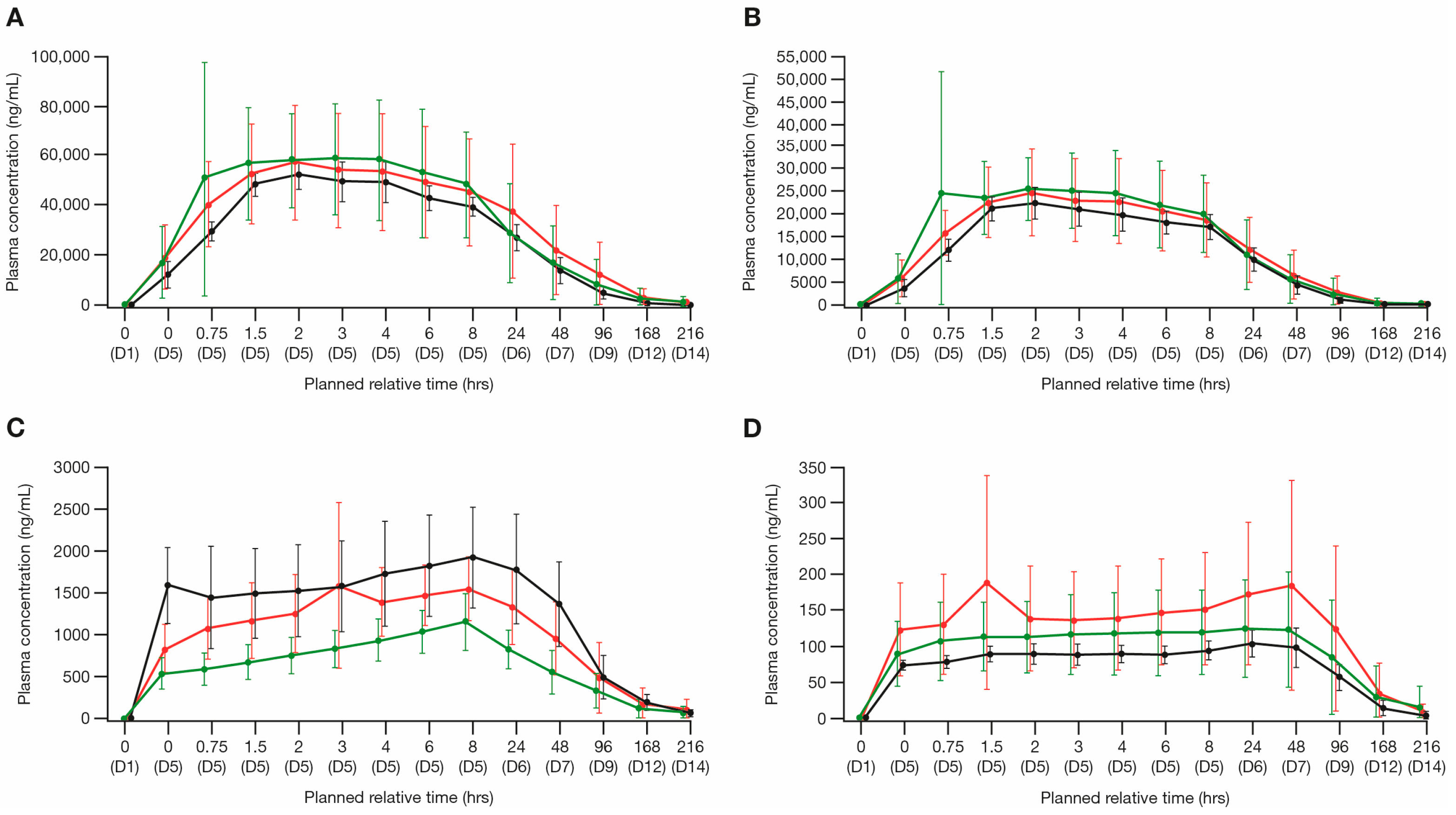
3.3. Pharmacokinetics of CPX-351
3.3.1. Cytarabine and Ara-U
3.3.2. Daunorubicin and Daunorubicinol
3.4. Safety and Tolerability
3.5. Efficacy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chanias, I.; Stojkov, K.; Stehle, G.T.; Daskalakis, M.; Simeunovic, H.; Njue, L.M.; Schnegg-Kaufmann, A.S.; Porret, N.A.; Allam, R.; Rao, T.N.; et al. Myelodysplastic syndromes in the postgenomic era and future perspectives for precision medicine. Cancers 2021, 13, 3296. [Google Scholar] [CrossRef] [PubMed]
- Liu, H. Emerging agents and regimens for AML. J. Hematol. Oncol. 2021, 14, 49. [Google Scholar] [CrossRef] [PubMed]
- Terwilliger, T.; Abdul-Hay, M. Acute lymphoblastic leukemia: A comprehensive review and 2017 update. Blood Cancer J. 2017, 7, e577. [Google Scholar] [CrossRef] [PubMed]
- Cortes, J.E.; Goldberg, S.L.; Feldman, E.J.; Rizzeri, D.A.; Hogge, D.E.; Larson, M.; Pigneux, A.; Recher, C.; Schiller, G.; Warzocha, K.; et al. Phase II, multicenter, randomized trial of CPX-351 (cytarabine:daunorubicin) liposome injection versus intensive salvage therapy in adults with first relapse AML. Cancer 2015, 121, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Farag, S.S.; Archer, K.J.; Mrózek, K.; Ruppert, A.S.; Carroll, A.J.; Vardiman, J.W.; Pettenati, M.J.; Baer, M.R.; Qumsiyeh, M.B.; Koduru, P.R.; et al. Pretreatment cytogenetics add to other prognostic factors predicting complete remission and long-term outcome in patients 60 years of age or older with acute myeloid leukemia: Results from Cancer and Leukemia Group B 8461. Blood 2006, 108, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Wu, Y.; Luo, S.; Yang, H.; Li, L.; Zhou, S.; Shen, R.; Lin, H. Efficacy and toxicity of low-dose versus conventional-dose chemotherapy for malignant tumors: A meta-analysis of 6 randomized controlled trials. Asian Pac. J. Cancer Prev. 2017, 18, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Lancet, J.E.; Cortes, J.E.; Hogge, D.E.; Tallman, M.S.; Kovacsovics, T.J.; Damon, L.E.; Komrokji, R.; Solomon, S.R.; Kolitz, J.E.; Cooper, M.; et al. Phase 2 trial of CPX-351, a fixed 5:1 molar ratio of cytarabine/daunorubicin, vs cytarabine/daunorubicin in older adults with untreated AML. Blood 2014, 123, 3239–3246. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Pramanik, R.; Raj, S.; Ahmend, S.; Kumar, L. Acute kidney injury in newly diagnosed acute myeloid leukemia patients undergoing remission induction chemotherapy: Experience of a tertiary cancer centre of India. Ann. Oncol. 2017, 28, X97–X98. [Google Scholar] [CrossRef]
- Ballo, O.; Eladly, F.; Büttner, S.; Stratmann, J.A.; Rudolf, S.; Brunnberg, U.; Kreisel, E.M.; Steffen, B.; Wagner, S.; Finkelmeier, F.; et al. Acute kidney injury adversely affects the clinical course of acute myeloid leukemia patients undergoing induction chemotherapy. Ann. Hematol. 2021, 100, 1159–1167. [Google Scholar] [CrossRef] [PubMed]
- Lahoti, A.; Kantarjian, H.; Salahudeen, A.K.; Ravandi, F.; Cortes, J.E.; Faderl, S.; O’Brien, S.; Wierda, W.; Mattiuzzi, G.N. Predictors and outcome of acute kidney injury in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome. Cancer 2010, 116, 4063–4068. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.L.C.; de Brito, B.B.; da Silva, F.A.F.; Botelho, A.C.D.S.; de Melo, F.F. Nephrotoxicity in cancer treatment: An overview. World J. Clin. Oncol. 2020, 11, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Krens, S.D.; Lassche, G.; Jansman, F.G.A.; Desar, I.M.E.; Lankheet, N.A.G.; Burger, D.M.; van Herpen, C.M.L.; van Erp, N.P. Dose recommendations for anticancer drugs in patients with renal or hepatic impairment. Lancet Oncol. 2019, 20, e200–e207. [Google Scholar] [CrossRef] [PubMed]
- Statler, A.; Radivoyevitch, T.; Siebenaller, C.; Gerds, A.T.; Kalaycio, M.; Kodish, E.; Mukherjee, S.; Cheng, C.; Sekeres, M.A. The relationship between eligibility criteria and adverse events in randomized controlled trials of hematologic malignancies. Leukemia 2017, 31, 1808–1815. [Google Scholar] [CrossRef] [PubMed]
- Tardi, P.; Johnstone, S.; Harasym, N.; Xie, S.; Harasym, T.; Zisman, N.; Harvie, P.; Bermudes, D.; Mayer, L. In vivo maintenance of synergistic cytarabine:daunorubicin ratios greatly enhances therapeutic efficacy. Leuk. Res. 2009, 33, 129–139. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Vyxeos Liposomal Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/vyxeos-liposomal-epar-product-information_en.pdf (accessed on 14 March 2023).
- Jazz Pharmaceuticals Inc. VYXEOS® (Daunorubicin and Cytarabine) Prescribing Information. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/209401s011lbl.pdf (accessed on 14 March 2023).
- Jazz Pharmaceuticals Canada Inc. Vyxeos® (Daunorubicin and Cytarabine Liposome for Injection) Product Monograph. Available online: https://pp.jazzpharma.com/pi/vyxeos.ca.PM-en.pdf (accessed on 28 February 2023).
- Wang, Q.; Banerjee, K.; Vasilinin, G.; Marier, J.F.; Gibbons, J.A. Population pharmacokinetics and exposure-response analyses for CPX-351 in patients with hematologic malignancies. J. Clin. Pharmacol. 2019, 59, 748–762. [Google Scholar] [CrossRef] [PubMed]
- Cockcroft, D.W.; Gault, M.H. Prediction of creatinine clearance from serum creatinine. Nephron 1976, 16, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Lancet, J.E.; Uy, G.L.; Cortes, J.E.; Newell, L.F.; Lin, T.L.; Ritchie, E.K.; Stuart, R.K.; Strickland, S.A.; Hogge, D.; Solomon, S.R.; et al. CPX-351 (cytarabine and daunorubicin) liposome for injection versus conventional cytarabine plus daunorubicin in older patients with newly diagnosed secondary acute myeloid leukemia. J. Clin. Oncol. 2018, 36, 2684–2692. [Google Scholar] [CrossRef] [PubMed]
- Lancet, J.E.; Uy, G.L.; Newell, L.F.; Lin, T.L.; Ritchie, E.K.; Stuart, R.K.; Strickland, S.A.; Hogge, D.; Solomon, S.R.; Bixby, D.L.; et al. CPX-351 versus 7+3 cytarabine and daunorubicin chemotherapy in older adults with newly diagnosed high-risk or secondary acute myeloid leukaemia: 5-year results of a randomised, open-label, multicentre, phase 3 trial. Lancet Haematol. 2021, 8, e481–e491. [Google Scholar] [CrossRef] [PubMed]
- Kitchlu, A.; Shapiro, J.; Amir, E.; Garg, A.X.; Kim, S.J.; Wald, R.; Harel, Z. Representation of patients with chronic kidney disease in trials of cancer therapy. JAMA 2018, 319, 2437–2439. [Google Scholar] [CrossRef] [PubMed]
| Cohort 1: Normal Renal Function (n = 7) | Cohort 2: Moderate Renal Impairment (n = 8) | Cohort 3: Severe Renal Impairment (n = 6) | |
|---|---|---|---|
| Median age at baseline, years (min, max) | 67 (62, 76) | 69 (60, 77) | 74 (58, 85) |
| Male, n (%) | 5 (71) | 6 (75) | 3 (50) |
| Diagnosis, n (%) | |||
| AML | 5 (71) | 7 (88) | 6 (100) |
| Newly diagnosed | 5 (71) | 6 (75) | 5 (83) |
| De novo AML | 2 (29) | 2 (25) | 4 (67) |
| Secondary AML | 3 (43) | 4 (50) | 1 (17) |
| Refractory/relapsed | 0 | 1 (13) | 1 (17) |
| MDS | 2 (29) | 1 (13) | 0 |
| Race, n (%) | |||
| Black or African American | 0 | 2 (25) | 1 (17) |
| White | 7 (100) | 6 (75) | 5 (83) |
| Ethnicity, n (%) | |||
| Not Hispanic or Latino | 7 (100) | 8 (100) | 6 (100) |
| BSA (m2) a | |||
| Mean (SD) | 2.27 (0.16) | 1.98 (0.20) | 1.83 (0.30) |
| ECOG Performance Status, n (%) | |||
| 0 | 2 (29) | 0 | 0 |
| 1 | 2 (29) | 7 (88) | 3 (50) |
| 2 | 3 (43) | 1 (13) | 3 (50) |
| CrCl (mL/min) | |||
| Mean (SD) | 125.89 (28.73) | 47.49 (5.79) | 23.20 (4.12) |
| eGFR (mL/min/1.73 m2) | |||
| Mean (SD) | 86.00 (18.61) | 40.23 (8.51) | 21.86 (2.21) |
| Ratio (%) of Test/Reference | ||||
|---|---|---|---|---|
| Analyte Comparison | PK Parameter | Estimate | 90% CI | CV% |
| Cytarabine | ||||
| Cohort 2 vs. Cohort 1 | AUCtau (h × ng/mL) | 91.56 | (43.62–192.18) | 98.9 |
| Cmax (ng/mL) | 79.60 | (51.68–122.60) | 51.1 | |
| Cohort 3 vs. Cohort 1 | AUCtau (h × ng/mL) | 100.38 | (45.24–222.74) | 98.9 |
| Cmax (ng/mL) | 79.28 | (49.83–126.13) | 51.1 | |
| Daunorubicin | ||||
| Cohort 2 vs. Cohort 1 | AUCtau (h × ng/mL) | 94.44 | (52.24–170.73) | 73.9 |
| Cmax (ng/mL) | 77.53 | (52.36–114.78) | 45.9 | |
| Cohort 3 vs. Cohort 1 | AUCtau (h × ng/mL) | 97.04 | (51.35–183.40) | 73.9 |
| Cmax (ng/mL) | 74.54 | (48.88–113.65) | 45.9 | |
| Parameter a | Cohort 1: Normal Renal Function (n = 7) | Cohort 2: Moderate Renal Impairment (n = 8) | Cohort 3: Severe Renal Impairment (n = 6) |
|---|---|---|---|
| Cytarabine | |||
| Ae (µg) | 2066 (1856 ± 2163) b | 1524 (1203 ± 889.6) | NC (NC) |
| CLR (mL/h) | 1.387 (1.873 ± 2.645) c | 1.688 (2.526 ± 4.842) | NC (NC) c |
| Ara-U | |||
| Ae (µg) | 121,900 (123,000 ± 17,750) | 126,700 (132,200 ± 39,680) | 117,100 (123,000 ± 41,010) |
| Cytarabine and Ara-U | |||
| Ae_total | 123,200 (124,500 ± 19,740) | 127,200 (132,800 ± 40,080) | 116,600 (122,500 ± 40,780) |
| Ae% | 55.80 (56.05 ± 5.941) | 64.98 (68.04 ± 21.46) | 63.70 (67.32 ± 21.63) |
| Daunorubicin | |||
| Ae (µg) | 2481 (2567 ± 675.9) | 1314 (1345 ± 309.1) | 718.8 (899.6 ± 654.0) |
| CLR (mL/h) | 4.810 (5.942 ± 3.719) d | 2.653 (4.410 ± 6.325) | 1.381 (1.777 ± 1.365) d |
| Daunorubicinol | |||
| Ae (µg) | 5944 (6015 ± 982.2) | 3570 (3936 ± 1865) | 1586 (1761 ± 877.3) |
| Daunorubicin and daunorubicinol | |||
| Ae_total | 8432 (8563 ± 1594) d | 4937 (5265 ± 2035) | 2332 (2654 ± 1497) d |
| Ae% | 8.469 (8.577 ± 1.458) d | 5.733 (6.053 ± 2.027) | 2.893 (3.242 ± 1.737) d |
| Cohort 1: Normal Renal Function (n = 7) | Cohort 2: Moderate Renal Impairment (n = 8) | Cohort 3: Severe Renal Impairment (n = 6) | Overall (N = 21) | |
|---|---|---|---|---|
| Number of TEAEs, n | 141 | 170 | 166 | 477 |
| Number of patients with ≥1 TEAE, n (%) | 7 (100) | 8 (100) | 6 (100) | 21 (100) |
| Febrile neutropenia | 5 (71.4) | 6 (75.0) | 1 (16.7) | 12 (57.1) |
| Nausea | 4 (57.1) | 5 (62.5) | 3 (50.0) | 12 (57.1) |
| Hyperglycemia | 3 (42.9) | 2 (25.0) | 4 (66.7) | 9 (42.9) |
| Anemia | 4 (57.1) | 2 (25.0) | 2 (33.3) | 8 (38.1) |
| Fatigue | 2 (28.6) | 4 (50.0) | 2 (33.3) | 8 (38.1) |
| Leukopenia | 3 (42.9) | 2 (25.0) | 3 (50.0) | 8 (38.1) |
| Headache | 4 (57.1) | 2 (25.0) | 1 (16.7) | 7 (33.3) |
| Hypertension | 2 (28.6) | 2 (25.0) | 3 (50.0) | 7 (33.3) |
| Hypokalemia | 3 (42.9) | 1 (12.5) | 3 (50.0) | 7 (33.3) |
| Hyponatremia | 3 (42.9) | 2 (25.0) | 2 (33.3) | 7 (33.3) |
| Lymphopenia | 2 (28.6) | 2 (25.0) | 3 (50.0) | 7 (33.3) |
| Edema peripheral | 3 (42.9) | 2 (25.0) | 2 (33.3) | 7 (33.3) |
| Blood bilirubin increased | 3 (42.9) | 2 (25.0) | 1 (16.7) | 6 (28.6) |
| Constipation | 2 (28.6) | 2 (25.0) | 2 (33.3) | 6 (28.6) |
| Hypocalcemia | 1 (14.3) | 2 (25.0) | 3 (50.0) | 6 (28.6) |
| Neutropenia | 1 (14.3) | 2 (25.0) | 3 (50.0) | 6 (28.6) |
| Thrombocytopenia | 2 (28.6) | 2 (25.0) | 2 (33.3) | 6 (28.6) |
| Aspartate aminotransferase increased | 2 (28.6) | 2 (25.0) | 1 (16.7) | 5 (23.8) |
| Contusion | 2 (28.6) | 1 (12.5) | 2 (33.3) | 5 (23.8) |
| Decreased appetite | 2 (28.6) | 1 (12.5) | 2 (33.3) | 5 (23.8) |
| Response, n (%) | Cohort 1: Normal Renal Function (n = 7) | Cohort 2: Moderate Renal Impairment (n = 8) | Cohort 3: Severe Renal Impairment (n = 6) | Overall (N = 21) |
|---|---|---|---|---|
| CR | 2 (28.6) | 1 (12.5) | 3 (50.0) | 6 (28.6) |
| CRi | 2 (28.6) | 3 (37.5) | 0 | 5 (23.8) |
| PD | 3 (42.9) | 2 (25.0) | 2 (33.3) | 7 (33.3) |
| Relapsed | 0 | 0 | 0 | 0 |
| Not assessed | 0 | 2 (25.0) | 1 (16.7) | 3 (14.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Solomon, S.R.; Powell, B.L.; Koprivnikar, J.; Lai, C.; Male, H.; Michaelis, L.C.; Newell, L.F.; Sanford, D.; Jenkins, J.; Zelaya, A.; et al. CPX-351 Pharmacokinetics and Safety in Adults with Hematologic Malignancies and Renal Function Impairment: Phase 1 Trial. Cancers 2024, 16, 915. https://doi.org/10.3390/cancers16050915
Solomon SR, Powell BL, Koprivnikar J, Lai C, Male H, Michaelis LC, Newell LF, Sanford D, Jenkins J, Zelaya A, et al. CPX-351 Pharmacokinetics and Safety in Adults with Hematologic Malignancies and Renal Function Impairment: Phase 1 Trial. Cancers. 2024; 16(5):915. https://doi.org/10.3390/cancers16050915
Chicago/Turabian StyleSolomon, Scott R., Bayard L. Powell, Jamie Koprivnikar, Catherine Lai, Heather Male, Laura C. Michaelis, Laura F. Newell, David Sanford, Jack Jenkins, Amy Zelaya, and et al. 2024. "CPX-351 Pharmacokinetics and Safety in Adults with Hematologic Malignancies and Renal Function Impairment: Phase 1 Trial" Cancers 16, no. 5: 915. https://doi.org/10.3390/cancers16050915
APA StyleSolomon, S. R., Powell, B. L., Koprivnikar, J., Lai, C., Male, H., Michaelis, L. C., Newell, L. F., Sanford, D., Jenkins, J., Zelaya, A., Coppola, S., Faderl, S., & Walter, R. B. (2024). CPX-351 Pharmacokinetics and Safety in Adults with Hematologic Malignancies and Renal Function Impairment: Phase 1 Trial. Cancers, 16(5), 915. https://doi.org/10.3390/cancers16050915






