Continuous Intraoperative Nerve Monitoring of a Non-Recurrent Laryngeal Nerve: Real-Life Data of a High-Volume Thyroid Surgery Center
Abstract
Simple Summary
Abstract
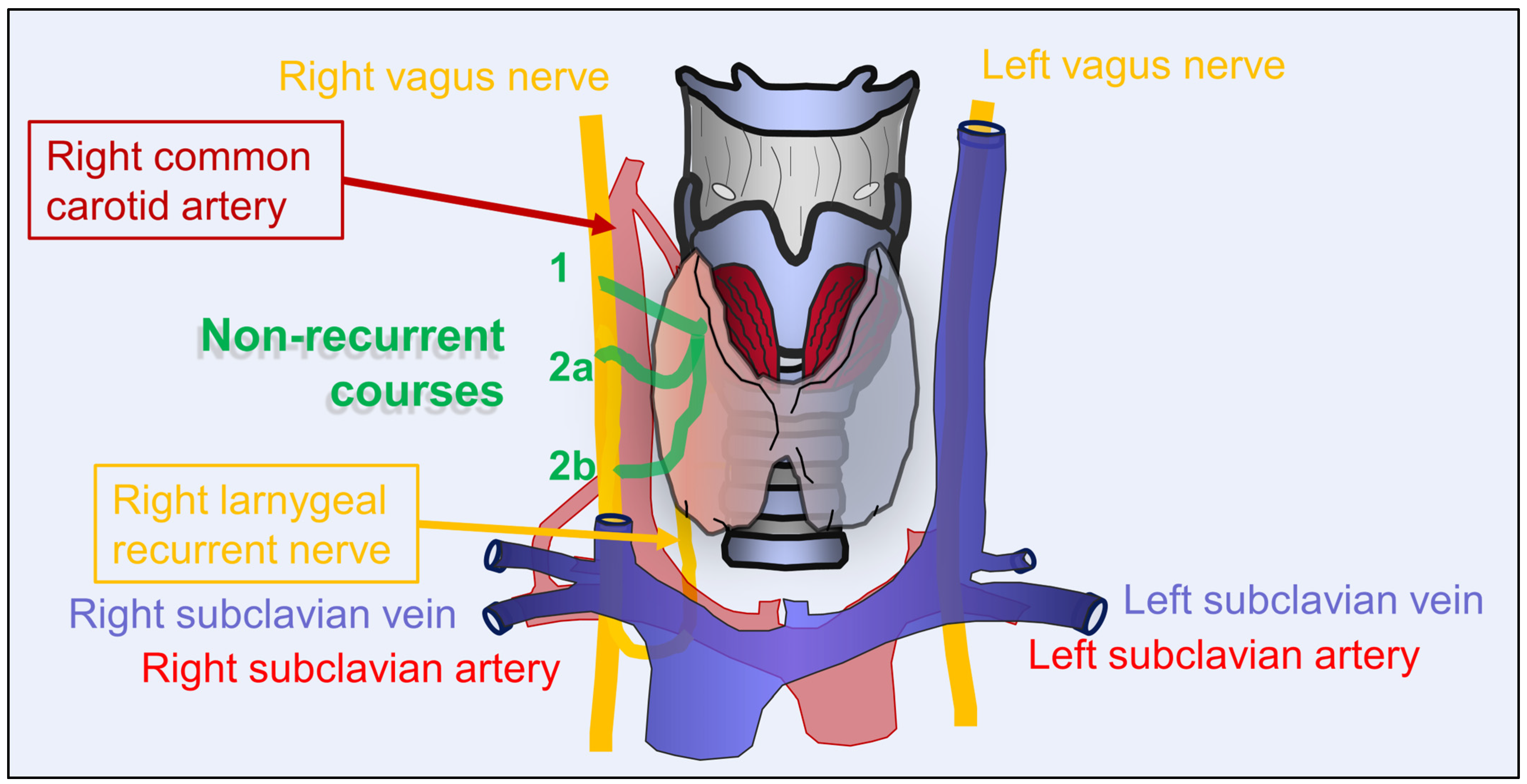
1. Introduction
2. Materials and Methods
Intraoperative Nerve Monitoring
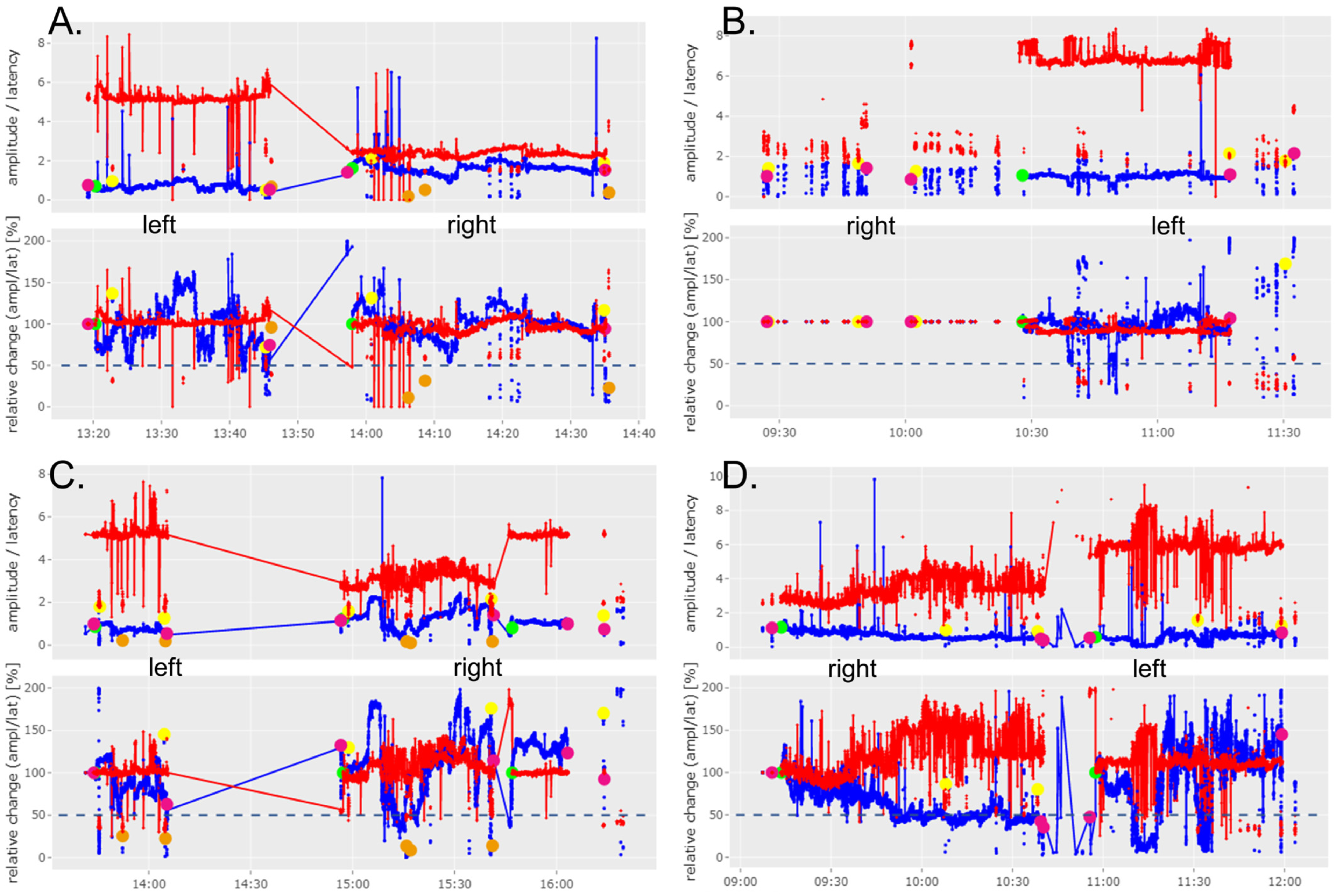
3. Results
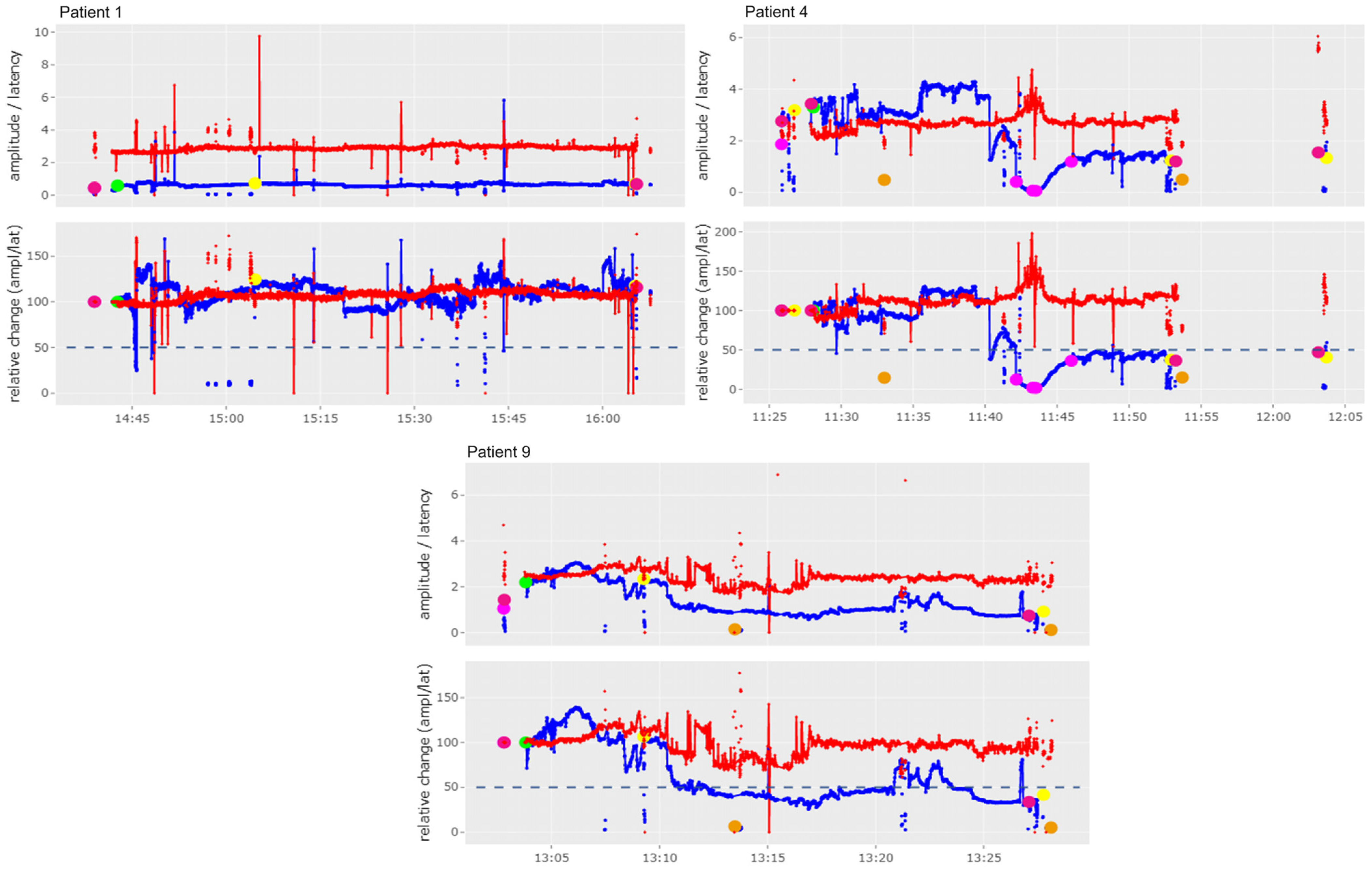
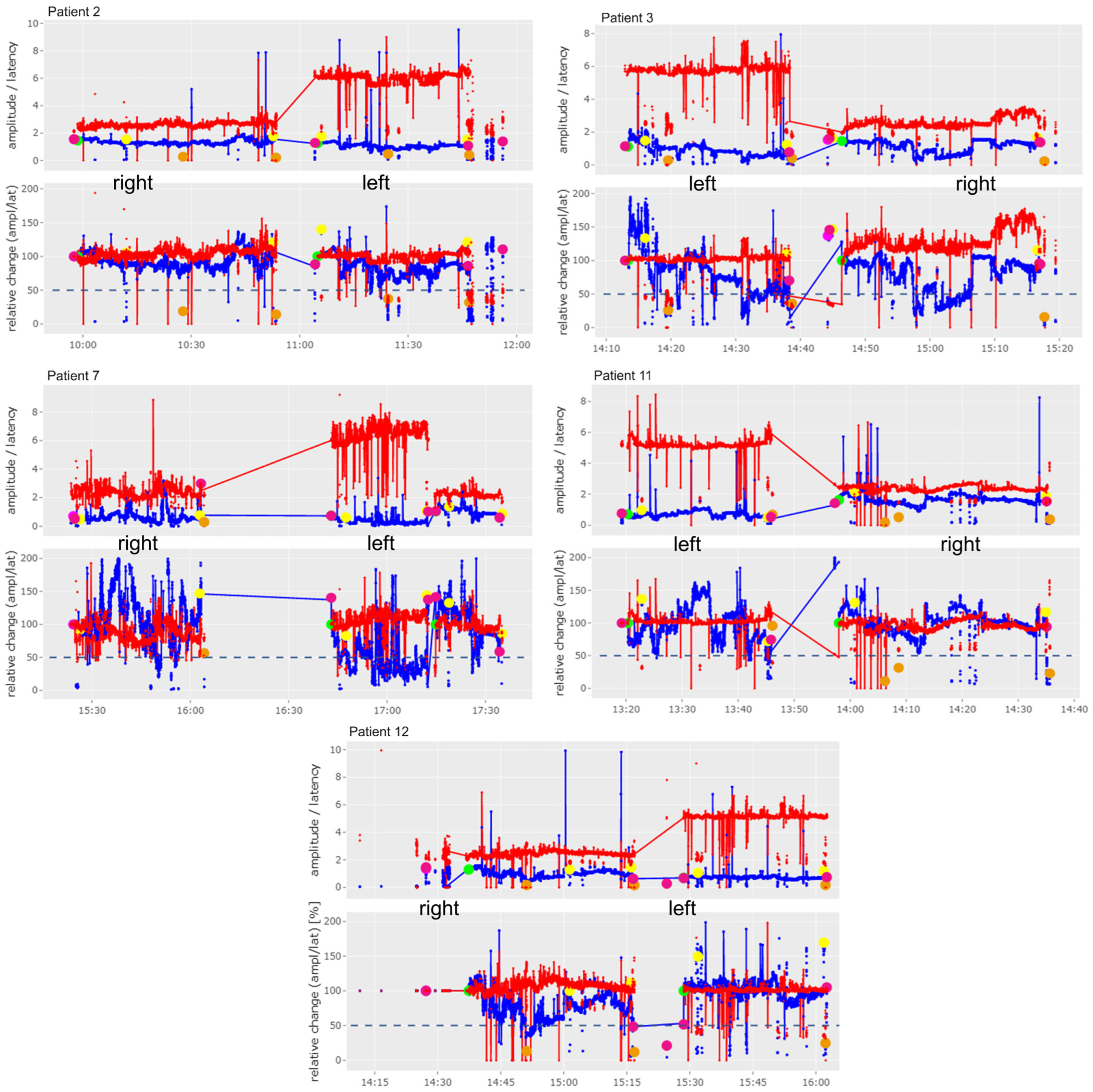
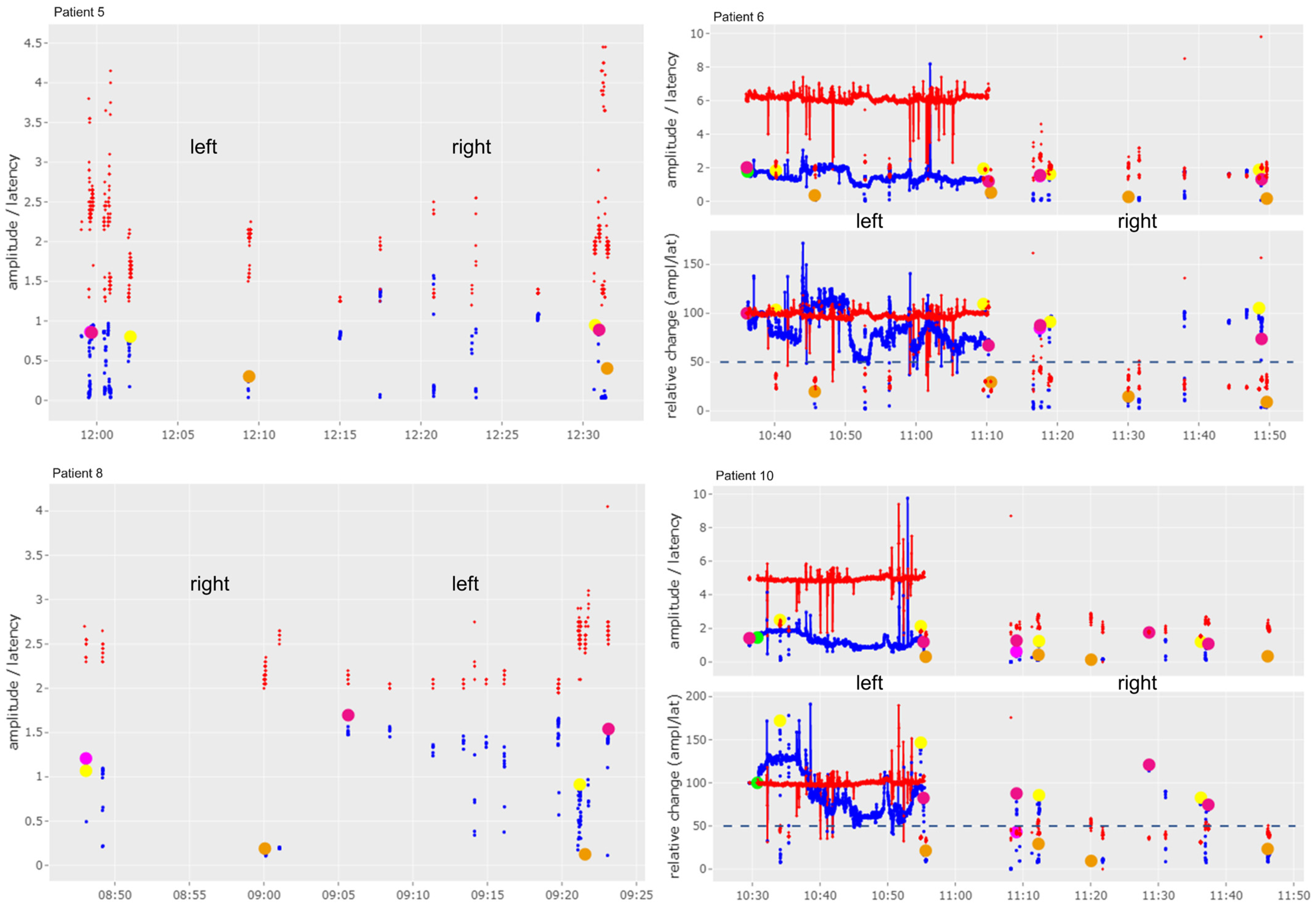
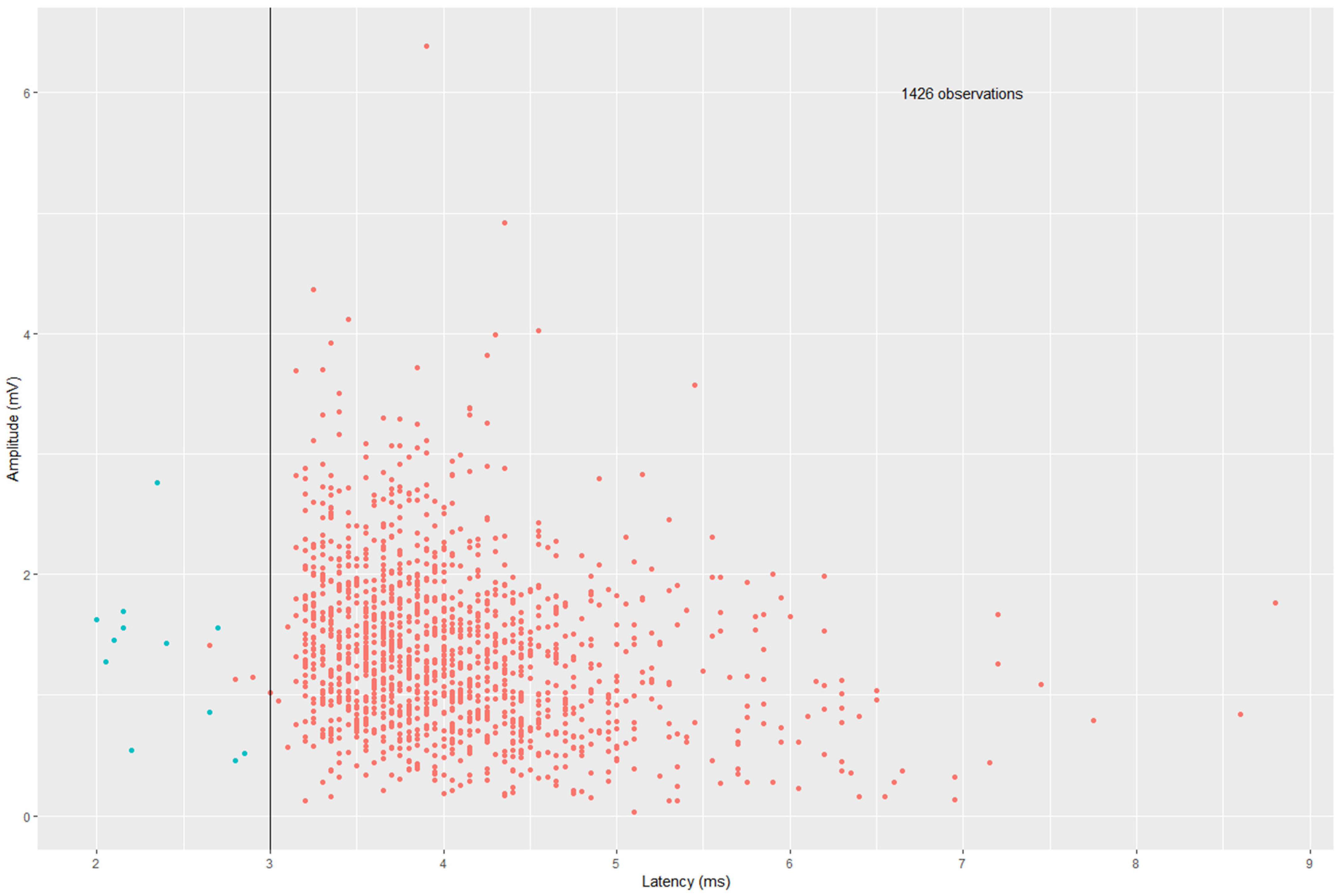
Short Digression: Latency of the Vagus Nerve in Case of NRLN
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial intelligence |
| cIONM | continuous intraoperative nerve monitoring |
| EMG | electromyography |
| IONM | intraoperative nerve monitoring |
| NRLN | non recurrent laryngeal nerve |
| n. s. | not specified |
| PTC | papillary thyroid carcinoma |
| RLN | recurrent laryngeal nerve |
| VCP | vocal cord palsy |
References
- Weiand, G.; Mangold, G. Verlaufsvarietäten des Nervus laryngeus inferior. Die Chir. 2004, 75, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Iacobone, M.; Citton, M.; Pagura, G.; Viel, G.; Nitti, D. Increased and safer detection of nonrecurrent inferior laryngeal nerve after preoperative ultrasonography. Laryngoscope 2015, 125, 1743–1747. [Google Scholar] [CrossRef] [PubMed]
- Toniato, A.; Mazzarotto, R.; Piotto, A.; Bernante, P.; Pagetta, C.; Pelizzo, M.R. Identification of the Nonrecurrent Laryngeal Nerve during Thyroid Surgery: 20-Year Experience. World J. Surg. 2004, 28, 659–661. [Google Scholar] [CrossRef] [PubMed]
- Zheng, V.; Rajeev, R.; Pinto, D.; de Jong, M.C.; Sreenivasan, D.K.; Parameswaran, R. Variant anatomy of non-recurrent laryngeal nerve: When and how should it be taught in surgical residency? Langenbeck’s Arch. Surg. 2023, 408, 185. [Google Scholar] [CrossRef] [PubMed]
- Hermans, R.; Dewandel, P.; Debruyne, F.; Delaere, P.R. Arteria lusoria identified on preoperative CT and nonrecurrent inferior laryngeal nerve during thyroidectomy: A retrospective study. Head Neck 2003, 25, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Sanna, S.; Graves, M.J.; Vikse, J.; Sanna, B.; Tomaszewska, I.M.; Tubbs, R.S.; Walocha, J.A.; Tomaszewski, K.A. The Non-Recurrent Laryngeal Nerve: A meta-analysis and clinical considerations. PeerJ 2017, 5, e3012. [Google Scholar] [CrossRef]
- Kartal, K.; Aygun, N.; Celayir, M.F.; Besler, E.; Citgez, B.; Isgor, A.; Uludag, M. Intraoperative Neuromonitoring in Thyroid Surgery: An Efficient Tool to Avoid Bilateral Vocal Cord Palsy. Ear Nose Throat J. 2021, 100, 694S–699S. [Google Scholar] [CrossRef]
- Gardner, G.M.; Smith, M.M.; Yaremchuk, K.L.; Peterson, E.L. The cost of vocal fold paralysis after thyroidectomy. Laryngoscope 2013, 123, 1455–1463. [Google Scholar] [CrossRef] [PubMed]
- Dralle, H.; Neu, J.; Musholt, T.J.; Nies, C. Bilaterale Stimmlippenparese nach totaler Thyreoidektomie. Die Chir. 2016, 87, 65–68. [Google Scholar] [CrossRef]
- Lisowska, G.; Sowa, P.; Misiolek, H.; Scierski, W.; Misiolek, M. Możliwości naprawcze porażeń fałdów głosowych w wyniku operacji gruczołu tarczowego. Endokrynol. Pol. 2015, 66, 412–416. [Google Scholar] [CrossRef][Green Version]
- Randolph, G.W.; Dralle, H.; Abdullah, H.; Barczynski, M.; Bellantone, R.; Brauckhoff, M.; Carnaille, B.; Cherenko, S.; Chiang, F.; Dionigi, G.; et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: International standards guideline statement. Laryngoscope 2011, 121, S1–S16. [Google Scholar] [CrossRef]
- Staubitz, J.I.; Watzka, F.; Poplawski, A.; Riss, P.; Clerici, T.; Bergenfelz, A.; Musholt, T.J.; Riss, P.; Slycke, S.; Iacobone, M.; et al. Effect of intraoperative nerve monitoring on postoperative vocal cord palsy rates after thyroidectomy: European multicentre registry-based study. BJS Open 2020, 4, 821–829. [Google Scholar] [CrossRef]
- Staubitz, J.I.; Musholt, T.J. Continuous Intraoperative Recurrent Laryngeal Nerve Monitoring: Techniques, Applications, and Controversies. Curr. Otorhinolaryngol. Rep. 2021, 9, 326–333. [Google Scholar] [CrossRef]
- Schneider, R.; Randolph, G.W.; Barczynski, M.; Dionigi, G.; Wu, C.-W.; Chiang, F.-Y.; Machens, A.; Kamani, D.; Dralle, H. Continuous intraoperative neural monitoring of the recurrent nerves in thyroid surgery: A quantum leap in technology. Gland Surg. 2016, 5, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.; Randolph, G.W.; Sekulla, C.; Phelan, E.; Thanh, P.N.; Bucher, M.; Machens, A.; Dralle, H.; Lorenz, K. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck 2013, 35, 1591–1598. [Google Scholar] [CrossRef]
- Sinclair, C.F.; Téllez, M.J.; Ulkatan, S. Continuous Laryngeal Adductor Reflex Versus Intermittent Nerve Monitoring in Neck Endocrine Surgery. Laryngoscope 2021, 131, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.; Randolph, G.; Dionigi, G.; Barczynski, M.; Chiang, F.; Wu, C.; Musholt, T.; Uludag, M.; Makay, Ö.; Sezer, A.; et al. Prediction of Postoperative Vocal Fold Function After Intraoperative Recovery of Loss of Signal. Laryngoscope 2019, 129, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Dionigi, G.; Van Slycke, S.; Boni, L.; Rausei, S.; Mangano, A. Limits of Neuromonitoring in Thyroid Surgery. Ann. Surg. 2013, 258, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.; Randolph, G.W.; Dionigi, G.; Wu, C.; Barczynski, M.; Chiang, F.; Al-Quaryshi, Z.; Angelos, P.; Brauckhoff, K.; Cernea, C.R.; et al. International neural monitoring study group guideline 2018 part I: Staging bilateral thyroid surgery with monitoring loss of signal. Laryngoscope 2018, 128, S1–S17. [Google Scholar] [CrossRef] [PubMed]
- Dralle, H.; Lorenz, K.; Schabram, P.; Musholt, T.J.; Dotzenrath, C.; Goretzki, P.E.; Kußmann, J.; Niederle, B.; Nies, C.; Schabram, J.; et al. Intraoperatives Neuromonitoring in der Schilddrüsenchirurgie. Die Chir. 2013, 84, 1049–1056. [Google Scholar] [CrossRef]
- Musholt, T.J.; Staubitz, J.I.; Musholt, P.B. Evaluation of intraoperative neuromonitoring (IONM) data with the Mainz IONM Quality Assurance and Analysis tool. BJS Open 2023, 7, zrad051. [Google Scholar] [CrossRef]
- Van Slycke, S.; Van Den Heede, K.; Magamadov, K.; Gillardin, J.-P.; Vermeersch, H.; Brusselaers, N. Intra-operative vagal neuromonitoring predicts non-recurrent laryngeal nerves: Technical notes and review of the recent literature. Acta Chir. Belg. 2021, 121, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Brauckhoff, M.; Walls, G.; Brauckhoff, K.; Thanh, P.; Thomusch, O.; Dralle, H. Identification of the non-recurrent inferior laryngeal nerve using intraoperative neurostimulation. Langenbeck’s Arch. Surg. 2002, 386, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Brauckhoff, M.; Machens, A.; Sekulla, C.; Lorenz, K.; Dralle, H. Latencies Shorter than 3.5 ms After Vagus Nerve Stimulation Signify a Nonrecurrent Inferior Laryngeal Nerve Before Dissection. Ann. Surg. 2011, 253, 1172–1177. [Google Scholar] [CrossRef]
- Lin, Y.; Dionigi, G.; Randolph, G.W.; Lu, I.; Chang, P.; Tsai, S.; Kim, H.Y.; Lee, H.Y.; Tufano, R.P.; Sun, H.; et al. Electrophysiologic monitoring correlates of recurrent laryngeal nerve heat thermal injury in a porcine model. Laryngoscope 2015, 125, E283–E290. [Google Scholar] [CrossRef]
- Lorenz, K.; Sekulla, C.; Schelle, J.; Schmeiß, B.; Brauckhoff, M.; Dralle, H. What are normal quantitative parameters of intraoperative neuromonitoring (IONM) in thyroid surgery? Langenbeck’s Arch. Surg. 2010, 395, 901–909. [Google Scholar] [CrossRef]
- Cossa, A.; Castagnola, G.; Romeo, G.; Bellucci, M.; Nigri, G.; Bellotti, C. Utility of intraoperative neuromonitoring in detecting recurrent nerve’s anatomical anomalies during thyroidectomy. Endocrine 2020, 70, 194–197. [Google Scholar] [CrossRef]
- Donatini, G.; Carnaille, B.; Dionigi, G. Increased Detection of Non-recurrent Inferior Laryngeal Nerve (NRLN) During Thyroid Surgery Using Systematic Intraoperative Neuromonitoring (IONM). World J. Surg. 2013, 37, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ji, Q.; Li, D.; Wu, Y.; Zhu, Y.; Huang, C.; Shen, Q.; Wang, Z.; Zhang, L.; Sun, T. Preoperative CT diagnosis of right nonrecurrent inferior laryngeal nerve. Head Neck 2011, 33, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.-J.; Sun, S.-Q.; Wang, X.-L.; Sun, Y.-X.; Huang, H.-X. An applied anatomical study on the recurrent laryngeal nerve and inferior thyroid artery. Surg. Radiol. Anat. 2012, 34, 325–332. [Google Scholar] [CrossRef]
- Gkrinia, E.; Nana, P.; Spanos, K.; Fiska, A.; Hajiioannou, J.; Skoulakis, C.; Zibis, A.H. Anatomical variations of the recurrent laryngeal nerve according to the inferior thyroid artery and their clinical impact in patients undergoing thyroidectomy. J. Laryngol. Otol. 2023, 137, 673–677. [Google Scholar] [CrossRef] [PubMed]
- Stankovic, P.; Wittlinger, J.; Georgiew, R.; Dominas, N.; Hoch, S.; Wilhelm, T. Kontinuierliches intraoperatives Neuromonitoring (cIONM) in der Kopf-Hals-Chirurgie—Eine Übersicht. HNO 2020, 68, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.C. Safety and feasibility of a novel recurrent laryngeal nerve monitoring technique. Laryngoscope 2018, 128, S1–S8. [Google Scholar] [CrossRef] [PubMed]
| No. | Age | Disease | Surgery | Laryngoscopy | |
|---|---|---|---|---|---|
| Preoperative | Postoperative | ||||
| 1 | 27 | PTC | lymphadenectomy | normal | normal |
| 2 | 40 | PTC | thyroidectomy | normal | normal |
| 3 | 49 | multinodular goiter | thyroidectomy | normal | normal |
| 4 | 20 | right nodular goiter | right lobectomy | normal | normal |
| 5 | 17 | right nodular goiter | right lobectomy | normal | normal |
| 6 | 30 | Graves’ disease | thyroidectomy | normal | normal |
| 7 | 34 | right nodular goiter | thyroidectomy | normal | normal |
| 8 | 38 | right nodular goiter | right lobectomy | normal | normal |
| 9 | 16 | right nodular goiter | right lobectomy | normal | normal |
| 10 | 39 | toxic multinodular goiter | thyroidectomy | normal | normal |
| 11 | 57 | Graves’ disease | thyroidectomy | normal | normal |
| 12 | 38 | multinodular goiter | thyroidectomy | normal | normal |
| No. | Vagus Nerve Anatomy * | cIONM | Type of NRLN |
|---|---|---|---|
| 1 | n. s. | yes | 2a |
| 2 | n. s. | yes | 2b |
| 3 | medial dorsal | yes | 2a |
| 4 | medial dorsal | yes | 2a |
| 5 | medial dorsal | no | 1 |
| 6 | medial dorsal | no | 1 |
| 7 | n. s. | yes | 2b |
| 8 | medial | no | 1 |
| 9 | n. s. | yes | 2a |
| 10 | medial | no | 2a |
| 11 | medial dorsal | yes | 2a |
| 12 | n. s. | yes | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lederer, A.-K.; Staubitz-Vernazza, J.I.; Margies, R.; Wild, F.; Musholt, T.J. Continuous Intraoperative Nerve Monitoring of a Non-Recurrent Laryngeal Nerve: Real-Life Data of a High-Volume Thyroid Surgery Center. Cancers 2024, 16, 1007. https://doi.org/10.3390/cancers16051007
Lederer A-K, Staubitz-Vernazza JI, Margies R, Wild F, Musholt TJ. Continuous Intraoperative Nerve Monitoring of a Non-Recurrent Laryngeal Nerve: Real-Life Data of a High-Volume Thyroid Surgery Center. Cancers. 2024; 16(5):1007. https://doi.org/10.3390/cancers16051007
Chicago/Turabian StyleLederer, Ann-Kathrin, Julia I. Staubitz-Vernazza, Rabea Margies, Florian Wild, and Thomas J. Musholt. 2024. "Continuous Intraoperative Nerve Monitoring of a Non-Recurrent Laryngeal Nerve: Real-Life Data of a High-Volume Thyroid Surgery Center" Cancers 16, no. 5: 1007. https://doi.org/10.3390/cancers16051007
APA StyleLederer, A.-K., Staubitz-Vernazza, J. I., Margies, R., Wild, F., & Musholt, T. J. (2024). Continuous Intraoperative Nerve Monitoring of a Non-Recurrent Laryngeal Nerve: Real-Life Data of a High-Volume Thyroid Surgery Center. Cancers, 16(5), 1007. https://doi.org/10.3390/cancers16051007





