Trends in Anti-Tumor Effects of Pseudomonas aeruginosa Mannose-Sensitive-Hemagglutinin (PA-MSHA): An Overview of Positive and Negative Effects
Abstract
Simple Summary
Abstract
1. Introduction
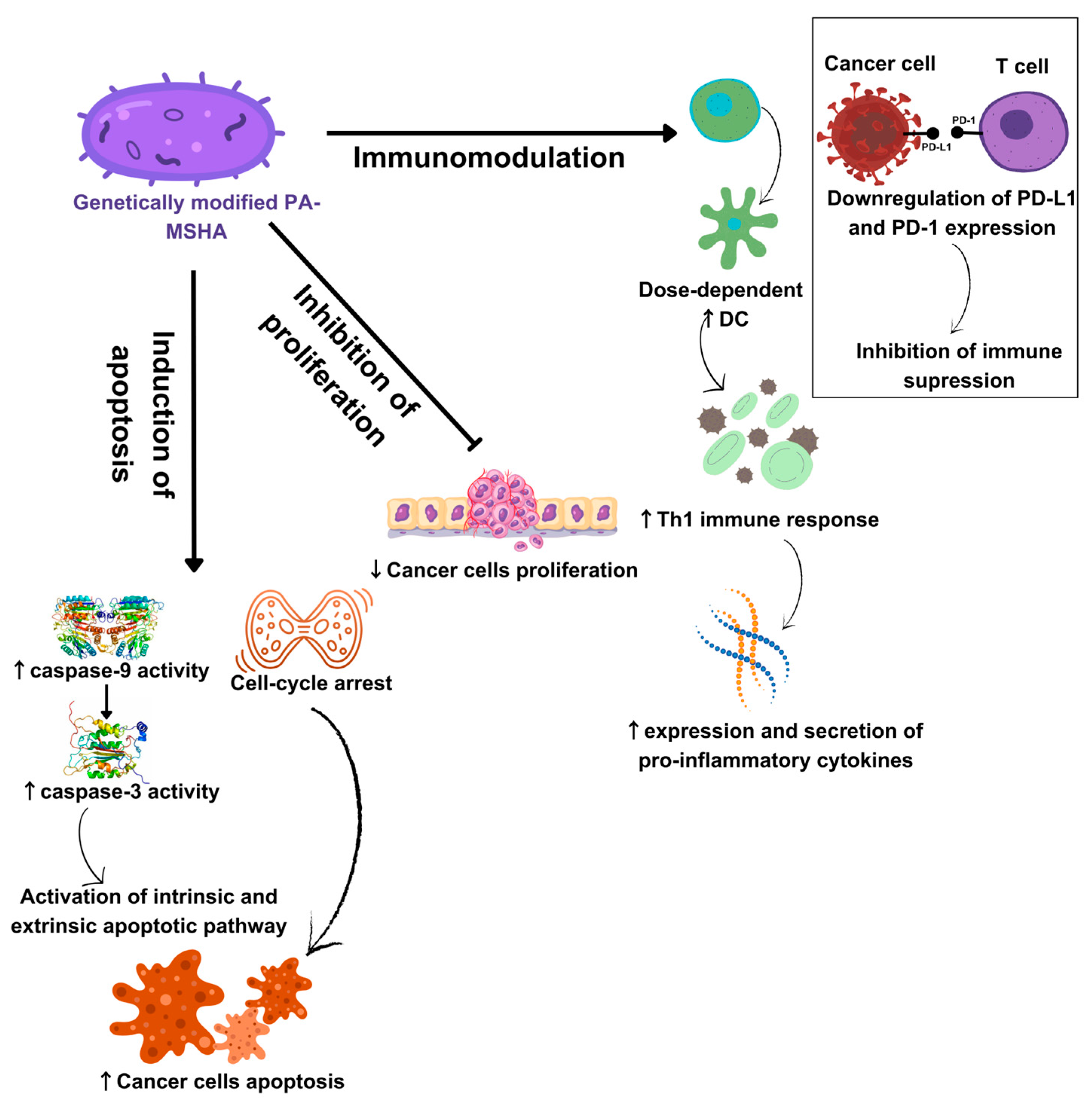
2. Anti-Tumor Potential of PA-MSHA: In Vitro Results
3. Anti-Tumor Potential of PA-MSHA: In Vivo Results on Animal Models
| Animal Species | Treatment Doses | Duration | Effects | References |
|---|---|---|---|---|
| BALB/c nude mice | 0.1 mL PA-MSHA (2.2 × 1010 cells/mL) s.c. | N/A | Suppressed breast tumorigenesis and the formation of metastases in the lungs | Liu et al., (2010) [42] |
| BALB/c nude mice | 0.1 mL 1.8 × 1010/mL percutaneous injection | 42 days | Reduced the size of bladder tumors and induced apoptosis of tumor cells | Chang et al., (2014) [3] |
| BALB/c nude mice | 0.1 mL 2 × 1010/mL s.c. | 6 weeks | It reduced the size of pancreatic tumors and induced the apoptosis of tumor cells | Cheng et al., (2016) [41] |
| BALB/c nude mice | 0.1 mL 2.2 × 1010 cells/mL s.c. | N/A | Increased sensitivity of non-small cell lung tumors to gefitinib | Zhao et al., (2016) [16] |
| BALB/c nude mice | 0.1 mL 2.2 × 1010 cells/mL s.c. | 6 weeks (every other day) | Induced ER stress and consequently promoted autophagy in HR-breast cancer | Xu et al., (2014) [28] |
| BALB/c nude mice | 0.1 mL 1 × 1010/mL peritumor injection | 2 weeks (every second day) | Reduced mass and volume of cetuximab-resistant colorectal cancer and prolonged survival | Zhang et al., (2022) [58] |
| BALB/c mice | 1 × 1010/d ip | 40 days | Inhibited the growth and progression of hepatocellular carcinoma and induced the apoptosis of tumor cells | Li et al., (2014) [63] |
| BALB/c mice | 106/mL s.c. | 38 days | Inhibited the progression of gastric tumors | Wang et al., (2015) [31] |
| C57bl/6J mice | 2 × 108 pcs/mL 4 × 108 pcs/mL 6 × 108 pcs/mL ip | 7–10 weeks (every fifth day) | Inhibited bladder tumor growth, reduced its invasiveness, and promoted tumor cell apoptosis | Huang et al., (2022) [55] |
| C57BL/6 wild-type and nude mice C57BL/6 TLR42/2, and TLR22/2 mice | 106 CFU/mL 107 CFU/mL 108 CFU/mL s.c. | Until the tumor has grown to a diameter of 12 mm or until metastases have developed | Slowed down the growth of lung tumors and prolonged the survival of mice | Zhang et al., (2014) [54] |
| C57BL/6 female mice | 1.6–2.0 × 109 3.2–4.0 × 108 6.4–8.0 × 107 CFU/mL s.c. | 3 weeks (twice a week) | Stimulated immune response in the murine tumor model prolonged mouse survival and reduced tumor growth. | Li et al., (2015) [57] |
| Orthotopic mice | 1 × 10⁹ CFU/mL | 3 weeks (once a week) | Induction of effector T cells and stimulation of immune-suppressing mechanisms | Wang et al., (2022) [61] |
| Nude mice | 1.6–2 × 109 cells/mL s.c. | 6 weeks | Inhibited breast tumor growth and induced apoptosis of tumor cells resistant to doxorubicin | Wei et al., (2016) [44] |
| Wistar rats | 1 × 106/mL iv | 10 weeks (every third day) | Inhibited the growth of bladder tumors, reduced invasiveness | Liu et al., (2017) [56] |
4. Anti-Tumor Potential of PA-MSHA in Humans: Past and Current Clinical Studies
5. PA-MSHA-Induced Side Effects
6. Future Directions
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Asano, T. Drug Resistance in Cancer Therapy and the Role of Epigenetics. J. Nippon. Med. Sch. 2020, 87, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Bozic, D.; Živančević, K.; Baralić, K.; Javorac, D.; Marić, Đ.; Đorđević, A.B.; Bulat, Z.; Đukić-Ćosić, D. Toxic potential of Pseudomonas aeruginosa mannose-sensitive hemagglutinin: In silico investigation of adverse outcomes in cancer patients. Maced. Pharm. Bull. 2022, 68, 371–372. [Google Scholar] [CrossRef]
- Chang, L.; Xiao, W.; Yang, Y.; Li, H.; Xia, D.; Yu, G.; Guo, X.; Guan, W.; Hu, Z.; Xu, H.; et al. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits epidermal growth factor receptor signaling pathway activation and induces apoptosis in bladder cancer cells in vitro and in vivo. Urol. Oncol. Semin. Orig. Investig. 2014, 32, 36.e11–36.e18. [Google Scholar] [CrossRef] [PubMed]
- Rezayatmand, H.; Razmkhah, M.; Razeghian-Jahromi, I. Drug resistance in cancer therapy: The Pandora’s Box of cancer stem cells. Stem Cell Res. Ther. 2022, 13, 181. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Soleimani, N.; Javadi, M.M. Future prospects of bacteria-mediated cancer therapies: Affliction or opportunity? Microb. Pathog. 2022, 172, 105795. [Google Scholar] [CrossRef] [PubMed]
- Hawash, M. Highlights on Specific Biological Targets; Cyclin-Dependent Kinases, Epidermal Growth Factor Receptors, Ras Protein, and Cancer Stem Cells in Anticancer Drug Development. Drug Res. 2019, 69, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Hawash, M. Recent Advances of Tubulin Inhibitors Targeting the Colchicine Binding Site for Cancer Therapy. Biomolecules 2022, 12, 1843. [Google Scholar] [CrossRef]
- Duan, Y.; Liu, W.; Tian, L.; Mao, Y.; Song, C. Targeting Tubulin-colchicine Site for Cancer Therapy: Inhibitors, Antibody- Drug Conjugates and Degradation Agents. Curr. Top. Med. Chem. 2019, 19, 1289–1304. [Google Scholar] [CrossRef]
- Sofi, S.; Mehraj, U.; Qayoom, H.; Aisha, S.; Asdaq, S.M.B.; Almilaibary, A.; Mir, M.A. Cyclin-dependent kinases in breast cancer: Expression pattern and therapeutic implications. Med. Oncol. 2022, 39, 106. [Google Scholar] [CrossRef]
- Talukdar, S.; Emdad, L.; Das, S.K.; Fisher, P.B. EGFR: An essential receptor tyrosine kinase-regulator of cancer stem cells. Adv. Cancer Res. 2020, 147, 161–188. [Google Scholar] [CrossRef] [PubMed]
- Mayakrishnan, V.; Kannappan, P.; Tharmalingam, N.; Bose, R.J.C.; Madheswaran, T.; Ramasamy, M. Bacterial cancer therapy: A turning point for new paradigms. Drug Discov. Today 2022, 27, 2043–2050. [Google Scholar] [CrossRef] [PubMed]
- Rommasi, F. Bacterial-Based Methods for Cancer Treatment: What We Know and Where We Are. Oncol. Ther. 2022, 10, 23–54. [Google Scholar] [CrossRef] [PubMed]
- Sedighi, M.; Bialvaei, A.Z.; Hamblin, M.R.; Ohadi, E.; Asadi, A.; Halajzadeh, M.; Lohrasbi, V.; Mohammadzadeh, N.; Amiriani, T.; Krutova, M.; et al. Therapeutic bacteria to combat cancer; current advances, challenges, and opportunities. Cancer Med. 2019, 8, 3167–3181. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Li, A.; Wang, Y.; Zhang, Y. Intratumoral microbiota: Roles in cancer initiation, development and therapeutic efficacy. Signal Transduct. Target. Ther. 2023, 8, 35. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wu, X.; Yu, W.; Cai, X.; Liu, Q.; Fu, X.; Liu, Z.; Hu, D.; Pan, S.; Huang, Q. PA-MSHA inhibits proliferation and induces apoptosis in human non-small cell lung cancer cell lines with different genotypes. Mol. Med. Rep. 2016, 14, 5369–5376. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roberts, N.J.; Zhang, L.; Janku, F.; Collins, A.; Bai, R.; Staedtke, V.; Rusk, A.W.; Tung, D.; Miller, M.; Roix, J.; et al. Intratumoral injection of Clostridium novyi-NT spores induces anti-tumor responses. Sci. Transl. Med. 2015, 6, 249ra111. [Google Scholar]
- Malmgren, R.A.; Flanigan, C.C. Localization of the vegetative form of Clostridium tetani in mouse tumors following intravenous spore administration. Cancer Res. 1955, 15, 473–478. [Google Scholar]
- Huang, X.; Pan, J.; Xu, F.; Shao, B.; Wang, Y.; Guo, X.; Zhou, S. Bacteria-Based Cancer Immunotherapy. Adv. Sci. 2021, 8, 2003572. [Google Scholar] [CrossRef]
- Zhou, S.; Gravekamp, C.; Bermudes, D.; Liu, K. Tumour-targeting bacteria engineered to fight cancer. Nat. Rev. Cancer 2018, 18, 727–743. [Google Scholar] [CrossRef]
- Faure, E.; Kwong, K.; Nguyen, D. Pseudomonas aeruginosa in Chronic Lung Infections: How to Adapt Within the Host? Front. Immunol. 2018, 9, 2416. [Google Scholar] [CrossRef] [PubMed]
- Arai, H. Regulation and function of versatile aerobic and anaerobic respiratory metabolism in Pseudomonas aeruginosa. Front. Microbiol. 2011, 2, 103. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, Y.; Liu, J. Regulatory effect of Pseudomonas aeruginosa mannose-sensitive hemagglutinin on inflammation and immune function in percutaneous nephrolithotomy patients with upper urinary tract calculi complicated with infection. Front. Immunol. 2023, 14, 1181688. [Google Scholar] [CrossRef] [PubMed]
- Pang, Z.; Gu, M.D.; Tang, T. Pseudomonas aeruginosa in Cancer Therapy: Current Knowledge, Challenges and Future Perspectives. Front. Oncol. 2022, 12, 891187. [Google Scholar] [CrossRef] [PubMed]
- Xiu, D.; Cheng, M.; Zhang, W.; Ma, X.; Liu, L. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits chemical-induced skin cancer through suppressing hedgehog signaling. Exp. Biol. Med. 2020, 245, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Liu, Y.; Liu, Y.; Shao, Y. The MSHA Strain of Pseudomonas aeruginosa Activated TLR Pathway and Enhanced HIV-1 DNA Vaccine Immunoreactivity. PLoS ONE 2012, 7, e47724. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Wang, S.; Shen, L.; Wang, W.; Zhao, F.; Cao, T. Effects of Pseudomonas aeruginosa mannose-sensitive hemagglutinin (PA-MSHA) pretreatment on septic rats. Int. Immunopharmacol. 2013, 17, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.-H.; Liu, Z.-B.; Hou, Y.-F.; Hong, Q.; Hu, D.-L.; Shao, Z.-M. Inhibition of autophagy enhances the cytotoxic effect of PA-MSHA in breast cancer. BMC Cancer 2014, 14, 273. [Google Scholar] [CrossRef][Green Version]
- Gong, Y.; Zuo, H.; Zhou, Y.; Yu, K.D.; Liu, G.Y.; Di, G.H.; Wu, J.; Liu, Z.B.; Shao, Z.M. Neoadjuvant Pseudomonas aeruginosa mannose-sensitive hemagglutinin (PA-MSHA) and chemotherapy versus placebo plus chemotherapy in patients with HER2-negative breast cancer: A randomized, controlled, double-blind trial. Ann. Transl. Med. 2023, 11, 243. [Google Scholar] [CrossRef]
- Jian, X.; Chao, S.; Xiaoli, Z.; Aiwu, W. Inactivated, P. aeruginosa restores immune imbalance of chronic idiopathic urticaria. Arch. Dermatol. Res. 2020, 312, 353–359. [Google Scholar] [CrossRef]
- Wang, C.; Hu, Z.; Zhu, Z.; Zhang, X.; Wei, Z.; Zhang, Y.; Hu, D.; Cai, Q. The MSHA strain of Pseudomonas aeruginosa (PA-MSHA) inhibits gastric carcinoma progression by inducing M1 macrophage polarization. Tumor Biol. 2016, 37, 6913–6921. [Google Scholar] [CrossRef] [PubMed]
- Lv, F.; Cao, J.; Liu, Z.; Wang, Z.; Zhang, J.; Zhang, S.; Wang, L.; Zhao, X.; Shao, Z.; Wang, B.; et al. Phase II study of Pseudomonas aeruginosa-Mannose-Sensitive hemagglutinin in combination with capecitabine for Her-2-negative metastatic breast cancer pretreated with anthracycline and taxane. PLoS ONE 2015, 10, e0118607. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Duan, Z.; Yang, B.; Xiao, C. The effective regulation of pro-and anti-inflammatory cytokines induced by combination of PA-MSHA and BPIFB1 in initiation of innate immune responses. Open Med. 2017, 12, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, G.; Samal, D.; Khandayataray, P.; Murthy, M.K. A Review on Caspases: Key Regulators of Biological Activities and Apoptosis. Mol. Neurobiol. 2023, 60, 5805–5837. [Google Scholar] [CrossRef] [PubMed]
- Asadi, M.; Taghizadeh, S.; Kaviani, E.; Vakili, O.; Taheri-Anganeh, M.; Tahamtan, M.; Savardashtaki, A. Caspase-3: Structure, function, and biotechnological aspects. Biotechnol. Appl. Biochem. 2022, 69, 1633–1645. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, N.; Saxena, A.K. Caspase-3 Activators as Anticancer Agents. Curr. Protein Pept. Sci. 2023, 24, 783–804. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.-M.; Pan, S.-Y.; Huang, Q.-L.; Lu, Y.-N.; Wu, X.-H.; Chang, J.-H.; Liu, Z.-B.; Cai, X.-W.; Liu, Q.; Wang, J.-L.; et al. PA-MSHA in combination with EGFR tyrosine kinase inhibitor: A new strategy to overcome the drug resistance of non-small cell lung cancer cells. Oncotarget 2016, 7, 49384–49396. [Google Scholar] [CrossRef]
- London, M.; Gallo, E. Epidermal growth factor receptor (EGFR) involvement in epithelial-derived cancers and its current antibody-based immunotherapies. Cell Biol. Int. 2020, 44, 1267–1282. [Google Scholar] [CrossRef]
- Liu, X.; Wang, P.; Zhang, C.; Ma, Z. Epidermal growth factor receptor (EGFR): A rising star in the era of precision medicine of lung cancer. Oncotarget 2017, 8, 50209–50220. [Google Scholar] [CrossRef]
- Chang, J.; Liu, Y.; Han, B.; Zhou, C.; Bai, C.; Li, J. Pseudomonas aeruginosa preparation plus chemotherapy for advanced non-small-cell lung cancer: A randomized, multicenter, double-blind phase III study. Med. Oncol. 2015, 32, 139. [Google Scholar] [CrossRef]
- Cheng, X.; Wang, B.; Jin, Z.; Ma, D.; Yang, W.; Zhao, R.; Jing, X.; Shen, B.; Peng, C.; Qiu, W. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits pancreatic cancer cell proliferation and induces apoptosis via the EGFR pathway and caspase signaling. Oncotarget 2016, 7, 77916–77925. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.B.; Hou, Y.F.; Zhu, J.; Hu, D.L.; Jin, W.; Ou, Z.L.; Di, G.H.; Wu, J.; Shen, Z.Z.; Shao, Z.M. Inhibition of EGFR pathway signaling and the metastatic potential of breast cancer cells by PA-MSHA mediated by type 1 fimbriae via a mannose-dependent manner. Oncogene 2010, 29, 2996–3009. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Hou, Y.; Dong, M.; Di, G.; Wu, J.; Shen, Z.; Shao, Z. 0015 PA-MSHA inhibits proliferation and induces apoptosis through the up-regulation and activation of caspases in the human breast cancer cell lines. Breast 2009, 18, S22. [Google Scholar] [CrossRef]
- Wei, Y.; Liu, D.; Jin, X.; Gao, P.; Wang, Q.; Zhang, J.; Zhang, N. PA-MSHA inhibits the growth of doxorubicin-resistant MCF-7/ADR human breast cancer cells by downregulating Nrf2/p62. Cancer Med. 2016, 5, 3520–3531. [Google Scholar] [CrossRef]
- Bartolini, D.; Dallaglio, K.; Torquato, P.; Piroddi, M.; Galli, F. Nrf2-p62 autophagy pathway and its response to oxidative stress in hepatocellular carcinoma. Transl. Res. 2018, 193, 54–71. [Google Scholar] [CrossRef]
- Yin, T.; Ou-yang, X.; Jiao, F.; Huang, L.; Tang, X.; Ren, B. Pseudomonas aeruginosa mannose-sensitive hemagglutinin inhibits proliferation and invasion via the PTEN/AKT pathway in HeLa cells. Oncotarget 2016, 7, 37121–37131. [Google Scholar] [CrossRef]
- Haddadi, N.; Lin, Y.; Travis, G.; Simpson, A.M.; Nassif, N.T.; McGowan, E.M. PTEN/PTENP1: ‘Regulating the regulator of RTK-dependent PI3K/Akt signalling’, new targets for cancer therapy. Mol. Cancer 2018, 17, 37–51. [Google Scholar] [CrossRef]
- Lee, Y.R.; Chen, M.; Pandolfi, P.P. The functions and regulation of the PTEN tumour suppressor: New modes and prospects. Nat. Rev. Mol. Cell Biol. 2018, 19, 547–562. [Google Scholar] [CrossRef]
- Zhu, Y.P.; Bian, X.J.; Ye, D.W.; Yao, X.D.; Zhang, S.L.; Dai, B.; Shen, Y.J. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits proliferation and induces apoptosis in a caspase-dependent manner in human bladder cancer cell lines. Oncol. Lett. 2013, 5, 1357–1362. [Google Scholar] [CrossRef][Green Version]
- Cao, Z.; Shi, L.; Li, Y.; Wang, J.; Wang, D.; Wang, G.; Sun, B.; Mu, L.; Yang, M.; Li, H. Pseudomonas aeruginosa: Mannose sensitive hemagglutinin inhibits the growth of human hepatocarcinoma cells via mannose-mediated apoptosis. Dig. Dis. Sci. 2008, 54, 2118–2127. [Google Scholar] [CrossRef]
- Wei, H.; Mao, Y.; Zhang, H.; Wu, F.; Zhang, Y. PA-MSHA Regulates PD-L1 Expression in Hepatoma Cells. Immunol. Investig. 2023, 52, 343–363. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Chen, M.; Nie, H.; Yuan, Y. PD-1 and PD-L1 in cancer immunotherapy: Clinical implications and future considerations. Hum. Vaccines Immunother. 2019, 15, 1111–1122. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, L.P.; Zhao, X.L.; Wang, F.; Huang, L.; Wang, M.; Chen, X.F.; Li, H.; Zhang, Y. Pseudomonas aeruginosa injection enhanced anti-tumor cytotoxicity of cytokine-induced killer cells derived from cord blood. Biomed. Pharmacother. 2014, 68, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Luo, F.; Zhang, Y.; Wang, L.; Lin, W.; Yang, M.; Hu, D.; Wu, X.; Chu, Y. Pseudomonas aeruginosa Mannose-Sensitive Hemagglutinin Promotes T-Cell Response via Toll-Like Receptor 4–Mediated Dendritic Cells to Slow Tumor Progression in Mice. J. Pharmacol. Exp. Ther. 2014, 349, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; He, F.; Li, D.; Xie, Y.J.; Jiang, Z.B.; Huang, J.M.; Zhao, X.-P.; Nasim, A.A.; Chen, J.H.; Fan, X.M.; et al. PA-MSHA induces inflamed tumor microenvironment and sensitizes tumor to anti-PD-1 therapy. Cell Death Dis. 2022, 13, 931. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Duan, X. PA-MSHA induces apoptosis and suppresses metastasis by tumor associated macrophages in bladder cancer cells. Cancer Cell Int. 2017, 17, 76. [Google Scholar] [CrossRef]
- Li, T.; Yang, L.; Fu, S.J.; Xiao, E.L.; Yuan, X.; Lu, J.Z.; Ma, B.L.; Shi, T.K.; Wang, Z.P. Subcutaneous Injections of the Mannose-Sensitive Hemagglutination Pilus Strain of Pseudomonas aeruginosa Stimulate Host Immunity, Reduce Bladder Cancer Size and Improve Tumor Survival in Mice. Cell Biochem. Biophys. 2015, 73, 245–252. [Google Scholar] [CrossRef]
- Zhang, H.; Shan, W.; Li, D.; Yan, Y.; Zhang, J. PA-MSHA Exerts Potent Activity against Cetuximab-Resistant Colorectal Cancer through miR-7-5p/Akt/Wnt-β-Catenin Pathway. 2022. Available online: https://assets.researchsquare.com/files/rs-1816082/v1/f2cc1c8f-88de-4bd8-8466-c62c3f1c3c73.pdf?c=1658162359 (accessed on 26 November 2023).
- Zhang, W.; Sun, J.; Shen, X.; Xue, Y.; Yuan, S.; Wang, X. Effect of PA-MSAH preprocessing on the expression of TLR-4-NF-κB pathway and inflammatory factors in the intestinal tract of rats with septic shock. Exp. Ther. Med. 2019, 17, 2567–2574. [Google Scholar] [CrossRef]
- Fu, X.; Cui, J.; Meng, X.; Jiang, P.; Zheng, Q.; Zhao, W.; Chen, X. Endoplasmic reticulum stress, cell death and tumor: Association between endoplasmic reticulum stress and the apoptosis pathway in tumors (Review). Oncol. Rep. 2021, 45, 801–808. [Google Scholar] [CrossRef]
- Wang, B.; He, Z.; Yu, H.; Ou, Z.; Chen, J.; Yang, M.; Fan, X.; Lin, T.; Huang, J. Intravesical Pseudomonas aeruginosa mannose-sensitive Hemagglutinin vaccine triggers a tumor-preventing immune environment in an orthotopic mouse bladder cancer model. Cancer Immunol. Immunother. 2022, 71, 1507–1517. [Google Scholar] [CrossRef]
- Miao, Z.F.; Zhao, T.T.; Miao, F.; Wang, Z.N.; Xu, Y.Y.; Mao, X.Y.; Gao, J.; Wu, J.H.; Liu, X.Y.; You, Y.; et al. The mannose-sensitive hemagglutination pilus strain of Pseudomonas aeruginosa shift peritoneal milky spot macrophages towards an M1 phenotype to dampen peritoneal dissemination. Tumour Biol. 2014, 35, 4285–4293. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Dong, Z.R.; Guo, Z.Y.; Wang, C.H.; Zhi, X.T.; Zhou, J.W.; Li, D.K.; Chen, Z.T.; Chen, Z.Q.; Hu, S.Y. Mannose-mediated inhibitory effects of PA-MSHA on invasion and metastasis of hepatocellular carcinoma via EGFR/Akt/IκBβ/NF-κB pathway. Liver Int. 2015, 35, 1416–1429. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Fang, Y.; Zou, X.; Wang, X.; Li, Z. Therapeutic potential of Pseudomonas aeruginosa-mannose sensitive hemagglutinin (PA-MSHA) in cancer treatment. Microb. Pathog. 2023, 185, 106422. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hao, D.; Li, L.; Zhou, X.; Ren, L.; Yang, Y.; Li, P.; Qin, H.; Luo, D.; Zhang, H.; et al. A clinical study on PA-MSHA vaccine in adjuvant therapy of lung cancer. Zhongguo Fei Ai Za Zhi 1999, 2, 20–22. (In Chinese) [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hao, D.; Zhang, H.; Ren, L.; Yang, Y.; Li, L.; Chai, J.; Zhou, X.; Fu, L. A clinical study on PA-MSHA vaccine used for adjuvant therapy of lymphoma and lung cancer. Hua Xi Yi Ke Da Xue Xue Bao 2000, 31, 334–337. (In Chinese) [Google Scholar] [PubMed]
- Chen, W.D.; Tang, Z.H.; Xu, F. Application of PA-MSHA vaccine adjuvant therapy and TAC scheme for treatment of breast carcinoma. Nan Fang Yi Ke Da Xue Xue Bao 2009, 29, 1204–1207. (In Chinese) [Google Scholar]
- Zhang, C.; Zhang, Z.; Wang, L.; Han, J.; Li, F.; Shen, C.; Li, H.; Huang, L.; Zhao, X.; Yue, D.; et al. Pseudomonas aeruginosa-mannose sensitive hemagglutinin injection treated cytokine-induced killer cells combined with chemotherapy in the treatment of malignancies. Int. Immunopharmacol. 2017, 51, 57–65, Erratum in Int. Immunopharmacol. 2022, 102, 108356. [Google Scholar] [CrossRef]
- Gish, R.G.; Gholam, P.M. Monotherapy vs multiple-drug therapy: The experts debate. Clevel. Clin. J. Med. 2009, 76 (Suppl. S3), S20–S24. [Google Scholar] [CrossRef]
| Treatment Doses | Duration | Effects | References |
|---|---|---|---|
| PA-MSHA 1 mL s.c. plus chemotherapy | Total: 10 weeks; 1st week: 0.5 mL of PA-MSHA was injected on the day 1, 3, 5. From 2nd to 10th week: 0.8 mL was injected at day 5 | PA-MSHA increases T cell proliferation and the production of pro-inflammatory cytokines in lung cancer patients to prevent super-infection. | Li et al., (1999) [65] |
| PA-MSHA 1 mL s.c. plus chemotherapy | PA-MSHA improves the effectiveness of treatment of lymphoma and lung cancer by modulating patients’ immune response. | Li et al., (2000) [66] | |
| PA-MSHA 1 mL s.c. in addition to the TAC * scheme | Cycle: 3 weeks Total: 2–4 cycles | PA-MSHA enhanced therapeutic response of breast carcinoma patients treated with TAC scheme. | Chen et al., (2009) [67] |
| PA-MSHA 1 mL s.c. in addition to 1000 mg/m2 of capecitabine twice a day | Cycle: every other day for 2 weeks, 1 week off. Total: 2–4 cycles | PA-MSHA and capecitabine possess superior clinical efficacy in patients with metastatic breast cancer compared to either treatment alone. | Lv et al., (2015) [32] |
| CIK cells treated with 4.5 × 106, 9 × 106, 13.5 × 106, 18 × 106, and 22.5 × 106 CFU/mL of PA-MSHA and combined with chemotherapy | Cycle: different chemotherapy protocols. CIK cells treated with PA-MSHA were administered 1 day after the chemotherapy. Total: 2–6 cycles | PA-MSHA stimulated the proliferation of CIK cells in a dose-dependent manner. CIK cells acquired a more cytotoxic phenotype: increased production of IFN-γ, IL-2, and CD107a. | Zhang et al., (2017) [68] |
| 1 mL every other day (0.5 mL on the first day) from the first day of neoadjuvant chemotherapy (paclitaxel and carboplatin) until 3 days before surgery | Cycle: 4 weeks Total: 4 cycles of neoadjuvant chemotherapy | The addition of PA-MSHA to neoadjuvant chemotherapy in HER2-negative breast cancer improves the tumor’s clinical response. Patients with immune-related adverse events could benefit more from the PA-MSHA treatment. | Gong et al., (2023) [29] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bozic, D.; Živanović, J.; Živančević, K.; Baralić, K.; Đukić-Ćosić, D. Trends in Anti-Tumor Effects of Pseudomonas aeruginosa Mannose-Sensitive-Hemagglutinin (PA-MSHA): An Overview of Positive and Negative Effects. Cancers 2024, 16, 524. https://doi.org/10.3390/cancers16030524
Bozic D, Živanović J, Živančević K, Baralić K, Đukić-Ćosić D. Trends in Anti-Tumor Effects of Pseudomonas aeruginosa Mannose-Sensitive-Hemagglutinin (PA-MSHA): An Overview of Positive and Negative Effects. Cancers. 2024; 16(3):524. https://doi.org/10.3390/cancers16030524
Chicago/Turabian StyleBozic, Dragica, Jovana Živanović, Katarina Živančević, Katarina Baralić, and Danijela Đukić-Ćosić. 2024. "Trends in Anti-Tumor Effects of Pseudomonas aeruginosa Mannose-Sensitive-Hemagglutinin (PA-MSHA): An Overview of Positive and Negative Effects" Cancers 16, no. 3: 524. https://doi.org/10.3390/cancers16030524
APA StyleBozic, D., Živanović, J., Živančević, K., Baralić, K., & Đukić-Ćosić, D. (2024). Trends in Anti-Tumor Effects of Pseudomonas aeruginosa Mannose-Sensitive-Hemagglutinin (PA-MSHA): An Overview of Positive and Negative Effects. Cancers, 16(3), 524. https://doi.org/10.3390/cancers16030524







