Are Imaging Evaluations of Soft-Tissue Masses Before Referral to a Specialized Center Being Performed Properly? A Systematic Review
Simple Summary
Abstract
1. Introduction
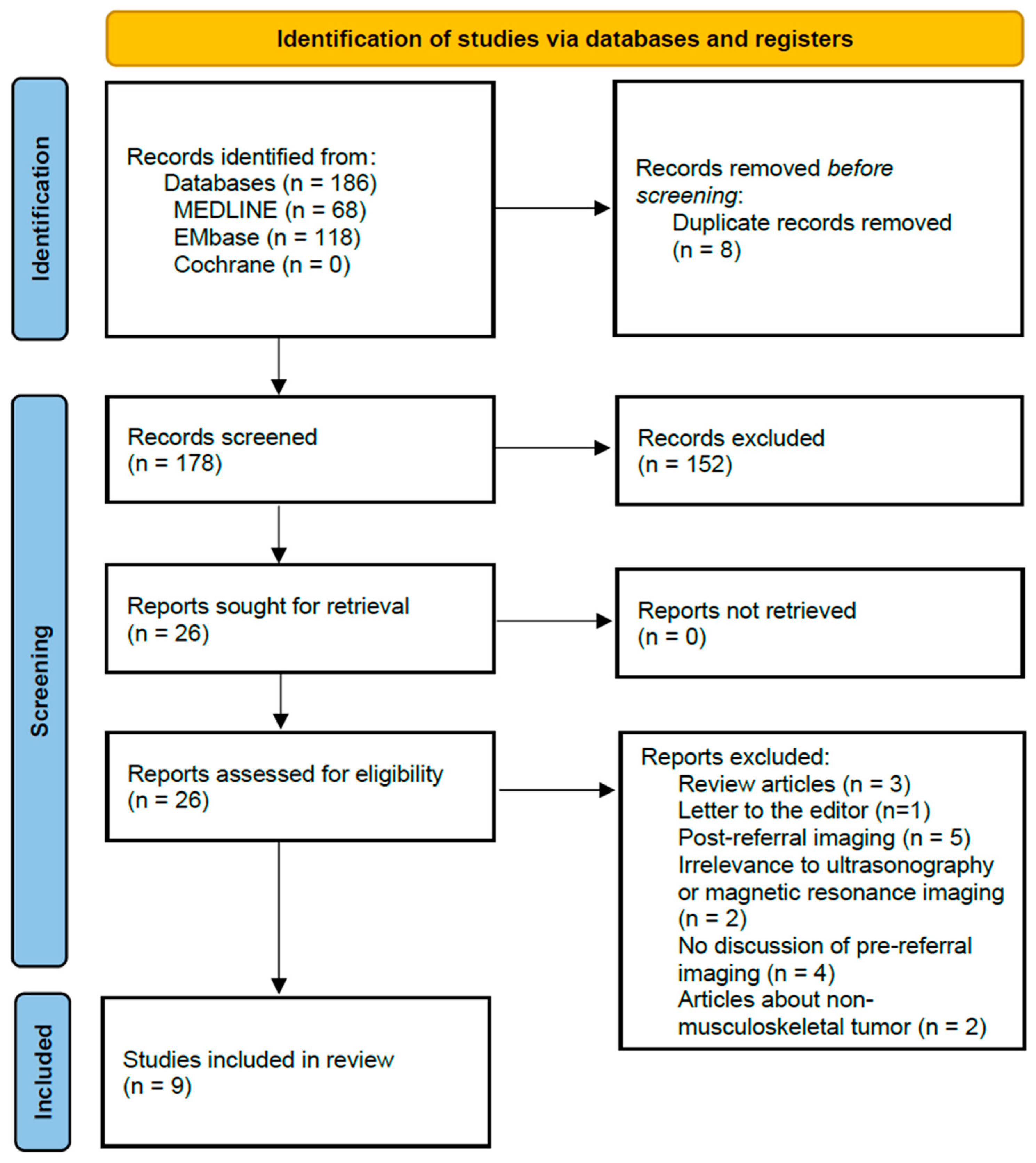
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Selection Process
2.3. Data Synthesis
3. Results
3.1. Study Characteristics
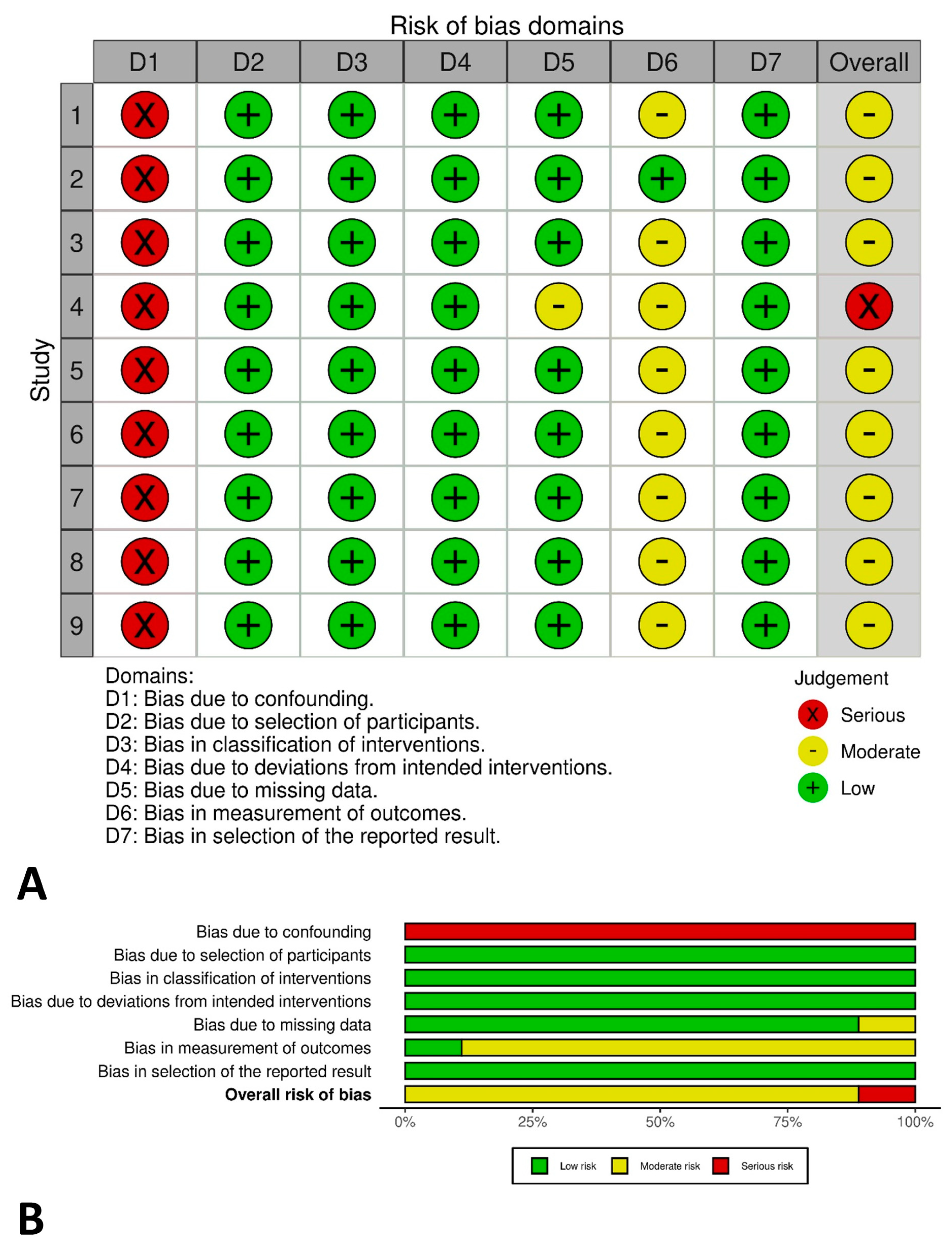
3.2. Risk of Bias
3.3. Ultrasonography
3.4. Magnetic Resonance Imaging
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kang, H.G. Diagnoses and Approaches of Soft Tissue Tumors for Orthopaedic Non-Oncologists. J. Korean Orthop. Assoc. 2015, 50, 269–279. [Google Scholar] [CrossRef][Green Version]
- Crombé, A.; Kind, M.; Fadli, D.; Miceli, M.; Linck, P.-A.; Bianchi, G.; Sambri, A.; Spinnato, P. Soft-tissue sarcoma in adults: Imaging appearances, pitfalls and diagnostic algorithms. Diagn. Interv. Imaging 2023, 104, 207–220. [Google Scholar] [CrossRef] [PubMed]
- Korea Central Cancer Registry; National Cancer Center. Annual Report of Cancer Statistics in Korea in 2020; Ministry of Health and Welfare: Sejong, Republic of Korea, 2022.
- SSG Guidelines for Referral of Patients with Soft Tissue Tumors of the Extremities and Trunk Wall. Available online: https://www.ssg-org.net/treatment-protocols-and-recommendations/ongoing (accessed on 3 September 2023).
- López-Pousa, A.; Broto, J.M.; Trufero, J.M.; Sevilla, I.; Valverde, C.; Alvarez, R.; Alvarez, J.A.C.; Jurado, J.C.; Hindi, N.; Del Muro, X.G. SEOM Clinical Guideline of management of soft-tissue sarcoma. Clin. Transl. Oncol. 2016, 18, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Clinical Excellence. Guidance on Cancer Services: Improving Outcomes for People with Sarcoma; National Institute for Health and Clinical Excellence: London, UK, 2006. [Google Scholar]
- Nystrom, L.M.; Reimer, N.B.; Dean, C.W.; Bush, C.H.; Scarborough, M.T.; Gibbs, C.P., Jr. Evaluation of imaging utilization prior to referral of musculoskeletal tumors: A prospective study. J. Bone Jt. Surg. Am. 2015, 97, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Noebauer-Huhmann, I.M.; Weber, M.A.; Lalam, R.K.; Trattnig, S.; Bohndorf, K.; Vanhoenacker, F.; Tagliafico, A.; van Rijswijk, C.; Vilanova, J.C.; Afonso, P.D.; et al. Soft Tissue Tumors in Adults: ESSR-Approved Guidelines for Diagnostic Imaging. Semin. Musculoskelet. Radiol. 2015, 19, 475–482. [Google Scholar]
- Kwok, H.C.; Pinto, C.H.; Doyle, A.J. The pitfalls of ultrasonography in the evaluation of soft tissue masses. J. Med. Imaging Radiat. Oncol. 2012, 56, 519–524. [Google Scholar] [CrossRef]
- Martin, C.T.; Morcuende, J.; Buckwalter, J.A.; Miller, B.J. Prereferral MRI use in patients with musculoskeletal tumors is not excessive. Clin. Orthop. Relat. Res. 2012, 470, 3240–3245. [Google Scholar] [CrossRef]
- Saifuddin, A.; Twinn, P.; Emanuel, R.; Cannon, S.R. An audit of MRI for bone and soft-tissue tumours performed at referral centres. Clin. Radiol. 2000, 55, 537–541. [Google Scholar] [CrossRef]
- Dan, B.; Kim, S.Y.; Hwang, S.E.; Yoo, K.H. Analysis of the Current Status of Medical Device Use by Domestic Medical Institutions: Focusing on HIRA’s Medical Equipment Possession and Treatment Material Claim Statistics; Korea Health Industry Development Institute: Cheongju, Republic of Korea, 2021. [Google Scholar]
- Szucs, Z.; Davidson, D.; Wong, H.H.; Horan, G.; Bearcroft, P.W.; Grant, I.; Grimer, R.; Hopper, M.A.; Hatcher, H.; Earl, H.A. Comprehensive Single Institutional Review of 2 Years in a Designated Fast-Track Sarcoma Diagnostic Clinic Linked with a Sarcoma Specialist Advisory Group: Meeting the Target but Failing the Task? Sarcoma 2016, 2016, 6032606. [Google Scholar] [CrossRef]
- Reid, C.; Saifuddin, A. A review of paediatric soft tissues masses referred to a tertiary musculoskeletal sarcoma centre. Br. J. Radiol. 2021, 94, 20200790. [Google Scholar] [CrossRef]
- Ashwood, N.; Witt, J.D.; Hallam, P.J.; Cobb, J.P. Analysis of the referral pattern to a supraregional bone and soft tissue tumour service. Ann. R. Coll. Surg. Engl. 2003, 85, 272–276. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dyrop, H.B.; Vedsted, P.; Rædkjær, M.; Safwat, A.; Keller, J. Imaging investigations before referral to a sarcoma center delay the final diagnosis of musculoskeletal sarcoma. Acta Orthop. 2017, 88, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Aboulafia, A.J.; Levin, A.M.; Blum, J. Prereferral evaluation of patients with suspected bone and soft tissue tumors. Clin. Orthop. Relat. Res. 2002, 397, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.J.; Avedian, R.S.; Rajani, R.; Leddy, L.; White, J.R.; Cummings, J.; Balach, T.; MacDonald, K. What is the use of imaging before referral to an orthopaedic oncologist? A prospective, multicenter investigation. Clin. Orthop. Relat. Res. 2015, 473, 868–874. [Google Scholar] [CrossRef]
- Chun, Y.S.; Song, S.H. Diagnostic Approach to a Soft Tissue Mass. J. Korean Orthop. Assoc. 2019, 54, 293–301. [Google Scholar] [CrossRef]
- Yoo, H.J. Sonographic Features of Common Soft Tissue Masses in the Extremities. J. Korean Orthop. Assoc. 2014, 49, 422–430. [Google Scholar] [CrossRef][Green Version]
- Shin, D.-S.; Ryu, S.-M.; Park, C.-H. The Diagnostic Strategy for Malignant Bone Tumors. J. Korean Orthop. Assoc. 2015, 50, 429–437. [Google Scholar] [CrossRef]
- Ng, M.K.; Magruder, M.L.; Heckmann, N.D.; Delanois, R.E.; Piuzzi, N.S.; Krebs, V.E.; Mont, M.A. How-To Create an Orthopaedic Systematic Review: A Step-by-Step Guide Part I: Study Design. J. Arthroplast. 2024, 39, 1863–1868. [Google Scholar] [CrossRef]
- Ng, M.K.; Magruder, M.L.; Piuzzi, N.S.; Heckmann, N.D.; Delanois, R.E.; Krebs, V.E.; Mont, M.A. How-To Create an Orthopaedic Systematic Review: A Step-by-step Guide Part II: Study Execution. J. Arthroplast. 2024, 39, 2124–2129. [Google Scholar] [CrossRef]
- Yoon, J.H.; Kwon, I.H.; Park, H.W. The South Korean health-care system in crisis. Lancet 2024, 403, 2589. [Google Scholar] [CrossRef]
- Smolle, M.A.; Leithner, A.; Grimer, R.J. Evaluating the British sarcoma referral form. Ann. R. Coll. Surg. Engl. 2015, 97, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Styring, E.; Billing, V.; Hartman, L.; Nilbert, M.; Seinen, J.M.; Veurink, N.; Vult von Steyern, F.; Rydholm, A. Simple guidelines for efficient referral of soft-tissue sarcomas: A population-based evaluation of adherence to guidelines and referral patterns. J. Bone Jt. Surg. Am. 2012, 94, 1291–1296. [Google Scholar] [CrossRef] [PubMed]
- Noebauer-Huhmann, I.M.; Vanhoenacker, F.M.; Vilanova, J.C.; Tagliafico, A.S.; Weber, M.A.; Lalam, R.K.; Grieser, T.; Nikodinovska, V.V.; de Rooy, J.W.J.; Papakonstantinou, O.; et al. Soft tissue tumor imaging in adults: European Society of Musculoskeletal Radiology-Guidelines 2023-overview, and primary local imaging: How and where? Eur. Radiol. 2024, 34, 4427–4437. [Google Scholar] [CrossRef] [PubMed]
- Korthaus, A.; Weiss, S.; Barg, A.; Salamon, J.; Schlickewei, C.; Frosch, K.-H.; Priemel, M. Clinical Routine and Necessary Advances in Soft Tissue Tumor Imaging Based on the ESSR Guideline: Initial Findings. Tomography 2022, 8, 1586–1594. [Google Scholar] [CrossRef] [PubMed]
- Weiss, S.; Korthaus, A.; Baumann, N.; Yamamura, J.; Spiro, A.S.; Lübke, A.M.; Frosch, K.-H.; Schlickewei, C.; Priemel, M. Musculoskeletal Soft-Tissue Sarcoma: Quality Assessment of Initial MRI Reports Shows Frequent Deviation from ESSR Guidelines. Diagnostics 2021, 11, 695. [Google Scholar] [CrossRef]
- Baicker, K.; Obermeyer, Z. Overuse and Underuse of Health Care: New Insights from Economics and Machine Learning. JAMA Health Forum 2022, 3, e220428. [Google Scholar] [CrossRef]
| Study (Year) | Country | Type of Study | Population | Period | Imaging Investigation | Main Results |
|---|---|---|---|---|---|---|
| Kwok et al. [9] (2012) | New Zealand | Retrospective | Patients referred to multidisciplinary team | 1999–2009 | USG (n = 175) | Correct diagnosis of non-benign pathology = 35/60 No recommendations for further management in non-benign pathology 8/31: median 1.5-month delay in definitive diagnosis |
| Miller et al. [18] (2015) | US | Prospective | Patients referred to fellowship-trained orthopedic oncologist | - | USG (n = 21) | Unhelpful USG = 16/21 (76%) |
| Szucs et al. [13] (2016) | UK | Retrospective | Patients referred to sarcoma diagnostic clinic | 2013–2014 | USG (n = 64) | Malignancy USG = 0% |
| Study (Year) | Country | Type of Study | Population | Period | Imaging Investigation | Main Results |
|---|---|---|---|---|---|---|
| Saifuddin et al. [11] (2000) | UK | Retrospective | Patients referred to orthopedic oncologists | - | MRI (n = 50) | Non-enhanced MRI = 62% Information in reports for soft-tissue tumors (n = 14)
|
| Aboulafia et al. [17] (2002) | US | Prospective | Patients referred to orthopedic oncology practice | - | MRI (n = 76) | Unnecessary MRI = 26/76 (34.2%)
|
| Ashwood et al. [15] (2003) | UK | Retrospective | Patients referred to supraregional bone and soft-tissue tumor service | October 1997–December 1998 | MRI (n ≈ 40) | Repetition of almost all MRI |
| Martin et al. [10] (2012) | US | Retrospective | Patients referred to musculoskeletal oncology clinic | January 2009–December 2010 | MRI (n = 320) | Inappropriate MRI = 20 (6.2%)
|
| Miller et al. [18] (2015) | US | Prospective | Patients referred to fellowship-trained orthopedic oncologist | - | MRI (n = 263) | Unhelpful MRI = 46/236 (17%) Repetition of MRI = 17/236 (6%)
|
| Nystrom et al. [7] (2015) | US | Retrospective | Patients presenting to tertiary care referral center | - | MRI (n = 210) | Inappropriate MRI = 26.7% |
| Szucs et al. [13] (2016) | UK | Retrospective | Patients referred to sarcoma diagnostic clinic | 2013–2014 | MRI (n = 61) USG + MRI (n = 113) | Malignancy
|
| Reid et al. [14] (2020) | UK | Retrospective | Patients referred to a specialist musculoskeletal oncology unit | September 2018–May 2020 | MRI (n = 93) | Varied combination of imaging protocols in pre-referral MRI Pre-referral imaging diagnosis of possible sarcoma: final diagnosis = 59.5%:5.2% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joo, M.W.; Park, C.J.; Lee, Y.-S.; Cho, Y.J.; Bernthal, N.M.; Lee, S.K.; Kim, H.; Lee, J.H.; Kim, S.H.; Chung, Y.-G. Are Imaging Evaluations of Soft-Tissue Masses Before Referral to a Specialized Center Being Performed Properly? A Systematic Review. Cancers 2024, 16, 3935. https://doi.org/10.3390/cancers16233935
Joo MW, Park CJ, Lee Y-S, Cho YJ, Bernthal NM, Lee SK, Kim H, Lee JH, Kim SH, Chung Y-G. Are Imaging Evaluations of Soft-Tissue Masses Before Referral to a Specialized Center Being Performed Properly? A Systematic Review. Cancers. 2024; 16(23):3935. https://doi.org/10.3390/cancers16233935
Chicago/Turabian StyleJoo, Min Wook, Chan Jin Park, Yong-Suk Lee, Yoon Joo Cho, Nicholas Matthew Bernthal, Seul Ki Lee, Hyunho Kim, Joo Hwan Lee, Sung Hwan Kim, and Yang-Guk Chung. 2024. "Are Imaging Evaluations of Soft-Tissue Masses Before Referral to a Specialized Center Being Performed Properly? A Systematic Review" Cancers 16, no. 23: 3935. https://doi.org/10.3390/cancers16233935
APA StyleJoo, M. W., Park, C. J., Lee, Y.-S., Cho, Y. J., Bernthal, N. M., Lee, S. K., Kim, H., Lee, J. H., Kim, S. H., & Chung, Y.-G. (2024). Are Imaging Evaluations of Soft-Tissue Masses Before Referral to a Specialized Center Being Performed Properly? A Systematic Review. Cancers, 16(23), 3935. https://doi.org/10.3390/cancers16233935






