Simple Summary
Breast cancer is a leading cause of death for women worldwide. This study aims to examine the mechanisms for the anti-cancer effects of a therapeutic peptide agent targeted to connexin 43 (Cx43) called alpha-connexin carboxyl-terminal peptide (aCT1). Findings from this study confirm that aCT1 promotes gap junction intercellular communication and Cx43 protein stabilization and that the peptide binds to Zonal Occludens-1 (ZO-1), consistent with prior reports on the mechanism of action of this agent. New findings from this study identify novel aCT1-interacting proteins and the effect of aCT1 on breast cancer signaling.
Abstract
Connexin 43 (Cx43) is a protein encoded by the GJA1 gene and is a component of cell membrane structures called gap junctions, which facilitate intercellular communication. Prior evidence indicates that elevated GJA1 expression in the HER2-positive (HER2+) subtype of breast cancer is associated with poor prognosis. Prior evidence also suggests that HER2+ breast cancers that have become refractory to HER2-targeted agents have a loss of Cx43 gap junction intercellular communication (GJIC). In this study, a Cx43-targeted agent called alpha-connexin carboxyl-terminal peptide (aCT1) is examined to determine whether GJIC can be rescued in refractory HER2+ breast cancer cells. A proposed mechanism of action for aCT1 is binding to the tight junction protein Zonal Occludens-1 (ZO-1). However, the true scope of activity for aCT1 has not been explored. In this study, mass spectrometry proteomic analysis is used to determine the breadth of aCT1-interacting proteins. The NanoString nCounter Breast Cancer 360 panel is also used to examine the effect of aCT1 on cancer signaling in HER2+ breast cancer cells. Findings from this study show a dynamic range of binding partners for aCT1, many of which regulate gene expression and RNA biology. nCounter analysis shows that a number of pathways are significantly impacted by aCT1, including upregulation of apoptotic factors, leading to the prediction and demonstration that aCT1 can boost the cell death effects of cisplatin and lapatinib in HER2+ breast cancer cells that have become resistant to HER2-targeted agents.
1. Introduction
Gap junctions are membrane channels composed of six connexin proteins. The role of gap junctions is to connect adjoining cells allowing for intercellular communication through the exchange of ions, second messengers, and small metabolites (generally < 1 kDa in size). Connexins are transmembrane proteins that contain extracellular and cytoplasmic tails and loops. Each cell connected by a gap junction contains a six-protein channel with a pair of these channels composing the gap junction. The human genome encodes for 21 connexin genes.
Connexin 43 (Cx43) is one of the most well-studied connexin proteins and has been studied in a variety of human tissues and diseases [1,2,3,4,5,6,7,8,9]. We and others have studied the role of Cx43 in breast cancer [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Prior studies suggest that, in tumors, Cx43 expression can be either decreased or increased and that Cx43’s localization can shift intracellularly from the cell membrane [19,22,27,28,29,30,31,32]. Maintaining gap junction intercellular communication (GJIC) by keeping Cx43 within gap junction plaques in breast cancer cells has been suggested to elicit a “bystander” effect [33,34,35,36]. Under this paradigm, promoting GJIC would result in an amplification of therapeutic responses [37,38]. However, the development and evaluation of Cx43-targeted agents in breast and other cancers is complicated because Cx43 appears to have both canonical gap junction roles as well as non-canonical intracellular roles [4,39]. Furthermore, findings suggest that gap junctions could play a role in the establishment of metastatic colonies in tissues where tumor cells have disseminated [23,40].
There are a number of connexin-based therapeutics in various phases of development for the treatment of diseases including breast cancer [41,42,43]. α-connexin carboxyl-terminal (aCT1) is a therapeutic peptide modeled on the sequence of the C-terminal tail of Cx43. Application of aCT1 was shown to increase gap junction size and GJIC [12,44]. Prior work shows the anti-cancer effects of aCT1 in the brain, melanoma, and breast cancer [12,45,46]. These reports suggest that aCT1 may have anti-cancer effects of its own and is quite effective at boosting the impact of other anti-cancer agents when added in combination, consistent with the concept of the bystander effect. We and others have made prior observations that the upregulation of Cx43 in HER2-positive (HER2+) breast cancer correlates with poorer outcomes [9,21]. Our previous findings have also shown that refractory HER2+ breast cancer cells downregulate Cx43-mediated GJIC [21]. In this study, we examine the mechanisms by which aCT1 exerts its anti-cancer properties by conducting proteomic and genomic analyses of resistant HER2+ breast cancer cells treated with aCT1.
2. Materials and Methods
2.1. Chemicals and Reagents
Biotinylated α-connexin carboxyl-terminal (aCT1) peptide was purchased from AmbioPharm Inc. (North Augusta, SC, USA) and was reconstituted in 1X PBS (Corning, Corning, NY, USA), as previously described [12]. The aCT1 peptide corresponds to a short sequence at the Cx43 C-terminus linked to an antennapedia internalization sequence. Lapatinib was purchased from LC Laboratories (Woburn, MA, USA) and reconstituted in DMSO. Cisplatin, purchased from Selleck Chemicals LLC (Houston, TX, USA), was reconstituted in distilled PBS. All reagents were aliquoted and stored at −80 °C. Cycloheximide was purchased from Acros Organic (Thermo Scientific Chemicals, Waltham, MA, USA). Antibodies: Cx43 (C6219 and MAB3067, Millipore Sigma, St. Louis, MO, USA); β-tubulin (sc-55529, Santa Cruz Biotechnology, Dallas, TX, USA); ZO-1 (8193, Cell Signaling Technology, Danvers, MA, USA).
2.2. Cell Culture
JIMT-1 cells obtained from AddexBio (San Diego, CA, USA) were cultured in Dulbecco’s modified Eagle’s medium (DMEM) (Corning, Corning, NY, USA) supplemented with 10% heat-inactivated fetal bovine serum (Gibco, Waltham, MA, USA), 1% L-glutamine, and 1% penicillin/streptomycin (Corning, Corning, NY, USA). Cells were maintained in a 37 °C humidified incubator with 5% CO2.
2.3. Parachute Assay
JIMT-1 acceptor cells were plated in 96-well plates at a density of 20,000 cells per well and additional JIMT-1 donor cells were plated in 10 cm plates. The next day, both the acceptor and donor cells were treated with either vehicle (PBS) or 250 µM aCT1. On the third day, the donor JIMT-1 cells were loaded with calcein AM (BD Biosciences, Bedford, MA, USA) or vehicle, treated in serum-free DMEM for 30 min, and then counted using a LUNA-FL dual fluorescence cell counter (Logos Biosystems, Annandale, VA, USA). Five thousand calcein AM-loaded donor cells or vehicle donor cells were added to the adherent acceptor cells in the 96-well plates and incubated for 6 h. Cells were then trypsinized and counted using a LUNA-FL cell counter. N = 3 independent experiments with at least 8 replicates per treatment.
2.4. Cell Death Assay
JIMT-1 cells were plated in 96-well plates at a density of 20,000 cells per well and treated the following day with 250 µM aCT1 or PBS for 24 h prior to analysis by trypan blue exclusion and cell counting using a LUNA-FL cell counter. N = 3 independent experiments with at least 8 replicates per treatment.
2.5. Proteomic Analysis
Total protein was isolated from JIMT-1 cells treated with 100 µM aCT1 or PBS for 4 h using lysis buffer containing 50 mM Tris pH7.5, 150 mM NaCl, 1 mM EDTA, and 15 Triton X-100. Lysate was cleared by centrifugation and then normalized to 10 mg per sample. Streptavidin matrix (Thermo Scientific, Waltham, MA, USA) was added to the lysate and samples were incubated at 4 °C overnight. Streptavidin–biotin–aCT1 pulldown was then washed in lysis buffer and PBS prior to proteomic analysis.
2.5.1. Sample Preparation
A total of 6 on-bead samples (n = 3 of CTL JIMT and n = 3 of ACT1 JIMT) were submitted to the IUSM Center for proteome analysis where proteins were denatured in 8 M urea and 100 mM Tris-HCl, pH 8.5, and reduced with 5 mM tris(2-carboxyethyl)phosphine hydrochloride (TCEPSigma-Aldrich, St. Louis, MO, USA, Cat No: C4706) for 30 min at room temperature. Samples were then alkylated with 10 mM chloroacetamide (CAA, Sigma Aldrich Cat No: C0267) for 30 min at room temperature in the dark, prior to dilution with 50 mM Tris-HCl, pH 8.5, to a final urea concentration of 2 M for trypsin/Lys-C-based overnight protein digestion at 37 °C (0.5 µg protease, mass spectrometry grade, Promega Corporation, Madison, WI, USA, Cat No: V5072). Digestions were acidified with trifluoroacetic acid (TFA, 0.5% v/v) and desalted on Pierce C18 spin columns (Thermo Fisher, Waltham, MA, USA, Cat No: 89870) with a wash of 0.5% TFA followed by elution in 70% acetonitrile 0.1% formic acid (FA).
2.5.2. Nano-LC-MS/MS
Mass spectrometry was performed utilizing an EASY-nLC 1200 HPLC system (SCR: 014993, Thermo Fisher Scientific) coupled to an Exploris 480™ mass spectrometer with a FAIMSpro interface (Thermo Fisher Scientific). One-fifth of each fraction was loaded onto a 25 cm IonOpticks-TS column (Ionopticks Aurora Ultimate TS 25 cm) at 350 nL/min. The gradient was held at 5% B for 5 min (mobile phases A: 0.1% formic acid (FA), water; B: 0.1% FA, 80% acetonitrile (Thermo Fisher Scientific Cat No: LS122500)), then increased from 4 to 30% B over 98 min, 30 to 80% B over 10 min, held at 80% for 2 min, and dropped from 80 to 4% B over the final 5 min. The mass spectrometer was operated in positive ion mode, default charge state of 2, advanced peak determination on, and lock mass of 445.12003. Three FAIMS CVs were utilized (−40 CV; −55 CV; −70 CV), each with a cycle time of 1.3 s and with identical MS and MS2 parameters. Precursor scans (m/z 375–1500) were performed with an orbitrap resolution of 120,000, RF lens% 40, automatic maximum inject time, standard AGC target, minimum MS2 intensity threshold of 5 × 103, MIPS mode to peptide, including charges of 2 to 7 for fragmentation with 30 sec dynamic exclusion. MS2 scans were performed with a quadrupole isolation window of 1.6 m/z, 30% HCD CE, 15,000 resolution, standard AGC target, automatic maximum IT, and fixed first mass of 110 m/z.
2.5.3. Mass Spectrometry Data Analysis
Resulting RAW files were analyzed in Proteome Discover™ 2.5 (Thermo Fisher Scientific) with a Homo sapiens reference proteome FASTA (downloaded from Uniprot 13 May 2022, 78,806 entries) plus common contaminants (73 entries) [47]. Default Minora Feature selection settings were used. SEQUEST HT searches were conducted with a maximum number of 3 missed cleavages, a precursor mass tolerance of 10 ppm, and a fragment mass tolerance of 0.02 Da. Static modifications used for the search were carbamidomethylation on cysteine (C). Dynamic modifications included oxidation of methionine (M), and acetylation, methionine loss, or methionine loss plus acetylation on protein N-termini. Percolator False Discovery Rate was set to a strict peptide spectral match FDR setting of 0.01 and a relaxed setting of 0.05. In the consensus workflow, the default feature mapper settings of a maximum RT shift of 10 min and a minimum S/N threshold of 5 were used. Precursor ion quantification settings use unique razor peptides for quantification, base precurson ion abundance for intensity, and no normalization of scaling. For Quant rollup and hypothesis testing, summed abundances were used with pairwise ratio-based calculations and no imputation. The resulting abundance values for each sample, abundance ratio and log2(abundance ratio) values, and respective p-values from Proteome Discover™ were exported to Microsoft Excel (version 2308).
2.6. Gene Expression Analysis
Total RNA was isolated from JIMT-1 cells treated with 250 µM aCT1 or PBS for 24 h using the GeneJet RNA isolation kit (Thermo Fisher Scientific, Waltham, MA, USA). Gene expression was analyzed using the Breast Cancer 360™ Panel, composed of 758 genes relevant to breast cancer biology and 18 housekeeping genes, on the nCounter platform (NanoString Technologies, Seattle, WA, USA) as described by the manufacturer. NanoString nSolver 4.0 software was used for the analysis of gene expression values, which were normalized using the housekeeping genes and log2 transformed. The software incorporates the R statistics program. N = 3 control or aCT1-treated samples per group were analyzed.
2.7. Mammosphere Assay
JIMT-1 cells were plated in low-adhesion 96-well plates (BrandTech Scientific Inc., Essex, CT, USA) at a density of 500 cells per well in serum-free DMEM/Ham’s F-12 50/50 medium with L-glutamine (Corning, Corning, NY, USA) supplemented with 1× B27 (Gibco, Waltham, MA, USA), 20 ng/mL basic fibroblast growth factor (Gibco, Waltham, MA, USA), 20 ng/mL epidermal growth factor (Sigma-Aldrich, Inc., St. Louis, MO, USA), and 2 µg/mL heparin (StemCell Technologies Inc., Vancouver, BC, Canada). On the day of plating, cells were treated with either vehicle (PBS), lapatinib (100 nM), aCT1 (50 µM), cisplatin (500 nM), a combination of aCT1 and lapatinib, or a combination of aCT1 and cisplatin. After 14 days, the number of spheres with a diameter ≥50 μm was counted using a TCM 400 inverted light microscope (Labomed, Fremont, CA, USA) at 40× magnification. N ≥ 3 independent experiments with at least 8 replicates per treatment.
2.8. Statistical Analysis
GraphPad Prism software (version 8) was used for statistical analysis. Data were expressed as the mean ± standard error (SE) where n = number of independent experiments. Statistical differences among the groups were analyzed using either Student’s t-test for comparisons between two groups or one-way analysis of variance (ANOVA) followed by Tukey’s multiple comparisons test. A statistically significant difference was set at p < 0.05. (* p <0.05, ** p ≤ 0.01, *** p ≤0.001, **** p ≤ 0.0001, ns = not significant).
3. Results
3.1. aCT1 Promotes Gap Junction Intercellular Communication in Refractory HER2+ Breast Cancer Cells
Prior work determined that HER2+ breast cancer cells that have become resistant to HER2-targeted agents have reduced Cx43-mediated GJIC [21]. Therefore, we aimed to determine whether we could reestablish Cx43-mediated GJIC using the Cx43-targeted agent aCT1. To evaluate the effects of aCT1 in this context, we performed a cell-coupling assay (Figure 1A) using the JIMT-1 cell line, which is a HER2+ breast cancer cell line that was isolated from a patient that had developed resistance to trastuzumab (aka Herceptin) [48]. Cells were treated with PBS (CTL) or aCT1 and assessed for coupling. aCT1-treated cells showed increased coupling, suggesting that GJIC was restored (Figure 1B).
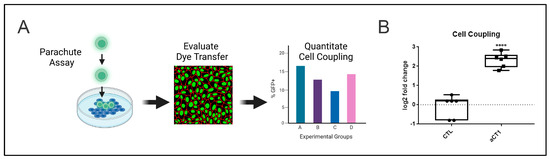
Figure 1.
aCT1 promotes gap junction intercellular communication in refractory HER2+ breast cancer cells. (A) Parachute assay used to determine cell coupling as a measure of gap junction intercellular communication. Created with Biorender. (B) Quantitation of parachute assay from JIMT-1 cells treated with PBS as a control (CTL) or 250 μM aCT1 for 6 hrs. Student’s t-test, unpaired with Welch’s correction **** p < 0.0001.
3.2. Reestablishment of Gap Junction Intercellular Communication by aCT1 Promotes Cx43 Protein Stabilization
A number of reports have indicated that the half-life of Cx43 is within a range of <4 h (hrs) [49,50,51,52,53,54,55]. However, the stability of Cx43 appears to be extended by being within the gap junction plaque structure [56]. These reported observations prompted us to investigate whether the increased GJIC we observed upon aCT1 treatment would lead to increased Cx43 protein stabilization. We treated JIMT-1 cells with PBS or aCT1 for up to 4 h in the presence of the protein synthesis inhibitor cycloheximide to look at protein degradation. We then evaluated the levels of Cx43 protein expression by Western blotting and saw that aCT1 treatment prevented Cx43 degradation, whereas Cx43 levels declined in the absence of aCT1 (Figure 2A). Cells treated with aCT1 and cycloheximide had higher levels of Cx43 than CTL cells treated with cycloheximide (Figure 2B).
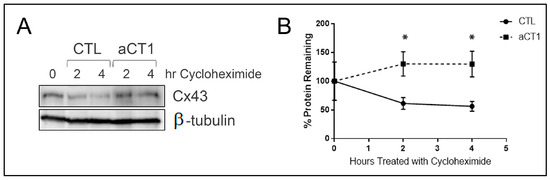
Figure 2.
aCT1 stabilizes Cx43 protein. (A) Western blot of JIMT-1 cells treated with PBS or 100 μM aCT1 in the presence of cycloheximide. (B) Quantitation of Cx43 protein corrected for loading with β-tubulin from n = 3 individual western blots. Student’s t-test, unpaired with Welch’s correction * p < 0.05. The uncropped blots are shown in Supplementary Materials.
3.3. Proteomic Analysis of Proteins that Bind to aCT1
The aCT1 sequence is modeled after the C-terminal sequence of Cx43, which is reported to interact with the tight junction protein ZO-1 [57,58,59]. The reported mechanism of action for aCT1 leading to increased GJIC is binding to ZO-1, thereby physically impairing ZO-1 from preventing gap junction accretion [44]. Additionally, the c-terminus of Cx43 is known to interact with a large number of proteins including src, caveolin, β-catenin, p120-catenin, and tubulin [8,60,61,62]. Therefore, we wanted to assess interacting partners of aCT1 specifically in JIMT-1, resistant HER2+ breast cancer cells. We treated cells with PBS or aCT1 for 4 h and 24 h. Since aCT1 is biotin-tagged, we then pulled down aCT1 using a streptavidin matrix. Coomassie staining to assess for proteins bound to aCT1 showed a large number of proteins present in the 4 h sample but not in the 24 h sample, which resembled the no-peptide control samples (Figure 3A). Although peptide therapeutics are quite promising (currently >80 FDA-approved peptide-based therapies), a major challenge is that peptides have poor stability [63,64]. Consistent with this concept and the reported half-life of Cx43, aCT1 was not detected in the 24 h samples.
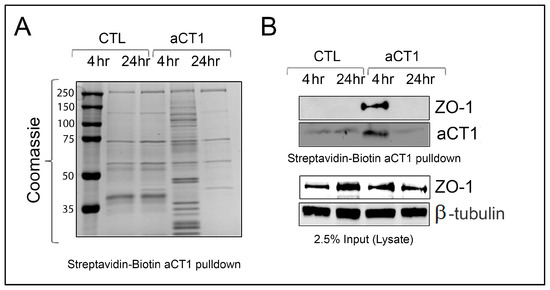
Figure 3.
Proteomic analysis of proteins that bind to aCT1. (A) Streptavidin matrix was used to pulldown Biotin-tagged aCT1 from JIMT-1 cells treated with peptide for indicated time. Coomassie stained gel showing that after 4 hrs of 100 μM aCT1 treatment, a number of proteins bind to aCT1. (B) Western blot analysis showing that aCT1 binds to ZO-1. (Top—pulldown; bottom—input from lysate). The uncropped blots are shown in Supplementary Materials.
To identify proteins bound to aCT1, we submitted aCT1 pulldown samples generated from JIMT-1 cells treated for 4 h for sequencing at the Indiana University School of Medicine Center for Proteome Analysis. To confirm the validity of our assay, we assessed the aCT1 pulldown samples for binding to ZO-1 and confirmed that aCT1 binds ZO-1 by Western blot (Figure 3B). Overall, the proteomic analysis identified >2500 proteins, and 354 of those proteins were bound to aCT1 with high confidence (p-value < 0.0001; Supplemental File S1). We also confirmed the presence of ZO-1 bound to aCT1 in our proteomics data. Caveolin, β-catenin, p120-catenin, and tubulin were also among the >2500 proteins identified.
Because the mechanism of action for aCT1 is that it binds to ZO-1 and other proteins that would normally bind to the C-terminus of Cx43, we assessed the potential consequences of the aCT1 binding partners by performing pathway analysis using the STRING protein–protein interaction network tool (string-db.org; accessed on 26 October 2023) to examine the proteins significantly bound to aCT1 compared to CTL [8]. Here, we report the top pathways identified (Table 1). The full analysis can be found in Supplementary File S2. The results from Gene Ontology (GO) Biological Process, GO Biological Function, KEGG, and Reactome analysis indicated that proteins bound to aCT1 are involved in gene expression, RNA binding, ribosome, and RNA metabolism, respectively (Table 1). Gene Ontology (GO) Biological Process analysis suggests that the proteins we identified that bound to aCT1 are involved in gene expression. This finding is consistent with prior reports that implicate Cx43 as having gene expression regulatory functions [4,65,66]. In particular, Cx43 was found to directly interact with a basic transcription factor 3 (BTF3) to directly regulate transcription of the gene that encodes for N-cadherin, CDH2 [66]. aCT1 bound to BTF3 in our analysis, consistent with these prior findings (Supplemental File S1).

Table 1.
Top pathways from pathway analysis examining the proteins significantly bound to aCT1 compared to CTL.
3.4. aCT1 Impacts Gene Expression
To further assess the ability of aCT1 to alter gene expression, we performed an analysis to determine whether breast cancer signaling pathways are altered in response to aCT1 treatment. Here, we assessed JIMT-1 cells treated with PBS or aCT1 using the NanoString nCounter Breast Cancer 360 panel. Although our data suggest that aCT1 stability is limited beyond 4 h, we were interested to observe if any longer-term effects could be seen in response to peptide treatment. Therefore, we collected JIMT-1 cells after 24 h of aCT1 treatment and analyzed the RNA using the nCounter technology. Using a p-value cutoff of p < 0.05 as significant, we found that 52 of the ~700 genes represented in the panel were significantly altered 24 h after aCT1 treatment (Supplemental File S3 and Figure 4A). nCounter analysis includes 23 different breast cancer-related pathways with specific genes that have been curated to represent those pathways. Directed differential expression analysis comparing aCT1 vs. a baseline of non-aCT1-treated CTL cells showed that aCT1-treated cells had upregulated genes in seventeen of those pathways and downregulated genes in six (Figure 4B). We also analyzed the 52 altered genes using STRING and found that the results from GO Biological Process, GO Biological Function, KEGG, and Reactome analysis indicated that aCT1-altered genes were involved in the cell cycle, protein binding, cancer pathways, and cell junction organization, respectively (Table 2 and Supplemental File S4). Of note, the top two upregulated pathways in the nCounter analysis from aCT1-treated samples are epigenetic regulation and apoptosis, and the top pathway that showed decreased expression was adhesion and migration (Figure 4B).
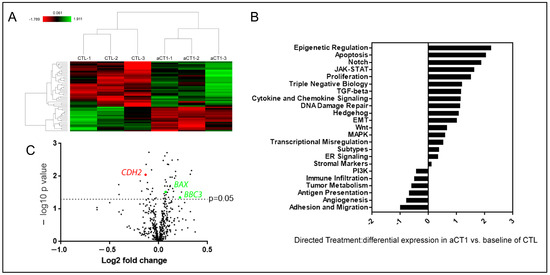
Figure 4.
aCT1 impacts gene expression. (A) Heat map showing genes that were significantly upregulated (in green) and downregulated (in red) in JIMT-1 cells comparing CTL and aCT1 treatment. (B) Directed differential expression analysis of aCT1- vs. CTL- treated JIMT-1 cells and sorted into the pathways represented by the NanoString Breast Cancer 360 nCounter panel. (C) Volcano plot of individual genes that were altered in aCT1 vs. CTL treated JIMT-1 cells. Upregulated genes BAX and BBC3 outlined in green and downregulated gene CDH2 outlined in red. Analysis performed using the nSolver 4.0 software.

Table 2.
Pathway analysis of aCT1 altered genes.
Since N-cadherin, which is regulated by the Cx43 binding protein BTF3, regulates adhesion and migration, we looked for the expression levels of CDH2, which encodes for N-cadherin within our gene expression data. We found that CDH2 is significantly reduced in aCT1-treated samples (Figure 4C).
To further investigate these findings and the anti-cancer effects of aCT1, we evaluated apoptotic genes that were upregulated by aCT1. We observed that the pro-apoptotic factors BAX and BBC3 (aka PUMA) were significantly upregulated by aCT1 (Figure 4C). Prior reports indicate that the reestablishment of GJIC in resistant HER2+ breast cancer cells will resensitize these cells to HER2 inhibitors [21]. Similarly, the upregulation of PUMA promotes the sensitization of cancers, including ovarian and melanoma, to cisplatin [67,68,69]. Therefore, we assessed the ability of aCT1 alone and in combination with lapatinib and cisplatin to impair the tumorigenic properties of the JIMT-1 cells using measurements of cell death and tumorsphere formation. First, we assessed whether aCT1 alone could effectively induce cell death and found that cell death was increased by aCT1 (Figure 5A). We then performed a mammosphere assay as a surrogate for non-adherent tumor cell growth and treated cells with aCT1, lapatinib, or cisplatin alone, or aCT1 in combination with lapatinib or cisplatin. We found that the combination of aCT1 with either agent was significantly more effective at impairing mammosphere growth than any agent alone (Figure 5B).
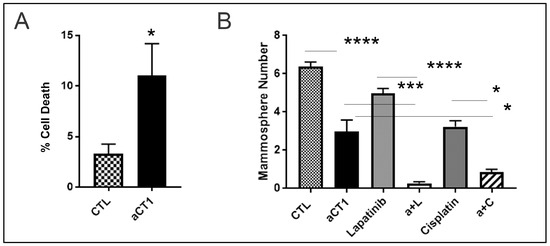
Figure 5.
aCT1 promotes cell death. (A) JIMT-1 cells treated with PBS as a control (CTL) or 250 μM aCT1 were analyzed in monolayer culture using trypan blue exclusion. Unpaired student’s t-test with Welch’s correction * p < 0.05. (B) JIMT-1 cells treated with PBS as a CTL, 50 μM aCT1, 100 nM lapatinib, 500 nM of cisplatin, a combination of aCT1 + laptinib (a + L) or aCT1 + cisplatin (a + C) were assessed by mammosphere assay. One-way ANOVA with Tukey’s multiple comparisons. * p < 0.05, *** p < 0.001, **** p < 0.0001.
4. Discussion
Numerous studies have evaluated Cx43 in breast cancer or other human cancers but fewer have looked at targeting Cx43 with a targeted agent [39,41]. Only a handful of prior studies evaluated the agent aCT1 for use in cancer [12,46,70]. Prior reports have indicated that the mechanism of action for aCT1 is the binding of ZO-1, leading to gap junction accretion, which promotes GJIC [44]. The predicted consequence of aCT1 application leading to increased GJIC is Cx43 stabilization [56]. In this study, we show for the first time in a resistant HER2+ breast cancer cell line that has lost GJIC that aCT1 reestablished GJIC, leading to Cx43 stabilization. Using proteomic and traditional protein–protein biochemical binding analyses, we also demonstrate that aCT1 directly binds ZO-1. New findings from this study show that aCT1 binds to a wide range of proteins, some of which have been previously identified as Cx43 C-terminal interaction proteins as predicted, but also factors that have potentially not been previously studied in such a capacity. We have highlighted previously reported binding partners of the C-terminus of Cx43 in this study: src, caveolin, β-catenin, p120-catenin, and tubulin. These were identified in our screen. We also noted that there was a report that cyclin E1 and p110β are also binding partners of either the C-terminus of Cx43 or aCT1 [45,71]. We did not identify these factors in our proteomic analysis. However, our genomic analysis showed decreased PI3K signaling, which is consistent with the effect aCT1 would have by binding to p110β.
Canonical signaling places Cx43 at the cell membrane in gap junctions and hemichannels. However, non-canonical functions of Cx43 in relation to its interactome are also reported [8,72,73,74,75]. A prior study in prostate cancer showed that Cx43 elevation was associated with increased metastatic potential of prostate cancer cells. However, application of aCT1 did not have anti-cancer effects and it was suggested by the authors that there may be gap junction-independent (i.e., non-canonical) roles for Cx43 in prostate cancer [76]. Our studies found that aCT1, like the C-terminus of Cx43, binds to a host of proteins, and as expected, a portion of these interacting proteins are pertinent to Cx43 functions at the membrane, while others are important for other cellular functions, most notably gene expression and RNA regulation. Others have reported a direct ability of Cx43 to enter the nucleus and regulate transcription [66,77]. The example that we presented was the regulation of BTF3. Cx43 binds to BTF3 to regulate the transcription of CDH2, which encodes for the N-cadherin protein [66]. aCT1 bound to BTF3 in our proteomic analysis and consistent with this, the gene that encodes N-cadherin, CDH2, was significantly reduced in aCT1-treated samples in our gene expression analysis using the NanoString nCounter Breast Cancer 360 panel. This finding is consistent with the role of Cx43 in promoting N-cadherin expression as a pro-cancer function and with the predicted effect of aCT1 having an anti-cancer effect. Our data show that aCT1 binds to BTF3, presumably impairing its ability to interact with Cx43. As a consequence, we would expect CDH2 expression to also be reduced in aCT1-treated samples, and this is what we observed.
An area of ongoing investigation is Cx43′s role in metastasis. Some findings suggest that gap junctions could play a role in the establishment of metastatic colonies in tissues where tumor cells have disseminated [23,40]. In support of this conjecture, prior studies with aCT1 in cells, rodents, and humans indicate that aCT1 has wound-healing properties [78,79,80,81,82]. However, other studies suggest an anti-angiogenic effect of aCT1 [83] and a pro-metastatic effect of preventing Cx43 GJIC [21].
Like other studies that have reported the anti-cancer effects of aCT1 [45,84], our prior studies have implicated Cx43 as a therapeutic target in HER2+ breast cancer [12,21]. Based on our prior findings, it is predicted that the reestablishment of GJIC in resistant HER2+ breast cancer cells, which are gap junction-deficient, will resensitize cells to HER2-targeted agents. We now show this prediction to be true using a mammophere assay, which acts as a type of in vitro surrogate for tumor growth. Our findings demonstrate that the combination of aCT1 and lapatinib is highly effective at preventing sphere development and growth compared to CTL or single agents on their own. This finding is also consistent with previous studies that report an additive or synergistic effect of aCT1 with other anti-cancer chemotherapeutic agents [12,45,84]. Furthermore, new gene expression data indicates that aCT1 induces the expression of the pro-apoptotic genes BAX and BBC3. This finding is consistent with prior reports and the suggested outcome of BBC3 induction leading to the sensitization of cancer cells to cisplatin [67,68,69], we find that aCT1 combined with cisplatin has a greater effect than either single agent on its own. Taken together, our findings provide a more complete picture of the scope of anti-cancer effects induced by the Cx43-targeted agent, aCT1, painting a picture of how to move forward with implementing a strategy for the use of this agent for HER2+ breast cancers, and perhaps other human cancers.
5. Conclusions
In this study, we examined the mechanisms for the anti-cancer effects of a therapeutic peptide agent targeted to Cx43 called aCT1. Findings from this study confirm that aCT1 promotes gap junction intercellular communication and Cx43 protein stabilization and binds to ZO-1 in resistant HER2+ breast cancer cells. These findings are consistent with prior reports on the mechanism of action of this agent. New findings from this study identify novel aCT1-interacting proteins and the effects of aCT1 on breast cancer signaling. nCounter analysis using the NanoString Breast Cancer 360 panel showed that aCT1 significantly altered apoptosis, leading to improved efficacy of lapatinib and cisplatin in combination with aCT1.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/cancers16020423/s1, Supplementary File S1: aCT1 proteomic data; Supplementary File S2: aCT1 binding partner STRING pathway analysis.; Supplementary File S3: aCT1 v CTL nCounter; Supplementary File S4: aCT1 nCounter STRING pathway analysis. Uncropped blots for Figure 2 and Figure 3 are also found in supplementary files.
Author Contributions
Conceptualization, E.S.Y. and K.M.B.; methodology, E.S.Y., M.A., E.H.D., A.L.O. and K.M.B.; formal analysis, E.S.Y. and K.M.B.; resources, E.S.Y.; writing—original draft preparation, E.S.Y., E.H.D. and K.M.B.; writing—review and editing, E.S.Y. and K.M.B.; supervision, E.S.Y.; project administration, E.S.Y.; funding acquisition, E.S.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported in part by a generous gift from the Catherine Peachey Fund.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Raw and processed mass spectrometry data are available through the MassIVE Repository (a ProteomeXchange partner. Accession MSV000093550; Reviewer login information username Reviewer_ MSV000093550; Password: Act1). nCounter data are available at NCBI GEO (GSE250543). Data are also available in Supplemental Files S1–S4.
Acknowledgments
The authors acknowledge the many researchers who have contributed to this field of research. We apologize if we missed any key articles among the citations, which was not intended. Mass spectrometry was provided by the Indiana University School of Medicine Center for Proteome Analysis. NanoString nCounter analysis was provided by the Indiana University School of Medicine SNRI Biomarkers Core.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bonacquisti, E.E.; Nguyen, J. Connexin 43 (Cx43) in cancer: Implications for therapeutic approaches via gap junctions. Cancer Lett. 2019, 442, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Wang, Z.Z.; Chen, N.H. Connexin 43 Phosphorylation: Implications in Multiple Diseases. Molecules 2023, 28, 4914. [Google Scholar] [CrossRef]
- Montgomery, J.; Ghatnekar, G.S.; Grek, C.L.; Moyer, K.E.; Gourdie, R.G. Connexin 43-Based Therapeutics for Dermal Wound Healing. Int. J. Mol. Sci. 2018, 19, 1778. [Google Scholar] [CrossRef]
- Phillips, S.L.; Williams, C.B.; Zambrano, J.N.; Williams, C.J.; Yeh, E.S. Connexin 43 in the development and progression of breast cancer: What’s the connection? (Review). Int. J. Oncol. 2017, 51, 1005–1013. [Google Scholar] [CrossRef]
- Prakoura, N.; Kavvadas, P.; Chadjichristos, C.E. Connexin 43: A New Therapeutic Target Against Chronic Kidney Disease. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2018, 49, 985. [Google Scholar] [CrossRef] [PubMed]
- Andelova, K.; Egan Benova, T.; Szeiffova Bacova, B.; Sykora, M.; Prado, N.J.; Diez, E.R.; Hlivak, P.; Tribulova, N. Cardiac Connexin-43 Hemichannels and Pannexin1 Channels: Provocative Antiarrhythmic Targets. Int. J. Mol. Sci. 2020, 22, 260. [Google Scholar] [CrossRef]
- Schulz, R.; Gorge, P.M.; Gorbe, A.; Ferdinandy, P.; Lampe, P.D.; Leybaert, L. Connexin 43 is an emerging therapeutic target in ischemia/reperfusion injury, cardioprotection and neuroprotection. Pharmacol. Ther. 2015, 153, 90–106. [Google Scholar] [CrossRef] [PubMed]
- Leithe, E.; Mesnil, M.; Aasen, T. The connexin 43 C-terminus: A tail of many tales. Biochim. Biophys. Acta 2017, 1860, 48–64. [Google Scholar] [CrossRef]
- Busby, M.; Hallett, M.T.; Plante, I. The Complex Subtype-Dependent Role of Connexin 43 (GJA1) in Breast Cancer. Int. J. Mol. Sci. 2018, 19, 693. [Google Scholar] [CrossRef]
- Choudhary, M.; Naczki, C.; Chen, W.; Barlow, K.D.; Case, L.D.; Metheny-Barlow, L.J. Tumor-induced loss of mural Connexin 43 gap junction activity promotes endothelial proliferation. BMC Cancer 2015, 15, 427. [Google Scholar] [CrossRef]
- Lee, S.W.; Tomasetto, C.; Paul, D.; Keyomarsi, K.; Sager, R. Transcriptional downregulation of gap-junction proteins blocks junctional communication in human mammary tumor cell lines. J. Cell Biol. 1992, 118, 1213–1221. [Google Scholar] [CrossRef]
- Grek, C.L.; Rhett, J.M.; Bruce, J.S.; Abt, M.A.; Ghatnekar, G.S.; Yeh, E.S. Targeting connexin 43 with alpha-connexin carboxyl-terminal (ACT1) peptide enhances the activity of the targeted inhibitors, tamoxifen and lapatinib, in breast cancer: Clinical implication for ACT1. BMC Cancer 2015, 15, 296. [Google Scholar] [CrossRef] [PubMed]
- Jiang, G.; Dong, S.; Yu, M.; Han, X.; Zheng, C.; Zhu, X.; Tong, X. Influence of gap junction intercellular communication composed of connexin 43 on the antineoplastic effect of adriamycin in breast cancer cells. Oncol. Lett. 2017, 13, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Kanczuga-Koda, L.; Sulkowski, S.; Lenczewski, A.; Koda, M.; Wincewicz, A.; Baltaziak, M.; Sulkowska, M. Increased expression of connexins 26 and 43 in lymph node metastases of breast cancer. J. Clin. Pathol. 2006, 59, 429–433. [Google Scholar] [CrossRef]
- Cai, J.; Jiang, W.G.; Mansel, R.E. Gap junctional communication and the tyrosine phosphorylation of connexin 43 in interaction between breast cancer and endothelial cells. Int. J. Mol. Med. 1998, 1, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Hirschi, K.K.; Xu, C.E.; Tsukamoto, T.; Sager, R. Gap junction genes Cx26 and Cx43 individually suppress the cancer phenotype of human mammary carcinoma cells and restore differentiation potential. Cell Growth Differ. Mol. Biol. J. Am. Assoc. Cancer Res. 1996, 7, 861–870. [Google Scholar]
- Ding, Y.; Nguyen, T.A. Gap Junction Enhancer Potentiates Cytotoxicity of Cisplatin in Breast Cancer Cells. J. Cancer Sci. Ther. 2012, 4, 371–378. [Google Scholar] [CrossRef]
- Monaghan, P.; Clarke, C.; Perusinghe, N.P.; Moss, D.W.; Chen, X.Y.; Evans, W.H. Gap junction distribution and connexin expression in human breast. Exp. Cell Res. 1996, 223, 29–38. [Google Scholar] [CrossRef]
- Kanczuga-Koda, L.; Sulkowska, M.; Koda, M.; Reszec, J.; Famulski, W.; Baltaziak, M.; Sulkowski, S. Expression of connexin 43 in breast cancer in comparison with mammary dysplasia and the normal mammary gland. Folia Morphol. 2003, 62, 439–442. [Google Scholar]
- Li, Z.; Zhou, Z.; Welch, D.R.; Donahue, H.J. Expressing connexin 43 in breast cancer cells reduces their metastasis to lungs. Clin. Exp. Metastasis 2008, 25, 893–901. [Google Scholar] [CrossRef]
- Yeh, E.S.; Williams, C.J.; Williams, C.B.; Bonilla, I.V.; Klauber-DeMore, N.; Phillips, S.L. Dysregulated connexin 43 in HER2-positive drug resistant breast cancer cells enhances proliferation and migration. Oncotarget 2017, 8, 109358–109369. [Google Scholar] [CrossRef]
- Laird, D.W.; Fistouris, P.; Batist, G.; Alpert, L.; Huynh, H.T.; Carystinos, G.D.; Alaoui-Jamali, M.A. Deficiency of connexin43 gap junctions is an independent marker for breast tumors. Cancer Res. 1999, 59, 4104–4110. [Google Scholar]
- Plante, I.; Stewart, M.K.; Barr, K.; Allan, A.L.; Laird, D.W. Cx43 suppresses mammary tumor metastasis to the lung in a Cx43 mutant mouse model of human disease. Oncogene 2011, 30, 1681–1692. [Google Scholar] [CrossRef] [PubMed]
- McLachlan, E.; Shao, Q.; Laird, D.W. Connexins and gap junctions in mammary gland development and breast cancer progression. J. Membr. Biol. 2007, 218, 107–121. [Google Scholar] [CrossRef] [PubMed]
- McLachlan, E.; Shao, Q.; Wang, H.L.; Langlois, S.; Laird, D.W. Connexins act as tumor suppressors in three-dimensional mammary cell organoids by regulating differentiation and angiogenesis. Cancer Res. 2006, 66, 9886–9894. [Google Scholar] [CrossRef]
- Shishido, S.N.; Delahaye, A.; Beck, A.; Nguyen, T.A. The anticancer effect of PQ1 in the MMTV-PyVT mouse model. Int. J. Cancer 2014, 134, 1474–1483. [Google Scholar] [CrossRef]
- Kanczuga-Koda, L.; Sulkowski, S.; Tomaszewski, J.; Koda, M.; Sulkowska, M.; Przystupa, W.; Golaszewska, J.; Baltaziak, M. Connexins 26 and 43 correlate with Bak, but not with Bcl-2 protein in breast cancer. Oncol. Rep. 2005, 14, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, S.; Going, J.J.; D’Arcy, R.; George, W.D. Expression of gap junction proteins connexin 26 and connexin 43 in normal human breast and in breast tumours. J. Pathol. 1998, 184, 37–43. [Google Scholar] [CrossRef]
- Wilgenbus, K.K.; Kirkpatrick, C.J.; Knuechel, R.; Willecke, K.; Traub, O. Expression of Cx26, Cx32 and Cx43 gap junction proteins in normal and neoplastic human tissues. Int. J. Cancer J. 1992, 51, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Teleki, I.; Szasz, A.M.; Maros, M.E.; Gyorffy, B.; Kulka, J.; Meggyeshazi, N.; Kiszner, G.; Balla, P.; Samu, A.; Krenacs, T. Correlations of differentially expressed gap junction connexins Cx26, Cx30, Cx32, Cx43 and Cx46 with breast cancer progression and prognosis. PLoS ONE 2014, 9, e112541. [Google Scholar] [CrossRef]
- Teleki, I.; Krenacs, T.; Szasz, M.A.; Kulka, J.; Wichmann, B.; Leo, C.; Papassotiropoulos, B.; Riemenschnitter, C.; Moch, H.; Varga, Z. The potential prognostic value of connexin 26 and 46 expression in neoadjuvant-treated breast cancer. BMC Cancer 2013, 13, 50. [Google Scholar] [CrossRef]
- Stoletov, K.; Strnadel, J.; Zardouzian, E.; Momiyama, M.; Park, F.D.; Kelber, J.A.; Pizzo, D.P.; Hoffman, R.; VandenBerg, S.R.; Klemke, R.L. Role of connexins in metastatic breast cancer and melanoma brain colonization. J. Cell Sci. 2013, 126 Pt 4, 904–913. [Google Scholar] [CrossRef]
- Tanaka, T.; Yamasaki, H.; Mesnil, M. Stimulation of intercellular communication of poor-communicating cells by gap-junction-competent cells enhances the HSV-TK/GCV bystander effect in vitro. Int. J. Cancer J. 2001, 91, 538–542. [Google Scholar] [CrossRef]
- Mancuso, M.; Pasquali, E.; Leonardi, S.; Rebessi, S.; Tanori, M.; Giardullo, P.; Borra, F.; Pazzaglia, S.; Naus, C.C.; Di Majo, V.; et al. Role of connexin43 and ATP in long-range bystander radiation damage and oncogenesis in vivo. Oncogene 2011, 30, 4601–4608. [Google Scholar] [CrossRef]
- Kandouz, M.; Batist, G. Gap junctions and connexins as therapeutic targets in cancer. Expert Opin. Ther. Targets 2010, 14, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Sanson, M.; Marcaud, V.; Robin, E.; Valery, C.; Sturtz, F.; Zalc, B. Connexin 43-mediated bystander effect in two rat glioma cell models. Cancer Gene Ther. 2002, 9, 149–155. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Naus, C.C.; Laird, D.W. Implications and challenges of connexin connections to cancer. Nat. Rev. Cancer 2010, 10, 435–441. [Google Scholar] [CrossRef]
- Spray, D.C.; Hanstein, R.; Lopez-Quintero, S.V.; Stout, R.F.; Jr Suadicani, S.O.; Thi, M.M. Gap junctions and Bystander Effects: Good Samaritans and executioners. Wiley Interdiscip. Rev. Membr. Transp. Signal. 2013, 2, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Grek, C.L.; Rhett, J.M.; Bruce, J.S.; Ghatnekar, G.S.; Yeh, E.S. Connexin 43, breast cancer tumor suppressor: Missed connections? Cancer Lett. 2016, 374, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Boire, A.; Jin, X.; Valiente, M.; Er, E.E.; Lopez-Soto, A.; Jacob, L.; Patwa, R.; Shah, H.; Xu, K.; et al. Carcinoma-astrocyte gap junctions promote brain metastasis by cGAMP transfer. Nature 2016, 533, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Rhett, J.M.; Yeh, E.S. The Potential for Connexin Hemichannels to Drive Breast Cancer Progression through Regulation of the Inflammatory Response. Int. J. Mol. Sci. 2018, 19, 1043. [Google Scholar] [CrossRef]
- Evans, W.H.; Bultynck, G.; Leybaert, L. Manipulating connexin communication channels: Use of peptidomimetics and the translational outputs. J. Membr. Biol. 2012, 245, 437–449. [Google Scholar] [CrossRef] [PubMed]
- De Vuyst, E.; Boengler, K.; Antoons, G.; Sipido, K.R.; Schulz, R.; Leybaert, L. Pharmacological modulation of connexin-formed channels in cardiac pathophysiology. Br. J. Pharmacol. 2011, 163, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Hunter, A.W.; Barker, R.J.; Zhu, C.; Gourdie, R.G. Zonula occludens-1 alters connexin43 gap junction size and organization by influencing channel accretion. Mol. Biol. Cell 2005, 16, 5686–5698. [Google Scholar] [CrossRef] [PubMed]
- Pridham, K.J.; Shah, F.; Hutchings, K.R.; Sheng, K.L.; Guo, S.; Liu, M.; Kanabur, P.; Lamouille, S.; Lewis, G.; Morales, M.; et al. Connexin 43 confers chemoresistance through activating PI3K. Oncogenesis 2022, 11, 2. [Google Scholar] [CrossRef]
- Sato, A.; da Fonseca, I.I.M.; Nagamine, M.K.; de Toledo, G.F.; Olio, R.; Hernandez-Blazquez, F.J.; Yano, T.; Yeh, E.S.; Dagli, M.L.Z. Effects of Alpha-Connexin Carboxyl-Terminal Peptide (aCT1) and Bowman-Birk Protease Inhibitor (BBI) on Canine Oral Mucosal Melanoma (OMM) Cells. Front. Vet. Sci. 2021, 8, 670451. [Google Scholar] [CrossRef]
- Orsburn, B.C. Proteome Discoverer-A Community Enhanced Data Processing Suite for Protein Informatics. Proteomes 2021, 9, 15. [Google Scholar] [CrossRef]
- Tanner, M.; Kapanen, A.I.; Junttila, T.; Raheem, O.; Grenman, S.; Elo, J.; Elenius, K.; Isola, J. Characterization of a novel cell line established from a patient with Herceptin-resistant breast cancer. Mol. Cancer Ther. 2004, 3, 1585–1592. [Google Scholar] [CrossRef]
- Laird, D.W.; Puranam, K.L.; Revel, J.P. Turnover and phosphorylation dynamics of connexin43 gap junction protein in cultured cardiac myocytes. Biochem. J. 1991, 273 Pt 1, 67–72. [Google Scholar] [CrossRef]
- Crow, D.S.; Beyer, E.C.; Paul, D.L.; Kobe, S.S.; Lau, A.F. Phosphorylation of connexin43 gap junction protein in uninfected and Rous sarcoma virus-transformed mammalian fibroblasts. Mol. Cell. Biol. 1990, 10, 1754–1763. [Google Scholar]
- Lampe, P.D. Analyzing phorbol ester effects on gap junctional communication: A dramatic inhibition of assembly. J. Cell Biol. 1994, 127 Pt 2, 1895–1905. [Google Scholar] [CrossRef] [PubMed]
- Musil, L.S.; Beyer, E.C.; Goodenough, D.A. Expression of the gap junction protein connexin43 in embryonic chick lens: Molecular cloning, ultrastructural localization, and post-translational phosphorylation. J. Membr. Biol. 1990, 116, 163–175. [Google Scholar] [CrossRef]
- Beardslee, M.A.; Laing, J.G.; Beyer, E.C.; Saffitz, J.E. Rapid turnover of connexin43 in the adult rat heart. Circ. Res. 1998, 83, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Hertlein, B.; Butterweck, A.; Haubrich, S.; Willecke, K.; Traub, O. Phosphorylated carboxy terminal serine residues stabilize the mouse gap junction protein connexin45 against degradation. J. Membr. Biol. 1998, 162, 247–257. [Google Scholar] [CrossRef]
- Darrow, B.J.; Laing, J.G.; Lampe, P.D.; Saffitz, J.E.; Beyer, E.C. Expression of multiple connexins in cultured neonatal rat ventricular myocytes. Circ. Res. 1995, 76, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Gilleron, J.; Fiorini, C.; Carette, D.; Avondet, C.; Falk, M.M.; Segretain, D.; Pointis, G. Molecular reorganization of Cx43, Zo-1 and Src complexes during the endocytosis of gap junction plaques in response to a non-genomic carcinogen. J. Cell Sci. 2008, 121 Pt 24, 4069–4078. [Google Scholar] [CrossRef]
- Sorgen, P.L.; Duffy, H.S.; Sahoo, P.; Coombs, W.; Delmar, M.; Spray, D.C. Structural changes in the carboxyl terminus of the gap junction protein connexin43 indicates signaling between binding domains for c-Src and zonula occludens-1. J. Biol. Chem. 2004, 279, 54695–54701. [Google Scholar] [CrossRef]
- Sorgen, P.L.; Trease, A.J.; Spagnol, G.; Delmar, M.; Nielsen, M.S. Protein(-)Protein Interactions with Connexin 43: Regulation and Function. Int. J. Mol. Sci. 2018, 19, 1428. [Google Scholar] [CrossRef]
- Giepmans, B.N.; Moolenaar, W.H. The gap junction protein connexin43 interacts with the second PDZ domain of the zona occludens-1 protein. Curr. Biol. CB 1998, 8, 931–934. [Google Scholar] [CrossRef]
- Giepmans, B.N.; Hengeveld, T.; Postma, F.R.; Moolenaar, W.H. Interaction of c-Src with gap junction protein connexin-43. Role in the regulation of cell-cell communication. J. Biol. Chem. 2001, 276, 8544–8549. [Google Scholar] [CrossRef]
- Schubert, A.L.; Schubert, W.; Spray, D.C.; Lisanti, M.P. Connexin family members target to lipid raft domains and interact with caveolin-1. Biochemistry 2002, 41, 5754–5764. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Li, W.E.; Huang, G.Y.; Meyer, R.; Chen, T.; Luo, Y.; Thomas, M.P.; Radice, G.L.; Lo, C.W. Modulation of mouse neural crest cell motility by N-cadherin and connexin 43 gap junctions. J. Cell Biol. 2001, 154, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Lamers, C. Overcoming the shortcomings of peptide-based therapeutics. Future Drug Discov. 2022, 4, FDD75. [Google Scholar] [CrossRef]
- Wang, L.; Wang, N.; Zhang, W.; Cheng, X.; Yan, Z.; Shao, G.; Wang, X.; Wang, R.; Fu, C. Therapeutic peptides: Current applications and future directions. Signal Transduct. Target. Ther. 2022, 7, 48. [Google Scholar] [CrossRef] [PubMed]
- Hebert, C.; Stains, J.P. An intact connexin43 is required to enhance signaling and gene expression in osteoblast-like cells. J. Cell. Biochem. 2013, 114, 2542–2550. [Google Scholar] [CrossRef] [PubMed]
- Kotini, M.; Barriga, E.H.; Leslie, J.; Gentzel, M.; Rauschenberger, V.; Schambony, A.; Mayor, R. Gap junction protein Connexin-43 is a direct transcriptional regulator of N-cadherin in vivo. Nat. Commun. 2018, 9, 3846. [Google Scholar] [CrossRef]
- Yuan, Z.; Cao, K.; Lin, C.; Li, L.; Liu, H.Y.; Zhao, X.Y.; Liu, L.; Deng, H.X.; Li, J.; Nie, C.L.; et al. The p53 upregulated modulator of apoptosis (PUMA) chemosensitizes intrinsically resistant ovarian cancer cells to cisplatin by lowering the threshold set by Bcl-x(L) and Mcl-1. Mol. Med. 2011, 17, 1262–1274. [Google Scholar] [CrossRef]
- Jiang, F.; Zhao, W.; Zhou, L.; Liu, Z.; Li, W.; Yu, D. MiR-222 targeted PUMA to improve sensitization of UM1 cells to cisplatin. Int. J. Mol. Sci. 2014, 15, 22128–22141. [Google Scholar] [CrossRef]
- Haydn, J.M.; Hufnagel, A.; Grimm, J.; Maurus, K.; Schartl, M.; Meierjohann, S. The MAPK pathway as an apoptosis enhancer in melanoma. Oncotarget 2014, 5, 5040–5053. [Google Scholar] [CrossRef]
- Montgomery, J.; Richardson, W.J.; Marsh, S.; Rhett, J.M.; Bustos, F.; Degen, K.; Ghatnekar, G.S.; Grek, C.L.; Jourdan, L.J.; Holmes, J.W.; et al. The connexin 43 carboxyl terminal mimetic peptide alphaCT1 prompts differentiation of a collagen scar matrix in humans resembling unwounded skin. FASEB J. 2021, 35, e21762. [Google Scholar] [CrossRef]
- Johnstone, S.R.; Kroncke, B.M.; Straub, A.C.; Best, A.K.; Dunn, C.A.; Mitchell, L.A.; Peskova, Y.; Nakamoto, R.K.; Koval, M.; Lo, C.W.; et al. MAPK phosphorylation of connexin 43 promotes binding of cyclin E and smooth muscle cell proliferation. Circ. Res. 2012, 111, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Giepmans, B.N. Role of connexin43-interacting proteins at gap junctions. Adv. Cardiol. 2006, 42, 41–56. [Google Scholar] [PubMed]
- Giepmans, B.N. Gap junctions and connexin-interacting proteins. Cardiovasc. Res. 2004, 62, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Herve, J.C.; Derangeon, M.; Sarrouilhe, D.; Giepmans, B.N.; Bourmeyster, N. Gap junctional channels are parts of multiprotein complexes. Biochim. Biophys. Acta 2012, 1818, 1844–1865. [Google Scholar] [CrossRef] [PubMed]
- Laird, D.W. The gap junction proteome and its relationship to disease. Trends Cell Biol. 2010, 20, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Hitomi, M.; Bar-Shain, N.; Dalimov, Z.; Ellis, L.; Velpula, K.K.; Fraizer, G.C.; Gourdie, R.G.; Lathia, J.D. Connexin 43 expression is associated with increased malignancy in prostate cancer cell lines and functions to promote migration. Oncotarget 2015, 6, 11640–11651. [Google Scholar] [CrossRef]
- Dang, X.; Doble, B.W.; Kardami, E. The carboxy-tail of connexin-43 localizes to the nucleus and inhibits cell growth. Mol. Cell. Biochem. 2003, 242, 35–38. [Google Scholar] [CrossRef]
- Ghatnekar, G.S.; Grek, C.L.; Armstrong, D.G.; Desai, S.C.; Gourdie, R.G. The effect of a connexin43-based Peptide on the healing of chronic venous leg ulcers: A multicenter, randomized trial. J. Investig. Dermatol. 2015, 135, 289–298. [Google Scholar] [CrossRef]
- Ghatnekar, G.S.; O’Quinn, M.P.; Jourdan, L.J.; Gurjarpadhye, A.A.; Draughn, R.L.; Gourdie, R.G. Connexin43 carboxyl-terminal peptides reduce scar progenitor and promote regenerative healing following skin wounding. Regen. Med. 2009, 4, 205–223. [Google Scholar] [CrossRef]
- Soder, B.L.; Propst, J.T.; Brooks, T.M.; Goodwin, R.L.; Friedman, H.I.; Yost, M.J.; Gourdie, R.G. The connexin43 carboxyl-terminal peptide ACT1 modulates the biological response to silicone implants. Plast. Reconstr. Surg. 2009, 123, 1440–1451. [Google Scholar] [CrossRef]
- Grek, C.L.; Prasad, G.M.; Viswanathan, V.; Armstrong, D.G.; Gourdie, R.G.; Ghatnekar, G.S. Topical administration of a Connexin43-based peptide augments healing of chronic neuropathic diabetic foot ulcers: A multicenter, randomized trial. Wound Repair Regen. Off. Publ. Wound Heal. Soc. Eur. Tissue Repair Soc. 2015, 23, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Grek, C.L.; Montgomery, J.; Sharma, M.; Ravi, A.; Rajkumar, J.S.; Moyer, K.E.; Gourdie, R.G.; Ghatnekar, G.S. A Multicenter Randomized Controlled Trial Evaluating a Cx43-Mimetic Peptide in Cutaneous Scarring. J. Investig. Dermatol. 2017, 137, 620–630. [Google Scholar] [CrossRef] [PubMed]
- Obert, E.; Grek, C.; Ghatnekar, G.; Rohrer, B. Evaluation of a connexin-based peptide for the treatment of age-related macular degeneration. Heliyon 2022, 8, e11359. [Google Scholar] [CrossRef] [PubMed]
- Che, J.; DePalma, T.J.; Sivakumar, H.; Mezache, L.S.; Tallman, M.M.; Venere, M.; Swindle-Reilly, K.; Veeraraghavan, R.; Skardal, A. alphaCT1 peptide sensitizes glioma cells to temozolomide in a glioblastoma organoid platform. Biotechnol. Bioeng. 2023, 120, 1108–1119. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).