Tumor Response on Diagnostic Imaging after Proton Beam Therapy for Hepatocellular Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Patients
2.2. Proton Beam Therapy
2.3. Follow-Up Procedure
2.4. Statistical Analysis
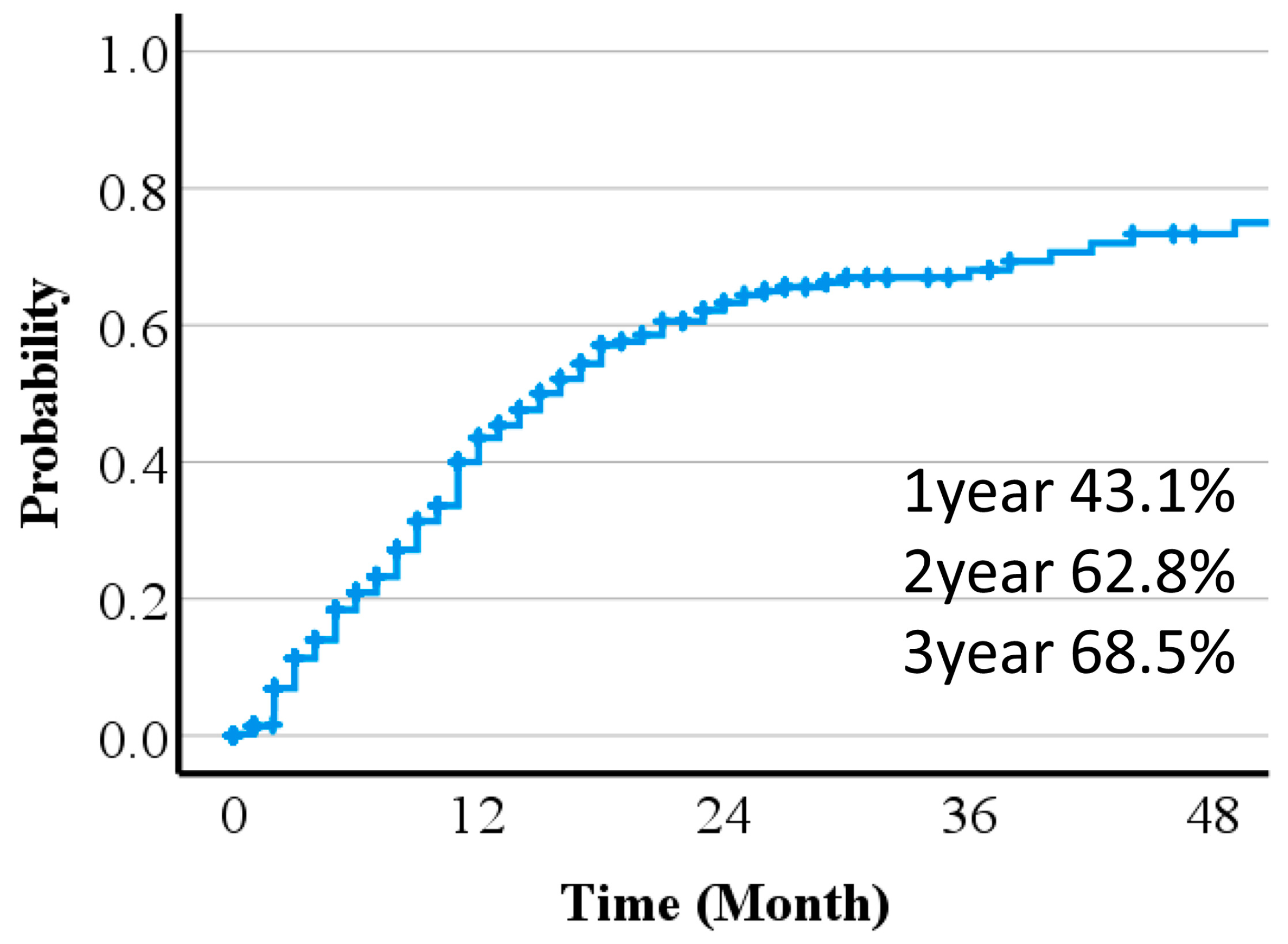
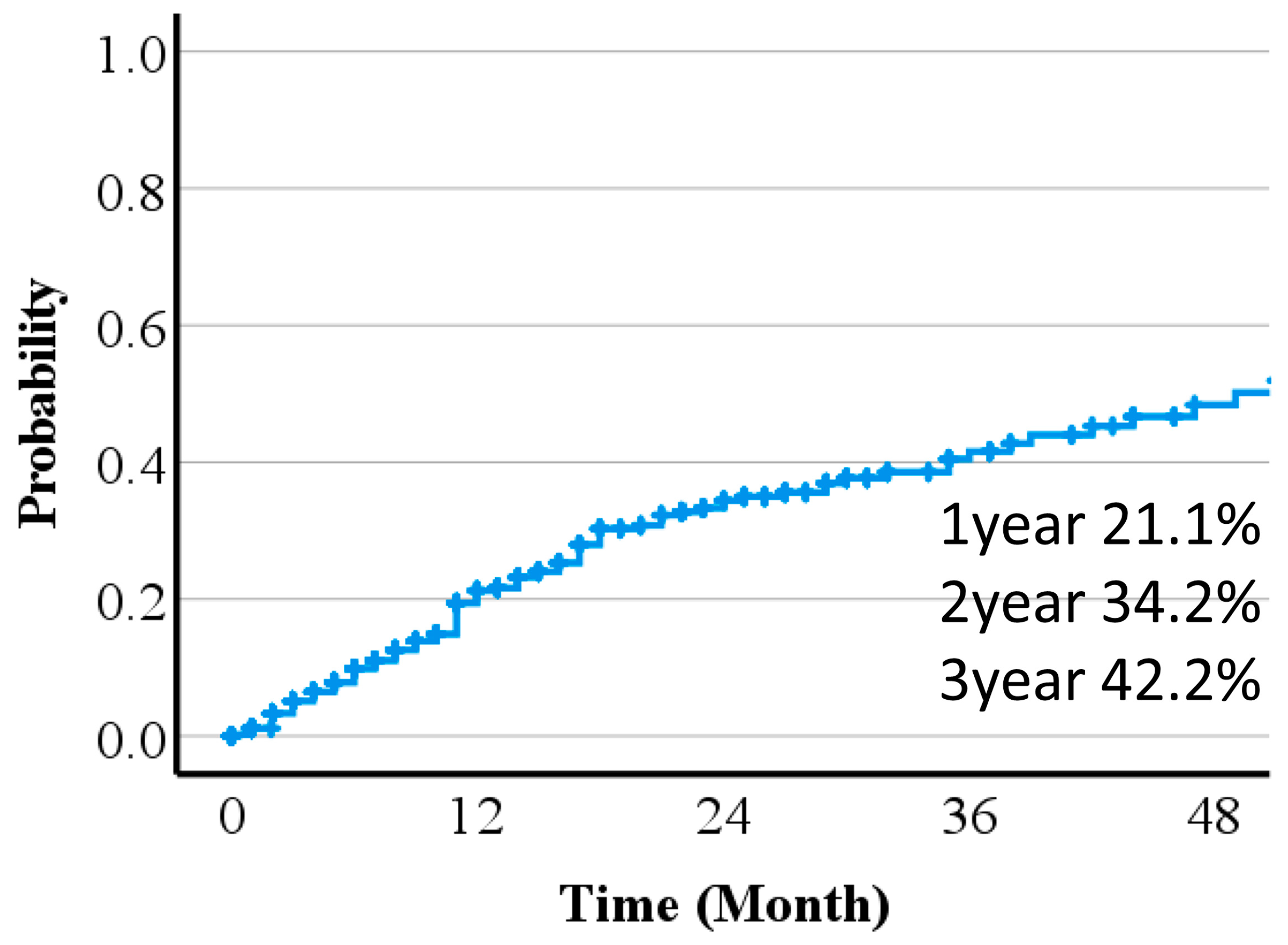
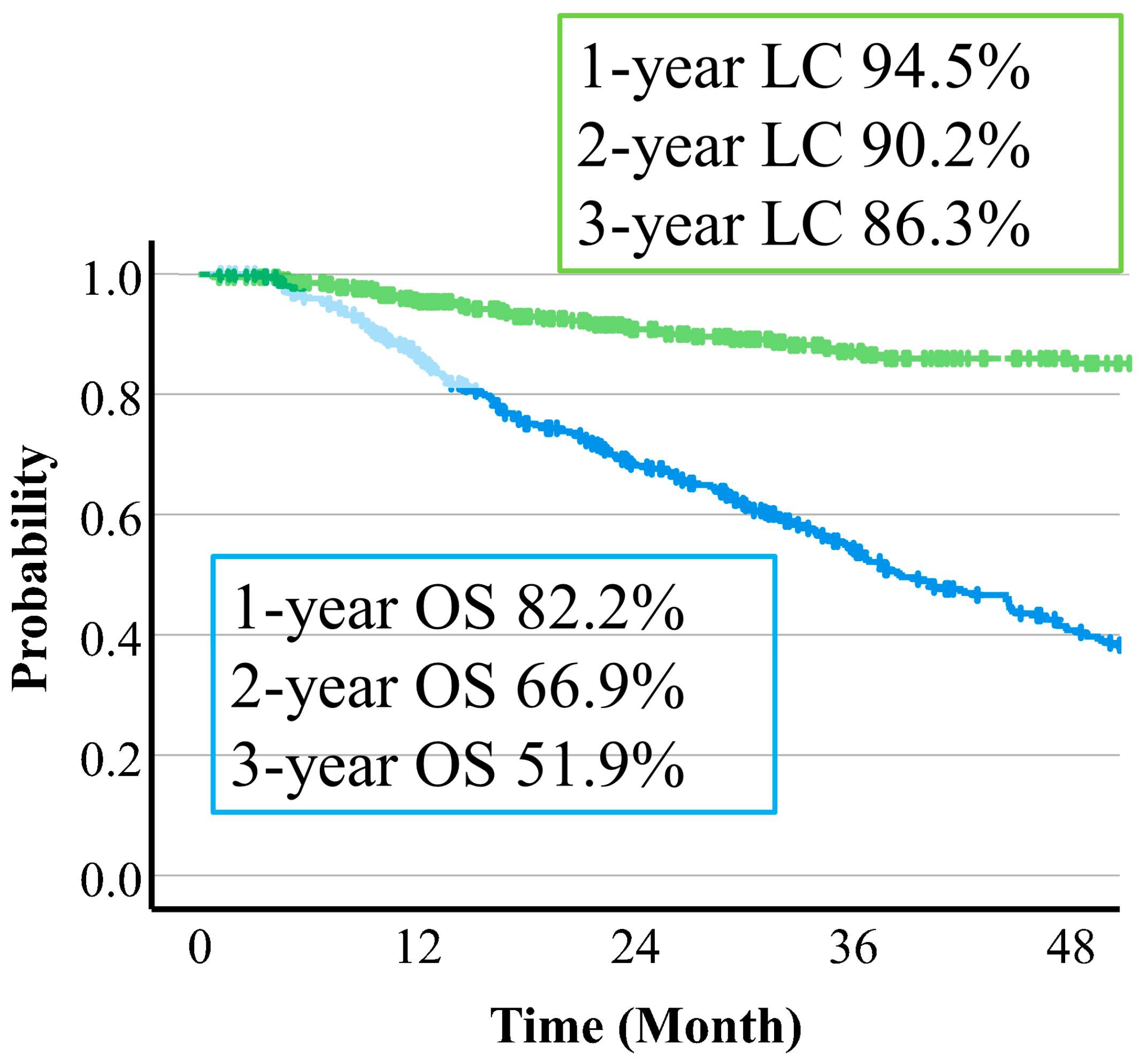
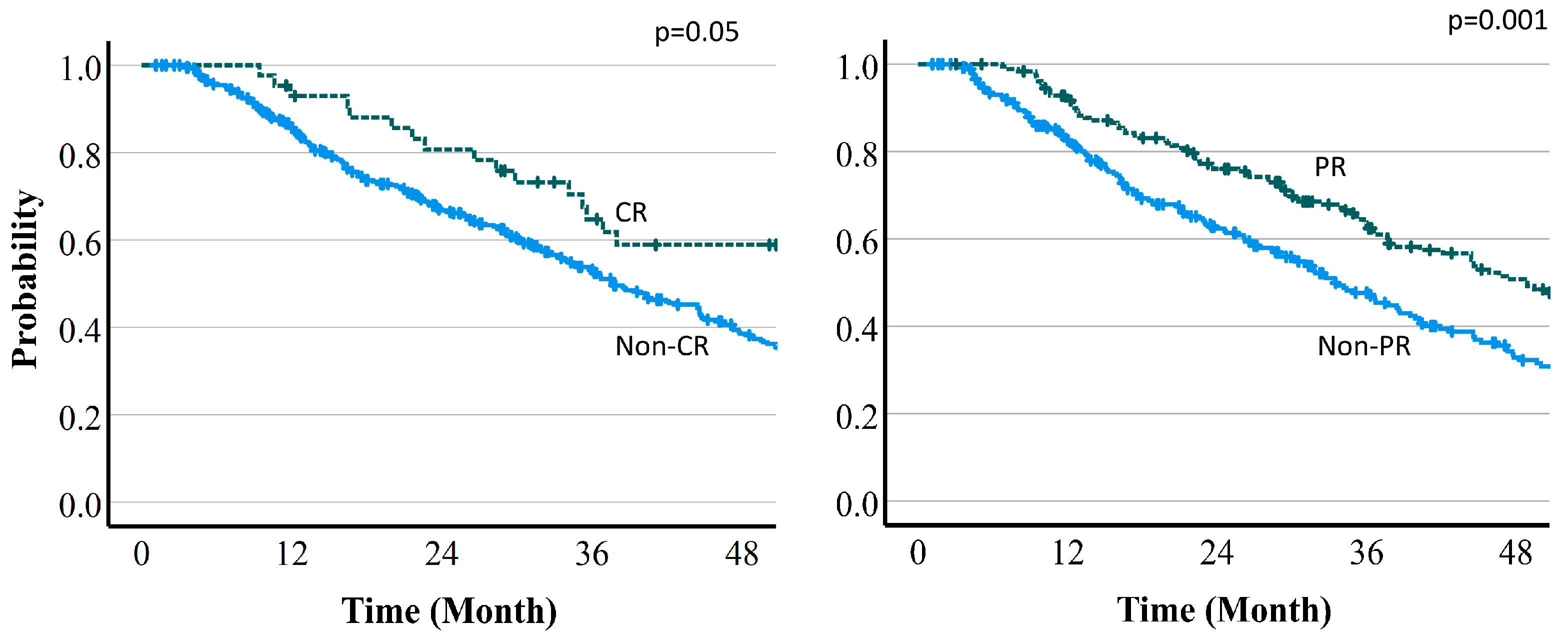
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Sanuki, N.; Takeda, A.; Oku, Y.; Mizuno, T.; Aoki, Y.; Eriguchi, T.; Iwabuchi, S.; Kunieda, E. Stereotactic body radiotherapy for small hepatocellular carcinoma: A retrospective outcome analysis in 185 patients. Acta Oncol. 2014, 53, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Sanuki, N.; Eriguchi, T.; Kobayashi, T.; Iwabutchi, S.; Matsunaga, K.; Mizuno, T.; Yashiro, K.; Nisimura, S.; Kunieda, E. Stereotactic ablative body radiotherapy for previously untreated solitary hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2014, 29, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Sanuki, N.; Tsurugai, Y.; Iwabuchi, S.; Matsunaga, K.; Ebinuma, H.; Imajo, K.; Aoki, Y.; Saito, H.; Kunieda, E. Phase 2 study of stereotactic body radiotherapy and optional transarterial chemoembolization for solitary hepatocellular carcinoma not amenable to resection and radiofrequency ablation. Cancer 2016, 122, 2041–2049. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Park, J.-W.; Kim, Y.-J.; Kim, B.H.; Woo, S.M.; Moon, S.H.; Kim, S.S.; Koh, Y.-H.; Lee, W.J.; Park, S.J.; et al. Phase I dose-escalation study of proton beam therapy for inoperable hepatocellular carcinoma. Cancer Res. Treat. 2015, 47, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, M.; Okumura, T.; Hashimoto, T.; Fukuda, K.; Oshiro, Y.; Fukumitsu, N.; Abei, M.; Kawaguchi, A.; Hayashi, Y.; Ookawa, A.; et al. Proton beam therapy for hepatocellular carcinoma: A comparison of three treatment protocols. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 1039–1045. [Google Scholar] [CrossRef]
- Kawashima, M.; Kohno, R.; Nakachi, K.; Nishio, T.; Mitsunaga, S.; Ikeda, M.; Konishi, M.; Takahashi, S.; Gotohda, N.; Arahira, S.; et al. Dose-volume histogram analysis of the safety of proton beam therapy for unresectable hepatocellular carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 1479–1486. [Google Scholar] [CrossRef]
- Mizumoto, M.; Fuji, H.; Miyachi, M.; Soejima, T.; Yamamoto, T.; Aibe, N.; Demizu, Y.; Iwata, H.; Hashimoto, T.; Motegi, A.; et al. Proton beam therapy for children and adolescents and young adults (AYAs): JASTRO and JSPHO Guidelines. Cancer Treat. Rev. 2021, 98, 102209. [Google Scholar] [CrossRef]
- Oshiro, Y.; Mizumoto, M.; Okumura, T.; Hashimoto, T.; Fukumitsu, N.; Ohkawa, A.; Kanemoto, A.; Hashii, H.; Ohno, T.; Sakae, T.; et al. Results of proton beam therapy without concurrent chemotherapy for patients with unresectable stage III non-small cell lung cancer. J. Thorac. Oncol. 2012, 7, 370–375. [Google Scholar] [CrossRef]
- The Japan Society of Hepatology. Clinical Practice Guidelines for Hepatocellular Carcinoma 2021 Version. Available online: https://www.jsh.or.jp/lib/files/english/examination_en/guidelines_hepatocellular_carcinoma_2021_03.pdf (accessed on 7 January 2024).
- Price, T.R.; Perkins, S.M.; Sandrasegaran, K.; Henderson, M.A.; Maluccio, M.A.; Zook, J.E.; Tector, A.J.; Vianna, R.M.; Johnstone, P.A.S.; Cardenes, H.R. Evaluation of response after stereotactic body radiotherapy for hepatocellular carcinoma. Cancer 2012, 118, 3191–3198. [Google Scholar] [CrossRef]
- Sanuki, N.; Takeda, A.; Mizuno, T.; Oku, Y.; Eriguchi, T.; Iwabuchi, S.; Kunieda, E. Tumor response on CT following hypofractionated stereotactic ablative body radiotherapy for small hypervascular hepatocellular carcinoma with cirrhosis. AJR Am. J. Roentgenol. 2013, 201, W812–W820. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Choi, D.; Lim, D.H.; Lee, W.J.; Yoo, B.C.; Paik, S.W. Change in contrast enhancement of HCC on 1-month follow-up CT after local radiotherapy: An early predictor of final treatment response. Eur. J. Radiol. 2009, 72, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Durand-Labrunie, J.; Baumann, A.S.; Ayav, A.; Laurent, V.; Boleslawski, E.; Cattan, S.; Bogart, E.; Le Deley, M.C.; Steen, V.; Lacornerie, T.; et al. Curative Irradiation Treatment of Hepatocellular Carcinoma: A Multicenter Phase 2 Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Takeda, A.; Sanuki, N.; Ariyoshi, K.; Yamaguchi, T.; Imagumbai, T.; Katoh, N.; Eriguchi, T.; Oku, Y.; Ozawa, S.; et al. Multicenter prospective study of stereotactic body radiotherapy for previously untreated solitary primary hepatocellular carcinoma: The STRSPH study. Hepatol. Res. 2021, 51, 461–471. [Google Scholar] [CrossRef]
- Hong, T.S.; Wo, J.Y.; Yeap, B.Y.; Ben-Josef, E.; McDonnell, E.I.; Blaszkowsky, L.S.; Kwak, E.L.; Allen, J.N.; Clark, J.W.; Goyal, L.; et al. Multi-Institutional Phase II Study of High-Dose Hypofractionated Proton Beam Therapy in Patients with Localized, Unresectable Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. J. Clin. Oncol. 2016, 34, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Sekino, Y.; Tateishi, R.; Fukumitsu, N.; Okumura, T.; Maruo, K.; Iizumi, T.; Numajiri, H.; Mizumoto, M.; Minami, T.; Nakagomi, R.; et al. Proton Beam Therapy versus Radiofrequency Ablation for Patients with Treatment-Naïve Single Hepatocellular Carcinoma: A Propensity Score Analysis. Liver Cancer 2022, 12, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, M.; Ogino, H.; Okumura, T.; Terashima, K.; Murakami, M.; Ogino, T.; Tamamura, H.; Akimoto, T.; Waki, T.; Katoh, N.; et al. Proton beam therapy for hepatocellular carcinoma: Multicenter prospective registry study in Japan. Int. J. Radiat. Oncol. Biol. Phys. 2023, in press. [Google Scholar] [CrossRef]
- Takayasu, K.; Arii, S.; Matsuo, N.; Yoshikawa, M.; Ryu, M.; Takasaki, K.; Sato, M.; Yamanaka, N.; Shimamura, Y.; Ohto, M. Comparison of CT findings with resected specimens after chemoembolization with iodized oil for hepatocellular carcinoma. AJR Am. J. Roentgenol. 2000, 175, 699–704. [Google Scholar] [CrossRef]
- Brook, O.R.; Thornton, E.; Mendiratta-Lala, M.; Mahadevan, A.; Raptopoulos, V.; Brook, A.; Najarian, R.; Sheiman, R.; Siewert, B. CT Imaging Findings after Stereotactic Radiotherapy for Liver Tumors. Gastroenterol. Res. Pract. 2015, 2015, 126245. [Google Scholar] [CrossRef]
- Kim, T.H.; Park, J.-W.; Kim, B.H.; Kim, D.Y.; Moon, S.H.; Kim, S.S.; Lee, J.H.; Woo, S.M.; Koh, Y.-H.; Lee, W.J.; et al. Optimal time of tumour response evaluation and effectiveness of hypofractionated proton beam therapy for inoperable or recurrent hepatocellular carcinoma. Oncotarget 2017, 9, 4034–4043. [Google Scholar] [CrossRef]
- Takahashi, H.; Sekino, Y.; Mori, K.; Okumura, T.; Nasu, K.; Fukuda, K.; Masuoka, S.; Iizumi, T.; Hasegawa, N.; Sakurai, H.; et al. Indicator for local recurrence of hepatocellular carcinoma after proton beam therapy: Analysis of attenuation difference between the irradiated tumor and liver parenchyma on contrast enhancement CT. Br. J. Radiol. 2020, 93, 20190375. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.Y.; Chen, C.M.; Huang, B.S.; Lai, Y.C.; Pan, K.T.; Lin, S.M.; Chu, S.Y.; Tseng, J.H. A preliminary study of hepatocellular carcinoma post proton beam therapy using MRI as an early prediction of treatment effectiveness. PLoS ONE 2021, 16, e0249003. [Google Scholar] [CrossRef] [PubMed]
- Sanuki, N.; Takeda, A.; Kunieda, E. Role of stereotactic body radiation therapy for hepatocellular carcinoma. World J. Gastroenterol. 2014, 20, 3100–3111. [Google Scholar] [CrossRef] [PubMed]
- Yoo, G.S.; Yu, J.I.; Park, H.C. Proton therapy for hepatocellular carcinoma: Current knowledges and future perspectives. World J. Gastroenterol. 2018, 24, 3090–3100. [Google Scholar] [CrossRef] [PubMed]
- Sanuki, N.; Takeda, A.; Oku, Y.; Eriguchi, T.; Nishimura, S.; Aoki, Y.; Kunieda, E. Influence of liver toxicities on prognosis after stereotactic body radiation therapy for hepatocellular carcinoma. Hepatol. Res. 2015, 45, 540–547. [Google Scholar] [CrossRef]
- Olsen, C.C.; Welsh, J.; Kavanagh, B.D.; Franklin, W.; McCarter, M.; Cardenes, H.R.; Gaspar, L.E.; Schefter, T.E. Microscopic and macroscopic tumor and parenchymal effects of liver stereotactic body radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 1414–1424. [Google Scholar] [CrossRef] [PubMed]
- Haddad, M.M.; Merrell, K.W.; Hallemeier, C.L.; Johnson, G.B.; Mounajjed, T.; Olivier, K.R.; Fidler, J.L.; Venkatesh, S.K. Stereotactic body radiation therapy of liver tumors: Post-treatment appearances and evaluation of treatment response: A pictorial review. Abdom. Radiol. 2016, 41, 2061–2077. [Google Scholar] [CrossRef] [PubMed]
- Schmid-Tannwald, C.; Strobl, F.F.; Theisen, D.; Muacevic, A.; Stintzing, S.; Reiser, M.F.; Trumm, C.G. Diffusion-weighted MRI Before and After Robotic Radiosurgery (Cyberknife®) in Primary and Secondary Liver Malignancies: A Pilot Study. Technol. Cancer Res. Treat. 2015, 14, 191–199. [Google Scholar] [CrossRef]
- Mendiratta-Lala, M.; Gu, E.; Owen, D.; Cuneo, K.C.; Bazzi, L.; Lawrence, T.S.; Hussain, H.K.; Davenport, M.S. Imaging Findings within the First 12 Months of Hepatocellular Carcinoma Treated with Stereotactic Body Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 1063–1069. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.; Galle, P.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network: NCCN Clinical Practice Guidelines in Oncology: Hepatocellular Carcinoma Version2. 2023. Available online: https://www.nccn.org/professionals/physician_gls/pdf/hcc.pdf (accessed on 7 January 2024).
- Proton Beam Therapy Model Policy. 2017. Available online: https://www.astro.org/uploadedFiles/_MAIN_SITE/Daily_Practice/Reimbursement/Model_Policies/Content_Pieces/ASTROPBTModelPolicy.pdf (accessed on 7 January 2024).
- Apisarnthanarax, S.; Barry, A.; Cao, M.; Czito, B.; DeMatteo, R.; Drinane, M.; Hallemeier, C.; Koay, E.; Lasley, F.; Meyer, J.; et al. External Beam Radiation Therapy for Primary Liver Cancers: An ASTRO Clinical Practice Guideline. Pract. Radiat. Oncol. 2022, 12, 28–51. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Lim, Y.K.; Kim, T.H.; Cho, K.H.; Choi, S.H.; Jeong, H.; Kim, D.W.; Park, J.H.; Shin, D.H.; Lee, S.B.; et al. Normal liver sparing by proton beam therapy for hepatocellular carcinoma: Comparison with helical intensity modulated radiotherapy and volumetric modulated arc therapy. Acta Oncol. 2015, 54, 1827–1832. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Wu, P.; Kao, W.; Lai, Y.; Hsu, J.; Chiou, J.; Wu, M.; Lee, H. Comparison of local ablative therapies, including radiofrequency ablation, microwave ablation, stereotactic ablative radiotherapy, and particle radiotherapy, for inoperable hepatocellular carcinoma: A systematic review and meta-analysis. Exp. Hematol. Oncol. 2023, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Nosaka, T.; Matsuda, H.; Sugata, R.; Akazawa, Y.; Takahashi, K.; Naito, T.; Ohtani, M.; Kinoshita, K.; Tsujikawa, T.; Sato, Y.; et al. Longer Survival and Preserved Liver Function after Proton Beam Therapy for Patients with Unresectable Hepatocellular. Curr. Oncol. 2023, 30, 3915–3926. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.-Y.; Liu, C.-M.; Wang, Y.-M.; Hsu, H.-C.; Huang, E.-Y.; Huang, T.-T.; Lee, C.-H.; Hung, S.-P.; Huang, B.-S. Proton versus photon radiotherapy for primary hepatocellular carcinoma: A propensity-matched analysis. Radiat. Oncol. 2020, 15, 159. [Google Scholar] [CrossRef] [PubMed]
- Tamura, S.; Okamura, Y.; Sugiura, T.; Ito, T.; Yamamoto, Y.; Ashida, R.; Ohgi, K.; Murayama, S.; Uesaka, K. A comparison of the outcomes between surgical resection and proton beam therapy for single primary hepatocellular carcinoma. Surg. Today 2020, 50, 369–378. [Google Scholar] [CrossRef]
- Iwata, H.; Ogino, H.; Hattori, Y.; Nakajima, K.; Nomura, K.; Hashimoto, S.; Hayashi, K.; Toshito, T.; Sasaki, S.; Mizoe, J.; et al. A Phase 2 Study of Image-Guided Proton Therapy for Operable or Ablation-Treatable Primary Hepatocellular Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 117–126. [Google Scholar] [CrossRef]
- Bush, D.; Volk, M.; Smith, J.; Reeves, M.; Sanghvi, S.; Slater, J.; deVere, M. Proton beam radiotherapy versus transarterial chemoembolization for hepatocellular carcinoma: Results of a randomized clinical trial. Cancer 2023, 129, 3554–3563. [Google Scholar] [CrossRef]
- Kim, T.H.; Koh, Y.H.; Kim, B.H.; Kim, M.J.; Lee, J.H.; Park, B.; Park, J.-W. Proton beam radiotherapy vs. radiofrequency ablation for recurrent hepatocellular carcinoma: A randomized phase III trial. J. Hepatol. 2021, 74, 603–612. [Google Scholar] [CrossRef]




| Characteristics | Number | % |
|---|---|---|
| Age (years) | 21–91 | 72 (median) |
| Gender | ||
| Male | 339 | 75.2 |
| Female | 112 | 24.8 |
| ECOG performance status | ||
| 0 | 244 | 54.1 |
| 1 | 182 | 40.3 |
| 2 | 24 | 5.3 |
| 3 | 3 | 0.7 |
| History of hepatitis | ||
| Non-B, non-C | 204 | 45.2 |
| HCV | 177 | 39.2 |
| HBV | 70 | 15.5 |
| Child–Pugh class | ||
| A | 321 | 71.2 |
| B | 123 | 27.3 |
| C | 7 | 1.5 |
| Tumor location | ||
| Peripheral | 66 | 14.6 |
| Hepatic portal | 301 | 66.7 |
| Gastrointestinal proximity | 84 | 18.6 |
| Tumor size (mm) | 8–160 | 39 (median) |
| <30 | 162 | 35.9 |
| 30–49 | 149 | 33.0 |
| 50–99 | 117 | 25.9 |
| ≥100 | 23 | 5.1 |
| Portal vein tumor thrombus | ||
| Vp 0–2 | 400 | 88.7 |
| Vp 3–4 | 51 | 11.3 |
| Surgical indication | ||
| Operable | 68 | 15.0 |
| Inoperable | 383 | 84.9 |
| Prior treatment | ||
| Yes | 205 | 45.5 |
| No | 246 | 54.5 |
| Prior radiotherapy | ||
| Yes | 15 | 3.3 |
| No | 436 | 96.7 |
| Clinical stage | ||
| I | 173 | 38.4 |
| II | 126 | 27.9 |
| III | 87 | 19.3 |
| IV | 65 | 14.4 |
| Factors | HR | p Value |
|---|---|---|
| 50% Reduction | ||
| Sex | 0.94 (0.68–1.30) | 0.69 |
| Age | 1.00 (0.99–1.01) | 0.96 |
| Protocol A (control C) | 1.10 (0.71–1.71) | 0.67 |
| Protocol B (control C) | 0.79 (0.54–1.14) | 0.21 |
| Tumor size | 0.89 (0.84–0.96) | <0.01 |
| 100% Reduction | ||
| Sex | 0.81 (0.53–1.24) | 0.336 |
| Age | 1.00 (0.98–1.02) | 0.750 |
| Protocol A (control: C) | 1.66 (0.89–3.09) | 0.113 |
| Protocol B (control: C) | 1.34 (0.75–2.39) | 0.328 |
| Tumor size | 0.54 (0.46–0.63) | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niitsu, H.; Mizumoto, M.; Li, Y.; Nakamura, M.; Ishida, T.; Iizumi, T.; Saito, T.; Numajiri, H.; Makishima, H.; Nakai, K.; et al. Tumor Response on Diagnostic Imaging after Proton Beam Therapy for Hepatocellular Carcinoma. Cancers 2024, 16, 357. https://doi.org/10.3390/cancers16020357
Niitsu H, Mizumoto M, Li Y, Nakamura M, Ishida T, Iizumi T, Saito T, Numajiri H, Makishima H, Nakai K, et al. Tumor Response on Diagnostic Imaging after Proton Beam Therapy for Hepatocellular Carcinoma. Cancers. 2024; 16(2):357. https://doi.org/10.3390/cancers16020357
Chicago/Turabian StyleNiitsu, Hikaru, Masashi Mizumoto, Yinuo Li, Masatoshi Nakamura, Toshiki Ishida, Takashi Iizumi, Takashi Saito, Haruko Numajiri, Hirokazu Makishima, Kei Nakai, and et al. 2024. "Tumor Response on Diagnostic Imaging after Proton Beam Therapy for Hepatocellular Carcinoma" Cancers 16, no. 2: 357. https://doi.org/10.3390/cancers16020357
APA StyleNiitsu, H., Mizumoto, M., Li, Y., Nakamura, M., Ishida, T., Iizumi, T., Saito, T., Numajiri, H., Makishima, H., Nakai, K., Oshiro, Y., Maruo, K., & Sakurai, H. (2024). Tumor Response on Diagnostic Imaging after Proton Beam Therapy for Hepatocellular Carcinoma. Cancers, 16(2), 357. https://doi.org/10.3390/cancers16020357






