A Comprehensive Analysis of Skin Cancer Concerns and Protective Practices in Manitoba, Canada, Highlights Lack of Skin Cancer Awareness and Predominance of High-Risk Sun Exposure Behaviors
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethics Statement
2.3. Development and Pre-Testing
2.4. Recruitment Process and Survey Administration
2.5. Analysis
3. Results
3.1. Participants and Descriptive Data
3.2. Overall Sun Habits, Skin Cancer Risk Factors, and Level of Worry
3.3. Participants’ Knowledge and Reactions
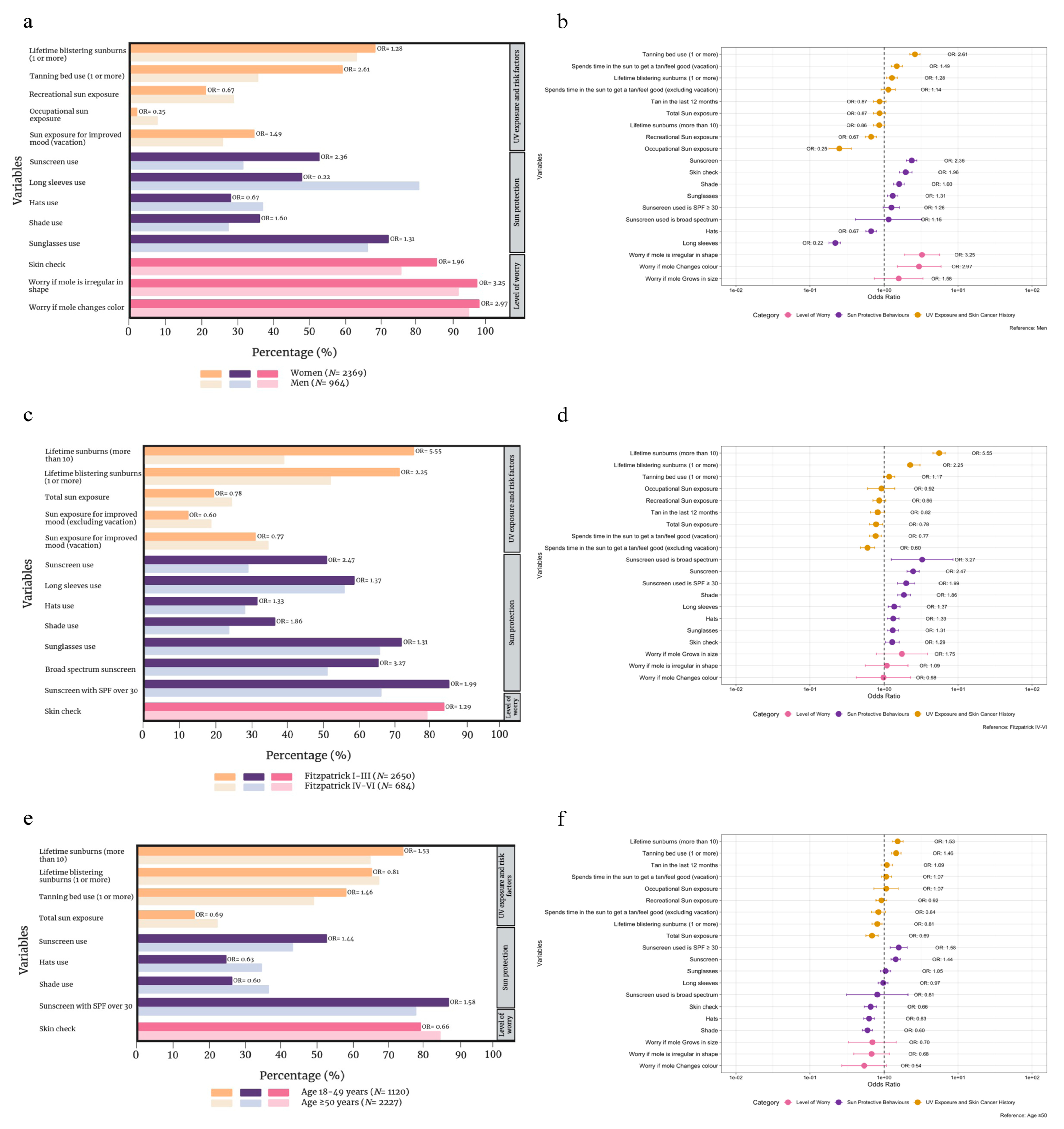
3.4. Women vs. Men Participants
3.5. Fitzpatrick Skin Phototypes I–III vs. IV–VI
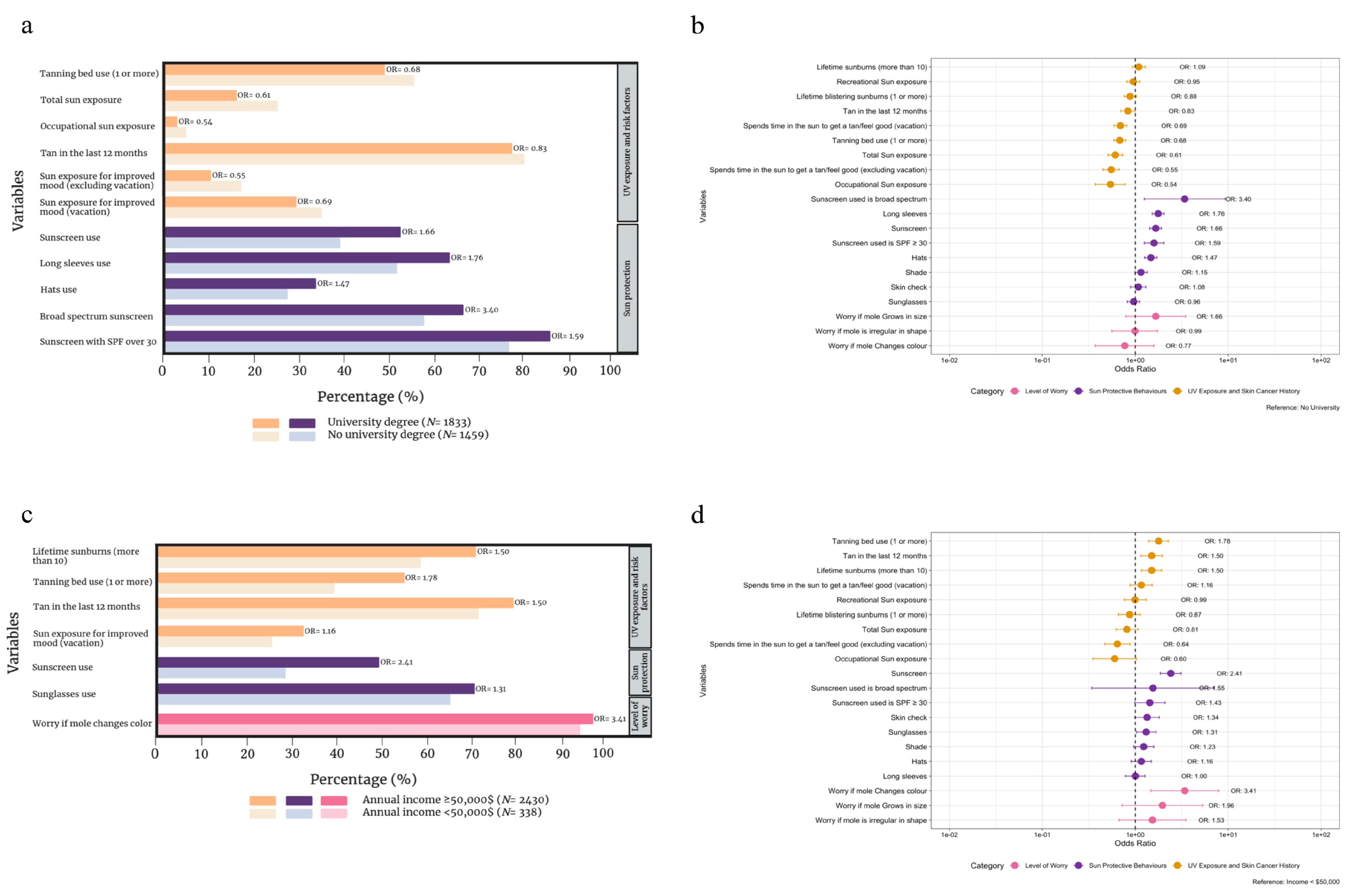
3.6. Participants with vs. without a University Education
3.7. Annual Income ≥ CAD 50,000 vs. <CAD 50,000
3.8. Age-Based Comparison
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Conte, S.; Ghazawi, F.M.; Le, M.; Nedjar, H.; Alakel, A.; Lagacé, F.; Mukovozov, I.M.; Cyr, J.; Mourad, A.; Miller Jr, W.H.; et al. Population-Based Study Detailing Cutaneous Melanoma Incidence and Mortality Trends in Canada. Front. Med. 2022, 9, 830254. [Google Scholar] [CrossRef] [PubMed]
- Berman-Rosa, M.; Logan, J.; Ghazawi, F.M.; Le, M.; Conte, S.; Netchiporouk, E.; Mukovozov, I.M.; Cyr, J.; Mourad, A.; Miller, W.H.; et al. Analysis of Geographic and Environmental Factors and Their Association with Cutaneous Melanoma Incidence in Canada. Dermatology 2022, 238, 1006–1017. [Google Scholar] [CrossRef]
- Ghazawi, F.M.; Le, M.; Alghazawi, N.; Rahme, E.; Moreau, L.; Netchiporouk, E.; Zubarev, A.; Roshdy, O.; Glassman, S.J.; Sasseville, D.; et al. Trends in incidence of cutaneous malignant melanoma in Canada: 1992–2010 versus 2011–2015. J. Am. Acad. Dermatol. 2019, 80, 1157–1159. [Google Scholar] [CrossRef]
- Ghazawi, F.M.; Cyr, J.; Darwich, R.; Le, M.; Rahme, E.; Moreau, L.; Netchiporouk, E.; Zubarev, A.; Roshdy, O.; Glassman, S.J.; et al. Cutaneous malignant melanoma incidence and mortality trends in Canada: A comprehensive population-based study. J. Am. Acad. Dermatol. 2019, 80, 448–459. [Google Scholar] [CrossRef]
- Moustaqim-Barrette, A.; Conte, S.; Kelly, A.; Lebeau, J.; Alli, S.; Lagacé, F.; Litvinov, I.V. Evaluation of weather and environmental factors and their association with cutaneous melanoma incidence: A national ecological study. JAAD Int. 2024, 16, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Ghazawi, F.M.; Le, M.; Lagacé, F.; Cyr, J.; Alghazawi, N.; Zubarev, A.; Roy, S.F.; Rahme, E.; Netchiporouk, E.; Roshdy, O.; et al. Incidence, Mortality, and Spatiotemporal Distribution of Cutaneous Malignant Melanoma Cases Across Canada. J. Cutan. Med. Surg. 2019, 23, 394–412. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.F.; Beca, J.M.; Croxford, R.; Isaranawatchai, W.; Menjak, I.B.; Petrella, T.M.; Mittmann, N.; Earle, C.C.; Gavura, S.; Hanna, T.P.; et al. Real-world comparative effectiveness of second-line ipilimumab for metastatic melanoma: A population-based cohort study in Ontario, Canada. BMC Cancer 2020, 20, 304. [Google Scholar] [CrossRef]
- Kahlon, N.; Doddi, S.; Yousif, R.; Najib, S.; Sheikh, T.; Abuhelwa, Z.; Burmeister, C.; Hamouda, D.M. Melanoma Treatments and Mortality Rate Trends in the US, 1975 to 2019. JAMA Netw. Open 2022, 5, e2245269. [Google Scholar] [CrossRef]
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Barsouk, A. Epidemiology of Melanoma. Med. Sci. 2021, 9, 63. [Google Scholar] [CrossRef]
- Didier, A.J.; Nandwani, S.V.; Watkins, D.; Fahoury, A.M.; Campbell, A.; Craig, D.J.; Vijendra, D.; Parquet, N. Patterns and trends in melanoma mortality in the United States, 1999–2020. BMC Cancer 2024, 24, 790. [Google Scholar] [CrossRef]
- Conte, S.; Aldien, A.S.; Jetté, S.; LeBeau, J.; Alli, S.; Netchiporouk, E.; Lagacé, F.; Lefrançois, P.; Iannattone, L.; Litvinov, I.V. Skin Cancer Prevention across the G7, Australia and New Zealand: A Review of Legislation and Guidelines. Curr. Oncol. 2023, 30, 6019–6040. [Google Scholar] [CrossRef] [PubMed]
- Lagacé, F.; Noorah, B.N.; Conte, S.; Mija, L.A.; Chang, J.; Cattelan, L.; LeBeau, J.; Claveau, J.; Turchin, I.; Gulliver, W.; et al. Assessing Skin Cancer Risk Factors, Sun Safety Behaviors and Melanoma Concern in Atlantic Canada: A Comprehensive Survey Study. Cancers 2023, 15, 3753. [Google Scholar] [CrossRef] [PubMed]
- Aitken, J.F.; Youlden, D.R.; Baade, P.D.; Soyer, H.P.; Green, A.C.; Smithers, B.M. Generational shift in melanoma incidence and mortality in Queensland, Australia, 1995–2014. Int. J. Cancer 2018, 142, 1528–1535. [Google Scholar] [CrossRef] [PubMed]
- Iannacone, M.R.; Youlden, D.R.; Baade, P.D.; Aitken, J.F.; Green, A.C. Melanoma incidence trends and survival in adolescents and young adults in Queensland, Australia. Int. J. Cancer 2015, 136, 603–609. [Google Scholar] [CrossRef]
- Walker, H.; Maitland, C.; Tabbakh, T.; Preston, P.; Wakefield, M.; Sinclair, C. Forty years of Slip! Slop! Slap! A call to action on skin cancer prevention for Australia. Public Health Res. Pract. 2022, 32, e31452117. [Google Scholar] [CrossRef]
- Conte, S.; Le, M.; Moustaqim-Barrette, A.; Ghazawi, F.M.; Muntyanu, A.; Lagacé, F.; Alakel, A.; Rahme, E.; Glassman, S.J.; Litvinov, I.V. Cutaneous Melanoma Mortality-to-Incidence Ratio and Its Association with Socioeconomic and Healthcare Factors in Canada: A National Ecological Study. J. Cutan. Med. Surg. 2024, 12034754241265694. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, R.P.; Elwood, J.M.; Threlfall, W.J.; Spinelli, J.J.; Fincham, S.; Hill, G.B. Socioeconomic status, sunlight exposure, and risk of malignant melanoma: The Western Canada Melanoma Study. J. Natl. Cancer Inst. 1987, 79, 647–652. [Google Scholar]
- Lee, T.K.; MacArthur, A.C.; Gallagher, R.P.; Elwood, M.J. Occupational physical activity and risk of malignant melanoma: The Western Canada Melanoma Study. Melanoma Res. 2009, 19, 260–266. [Google Scholar] [CrossRef]
- Gallagher, R.P.; Elwood, J.M.; Yang, C.P. Is chronic sunlight exposure important in accounting for increases in melanoma incidence? Int. J. Cancer 1989, 44, 813–815. [Google Scholar] [CrossRef]
- Harland, E.; Griffith, J.; Lu, H.; Erickson, T.; Magsino, K. Health behaviours associated with indoor tanning based on the 2012/13 Manitoba Youth Health Survey. Health Promot. Chronic Dis. Prev. Canada 2016, 36, 149–162. [Google Scholar] [CrossRef][Green Version]
- Héry, C.; Tryggvadóttir, L.; Sigurdsson, T.; Ólafsdóttir, E.; Sigurgeirsson, B.; Jonasson, J.G.; Olafsson, J.H.; Boniol, M.; Byrnes, G.B.; Doré, J.-F.; et al. A melanoma epidemic in Iceland: Possible influence of sunbed use. Am. J. Epidemiol. 2010, 172, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Kvaskoff, M.; Thuret, A.; Guénel, P.; Bray, F.; Soerjomataram, I. Cutaneous melanoma in France in 2015 attributable to solar ultraviolet radiation and the use of sunbeds. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1681–1686. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.K.; Rigel, D.S.; Amonette, R.A. Trends in sun exposure knowledge, attitudes, and behaviors: 1986 to 1996. J. Am. Acad. Dermatol. 1997, 37 Pt 1, 179–186. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Jennings, L.; Karia, P.S.; Jambusaria-Pahlajani, A.; Whalen, F.M.; Schmults, C.D. The Sun Exposure and Behaviour Inventory (SEBI): Validation of an instrument to assess sun exposure and sun protective practices. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 706–715. [Google Scholar] [CrossRef]
- Background: Maelstron Research. Available online: https://www.maelstrom-research.org/page/background (accessed on 1 July 2023).
- Manitoba, C. The Manitoba Tomorrow Project. 2024. Available online: https://www.cancercare.mb.ca/Research/research-institute-at-cancercare-manitoba/research-programs/manitoba-tomorrow-project (accessed on 1 July 2024).
- Taylor, S.C.; Cook-Bolden, F. Defining skin of color. Cutis 2002, 69, 435–437. [Google Scholar]
- Dennis, L.K.; Lowe, J.B.; Snetselaar, L.G. Tanning behavior among young frequent tanners is related to attitudes and not lack of knowledge about the dangers. Health Educ. J. 2009, 68, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, J.L.; Manne, S.L.; Greene, K.; Darabos, K.; Carpenter, A.; Hudson, S.V.; Coups, E.J. Sociocultural experiences, body image, and indoor tanning among young adult women. J. Health Psychol. 2017, 22, 1582–1590. [Google Scholar] [CrossRef]
- Ashinoff, R.; Levine, V.J.; Steuer, A.B.; Sedwick, C. Teens and tanning knowledge and attitudes. J. Clin. Aesthet. Dermatol. 2009, 2, 48–50. [Google Scholar]
- Martin, J.M.; Ghaferi, J.M.; Cummins, D.L.; Mamelak, A.J.; Schmults, C.D.; Parikh, M.; Speyer, L.-A.; Chuang, A.; Richardson, H.V.; Stein, D.; et al. Changes in skin tanning attitudes. Fashion articles and advertisements in the early 20th century. Am. J. Public Health 2009, 99, 2140–2146. [Google Scholar] [CrossRef]
- Glanz, K.; Jordan, A.; Lazovich, D.; Bleakley, A. Frequent Indoor Tanners’ Beliefs About Indoor Tanning and Cessation. Am. J. Health Promot. 2019, 33, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Mahler, H.; Beckerley, S.; Vogel, M. Effects of Media Images on Attitudes Toward Tanning. Basic Appl. Soc. Psychol. 2010, 32, 118–127. [Google Scholar] [CrossRef]
- Heneghan, M.K.; Hazan, C.; Halpern, A.C.; Oliveria, S.A. Skin cancer coverage in a national newspaper: A teachable moment. J. Cancer Educ. 2007, 22, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Focus, M. Concerns That Cost of Sunscreen Is Increasing Skin Cancer Risk. 2023. Available online: https://melanomafocus.org/news-blog/concerns-that-cost-of-sunscreen-is-increasing-skin-cancer-risk/ (accessed on 1 July 2024).
- Diehl, K.; Schneider, S.; Seuffert, S.; Greinert, R.; Görig, T. Who Are the Nonusers of Sunscreen, and What Are Their Reasons? Development of a New Item Set. J. Cancer Educ. 2021, 36, 1045–1053. [Google Scholar] [CrossRef]
- ARPANSA. An Australian Study Finds That Sunscreen Is the Best Method to Reduce the Impact of Skin Cancer. 2020. Available online: https://www.arpansa.gov.au/australian-study-finds-sunscreen-best-method-reduce-impact-skin-cancer (accessed on 1 July 2024).
- Hirst, N.G.; Gordon, L.G.; Scuffham, P.A.; Green, A.C. Lifetime cost-effectiveness of skin cancer prevention through promotion of daily sunscreen use. Value Health 2012, 15, 261–268. [Google Scholar] [CrossRef]
- Falk, M.; Anderson, C.D. Influence of age, gender, educational level and self-estimation of skin type on sun exposure habits and readiness to increase sun protection. Cancer Epidemiol. 2013, 37, 127–132. [Google Scholar] [CrossRef]
- Mueller, A.M.; Goessinger, E.V.; Cerminara, S.E.; Kostner, L.; Amaral, M.; Huber, S.M.; Passweg, L.P.; Moreno, L.G.; Bodenmann, D.; Kunz, M.; et al. Educational level-dependent melanoma awareness in a high-risk population in Switzerland. Front. Oncol. 2023, 13, 1174542. [Google Scholar] [CrossRef]
- Alli, S.; LeBeau, J.; Hasbani, A.; Lagacé, F.; Litvinov, I.V.; Peláez, S. Understanding the Perceived Relationship between Sun Exposure and Melanoma in Atlantic Canada: A Consensual Qualitative Study Highlighting a “Sunscreen Paradox”. Cancers 2023, 15, 4726. [Google Scholar] [CrossRef]
- Autier, P. Sunscreen abuse for intentional sun exposure. Br. J. Dermatol. 2009, 161 (Suppl. 3), 40–45. [Google Scholar] [CrossRef]
- Sander, M.; Sander, M.; Burbidge, T.; Beecker, J. The efficacy and safety of sunscreen use for the prevention of skin cancer. Cmaj 2020, 192, E1802–E1808. [Google Scholar] [CrossRef]
- Heerfordt, I.M.; Torsnes, L.R.; Philipsen, P.A.; Wulf, H.C. Sunscreen use optimized by two consecutive applications. PLoS ONE 2018, 13, e0193916. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Colantonio, S.; Dawson, A.; Lin, X.; Beecker, J. Sunscreen Application, Safety, and Sun Protection: The Evidence. J. Cutan. Med. Surg. 2019, 23, 357–369. [Google Scholar] [CrossRef]
- Hafez, S.Y.; Alraddadi, E.A.; Ramadan, M.; Alsalamah, F.; Alghumuy, R.; Aljuhani, F.F. Assessment of prevalence of sunscreen use and related practices among people living in Saudi Arabia: A cross-sectional survey-based study. J. Cosmet. Dermatol. 2024, 23, 1718–1725. [Google Scholar] [CrossRef]
- Diffey, B.L.; Fajuyigbe, D.; Wright, C.Y. Sunburn and sun protection in black skin. Int. J. Dermatol. 2019, 58, 1053–1055. [Google Scholar] [CrossRef]
- Hall, H.I.; Rogers, J.D. Sun protection behaviors among African Americans. Ethn. Dis. 1999, 9, 126–131. [Google Scholar] [PubMed]
- Tsai, J.; Chien, A.L. Photoprotection for Skin of Color. Am. J. Clin. Dermatol. 2022, 23, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Rijal, H.; Moustaqim-Barrette, A.; Maazi, M.; Kelly, A.; Litvinov, I.V. Differences in Photoprotective Behaviours Based on Immigration Status: A Systematic Review. J. Cutan. Med. Surg. 2024, 12034754241274368. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Bharadwaj, M.; Mehrotra, R. Skin Cancer Concerns in People of Color: Risk Factors and Prevention. Asian Pac. J. Cancer Prev. 2016, 17, 5257–5264. [Google Scholar] [PubMed]
- Jacobsen, A.A.; Galvan, A.; Lachapelle, C.C.; Wohl, C.B.; Kirsner, R.S.; Strasswimmer, J. Defining the Need for Skin Cancer Prevention Education in Uninsured, Minority, and Immigrant Communities. JAMA Dermatol. 2016, 152, 1342–1347. [Google Scholar] [CrossRef]
- Fajuyigbe, D.; Verschoore, M. Sun Exposure and Black Skin. Curr. Probl. Dermatol. 2021, 55, 62–71. [Google Scholar]
- Moradi Tuchayi, S.; Wang, Z.; Yan, J.; Garibyan, L.; Bai, X.; Gilchrest, B.A. Sunscreens: Misconceptions and Misinformation. J. Investig. Dermatol. 2023, 143, 1406–1411. [Google Scholar] [CrossRef] [PubMed]
- Kong, B.Y.; Sheu, S.L.; Kundu, R.V. Assessment of Consumer Knowledge of New Sunscreen Labels. JAMA Dermatol. 2015, 151, 1028–1030. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.A.; Monreal, A.J.; Diaz, E.L.; Castro, G.; de la Vega, P.R.; Varella, M. Marital Status and Survival in Patients Diagnosed with Melanoma. Dermatol. Res. Pract. 2020, 2020, 2485401. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%) |
|---|---|
| Mean age (SD) | 55.7 (12.4) |
| Median age (range) | 58 (18–84) |
| Gender | |
| Men | 964 (28.8) |
| Women | 2369 (70.8) |
| Other | 14 (0.4) |
| LGBTQ2S+ | 139 (4.2) |
| Ethnicity | |
| Non-Hispanic White or Euro-Canadian | 3034 (90.6) |
| Other | 313 (9.4) |
| Annual income (CAD) | |
| <20,000 | 35 (1.0) |
| 20,000–49,999 | 303 (9.1) |
| 50,000–69,999 | 409 (12.2) |
| 70,000–89,999 | 489 (14.6) |
| ≥90,000 | 1532 (45.8) |
| Highest level of education completed | |
| No high school | 31 (0.9) |
| High school | 538 (16.1) |
| Junior college or associate degree | 890 (26.6) |
| University bachelor’s degree | 1181 (35.3) |
| Graduate or doctoral studies | 652 (19.5) |
| Fitzpatrick | |
| Type I | 225 (6.7) |
| Type II | 1010 (30.2) |
| Type III | 1415 (42.3) |
| Type IV | 573 (17.1) |
| Type V | 106 (3.2) |
| Type VI | 5 (0.1) |
| Personal history of skin cancer | 285 (8.5) |
| Melanoma | 68 (23.9) |
| Squamous cell carcinoma (SCC) | 36 (12.6) |
| Basal cell carcinoma (BCC) | 153 (53.7) |
| Family history of skin cancer | 943 (28.2) |
| Lifetime sunburns (more than 10) | 2267 (67.7) |
| Lifetime blistering sunburns (1 or more) | 2250 (67.2) |
| Tanning bed use (1 or more) | 1741 (52.0) |
| Sun exposure (‘high’ or ‘very high’) | |
| Total | 682 (20.4) |
| Recreational | 788 (23.6) |
| Occupational | 128 (3.8) |
| Tan in the last 12 months | 2641 (78.9) |
| Spends time in the sun daily or multiple days per week to get a tan or to feel good (excluding vacation) | 453 (13.5) |
| Spends time in the sun daily or multiple days per week to get a tan or to feel good (vacation) | 1061 (31.8) |
| Sun protection (‘often’ or ‘always’) | |
| Sunscreen | 1555 (46.5) |
| Long sleeves | 1932 (57.7) |
| Hats | 1038 (31.0) |
| Shade | 1131 (33.8) |
| Sunglasses | 2361 (70.5) |
| Sunscreen | |
| Broad spectrum | 2084 (62.3) |
| SPF ≥ 30 | 2714 (81.1) |
| Skin check | 2775 (82.9) |
| Reaction to a new mole | |
| Family doctor visit | 1278 (38.2) |
| Check by friend/family member | 1472 (44.0) |
| Ignore | 186 (5.6) |
| Search the internet | 305 (9.1) |
| Worry if mole | |
| Is irregular in shape | 3206 (95.8) |
| Changes color | 3246 (97.0) |
| Grows in size | 3270 (97.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lagacé, F.; Conte, S.; Mija, L.A.; Moustaqim-Barrette, A.; Mahmood, F.; LeBeau, J.; McKenna, A.; Maazi, M.; Hanna, J.; Kelly, A.S.V.; et al. A Comprehensive Analysis of Skin Cancer Concerns and Protective Practices in Manitoba, Canada, Highlights Lack of Skin Cancer Awareness and Predominance of High-Risk Sun Exposure Behaviors. Cancers 2024, 16, 3093. https://doi.org/10.3390/cancers16173093
Lagacé F, Conte S, Mija LA, Moustaqim-Barrette A, Mahmood F, LeBeau J, McKenna A, Maazi M, Hanna J, Kelly ASV, et al. A Comprehensive Analysis of Skin Cancer Concerns and Protective Practices in Manitoba, Canada, Highlights Lack of Skin Cancer Awareness and Predominance of High-Risk Sun Exposure Behaviors. Cancers. 2024; 16(17):3093. https://doi.org/10.3390/cancers16173093
Chicago/Turabian StyleLagacé, François, Santina Conte, Lorena A. Mija, Amina Moustaqim-Barrette, Farhan Mahmood, Jonathan LeBeau, Alyson McKenna, Mahan Maazi, Johnny Hanna, Alexandra Sarah Victoria Kelly, and et al. 2024. "A Comprehensive Analysis of Skin Cancer Concerns and Protective Practices in Manitoba, Canada, Highlights Lack of Skin Cancer Awareness and Predominance of High-Risk Sun Exposure Behaviors" Cancers 16, no. 17: 3093. https://doi.org/10.3390/cancers16173093
APA StyleLagacé, F., Conte, S., Mija, L. A., Moustaqim-Barrette, A., Mahmood, F., LeBeau, J., McKenna, A., Maazi, M., Hanna, J., Kelly, A. S. V., Rahme, E., Hrubeniuk, T. J., Peláez, S., & Litvinov, I. V. (2024). A Comprehensive Analysis of Skin Cancer Concerns and Protective Practices in Manitoba, Canada, Highlights Lack of Skin Cancer Awareness and Predominance of High-Risk Sun Exposure Behaviors. Cancers, 16(17), 3093. https://doi.org/10.3390/cancers16173093









