Predicting Postoperative Length of Stay in Patients Undergoing Laparoscopic Right Hemicolectomy for Colon Cancer: A Machine Learning Approach Using SICE (Società Italiana di Chirurgia Endoscopica) CoDIG Data
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
- The CoDIG 1 [3] data were obtained from a large, multicenter, Italian study aimed at evaluating the surgical outcomes associated with two different techniques of ileocolic anastomosis (intracorporeal [ICA] and extracorporeal [ECA]) during laparoscopic right hemicolectomy. This prospective cohort study, endorsed by the Italian Society of Endoscopic Surgery and New Technologies (SICE), involved 85 surgical units across Italy, which contributed data on 1225 patients who underwent elective laparoscopic or robotic right hemicolectomy between March 2018 and September 2018.
- CoDIG 2 [2] data were used to externally validate the MLTs. The CoDIG 2 study is an observational multicenter national study involving 76 Italian surgical wards specializing in colorectal surgery aimed at assessing the practices of Italian surgeons regarding the extent of lymphadenectomy performed during right hemicolectomy (RH) for colon cancer. We sought to understand the current surgical approaches and any evolving trends compared with the previous CoDIG 1 study.
2.2. Descriptive Statistics
2.3. Machine Learning
2.3.1. Patient Variables
2.3.2. Machine Learning Model Training and Validation
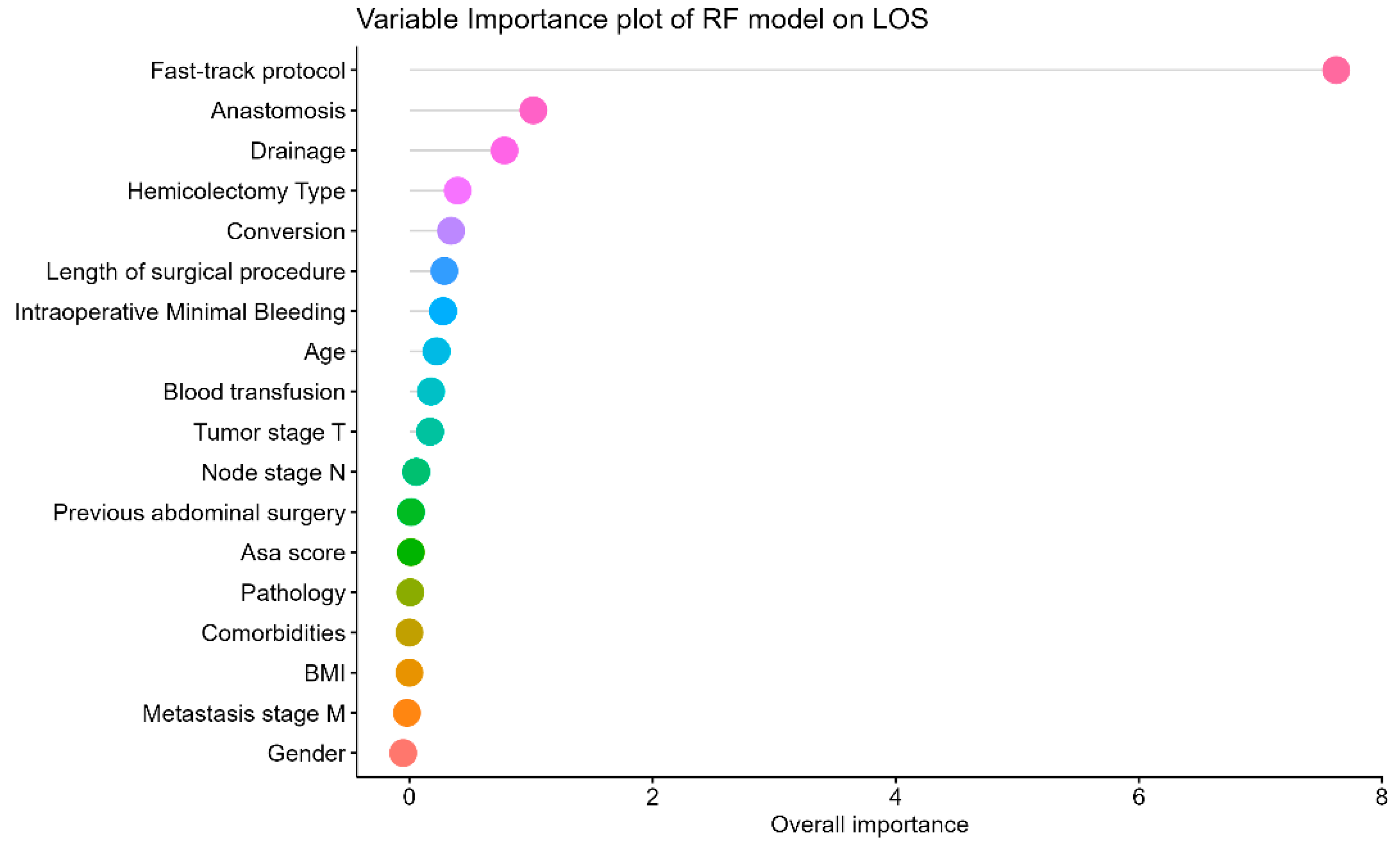
2.3.3. Variable Importance
2.3.4. Shiny Application Development
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CME | Complete mesocolic excision |
| CVL | Central vascular ligation |
| LoS | Length of stay |
| MLT | Machine learning techniques |
| RF | Random forest |
| RMSE | Root-mean-square error |
| SVM | Support vector machine |
| CME | Complete mesocolic excision |
| CVL | Central vascular ligation |
| SICE | Italian Society of Endoscopic Surgery and New Technologies |
| RH | Right hemicolectomy |
| ASA | American Society of Anesthesiologists |
| GBM | Gradient-boosting machine |
| GLMNET | Generalized linear model via penalization |
| SVM | Support vector machine |
| LM | Linear model |
| MAPE | Mean absolute percentage error |
| MSE | Mean square error |
| BMI | Body mass index |
| AUC | Area under curve |
| VIP | Variable importance plot |
| MDA | Mean decrease accuracy |
| RH | Right hemicolectomy |
| ERAS | Enhanced recovery after surgery |
References
- Seow-En, I.; Chen, W.T.-L. Complete Mesocolic Excision with Central Venous Ligation/D3 Lymphadenectomy for Colon Cancer—A Comprehensive Review of the Evidence. Surg. Oncol. 2022, 42, 101755. [Google Scholar] [CrossRef]
- Anania, G.; Chiozza, M.; Campagnaro, A.; Bagolini, F.; Resta, G.; Azzolina, D.; Silecchia, G.; Cirocchi, R.; Agrusa, A.; Cuccurullo, D.; et al. Laparoscopic Right Hemicolectomy: A SICE (Società Italiana Di Chirurgia Endoscopica e Nuove Tecnologie) Network Prospective Study on the Approach to Right Colon Lymphadenectomy in Italy: Is There a Standard?—CoDIG 2 (ColonDx Italian Group). Surg. Endosc. 2024, 38, 1432–1441. [Google Scholar] [CrossRef] [PubMed]
- Anania, G.; Agresta, F.; Artioli, E.; Rubino, S.; Resta, G.; Vettoretto, N.; Petz, W.; Bergamini, C.M.; Arezzo, A.; Valpiani, G.; et al. Laparoscopic Right Hemicolectomy: The SICE (Societa’ Italiana Di Chirurgia Endoscopica e Nuove Tecnologie) Network Prospective Trial on 1225 Cases Comparing Intra Corporeal versus Extra Corporeal Ileo-Colic Side-to-Side Anastomosis. Surg. Endosc. Interv. Tech. 2020, 34, 4788–4800. [Google Scholar] [CrossRef]
- Stone, K.; Zwiggelaar, R.; Jones, P.; Mac Parthaláin, N. A Systematic Review of the Prediction of Hospital Length of Stay: Towards a Unified Framework. PLoS Digit. Health 2022, 1, e0000017. [Google Scholar] [CrossRef] [PubMed]
- Åhlin, P.; Almström, P.; Wänström, C. Solutions for Improved Hospital-Wide Patient Flows—A Qualitative Interview Study of Leading Healthcare Providers. BMC Health Serv. Res. 2023, 23, 17. [Google Scholar] [CrossRef] [PubMed]
- Diwan, W.; Nakonezny, P.; Wells, J. Effect of Length of Hospital Stay and Patient Factors on Patient Satisfaction in an Academic Hospital. Orthopedics 2020, 43, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Zeleke, A.J.; Palumbo, P.; Tubertini, P.; Miglio, R.; Chiari, L. Machine Learning-Based Prediction of Hospital Prolonged Length of Stay Admission at Emergency Department: A Gradient Boosting Algorithm Analysis. Front. Artif. Intell. 2023, 6, 1179226. [Google Scholar] [CrossRef]
- Tu, J.B.; Liao, W.J.; Liu, W.C.; Gao, X.H. Using Machine Learning Techniques to Predict the Risk of Osteoporosis Based on Nationwide Chronic Disease Data. Sci. Rep. 2024, 14, 5245. [Google Scholar] [CrossRef]
- Loftus, T.J.; Tighe, P.J.; Filiberto, A.C.; Efron, P.A.; Brakenridge, S.C.; Mohr, A.M.; Rashidi, P.; Upchurch, G.R.; Bihorac, A. Artificial Intelligence and Surgical Decision-Making. JAMA Surg. 2020, 155, 148. [Google Scholar] [CrossRef]
- Chiu, S.U.F.; Hung, C.M.; Chiu, C.C. A Commentary on “Application of Machine Learning in Surgery Research: Current Uses and Future Directions—Editorial”. Int. J. Surg. 2023, 109, 3661–3662. [Google Scholar] [CrossRef]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees; The Wadsworth and Brooks-Cole Statistics-Probability Series; Wadsworth Statistics/Probability Series; CRC Press: Boca Raton, FL, USA, 1984. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Friedman, J.H. Stochastic gradient boosting. Comput. Stat. Data Anal. 2002, 38, 367–378. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J. Stat. Softw. 2010, 33, 1–22. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Kuhn, M. Building Predictive Models in R Using the Caret Package. J. Stat. Softw. 2008, 28, 1–26. [Google Scholar] [CrossRef]
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2015. [Google Scholar]
- Meyer, J.; Meyer, E.; Meurette, G.; Liot, E.; Toso, C.; Ris, F. Robotic versus Laparoscopic Right Hemicolectomy: A Systematic Review of the Evidence. J. Robot. Surg. 2024, 18, 116. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, R.; Bajorath, J. Interpretation of Machine Learning Models Using Shapley Values: Application to Compound Potency and Multi-Target Activity Predictions. J. Comput. Aided Mol. Des. 2020, 34, 1013–1026. [Google Scholar] [CrossRef]
- Chang, W.; Cheng, J.; Allaire, J.J.; Xie, Y.; McPherson, J. Shiny: Web Application Framework for R; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Degiuli, M.; Azzolina, D.; Corcione, F.; Bracale, U.; Peltrini, R.; Baldazzi, G.; Sica, G.S.; Muratore, A.; Jovine, E.; Anania, G.; et al. ASO Author Reflections: Complete Mesocolic Excision versus Conventional Surgery for Right Colon Cancer (CoME-in Trial): An Interim Analysis of a Multicenter, Randomized, Controlled Trial. Ann. Surg. Oncol. 2024, 31, 1694–1695. [Google Scholar] [CrossRef] [PubMed]
- Degiuli, M.; Aguilar, A.H.R.; Solej, M.; Azzolina, D.; Marchiori, G.; Corcione, F.; Bracale, U.; Peltrini, R.; Di Nuzzo, M.M.; Baldazzi, G.; et al. A Randomized Phase III Trial of Complete Mesocolic Excision Compared with Conventional Surgery for Right Colon Cancer: Interim Analysis of a Nationwide Multicenter Study of the Italian Society of Surgical Oncology Colorectal Cancer Network (CoME-in Trial). Ann. Surg. Oncol. 2024, 31, 1671–1680. [Google Scholar] [CrossRef]
- Basunbul, L.I.; Alhazmi, L.S.S.; Almughamisi, S.A.; Aljuaid, N.M.; Rizk, H.; Moshref, R. Recent Technical Developments in the Field of Laparoscopic Surgery: A Literature Review. Cureus 2022, 14. [Google Scholar] [CrossRef]
- Li, H.; Luo, T.F.; Zhang, N.R.; Zhang, L.Z.; Huang, X.; Jin, S.Q. Factors Associated with Prolonged Postoperative Length of Hospital Stay after Laparoscopic Colorectal Cancer Resection: A Secondary Analysis of a Randomized Controlled Trial. BMC Surg. 2022, 22, 438. [Google Scholar] [CrossRef] [PubMed]
- Mekhaldi, R.N.; Caulier, P.; Chaabane, S.; Chraibi, A.; Piechowiak, S. A Comparative Study of Machine Learning Models for Predicting Length of Stay in Hospitals. J. Inf. Sci. Eng. 2021, 37, 1025–1038. [Google Scholar]
- Garau, N.; Paganelli, C.; Summers, P.; Choi, W.; Alam, S.; Lu, W.; Fanciullo, C.; Bellomi, M.; Baroni, G.; Rampinelli, C. External Validation of Radiomics-based Predictive Models in Low-dose CT Screening for Early Lung Cancer Diagnosis. Med. Phys. 2020, 47, 4125–4136. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, U.O.; Scott, M.J.; Hubner, M.; Nygren, J.; Demartines, N.; Francis, N.; Rockall, T.A.; Young-Fadok, T.M.; Hill, A.G.; Soop, M.; et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: 2018. World J. Surg. 2019, 43, 659–695. [Google Scholar] [CrossRef] [PubMed]
- Feroci, F.; Kröning, K.C.; Lenzi, E.; Moraldi, L.; Cantafio, S.; Scatizzi, M. Laparoscopy within a Fast-Track Program Enhances the Short-Term Results after Elective Surgery for Resectable Colorectal Cancer. Surg. Endosc. 2011, 25, 2919–2925. [Google Scholar] [CrossRef]
- Peterson, C.Y.; Blank, J.; Ludwig, K. Colorectal Cancer in Elderly Patients: Considerations in Treatment and Management. In Principles and Practice of Geriatric Surgery; Rosenthal, R.A., Zenilman, M.E., Katlic, M.R., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 903–929. ISBN 978-3-319-47770-1. [Google Scholar]
- Ahmed, J.; Khan, S.; Lim, M.; Chandrasekaran, T.V.; MacFie, J. Enhanced Recovery after Surgery Protocols—Compliance and Variations in Practice during Routine Colorectal Surgery. Colorectal Dis. 2012, 14, 1045–1051. [Google Scholar] [CrossRef]
- Pandolfini, L.; Conti, D.; Ballo, P.; Laessig, R.; Falsetto, A.; Paroli, G.M.; Genzano, C.; Cantini, S.; Pavoni, V.; Scatizzi, M. ERAS Pathway Adherence in Laparoscopic Colorectal Surgery: Results of a Newly Adopted Program in a Single Italian Institution. Il G. Chir. J. Ital. Assoc. Hosp. Surg. 2022, 42, e10. [Google Scholar] [CrossRef]
- Frasson, M.; Flor-Lorente, B.; Ramos Rodríguez, J.L.; Granero-Castro, P.; Hervás, D.; Alvarez Rico, M.A.; Brao, M.J.G.; Sánchez González, J.M.; Garcia-Granero, E. Risk Factors for Anastomotic Leak after Colon Resection for Cancer: Multivariate Analysis and Nomogram from a Multicentric, Prospective, National Study with 3193 Patients. Ann. Surg. 2015, 262, 321–330. [Google Scholar] [CrossRef]
- Van Oostendorp, S.; Elfrink, A.; Borstlap, W.; Schoonmade, L.; Sietses, C.; Meijerink, J.; Tuynman, J. Intracorporeal versus Extracorporeal Anastomosis in Right Hemicolectomy: A Systematic Review and Meta-Analysis. Surg. Endosc. 2017, 31, 64–77. [Google Scholar] [CrossRef]
- Puleo, F.; Mishra, N.; Hall, J. Use of Intra-Abdominal Drains. Clin. Colon Rectal Surg. 2013, 26, 174–177. [Google Scholar] [CrossRef]
- Mujagic, E.; Zeindler, J.; Coslovsky, M.; Hoffmann, H.; Soysal, S.D.; Mechera, R.; Von Strauss, M.; Delko, T.; Saxer, F.; Glaab, R.; et al. The Association of Surgical Drains with Surgical Site Infections—A Prospective Observational Study. Am. J. Surg. 2019, 217, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, U.O. Adherence to the Enhanced Recovery after Surgery Protocol and Outcomes after Colorectal Cancer Surgery. Arch. Surg. 2011, 146, 571. [Google Scholar] [CrossRef] [PubMed]
- Guadagni, S.; Catarci, M.; Masedu, F.; Karim, M.E.; Clementi, M.; Ruffo, G.; Viola, M.G.; Borghi, F.; Baldazzi, G.; Scatizzi, M.; et al. Abdominal Drainage after Elective Colorectal Surgery: Propensity Score-Matched Retrospective Analysis of an Italian Cohort. BJS Open 2024, 8, zrad107. [Google Scholar] [CrossRef]
- Rooijen, S.J.V.; Jongen, A.C.; Wu, Z.-Q.; Ji, J.-F.; Slooter, G.D.; Roumen, R.M.; Bouvy, N.D. Definition of Colorectal Anastomotic Leakage: A Consensus Survey among Dutch and Chinese Colorectal Surgeons. World J. Gastroenterol. 2017, 23, 6172–6180. [Google Scholar] [CrossRef]
- Martínez-Pérez, A.; Piccoli, M.; Casoni Pattacini, G.; Winter, D.C.; Carcoforo, P.; Celentano, V.; Chiarugi, M.; Di Saverio, S.; Bianchi, G.; Frontali, A.; et al. Conversion to Open Surgery During Minimally Invasive Right Colectomy for Cancer: Results from a Large Multinational European Study. J. Laparoendosc. Adv. Surg. Tech. 2023, 33, 344–350. [Google Scholar] [CrossRef]
- Ayinde, B.O.; Chokshi, P.; Adhikari, S.; Jaimalani, A.; Yeritsyan, A.; Surve, A.V.; Khan, S. Challenges and Elements Hindering the Adoption of Enhanced Recovery after Surgery (ERAS) Protocols in Colorectal Surgery and Their Resolutions: A Systematic Review. Cureus 2024, 16. [Google Scholar] [CrossRef] [PubMed]
- Fellahi, J.L.; Futier, E.; Vaisse, C.; Collange, O.; Huet, O.; Loriau, J.; Gayat, E.; Tavernier, B.; Biais, M.; Asehnoune, K.; et al. Perioperative Hemodynamic Optimization: From Guidelines to Implementation—An Experts’ Opinion Paper. Ann. Intensive Care 2021, 11, 58. [Google Scholar] [CrossRef]
- Trinkley, K.E.; An, R.; Maw, A.M.; Glasgow, R.E.; Brownson, R.C. Leveraging Artificial Intelligence to Advance Implementation Science: Potential Opportunities and Cautions. Implement. Sci. 2024, 19, 17. [Google Scholar] [CrossRef]

| CoDIG 1 (Internal Validation Sample) | CoDIG 2 (External Validation Sample) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Less than 1 Week | More than 1 Week | Total | p | Less than 1 Week | More than 1 Week | Total | p |
| (n = 570) | (n = 654) | (n = 1224) | (n = 454) | (n = 334) | (n = 788) | |||
| Preoperative | ||||||||
| Age (years) (median [IQR]) | 74.0 [65.0;80.0] | 73.0 [64.0;80.0] | 74.0 [65.0;80.0] | 0.315 | 73.0 [65.0;80.0] | 76.0 [70.0;82.0] | 74.0 [67.0;81.0] | <0.001 |
| Gender, n (%) | 0.99 | 0.075 | ||||||
| Male | 293 (51.4%) | 337 (51.5%) | 630 (51.5%) | 228 (50.2%) | 190 (56.9%) | 418 (53.0%) | ||
| Female | 277 (48.6%) | 317 (48.5%) | 594 (48.5%) | 226 (49.8%) | 144 (43.1%) | 370 (47.0%) | ||
| BMI, n (%) | 0.137 | 0.421 | ||||||
| <18 | 13 (2.28%) | 27 (4.13%) | 40 (3.27%) | 10 (2.20%) | 4 (1.20%) | 14 (1.78%) | ||
| 18–24 | 272 (47.7%) | 294 (45.0%) | 566 (46.2%) | 216 (47.6%) | 154 (46.1%) | 370 (47.0%) | ||
| 25–30 | 203 (35.6%) | 253 (38.7%) | 456 (37.3%) | 175 (38.5%) | 126 (37.7%) | 301 (38.2%) | ||
| >30 | 82 (14.4%) | 80 (12.2%) | 162 (13.2%) | 53 (11.7%) | 50 (15.0%) | 103 (13.1%) | ||
| ASA score, n (%) | 0.2 | <0.001 | ||||||
| I | 42 (7.37%) | 51 (7.80%) | 93 (7.60%) | 23 (5.07%) | 4 (1.20%) | 27 (3.43%) | ||
| II | 269 (47.2%) | 338 (51.7%) | 607 (49.6%) | 238 (52.4%) | 121 (36.2%) | 359 (45.6%) | ||
| III | 237 (41.6%) | 250 (38.2%) | 487 (39.8%) | 179 (39.4%) | 173 (51.8%) | 352 (44.7%) | ||
| IV | 22 (3.86%) | 15 (2.29%) | 37 (3.02%) | 14 (3.08%) | 36 (10.8%) | 50 (6.35%) | ||
| Pathology, n (%) | 0.562 | 0.314 | ||||||
| Benign | 77 (13.5%) | 80 (12.2%) | 157 (12.8%) | 26 (5.73%) | 13 (3.89%) | 39 (4.95%) | ||
| Malignant | 493 (86.5%) | 574 (87.8%) | 1067 (87.2%) | 428 (94.3%) | 321 (96.1%) | 749 (95.1%) | ||
| Comorbidities, n (%) | 0.987 | 0.001 | ||||||
| None | 330 (57.9%) | 380 (58.1%) | 710 (58.0%) | 297 (65.4%) | 180 (53.9%) | 477 (60.5%) | ||
| One or more | 240 (42.1%) | 274 (41.9%) | 514 (42.0%) | 157 (34.6%) | 154 (46.1%) | 311 (39.5%) | ||
| Previous abdominal surgery, n (%) | 0.635 | 0.297 | ||||||
| None | 299 (52.5%) | 353 (54.0%) | 652 (53.3%) | 252 (55.5%) | 172 (51.5%) | 424 (53.8%) | ||
| One or more | 271 (47.5%) | 301 (46.0%) | 572 (46.7%) | 202 (44.5%) | 162 (48.5%) | 364 (46.2%) | ||
| Tumor, n(%) | 0.255 | <0.001 | ||||||
| T1 | 69 (14.7%) | 66 (12.3%) | 135 (13.5%) | 68 (17.0%) | 33 (11.2%) | 101 (14.6%) | ||
| T2 | 94 (20.1%) | 114 (21.3%) | 208 (20.7%) | 121 (30.3%) | 57 (19.4%) | 178 (25.7%) | ||
| T3 | 249 (53.2%) | 271 (50.7%) | 520 (51.8%) | 172 (43.1%) | 161 (54.8%) | 333 (48.1%) | ||
| T4 | 56 (12.0%) | 84 (15.7%) | 140 (14.0%) | 38 (9.52%) | 43 (14.6%) | 81 (11.7%) | ||
| Node, n (%) | 0.6 | 0.016 | ||||||
| N+ | 58 (12.2%) | 75 (13.9%) | 133 (13.1%) | 34 (8.59%) | 45 (15.5%) | 79 (11.5%) | ||
| N0 | 308 (64.6%) | 348 (64.7%) | 656 (64.6%) | 258 (65.2%) | 169 (58.3%) | 427 (62.2%) | ||
| N1 | 111 (23.3%) | 115 (21.4%) | 226 (22.3%) | 104 (26.3%) | 76 (26.2%) | 180 (26.2%) | ||
| Metastasis, n(%) | 0.496 | 0.187 | ||||||
| M0 | 443 (94.7%) | 498 (93.4%) | 941 (94.0%) | 377 (95.4%) | 270 (92.8%) | 647 (94.3%) | ||
| M+ | 25 (5.34%) | 35 (6.57%) | 60 (5.99%) | 18 (4.56%) | 21 (7.22%) | 39 (5.69%) | ||
| Intraoperative | ||||||||
| Length of surgical procedure, n (%) | 0.089 | <0.001 | ||||||
| >270 min | 27 (4.74%) | 48 (7.34%) | 75 (6.13%) | 37 (8.15%) | 46 (13.8%) | 83 (10.5%) | ||
| 181–270 min | 180 (31.6%) | 220 (33.6%) | 400 (32.7%) | 152 (33.5%) | 141 (42.2%) | 293 (37.2%) | ||
| 90–180 min | 363 (63.7%) | 386 (59.0%) | 749 (61.2%) | 265 (58.4%) | 147 (44.0%) | 412 (52.3%) | ||
| Blood transfusion, n (%) | <0.001 | <0.001 | ||||||
| No | 20 (3.51%) | 59 (9.02%) | 79 (6.45%) | 448 (98.7%) | 312 (93.4%) | 760 (96.4%) | ||
| Yes | 550 (96.5%) | 595 (91.0%) | 1145 (93.5%) | 6 (1.32%) | 22 (6.59%) | 28 (3.55%) | ||
| Intraoperative minimal bleeding > 200 mL, n (%) | <0.001 | 0.001 | ||||||
| No | 551 (96.7%) | 603 (92.2%) | 1154 (94.3%) | 419 (92.3%) | 288 (86.2%) | 707 (89.7%) | ||
| Yes | 19 (3.33%) | 51 (7.80%) | 70 (5.72%) | 35 (7.71%) | 46 (13.8%) | 81 (10.3%) | ||
| Anastomosis, n (%) | <0.001 | <0.001 | ||||||
| Extracorporeal | 87 (15.3%) | 276 (42.2%) | 363 (29.7%) | 89 (19.6%) | 121 (36.2%) | 210 (26.6%) | ||
| Intracorporeal | 483 (84.7%) | 378 (57.8%) | 861 (70.3%) | 365 (80.4%) | 213 (63.8%) | 578 (73.4%) | ||
| Drainage, n(%) | <0.001 | <0.001 | ||||||
| No | 303 (53.2%) | 171 (26.1%) | 474 (38.7%) | 185 (40.7%) | 92 (27.5%) | 277 (35.2%) | ||
| Yes | 267 (46.8%) | 483 (73.9%) | 750 (61.3%) | 269 (59.3%) | 242 (72.5%) | 511 (64.8%) | ||
| Conversion *, n (%) | <0.001 | 0.004 | ||||||
| No | 566 (99.3%) | 592 (90.5%) | 1158 (94.6%) | 431 (94.9%) | 298 (89.2%) | 729 (92.5%) | ||
| Yes | 4 (0.70%) | 62 (9.48%) | 66 (5.39%) | 23 (5.07%) | 36 (10.8%) | 59 (7.49%) | ||
| Fast-track protocol, n (%) | <0.001 | <0.001 | ||||||
| No | 135 (23.7%) | 435 (66.5%) | 570 (46.6%) | 80 (17.6%) | 167 (50.0%) | 247 (31.3%) | ||
| Yes | 435 (76.3%) | 219 (33.5%) | 654 (53.4%) | 374 (82.4%) | 167 (50.0%) | 541 (68.7%) | ||
| Right hemicolectomy **, n(%) | 0.068 | 0.262 | ||||||
| Laparoscopic | 513 (90.0%) | 575 (87.9%) | 1088 (88.9%) | 369 (81.3%) | 278 (83.2%) | 647 (82.1%) | ||
| Robotic | 34 (5.96%) | 60 (9.17%) | 94 (7.68%) | 59 (13.0%) | 32 (9.58%) | 91 (11.5%) | ||
| Video-assisted *** | 23 (4.04%) | 19 (2.91%) | 42 (3.43%) | 26 (5.73%) | 24 (7.19%) | 50 (6.35%) | ||
| Outcome | ||||||||
| LoS | 3.00 [2.00;3.00] | 7.00 [5.00;9.00] | 7.00 [5.00;8.00] | <0.001 | 6.00 [5.00;8.00] | 8.00 [7.00;11.0] | 6.00 [5.00;8.00] | <0.001 |
| CoDIG 1 Internal Validation | CoDIG 2 External Validation | |||||||
|---|---|---|---|---|---|---|---|---|
| Model | MAPE | RMSE | ROC | Accuracy | MAPE | RMSE | ROC | Accuracy |
| Random forest (RF) | 0.21 | 2.8 | 0.92 | 0.94 | 0.81 | 6.04 | 0.65 | 0.42 |
| Support vector machine (SVM) | 0.29 | 5.00 | 0.86 | 0.83 | 0.48 | 4.68 | 0.75 | 0.79 |
| Gradient-boosting machine (GBM) | 0.38 | 4.78 | 0.81 | 0.81 | 0.91 | 6.15 | 0.67 | 0.3 |
| Generalized linear model with penalized maximum likelihood (GLMNET) | 0.38 | 4.8 | 0.8 | 0.81 | 0.76 | 5.54 | 0.68 | 0.43 |
| Linear model (LM) | 0.38 | 4.75 | 0.78 | 0.8 | 0.93 | 6.3 | 0.67 | 0.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anania, G.; Chiozza, M.; Pedarzani, E.; Resta, G.; Campagnaro, A.; Pedon, S.; Valpiani, G.; Silecchia, G.; Mascagni, P.; Cuccurullo, D.; et al. Predicting Postoperative Length of Stay in Patients Undergoing Laparoscopic Right Hemicolectomy for Colon Cancer: A Machine Learning Approach Using SICE (Società Italiana di Chirurgia Endoscopica) CoDIG Data. Cancers 2024, 16, 2857. https://doi.org/10.3390/cancers16162857
Anania G, Chiozza M, Pedarzani E, Resta G, Campagnaro A, Pedon S, Valpiani G, Silecchia G, Mascagni P, Cuccurullo D, et al. Predicting Postoperative Length of Stay in Patients Undergoing Laparoscopic Right Hemicolectomy for Colon Cancer: A Machine Learning Approach Using SICE (Società Italiana di Chirurgia Endoscopica) CoDIG Data. Cancers. 2024; 16(16):2857. https://doi.org/10.3390/cancers16162857
Chicago/Turabian StyleAnania, Gabriele, Matteo Chiozza, Emma Pedarzani, Giuseppe Resta, Alberto Campagnaro, Sabrina Pedon, Giorgia Valpiani, Gianfranco Silecchia, Pietro Mascagni, Diego Cuccurullo, and et al. 2024. "Predicting Postoperative Length of Stay in Patients Undergoing Laparoscopic Right Hemicolectomy for Colon Cancer: A Machine Learning Approach Using SICE (Società Italiana di Chirurgia Endoscopica) CoDIG Data" Cancers 16, no. 16: 2857. https://doi.org/10.3390/cancers16162857
APA StyleAnania, G., Chiozza, M., Pedarzani, E., Resta, G., Campagnaro, A., Pedon, S., Valpiani, G., Silecchia, G., Mascagni, P., Cuccurullo, D., Reddavid, R., Azzolina, D., & On behalf of SICE CoDIG (ColonDx Italian Group). (2024). Predicting Postoperative Length of Stay in Patients Undergoing Laparoscopic Right Hemicolectomy for Colon Cancer: A Machine Learning Approach Using SICE (Società Italiana di Chirurgia Endoscopica) CoDIG Data. Cancers, 16(16), 2857. https://doi.org/10.3390/cancers16162857







