What Does N2 Lymph Node Involvement Mean for Patients with Non-Small Cell Lung Cancer (NSCLC)?—A Review of Implications for Diagnosis and Treatment
Abstract
Simple Summary
Abstract
1. Introduction
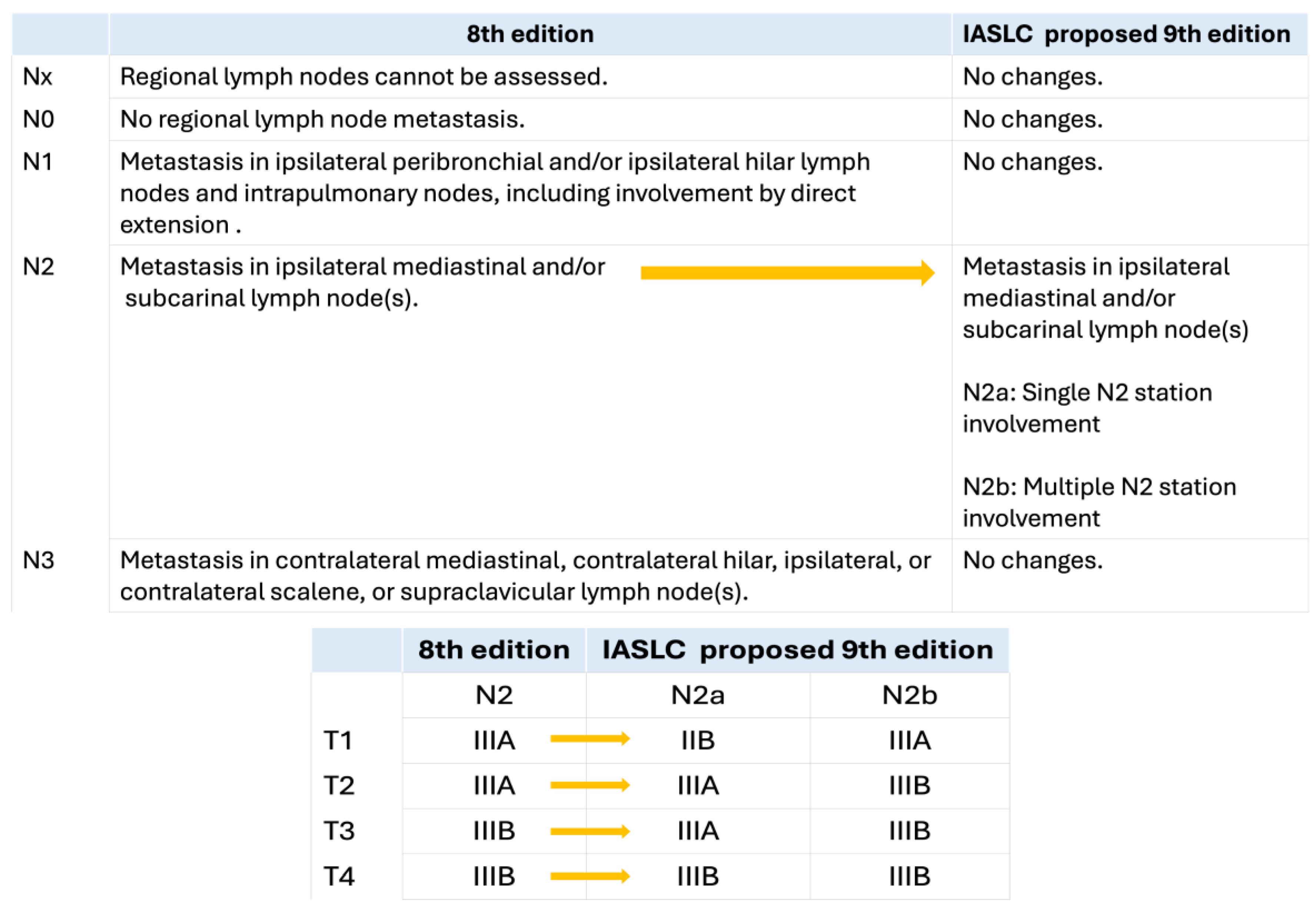
2. Definition of N2 Disease
3. Implications for Diagnosis
3.1. Imaging Diagnosis
3.2. Invasive Diagnosis
4. Implications for Treatment
4.1. Surgical Resectability
4.2. Peri-Operative Treatment
4.2.1. Neoadjuvant Systemic Treatment
| Type of Treatment | Trial Name | Phase | Treatment Arms | Adenocarcinoma/ Non-Squamous | TNM Version | N of Patients | Stage III | N2 Patients | N2 Single -Station | N2 Multi-Station | Pre-Treatment Nodal Pathological Confirmation Required | Technique for Pathological Confirmation (Pre-Treatment) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neoadjuvant Setting | ||||||||||||
| CT | Song et al. [33] | MA | CT | NA | 3–6 | 1637 | 50% | NA | NA | NA | NA | NA |
| BSC | NA | 1587 | 48% | NA | NA | NA | ||||||
| CT+ Immunotherapy | Checkmate-816 [35] | III | CT + Nivolumab | 51% | 8 | 179 | 63% | NA | NA | NA | Yes | Mediastinoscopy, thoracotomy, or EBUS |
| CT | 47% | 179 | 64% | NA | NA | NA | ||||||
| TD-FOREKNOW [36] | II | CT + Camrelizumab | 37% | 8 | 43 | 100% | 79% | NA | NA | No | NA | |
| CT | 29% | 45 | 100% | 69% | NA | NA | ||||||
| Targeted therapy | Aredo et al. [37] | II | Osimertinib | 100% | 7 | 27 | 33% | NA | NA | NA | No | NA |
| NEOS [38] | IIB | Osimertinib | 100% | 8 | 38 | 65% | 17% | NA | NA | Yes, if PET-CT was negative | EBUS | |
| Adjuvant Setting | ||||||||||||
| CT | LACE [34] | MA | CT | 51% | 5–6 | 2281 | 27% | 23% | NA | NA | -- | -- |
| Placebo | 51% | 2303 | 27% | 22% | NA | NA | ||||||
| CT+ Immunotherapy | PEARLS/KEYNOTE 091 [40] | III | Pembrolizumab | 67% | 7 | 590 | 30% | 21% | NA | NA | -- | -- |
| Placebo | 62% | 587 | 28% | 18% | NA | NA | ||||||
| IMpower 010 [41,42] | III | Atezolizumab | 65% | 7 | 507 | 40% | 30% | NA | NA | -- | -- | |
| BSC | 67% | 498 | 42% | 30% | NA | NA | ||||||
| Targeted therapy | CTONG1104 [43] | III | Gefitinib | 92% | 111 | 65% | 64% | NA | NA | -- | -- | |
| CT | 95% | 111 | 64% | 65% | NA | NA | -- | -- | ||||
| ADAURA [44,45] | III | Osimertinib | 96% | 7 | 339 | 35% | 31% | NA | NA | -- | -- | |
| Placebo | 97% | 343 | 34% | 30% | NA | NA | ||||||
| ALINA [46] | III | Alectinib | 95% | 7 | 130 | 53% | 49% | NA | NA | -- | -- | |
| CT | 98% | 127 | 55% | 52% | NA | NA | ||||||
| Perioperative Setting | ||||||||||||
| CT+ Immunotherapy | AEGEAN [5] | III | CT + Durvalumab | 54% | 8 | 366 | 71% | 50% | 39% | 9% | Yes, if PET-CT was negative | Mediastinoscopy, thoracotomy, or EBUS |
| CT + Placebo | 48% | 374 | 70% | 50% | 35% | 11% | ||||||
| KEYNOTE 671 [6] | III | CT + Pembrolizumab | 57% | 8 | 397 | 70% | 42% | NA | NA | Yes, if PET-CT was negative | Mediastinoscopy, thoracotomy, or EBUS | |
| CT + Placebo | 57% | 400 | 70% | 47% | NA | NA | ||||||
| Checkmate 77T [7] | III | CT + Nivolumab | 49% | 8 | 229 | 65% | 65% | 26% | 14% | NA | NA | |
| CT + Placebo | 49% | 232 | 64% | 64% | 23% | 16% | ||||||
| Neotorch [8] | III | CT + Toripalimab | 22% | 8 | 202 | 100% | 68% | NA | NA | Yes, if PET-CT was negative | Mediastinoscopy, thoracotomy, or EBUS | |
| CT + Placebo | 22% | 202 | 99% | 72% | NA | NA | ||||||
| Rationale 315 [9] | III | CT + Tislelizumab | NA | 8 | 226 | 58% | 36% | NA | NA | NA | NA | |
| CT + Placebo | NA | 227 | 59% | 35% | NA | NA | ||||||
| NADIM II [47] | II | CT + Nivolumab | 44% | 8 | 57 | 100% | 72% | 33% | 39% | Yes, if N2 disease was suspected by PET-CT | Mediastinoscopy, thoracotomy, or EBUS | |
| CT | 38% | 29 | 100% | 55% | 17% | 38% | ||||||
| Trial Name | Treatment Arms | pCR Rate—% (95% CI) * | EFS/DFS/PFS—Median (95% CI) & HR (95% CI) * | OS—Median (95% CI) & HR (95% CI) * | Surgical Outcomes | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| All Patients | N2/Stage III | End-Point | All Patients | N2/Stage III | All Patients | N2/Stage III | R0 § | Did Not Complete Surgery | ||
| NEOADJUVANT | ||||||||||
| Song et al. [33] | CT | NA | NA | NA | NA | NA | NA. HR 0.84 (0.77–0.92) | Stage III: NA. HR 0.84 (0.75–0.95) | NA | NA |
| Placebo | ||||||||||
| Checkmate 816 [35] | CT + Nivolumab | 24% (18.0–31.0) | Stage IIIA: 23% (15.6–31.9) | EFS | 31.6 (30.2-NR) vs. 20.8 (14.0–26.7) HR 0.63 (0.43–0.91) | Stage IIIA: 31.6 (26.6–NR) vs. 15.7 (10.8–22.7) HR 0.54 (0.37–0.80) | NR vs. NR HR 0.62 (0.36–1.05) | NA | 83% | 16% |
| CT | 2% (0.6–5.6) | Stage IIIA: 0.9% (<0.1–4.7) | 78% | 21% | ||||||
| TD-FOREKNOW [36] | CT + Camrelizumab | 32.6% (19.1–48.5) | NA | EFS | NR vs. NR HR 0.52 (0.21–1.29) | NA | NA | NA | NA | NA |
| CT | 8.9% (2.5–21.2) | |||||||||
| Aredo et al. [37] | Osimertinib | 0% | NA | DFS | 32.4 (25.9-NR) | NA | NA | NA | 89% | NA |
| NEOS [38] | Osimertinib | 4% | NA | NA | NA | NA | NA | NA | 94% | NA |
| ADJUVANT | ||||||||||
| LACE [34] | CT | -- | -- | DFS | NA HR 0.84 (0.78–0.91) | NA | NA HR 0.89 (0.82–0.96) | Stage III: NA HR 0.83 (0.72–0.94) | -- | -- |
| Placebo | ||||||||||
| PEARLS/KEYNOTE 091 [40] | Pembro-lizumab | -- | -- | DFS | 53.6 (39.2-NR) vs. 42.0 (31.3-NR) HR 0.76 (0.63–0.91) | Stage IIIA: NA HR 0.92 (0.69–1.24) | NR vs. NR HR 0.87, 95% CI, 0.67–1.15 | NA | -- | -- |
| Placebo | -- | -- | -- | -- | ||||||
| IMpower 010 [41,42] | Atezolizumab | -- | -- | DFS | Final DFS analysis: ITT: 65.6 vs. 47.8, HR 0.85 (0.71–1.01) PD-L1 ≥ 50%: NR vs. 41.1, HR 0.48 (0.32–0.72) PD-L1 1–49%: 68.5 vs. 37.3, HR 0.70 (0.55–0.91) | Primary DFS analysis: All N2 & PD-L1 ≥ 1%: 32.3 (24.2–NE) vs. 21.3 (15.7–31.4) HR 0.66 (0.44–0.99) All N2: 30.2 (24.0–42.3) vs. 24.1 (18.0–31.4) HR 0.83 (0.61–1.13) | Second OS analysis: II-IIIA and: PD-L1 ≥ 50%: NE vs. 87.1, HR 0.47 (0.28–0.77) PD-L1 1-49%: NE vs. 87.1, HR 0.77 (0.56–1.06) PD-L1 < 1%: NA | Primary OS analysis: All N2 and: PD-L1 ≥ 50%: NE vs. NE. HR 0.36 (0.14-0.95) PD-L1 1–49%: NE vs. NE. HR 1.38 (0.73–2.61) PD-L1 < 1%: NE vs. NE. HR 1.26 (0.72–2.22) | -- | -- |
| BSC | -- | -- | -- | -- | ||||||
| CTONG1104 [43] | Gefitinib | -- | -- | DFS | 30.8 (26.7–36.6) vs. 19.8 (15.4–23.0) HR 0.56 (0.40–0.79) | All N2: NA. HR 0.52 (0.34–0.80) | 75.5 (46.6-NE) vs. 62.8 (45.8-NE) HR 0.92 (0.62–1.36) | All N2: NA. HR 0.92 (0.58–1.45) | -- | -- |
| CT | -- | -- | -- | -- | ||||||
| ADAURA [44,45] | Osimertinib | -- | -- | DFS | NR (38.8-NE) vs. 27.5 (22–35) HR 0.20 (0.14-0.30) | Stage IIIA: NA. HR 0.12 (0.07–0.20) | At 5 years: 88% (83–91%) vs. 78% (73–82%) HR 0.49 (0.34–070) | Stage IIIA: At 5 years: 85% (76–91%) vs. 67% (57–75%) HR 0.37 (0.20–0.64) | -- | -- |
| Placebo | -- | -- | -- | -- | ||||||
| ALINA [46] | Alectinib | -- | -- | DFS | NR vs. 41.3 (28.5-NC) HR 0.24 (0.13–0.45) | All N2: NA. HR 0.21 (0.09–0.47) | NA | NA | -- | -- |
| CT | -- | -- | -- | -- | ||||||
4.2.2. Adjuvant Systemic Treatment
4.2.3. Perioperative Systemic Treatment
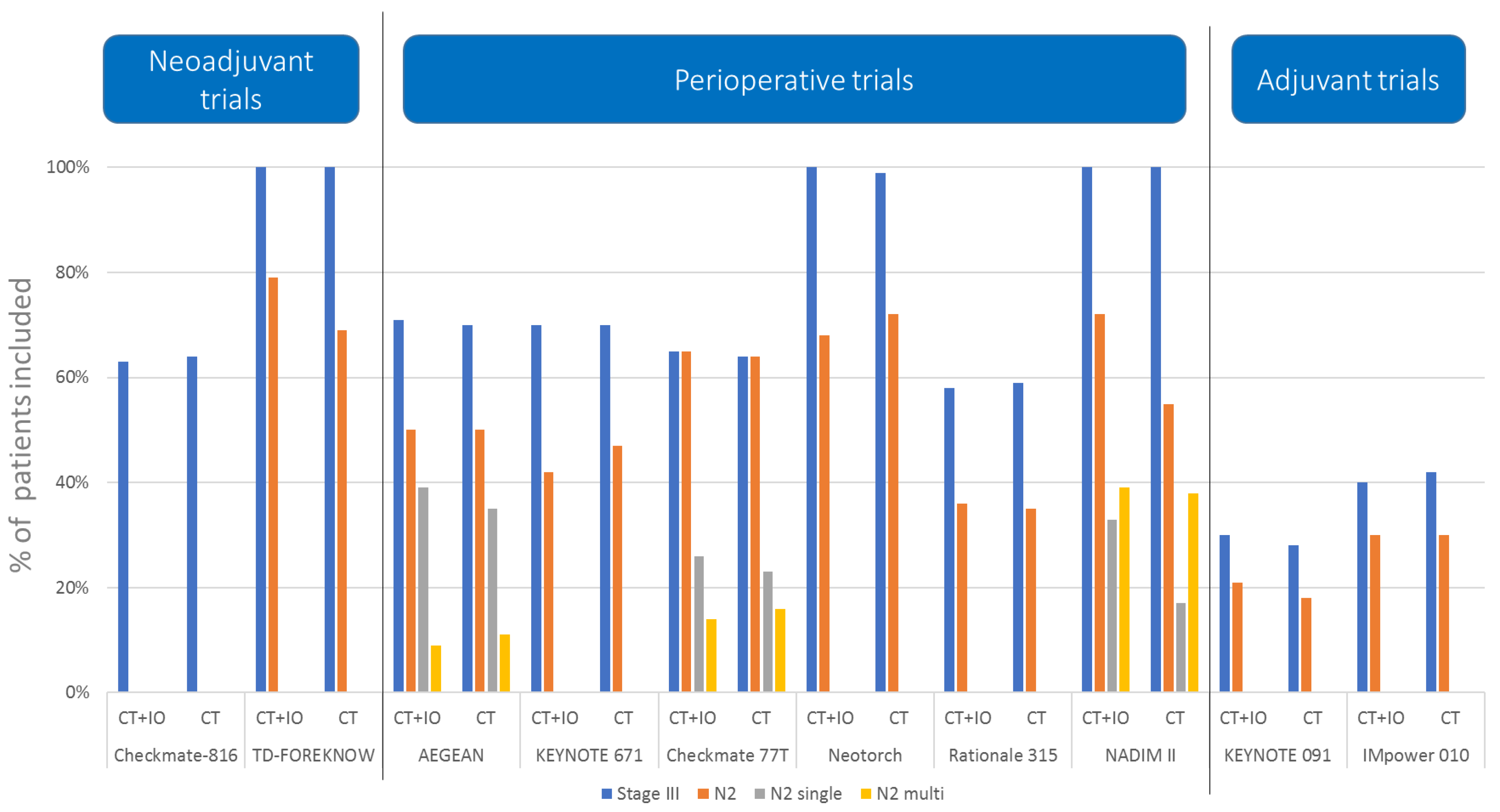
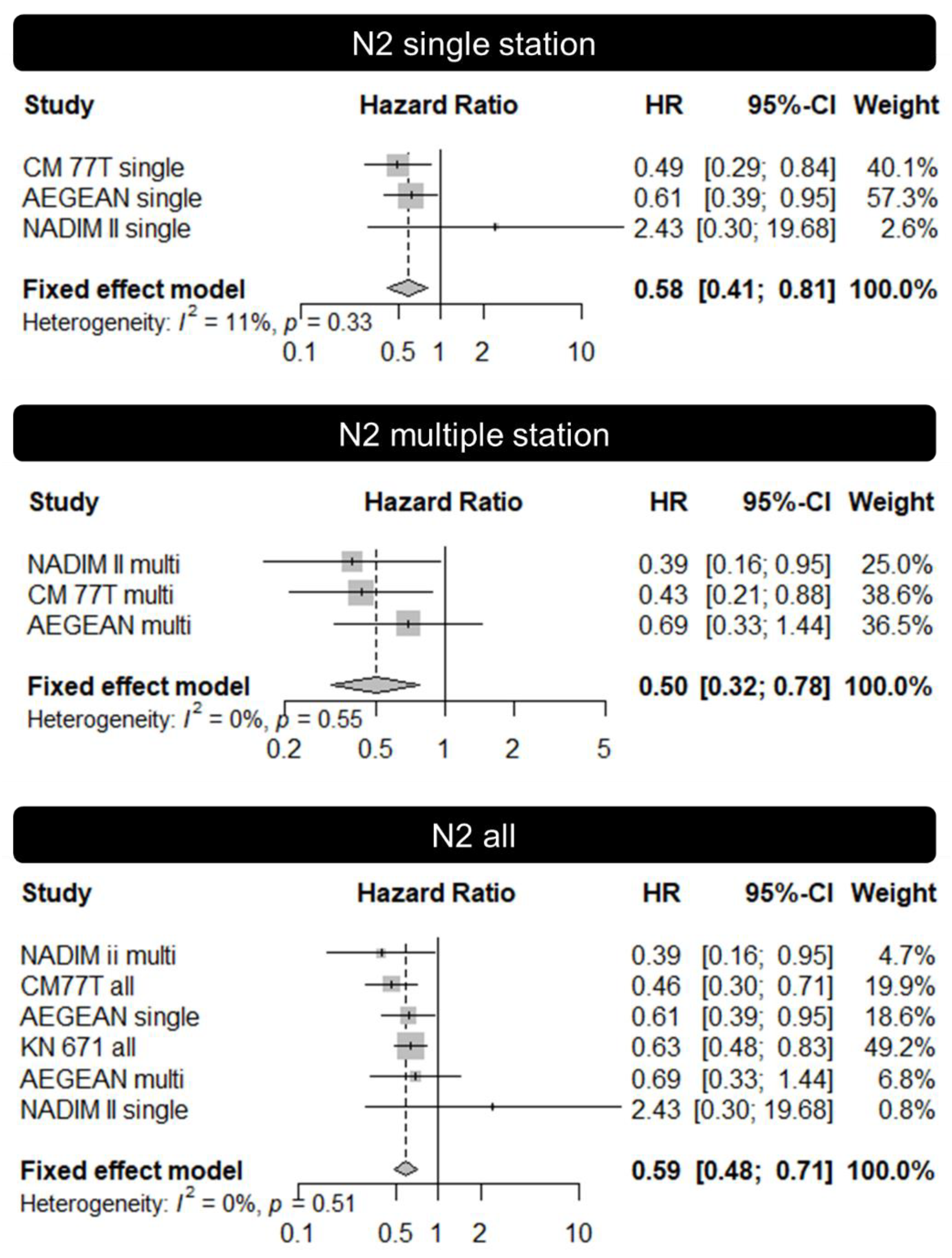
4.2.4. Perioperative Chemo-Immunotherapy—Pooled Analysis for N2 Disease
4.2.5. Postoperative Radiotherapy (PORT)
4.3. Radical Treatment in Unresectable Locally Advanced NSCLC
5. Areas of Future Research
5.1. Best Local Treatment Modality for Operable Patients with Resectable N2 Disease
5.2. “Borderline” Resectable Tumors
5.3. Tailored Treatment
5.3.1. Actionable Genomic Alterations
5.3.2. Genomic Signatures
5.3.3. Circulating Tumor DNA (ctDNA)
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Casal-Mouriño, A.; Ruano-Ravina, A.; Lorenzo-González, M.; Rodríguez-Martínez, Á.; Giraldo-Osorio, A.; Varela-Lema, L.; Pereiro-Brea, T.; Barros-Dios, J.M.; Valdés-Cuadrado, L.; Pérez-Ríos, M. Epidemiology of stage III lung cancer: Frequency, diagnostic characteristics, and survival. Transl. Lung Cancer Res. 2021, 10, 506–518. [Google Scholar] [CrossRef] [PubMed]
- Behera, M.; Steuer, C.E.; Liu, Y.; Fernandez, F.; Fu, C.; Higgins, K.A.; Gillespie, T.W.; Pakkala, S.; Pillai, R.N.; Force, S.; et al. Trimodality therapy in the treatment of Stage III N2-positive non-small cell lung cancer: A national cancer database analysis. Oncologist 2020, 25, e964–e975. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Li, N.; Xu, Y.; Yang, G. Evaluation of postoperative radiotherapy effect on survival of resected stage III-N2 non-small cell lung cancer patients. Front. Oncol. 2020, 10, 1135. [Google Scholar] [CrossRef] [PubMed]
- Remon, J.; Soria, J.-C.; Peters, S. Early and locally advanced non-small-cell lung cancer: An update of the ESMO clinical practice guidelines focusing on diagnosis, staging, systemic and local therapy. Ann. Oncol. 2021, 32, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Heymach, J.V.; Harpole, D.; Mitsudomi, T.; Taube, J.M.; Galffy, G.; Hochmair, M.; Winder, T.; Zukov, R.; Garbaos, G.; Gao, S.; et al. Perioperative durvalumab for resectable non–small-cell lung cancer. N. Engl. J. Med. 2023, 389, 1672–1684. [Google Scholar] [CrossRef] [PubMed]
- Wakelee, H.; Liberman, M.; Kato, T.; Tsuboi, M.; Lee, S.-H.; Gao, S.; Chen, K.-N.; Dooms, C.; Majem, M.; Eigendorff, E.; et al. Perioperative pembrolizumab for early-stage non–small-cell lung cancer. N. Engl. J. Med. 2023, 389, 491–503. [Google Scholar] [CrossRef]
- Cascone, T.; Awad, M.M.; Spicer, J.D.; He, J.; Lu, S.; Sepesi, B.; Tanaka, F.; Taube, J.M.; Cornelissen, R.; Havel, L.; et al. Perioperative nivolumab in resectable lung cancer. New Engl. J. Med. 2024, 390, 1756–1769. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Zhang, W.; Wu, L.; Wang, W.; Zhang, P.; Fang, W.; Xing, W.; Chen, Q.; Yang, L.; Mei, J.; et al. Perioperative Toripalimab plus chemotherapy for patients with resectable non–small cell lung cancer. J. Am. Med. Assoc. 2024, 331, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Yue, D.; Wang, W.; Liu, H.; Chen, Q.; Chen, C.; Liu, L.; Zhang, P.; Zhao, G.; Yang, F.; Han, G.; et al. VP1-2024: Rationale-315: Event-free survival (EFS) and overall survival (OS) of Neoadjuvant tislelizumab (TIS) plus chemotherapy (CT) with adjuvant tis in resectable non-small cell lung cancer (NSCLC). Ann. Oncol. 2024, 35, 332–333. [Google Scholar] [CrossRef]
- Huang, J.; Osarogiagbon, R.U.; Giroux, D.J.; Nishimura, K.K.; Bille, A.; Cardillo, G.; Detterbeck, F.; Kernstine, K.; Kim, H.K.; Lievens, Y.; et al. The International Association for the Study of Lung Cancer Staging Project for Lung Cancer: Proposals for the revision of the N descriptors in the forthcoming ninth edition of the TNM classification for Lung Cancer. J. Thorac. Oncol. 2023, 19, 766–785. [Google Scholar] [CrossRef]
- Lababede, O.; Meziane, M.A. The eighth edition of TNM staging of lung cancer: Reference Chart and diagrams. Oncologist 2018, 23, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Rusch, V.W.; Asamura, H.; Watanabe, H.; Giroux, D.J.; Rami-Porta, R.; Goldstraw, P. The IASLC lung cancer staging project. A proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J. Thorac. Oncol. 2009, 4, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Putora, P.M.; Leskow, P.; McDonald, F.; Batchelor, T.; Evison, M. International guidelines on stage III N2 nonsmall cell lung cancer: Surgery or radiotherapy? ERJ Open Res. 2020, 6, 00159. [Google Scholar] [CrossRef] [PubMed]
- De Leyn, P.; Dooms, C.; Kuzdzal, J.; Lardinois, D.; Passlick, B.; Rami-Porta, R.; Turna, A.; Schil, P.V.; Venuta, F.; Waller, D.; et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur. J. Cardiothorac. Surg. 2014, 45, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Evison, M. The current treatment landscape in the UK for stage III NSCLC. Br. J. Cancer 2020, 123, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Asamura, H.; Chansky, K.; Crowley, J.; Goldstraw, P.; Rusch, V.W.; Vansteenkiste, J.F.; Watanabe, H.; Wu, Y.-L.; Zielinski, M.; Ball, D.; et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the revision of the N descriptors in the forthcoming 8th edition of the TNM Classification for lung cancer. J. Thorac. Oncol. 2015, 10, 1675–1684. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. NCCN Guidelines for Non-Small Cell Lung Cancer. Non-Small Cell Lung Cancer, version 3.2024. Available online: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf (accessed on 20 March 2024).
- Schmidt-Hansen, M.; Baldwin, D.R.; Hasler, E.; Zamora, J.; Abraira, V.; Roqué, I. PET-CT for assessing mediastinal lymph node involvement in patients with suspected resectable non-small cell lung cancer. Cochrane Database Syst. Rev. 2014, 2014, CD009519. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Lee, K.S.; Kim, B.; Choi, J.Y.; Kim, H.; Kwon, O.J.; Shim, Y.M.; A Yi, C.; Kim, H.Y.; Chung, M.J. Mediastinal nodal staging of Nonsmall cell lung cancer using integrated 18F-FDG PET/CT in a tuberculosis-endemic country. Cancer 2007, 109, 1068–1077. [Google Scholar] [CrossRef] [PubMed]
- Kameyama, K.; Imai, K.; Ishiyama, K.; Takashima, S.; Kuriyama, S.; Atari, M.; Ishii, Y.; Kobayashi, A.; Takahashi, S.; Kobayashi, M.; et al. New PET/CT criterion for predicting lymph node metastasis in resectable advanced (stage IB-III) lung cancer: The standard uptake values ratio of ipsilateral/contralateral hilar nodes. Thorac. Cancer 2022, 13, 708–715. [Google Scholar] [CrossRef]
- Kim, H.K.; Jeon, Y.J.; Um, S.-W.; Shin, S.H.; Jeong, B.-H.; Lee, K.; Kim, H.; Lee, H.Y.; Kim, T.J.; Lee, K.S.; et al. Role of invasive mediastinal nodal staging in survival outcomes of patients with non-small cell lung cancer and without radiologic lymph node metastasis: A retrospective cohort study. eClinicalMedicine 2024, 69, 102478. [Google Scholar] [CrossRef]
- Vilmann, P.; Clementsen, P.F.; Colella, S.; Siemsen, M.; De Leyn, P.; Dumonceau, J.-M.; Herth, F.J.; Larghi, A.; Vasquez-Sequeiros, E.; Hassan, C.; et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ests). Endoscopy 2015, 47, 545–559. [Google Scholar] [CrossRef] [PubMed]
- Annema, J.T.; van Meerbeeck, J.P.; Rintoul, R.C.; Dooms, C.; Deschepper, E.; Dekkers, O.M.; Leyn, P.D.; Braun, J.; Carroll, N.R.; Praet, M.; et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: A randomized trial. J. Am. Med. Assoc. 2010, 304, 2245–2252. [Google Scholar] [CrossRef] [PubMed]
- Bousema, J.E.; Dijkgraaf, M.G.; van der Heijden, E.H.; Verhagen, A.F.; Annema, J.T.; Broek, F.J.v.D.; Papen-Botterhuis, N.E.; Soud, M.Y.-E.; van Boven, W.J.; Daniels, J.M.; et al. Endosonography with or without confirmatory Mediastinoscopy for resectable lung cancer: A randomized clinical trial. J. Clin. Oncol. 2023, 41, 3805. [Google Scholar] [CrossRef] [PubMed]
- Farjah, F. Tradeoffs of proceeding to resection rather than mediastinoscopy after negative endosonography. J. Clin. Oncol. 2023, 41, 3782–3784. [Google Scholar] [CrossRef]
- Steinfort, D.P.; Kothari, G.; Wallace, N.; Hardcastle, N.; Rangamuwa, K.; Dieleman, E.M.T.; Lee, P.; Li, P.; A Simpson, J.; Yo, S.; et al. Systematic endoscopic staging of Mediastinum to guide radiotherapy planning in patients with locally advanced non-small-cell lung cancer (seismic): An international, Multicentre, single-arm, clinical trial. Lancet Respir. Med. 2024, 12, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Albain, K.S.; Swann, R.S.; Rusch, V.W.; Turrisi, A.T., 3rd; A Shepherd, F.A.; Smith, C.; Chen, Y.; Livingston, R.B.; Feins, R.H.; Gandara, D.R.; et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: A phase III randomised controlled trial. Lancet 2009, 374, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Xenophontos, E.; Levra, N.G.; Durieux, V.; Van Geffen, W.; Grisay, G.; Alonso, C.D.l.P.; Esteban, H.A.; Prisciandaro, E.; Ferrara, R.; Derks, J.; et al. P1.28-08 definition of resectable stage III non-small cell lung cancer: A systematic review from Eortc Lung Cancer Group. J. Thorac. Oncol. 2023, 18, S292. [Google Scholar] [CrossRef]
- Houda, I.; Bahce, I.; Dickhoff, C.; Kroese, T.; Kroeze, S.; Mariolo, A.; Tagliamento, M.; Moliner, L.; Brandao, M.; Edwards, J.; et al. OA06.03 An International EORTC Survey on Resectability of Stage III Non-small Cell Lung Cancer. J. Thorac. Oncol. 2023, 18, S55–S56. [Google Scholar] [CrossRef]
- Brandao, M.; Prisciandaro, E.; Xenophontos, E.; Mariolo, A.; Sadeghi, A.; Filippi, A.; Levy, A.; Bandura, A.; Caramella, C.; Dickhoff, C.; et al. P1.28-09 definition of Resectable Stage III non-small cell lung cancer (NSCLC): A clinical case review by a Pan-European expert panel. J. Thorac. Oncol. 2023, 18, S292–S293. [Google Scholar] [CrossRef]
- Dingemans, A.-M.; Remon, J.; Hendriks, L.; Edwards, J.; Faivre-Finn, C.; Reguart, N.; Smit, E.; Levy, A.; Sanchez, D.; Trujillo, J.; et al. OA06.05 consensual definition of Stage III NSCLC Resectability: EORTC-Lung Cancer Group initiative with other scientific societies. J. Thorac. Oncol. 2023, 18, S57–S58. [Google Scholar] [CrossRef]
- Shah, A.A.; Berry, M.F.; Tzao, C.; Gandhi, M.; Worni, M.; Pietrobon, R.; D’Amico, T.A. Induction chemoradiation is not superior to induction chemotherapy alone in Stage IIIA Lung Cancer. Ann. Thorac. Surg. 2012, 93, 1807–1812. [Google Scholar] [CrossRef] [PubMed]
- Song, W.-A.; Zhou, N.-K.; Wang, W.; Chu, X.-Y.; Liang, C.-Y.; Tian, X.-D.; Guo, J.-T.; Liu, X.; Liu, Y.; Dai, W.-M. Survival benefit of neoadjuvant chemotherapy in non-small cell lung cancer: An updated meta-analysis of 13 randomized control trials. J. Thorac. Oncol. 2010, 5, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Pignon, J.-P.; Tribodet, H.; Scagliotti, G.V.; Douillard, J.-Y.; Shepherd, F.A.; Stephens, R.J.; Dunant, A.; Torri, V.; Rosell, R.; Seymour, L.; et al. Lung adjuvant cisplatin evaluation: A pooled analysis by the LACE Collaborative Group. J. Clin. Oncol. 2008, 26, 3552–3559. [Google Scholar] [CrossRef]
- Forde, P.M.; Spicer, J.; Lu, S.; Provencio, M.; Mitsudomi, T.; Awad, M.M.; Felip, E.; Broderick, S.R.; Brahmer, J.R.; Swanson, S.J.; et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N. Engl. J. Med. 2022, 386, 1973–1985. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Zhao, J.; Gong, L.; Ni, Y.; Zhou, Y.; Tian, F.; Liu, H.; Gu, Z.; Huang, L.; Lu, Q.; et al. Neoadjuvant camrelizumab plus platinum-based chemotherapy vs chemotherapy alone for Chinese patients with Resectable Stage IIIA or IIIB (T3N2) non–small cell lung cancer. JAMA Oncol. 2023, 9, 1348. [Google Scholar] [CrossRef] [PubMed]
- Aredo, J.V.; Aredo, J.V.; Urisman, A.; Urisman, A.; Gubens, M.A.; Gubens, M.A.; Mulvey, C.; Mulvey, C.; Allen, G.M.; Allen, G.M.; et al. Phase II trial of neoadjuvant osimertinib for surgically resectable EGFR-mutated non-small cell lung cancer. J. Clin. Oncol. 2023, 41 (Suppl. S16), 8508. [Google Scholar] [CrossRef]
- Lv, C.; Fang, W.; Wu, N.; Jiao, W.; Xu, S.; Ma, H.; Wang, J.; Wang, R.; Ji, C.; Li, S.; et al. Osimertinib as neoadjuvant therapy in patients with EGFR-mutant Resectable Stage II-IIIB lung adenocarcinoma (NEOS): A multicenter, single-arm, open-label phase 2B trial. Lung Cancer 2023, 178, 151–156. [Google Scholar] [CrossRef]
- Tsuboi, M.; Weder, W.; Escriu, C.; Blakely, C.; He, J.; Dacic, S.; Yatabe, Y.; Zeng, L.; Walding, A.; Chaft, J.E. Neoadjuvant osimertinib with/without chemotherapy versus chemotherapy alone for EGFR-mutated resectable non-small-cell lung cancer: NeoADAURA. Future Oncol. 2021, 17, 4045–4055. [Google Scholar] [CrossRef]
- Paz-Ares, L.; O’Brien, M.; Mauer, M.; Dafni, U.; Oselin, K.; Havel, L.; Gonzalez, E.E.; Isla, D.; Martinez-Marti, A.; Faehling, M.; et al. VP3-2022: Pembrolizumab (pembro) versus placebo for early-stage non-small cell lung cancer (NSCLC) following complete resection and adjuvant chemotherapy (chemo) when indicated: Randomized, Triple-Blind, phase III EORTC-1416-LCG/ETOP 8-15—Pearls/keynote-091 study. Ann. Oncol. 2022, 33, 451–453. [Google Scholar] [CrossRef]
- Felip, E.; Altorki, N.; Zhou, C.; Csőszi, T.; Vynnychenko, I.; Goloborodko, O.; Luft, A.; Akopov, A.; Martinez-Marti, A.; Kenmotsu, H.; et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMPOWER010): A randomised, multicentre, open-label, phase 3 trial. Lancet 2021, 398, 1344–1357. [Google Scholar] [CrossRef]
- Wakelee, H.A.; Altorki, N.K.; Zhou, C.; Csőszi, T.; Vynnychenko, I.O.; Goloborodko, O.; Rittmeyer, A.; Reck, M.; Martinez-Marti, A.; Kenmotsu, H.; et al. IMPOWER010: Final disease-free survival (DFS) and Second overall survival (OS) interim results after ≥5 years of follow up of a phase III study of adjuvant atezolizumab vs best supportive care in resected stage IB-IIIA Non-small cell lung cancer (NSCLC). J. Clin. Oncol. 2024, 42 (Suppl. S17), LBA8035. [Google Scholar] [CrossRef]
- Zhong, W.-Z.; Wang, Q.; Mao, W.-M.; Xu, S.-T.; Wu, L.; Wei, Y.-C.; Liu, Y.-Y.; Chen, C.; Cheng, Y.; Yin, R.; et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for Stage II-IIIA (N1-N2) EGFR-mutant NSCLC: Final overall survival analysis of CTONG1104 phase III trial. J. Clin. Oncol. 2021, 39, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-L.; Tsuboi, M.; He, J.; John, T.; Grohe, C.; Majem, M.; Goldman, J.W.; Laktionov, K.; Kim, S.-W.; Kato, T.; et al. Osimertinib in resected EGFR-mutated non–small-cell lung cancer. N. Engl. J. Med. 2020, 383, 1711–1723. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, M.; Herbst, R.S.; John, T.; Kato, T.; Majem, M.; Grohé, C.; Wang, J.; Goldman, J.W.; Lu, S.; Su, W.-C.; et al. Overall survival with osimertinib in resected EGFR-mutated NSCLC. N. Engl. J. Med. 2023, 389, 137–147. [Google Scholar] [CrossRef]
- Solomon, B.; Ahn, J.; Dziadziuszko, R.; Barlesi, F.; Nishio, M.; Lee, D.; Lee, J.-S.; Zhong, W.-Z.; Horinouchi, H.; Mao, W.; et al. LBA2 ALINA: Efficacy and safety of adjuvant alectinib versus chemotherapy in patients with early-stage ALK+ non-small cell lung cancer (NSCLC). Ann. Oncol. 2023, 34, S1295–S1296. [Google Scholar] [CrossRef]
- Provencio, M.; Nadal, E.; González-Larriba, J.L.D.; Martínez-Martí, A.; Bernabé, R.; Bosch-Barrera, J.; Casal-Rubio, J.; Calvo, V.; Insa, A.; Ponce, S.; et al. Perioperative nivolumab and chemotherapy in stage III non–small-cell lung cancer. N. Engl. J. Med. 2023, 389, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Kato, T.; Dong, X.; Ahn, M.-J.; Quang, L.-V.; Soparattanapaisarn, N.; Inoue, T.; Wang, C.-L.; Huang, M.; Yang, J.C.-H.; et al. Osimertinib after Chemoradiotherapy in Stage III EGFR -Mutated NSCLC. N. Engl. J. Med. 2024. [Google Scholar] [CrossRef] [PubMed]
- Banna, G.L.; Hassan, M.A.; Signori, A.; Giunta, E.F.; Maniam, A.; Anpalakhan, S.; Acharige, S.; Ghose, A.; Addeo, A. Neoadjuvant Chemo-Immunotherapy for Early-Stage Non–Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2024, 7, e246837. [Google Scholar] [CrossRef] [PubMed]
- Serrano, J.; Crespo, P.C.; Taboada, B.; Gonzalez, A.A.; García, R.G.; Caamaño, A.G.; Reyes, J.C.T.; Rubio, X.M.; Couñago, F. Postoperative radiotherapy in resected non-small cell lung cancer: The never-ending story. World, J. Clin. Oncol. 2021, 12, 833–844. [Google Scholar] [CrossRef]
- Le Pechoux, C.; Pourel, N.; Barlesi, F.; Lerouge, D.; Antoni, D.; Lamezec, B.; Nestle, U.; Boisselier, P.; Dansin, E.; Paumier, A.; et al. Postoperative radiotherapy versus no postoperative radiotherapy in patients with completely resected non-small-cell lung cancer and proven mediastinal N2 involvement (Lung ART): An open-label, randomised, phase 3 trial. Lancet Oncol. 2022, 23, 104–114. [Google Scholar] [CrossRef]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; De Wit, M.; et al. Durvalumab after chemoradiotherapy in stage III non–small-cell lung cancer. N. Engl. J. Med. 2017, 377, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Filippi, A.; Bar, J.; Chouaid, C.; Christoph, D.; Field, J.; Fietkau, R.; Garassino, M.; Garrido, P.; Haakensen, V.; Kao, S.; et al. Real-world outcomes with durvalumab after chemoradiotherapy in patients with unresectable stage III NSCLC: Interim analysis of overall survival from Pacific-R. ESMO Open 2024, 9, 103464. [Google Scholar] [CrossRef] [PubMed]
- Senan, S.; Özgüroğlu, M.; Daniel, D.; Villegas, A.; Vicente, D.; Murakami, S.; Hui, R.; Faivre-Finn, C.; Paz-Ares, L.; Wu, Y.; et al. Outcomes with Durvalumab after chemoradiotherapy in Stage IIIA-N2 non-small-cell lung cancer: An exploratory analysis from the PACIFIC Trial. ESMO Open 2022, 7, 100410. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.; Sugawara, S.; Lee, K.; Ostoros, G.; Demirkazik, A.; Zemanova, M.; Sriuranpong, V.; Gelatti, A.; Menezes, J.; Zurawski, B.; et al. LBA1 durvalumab in combination with chemoradiotherapy for patients with unresectable stage III NSCLC: Final results from pacific-2. ESMO Open 2024, 9, 102986. [Google Scholar] [CrossRef]
- Herbst, R.S.; Majem, M.; Barlesi, F.; Carcereny, E.; Chu, Q.; Monnet, I.; Sanchez-Hernandez, A.; Dakhil, S.; Camidge, D.R.; Winzer, L.; et al. COAST: An open-label, phase II, Multidrug platform study of durvalumab alone or in combination with oleclumab or monalizumab in patients with unresectable, stage III non–small-cell lung cancer. J. Clin. Oncol. 2022, 40, 3383–3393. [Google Scholar] [CrossRef] [PubMed]
- Spicer, J.; Gao, S.; Liberman, M.; Kato, T.; Tsuboi, M.; Lee, S.-H.; Chen, K.-N.; Dooms, C.; Majem, M.; Eigendorff, E.; et al. LBA56 Overall survival in the KEYNOTE-671 study of perioperative pembrolizumab for early-stage non-small-cell lung cancer (NSCLC). Ann. Oncol. 2023, 34, S1297–S1298. [Google Scholar] [CrossRef]
- Spigel, D.R.; Faivre-Finn, C.; Gray, J.E.; Vicente, D.; Planchard, D.; Paz-Ares, L.; Vansteenkiste, J.F.; Garassino, M.C.; Hui, R.; Quantin, X.; et al. Five-year survival outcomes from the PACIFIC trial: Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. J. Clin. Oncol. 2022, 40, 1301–1311. [Google Scholar] [CrossRef]
- Tagliamento, M.; Morfouace, M.; Loizides, C.; Oliveira, J.; Greillier, L.; Raimbourg, J.; Toffart, A.-C.; Chatellier, T.; Cloarec, N.; Sullivan, I.; et al. EORTC-Specta Arcagen Study, comprehensive genomic profiling and treatment adaptation of rare thoracic cancers. Npj Precis. Oncol. 2024, 8, 37. [Google Scholar] [CrossRef] [PubMed]
- van Meerbeeck, J.P.; Kramer, G.W.P.M.; Van Schil, P.E.Y.; Legrand, C.; Smit, E.F.; Schramel, F.; Tjan-Heijnen, V.C.; Biesma, B.; Debruyne, C.; van Zandwijk, N.; et al. Randomized controlled trial of resection versus radiotherapy after induction chemotherapy in Stage IIIA-N2 non-small-cell lung cancer. J. Natl. Cancer Inst. 2007, 99, 442–450. [Google Scholar] [CrossRef]
- Study to Assess Neoadjuvant Durvalumab (D) and Platinum-Based Chemotherapy (CT), Followed by Either Surgery and Adjuvant D or CRT and Consolidation D, in Resectable or Borderline Resectable Stage IIB-IIIB NSCLC (MDT-Bridge)—Full Text View (No Date) ClinicalTrials.gov. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT05925530 (accessed on 12 May 2024).
- Leonetti, A.; Minari, R.; Boni, L.; Gnetti, L.; Verzè, M.; Ventura, L.; Musini, L.; Tognetto, M.; Tiseo, M. Phase II, open-label, single-arm, multicenter study to assess the activity and safety of alectinib as neoadjuvant treatment in surgically resectable stage III ALK-positive NSCLC: ALNEO trial. Clin. Lung Cancer 2021, 22, 473–477. [Google Scholar] [CrossRef]
- A Study of Multiple Therapies in Biomarker-Selected Patients with Resectable Stages IB-III Non-Small Cell Lung Cancer [Internet]. Available online: https://clinicaltrials.gov/study/NCT04302025 (accessed on 11 May 2024).
- Forde, P.M.; Spicer, J.; Girard, N.; Provencio, M.; Lu, S.; Wang, C.; Awad, M.; Mitsudomi, T.; Felip, E.; Swanson, S.J.; et al. 84O-Neoadjuvant nivolumab (N) + platinum-doublet chemotherapy (C) for resectable NSCLC: 3-y update from CheckMate 816J. Thorac. Oncol. 2023, 18, S89–S100. [Google Scholar] [CrossRef]
- Tie, J.; Tie, J.; Cohen, J.D.; Cohen, J.D.; Lahouel, K.; Lahouel, K.; Lo, S.N.; Lo, S.N.; Wang, Y.; Wang, Y.; et al. Circulating tumor DNA analysis guiding adjuvant therapy in stage II colon cancer. N. Engl. J. Med. 2022, 386, 2261–2272. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.-A.; Ku, B.M.; Kim, Y.J.; Park, S.; Sun, J.-M.; Lee, S.-H.; Ahn, J.S.; Cho, J.H.; Kim, H.K.; Choi, Y.S.; et al. Longitudinal monitoring of circulating tumor DNA from plasma in patients with curative resected stages I to IIIA EGFR-mutant non-small cell lung cancer. J. Thorac. Oncol. 2023, 18, 1199–1208. [Google Scholar] [CrossRef]
- Molecular Residual Disease (MRD) Analysis from the ADAURA Trial of Adjuvant (adj) Osimertinib in Patients (pts) with Resected EGFR-Mutated (EGFRm) Stage IB–IIIA Non-Small Cell Lung Cancer (NSCLC) [Internet]. Available online: https://ascopubs.org/doi/10.1200/JCO.2024.42.16_suppl.8005 (accessed on 1 June 2024).
- Reck, M.; Gale, D.; Harpole, D.; Taube, J.; Mitsudomi, T.; Hochmair, M.; Winder, T.; Zhu, Z.; Lai, Z.; Stewart, R.; et al. Associations of ctdna clearance and pathological response with neoadjuvant treatment in patients with resectable NSCLC from the phase III aegean trial. Ann. Oncol. 2023, 34, S1300. [Google Scholar] [CrossRef]
| pCR Rate—% (95% CI) | EFS/DFS/PFS—Median (95% CI) & HR (95% CI) | OS—Median (95% CI) & HR (95% CI) | Surgical Outcomes | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Trial Name | Treatment Arms | All Patients | N2/Stage III * | End-Point | All Patients | N2/Stage III * | All Patients | N2/Stage III * | R0 § | Did Not Complete Surgery |
| AEGEAN [5] | CT + Durvalumab | 17.2% (13.5–21.5) | All N2: NA Single-N2: 18.4% (12.4–25.8) Multi-N2: 8.8 (1.9–23.7) | EFS | NR (31.9-NR) vs. 25.9 (18.9-NR) HR 0.68 (0.53–0.88) | All N2: NA Single-N2: NR (NR-NR) vs. 22.8 (12.6-NR) HR 0.61 (0.39-0.94) Multi-N2: 31.9 (9.3-NR) vs. 12.2 (7.2-NR) HR 0.69 (0.33–1.38) | NA | NA | 950% | 22% |
| CT + Placebo | 4.3% (2.5–6.9) | All N2: NA Single-N2: 4.5% (1.7–9.6) Multi-N2: 5.0% (0.6-16.9) | NA | NA | 91% | 23% | ||||
| KEYNOTE 671 [6,48] | CT + Pembrolizumab | 18.1% (14.5–22.3) | NA | EFS | 47.2 (32.9-NR) vs. 18.3 (14.8–22.1) HR 0.59 (0.48–0.72) | All N2: NA. HR 0.63 (0.48–0.82) | NR (NR-NR) vs. 52.4 (45.7–NR) HR 0.72 (0.56–0.93) | All N2: NA. HR 0.74 (0.52–1.07) | 92% | 18% |
| CT + Placebo | 4.0% (2.3–6.4) | 840% | 21% | |||||||
| Checkmate 77T [7] | CT + Nivolumab | 25.3% (19.8–31.5) | All N2: 22.0% (14.0–31.9) Single-N2: 18.6% (9.7–30.9) Multi-N2: 29.0% (14.2–48.0) | EFS | NR (28.9-NR) vs. 18.4 (13.6–28.1) HR 0.58 (0.42–0.81) | All N2: 30.2 (26.9-NR) vs. 10.0 (8.1–15.1) HR 0.46 (0.30–0.70) Single-N2: 30.2 (26.9-NR) vs. 10.0 (8.1–15.1) HR 0.49 (0.29–0.84) Multi-N2: NR (13.2-NR) vs. 10.0 (8.0–18.8) HR 0.43 (0.21–0.88) | NA | NA | 89% | 22% |
| CT + Placebo | 4.7% (2.4–8.3) | All N2: 5.6% (1.8–12.5) Single N2: 7.5% (2.1–18.2) Multi-N2: 2.7% (0.1–14.2) | NA | NA | 90% | 23% | ||||
| Neotorch [8] | CT + Toripalimab | 24.8% (19.0–31.3) | Stage III: 24.8% | EFS | NE (24.4-NE) vs. 15.1 (10.6–21.9) HR 0.40 (0.28–0.57) | Stage III: NE (NE-NE) vs. 15.5 (9.9–NE) HR 0.40 (0.27–0.57) | NE (NE-NE) vs. 30.4 (29.2-NE) HR 0.62 (0.38–0.999) | NA | 96% | NA |
| CT + Placebo | 1.0% (0.1%–3.5% | Stage III: 1.0% | 93% | NA | ||||||
| Rationale 315 [9] | CT + Tislelizumab | 40.7% | NA | EFS | NR vs. NR HR 0.56 (0.40–0.79) | Stage III: NR (29.6-NE) vs. 19.8 (13.1-NE) HR 0.62 (0.42–0.94) | NR (NR-NR) vs. NR (35.0-NE) HR 0.62 (0.39–0.98) | NA | NA | 16% |
| CT + Placebo | 5.7% | NA | NA | NA | 24% | |||||
| NADIM II [47] | CT + Nivolumab | 37% | Single-N2†: 42.1% (19.9–64.3) Multi-N2: 36.4% (16.3–56.5) | PFS | NR (27.6–NR) vs. 15.4 (10.6–NR) HR 0.47 95% CI 0.25–0.88 | All N2: NA Single N2: NA. HR 2.43 (0.3–19.46) Multi-N2: NA. HR 0.39 (0.16–0.94) | NR (33.5-NR) vs. NR (21.1-NR) HR 0.43 (0.19–0.98) | All N2: NA Single-N2: NA. HR NE Multi-N2: NA. HR 0.30 (0.09–1.07) | 94% | 7% |
| CT + BSC | 7% | Single-N2†: 0% (0–0) Multi-N2: 10% (-8.6–28.6) | 85% | 31% | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Linares Díaz, J.; Edwards, J.; Deleu, A.-L.; Giaj-Levra, N.; Prisciandaro, E.; Roch, B.; Paesmans, M.; Berghmans, T.; Brandão, M. What Does N2 Lymph Node Involvement Mean for Patients with Non-Small Cell Lung Cancer (NSCLC)?—A Review of Implications for Diagnosis and Treatment. Cancers 2024, 16, 2673. https://doi.org/10.3390/cancers16152673
Linares Díaz J, Edwards J, Deleu A-L, Giaj-Levra N, Prisciandaro E, Roch B, Paesmans M, Berghmans T, Brandão M. What Does N2 Lymph Node Involvement Mean for Patients with Non-Small Cell Lung Cancer (NSCLC)?—A Review of Implications for Diagnosis and Treatment. Cancers. 2024; 16(15):2673. https://doi.org/10.3390/cancers16152673
Chicago/Turabian StyleLinares Díaz, Julio, John Edwards, Anne-Leen Deleu, Niccolo Giaj-Levra, Elena Prisciandaro, Benoit Roch, Marianne Paesmans, Thierry Berghmans, and Mariana Brandão. 2024. "What Does N2 Lymph Node Involvement Mean for Patients with Non-Small Cell Lung Cancer (NSCLC)?—A Review of Implications for Diagnosis and Treatment" Cancers 16, no. 15: 2673. https://doi.org/10.3390/cancers16152673
APA StyleLinares Díaz, J., Edwards, J., Deleu, A.-L., Giaj-Levra, N., Prisciandaro, E., Roch, B., Paesmans, M., Berghmans, T., & Brandão, M. (2024). What Does N2 Lymph Node Involvement Mean for Patients with Non-Small Cell Lung Cancer (NSCLC)?—A Review of Implications for Diagnosis and Treatment. Cancers, 16(15), 2673. https://doi.org/10.3390/cancers16152673







