Exposure to Light at Night and Risk of Cancer: A Systematic Review, Meta-Analysis, and Data Synthesis
Abstract
Simple Summary
Abstract
1. Introduction
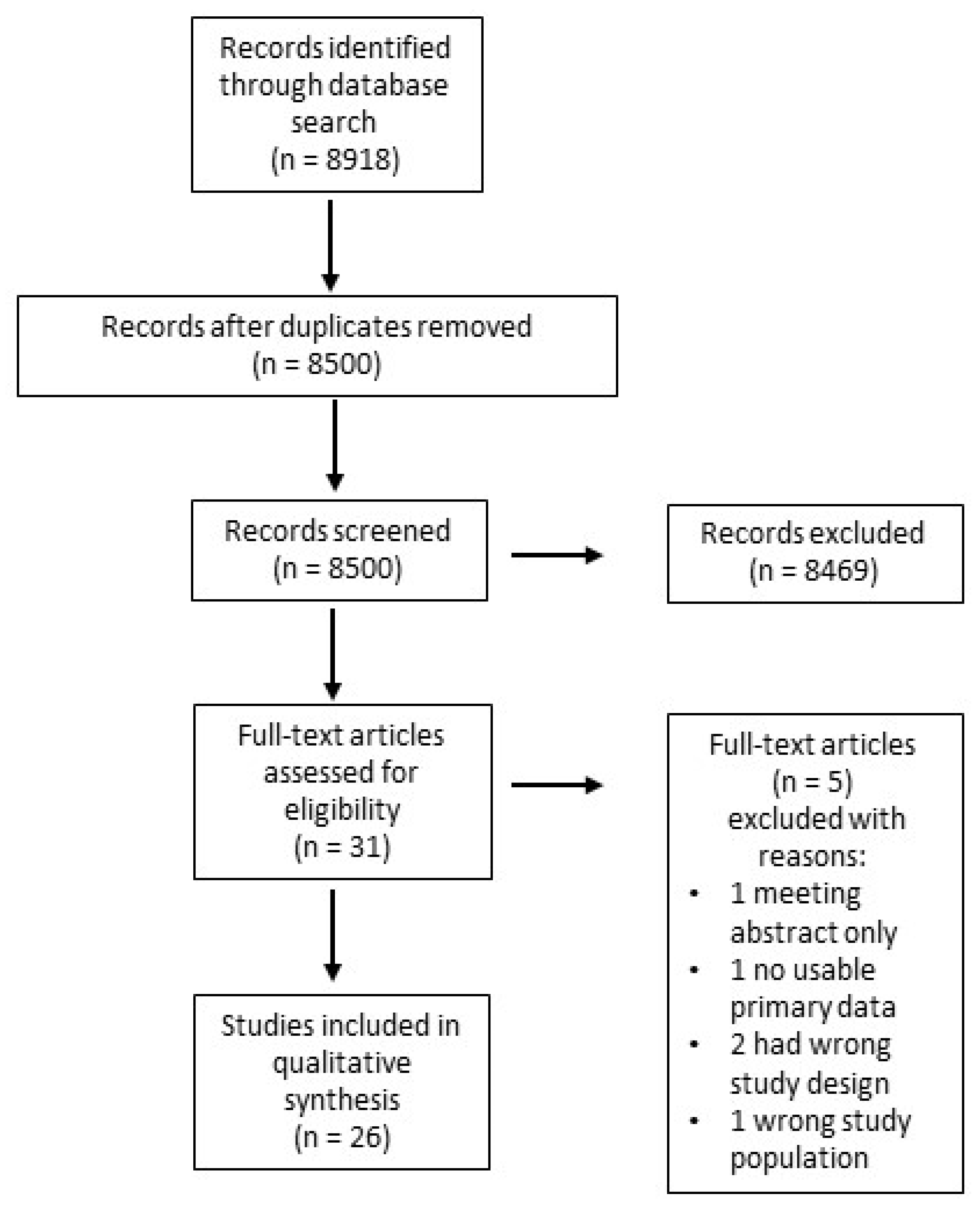
2. Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
2.6. Data Synthesis
3. Results
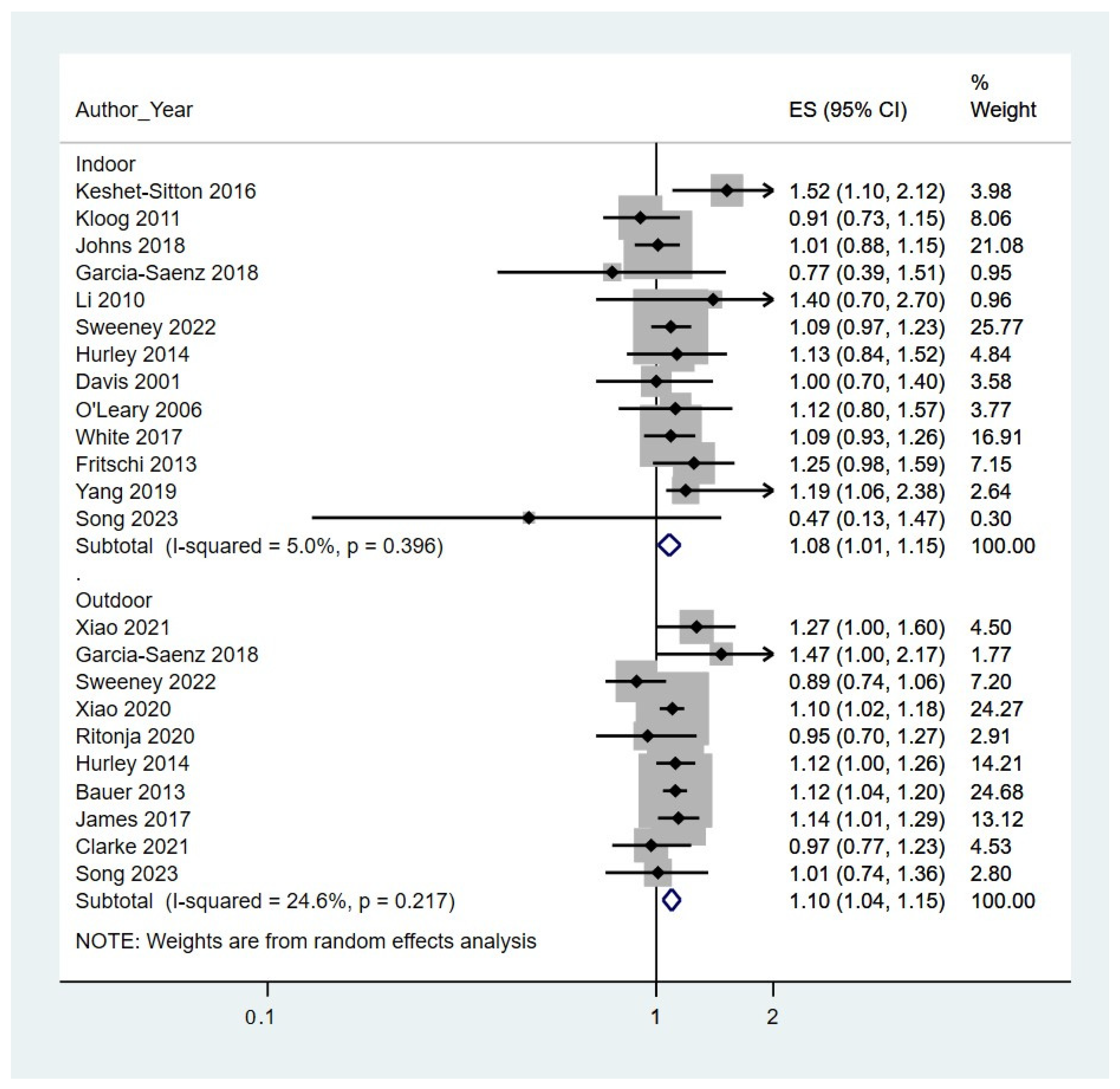
3.1. Meta-Analysis of LAN and Risk of Breast Cancer
3.2. Other Cancers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; Xu, R.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019 A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022, 8, 420–444. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Danaei, G.; Vander Hoorn, S.; Lopez, A.D.; Murray, C.J.L.; Ezzati, M. Causes of cancer in the world: Comparative risk assessment of nine behavioural and environmental risk factors. Lancet 2005, 366, 1784–1793. [Google Scholar] [CrossRef]
- Giovannucci, E. Modifiable risk factors for colon cancer. Gastroenterol. Clin. N. Am. 2002, 31, 925–943. [Google Scholar] [CrossRef]
- Papadimitriou, N.; Markozannes, G.; Kanellopoulou, A.; Critselis, E.; Alhardan, S.; Karafousia, V.; Kasimis, J.C.; Katsaraki, C.; Papadopoulou, A.; Zografou, M.; et al. An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites. Nat. Commun. 2021, 12, 4579. [Google Scholar] [CrossRef]
- Rojas, K.; Stuckey, A. Breast Cancer Epidemiology and Risk Factors. Clin. Obstet. Gynecol. 2016, 59, 651–672. [Google Scholar] [CrossRef]
- Islami, F.; Goding Sauer, A.; Miller, K.D.; Siegel, R.L.; Fedewa, S.A.; Jacobs, E.J.; McCullough, M.L.; Patel, A.V.; Ma, J.; Soerjomataram, I.; et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J. Clin. 2018, 68, 31–54. [Google Scholar] [CrossRef]
- Friedenreich, C.M.; Ryder-Burbidge, C.; McNeil, J. Physical activity, obesity and sedentary behavior in cancer etiology: Epidemiologic evidence and biologic mechanisms. Mol. Oncol. 2021, 15, 790–800. [Google Scholar] [CrossRef]
- Leung, L.; Lavoué, J.; Siemiatycki, J.; Guénel, P.; Koushik, A. Occupational environment and ovarian cancer risk. Occup. Environ. Med. 2023, 80, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Johnsson, A.; Broberg, P.; Johnsson, A.; Tornberg, Å.B.; Olsson, H. Occupational sedentariness and breast cancer risk. Acta Oncol. 2017, 56, 75–80. [Google Scholar] [CrossRef]
- Falchi, F.; Cinzano, P.; Duriscoe, D.; Kyba, C.C.M.; Elvidge, C.D.; Baugh, K.; Portnov, B.A.; Rybnikova, N.A.; Furgoni, R. The new world atlas of artificial night sky brightness. Sci. Adv. 2016, 2, e1600377. [Google Scholar] [CrossRef]
- Blair, A.; Blask, D.; Bråtveit, M.; IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Painting, firefighting, and shiftwork. IARC Monogr. Eval. Carcinog. Risks Hum. 2010, 98, 9–764. [Google Scholar]
- Fritschi, L.; Glass, D.C.; Heyworth, J.S.; Aronson, K.; Girschik, J.; Boyle, T.; Grundy, A.; Erren, T. Hypotheses for mechanisms linking shiftwork and cancer. Med. Hypotheses 2011, 77, 430–436. [Google Scholar] [CrossRef]
- Rumanova, V.S.; Okuliarova, M.; Zeman, M. Differential effects of constant light and dim light at night on the circadian control of metabolism and behavior. Int. J. Mol. Sci. 2020, 21, 5478. [Google Scholar] [CrossRef]
- Anisimov, V.N.; Baturin, D.A.; Popovich, I.G.; Zabezhinski, M.A.; Manton, K.G.; Semenchenko, A.V.; Yashin, A.I. Effect of exposure to light-at-night on life span and spontaneous carcinogenesis in female CBA mice. Int. J. Cancer 2004, 111, 475–479. [Google Scholar] [CrossRef]
- Chang, A.M.; Aeschbach, D.; Duffy, J.F.; Czeisler, C.A. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc. Natl. Acad. Sci. USA 2015, 112, 1232–1237. [Google Scholar] [CrossRef]
- Urbano, T.; Vinceti, M.; Wise, L.A.; Filippini, T. Light at night and risk of breast cancer: A systematic review and dose–response meta-analysis. Int. J. Health Geogr. 2021, 20, 44. [Google Scholar] [CrossRef]
- Lai, K.Y.; Sarkar, C.; Ni, M.Y.; Cheung, L.W.T.; Gallacher, J.; Webster, C. Exposure to light at night (LAN) and risk of breast cancer: A systematic review and meta-analysis. Sci. Total Environ. 2021, 762, 143159. [Google Scholar] [CrossRef]
- Wu, Y.; Gui, S.Y.; Fang, Y.; Zhang, M.; Hu, C.Y. Exposure to outdoor light at night and risk of breast cancer: A systematic review and meta-analysis of observational studies. Environ. Pollut. 2021, 269, 116114. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. J. Am. Med. Assoc. 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Morgan, R.L.; Thayer, K.A.; Santesso, N.; Holloway, A.C.; Blain, R.; Eftim, S.E.; Goldstone, A.E.; Ross, P.; Ansari, M.; Akl, E.A.; et al. A risk of bias instrument for non-randomized studies of exposures: A users’ guide to its application in the context of GRADE. Environ. Int. 2019, 122, 168–184. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- James, P.; Bertrand, K.A.; Hart, J.E.; Schernhammer, E.S.; Tamimi, R.M.; Laden, F. Outdoor Light at Night and Breast Cancer Incidence in the Nurses’ Health Study II. Environ. Health Perspect. 2017, 125, 087010. [Google Scholar] [CrossRef]
- Xiao, Q.; Gierach, G.L.; Bauer, C.; Blot, W.J.; James, P.; Jones, R.R. The Association between Outdoor Artificial Light at Night and Breast Cancer Risk in Black and White Women in the Southern Community Cohort Study. Environ. Health Perspect. 2021, 129, 87701. [Google Scholar] [CrossRef]
- Xiao, Q.; James, P.; Breheny, P.; Jia, P.; Park, Y.; Zhang, D.; Fisher, J.A.; Ward, M.H.; Jones, R.R. Outdoor light at night and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Int. J. Cancer 2020, 147, 2363–2372. [Google Scholar] [CrossRef]
- Ritonja, J.; McIsaac, M.A.; Sanders, E.; Kyba, C.C.M.; Grundy, A.; Cordina-Duverger, E.; Spinelli, J.J.; Aronson, K.J. Outdoor light at night at residences and breast cancer risk in Canada. Eur. J. Epidemiol. 2020, 35, 579–589. [Google Scholar] [CrossRef]
- Bauer, S.E.; Wagner, S.E.; Burch, J.; Bayakly, R.; Vena, J.E. A case-referent study: Light at night and breast cancer risk in Georgia. Int. J. Health Geogr. 2013, 12, 23. [Google Scholar] [CrossRef]
- Hurley, S.; Goldberg, D.; Nelson, D.; Hertz, A.; Horn-Ross, P.L.; Bernstein, L.; Reynolds, P. Light at Night and Breast Cancer Risk Among California Teachers. Epidemiology 2014, 25, 697–706. [Google Scholar] [CrossRef]
- Sweeney, M.R.; Nichols, H.B.; Jones, R.R.; Olshan, A.F.; Keil, A.P.; Engel, L.S.; James, P.; Jackson, C.L.; Sandler, D.P.; White, A.J. Light at night and the risk of breast cancer: Findings from the Sister study. Environ. Int. 2022, 169, 107495. [Google Scholar] [CrossRef]
- White, A.J.; Weinberg, C.R.; Park, Y.; D’Aloisio, A.A.; Vogtmann, E.; Nichols, H.B.; Sandler, D.P. Sleep characteristics, light at night and breast cancer risk in a prospective cohort. Int. J. Cancer 2017, 141, 2204–2214. [Google Scholar] [CrossRef]
- Li, Q.; Zheng, T.; Holford, T.R.; Boyle, P.; Zhang, Y.; Dai, M. Light at night and breast cancer risk: Results from a population-based case–control study in Connecticut, USA. Cancer Causes Control 2010, 21, 2281–2285. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, E.S.; Schoenfeld, E.R.; Stevens, R.G.; Kabat, G.C.; Henderson, K.; Grimson, R.; Gammon, M.D.; Leske, M.C. Shift Work, Light at Night, and Breast Cancer on Long Island, New York. Am. J. Epidemiol. 2006, 164, 358–366. [Google Scholar] [CrossRef]
- Davis, S.; Mirick, D.K.; Stevens, R.G. Night Shift Work, Light at Night, and Risk of Breast Cancer. JNCI J. Natl. Cancer Inst. 2001, 93, 1557–1562. [Google Scholar] [CrossRef]
- Medgyesi, D.N.; Trabert, B.; Fisher, J.A.; Xiao, Q.; James, P.; White, A.J.; Madrigal, J.M.; Jones, R.R. Outdoor light at night and risk of endometrial cancer in the NIH-AARP diet and health study. Cancer Causes Control 2023, 34, 181–187. [Google Scholar] [CrossRef]
- Park, Y.; Ramirez, Y.; Xiao, Q.; Liao, L.M.; Jones, G.S.; McGlynn, K.A. Outdoor light at night and risk of liver cancer in the NIH-AARP diet and health study. Cancer Causes Control. 2022, 33, 1215–1218. [Google Scholar] [CrossRef]
- Zhang, D.; Jones, R.R.; James, P.; Kitahara, C.M.; Xiao, Q. Associations between artificial light at night and risk for thyroid cancer: A large US cohort study. Cancer 2021, 127, 1448–1458. [Google Scholar] [CrossRef]
- Xiao, Q.; Jones, R.R.; James, P.; Stolzenberg-Solomon, R.Z. Light at Night and Risk of Pancreatic Cancer in the NIH-AARP Diet and Health Study. Cancer Res. 2021, 81, 1616–1622. [Google Scholar] [CrossRef] [PubMed]
- Zhong, C.; Franklin, M.; Wiemels, J.; McKean-Cowdin, R.; Chung, N.T.; Benbow, J.; Wang, S.S.; Lacey, J.V.; Longcore, T. Outdoor artificial light at night and risk of non-Hodgkin lymphoma among women in the California Teachers Study cohort. Cancer Epidemiol. 2020, 69, 101811. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Shi, Y.; Ke, X.; Sun, H.; Guo, J.; Wang, X. Long-term sleep habits and the risk of breast cancer among Chinese women: A case–control study. Eur. J. Cancer Prev. 2019, 28, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Lei, L.; Zhang, R.; Liu, H.; Du, J.; Li, N.; Chen, W.; Peng, J.; Ren, J. Circadian Disruption and Breast Cancer Risk: Evidence from a Case-Control Study in China. Cancers 2023, 15, 419. [Google Scholar] [CrossRef] [PubMed]
- Keshet-Sitton, A.; Or-Chen, K.; Yitzhak, S.; Tzabary, I.; Haim, A. Can Avoiding Light at Night Reduce the Risk of Breast Cancer? Integr. Cancer Ther. 2016, 15, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Kloog, I.; Portnov, B.A.; Rennert, H.S.; Haim, A. Does the Modern Urbanized Sleeping Habitat Pose a Breast Cancer Risk? Chronobiol. Int. 2011, 28, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Saenz, A.; Sánchez de Miguel, A.; Espinosa, A.; Valentin, A.; Aragonés, N.; Llorca, J.; Amiano, P.; Sánchez, V.M.; Guevara, M.; Capelo, R.; et al. Evaluating the Association between Artificial Light-at-Night Exposure and Breast and Prostate Cancer Risk in Spain (MCC-Spain Study). Environ. Health Perspect. 2018, 126, 047011. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Saenz, A.; de Miguel, A.S.; Espinosa, A.; Costas, L.; Aragonés, N.; Tonne, C.; Moreno, V.; Pérez-Gómez, B.; Valentin, A.; Pollán, M.; et al. Association between Outdoor Light-at-night Exposure and Colorectal Cancer in Spain. Epidemiology 2020, 31, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Johns, L.E.; Jones, M.E.; Schoemaker, M.J.; McFadden, E.; Ashworth, A.; Swerdlow, A.J. Domestic light at night and breast cancer risk: A prospective analysis of 105 000 UK women in the Generations Study. Br. J. Cancer 2018, 118, 600–606. [Google Scholar] [CrossRef]
- Clarke, R.B.; Amini, H.; James, P.; von Euler-Chelpin, M.; Jørgensen, J.T.; Mehta, A.; Cole-Hunter, T.; Westendorp, R.; Mortensen, L.H.; Loft, S.; et al. Outdoor light at night and breast cancer incidence in the Danish Nurse Cohort. Environ. Res. 2021, 194, 110631. [Google Scholar] [CrossRef] [PubMed]
- Walasa, W.M.; Carey, R.N.; Si, S.; Fritschi, L.; Heyworth, J.S.; Fernandez, R.C.; Boyle, T. Association between shiftwork and the risk of colorectal cancer in females: A population-based case–control study. Occup. Environ. Med. 2018, 75, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Fritschi, L.; Erren, T.C.; Glass, D.C.; Girschik, J.; Thomson, A.K.; Saunders, C.; Boyle, T.; El-Zaemey, S.; Rogers, P.; Peters, S.; et al. The association between different night shiftwork factors and breast cancer: A case–control study. Br. J. Cancer 2013, 109, 2472–2480. [Google Scholar] [CrossRef]
- Zare Sakhvidi, M.J.; Lequy, E.; Goldberg, M.; Jacquemin, B. Air pollution exposure and bladder, kidney and urinary tract cancer risk: A systematic review. Environ. Pollut. 2020, 267, 115328. [Google Scholar] [CrossRef]
- Hamra, G.B.; Guha, N.; Cohen, A.; Laden, F.; Raaschou-Nielsen, O.; Samet, J.M.; Vineis, P.; Forastiere, F.; Saldiva, P.; Yorifuji, T.; et al. Outdoor Particulate Matter Exposure and Lung Cancer: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2014, 122, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Mok, Y.; Jeon, C.; Jee, S.H.; Samet, J.M. Tuberculosis, smoking and risk for lung cancer incidence and mortality. Int. J. Cancer 2016, 139, 2447–2455. [Google Scholar] [CrossRef] [PubMed]
- Macacu, A.; Autier, P.; Boniol, M.; Boyle, P. Active and passive smoking and risk of breast cancer: A meta-analysis. Breast Cancer Res. Treat. 2015, 154, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Koo, Y.S.; Song, J.Y.; Joo, E.Y.; Lee, H.-J.; Lee, E.; Lee, S.-K.; Jung, K.-Y. Outdoor artificial light at night, obesity, and sleep health: Cross-sectional analysis in the KoGES study. Chronobiol. Int. 2016, 33, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Obayashi, K.; Yamagami, Y.; Kurumatani, N.; Saeki, K. Bedroom lighting environment and incident diabetes mellitus: A longitudinal study of the HEIJO-KYO cohort. Sleep Med. 2020, 65, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Russart, K.L.G.; Nelson, R.J. Light at night as an environmental endocrine disruptor. Physiol. Behav. 2018, 190, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.R.; Olmstead, R.; Carroll, J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef]
- Castanon-Cervantes, O.; Wu, M.; Ehlen, J.C.; Paul, K.; Gamble, K.L.; Johnson, R.L.; Besing, R.C.; Menaker, M.; Gewirtz, A.T.; Davidson, A.J. Dysregulation of Inflammatory Responses by Chronic Circadian Disruption. J. Immunol. 2010, 185, 5796–5805. [Google Scholar] [CrossRef] [PubMed]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef]
- Masri, S.; Sassone-Corsi, P. The emerging link between cancer, metabolism, and circadian rhythms. Nat. Med. 2018, 24, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Kettner, N.M.; Voicu, H.; Finegold, M.J.; Coarfa, C.; Sreekumar, A.; Putluri, N.; Katchy, C.A.; Lee, C.; Moore, D.D.; Fu, L. Circadian Homeostasis of Liver Metabolism Suppresses Hepatocarcinogenesis. Cancer Cell 2016, 30, 909–924. [Google Scholar] [CrossRef] [PubMed]
- Song, J.W.; Chung, K.C. Observational studies: Cohort and case-control studies. Plast. Reconstr. Surg. 2010, 126, 2234–2242. [Google Scholar] [CrossRef] [PubMed]
- Fedak, K.M.; Bernal, A.; Capshaw, Z.A.; Gross, S. Applying the Bradford Hill criteria in the 21st century: How data integration has changed causal inference in molecular epidemiology. Emerg. Themes Epidemiol. 2015, 12, 14. [Google Scholar] [CrossRef]
- Miki, Y. Hormone-Dependent Cancers: New Aspects on Biochemistry and Molecular Pathology. Int. J. Mol. Sci. 2023, 24, 10830. [Google Scholar] [CrossRef]
| First Author and Year | Cancer Type | LAN Assessment | Study Design |
|---|---|---|---|
| Davis, 2001 [35] | Breast | Indoor | Case–Control |
| O’Leary, 2006 [34] | Breast | Indoor | Case–Control |
| Li, 2010 [33] | Breast | Indoor | Case–Control |
| Kloog, 2011 [44] | Breast | Indoor | Case–Control |
| Fritschi, 2013 [50] | Breast | Indoor | Case–Control |
| Keshet-Sitton, 2016 [43] | Breast | Indoor | Case–Control |
| White, 2017 [32] | Breast | Indoor | Prospective Cohort |
| Johns, 2018 [47] | Breast | Indoor | Prospective Cohort |
| Yang, 2019 [41] | Breast | Indoor | Case–Control |
| Hurley, 2014 [30] | Breast | Indoor and Outdoor | Prospective Cohort |
| Garcia-Saenz, 2018 [45] | Breast | Indoor and Outdoor | Case–Control |
| Sweeney, 2022 [31] | Breast | Indoor and Outdoor | Prospective Cohort |
| Song, 2023 [42] | Breast | Indoor and Outdoor | Case–Control |
| Bauer, 2013 [29] | Breast | Outdoor | Case–Control |
| James, 2017 [25] | Breast | Outdoor | Prospective Cohort |
| Ritonja, 2020 [28] | Breast | Outdoor | Case–Control |
| Xiao, 2020 [27] | Breast | Outdoor | Prospective Cohort |
| Clarke, 2021 [48] | Breast | Outdoor | Prospective Cohort |
| Xiao, 2021 [39] | Breast | Outdoor | Prospective Cohort |
| n = 19 studies | |||
| Walasa, 2018 [49] | Colorectal | Indoor | Case–Control |
| Garcia-Saenz, 2018 [45] | Prostate | Indoor & Outdoor | Case–Control |
| Garcia-Saenz, 2020 [46] | Colorectal | Outdoor | Case–Control |
| Zhong, 2020 [40] | NHL | Outdoor | Prospective Cohort |
| Xiao, 2021 [26] | Pancreatic | Outdoor | Prospective Cohort |
| Zhang, 2021 [38] | Thyroid | Outdoor | Prospective Cohort |
| Park, 2022 [37] | Liver | Outdoor | Prospective Cohort |
| Medgyesi, 2023 [36] | Endometrial | Outdoor | Prospective Cohort |
| n = 8 studies | |||
| Author and Year | Cancer Type | LAN Exposure | Study Design | Sampling Frame | Participant Source | LAN Assessment | Reference Group | Exposure | Adjusted OR/RR | Adjusted/Matched Factors |
|---|---|---|---|---|---|---|---|---|---|---|
| Walasa, 2018 [49] | Colorectal | Indoor | Case-Control | Population-based | Western Australia Bowel Health Study | Self-reported | No shifts with Light at night | 7.5+ years of shiftwork with light at night | 0.91 (0.55–1.53) | age, education, SES, smoking, and alcohol use |
| Garcia-Saenz, 2018 [45] | Prostate | Indoor | Case-Control | Population-based | MCC-Spain | Self-reported | Total Darkness | Very Illuminated | 2.79 (1.55–5.04) | age, center, educational level, socioeconomic status, UVI, BMI, tobacco, family history of breast/prostate cancer, chronotype, menopausal status (breast cancer), and mutual adjustment for other light exposures |
| Garcia-Saenz, 2018 [45] | Prostate | Outdoor | Case-Control | Population-based | MCC-Spain | Measured | Outdoor LAN Q1 | Outdoor LAN Q3 | 0.56 (0.38–0.84) | age, center, educational level, socioeconomic status, UVI, BMI, tobacco, family history of breast/prostate cancer, chronotype, menopausal status (breast cancer), and mutual adjustment for other light exposures |
| Measured | Outdoor Blue LAN Q1 | Outdoor Blue LAN Q3 | 2.05 (1.38–3.03) | |||||||
| Garcia-Saenz, 2020 [46] | Colorectal | Outdoor | Case-Control | Population-based | MCC-Spain | Measured | Outdoor LAN Q1 | Outdoor LAN Q3 | 0.9 (0.7–1.1) | Area, age, sex, educational level, WCRF score, Urban Vulnerability Index, family history, smoking habits, sleeping problems, and sleep duration |
| Measured | Outdoor Blue LAN Q1 | Outdoor Blue LAN Q3 | 1.7 (1.3–2.3) | |||||||
| Zhong, 2020 [40] | NHL | Outdoor | Prospective Cohort | Population-based | California Teachers Study | Measured | Outdoor LAN Q1 | Outdoor LAN Q5 | 1.32 (1.05–1.66) | age, race, SES, BMI, smoking, alcohol, and FH of NHL |
| Xiao, 2021 [39] | Pancreatic | Outdoor | Prospective Cohort | Population-based | NIH-AARP | Measured | Outdoor LAN Q1 | Outdoor LAN Q5 | 1.24 (1.03–1.49) | Age, sex, race, education, marital status, state of residence, median home value, poverty rate, and population density at the census tract level |
| Zhang, 2021 [38] | Thyroid | Outdoor | Prospective Cohort | Population-based | NIH-AARP | Measured | Outdoor LAN Q1 | Outdoor LAN Q5 | 1.55 (1.18–2.02) | Age, sex, race, education, marital status, state of residence, median home value, poverty rate, and population density at the census tract level |
| Park, 2022 [37] | Liver | Outdoor | Prospective Cohort | Population-based | NIH-AARP | Measured | Outdoor LAN Q1 | Outdoor LAN Q5 | 0.96 (0.77–1.20) | age, sex, race/ethnicity, education, BMI, diabetes, aspirin use, coffee consumption, night-time sleep duration, state, income, and urban–rural code |
| Medgyesi, 2023 [36] | Endometrial | Outdoor | Prospective Cohort | Population-based | NIH-AARP | Measured | Outdoor LAN Q1 | Outdoor LAN Q5 | 0.93 (0.77–1.1) | Age, race/ethnicity, poverty, state, BMI, years of OC use, age at menopause, HRT use, parity, PM2.5, and metro-rural area |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, S.; Alsabawi, Y.; El-Serag, H.B.; Thrift, A.P. Exposure to Light at Night and Risk of Cancer: A Systematic Review, Meta-Analysis, and Data Synthesis. Cancers 2024, 16, 2653. https://doi.org/10.3390/cancers16152653
Ma S, Alsabawi Y, El-Serag HB, Thrift AP. Exposure to Light at Night and Risk of Cancer: A Systematic Review, Meta-Analysis, and Data Synthesis. Cancers. 2024; 16(15):2653. https://doi.org/10.3390/cancers16152653
Chicago/Turabian StyleMa, Samuel, Yossef Alsabawi, Hashem B El-Serag, and Aaron P Thrift. 2024. "Exposure to Light at Night and Risk of Cancer: A Systematic Review, Meta-Analysis, and Data Synthesis" Cancers 16, no. 15: 2653. https://doi.org/10.3390/cancers16152653
APA StyleMa, S., Alsabawi, Y., El-Serag, H. B., & Thrift, A. P. (2024). Exposure to Light at Night and Risk of Cancer: A Systematic Review, Meta-Analysis, and Data Synthesis. Cancers, 16(15), 2653. https://doi.org/10.3390/cancers16152653







