Timing of Resection of Spinal Meningiomas and Its Influence on Quality of Life and Treatment
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
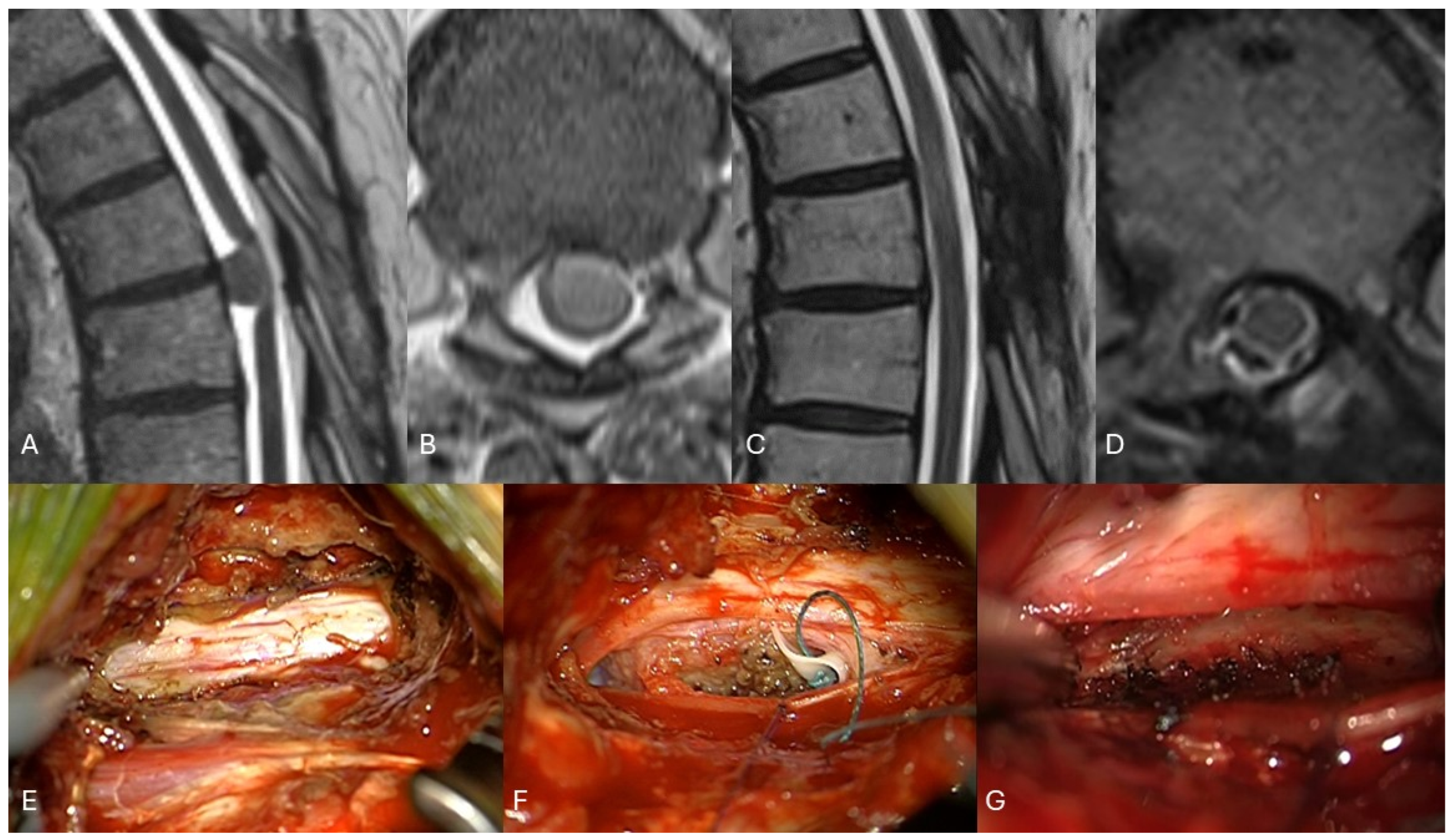
2.2. Surgical Intervention
2.3. Outcome and Assessment of QoL and Functionality
2.4. Evaluation of Images
2.5. Statistical Analysis
3. Results
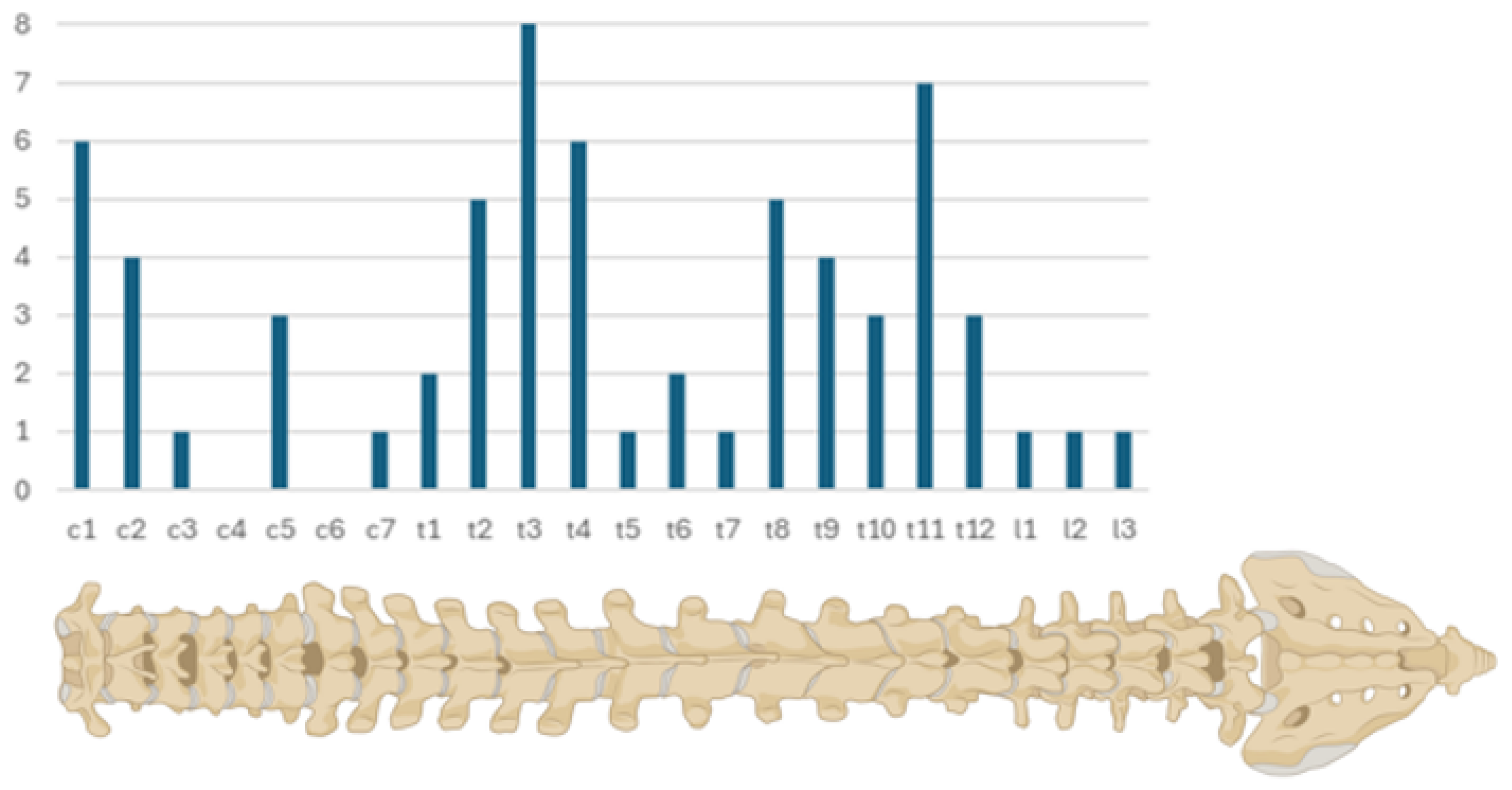
3.1. Patients’ Characteristics
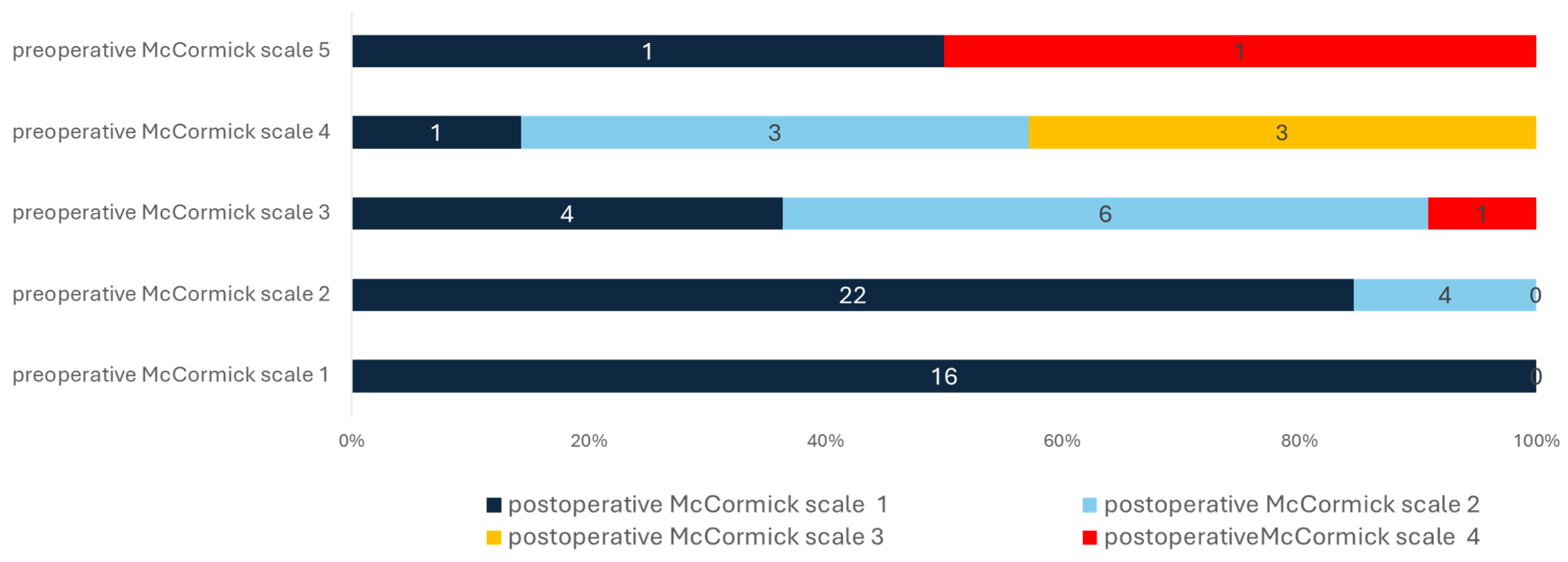
3.2. Neurological Outcome and Quality Indicators
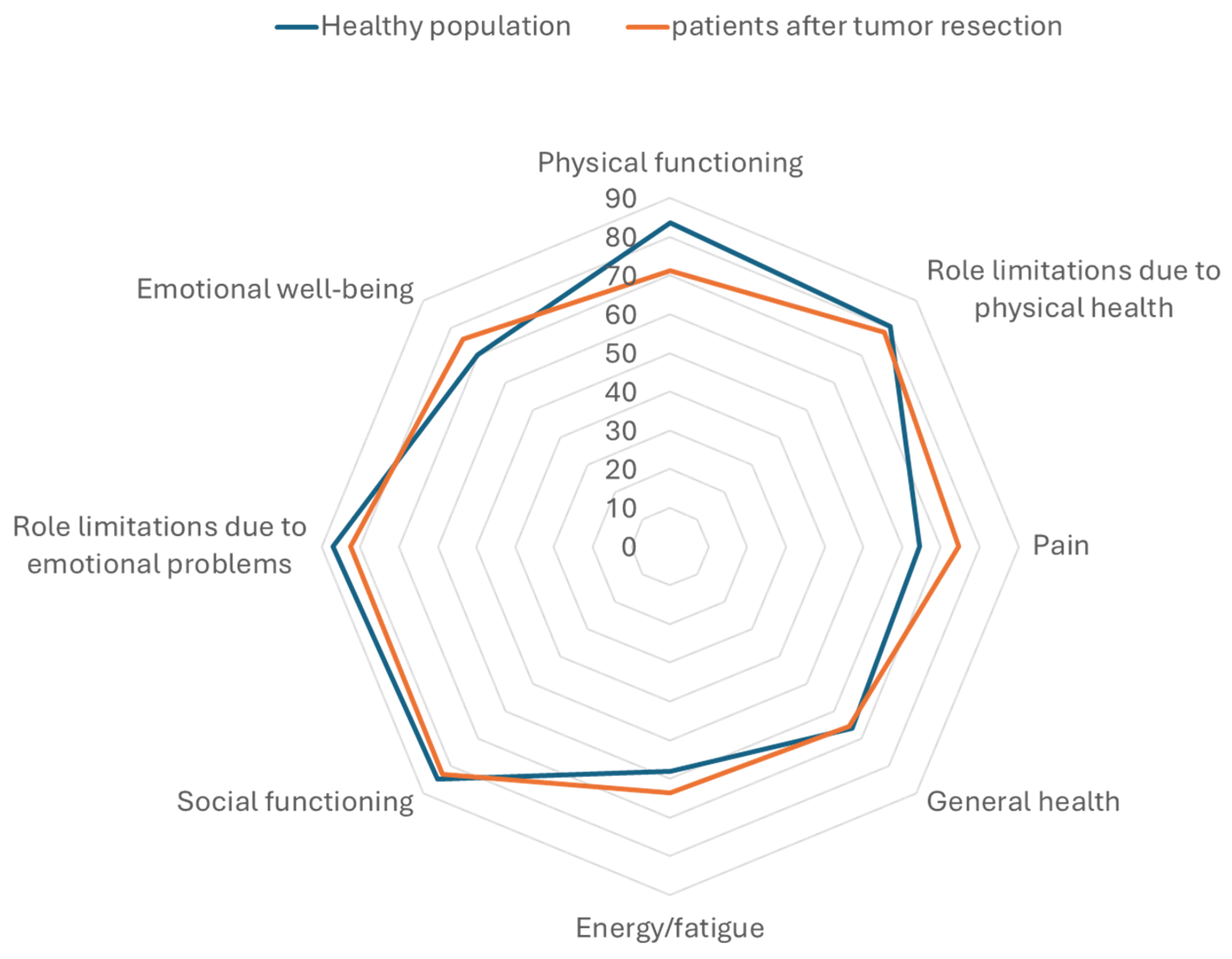
3.3. Functionality and Quality of Life
3.4. Tumor Recurrence and Progression
4. Discussion
4.1. Neurological Outcome after Minimal-Invasive Resection
4.2. Effect of Neurological Outcome on Functionality and Quality of Life
4.3. Quality Indicators and Adverse Events
4.4. Minimal-Invasive Surgery
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Capo, G.; Moiraghi, A.; Baro, V.; Tahhan, N.; Delaidelli, A.; Saladino, A.; Paun, L.; DiMeco, F.; Denaro, L.; Meling, T.R.; et al. Surgical Treatment of Spinal Meningiomas in the Elderly (≥75 Years): Which Factors Affect the Neurological Outcome? An International Multicentric Study of 72 Cases. Cancers 2022, 14, 4790. [Google Scholar] [CrossRef] [PubMed]
- Schwake, M.; Adeli, A.; Sporns, P.; Ewelt, C.; Schmitz, T.; Sicking, J.; Hess, K.; Cäcilia Spille, D.; Paulus, W.; Stummer, W.; et al. Spinal Meningiomas—Risks and Potential of an Increasing Age at the Time of Surgery. J. Clin. Neurosci. 2018, 57, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Setzer, M.; Vatter, H.; Marquardt, G.; Seifert, V.; Vrionis, F.D. Management of Spinal Meningiomas: Surgical Results and a Review of the Literature. Neurosurg. Focus. 2007, 23, E14. [Google Scholar] [CrossRef] [PubMed]
- Pettersson-Segerlind, J.; Fletcher-Sandersjöö, A.; Tatter, C.; Burström, G.; Persson, O.; Förander, P.; Mathiesen, T.; Bartek, J.; Edström, E.; Elmi-Terander, A. Long-Term Follow-Up and Predictors of Functional Outcome after Surgery for Spinal Meningiomas: A Population-Based Cohort Study. Cancers 2021, 13, 3244. [Google Scholar] [CrossRef] [PubMed]
- Schipmann, S.; Schwake, M.; Suero Molina, E.; Stummer, W. Markers for Identifying and Targeting Glioblastoma Cells during Surgery. J. Neurol. Surg. Part A Cent. Eur. Neurosurg. 2019, 80, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Spille, D.C.; Lohmann, S.; Schwake, M.; Spille, J.H.; Alsofy, S.Z.; Stummer, W.; Brokinkel, B.; Schipmann, S. Can Currently Suggested Quality Indicators Be Transferred to Meningioma Surgery?—A Single-Centre Pilot Study. J. Neurol. Surg. Part A Cent. Eur. Neurosurg. 2022, 84, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Schipmann, S.; Sletvold, T.P.; Wollertsen, Y.; Schwake, M.; Raknes, I.C.; Miletić, H.; Mahesparan, R. Quality Indicators and Early Adverse in Surgery for Atypical Meningiomas: A 16-Year Single Centre Study and Systematic Review of the Literature. Brain Spine 2023, 3, 101739. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, F.; Setzer, M.; Marquardt, G.; Keil, F.; Dubinski, D.; Bruder, M.; Seifert, V.; Behmanesh, B. Functional Outcome and Morbidity after Microsurgical Resection of Spinal Meningiomas. Neurosurg. Focus 2021, 50, E20. [Google Scholar] [CrossRef]
- Viereck, M.J.; Ghobrial, G.M.; Beygi, S.; Harrop, J.S. Improved Patient Quality of Life Following Intradural Extramedullary Spinal Tumor Resection. J. Neurosurg. Spine 2016, 25, 640–645. [Google Scholar] [CrossRef]
- Newman, W.C.; Berry-Candelario, J.; Villavieja, J.; Reiner, A.S.; Bilsky, M.H.; Laufer, I.; Barzilai, O. Improvement in Quality of Life Following Surgical Resection of Benign Intradural Extramedullary Tumors: A Prospective Evaluation of Patient-Reported Outcomes. Neurosurgery 2021, 88, 989–995. [Google Scholar] [CrossRef]
- Said, W.; Maragno, E.; Leibrandt, L.; Spille, D.; Schipmann, S.; Stummer, W.; Gallus, M.; Schwake, M. A Retrospective Cohort Study Evaluating the Comparative Effectiveness of Unilateral Hemilaminectomy and Bilateral Laminectomy in the Resection of Spinal Meningiomas. Oper. Neurosurg. 2024; online ahead of print. [Google Scholar] [CrossRef]
- Chiou, S.M.; Eggert, H.R.; Laborde, G.; Seeger, W. Microsurgical Unilateral Approaches for Spinal Tumour Surgery: Eight Years’ Experience in 256 Primary Operated Patients. Acta Neurochir. 1989, 100, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Schöller, K.; Alimi, M.; Cong, G.T.; Christos, P.; Härtl, R. Lumbar Spinal Stenosis Associated with Degenerative Lumbar Spondylolisthesis: A Systematic Review and Meta-Analysis of Secondary Fusion Rates following Open vs Minimally Invasive Decompression. Neurosurgery 2017, 80, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Javid, M.J.; Hadar, E.J. Long-Term Follow-Up Review of Patients Who Underwent Laminectomy for Lumbar Stenosis: A Prospective Study. J. Neurosurg. 1998, 89, E1. [Google Scholar] [CrossRef] [PubMed]
- Goldbrunner, R.; Stavrinou, P.; Jenkinson, M.D.; Sahm, F.; Mawrin, C.; Weber, D.C.; Preusser, M.; Minniti, G.; Lund-Johansen, M.; Lefranc, F.; et al. EANO Guideline on the Diagnosis and Management of Meningiomas. Neuro Oncol. 2021, 23, 1821–1834. [Google Scholar] [CrossRef] [PubMed]
- Simpson, D. The Recurrence of Intracranial Meningiomas after Surgical Treatment. J. Neurol. Neurosurg. Psychiatry 1957, 20, 22–39. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.T.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef] [PubMed]
- Vernon, H. The Neck Disability Index: State-of-the-Art, 1991–2008. J. Manip. Physiol. Ther. 2008, 31, 491–502. [Google Scholar] [CrossRef]
- McCormick, P.C.; Torres, R.; Post, K.D.; Stein, B.M. Intramedullary Ependymoma of the Spinal Cord. J. Neurosurg. 1990, 72, 523–532. [Google Scholar] [CrossRef]
- Maurischat, C.; Ehlebracht-König, I.; Kühn, A.; Bullinger, M. [Structural Validity of the Short Form 36 (SF-36) in Patients with Rheumatic Diseases]. Z. Rheumatol. 2005, 64, 255–264. [Google Scholar] [CrossRef]
- Jankovic, D.; Kalasauskas, D.; Othman, A.; Brockmann, M.A.; Sommer, C.J.; Ringel, F.; Keric, N. Predictors of Neurological Worsening after Resection of Spinal Meningiomas. Cancers 2023, 15, 5408. [Google Scholar] [CrossRef]
- Schwake, M.; Ricchizzi, S.; Krahwinkel, S.; Maragno, E.; Schipmann, S.; Stummer, W.; Gallus, M.; Holling, M. Resection of Intramedullary Hemangioblastoma: Timing of Surgery and Its Impact on Neurological Outcome and Quality of Life. Medicina 2023, 59, 1611. [Google Scholar] [CrossRef] [PubMed]
- El-Hajj, V.G.; Pettersson-Segerlind, J.; Fletcher-Sandersjöö, A.; Edström, E.; Elmi-Terander, A. Current Knowledge on Spinal Meningiomas-Surgical Treatment, Complications, and Outcomes: A Systematic Review and Meta-Analysis (Part 2). Cancers 2022, 14, 6221. [Google Scholar] [CrossRef] [PubMed]
- Wach, J.; Banat, M.; Schuss, P.; Güresir, E.; Vatter, H.; Scorzin, J. Age at Diagnosis and Baseline Myelomalacia Sign Predict Functional Outcome after Spinal Meningioma Surgery. Front. Surg. 2021, 8, 682930. [Google Scholar] [CrossRef] [PubMed]
- Raco, A.; Pesce, A.; Toccaceli, G.; Domenicucci, M.; Miscusi, M.; Delfini, R. Factors Leading to a Poor Functional Outcome in Spinal Meningioma Surgery: Remarks on 173 Cases. Neurosurgery 2017, 80, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Jesse, C.M.; Alvarez Abut, P.; Wermelinger, J.; Raabe, A.; Schär, R.T.; Seidel, K. Functional Outcome in Spinal Meningioma Surgery and Use of Intraoperative Neurophysiological Monitoring. Cancers 2022, 14, 3989. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Menezes, A.H.; Shimizu, K.; Woodroffe, R.W.; Helland, L.C.; Hitchon, P.W.; Howard, M.A. Differences and Characteristics of Symptoms by Tumor Location, Size, and Degree of Spinal Cord Compression: A Retrospective Study on 53 Surgically Treated, Symptomatic Spinal Meningiomas. J. Neurosurg. Spine 2020, 32, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Boström, A.; Bürgel, U.; Reinacher, P.; Krings, T.; Rohde, V.; Gilsbach, J.M.; Hans, F.J. A Less Invasive Surgical Concept for the Resection of Spinal Meningiomas. Acta Neurochir. 2008, 150, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Harati, A.; Satopää, J.; Mahler, L.; Billon-Grand, R.; Elsharkawy, A.; Niemelä, M.; Hernesniemi, J. Early Microsurgical Treatment for Spinal Hemangioblastomas Improves Outcome in Patients with von Hippel-Lindau Disease. Surg. Neurol. Int. 2012, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Butenschoen, V.M.; Gloßner, T.; Hostettler, I.C.; Meyer, B.; Wostrack, M. Quality of Life and Return to Work and Sports after Spinal Ependymoma Resection. Sci. Rep. 2022, 12, 4926. [Google Scholar] [CrossRef]
- Goodwin, C.R.; Price, M.; Goodwin, A.N.; Dalton, T.; Versteeg, A.L.; Sahgal, A.; Rhines, L.D.; Schuster, J.M.; Weber, M.H.; Lazary, A.; et al. Gender and Sex Differences in Health-Related Quality of Life, Clinical Outcomes and Survival after Treatment of Metastatic Spine Disease. Spine, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Bond, M.R.; Versteeg, A.L.; Sahgal, A.; Rhines, L.D.; Sciubba, D.M.; Schuster, J.M.; Weber, M.H.; Fehlings, M.G.; Lazary, A.; Clarke, M.J.; et al. Surgical or Radiation Therapy for the Treatment of Cervical Spine Metastases: Results from the Epidemiology, Process, and Outcomes of Spine Oncology (EPOSO) Cohort. Global Spine J. 2020, 10, 21–29. [Google Scholar] [CrossRef]
- Guarino, A.; Polini, C.; Forte, G.; Favieri, F.; Boncompagni, I.; Casagrande, M. The Effectiveness of Psychological Treatments in Women with Breast Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 209. [Google Scholar] [CrossRef] [PubMed]
- Rick, O.; Dauelsberg, T.; Kalusche-Bontemps, E.M. Oncological Rehabilitation. Oncol. Res. Treat. 2017, 40, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Boersma, I.; Miyasaki, J.; Kutner, J.; Kluger, B. Palliative Care and Neurology: Time for a Paradigm Shift. Neurology 2014, 83, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Thakur, J.; Ulrich, C.T.; Schär, R.T.; Seidel, K.; Raabe, A.; Jesse, C.M. The Surgical Challenge of Ossified Ventrolateral Spinal Meningiomas: Tricks and Pearls for Managing Large Ossified Meningiomas of the Thoracic Spine. J. Neurosurg. Spine 2021, 35, 516–526. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Park, P.; Shaffrey, C.I.; Wang, M.Y.; Uribe, J.S.; Fessler, R.G.; Chou, D.; Kanter, A.S.; Okonkwo, D.O.; Mundis, G.M.; et al. The MISDEF2 Algorithm: An Updated Algorithm for Patient Selection in Minimally Invasive Deformity Surgery. J. Neurosurg. Spine 2019, 32, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Debono, B.; Wainwright, T.W.; Wang, M.Y.; Sigmundsson, F.G.; Yang, M.M.H.; Smid-Nanninga, H.; Bonnal, A.; Le Huec, J.C.; Fawcett, W.J.; Ljungqvist, O.; et al. Consensus Statement for Perioperative Care in Lumbar Spinal Fusion: Enhanced Recovery After Surgery (ERAS®) Society Recommendations. Spine J. 2021, 21, 729–752. [Google Scholar] [CrossRef]
- Dobran, M.; Paracino, R.; Nasi, D.; Aiudi, D.; Capece, M.; Carrassi, E.; Lattanzi, S.; Rienzo, A.D.I.; Iacoangeli, M. Laminectomy versus Unilateral Hemilaminectomy for the Removal of Intraspinal Schwannoma: Experience of a Single Institution and Review of Literature. J. Neurol. Surg. Part A Cent. Eur. Neurosurg. 2021, 82, 552–555. [Google Scholar] [CrossRef] [PubMed]
- Acosta, F.L.; Aryan, H.E.; Chi, J.; Parsa, A.T.; Ames, C.P. Modified Paramedian Transpedicular Approach and Spinal Reconstruction for Intradural Tumors of the Cervical and Cervicothoracic Spine: Clinical Experience. Spine 2007, 32, E203–E210. [Google Scholar] [CrossRef] [PubMed]
- Onken, J.; Obermüller, K.; Staub-Bartelt, F.; Meyer, B.; Vajkoczy, P.; Wostrack, M. Surgical Management of Spinal Meningiomas: Focus on Unilateral Posterior Approach and Anterior Localization. J. Neurosurg. Spine 2018, 30, 308–313. [Google Scholar] [CrossRef]
- Liao, D.; Li, D.; Wang, R.; Xu, J.; Chen, H. Hemilaminectomy for the Removal of the Spinal Tumors: An Analysis of 901 Patients. Front. Neurol. 2022, 13, 1094073. [Google Scholar] [CrossRef]
- Krahwinkel, S.; Schipmann, S.; Spille, D.; Maragno, E.; Al Barim, B.; Warneke, N.; Stummer, W.; Gallus, M.; Schwake, M. The Role of Prolonged Bed Rest in Postoperative Cerebrospinal Fluid Leakage after Surgery of Intradural Pathology—A Retrospective Cohort Study. Neurosurgery 2023, 93, 563–575. [Google Scholar] [CrossRef] [PubMed]
- Schwake, M.; Krahwinkel, S.; Gallus, M.; Schipmann, S.; Maragno, E.; Neuschmelting, V.; Perrech, M.; Müther, M.; Lenschow, M. Does Early Mobilization following Resection of Spinal Intra-Dural Pathology Increase the Risk of Cerebrospinal Fluid Leaks?—A Dual-Center Comparative Effectiveness Research. Medicina 2024, 60, 171. [Google Scholar] [CrossRef]
- Müther, M.; Lüthge, S.; Gerwing, M.; Stummer, W.; Schwake, M. Management of Spinal Dumbbell Tumors via a Minimally Invasive Posterolateral Approach and Carbon Fiber-Reinforced Polyether Ether Ketone Instrumentation: Technical Note and Surgical Case Series. World Neurosurg. 2021, 151, 277–283.e1. [Google Scholar] [CrossRef]
- Schwake, M.; Maragno, E.; Gallus, M.; Schipmann, S.; Spille, D.; Al Barim, B.; Stummer, W.; Müther, M. Minimally Invasive Facetectomy and Fusion for Resection of Extensive Dumbbell Tumors in the Lumbar Spine. Medicina 2022, 58, 1613. [Google Scholar] [CrossRef]
- Gerszten, P.C.; Chen, S.; Quader, M.; Xu, Y.; Novotny, J.; Flickinger, J.C. Radiosurgery for Benign Tumors of the Spine Using the Synergy S with Cone-Beam Computed Tomography Image Guidance. J. Neurosurg. 2012, 117, 197–202. [Google Scholar] [CrossRef]
- Sachdev, S.; Dodd, R.L.; Chang, S.D.; Soltys, S.G.; Adler, J.R.; Luxton, G.; Choi, C.Y.H.; Tupper, L.; Gibbs, I.C. Stereotactic Radiosurgery Yields Long-Term Control for Benign Intradural, Extramedullary Spinal Tumors. Neurosurgery 2011, 69, 533–539. [Google Scholar] [CrossRef]



| Variable | Mild Symptoms (n = 42) | Severe Symptoms (n = 23) | p-Value |
|---|---|---|---|
| Age (years, mean ± SD) | 55.29 (±13.52) | 64.09 (±13.62) | 0.015 |
| Female patients (n, %) | 28 (90.48%) | 21 (91.30%) | |
| Karnofsky performance scale preoperative (median, IQR) | 80 (70–80) | 70 (60–70) | <0.001 |
| Other spine procedures in the past (n, %) | 1 (2.38%) | 2 (8.70%) | 0.284 |
| Other neurological diseases (n, %) | 2 (4.76%) | 2 (8.70%) | 0.603 |
| Psychological disorders (n, %) | 1 (2.38%) | 1 (4.35%) | >0.99 |
| Other meningiomas in different localization (n, %) | 4 (9.52%) | 3 (13.04%) | 0.691 |
| Preoperative McCormick scale (median, IQR) | 2 (1–2) | 3 (3–4) | <0.001 |
| Preoperative McCormick scale 1 (n, %) | 16 (38.1%) | 0 | <0.001 |
| Preoperative McCormick scale 2 (n, %) | 26 (61.3%) | 0 | <0.001 |
| Preoperative McCormick scale 3 (n, %) | 0 | 15 (65.22%) | <0.001 |
| Preoperative McCormick scale 4 (n, %) | 0 | 6 (26.09%) | <0.001 |
| Preoperative McCormick scale 5 (n, %) | 0 | 2 (8.70%) | 0.114 |
| Motor weakness (n, %) | 6 (14.29%) | 15 (65.22%) | <0.001 |
| Gait ataxia (n, %) | 2 (4.76%) | 16 (69.57%) | <0.001 |
| Radicular pain (n, %) | 18 (42.86%) | 6 (26.09%) | 0.282 |
| Sensory deficit (n, %) | 14 (33.33%) | 20 (86.96%) | <0.001 |
| Bladder incontinence (n, %) | 2 (4.76%) | 6 (26.09%) | 0.016 |
| Local pain (n, %) | 16 (38.10%) | 5 (21.74%) | 0.275 |
| Duration of Symptoms (n, %) | 0.093 | ||
| More than 6 months (n, %) | 12 (28.57%) | 8 (34.78%) | 0.780 |
| Less than 6 months (n, %) | 19 (45.24%) | 14 (60.87%) | 0.302 |
| Unknown (n, %) | 11 (26.19%) | 1 (4.35%) | 0.043 |
| Primary case (n, %) | 38 (90.48%) | 23 (100%) | 0.290 |
| Recurrent tumor (n, %) | 4 (9.52%) | 0 | |
| Localization within the spinal canal | 0.087 | ||
| Cervical spine (n, %) | 14 (33.33%) | 3 (13.04%) | 0.087 |
| Thoracic spine (n, %) | 25 (59.52%) | 20 (86.96%) | 0.026 |
| Lumbar spine (n, %) | 3 (7.14%) | 0 | 0.546 |
| Tumor volume (ml, mean, SD) | 1.13 (±0.79) | 1.36 (±0.95) | 0.294 |
| Tumor/ spinal canal ratio (%, mean, SD) | 47.25% (±17.77%) | 59.73 (±21.07%) | 0.016 |
| Compression of spinal cord (n, %) | 36 (85.71%) | 23 (100%) | 0.082 |
| Spinal cord edema (n, %) | 5 (11.90%) | 8 (34.78%) | 0.049 |
| Variable | Mild Symptoms (n = 42) | Severe Symptoms (n = 23) | p-Value |
|---|---|---|---|
| Duration of surgery (min, mean, SD) | 238.34 (±111.77) | 231.13 (±68.51) | 0.785 |
| Uni-lateral approach (n, %) | 37 (88.1%) | 22 (95.65%) | 0.411 |
| Bilateral approach (n, %) | 5 (11.9%) | 1 (4.35%) | 0.411 |
| Extent of resection | |||
| Simpson grade 2 (n, %) | 40 (95.24%) | 22 (95.65%) | >0.99 |
| Simpson grade 3 (n, %) | 2 (4.76%) | 1 (4.35%) | |
| Estimated blood loss (ml, mean, SD) | 236.72 (±315.70) | 356.13 (±384) | 0.191 |
| Length of hospital stay (days, mean, SD) | 7.07 (±2.4) | 10.04 (±5.36) | 0.003 |
| Adverse events (n, %) | 2 (4.76%) | 2 (8.7%) | >0.99 |
| CSF leak (n, %) | 1 (2.38%) | 0 | >0.99 |
| Pulmonary embolism (n, %) | 1 (2.38%) | 0 | >0.99 |
| Cardial decompensation (n, %) | 0 | 1 (4.35%) | 0.354 |
| Urinary tract infection | 0 | 1 (4.35%) | 0.354 |
| Histology WHO 1 (n, %) | 42 (100%) | 23 (100%) | >0.99 |
| Karnofsky performance scale postoperative (Median, IQR) | 90 (90–100) | 80 (70–90) | 0.004 |
| Postoperative McCormick scale (Median, IQR) | 1 (1–1) | 2 (1–2) | 0.001 |
| Postoperative McCormick scale 1 (n, %) | 38 (90.48%) | 9 (39.13%) | <0.001 |
| Postoperative McCormick scale 2 (n, %) | 4 (9.52%) | 10 (43.48%) | 0.003 |
| Postoperative McCormick scale 3 (n, %) | 0 | 3 (13.04%) | 0.037 |
| Postoperative McCormick scale 4 (n, %) | 0 | 1 (4.35%) | 0.354 |
| Postoperative McCormick scale 5 (n, %) | 0 | 0 | >0.99 |
| Postoperative motoric weakness (n, %) | 0 | 2 (8.70%) | 0.122 |
| Gait ataxia (n, %) | 1 (2.38%) | 1 (4.35%) | >0.99 |
| Radicular pain (n, %) | 4 (9.52%) | 1 (4.35%) | 0.649 |
| Sensory loss (n, %) | 1 (2.38%) | 6 (26.09%) | 0.006 |
| Bladder incontinence (n, %) | 2 (4.76%) | 4 (17.39%) | 0.174 |
| Local pain (n, %) | 5 (11.90%) | 0 | 0.152 |
| Readmission in 90 days (n, %) | 1 (2.38%) | 0 | >0.99 |
| Re-Surgery in 90 days (n, %) | 1 (2.38%) | 0 | >0.99 |
| Tumor recurrence (n, %) | 3 (7.14%) | 0 | 0.547 |
| Progression-free survival (years, mean, SD) | 7.45 (±3.95) | 6 (±3.40) | 0.121 |
| Variable | Favorable Neurological Outcome (n = 27) | Incomplete Neurological Outcome (n = 11) | p-Value |
|---|---|---|---|
| Age at time of surgery (years, mean ± SD) | 56.93 ± 12.62 | 64.64 ± 12.04 | 0.092 |
| Age at present (years, mean ± SD) | 63.15 ± 12.77 | 68.73 ± 12.06 | 0.223 |
| Female patients (n, %) | 25 (93%) | 10 (91%) | >0.99 |
| Karnofsky performance scale preoperative (median, IQR) | 80 (70–80) | 70 (70) | <0.001 |
| Other spine procedures in the past (n, %) | 3 (11%) | 2 (18%) | 0.615 |
| Other neurological diseases (n, %) | 2 | 1 (9%) | >0.99 |
| Psychological disorders (n, %) | 0 | 1 (9%) | 0.290 |
| Other meningiomas (n, %) | 1 | 2 | 0.196 |
| McCormick scale (median, IQR) | |||
| McCormick scale 1 (n, %) | 6 | 0 | 0.154 |
| McCormick scale 2 (n, %) | 16 | 1 | 0.010 |
| McCormick scale 3 (n, %) | 3 | 6 | 0.009 |
| McCormick scale 4 (n, %) | 1 | 4 | 0.019 |
| McCormick scale 5 (n, %) | 0 | 0 | >0.99 |
| McCormick scale 1–2 (n, %) | 22 | 1 | <0.001 |
| Preoperative motoric weakness (n, %) | 6 (22%) | 5 (45%) | 0.238 |
| Gait ataxia (n, %) | 0 | 10 (91%) | <0.001 |
| Radicular pain (n, %) | 13 (48%) | 3 (27%) | 0.296 |
| Sensory loss (n, %) | 10 (37%) | 9 (32%) | 0.029 |
| Bladder incontinence (n, %) | 1 (4%) | 2 (18%) | 0.196 |
| Local pain (n, %) | 11 (41%) | 1 (9%) | 0.121 |
| Duration of Symptoms (n, %) | |||
| More than 6 months (n, %) | 5 | 5 | 0.116 |
| Less than 6 months (n, %) | 17 | 5 | 0.471 |
| Unknown (n, %) | 4 | 1 | >0.99 |
| Primary case (n, %) | 24 | 11 (100%) | 0.542 |
| Recurrent tumor (n, %) | 3 | 0 | 0.542 |
| Localization with spinal canal | |||
| Cervical spine (n, %) | 7 | 1 | 0.395 |
| Thoracic spine (n, %) | 17 | 10 | 0.124 |
| Lumbar spine (n, %) | 3 | 0 | 0.542 |
| Tumor volume (ml, mean, SD) | 1.17 ± 0.81 | 1.26 ± 1.10 | 0.787 |
| Tumor/ spinal canal ratio (%, mean, SD) | 52 ± 17% | 59% ± 22% | 0.468 |
| Compression of spinal cord (n, %) | 25 (93%) | 11 (100%) | >0.99 |
| Spinal cord edema (n, %) | 1 (4%) | 4 (36%) | 0.019 |
| Variable | Favorable Neurological Outcome (n = 27) | Incomplete Neurological Outcome (n = 11) | p-Value |
|---|---|---|---|
| Duration of surgery (min, mean, SD) | 211.48 ± 95.87 | 236.09 ± 88.07 | 0.468 |
| Unilateral approach (n, %) | 26 | 11 (11%) | >0.99 |
| Bilateral approach (n, %) | 1 | 0 | >0.99 |
| Extent of resection | |||
| Simpson grade 2 (n, %) | 24 (89%) | 10 (91%) | >0.99 |
| Simpson grade 3 (n, %) | 3 (11%) | 1 (9%) | >0.99 |
| Estimated blood loss (ml, mean, SD) | 260.78 ± 382.88 | 203.73 ± 218.18 | 0.647 |
| Length of hospital stay (days, mean, SD) | 6.85 ± 1.26 | 9 ± 4.29 | 0.022 |
| Adverse events (n, %) | 0 | 0 | |
| Histology WHO 1 (n, %) | 27 | 11 | >0.99 |
| Karnofsky scale postoperative (Median, IQR) | 100 (90–100) | 80 (70–90) | <0.001 |
| McCormick scale (Median, IQR) | |||
| McCormick scale 1 (n, %) | 27 | 0 | <0.001 |
| McCormick scale 2 (n, %) | 0 | 9 | <0.001 |
| McCormick scale 3 (n, %) | 0 | 2 (18%) | 0.078 |
| Postoperative motoric weakness (n, %) | 0 | 1 (9%) | 0.290 |
| Gait ataxia (n, %) | 0 | 1 (9%) | 0.290 |
| Radicular pain (n, %) | 2 (7%) | 2 (18%) | 0.564 |
| Sensory loss (n, %) | 0 | 3 (27%) | 0.020 |
| Bladder incontinence (n, %) | 0 | 0 | >0.99 |
| Local pain (n, %) | 1 (4%) | 1 (9%) | 0.501 |
| Readmission in 90 days (n, %) | 0 | 0 | >0.99 |
| Re-Surgery in 90 days (n, %) | 0 | 0 | >0.99 |
| Tumor recurrence (n, %) | 2 (7%) | 0 | >0.99 |
| Progression-free survival (years, mean, SD) | 6.78 ± 4.14 | 4.09 ± 1.64 | 0.046 |
| Variable | Favorable Neurological Outcome (n = 27) | Incomplete Neurological Outcome (n = 11) | p-Value |
|---|---|---|---|
| ODI/NDI (mean, SD) | 9.26% ± 11.60% | 23.27% ± 24.10% | 0.020 |
| Physical functioning (mean, SD) | 79.26 ± 20.03 | 51.82 ± 37.97 | 0.019 |
| Role limitations due to physical health (mean, SD) | 86.11 ± 27.15 | 59.09 ± 45.10 | 0.029 |
| Role limitations due to emotional problems (mean, SD) | 85.19 ± 29.72 | 75.75 ± 42.41 | 0.604 |
| Energy/fatigue (mean, SD) | 66.11 ± 21.81 | 57.27 ± 23.06 | 0.272 |
| Emotional well-being (mean, SD) | 78.48 ± 17.83 | 69.09 ± 22.42 | 0.180 |
| Social functioning (mean, SD) | 87.04 ± 18.50 | 73.86 ± 29.82 | 0.106 |
| Pain (mean, SD) | 80.19 ± 24.35 | 60.68 ± 32.66 | 0.050 |
| General health (mean, SD) | 68.33 ± 21.75 | 58.64 ± 22.59 | 0.226 |
| Health change (mean, SD) | 65.74 ± 25.14 | 61.36 ± 23.35 | 0.623 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwake, M.; Said, W.; Gallus, M.; Maragno, E.; Schipmann, S.; Spille, D.; Stummer, W.; Brokinkel, B. Timing of Resection of Spinal Meningiomas and Its Influence on Quality of Life and Treatment. Cancers 2024, 16, 2336. https://doi.org/10.3390/cancers16132336
Schwake M, Said W, Gallus M, Maragno E, Schipmann S, Spille D, Stummer W, Brokinkel B. Timing of Resection of Spinal Meningiomas and Its Influence on Quality of Life and Treatment. Cancers. 2024; 16(13):2336. https://doi.org/10.3390/cancers16132336
Chicago/Turabian StyleSchwake, Michael, Wesam Said, Marco Gallus, Emanuele Maragno, Stephanie Schipmann, Dorothee Spille, Walter Stummer, and Benjamin Brokinkel. 2024. "Timing of Resection of Spinal Meningiomas and Its Influence on Quality of Life and Treatment" Cancers 16, no. 13: 2336. https://doi.org/10.3390/cancers16132336
APA StyleSchwake, M., Said, W., Gallus, M., Maragno, E., Schipmann, S., Spille, D., Stummer, W., & Brokinkel, B. (2024). Timing of Resection of Spinal Meningiomas and Its Influence on Quality of Life and Treatment. Cancers, 16(13), 2336. https://doi.org/10.3390/cancers16132336





