Head-to-Head Comparison: P-POSSUM and ACS-NSQIP® in Predicting Perioperative Risk in Robotic Surgery for Gynaecological Cancers
Abstract
Simple Summary
Abstract
1. Introduction
2. Ethics and Approvals
3. Materials and Methods
3.1. Cohort Selection
3.2. Data Collection
3.3. Statistical Analysis
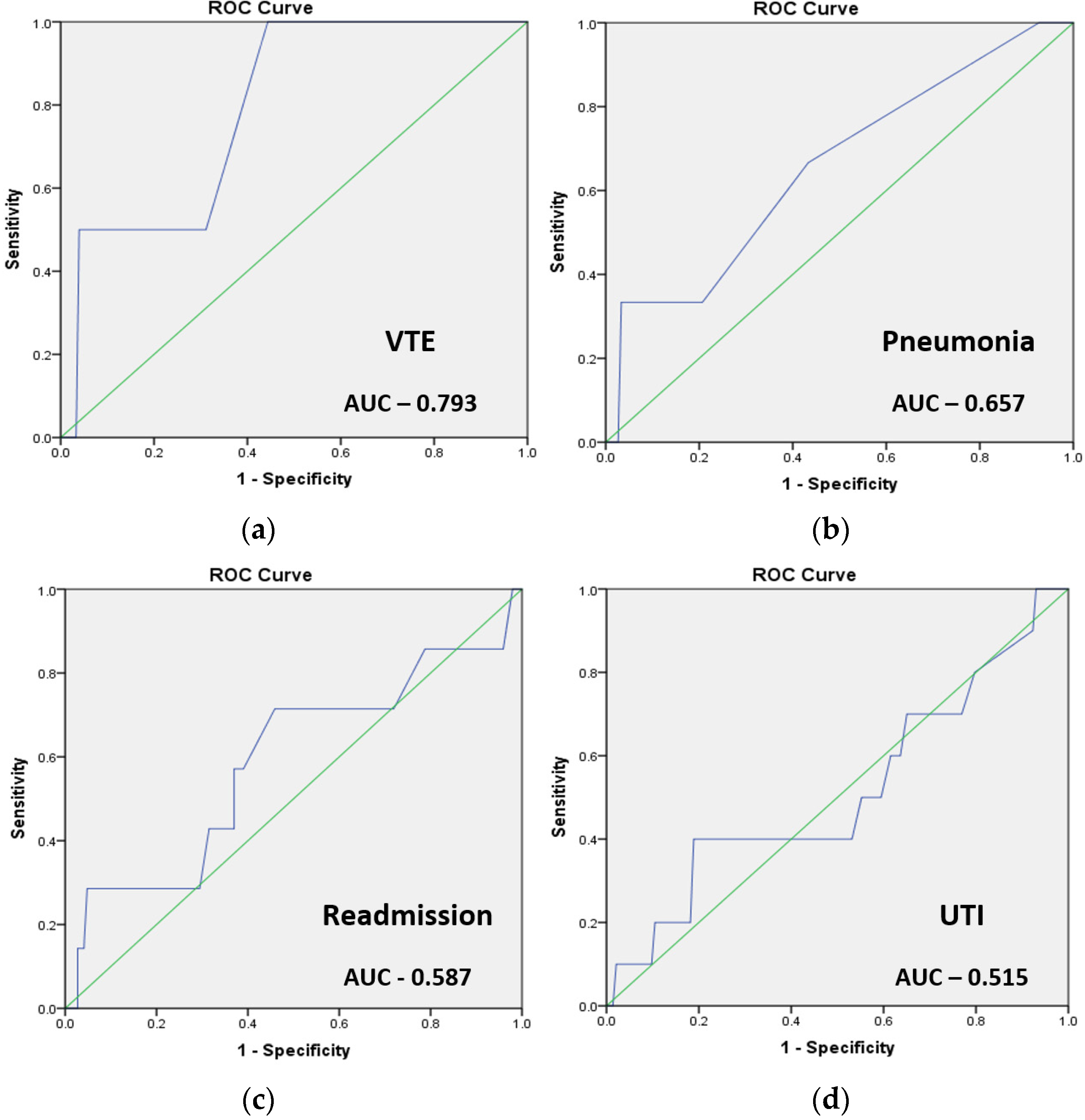
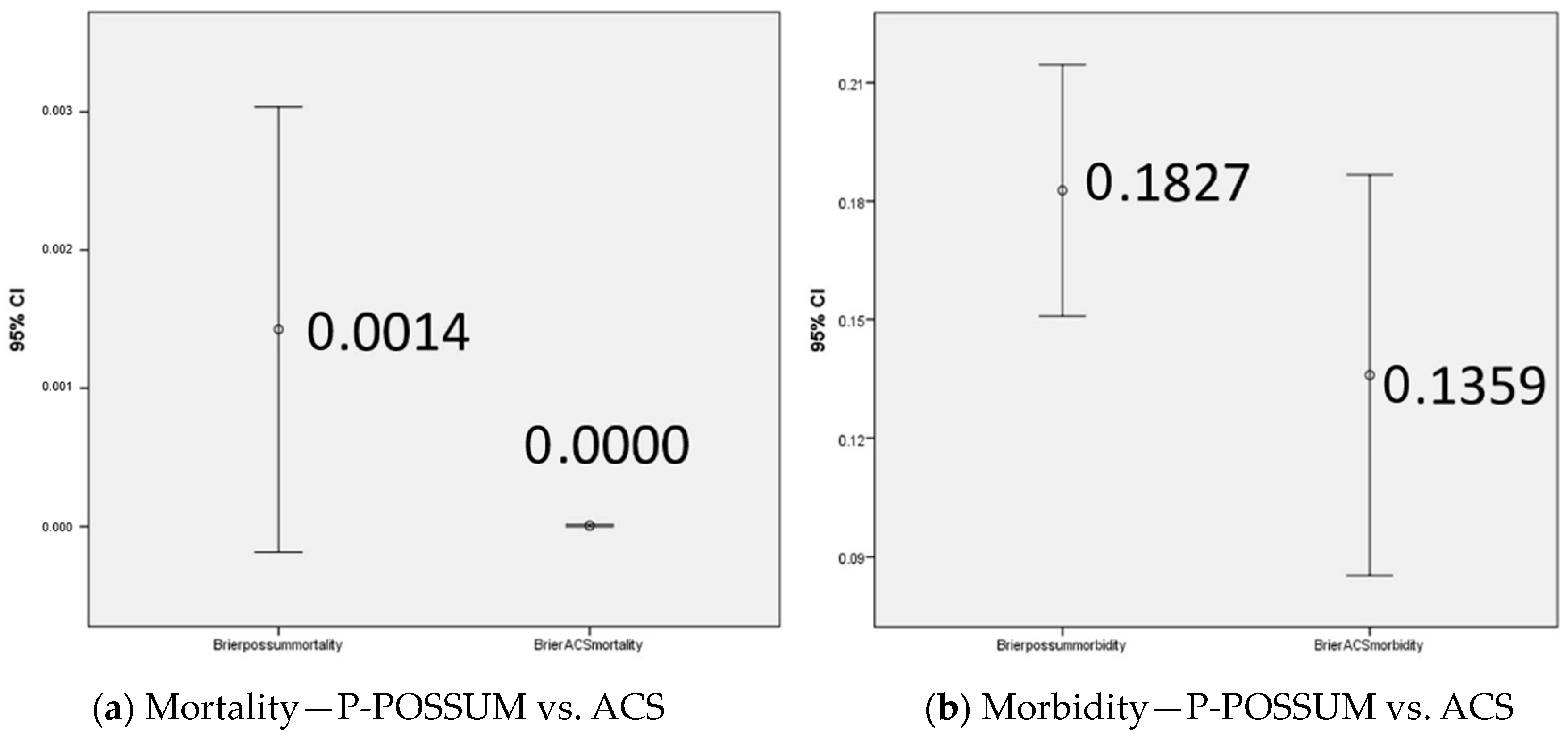
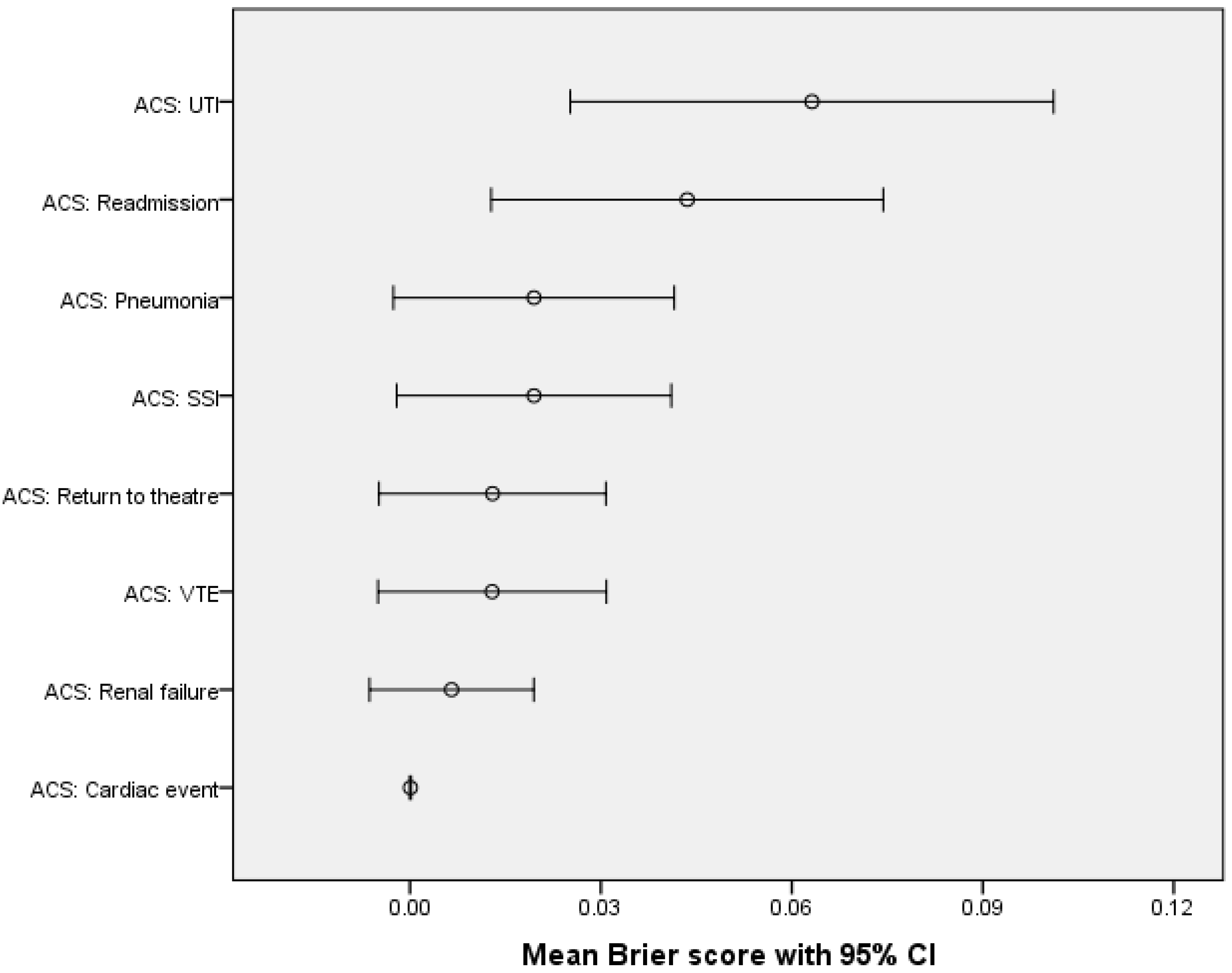
4. Results
5. Discussion
6. Limitations and Insights
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| P-POSSUM | Portsmouth POSSUM |
| POSSUM | Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity |
| ACS-NSQIP | The American College of Surgeons National Surgical Quality Improvement Program |
| NHS | The National Health Service |
| GO | Gynaecological–Oncological |
| RS | Robotic Surgery |
| VTE | Venous Thromboembolism |
| AUC | Area Under the Curve |
| MIS | Minimally Invasive Surgery |
| CPET | Cardio-Pulmonary Exercise Testing |
| UK | The United Kingdom |
| LOS | Length of Stay |
| USA | The United States of America |
| RSNFT | Royal Surrey NHS Foundation Trust |
| ASA | American Society of Anesthesiologists |
| SIRS | Systemic Inflammatory Response Syndrome |
| COPD | Chronic Obstructive Pulmonary Disease |
| BMI | Body Mass Index |
| POMS | Postoperative Morbidity Survey |
| FIGO | The International Federation of Gynecology and Obstetrics |
| CPT | Common Procedural Terminology |
| SSI | Surgical Site Infection |
| UTI | Urinary Tract Infection |
| PE | Pulmonary Embolism |
| DVT | Deep Vein Thrombosis |
| NPO | Nil Per Os |
| NGT | NasoGastric Tube |
| POD4 | Post Operative Day 4 |
| GI | Gastro-Intestinal |
| SPSS | Statistical Package for the Social Sciences |
| ROC | Receiver Operating Characteristic |
| EIN | Endometrial Intraepithelial Neoplasia |
| CIN | Cervical Intraepithelial Neoplasia |
| TLH | Total Laparoscopic Hysterectomy |
| BSO | Bilateral Salpingo Oophorectomy |
| RF | Renal Failure |
| GP | General Practitioner |
References
- Kinnersley, P.; Phillips, K.; Savage, K.; Kelly, M.J.; Farrell, E.; Morgan, B.; Whistance, R.; Lewis, V.; Mann, M.K.; Stephens, B.L.; et al. Interventions to promote informed consent for patients undergoing surgical and other invasive healthcare procedures. Cochrane Database Syst. Rev. 2013, 2013, 1–247. [Google Scholar] [CrossRef] [PubMed]
- Perrenoud, B.; Velonaki, V.S.; Bodenmann, P.; Ramelet, A.S. The effectiveness of health literacy interventions on the informed consent process of health care users: A systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 82–94. [Google Scholar] [CrossRef] [PubMed]
- Bowling, A.; Rowe, G.; Lambert, N.; Waddington, M.; Mahtani, K.; Kenten, C.; Howe, A.; Francis, S. The measurement of patients’ expectations for health care: A review and psychometric testing of a measure of patients’ expectations. Health Technol. Assess. 2012, 16, 1–515. [Google Scholar] [CrossRef] [PubMed]
- Stacey, D.; Légaré, F.; Col, N.F.; Bennett, C.L.; Barry, M.J.; Eden, K.B.; Holmes-Rovner, M.; Llewellyn-Thomas, H.; Lyddiatt, A.; Thomson, R.; et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst. Rev. 2014, 2014, CD001431. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Conrad, L.B.; Ramirez, P.T.; Burke, W.; Naumann, R.W.; Ring, K.L.; Munsell, M.F.; Frumovitz, M. Role of minimally invasive surgery in gynecologic oncology: An updated survey of members of the Society of Gynecologic Oncology. Int. J. Gynecol. Cancer 2015, 25, 1121. [Google Scholar] [CrossRef] [PubMed]
- Scarpelli, E.; Armano, G.; Monfardini, L.; Valenti, A.; Barresi, G.; De Finis, A.; Rotondella, I.; Scebba, D.; Butera, D. Minimally invasive surgery in gynecological cancers: Update and systematic review. Clin. Exp. Obstet. Gynecol. 2022, 49, 88. [Google Scholar] [CrossRef]
- Iyer, R.; Gentry-Maharaj, A.; Nordin, A.; Burnell, M.; Liston, R.; Manchanda, R.; Das, N.; Desai, R.; Gornall, R.; Beardmore-Gray, A.; et al. Predictors of complications in gynaecological oncological surgery: A prospective multicentre study (UKGOSOC-UK gynaecological oncology surgical outcomes and complications). Br. J. Cancer 2015, 112, 475–484. [Google Scholar] [CrossRef]
- Otto, J.M.; Levett, D.Z.H.; Grocott, M.P.W. Cardiopulmonary Exercise Testing for Preoperative Evaluation: What Does the Future Hold? Curr. Anesthesiol. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Reeves, T.; Bates, S.; Sharp, T.; Richardson, K.; Bali, S.; Plumb, J.; Anderson, H.; Prentis, J.; Swart, M.; Levett, D.Z.H.; et al. Cardiopulmonary exercise testing (CPET) in the United Kingdom-a national survey of the structure, conduct, interpretation and funding. Perioper. Med. 2018, 7, 2. [Google Scholar] [CrossRef]
- Copeland, G.P.; Jones, D.; Walters, M. POSSUM: A scoring system for surgical audit. Br. J. Surg. 2005, 78, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Prytherch, D.R.; Whiteley, M.S.; Higgins, B.; Weaver, P.C.; Prout, W.G.; Powell, S.J. POSSUM and Portsmouth POSSUM for predicting mortality. Br. J. Surg. 2003, 85, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Das, N.; Talaat, A.; Naik, R.; Lopes, A.; Godfrey, K.; Hatem, M.; Edmondson, R. Risk adjusted surgical audit in gynaecological oncology: P-POSSUM does not predict outcome. Eur. J. Surg. Oncol. 2006, 32, 1135–1138. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.; Lund, J.N.; Gold, S.; Elliott, R.; Vater, M.; Chakrabarty, M.P.; Heinink, T.P.; Williams, J.P. An evaluation of POSSUM and P-POSSUM scoring in predicting post-operative mortality in a level 1 critical care setting. BMC Anesthesiol. 2014, 14, 104. [Google Scholar] [CrossRef]
- Richards, C.H.; Leitch, F.E.; Horgan, P.G.; McMillan, D.C. A Systematic Review of POSSUM and its Related Models as Predictors of Post-operative Mortality and Morbidity in Patients Undergoing Surgery for Colorectal Cancer. J. Gastrointest. Surg. 2010, 14, 1511–1520. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Horgan, P.G.; McMillan, D.C. POSSUM and its related models as predictors of postoperative mortality and morbidity in patients undergoing surgery for gastro-oesophageal cancer: A systematic review. World J. Surg. 2010, 34, 2076–2082. [Google Scholar] [CrossRef] [PubMed]
- Second Patient Audit Report—The National Institute of Academic Anaesthesia. Available online: https://www.nela.org.uk/Second-Patient-Report-of-the-National-Emergency-Laparotomy-Audit (accessed on 6 April 2023).
- ACS NSQIP|ACS. Available online: https://www.facs.org/quality-programs/data-and-registries/acs-nsqip/ (accessed on 6 April 2023).
- Bilimoria, K.Y.; Liu, Y.; Paruch, J.L.; Zhou, L.; Kmiecik, T.E.; Ko, C.Y.; Cohen, M.E. Development and evaluation of the universal ACS NSQIP surgical risk calculator: A decision aid and informed consent tool for patients and surgeons. J. Am. Coll. Surg. 2013, 217, 833–842.e3. [Google Scholar] [CrossRef] [PubMed]
- Rivard, C.; Nahum, R.; Slagle, E.; Duininck, M.; Vogel, R.I.; Teoh, D. Evaluation of the performance of the ACS NSQIP surgical risk calculator in gynecologic oncology patients undergoing laparotomy. Gynecol. Oncol. 2016, 141, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Teoh, D.; Halloway, R.N.; Heim, J.; Vogel, R.I.; Rivard, C. Evaluation of the American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator in Gynecologic Oncology Patients Undergoing Minimally Invasive Surgery. J. Minim. Invasive Gynecol. 2017, 24, 48–54. [Google Scholar] [CrossRef]
- Murray, I.; Lim, K.; Howells, R.; Jones, R.; Sharma, A.; Jones, S. The Utility of a Personalised Risk Calculator in Gynae-Oncology Surgery. Clin. Oncol. Res. 2020, 3, 7. [Google Scholar] [CrossRef]
- Manning-Geist, B.; Cathcart, A.M.; Sullivan, M.W.; Pelletier, A.; Cham, S.; Muto, M.G.; Del Carmen, M.; Growdon, W.B.; Sisodia, R.C.; Berkowitz, R.; et al. Predictive validity of American College of Surgeons: National Surgical Quality Improvement Project risk calculator in patients with ovarian cancer undergoing interval debulking surgery. Int. J. Gynecol. Cancer 2021, 31, 1356–1362. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://riskcalculator.facs.org/RiskCalculator/PatientInfo.jsp (accessed on 24 May 2024).
- Austin, P.C.; Steyerberg, E.W. Interpreting the concordance statistic of a logistic regression model: Relation to the variance and odds ratio of a continuous explanatory variable. BMC Med. Res. Methodol. 2012, 12, 82. [Google Scholar] [CrossRef] [PubMed]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Kedia, A.; Goswami, J.; Chakraborty, A. Validity of P-POSSUM in adult cancer surgery (PACS). J. Anaesthesiol. Clin. Pharmacol. 2022, 38, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Dunn, S.M.; Patterson, P.U.; Butow, P.N.; Smartt, H.H.; McCarthy, W.H.; Tattersall, M.H.N. Cancer by another name: A randomized trial of the effects of euphemism and uncertainty in communicating with cancer patients. J. Clin. Oncol. 1993, 11, 989–996. [Google Scholar] [CrossRef]
- Szender, J.B.; Frederick, P.J.; Eng, K.H.; Akers, S.N.; Lele, S.B.; Odunsi, K. Evaluation of the National Surgical Quality Improvement Program Universal Surgical Risk Calculator for a gynecologic oncology service. Int. J. Gynecol. Cancer 2015, 25, 512–520. [Google Scholar] [CrossRef]
- Thigpen, B.; Eppes, C.; Schaumberg, J.; Johnson, E.; Sangi-Haghpeykar, H.; Swaim, L.S. Does the ACS NSQIP Surgical Risk Calculator Accurately Predict Surgical Outcomes for Benign Hysterectomy? [06H]. Obstet. Gynecol. 2020, 135, 82S–83S. [Google Scholar] [CrossRef]
- Cohen, M.E.; Bilimoria, K.Y.; Ko, C.Y.; Hall, B.L. Development of an American College of Surgeons National Surgery Quality Improvement Program: Morbidity and mortality risk calculator for colorectal surgery. J. Am. Coll. Surg. 2009, 208, 1009–1016. [Google Scholar] [CrossRef]

| Preoperative Parameters | Patient-Specific Options |
|---|---|
| Age group | Under 65 years/65–74 years/75–84 years/85 years or older |
| Sex | Female |
| Functional status | Independent/Partially Dependent/Totally Dependent |
| Emergency case | No/Yes |
| ASA class | I (healthy patient)/II (mild systemic disease)/III (severe systemic disease)/IV (severe systemic disease/constant threat to life)/V (moribund/not expected to survive surgery) |
| Steroid use for chronic condition | No/Yes |
| Ascites within 30 days of surgery | No/Yes |
| Systemic sepsis within 48 h prior to surgery | None/SIRS/Sepsis/Septic shock |
| Ventilator dependent | No/Yes |
| Disseminated cancer | No/Yes |
| Diabetes | No/Yes (on oral medication)/Yes (on insulin) |
| Hypertension requiring medication | No/Yes |
| Congestive heart failure in 30 days prior to surgery | No/Yes |
| Dyspnoea | No/With moderate exertion/At rest |
| Current smoker within 1 year | No/Yes |
| History of severe COPD | No/Yes |
| Dialysis | No/Yes |
| Acute renal failure | No/Yes |
| BMI | Kg/m2 |
| Outcome | Inclusion Criteria |
|---|---|
| Serious complication | Cardiac arrest, myocardial infarction, pneumonia, progressive renal insufficiency, acute renal failure, PE, DVT, return to the theatre, deep incisional SSI, organ space SSI, systemic sepsis, unplanned intubation, UTI, wound disruption. |
| Any complication | Superficial incisional SSI, deep incisional SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, PE, DVT, ventilator > 48 h, progressive renal insufficiency, acute renal failure, UTI, stroke, cardiac arrest, myocardial infarction, return to the theatre, systemic sepsis. |
| Pneumonia | Diagnosed using both radiologic (i.e., infiltrate, consolidation or opacity, cavitation) and clinical (e.g., fever, leukopenia/leukocytosis, culture results, patient symptoms) criteria. |
| Cardiac complication | Cardiac arrest or myocardial infarction. |
| SSI | Superficial incisional SSI, deep incisional SSI or organ space SSI. |
| UTI | Diagnosed using a combination of clinical symptoms and laboratory confirmation (e.g., urine culture, pyuria, positive dipstick) or initiation of appropriate antimicrobial therapy. |
| VTE | New thrombus within the venous system requiring therapy. |
| Renal failure | Progressive renal insufficiency or acute renal failure requiring dialysis. |
| Readmission | - |
| Return to theatre | Return to theatre for additional surgery that was not planned at the time of the initial surgery. |
| Death | - |
| Discharge to post-acute care | Discharge to a nursing home or rehabilitation facility. |
| Sepsis | - |
| Ileus * | Prolonged Postoperative NPO or NGT Use: Prolonged NPO status or NGT use for suctioning or decompression, more than 3 days postop (POD4 or later) OR reinsertion of NGT or reinstating NPO status any time POD4 or later within 30 days. |
| Anastomotic leak * | This includes air, fluid, GI contents or contrast material. With or without treatment. The presence of an infection/abscess thought to be related to an anastomosis, even if the leak cannot be definitively identified as visualised during an operation, or by contrast extravasation, would still be considered an anastomotic leak if this is indicated by the surgeon. |
| Variable | Overall Patients n = 153 N | % |
|---|---|---|
| Age Group | ||
| Under 65 years | 86 | 56.2% |
| 65–74 years | 38 | 24.8% |
| 75–84 years | 24 | 15.7% |
| 85 years or older | 5 | 3.3% |
| Mean age | 60 | |
| Standard deviation | 12.1 | |
| Functional Status | ||
| Independent | 152 | 99.4% |
| Partially dependent | 1 | 0.6% |
| Totally dependent | 0 | 0% |
| ASA Class | ||
| I | 22 | 14.4% |
| II | 101 | 66.0% |
| III | 30 | 19.6% |
| IV | 0 | 0% |
| V | 0 | 0% |
| Steroid Use | ||
| No | 150 | 98.0% |
| Yes | 3 | 2.0% |
| Ascites within 30 Days | ||
| No | 153 | 100.0% |
| Yes | 0 | 0% |
| Disseminated Cancer | ||
| No | 138 | 90.2% |
| Yes | 15 | 9.8% |
| Diabetes | ||
| No | 134 | 87.6% |
| Oral | 15 | 9.8% |
| Insulin | 4 | 2.6% |
| Hypertension | ||
| No | 99 | 64.7% |
| Yes | 54 | 35.3% |
| Heart Failure | ||
| No | 152 | 99.4% |
| Yes | 1 | 0.6% |
| Dyspnoea | ||
| No | 130 | 85.0% |
| With moderate exertion | 23 | 15.0% |
| At rest | 0 | 0% |
| Smoker | ||
| No | 130 | 85.0% |
| Yes | 23 | 15.0% |
| Severe COPD | ||
| No | 152 | 99.4% |
| Yes | 1 | 0.6% |
| BMI | ||
| Underweight (<18.5) | 0 | 0% |
| Normal (18.5–24.9) | 46 | 30.0% |
| Overweight (25.0–29.9) | 41 | 26.8% |
| Obese Class 1 (30.0–34.9) | 28 | 18.3% |
| Obese Class 2 (35.0–39.9) | 14 | 9.2% |
| Obese Class 3 (>39.9) | 24 | 15.7% |
| Mean BMI | 29.6 | |
| Standard Deviation | 8.63 |
| Tumour Site | N | % | N | FIGO Stage | N | |
|---|---|---|---|---|---|---|
| Ovary | 8 | 5.2 | Benign | 4 | n/a | n/a |
| Borderline | 1 | 1a | 1 | |||
| Invasive | 3 | 1c | 1 | |||
| 4a | 1 | |||||
| 4b | 1 | |||||
| Ovary operations | Uni-/bilateral salpingo- (and/or) oophorectomy | 8 | ||||
| Total laparoscopic hysterectomy | 6 | |||||
| Peritoneal washing | 3 | |||||
| Adhesiolysis | 2 | |||||
| Supracolic omentectomy | 2 | |||||
| Modified radical hysterectomy | 1 | |||||
| PLNS | 1 | |||||
| PALNS | 1 | |||||
| Infracolic omentectomy | 1 | |||||
| Appendicectomy | 1 | |||||
| Omental biopsy | 1 | |||||
| Uterus | 99 | 64.7 | Benign | 11 | n/a | n/a |
| EIN | 5 | n/a | n/a | |||
| Invasive | 83 | 1a | 43 | |||
| 1b | 25 | |||||
| 2 | 4 | |||||
| 2b | 1 | |||||
| 3a | 1 | |||||
| 3b | 2 | |||||
| 3c1 | 2 | |||||
| 3c2 | 1 | |||||
| 4a | 1 | |||||
| 4b | 3 | |||||
| Uterus operations | Total laparoscopic hysterectomy | 98 | ||||
| Uni-/bilateral salpingo- (and/or) oophorectomy | 94 | |||||
| Peritoneal washing | 80 | |||||
| PLNS | 43 | |||||
| Omental biopsy | 16 | |||||
| PALNS | 15 | |||||
| Adhesiolysis | 9 | |||||
| Mini-laparotomy | 7 | |||||
| Bilateral sentinel node assessment | 3 | |||||
| Excision of nodules from peritoneum | 2 | |||||
| Peritoneal biopsy | 2 | |||||
| Modified radical hysterectomy | 1 | |||||
| Infracolic omentectomy | 1 | |||||
| Appendicectomy | 1 | |||||
| Biopsy of lesion on round ligament | 1 | |||||
| Laparoscopic myomectomy | 1 | |||||
| Repair of intra-operative bladder injury | 1 | |||||
| Suture of vaginal tear | 1 | |||||
| Cervix | 45 | 29.4 | CIN | 1 | n/a | n/a |
| Invasive | 44 | 1a | 6 | |||
| 1b | 33 | |||||
| 2a | 1 * | |||||
| 2b | 2 * | |||||
| Cervix operations | Uni-/bilateral salpingo- (and/or) oophorectomy | 242 | ||||
| PLND | 23 | |||||
| Cystoscopy | 18 | |||||
| Laparoscopic radical hysterectomy | 16 | |||||
| Rigid sigmoidoscopy | 10 | |||||
| Total laparoscopic hysterectomy | 7 | |||||
| Insertion of cervical cerclage | 3 | |||||
| Sentinel node assessment | 2 | |||||
| Radical trachelectomy | 2 | |||||
| Vaginal trachelectomy | 2 | |||||
| Ovarian transposition | 1 | |||||
| Radical upper vaginectomy | 1 | |||||
| PLNS | 1 | |||||
| PALNS | 1 | |||||
| Zoladex injection | 1 | |||||
| Drainage of lymphocyst | 1 | |||||
| Excision of vulval lesion | 1 | |||||
| Ureteral stenting | 1 | |||||
| Peritoneal washings | 1 | |||||
| Other | 1 | 0.7 | n/a | n/a | n/a | n/a |
| Other operations | TLH, BSO, supracolic omentectomy | 1 | ||||
| Complication(s) Occurring within 30 Days | N | Mean | Std. Deviation | Std. Error Mean | |
|---|---|---|---|---|---|
| POSSUM morbidity | No | 130 | 30.926 | 18.319 | 1.607 |
| Yes | 23 | 31.869 | 15.310 | 3.192 | |
| ACS any complications | No | 130 | 4.920 | 2.524 | 0.221 |
| Yes | 23 | 5.865 | 2.955 | 0.616 | |
| ACS pneumonia | No | 150 | 0.212 | 0.323 | 0.028 |
| Yes | 3 | 0.209 | 0.176 | 0.037 | |
| ACS cardiac | No | 153 | 0.172 | 0.892 | 0.078 |
| Yes | 0 | 0.096 | 0.149 | 0.031 | |
| ACS SSI | No | 150 | 1.882 | 0.926 | 0.081 |
| Yes | 3 | 2.100 | 1.009 | 0.210 | |
| ACS UTI | No | 143 | 1.885 | 1.195 | 0.105 |
| Yes | 10 | 2.400 | 1.426 | 0.297 | |
| ACS VTE | No | 151 | 0.387 | 0.245 | 0.022 |
| Yes | 2 | 0.504 | 0.348 | 0.073 | |
| ACS RF | No | 152 | 0.080 | 0.155 | 0.014 |
| Yes | 1 | 0.135 | 0.187 | 0.039 | |
| ACS readmission | No | 146 | 3.425 | 1.863 | 0.163 |
| Yes | 7 | 3.943 | 1.986 | 0.414 | |
| ACS return to theatre | No | 151 | 1.212 | 0.394 | 0.035 |
| Yes | 2 | 1.183 | 0.351 | 0.073 |
| Mean | N | Std. Deviation | Std. Error Mean | ||
|---|---|---|---|---|---|
| Pair 1 | Brier P-POSSUM morbidity | 0.183 | 153 | 0.199 | 0.016 |
| Brier ACS morbidity | 0.136 | 153 | 0.318 | 0.026 | |
| Pair 2 | Brier P-POSSUM mortality | 0.001 | 153 | 0.010 | 0.001 |
| Brier ACS mortality | 0.000 | 153 | 0.000 | 0.000 | |
| N | Mean | Median | Std. Deviation | |
|---|---|---|---|---|
| Brier ACS pneumonia | 3 | 0.020 | 0.000 | 0.138 |
| Brier ACS cardiac | 0 | 0.000 | 0.000 | 0.001 |
| Brier ACS SSI | 3 | 0.020 | 0.000 | 0.135 |
| Brier ACS UTI | 10 | 0.063 | 0.000 | 0.238 |
| Brier ACS VTE | 2 | 0.013 | 0.000 | 0.112 |
| Brier ACS renal failure | 1 | 0.007 | 0.000 | 0.081 |
| Brier ACS readmission | 7 | 0.044 | 0.001 | 0.193 |
| Brier ACS return to theatre | 2 | 0.013 | 0.000 | 0.112 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sevinyan, L.; Asaalaarchchi, H.; Tailor, A.; Williams, P.; Evans, M.; Hodnett, D.; Arakkal, D.; Prabhu, P.; Flint, M.S.; Madhuri, T.K. Head-to-Head Comparison: P-POSSUM and ACS-NSQIP® in Predicting Perioperative Risk in Robotic Surgery for Gynaecological Cancers. Cancers 2024, 16, 2297. https://doi.org/10.3390/cancers16132297
Sevinyan L, Asaalaarchchi H, Tailor A, Williams P, Evans M, Hodnett D, Arakkal D, Prabhu P, Flint MS, Madhuri TK. Head-to-Head Comparison: P-POSSUM and ACS-NSQIP® in Predicting Perioperative Risk in Robotic Surgery for Gynaecological Cancers. Cancers. 2024; 16(13):2297. https://doi.org/10.3390/cancers16132297
Chicago/Turabian StyleSevinyan, Lusine, Hasanthi Asaalaarchchi, Anil Tailor, Peter Williams, Matthew Evans, Darragh Hodnett, Darshana Arakkal, Pradeep Prabhu, Melanie S. Flint, and Thumuluru Kavitha Madhuri. 2024. "Head-to-Head Comparison: P-POSSUM and ACS-NSQIP® in Predicting Perioperative Risk in Robotic Surgery for Gynaecological Cancers" Cancers 16, no. 13: 2297. https://doi.org/10.3390/cancers16132297
APA StyleSevinyan, L., Asaalaarchchi, H., Tailor, A., Williams, P., Evans, M., Hodnett, D., Arakkal, D., Prabhu, P., Flint, M. S., & Madhuri, T. K. (2024). Head-to-Head Comparison: P-POSSUM and ACS-NSQIP® in Predicting Perioperative Risk in Robotic Surgery for Gynaecological Cancers. Cancers, 16(13), 2297. https://doi.org/10.3390/cancers16132297





