No Indication for Routine Resection of Surgical Scars during Cytoreductive Surgery and HIPEC
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Macroscopic Assessment
2.3. CRS and HIPEC
2.4. Microscopic Assessment
2.5. Statistical Analysis
3. Results
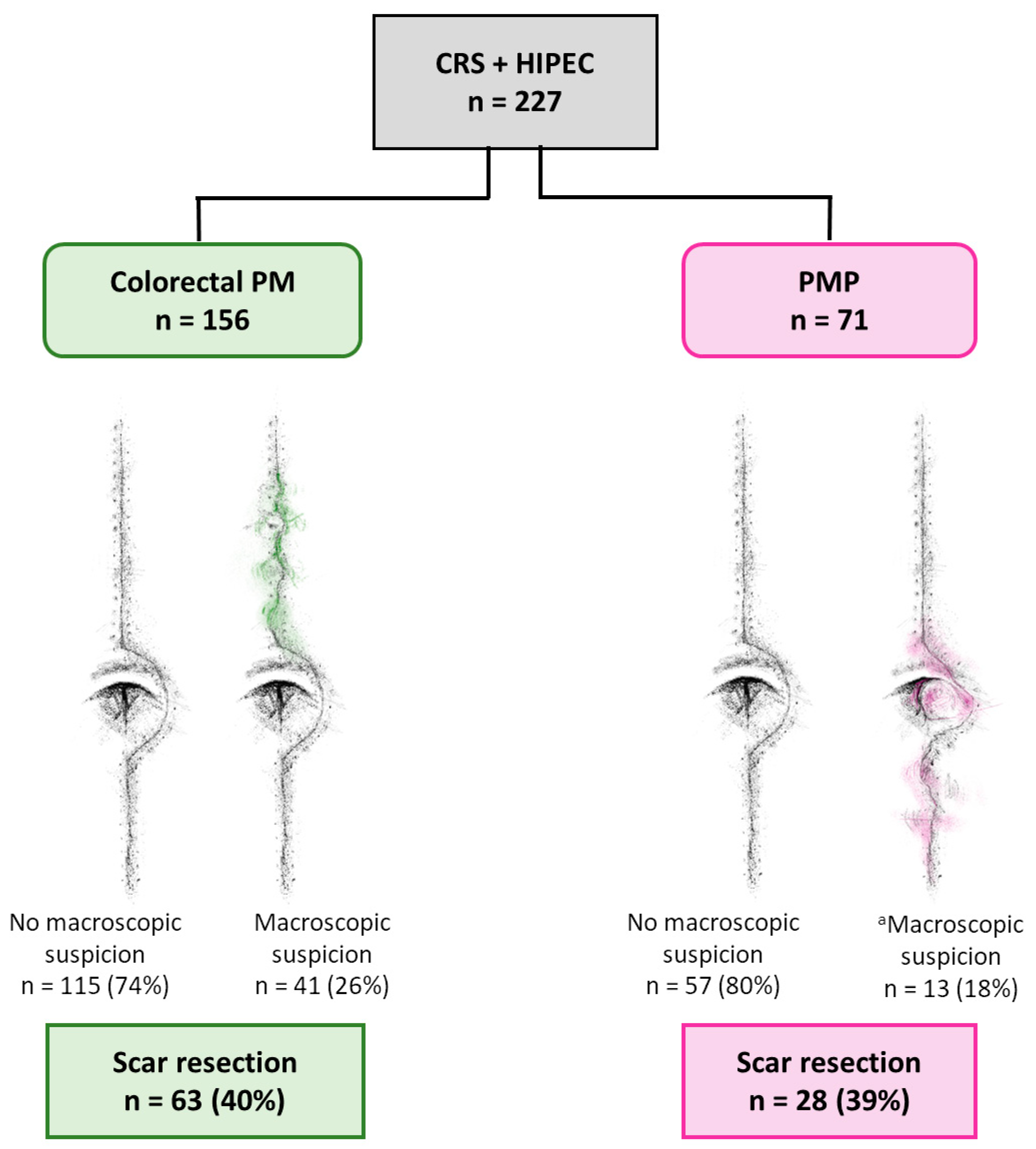
3.1. Study Population
3.2. Macroscopic Assessment
3.3. Histopathology of Colorectal PM
3.4. Histopathology of PMP
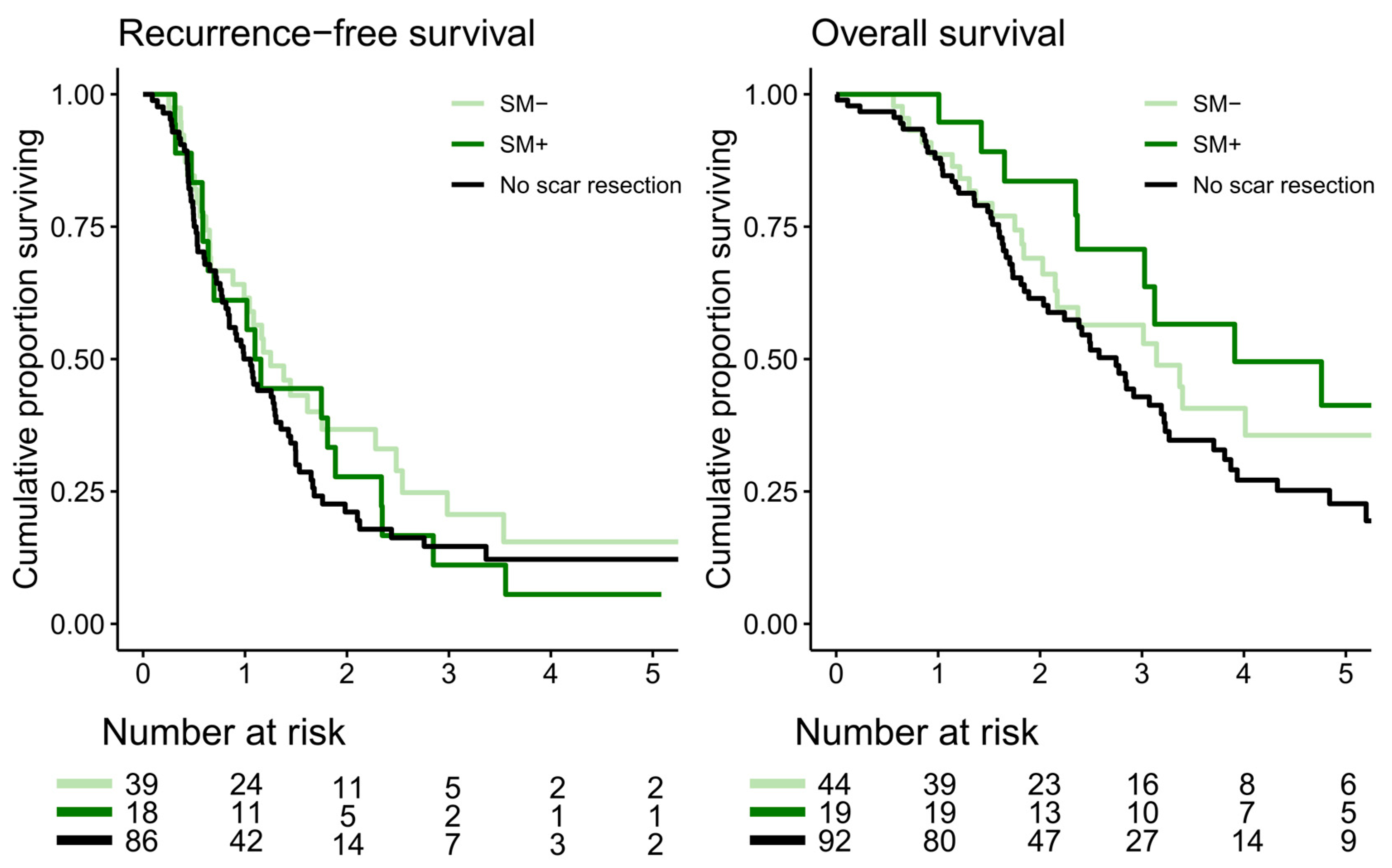
3.5. Recurrence and Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Verwaal, V.J.; Bruin, S.; Boot, H.; van Slooten, G.; van Tinteren, H. 8-year follow-up of randomized trial: Cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann. Surg. Oncol. 2008, 15, 2426–2432. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Q.; Min, Y.; Wang, S.Y.; Yang, X.J.; Liu, Y.; Xiong, B.; Yonemura, Y.; Li, Y. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy improves survival for peritoneal carcinomatosis from colorectal cancer: A systematic review and meta-analysis of current evidence. Oncotarget 2017, 8, 55657–55683. [Google Scholar] [CrossRef] [PubMed]
- Chua, T.C.; Moran, B.J.; Sugarbaker, P.H.; Levine, E.A.; Glehen, O.; Gilly, F.N.; Baratti, D.; Deraco, M.; Elias, D.; Sardi, A.; et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J. Clin. Oncol. 2012, 30, 2449–2456. [Google Scholar] [CrossRef] [PubMed]
- Sugarbaker, P.H. Peritonectomy procedures. Ann. Surg. 1995, 221, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Mittal, R.; Chandramohan, A.; Moran, B. Pseudomyxoma peritonei: Natural history and treatment. Int. J. Hyperthermia 2017, 33, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Reilly, W.T.; Nelson, H.; Schroeder, G.; Wieand, H.S.; Bolton, J.; O‘Connell, M.J. Wound recurrence following conventional treatment of colorectal cancer. A rare but perhaps underestimated problem. Dis. Colon. Rectum. 1996, 39, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Zoetmulder, F.A.; Sugarbaker, P.H. Patterns of failure following treatment of pseudomyxoma peritonei of appendiceal origin. Eur. J. Cancer. 1996, 32, 1727–1733. [Google Scholar] [CrossRef] [PubMed]
- Curet, M.J. Port site metastases. Am. J. Surg. 2004, 187, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Nunez, M.F.; Sardi, A.; Nieroda, C.; Jimenez, W.; Sittig, M.; MacDonald, R.; Aydin, N.; Milovanov, V.; Gushchin, V. Morbidity of the abdominal wall resection and reconstruction after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC). Ann. Surg. Oncol. 2015, 22, 1658–1663. [Google Scholar] [CrossRef]
- Parikh, R.; Shah, S.; Dhurandhar, V.; Alzahrani, N.; Fisher, O.M.; Arrowaili, A.; Liauw, W.; Morris, D. An analysis of the morbidity associated with abdominal wall resection and reconstruction after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC). Eur. J. Surg. Oncol. 2019, 45, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Jacquet, P.; Sugarbaker, P.H. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat. Res. 1996, 82, 359–374. [Google Scholar] [PubMed]
- Stephens, A.D.; Alderman, R.; Chang, D.; Edwards, G.D.; Esquivel, J.; Sebbag, G.; Steves, M.A.; Sugarbaker, P.H. Morbidity and mortality analysis of 200 treatments with cytoreductive surgery and hyperthermic intraoperative intraperitoneal chemotherapy using the coliseum technique. Ann. Surg. Oncol. 1999, 6, 790–796. [Google Scholar] [CrossRef]
- Gonzalez-Moreno, S.; Gonzalez-Bayon, L.A.; Ortega-Perez, G. Hyperthermic intraperitoneal chemotherapy: Rationale and technique. World J. Gastrointest. Oncol. 2010, 2, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Bosman, F.; Carniero, F.; Hruban, R.; Theise, N. WHO Classification of Tumours of the Digestive System; IARC Press: Lyon, France, 2010. [Google Scholar]
- Ronnett, B.M.; Zahn, C.M.; Kurman, R.J.; Kass, M.E.; Sugarbaker, P.H.; Shmookler, B.M. Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. A clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to “pseudomyxoma peritonei”. Am. J. Surg. Pathol. 1995, 19, 1390–1408. [Google Scholar] [CrossRef] [PubMed]
- Carr, N.J.; Cecil, T.D.; Mohamed, F.; Sobin, L.H.; Sugarbaker, P.H.; Gonzalez-Moreno, S.; Taflampas, P.; Chapman, S.; Moran, B.J. A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia: The Results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am. J. Surg. Pathol. 2016, 40, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Nunez, M.F.; Sardi, A.; Jimenez, W.; Nieroda, C.; Sittig, M.; MacDonald, R.; Aydin, N.; Milovanov, V.; Gushchin, V. Port-site metastases is an independent prognostic factor in patients with peritoneal carcinomatosis. Ann. Surg. Oncol. 2015, 22, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
- Carboni, F.; Federici, O.; Giofre, M.; Valle, M. An 18-Year Experience in Diagnostic Laparoscopy of Peritoneal Carcinomatosis: Results from 744 Patients. J. Gastrointest. Surg. 2020, 24, 2096–2103. [Google Scholar] [CrossRef] [PubMed]
- Berger, Y.; Jacoby, H.; Kaufmann, M.I.; Ben-Yaacov, A.; Westreich, G.; Sharon, I.; Barda, L.; Sharif, N.; Nadler, R.; Horesh, N.; et al. Correlation Between Intraoperative and Pathological Findings for Patients Undergoing Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy. Ann. Surg. Oncol. 2019, 26, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Enblad, M.; Birgisson, H.; Wanders, A.; Skoldberg, F.; Ghanipour, L.; Graf, W. Importance of Absent Neoplastic Epithelium in Patients Treated With Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy. Ann. Surg. Oncol. 2016, 23, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Al-Azzawi, M.; Misdraji, J.; van Velthuysen, M.F.; Shia, J.; Taggart, M.W.; Yantiss, R.K.; Svrcek, M.; Carr, N. Acellular mucin in pseudomyxoma peritonei of appendiceal origin: What is adequate sampling for histopathology? J. Clin. Pathol. 2020, 73, 220–222. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Colorectal PM n = 156 n (%) | PMP n = 71 n (%) |
|---|---|---|
| #Sex | ||
| Male | 71 (46) | 28 (39) |
| Female | 85 (54) | 43 (61) |
| Age, years (median, IQR) | 67 (56–71) | 59 (51–68) |
| Primary tumor localization | ||
| Appendix | 6 (4) | 70 (99) |
| Right colon | 73 (47) | 0 (0) |
| Left colon | 52 (33) | 0 (0) |
| Rectum | 20 (13) | 0 (0) |
| Colorectal NOS | 5 (3) | 1 (1) |
| Previous surgery | ||
| a Primary tumor resection | 46 (29) | 1 (1) |
| b Exploratory laparoscopy/laparotomy | 85 (54) | 68 (96) |
| c Both | 25 (16) | 1 (1) |
| Neoadjuvant treatment | 37 (24) | 2 (3) |
| PCI (median, IQR) | 10 (5–18) | 9 (6–20) |
| CCS | ||
| 0 | 149 (96) | 60 (85) |
| 1 | 7 (4) | 11 (15) |
| Characteristics | Scar Metastasis n = 19 n (%) | No Scar Metastasis n = 44 n (%) | p-Value |
|---|---|---|---|
| Sex | 0.58 | ||
| Male | 10 (53) | 19 (43) | |
| Female | 9 (47) | 25 (57) | |
| Age, years (median, IQR) | 67 (59–71) | 65 (53–71) | 0.52 |
| Previous surgery | 0.10 | ||
| a Primary tumor resection | 4 (21) | 2 (5) | |
| b Exploratory laparoscopy/laparotomy | 10 (53) | 31 (70) | |
| c Both | 5 (26) | 11 (25) | |
| Primary tumor localization | 0.73 | ||
| Appendix | 0 (0) | 3 (7) | |
| Right colon | 9 (47) | 23 (52) | |
| Left colon | 6 (32) | 11 (25) | |
| Rectum | 4 (21) | 7 (16) | |
| Colorectal NOS | 0 (0) | 0 (0) | |
| d Peritoneal metastasis histopathology | 0.27 | ||
| Adenocarcinoma | 10 (53) | 6 (14) | |
| Mucinous adenocarcinoma | 7 (37) | 12 (27) | |
| Signet ring cell carcinoma | 2 (11) | 1 (2) | |
| No neoplastic disease | 0 (0) | 3 (7) | |
| PCI (median, IQR) | 12 (9–18) | 10 (6–17) | 0.33 |
| CCS | 1.00 | ||
| 0 | 19 (100) | 42 (95) | |
| 1 | 0 (0) | 2 (5) |
| Characteristics | Scar Metastasis n = 12 n (%) | No Scar Metastasis n = 16 n (%) | p-Value |
|---|---|---|---|
| Sex | 0.70 | ||
| Male | 6 (50) | 6 (38) | |
| Female | 6 (50) | 10 (63) | |
| Age, years (median, IQR) | 67 (55–72) | 52 (46–57) | 0.03 |
| Previous surgery | 0.43 | ||
| a Primary tumor resection | 0 (0) | 0 (0) | |
| b Exploratory laparoscopy/laparotomy | 11 (92) | 16 (100) | |
| c Both | 1 (8) | 0 (0) | |
| d Peritoneal metastasis histopathology | 0.40 | ||
| Acellular mucin | 3 (25) | 2 (13) | |
| PSOGI MCP G1 | 1 (8) | 4 (25) | |
| PSOGI MCP G2 | 5 (45) | 5 (31) | |
| PSOGI MCP G3 | 3 (25) | 2 (13) | |
| No neoplastic disease | 0 (0) | 3 (19) | |
| PCI (median, IQR) | 20 (11–28) | 12 (6–22) | 0.77 |
| CCS | 0.65 | ||
| 0 | 9 (75) | 12 (75) | |
| 1 | 3 (25) | 4 (25) |
| RFS Univariate HR (95% CI) | RFS Multivariate HR (95% CI) | OS Univariate HR (95% CI) | OS Multivariate HR (95% CI) | |
|---|---|---|---|---|
| PCI | 1.04 (1.01–1.06) | 1.05 (1.02–1.07) | 1.06 (1.03–1.07) | 1.06 (1.03–1.09) |
| CCS | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 1.27 (0.51–3.13) | 0.48 (0.17–1.32) | 2.04 (0.82–5.03) | 0.63 (0.23–1.71) |
| Scar resection | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 0.80 (0.55–1.16) | 0.69 (0.47–1.01) | 0.71 (0.47–1.09) | 0.67 (0.44–1.04) |
| RFS Univariate HR (95% CI) | RFS Multivariate HR (95% CI) | OS Univariate HR (95% CI) | OS Multivariate HR (95% CI) | |
|---|---|---|---|---|
| PCI | 1.06 (1.02–1.11) | 1.011(1.05–1.18 | 1.04 (0.99–1.09) | 1.06 (1.03–1.09) |
| CCS | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 0.80 (0.24–2.73) | 0.18 (0.04–0.74) | 0.51 (0.11–2.82) | 0.16 (0.03–0.90) |
| Scar resection | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.16 (0.49–2.71) | 0.86 (0.34–2.15) | 1.09 (0.41–2.87) | 1.09 (1.02–1.16) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enblad, M.; Ghanipour, L.; Cashin, P.; Birgisson, H.; Graf, W. No Indication for Routine Resection of Surgical Scars during Cytoreductive Surgery and HIPEC. Cancers 2024, 16, 2099. https://doi.org/10.3390/cancers16112099
Enblad M, Ghanipour L, Cashin P, Birgisson H, Graf W. No Indication for Routine Resection of Surgical Scars during Cytoreductive Surgery and HIPEC. Cancers. 2024; 16(11):2099. https://doi.org/10.3390/cancers16112099
Chicago/Turabian StyleEnblad, Malin, Lana Ghanipour, Peter Cashin, Helgi Birgisson, and Wilhelm Graf. 2024. "No Indication for Routine Resection of Surgical Scars during Cytoreductive Surgery and HIPEC" Cancers 16, no. 11: 2099. https://doi.org/10.3390/cancers16112099
APA StyleEnblad, M., Ghanipour, L., Cashin, P., Birgisson, H., & Graf, W. (2024). No Indication for Routine Resection of Surgical Scars during Cytoreductive Surgery and HIPEC. Cancers, 16(11), 2099. https://doi.org/10.3390/cancers16112099





