Aesthetic Evaluation of Facial Scars in Patients Undergoing Surgery for Basal Cell Carcinoma: A Prospective Longitudinal Pilot Study and Validation of POSAS 2.0 in the Lithuanian Language
Abstract
Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Procedures and Ethics Statement
2.2. Patients
2.3. Administered Outcome Measures
2.3.1. The Patient and Observer Scar Assessment Scale
2.3.2. The Skin Cancer Index
2.3.3. The Dermatology Life Quality Index
2.4. Validation Phase
2.4.1. Translation and Cultural Adaptation
- Forward translation.
- Backward translation.
- Testing.
- Finalisation.
2.4.2. Statistical Analysis
- Internal consistency.
- Structural validity.
- Construct validity.
- Criterion validity.
- Positive correlation between PSAS-II and DLQI-II overall scores.
- Positive correlation between PSAS-II-Q1 and DLQI-II-Q1.
- Positive correlation between PSAS-II-Q2 and DLQI-II-Q2.
- Measurement error and reliability.
- Responsiveness.
2.5. Pilot Phase
2.5.1. PSAS Score Correlations with QoL
2.5.2. Segment Analysis and the POSAS Score Differences across Anatomic Units
3. Results
3.1. Descriptive Statistics
3.2. Translation and Cultural Adaptation
3.3. Internal Consistency
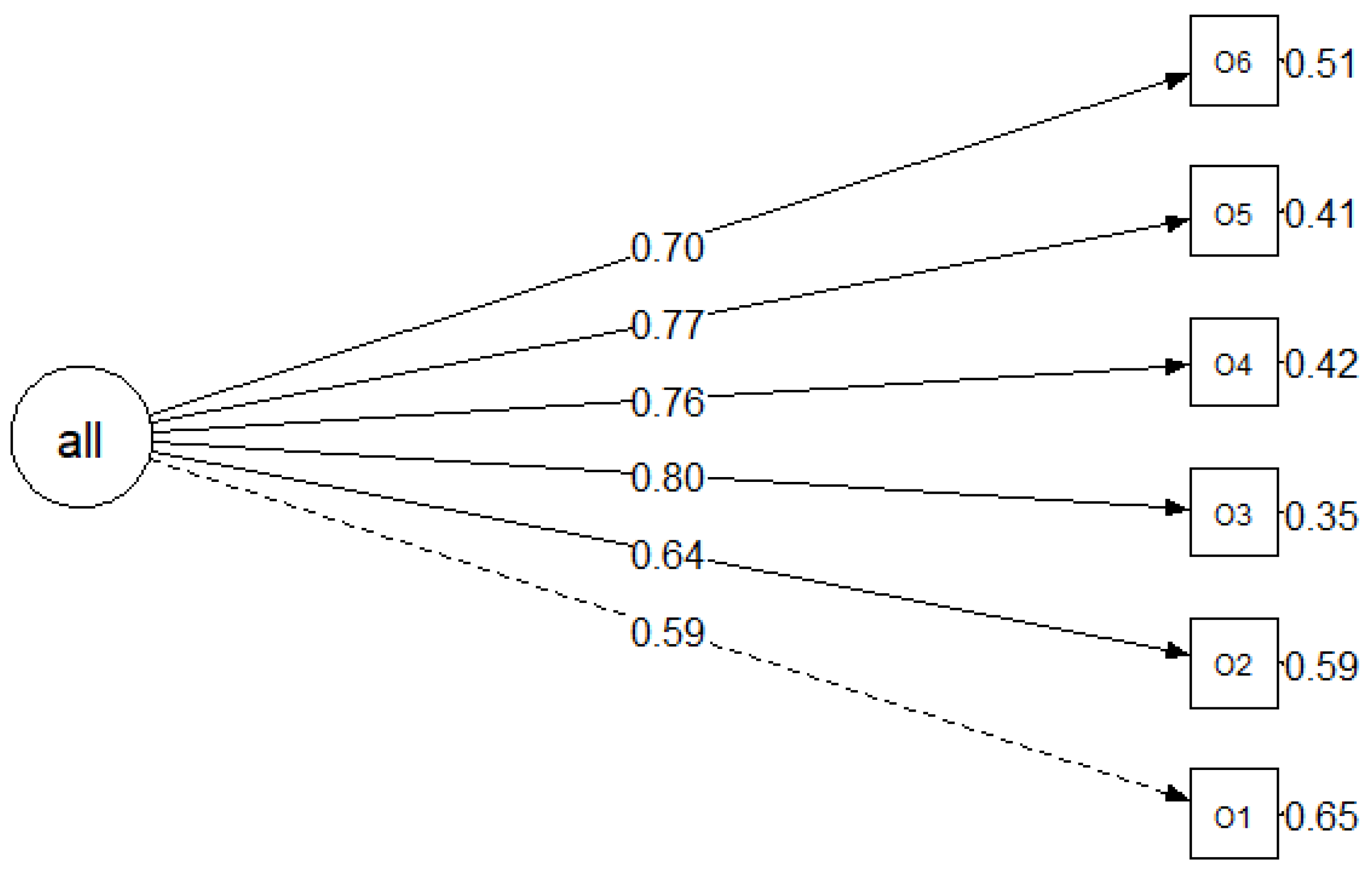
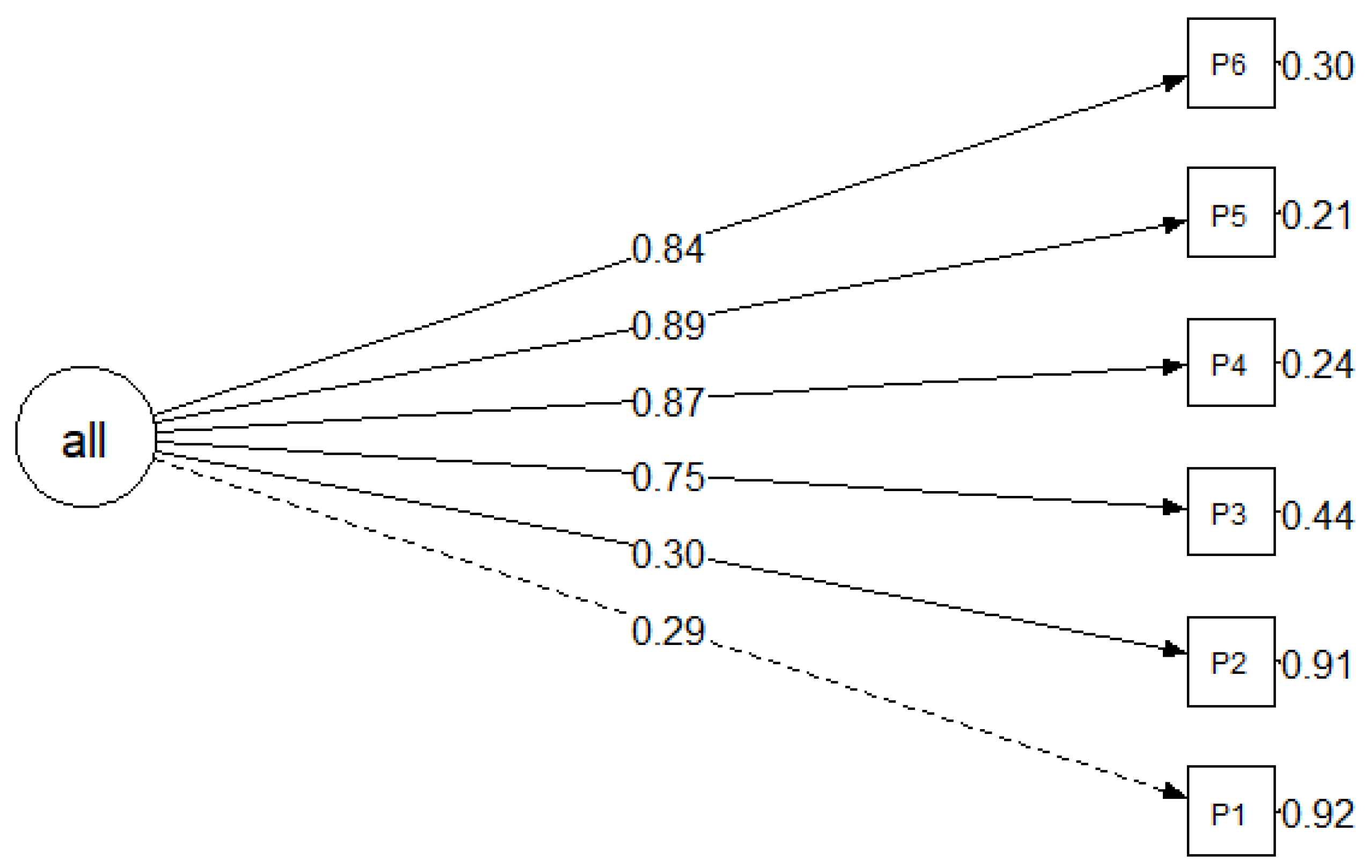
3.4. Structural Validity
3.5. Construct Validity
3.6. Criterion validity
3.7. Measurement Error and Reliability
3.7.1. PSAS
3.7.2. OSAS
3.8. Responsiveness and Agreement between the PSAS and OSAS
3.9. Correlations between the Scar Assessment and QoL
3.10. Segment Analysis and the POSAS Score Differences across Anatomic Units
- Eyelid 80–91 age group, n = 1;
- Upper lip 57–69 age group, n = 1;
- Eyelid T group, n = 1;
- Upper lip P group −1, n = 1;
- Upper lip T group, n = 1;
- Nose > 15 mm tumour group, n = 1;
- Eyelid > 15 mm tumour group, n = 1;
- Upper lip > 15 mm tumour group, n = 1.
3.10.1. Scar Assessment 1 Month Post-Surgery
3.10.2. Scar Assessment 6 Months Post-Surgery
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leiter, U.; Keim, U.; Garbe, C. Epidemiology of Skin Cancer: Update 2019. Adv. Exp. Med. Biol. 2020, 1268, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Ciążyńska, M.; Kamińska-Winciorek, G.; Lange, D.; Lewandowski, B.; Reich, A.; Sławińska, M.; Pabianek, M.; Szczepaniak, K.; Hankiewicz, A.; Ułańska, M.; et al. Author Correction: The Incidence and Clinical Analysis of Non-melanoma Skin Cancer. Sci. Rep. 2021, 11, 15705. [Google Scholar] [CrossRef] [PubMed]
- Basset-Seguin, N.; Herms, F. Update in the Management of Basal Cell Carcinoma. Acta Derm. Venereol. 2020, 100, adv00140. [Google Scholar] [CrossRef] [PubMed]
- Gulati, A.; Grekin, R.; Neuhaus, I.; Saylor, D.; Yu, S.; Park, A.; Seth, R.; Knott, P.D. Long-Term Appearance-Related Outcomes of Facial Reconstruction after Skin Cancer Resection. Facial Plast. Surg. Aesthet. Med. 2023, 25, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Tebble, N.J.; Adams, R.; Thomas, D.W.; Price, P. Anxiety and Self-Consciousness in Patients with Facial Lacerations One Week and Six Months Later. Br. J. Oral. Maxillofac. Surg. 2006, 44, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.C.; McKenna, S.P.; Siddhi, K.; McGrouther, D.A.; Bayat, A. The Hidden Cost of Skin Scars: Quality of Life after Skin Scarring. J. Plast. Reconstr. Aesthet. Surg. 2008, 61, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Sobanko, J.F.; Sarwer, D.B.; Zvargulis, Z.; Miller, C.J. Importance of Physical Appearance in Patients with Skin Cancer. Dermatol. Surg. 2015, 41, 183–188. [Google Scholar] [CrossRef]
- Shao, K.; Taylor, L.; Miller, C.J.; Etzkorn, J.R.; Shin, T.M.; Higgins, H.W.; Giordano, C.N.; Sobanko, J.F. The Natural Evolution of Facial Surgical Scars: A Retrospective Study of Physician-Assessed Scars Using the Patient and Observer Scar Assessment Scale Over Two Time Points. Facial Plast. Surg. Aesthet. Med. 2021, 23, 330–338. [Google Scholar] [CrossRef]
- Wang, T.T.; Wessels, L.; Hussain, G.; Merten, S. Discriminative Thresholds in Facial Asymmetry: A Review of the Literature. Aesthet. Surg. J. 2017, 37, 375–385. [Google Scholar] [CrossRef]
- Dixon, A.J.; Dixon, M.P.; Dixon, J.B. Prospective Study of Long-Term Patient Perceptions of Their Skin Cancer Surgery. J. Am. Acad. Dermatol. 2007, 57, 445–453. [Google Scholar] [CrossRef]
- Fix, W.C.; Etzkorn, J.R.; Zhang, J.; Sobanko, J.F. Patient Scar Assessment Correlates with Quality of Life after Mohs Micrographic Surgery. Dermatol. Surg. 2020, 46, 1745–1747. [Google Scholar] [CrossRef] [PubMed]
- van de Kar, A.L.; Corion, L.U.M.; Smeulders, M.J.C.; Draaijers, L.J.; van der Horst, C.M.A.M.; van Zuijlen, P.P.M. Reliable and Feasible Evaluation of Linear Scars by the Patient and Observer Scar Assessment Scale. Plast. Reconstr. Surg. 2005, 116, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Draaijers, L.J.; Tempelman, F.R.H.; Botman, Y.A.M.; Tuinebreijer, W.E.; Middelkoop, E.; Kreis, R.W.; van Zuijlen, P.P.M. The Patient and Observer Scar Assessment Scale: A Reliable and Feasible Tool for Scar Evaluation. Plast. Reconstr. Surg. 2004, 113, 1960–1965; discussion 1966–1967. [Google Scholar] [CrossRef] [PubMed]
- Vercelli, S.; Ferriero, G.; Sartorio, F.; Cisari, C.; Bravini, E. Clinimetric Properties and Clinical Utility in Rehabilitation of Postsurgical Scar Rating Scales: A Systematic Review. Int. J. Rehabil. Res. 2015, 38, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Franchignoni, F.; Giordano, A.; Vercelli, S.; Bravini, E.; Stissi, V.; Ferriero, G. Rasch Analysis of the Patient and Observer Scar Assessment Scale in Linear Scars: Suggestions for a Patient and Observer Scar Assessment Scale v2.1. Plast. Reconstr. Surg. 2019, 144, 1073e–1079e. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.-H.; Kwon, S.-H.; Kim, K.-J.; Lee, J.-M.; Yoon, J.-M.; Cheon, J.-H.; Yoon, E.-S.; Park, S.-H. Reliability of the Patient and Observer Scar Assessment Scale in Evaluating Linear Scars after Thyroidectomy. Adv. Skin. Wound Care 2021, 34, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Seyyah, M.; Yurdalan, S.U. Cultural Adaptation and Validation of Patient and Observer Scar Assessment Scale for Turkish Use. Burns 2018, 44, 1352–1356. [Google Scholar] [CrossRef] [PubMed]
- Lenzi, L.; Santos, J.; Raduan Neto, J.; Fernandes, C.H.; Faloppa, F. The Patient and Observer Scar Assessment Scale: Translation for Portuguese Language, Cultural Adaptation, and Validation. Int. Wound J. 2019, 16, 1513–1520. [Google Scholar] [CrossRef]
- Hjellestad, M.; Strand, L.I.; Eide, G.E.; Brekke, R.; Nesheim, A.; Gjelsvik, B.E.B. Clinimetric Properties of a Translated and Culturally Adapted Norwegian Version of the Patient and Observer Scar Assessment Scale for Use in Clinical Practice and Research. Burns 2021, 47, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Lahdenperä, N.-I.; Lindford, A.; Kautiainen, H.; Paloneva, J.; Hietanen, K.; Vuola, J.; Repo, J.P. Translation and Psychometric Validation of the Finnish Version of the Patient Scar Assessment Scale for Use in Patients with Burn Scars. Burns 2023, 49, 1113–1121. [Google Scholar] [CrossRef]
- Deslauriers, V.; Rouleau, D.M.; Alami, G.; MacDermid, J.C. Translation of the Patient Scar Assessment Scale (PSAS) to French with Cross-Cultural Adaptation, Reliability Evaluation and Validation. Can. J. Surg. 2009, 52, E259–E263. [Google Scholar]
- Al-Drees, T.; Albosaily, A.; Alanazi, L.; Alharethy, S.; AlHindi, G.; Altuwaijri, A.; Aldhahri, S. Translation and Cultural Adaptation of an Arabic Version of the Patient Scar Assessment Scale for Thyroidectomy Patients. Saudi Med. J. 2019, 40, 590–594. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN Checklist for Assessing the Methodological Quality of Studies on Measurement Properties of Health Status Measurement Instruments: An International Delphi Study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN Study Reached International Consensus on Taxonomy, Terminology, and Definitions of Measurement Properties for Health-Related Patient-Reported Outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef]
- Fattahi, T.T. An Overview of Facial Aesthetic Units. J. Oral. Maxillofac. Surg. 2003, 61, 1207–1211. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P.; ISPOR Task Force for Translation and Cultural Adaptation. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making Sense of Cronbach’s Alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Jackson, D.L.; Gillaspy, J.A.; Purc-Stephenson, R. Reporting Practices in Confirmatory Factor Analysis: An Overview and Some Recommendations. Psychol. Methods 2009, 14, 6–23. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality Criteria Were Proposed for Measurement Properties of Health Status Questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Vercelli, S.; Ferriero, G.; Bravini, E.; Stissi, V.; Ciceri, M.; Rossetti, S.; Bianchi, S.; Sartorio, F. Cross-Cultural Adaptation, Reproducibility and Validation of the Italian Version of the Patient and Observer Scar Assessment Scale (POSAS). Int. Wound J. 2017, 14, 1262–1268. [Google Scholar] [CrossRef] [PubMed]
- Shao, K.; Parker, J.C.; Taylor, L.; Mitra, N.; Sobanko, J.F. Reliability of the Patient and Observer Scar Assessment Scale When Used with Postsurgical Scar Photographs. Dermatol. Surg. 2018, 44, 1650–1652. [Google Scholar] [CrossRef] [PubMed]
- Shao, K.; Zullo, S.W.; Fix, W.; Taylor, L.; Zhang, J.; Miller, C.J.; Etzkorn, J.R.; Shin, T.M.; Giordano, C.N.; Higgins, W.H.; et al. Measuring Stakeholder Assessments of Postsurgical Facial Scars: A Retrospective Cohort Inter-Rater Analysis of Patients, Physicians, and Medical Student Observers. Dermatol. Surg. 2022, 48, 418–422. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.H.; Bae, Y.C. Analysis of Frequency of Use of Different Scar Assessment Scales Based on the Scar Condition and Treatment Method. Arch. Plast. Surg. 2014, 41, 111–115. [Google Scholar] [CrossRef]
- Vercelli, S.; Ferriero, G.; Sartorio, F.; Stissi, V.; Franchignoni, F. How to Assess Postsurgical Scars: A Review of Outcome Measures. Disabil. Rehabil. 2009, 31, 2055–2063. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics, n = 100 | |
|---|---|
| Age | 68.31 ± 12.979 |
| 34–56 years | 20 |
| 57–69 years | 27 |
| 70–79 years | 32 |
| 80–91 years | 21 |
| Gender, n (%) | |
| Female | 72 (72%) |
| Male | 28 (28%) |
| Marital status, n (%) | |
| Divorced | 9 (9%) |
| Widow/widower | 22 (22%) |
| Living together with a partner | 4 (4%) |
| Dating but living separately | 1 (1%) |
| Married | 59 (59%) |
| Single | 5 (5%) |
| Education, n (%) | |
| Non-university higher education | 22 (22%) |
| Other (professional schools) | 8 (8%) |
| Basic (8–10 grades) | 5 (5%) |
| Primary | 2 (2%) |
| University degree | 51 (51%) |
| Secondary (11–12 grades) | 12 (12%) |
| Residence, n (%) | |
| Village (<500 inhabitants) | 4 (4%) |
| City (>3000 inhabitants) | 90 (90%) |
| Town (500–3000 inhabitants) | 6 (6%) |
| Employment, n (%) | |
| Employed | 31 (31%) |
| Employed but retired | 1 (1%) |
| Employed (home office) | 2 (2%) |
| Unemployed | 6 (6%) |
| Retired | 60 (60%) |
| Do you have children/close relatives? n (%) | |
| No | 4 (4%) |
| Yes | 96 (96%) |
| Do you often meet them? n (%) | |
| No | 7 (7%) |
| Yes | 93 (93%) |
| Clinical Characteristics, n = 100 | |
|---|---|
| Largest tumour diameter, mm | 9.44 ± (4.948); range: 3–30 |
| Tumour size group, n (%) | |
| 0–5 mm | 16 (16%) |
| 6–10 mm | 57 (57%) |
| 11–15 mm | 16 (16%) |
| >15 mm | 11 (11%) |
| Tumour location by TT Fattahi, n (%) | |
| 1—Forehead unit | 32 (32%) |
| 1a—central subunit | 14 |
| 1b—lateral subunit | 18 |
| 2—Nasal unit | 26 (26%) |
| 2.1—tip subunit | 8 |
| 2.3,6—right and left alar base subunits | 9 |
| 2.4,5—right and left alar side wall subunits | 4 |
| 2.7—dorsal subunit | 5 |
| 2.8,9—right and left dorsal side wall subunits | 5 |
| 3—Eyelid unit | 8 (8%) |
| 3a—lower lid subunit | 4 |
| 3b—upper lid subunit | 1 |
| 3c—lateral canthal subunit | 1 |
| 3d—medial canthal subunit | 2 |
| 4—Cheek unit | 28 (28%) |
| 4a—medial subunit | 14 |
| 4b—zygomatic subunit | 3 |
| 4c—lateral subunit | 4 |
| 4d—buccal subunit | 7 |
| 5—Upper lip unit | 3 (3%) |
| 5b—lateral subunit | 3 |
| Surgery groups, n (%) | |
| E | 49 (49%) |
| P | 38 (38%) |
| T | 13 (13%) |
| II | III | |
|---|---|---|
| OSAS, AK | 0.855 | 0.822 |
| OSAS, DS | 0.845 | 0.793 |
| PSAS | 0.828 | 0.836 |
| Description | χ2 | df | RMSEA (95% CI) | CFI | TLI | SRMR | |
|---|---|---|---|---|---|---|---|
| Model 1 | The original model of the OSAS questionnaire with one factor | 19.691 | 9 | 0.109 (0.019; 0.186) | 0.956 | 0.926 | 0.052 |
| Model 2 | The original model of the PSAS questionnaire with one factor | 21.201 | 9 | 0.116 (0.035; 0.193) | 0.956 | 0.927 | 0.049 |
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | |
|---|---|---|---|---|---|---|---|
| PSAS-II Total score | 0.324 ** | 0.377 *** | 0.807 *** | 0.814 *** | 0.841 *** | 0.785 *** | 0.836 *** |
| O1 | O2 | O3 | O4 | O5 | O6 | O7 | |
|---|---|---|---|---|---|---|---|
| OSAS-II Total score | 0.733 *** | 0.736 *** | 0.754 *** | 0.734 *** | 0.786 *** | 0.756 *** | 0.813 *** |
| DLQI-II-Q1 | DLQI-II Total Score | |
|---|---|---|
| PSAS-II-Q1 | 0.428 *** | 0.44 *** |
| PSAS-II-Q2 | 0.724 *** | 0.583 *** |
| PSAS-II-Q3 | 0.253 * | 0.36 *** |
| PSAS-II-Q4 | 0.156 | 0.197 * |
| PSAS-II-Q5 | 0.129 | 0.194 |
| PSAS-II-Q6 | 0.127 | 0.232 * |
| PSAS-II-Q7 | 0.158 | 0.276 ** |
| PSAS-II Total score | 0.358 *** | 0.423 *** |
| Test | Retest | ICC (95% CI) | MD (95% CI) | SDdiff | SEM | SDCind | SDCgroup | 95% LoA | |
|---|---|---|---|---|---|---|---|---|---|
| Pain PSAS-Q1 | 2.02 ± 1.363 | 2.02 ± 1.478 | 0.721 (0.555; 0.832) | 0 (−0.296; 0.296) | 1.069 | 0.565 | 1.565 | 0.221 | −2.095; 2.095 |
| Itchiness PSAS-Q2 | 2.54 ± 1.764 | 2.56 ± 1.74 | 0.827 (0.713; 0.898) | −0.02 (−0.308; 0.268) | 1.04 | 0.433 | 1.199 | 0.17 | −2.058; 2.018 |
| Colour PSAS-Q3 | 3.36 ± 1.758 | 3.02 ± 1.79 | 0.74 (0.581; 0.844) | 0.34 (−0.08; 0.688) | 1.255 | 0.640 | 1.774 | 0.251 | −2.12; 2.8 |
| Stiffness PSAS-Q4 | 3.4 ± 1.906 | 3.32 ± 1.845 | 0.72 (0.544; 0.831) | 0.08 (−0.311; 0.471) | 1.412 | 0.747 | 2.071 | 0.293 | −2.687; 2.847 |
| Thickness PSAS-Q5 | 3.2 ± 1.895 | 3.02 ± 1.755 | 0.618 (0.413; 0.764) | 0.18 (−0.263; 0.623) | 1.6 | 0.989 | 2.741 | 0.388 | −2.955; 3.315 |
| Irregularity PSAS-Q6 | 3.02 ± 1.801 | 3.1 ± 1.776 | 0.679 (0.496; 0.805) | −0.08 (−0.479; 0.319) | 1.441 | 0.816 | 2.263 | 0.32 | −2.903; 2.743 |
| Overall opinion PSAS-Q7 | 2.88 ± 1.612 | 2.94 ± 1.621 | 0.727 (0.564; 0.835) | −0.06 (−0.393; 0.273) | 1.202 | 0.628 | 1.741 | 0.246 | −2.416; 2.296 |
| Total score | 17.54 ± 8.311 | 17.04 ± 7.918 | 0.729 (0.568; 0.837) | 0.5 (−1.163; 2.163) | 6.001 | 3.124 | 8.659 | 1.225 | −11.262; 12.262 |
| Test | Retest | ICC (95% CI) | MD (95% CI) | SDdiff | SEM | SDCind | SDCgroup | 95% LoA | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Vascularity OSAS-II-Q1 | DS | 2.59 ± 1.19 | 2.54 ± 1.039 | 0.844 (0.766; 0.892) | 0.05 (−0.073; 0.173) | 0.626 | 0.247 | 0.685 | 0.069 | −1.177; 1.277 |
| AK | 2.53 ± 1.201 | 2.53 ± 0.904 | 0.627 (0.491; 0.733) | 0 (−0.181; 0.181) | 0.921 | 0.562 | 1.559 | 0.156 | −1.805; 1.805 | |
| Pigmentation OSAS-II-Q2 | DS | 2.26 ± 0.906 | 2.3 ± 0.759 | 0.785 (0.696; 0.85) | −0.04 (−0.148; 0.068) | 0.549 | 0.255 | 0.706 | 0.071 | −1.116; 1.036 |
| AK | 2.82 ± 0.892 | 2.69 ± 0.734 | 0.532 (0.376; 0.658) | 0.13 (−0.024; 0.284) | 0.787 | 0.538 | 1.492 | 0.149 | −1.412; 1.672 | |
| Thickness OSAS-II-Q3 | DS | 2.45 ± 1.077 | 2.32 ± 0.942 | 0.82 (0.742; 0.876) | 0.13 (0.013; 0.247) | 0.597 | 0.253 | 0.702 | 0.07 | −1.041; 1.301 |
| AK | 2.79 ± 0.769 | 2.68 ± 0.75 | 0.457 (0.289; 0.599) | 0.11 (−0.045; 0.265) | 0.79 | 0.582 | 1.614 | 0.161 | −1.438; 1.658 | |
| Relief OSAS-II-Q4 | DS | 2.36 ± 1.142 | 2.29 ± 0.957 | 0.743 (0.641; 0.819) | 0.07 (−0.078; 0.218) | 0.756 | 0.383 | 1.062 | 0.106 | −1.411; 1.551 |
| AK | 2.67 ± 0.943 | 2.51 ± 0.87 | 0.544 (0.391; 0.668) | 0.16 (−0.009; 0.329) | 0.861 | 0.581 | 1.612 | 0.161 | −1.528; 1.848 | |
| Pliability OSAS-II-Q5 | - | |||||||||
| Surface Area OSAS-II-Q6 | DS | 1.82 ± 0.796 | 1.83 ± 0.766 | 0.762 (0.665; 0.833) | −0.01 (−0.116; 0.096) | 0.541 | 0.264 | 0.732 | 0.073 | −1.071; 1.051 |
| AK | 2.66 ± 0.807 | 2.43 ± 0.868 | 0.483 (0.315; 0.621) | 0.23 (0.066; 0.394) | 0.839 | 0.603 | 1.672 | 0.167 | −1.415; 1.875 | |
| Overall opinion OSAS-II-Q7 | DS | 2.64 ± 1.02 | 2.49 ± 0.916 | 0.805 (0.719; 0.866) | 0.15 (0.034; 0.266) | 0.592 | 0.289 | 0.801 | 0.08 | −1.011; 1.311 |
| AK | 2.96 ± 0.909 | 2.79 ± 0.856 | 0.665 (0.537; 0.763) | 0.17 (0.031; 0.309) | 0.711 | 0.412 | 1.141 | 0.114 | −1.224; 1.564 | |
| Total score | DS | 13.87 ± 5.15 | 13.4 ± 4.422 | 0.887 (0.836; 0.923) | 0.47 (0.03; 0.91) | 2.245 | 0.755 | 2.092 | 0.209 | −3.93; 4.87 |
| AK | 13.47 ± 3.597 | 12.84 ± 2.943 | 0.61 (0.47; 0.72) | 0.63 (0.068; 1.193) | 2.87 | 1.792 | 4.968 | 0.497 | −4.995; 6.255 | |
| Vascularity | Pigmentation | Thickness | Relief | Pliability | Surface Area | Overall Opinion | Total Score | ||
|---|---|---|---|---|---|---|---|---|---|
| ICC (95% CI) | First evaluation | 0.798 (0.699; 0.864) | 0.658 (0.216; 0.824) | 0.681 (0.487; 0.796) | 0.693 (0.529; 0.798) | - | 0.43 (−0.254; 0.716) | 0.783 (0.631; 0.866) | 0.79 (0.688; 0.859) |
| Second evaluation | 0.769 (0.656; 0.844) | 0.608 (0.297; 0.767) | 0.547 (0.291; 0.705) | 0.622 (0.437; 0.746) | - | 0.544 (0.033; 0.757) | 0.732 (0.564; 0.83) | 0.742 (0.617; 0.826) |
| p-Value | Mean Difference | SRM Value | 95% CI | PSAS-II vs. OSAS-II | PSAS-III vs. OSAS-III | ||||
|---|---|---|---|---|---|---|---|---|---|
| p-Value | Spearman’s Correlation | p-Value | Spearman’s Correlation | ||||||
| Second visit vs. third visit | PSAS | 0.000 | −8.44 | −1.06 | −1.30 to −0.80 | p = 0.001 | 0.32 | p = 0.000 | 0.51 |
| OSAS | 0.000 | −8.18 | −2.10 | −2.43 to −1.75 | |||||
| PSAS-II | PSAS-III | ||
|---|---|---|---|
| SCI Total | p-value | >0.05 | <0.001 |
| Spearman’s correlation | −0.17 | −0.47 | |
| SCI Emotional | p-value | >0.05 | <0.001 |
| Spearman’s correlation | −0.19 | −0.38 | |
| SCI Social | p-value | >0.05 | <0.001 |
| Spearman’s correlation | 0.00 | −0.39 | |
| SCI Appearance | p-value | >0.05 | <0.001 |
| Spearman’s correlation | −0.19 | −0.51 |
| Second Visit | Third Visit | |||
|---|---|---|---|---|
| PSAS-II | OSAS-II | PSAS-III | OSAS-III | |
| Anatomic Unit | No, p > 0.05 | No, p > 0.05 | No, p > 0.05 | No, p > 0.05 |
| Gender | No, p > 0.05 | No, p > 0.05 | Yes, p = 0.034 | No, p > 0.05 |
| - Score differences between men and women by anatomic units. | No | No | Yes | Yes |
| Age group | No, p > 0.05 | Yes, p = 0.031 | Yes, p = 0.000 | No, p > 0.05 |
| - Score differences between age groups by anatomic units. | Yes | Yes | Yes | No |
| Surgery group (E, P, T) | No, p > 0.05 | No, p > 0.05 | No, p > 0.05 | No, p > 0.05 |
| - Score differences between surgery groups by anatomic units. | No | No | No | No |
| Size group | No, p > 0.05 | No, p > 0.05 | No, p > 0.05 | No, p > 0.05 |
| - Score differences between size groups by anatomic units. | No | Yes | No | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kučinskaitė, A.; Stundys, D.; Gervickaitė, S.; Tarutytė, G.; Grigaitienė, J.; Tutkuvienė, J.; Jančorienė, L. Aesthetic Evaluation of Facial Scars in Patients Undergoing Surgery for Basal Cell Carcinoma: A Prospective Longitudinal Pilot Study and Validation of POSAS 2.0 in the Lithuanian Language. Cancers 2024, 16, 2091. https://doi.org/10.3390/cancers16112091
Kučinskaitė A, Stundys D, Gervickaitė S, Tarutytė G, Grigaitienė J, Tutkuvienė J, Jančorienė L. Aesthetic Evaluation of Facial Scars in Patients Undergoing Surgery for Basal Cell Carcinoma: A Prospective Longitudinal Pilot Study and Validation of POSAS 2.0 in the Lithuanian Language. Cancers. 2024; 16(11):2091. https://doi.org/10.3390/cancers16112091
Chicago/Turabian StyleKučinskaitė, Alvija, Domantas Stundys, Simona Gervickaitė, Gabrielė Tarutytė, Jūratė Grigaitienė, Janina Tutkuvienė, and Ligita Jančorienė. 2024. "Aesthetic Evaluation of Facial Scars in Patients Undergoing Surgery for Basal Cell Carcinoma: A Prospective Longitudinal Pilot Study and Validation of POSAS 2.0 in the Lithuanian Language" Cancers 16, no. 11: 2091. https://doi.org/10.3390/cancers16112091
APA StyleKučinskaitė, A., Stundys, D., Gervickaitė, S., Tarutytė, G., Grigaitienė, J., Tutkuvienė, J., & Jančorienė, L. (2024). Aesthetic Evaluation of Facial Scars in Patients Undergoing Surgery for Basal Cell Carcinoma: A Prospective Longitudinal Pilot Study and Validation of POSAS 2.0 in the Lithuanian Language. Cancers, 16(11), 2091. https://doi.org/10.3390/cancers16112091






