Hereditary Syndromes Associated with Pancreatic and Lung Neuroendocrine Tumors
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
3. Multiple Endocrine Neoplasia Type 1 (MEN1)
4. Pancreatic NETs in MEN1
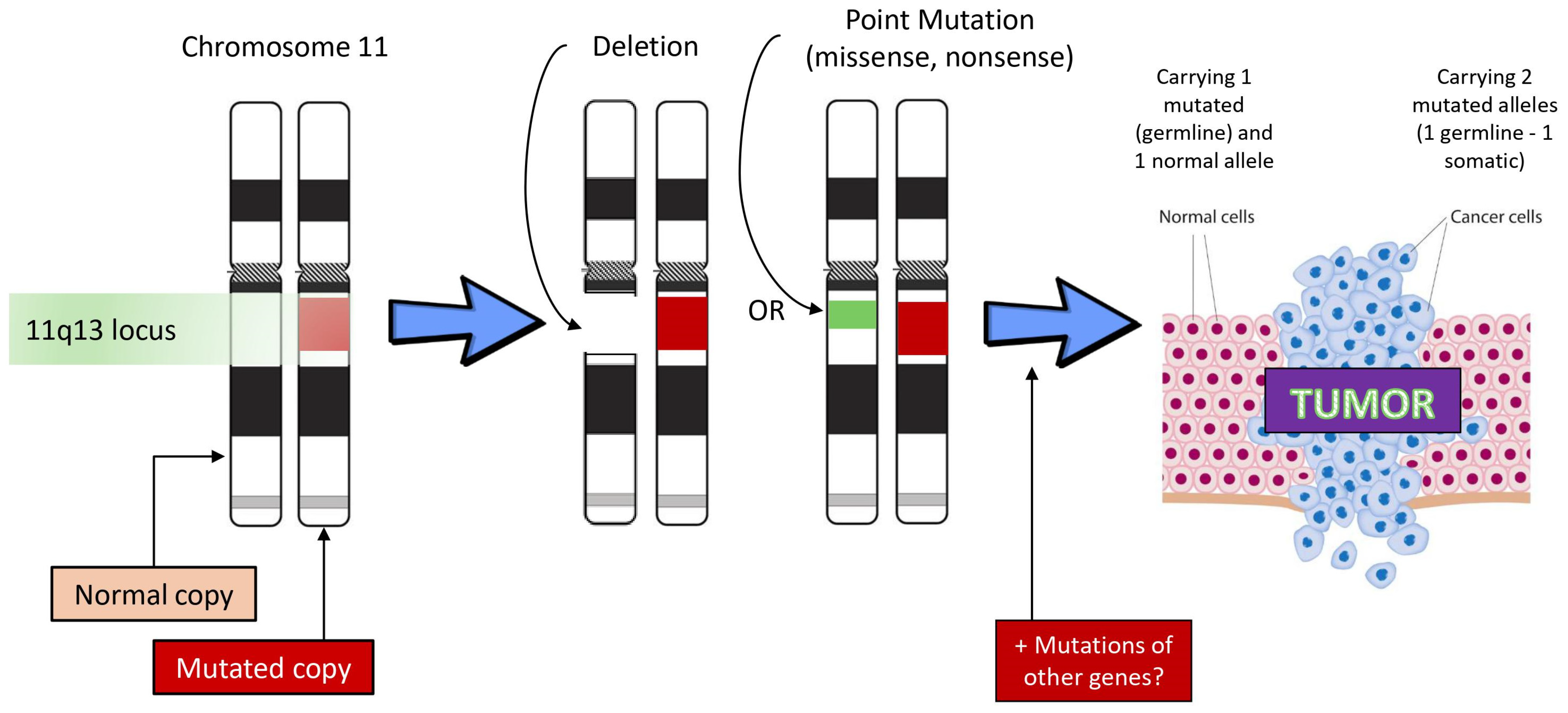
4.1. Genetics
4.2. Diagnosis and Surveillance
4.3. Management
4.4. Prognosis
5. Lung NETs in MEN1
6. Von Hippel–Lindau Syndrome (VHL)
7. Tuberous Sclerosis Complex (TSC)
| Sex | Type of PanNET | Age at NET Diagnosis (Years) | Reference |
|---|---|---|---|
| F | Insulinoma | 24 | Gutman & Leffkowitz (1959) [104] |
| M | Insulinoma | 23 | Davoren & Epstein (1992) [105] |
| M | Gastrinoma | 34 | Schwarzkopf & Pfisterer (1994) [106] |
| M | Insulinoma | 28 | Kim et al. (1995) [107] |
| F | Insulinoma | 18 | Boubaddi et al. (1997) [108] |
| M | Malignant islet cell tumor | 12 | Verhoef et al. (1999) [109] |
| M | Insulinoma | 43 | Eledrisi et al. (2002) [110] |
| M | Malignant islet cell tumor | 6 | Francalanci et al. (2003) [111] |
| M | Islet cell neoplasm | 39 | Merritt et al. (2006) [112] |
| M | Well-differentiated PanNET | 15 | Arva et al. (2012) [113] |
| F/M | Well-differentiated PanNET | 12 | Koc et al. (2017) [114] |
| M | Well-differentiated PanNET | 10 | Bombardieri et al. (2013) [115] |
| F | Well-differentiated PanNET | 35 | Mortaji et al. (2017) [116] |
| M | Well-differentiated PanNET | 3.5 | Mehta et al. (2019) [117] |
| 9M–7F | 16 cases of nonfunctioning PanNETs | 15.5–25.5 | Mowrey et al. (2021) [101] |
8. Neurofibromatosis Type 1 (NF1)
9. Multiple Endocrine Neoplasia Type 4
Future Directions
10. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| ENETS | European Neuroendocrine Tumor Society |
| EURACAN | European Reference Network on Rare Adult Cancers |
References
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients with Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Geurts, J.L. Inherited syndromes involving pancreatic neuroendocrine tumors. J. Gastrointest. Oncol. 2020, 11, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Scarpa, A.; Chang, D.K.; Nones, K.; Corbo, V.; Patch, A.-M.; Bailey, P.; Lawlor, R.T.; Johns, A.L.; Miller, D.K.; Mafficini, A.; et al. Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 2017, 543, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Thakker, R.V. Multiple endocrine neoplasia type 1 (MEN1) and type 4 (MEN4). Mol. Cell. Endocrinol. 2014, 386, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Alrezk, R.; Hannah-Shmouni, F.; Stratakis, C.A. MEN4 and CDKN1B mutations: The latest of the MEN syndromes. Endocr. Relat. Cancer 2017, 24, T195–T208. [Google Scholar] [CrossRef] [PubMed]
- Niederle, B.; Selberherr, A.; Bartsch, D.K.; Brandi, M.L.; Doherty, G.M.; Falconi, M.; Goudet, P.; Halfdanarson, T.R.; Ito, T.; Jensen, R.T.; et al. Multiple Endocrine Neoplasia Type 1 and the Pancreas: Diagnosis and Treatment of Functioning and Non-Functioning Pancreatic and Duodenal Neuroendocrine Neoplasia within the MEN1 Syndrome—An International Consensus Statement. Neuroendocrinology 2021, 111, 609–630. [Google Scholar] [CrossRef] [PubMed]
- Pieterman, C.R.C.; Valk, G.D. Update on the clinical management of multiple endocrine neoplasia type 1. Clin. Endocrinol. 2022, 97, 409–423. [Google Scholar] [CrossRef] [PubMed]
- Soczomski, P.; Jurecka-Lubieniecka, B.; Krzywon, A.; Cortez, A.J.; Zgliczynski, S.; Rogozik, N.; Oczko-Wojciechowska, M.; Pawlaczek, A.; Bednarczuk, T.; Jarzab, B. A Direct Comparison of Patients with Hereditary and Sporadic Pancreatic Neuroendocrine Tumors: Evaluation of Clinical Course, Prognostic Factors and Genotype-Phenotype Correlations. Front. Endocrinol. 2021, 12, 681013. [Google Scholar] [CrossRef] [PubMed]
- Hofland, J.; Falconi, M.; Christ, E.; Castaño, J.P.; Faggiano, A.; Lamarca, A.; Perren, A.; Petrucci, S.; Prasad, V.; Ruszniewski, P.; et al. European Neuroendocrine Tumor Society 2023 guidance paper for functioning pancreatic neuroendocrine tumour syndromes. J. Neuroendocr. 2023, 35, e13318. [Google Scholar] [CrossRef]
- Baudin, E.; Caplin, M.; Garcia-Carbonero, R.; Fazio, N.; Ferolla, P.; Filosso, P.L.; Frilling, A.; de Herder, W.W.; Hörsch, D.; Knigge, U.; et al. Lung and thymic carcinoids: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2021, 32, 439–451. [Google Scholar] [CrossRef]
- Lecomte, P.; Binquet, C.; Le Bras, M.; Tabarin, A.; Cardot-Bauters, C.; Borson-Chazot, F.; Lombard-Bohas, C.; Baudin, E.; Delemer, B.; Klein, M.; et al. Histologically Proven Bronchial Neuroendocrine Tumors in MEN1: A GTE 51-Case Cohort Study. World J. Surg. 2018, 42, 143–152. [Google Scholar] [CrossRef] [PubMed]
- van den Broek, M.F.M.; de Laat, J.M.; van Leeuwaarde, R.S.; van de Ven, A.C.; de Herder, W.W.; Dekkers, O.M.; Drent, M.L.; Kerstens, M.N.; Bisschop, P.H.; Havekes, B.; et al. The Management of Neuroendocrine Tumors of the Lung in MEN1: Results from the Dutch MEN1 Study Group. J. Clin. Endocrinol. Metab. 2021, 106, e1014–e1027. [Google Scholar] [CrossRef] [PubMed]
- de Laat, J.M.; Pieterman, C.R.; van den Broek, M.F.; Twisk, J.W.; Hermus, A.R.; Dekkers, O.M.; de Herder, W.W.; van der Horst-Schrivers, A.N.; Drent, M.L.; Bisschop, P.H.; et al. Natural course and survival of neuroendocrine tumors of thymus and lung in MEN1 patients. J. Clin. Endocrinol. Metab. 2014, 99, 3325–3333. [Google Scholar] [CrossRef] [PubMed]
- Jensen, R.T.; Berna, M.J.; Bingham, D.B.; Norton, J.A. Inherited pancreatic endocrine tumor syndromes: Advances in molecular pathogenesis, diagnosis, management, and controversies. Cancer 2008, 113 (Suppl. S7), 1807–1843. [Google Scholar] [CrossRef] [PubMed]
- Dreijerink, K.M.; Derks, J.L.; Cataldo, I.; Scarpa, A.; Valk, G.D.; Speel, E.J. Genetics and Epigenetics of Pancreatic Neuroendocrine Tumors and Pulmonary Carcinoids. Front. Horm. Res. 2015, 44, 115–138. [Google Scholar] [PubMed]
- Thakker, R.V.; Newey, P.J.; Walls, G.V.; Bilezikian, J.; Dralle, H.; Ebeling, P.R.; Melmed, S.; Sakurai, A.; Tonelli, F.; Brandi, M.L. Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J. Clin. Endocrinol. Metab. 2012, 97, 2990–3011. [Google Scholar] [CrossRef] [PubMed]
- Donegan, D.; Singh Ospina, N.; Rodriguez-Gutierrez, R.; Al-Hilli, Z.; Thompson, G.B.; Clarke, B.L.; Young, W.F., Jr. Long-term outcomes in patients with multiple endocrine neoplasia type 1 and pancreaticoduodenal neuroendocrine tumours. Clin. Endocrinol. 2017, 86, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekharappa, S.C.; Guru, S.C.; Manickam, P.; Olufemi, S.E.; Collins, F.S.; Emmert-Buck, M.R.; Debelenko, L.V.; Zhuang, Z.; Lubensky, I.A.; Liotta, L.A.; et al. Positional cloning of the gene for multiple endocrine neoplasia-type 1. Science 1997, 276, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Singh Ospina, N.; Sebo, T.J.; Thompson, G.B.; Clarke, B.L.; Young, W.F., Jr. Prevalence of parathyroid carcinoma in 348 patients with multiple endocrine neoplasia type 1—Case report and review of the literature. Clin. Endocrinol. 2016, 84, 244–249. [Google Scholar] [CrossRef]
- Lemos, M.C.; Thakker, R.V. Multiple endocrine neoplasia type 1 (MEN1): Analysis of 1336 mutations reported in the first decade following identification of the gene. Hum. Mutat. 2008, 29, 22–32. [Google Scholar] [CrossRef]
- Yaguchi, H.; Ohkura, N.; Takahashi, M.; Nagamura, Y.; Kitabayashi, I.; Tsukada, T. Menin missense mutants associated with multiple endocrine neoplasia type 1 are rapidly de-graded via the ubiquitin-proteasome pathway. Mol. Cell. Biol. 2004, 24, 6569–6580. [Google Scholar] [CrossRef] [PubMed]
- Romanet, P.; Mohamed, A.; Giraud, S.; Odou, M.F.; North, M.O.; Pertuit, M.; Pasmant, E.; Coppin, L.; Guien, C.; Calender, A.; et al. UMD-MEN1 Database: An Overview of the 370 MEN1 Variants Present in 1676 Patients from the French Population. J. Clin. Endocrinol. Metab. 2019, 104, 753–764. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.C.; He, M.; Powell, A.; Adem, A.; Lorang, D.; Heller, C.; Grover, A.C.; Ylaya, K.; Hewitt, S.M.; Marx, S.J.; et al. Recapitulation of Pancreatic Neuroendocrine Tumors in Human Multiple Endocrine Neoplasia Type I Syndrome via Pdx1-Directed Inactivation of Men1. Cancer Res. 2009, 69, 1858–1866. [Google Scholar] [CrossRef] [PubMed]
- Marini, F.; Giusti, F.; Tonelli, F.; Brandi, M.L. Pancreatic Neuroendocrine Neoplasms in Multiple Endocrine Neoplasia Type 1. Int. J. Mol. Sci. 2021, 22, 4041. [Google Scholar] [CrossRef] [PubMed]
- de Laat, J.M.; van der Luijt, R.B.; Pieterman, C.R.; Oostveen, M.P.; Hermus, A.R.; Dekkers, O.M.; de Herder, W.W.; van der Horst-Schrivers, A.N.; Drent, M.L.; Bisschop, P.H.; et al. MEN1 redefined, a clinical comparison of mutation-positive and mutation-negative patients. BMC Med. 2016, 14, 182. [Google Scholar] [CrossRef] [PubMed]
- Pieterman, C.R.C.; Hyde, S.M.; Wu, S.Y.; Landry, J.P.; Chiang, Y.J.; Christakis, I.; Grubbs, E.G.; Fisher, S.B.; Graham, P.H.; Waguespack, S.G.; et al. Understanding the clinical course of genotype-negative MEN1 patients can inform management strategies. Surgery 2021, 169, 175–184. [Google Scholar] [CrossRef]
- Agarwal, S.K. The future: Genetics advances in MEN1 therapeutic approaches and management strategies. Endocr. Relat. Cancer 2017, 24, T119–T134. [Google Scholar] [CrossRef]
- Goudet, P.; Murat, A.; Binquet, C.; Cardot-Bauters, C.; Costa, A.; Ruszniewski, P.; Niccoli, P.; Menegaux, F.; Chabrier, G.; Borson-Chazot, F.; et al. Risk factors and causes of death in MEN1 disease. A GTE (Groupe d’Etude des Tumeurs Endocrines) cohort study among 758 patients. World J. Surg. 2010, 34, 249–255. [Google Scholar] [CrossRef]
- Klein Haneveld, M.J.; van Treijen, M.J.C.; Pieterman, C.R.C.; Dekkers, O.M.; van de Ven, A.; de Herder, W.W.; Zandee, W.T.; Drent, M.L.; Bisschop, P.H.; Havekes, B.; et al. Initiating Pancreatic Neuroendocrine Tumor (pNET) Screening in Young MEN1 Patients: Results From the DutchMEN Study Group. J. Clin. Endocrinol. Metab. 2021, 106, 3515–3525. [Google Scholar] [CrossRef]
- Kos-Kudla, B.; Castano, J.P.; Denecke, T.; Grande, E.; Kjaer, A.; Koumarianou, A.; de Mestier, L.; Partelli, S.; Perren, A.; Stattner, S.; et al. European Neuroendocrine Tumour Society (ENETS) 2023 guidance paper for nonfunctioning pancreatic neuroendocrine tumours. J. Neuroendocr. 2023, 35, e13343. [Google Scholar] [CrossRef]
- Brandi, M.L.; Agarwal, S.K.; Perrier, N.D.; Lines, K.E.; Valk, G.D.; Thakker, R.V. Multiple Endocrine Neoplasia Type 1: Latest Insights. Endocr. Rev. 2021, 42, 133–170. [Google Scholar] [CrossRef] [PubMed]
- Goudet, P.; Dalac, A.; Le Bras, M.; Cardot-Bauters, C.; Niccoli, P.; Levy-Bohbot, N.; Boullay, H.D.; Bertagna, X.; Ruszniewski, P.; Borson-Chazot, F.; et al. MEN1 disease occurring before 21 years old: A 160-patient cohort study from the Groupe d’etude des Tumeurs Endocrines. J. Clin. Endocrinol. Metab. 2015, 100, 1568–1577. [Google Scholar] [CrossRef]
- Goncalves, T.D.; Toledo, R.A.; Sekiya, T.; Matuguma, S.E.; Filho, F.M.; Rocha, M.S.; Siqueira, S.A.; Glezer, A.; Bronstein, M.D.; Pereira, M.A.; et al. Penetrance of functioning and nonfunctioning pancreatic neuroendocrine tumors in multiple endocrine neoplasia type 1 in the second decade of life. J. Clin. Endocrinol. Metab. 2014, 99, E89–E96. [Google Scholar] [CrossRef] [PubMed]
- Challis, B.G.; Casey, R.T.; Grossman, A.; Newell-Price, J.; Newey, P.; Thakker, R.V. What is the appropriate management of nonfunctioning pancreatic neuroendocrine tumours disclosed on screening in adult patients with multiple endocrine neoplasia type 1? Clin. Endocrinol. 2019, 91, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Beek, D.J.; Nell, S.; Verkooijen, H.M.; Borel Rinkes, I.H.M.; Valk, G.D.; Vriens, M.R.; Goudet, P.; Vella, A.; Donegan, D.; Bartsch, D.K.; et al. Surgery for multiple endocrine neoplasia type 1-related insulinoma: Long-term outcomes in a large international cohort. Br. J. Surg. 2020, 107, 1489–1499. [Google Scholar] [CrossRef] [PubMed]
- Kamilaris, C.D.C.; Stratakis, C.A. Multiple Endocrine Neoplasia Type 1 (MEN1): An Update and the Significance of Early Genetic and Clinical Diagnosis. Front. Endocrinol. 2019, 10, 339. [Google Scholar] [CrossRef] [PubMed]
- Massironi, S.; Rossi, R.E.; Laffusa, A.; Eller-Vainicher, C.; Cavalcoli, F.; Zilli, A.; Ciafardini, C.; Sciola, V.; Invernizzi, P.; Peracchi, M. Sporadic and MEN1-related gastrinoma and Zollinger-Ellison syndrome: Differences in clinical characteristics and survival outcomes. J. Endocrinol. Investig. 2023, 46, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Gibril, F.; Schumann, M.; Pace, A.; Jensen, R.T. Multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome: A prospective study of 107 cases and comparison with 1009 cases from the literature. Medicine 2004, 83, 43–83. [Google Scholar] [CrossRef] [PubMed]
- Lévy-Bohbot, N.; Merle, C.; Goudet, P.; Delemer, B.; Calender, A.; Jolly, D.; Thiéfin, G.; Cadiot, G. Prevalence, characteristics and prognosis of MEN 1-associated glucagonomas, VIPomas, and somatostatinomas: Study from the GTE (Groupe des Tumeurs Endocrines) registry. Gastroentérol. Clin. Biol. 2004, 28, 1075–1081. [Google Scholar] [CrossRef]
- Sadowski, S.M.; Triponez, F. Management of pancreatic neuroendocrine tumors in patients with MEN 1. Gland Surg. 2015, 4, 63. [Google Scholar]
- Kim, G.Y.; Kim, S.; Ong, R.K.S.; Shawa, H. Simultaneous Glucagon and Vasoactive Intestinal Peptide Producing Pancreatic Neuroendocrine Tumors in a Patient with Multiple Endocrine Neoplasia Type 1: A Case Re-port and Literature. Pancreas 2018, 47, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Davila, A.; Menias, C.O.; Alhalabi, K.; Lall, C.; Pickhardt, P.J.; Lubner, M.; Elsayes, K.M. Multiple Endocrine Neoplasia: Spectrum of Abdominal Manifestations. Am. J. Roentgenol. 2020, 215, 885–895. [Google Scholar] [CrossRef] [PubMed]
- Garbrecht, N.; Anlauf, M.; Schmitt, A.; Henopp, T.; Sipos, B.; Raffel, A.; Eisenberger, C.F.; Knoefel, W.T.; Pavel, M.; Fottner, C.; et al. Somatostatin-producing neuroendocrine tumors of the duodenum and pancreas: Incidence, types, biological behavior, association with inherited syndromes, and functional activity. Endocr. Relat. Cancer 2008, 15, 229–241. [Google Scholar] [CrossRef]
- Thompson, R.; Landry, C.S. Multiple endocrine neoplasia 1: A broad overview. Ther. Adv. Chronic Dis. 2021, 12, 20406223211035288. [Google Scholar] [CrossRef] [PubMed]
- Mele, C.; Mancerelli, M.; Caputo, M.; Mai, S.; Pagano, L.; Aimaretti, G.; Scacchi, M.; Falchetti, A.-T.; Marzullo, P. Phenotypes Associated with MEN1 Syndrome: A Focus on Genotype-Phenotype Correlations. Front. Endocrinol. 2020, 11, 591501. [Google Scholar] [CrossRef]
- Pieterman, C.R.C.; de Laat, J.M.; Twisk, J.W.R.; van Leeuwaarde, R.S.; de Herder, W.W.; Dreijerink, K.M.A.; Hermus, A.; Dekkers, O.M.; van der Horst-Schrivers, A.N.A.; Drent, M.L.; et al. Long-Term Natural Course of Small Nonfunctional Pancreatic Neuroendocrine Tumors in MEN1-Results from the Dutch MEN1 Study Group. J. Clin. Endocrinol. Metab. 2017, 102, 3795–3805. [Google Scholar] [CrossRef] [PubMed]
- Cejas, P.; Drier, Y.; Dreijerink, K.M.A.; Brosens, L.A.A.; Deshpande, V.; Epstein, C.B.; Conemans, E.B.; Morsink, F.H.M.; Graham, M.K.; Valk, G.D.; et al. Enhancer signatures stratify and predict outcomes of non-functional pancreatic neuroendocrine tumors. Nat. Med. 2019, 25, 1260–1265. [Google Scholar] [CrossRef]
- de Wilde, R.F.; Heaphy, C.M.; Maitra, A.; Meeker, A.K.; Edil, B.H.; Wolfgang, C.L.; Ellison, T.A.; Schulick, R.D.; Molenaar, I.Q.; Valk, G.D.; et al. Loss of ATRX or DAXX expression and concomitant acquisition of the alternative lengthening of telomeres phenotype are late events in a small subset of MEN-1 syndrome pancreatic neuroendocrine tumors. Mod. Pathol. 2012, 25, 1033–1039. [Google Scholar] [CrossRef]
- Falchetti, A. Genetics of multiple endocrine neoplasia type 1 syndrome: What’s new and what’s old. F1000Research 2017, 6, 73. [Google Scholar] [CrossRef]
- Ramamoorthy, B.; Nilubol, N. Multiple Endocrine Neoplasia Type 1 Syndrome Pancreatic Neuroendocrine Tumor Genotype/Phenotype: Is There Any Advance on Predicting or Preventing? Surg. Oncol. Clin. N. Am. 2023, 32, 315–325. [Google Scholar] [CrossRef]
- Gurung, B.; Feng, Z.; Iwamoto, D.V.; Thiel, A.; Jin, G.; Fan, C.M.; Ng, J.M.; Curran, T.; Hua, X. Menin Epigenetically Represses Hedgehog Signaling in MEN1 Tumor Syndrome. Cancer Res. 2013, 73, 2650–2658. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Ma, J.; Hua, X. Epigenetic regulation by the menin pathway. Endocr.-Relat. Cancer 2017, 24, T147. [Google Scholar] [CrossRef] [PubMed]
- van Treijen, M.J.C.; van Beek, D.J.; van Leeuwaarde, R.S.; Vriens, M.R.; Valk, G.D. Diagnosing Nonfunctional Pancreatic NETs in MEN1: The Evidence Base. J. Endocr. Soc. 2018, 2, 1067–1088. [Google Scholar] [CrossRef] [PubMed]
- van Beek, D.J.; Pieterman, C.R.; Wessels, F.J.; van de Ven, A.C.; de Herder, W.W.; Dekkers, O.M.; Zandee, W.T.; Drent, M.L.; Bisschop, P.H.; Havekes, B.; et al. Diagnosing pancreatic neuroendocrine tumors in patients with multiple endocrine neo-plasia type 1 in daily practice. Front. Endocrinol. 2022, 13, 926491. [Google Scholar] [CrossRef]
- Vergauwen, E.; Vanbinst, A.M.; Brussaard, C.; Janssens, P.; De Clerck, D.; Van Lint, M.; Houtman, A.C.; Michel, O.; Keymolen, K.; Lefevere, B.; et al. Central nervous system gadolinium accumulation in patients undergoing periodical contrast MRI screening for hereditary tumor syndromes. Hered. Cancer Clin. Pract. 2018, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Couvelard, A.; Scoazec, J.Y. Inherited tumor syndromes of gastroenteropancreatic and thoracic neuroendocrine neoplasms. Ann. Pathol. 2020, 40, 120–133. [Google Scholar] [CrossRef]
- Ishii, T.; Katanuma, A.; Toyonaga, H.; Chikugo, K.; Nasuno, H.; Kin, T.; Hayashi, T.; Takahashi, K. Role of Endoscopic Ultrasound in the Diagnosis of Pancreatic Neuroendocrine Neoplasms. Diagnostics 2021, 11, 316. [Google Scholar] [CrossRef]
- Daskalakis, K.; Tsoli, M.; Alexandraki, K.I.; Angelousi, A.; Chatzellis, E.; Tsolakis, A.V.; Karoumpalis, I.; Kolomodi, D.; Kassi, E.; Kaltsas, G. Magnetic Resonance Imaging or Endoscopic Ultrasonography for Detection and Surveillance of Pancreatic Neuroendocrine Neoplasms in Patients with Multiple Endocrine Neoplasia Type 1? Horm. Metab. Res. 2019, 51, 580–585. [Google Scholar] [CrossRef]
- Newey, P.J.; Newell-Price, J. MEN1 Surveillance Guidelines: Time to (Re)Think? J. Endocr. Soc. 2022, 6, bvac001. [Google Scholar] [CrossRef]
- Jullien, M.; Reichert, T.; D’Anella, P.; Castinetti, F.; Barlier, A.; Brue, T.; Taieb, D.; Cuny, T. Comparison of 68Ga-Dotatate PET/CT and 18F-FDOPA PET/CT for the diagnosis of pancreatic neuroendocrine tumors in a MEN1 patient. Ann. Endocrinol. 2020, 81, 39–43. [Google Scholar] [CrossRef]
- Kostiainen, I.; Majala, S.; Schildt, J.; Parviainen, H.; Kauhanen, S.; Seppänen, H.; Miettinen, P.J.; Matikainen, N.; Ryhänen, E.M.; Schalin-Jäntti, C. Pancreatic imaging in MEN1—Comparison of conventional and somatostatin receptor positron emission tomography/computed tomography imaging in real-life setting. Eur. J. Endocrinol. 2023, 188, 421–429. [Google Scholar] [CrossRef]
- Manoharan, J.; Raue, F.; Lopez, C.L.; Albers, M.B.; Bollmann, C.; Fendrich, V.; Slater, E.P.; Bartsch, D.K. Is Routine Screening of Young Asymptomatic MEN1 Patients Necessary? World J. Surg. 2017, 41, 2026–2032. [Google Scholar] [CrossRef] [PubMed]
- O’Riordain, D.S.; O’Brien, T.; van Heerden, J.A.; Service, F.J.; Grant, C.S. Surgical management of insulinoma associated with multiple endocrine neoplasia type I. World J. Surg. 1994, 18, 488–493; discussion 493–494. [Google Scholar] [CrossRef] [PubMed]
- Reubi, J.C.; Waser, B. Concomitant expression of several peptide receptors in neuroendocrine tumours: Molecular basis for in vivo multireceptor tumour targeting. Eur. J. Nucl. Med. Mol. Imaging 2003, 30, 781–793. [Google Scholar] [CrossRef] [PubMed]
- Kappelle, W.F.; Valk, G.D.; Leenders, M.; Moons, L.M.; Bogte, A.; Siersema, P.D.; Vleggaar, F.P. Growth rate of small pancreatic neuroendocrine tumors in multiple endocrine neoplasia type 1: Results from an endoscopic ultrasound-based cohort study. Endoscopy 2017, 49, 27–34. [Google Scholar] [CrossRef]
- Triponez, F.; Sadowski, S.M.; Pattou, F.; Cardot-Bauters, C.; Mirallie, E.; Le Bras, M.; Sebag, F.; Niccoli, P.; Deguelte, S.; Cadiot, G.; et al. Long-term Follow-up of MEN1 Patients Who Do Not Have Initial Surgery for Small ≤2 cm Nonfunctioning Pancreatic Neuroendocrine Tumors, an AFCE and GTE Study: Association Francophone de Chirurgie Endocrinienne & Groupe d’Etude des Tumeurs Endocrines. Ann. Surg. 2018, 268, 158–164. [Google Scholar]
- Vinault, S.; Mariet, A.S.; Le Bras, M.; Mirallie, E.; Cardot-Bauters, C.; Pattou, F.; Ruszniewski, P.; Sauvanet, A.; Chanson, P.; Baudin, E.; et al. Metastatic Potential and Survival of Duodenal and Pancreatic Tumors in Multiple Endocrine Neoplasia Type 1: A GTE and AFCE Cohort Study (Groupe d’etude des Tumeurs Endocrines and Association Francophone de Chirurgie Endocrinienne). Ann. Surg. 2020, 272, 1094–1101. [Google Scholar] [CrossRef]
- Ishida, H.; Lam, A.K.-Y. Pancreatic neuroendocrine neoplasms: Updates on genomic changes in inherited tumour syndromes and sporadic tumours based on WHO classification. Crit. Rev. Oncol./Hematol. 2022, 172, 103648. [Google Scholar] [CrossRef]
- Sadowski, S.M.; Pieterman, C.R.C.; Perrier, N.D.; Triponez, F.; Valk, G.D. Prognostic factors for the outcome of nonfunctioning pancreatic neuroendocrine tumors in MEN1: A systematic review of literature. Endocr. Relat. Cancer 2020, 27, R145–R161. [Google Scholar] [CrossRef]
- Pavel, M.; Oberg, K.; Falconi, M.; Krenning, E.P.; Sundin, A.; Perren, A.; Berruti, A.; Esmo Guidelines Committee. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 844–860. [Google Scholar] [CrossRef]
- Norton, J.A.; Alexander, H.R.; Fraker, D.L.; Venzon, D.J.; Gibril, F.; Jensen, R.T. Comparison of surgical results in patients with advanced and limited disease with multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome. Ann. Surg. 2001, 234, 495–505; discussion 505–506. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.L.; Falconi, M.; Waldmann, J.; Boninsegna, L.; Fendrich, V.; Goretzki, P.K.; Langer, P.; Kann, P.H.; Partelli, S.; Bartsch, D.K. Partial pancreaticoduodenectomy can provide cure for duodenal gastrinoma associated with multiple endocrine neoplasia type 1. Ann. Surg. 2013, 257, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Anlauf, M.; Garbrecht, N.; Henopp, T.; Schmitt, A.; Schlenger, R.; Raffel, A.; Krausch, M.; Gimm, O.; Eisenberger, C.F.; Knoefel, W.T.; et al. Sporadic versus hereditary gastrinomas of the duodenum and pancreas: Distinct clinico-pathological and epidemiological features. World J. Gastroenterol. 2006, 12, 5440–5446. [Google Scholar] [CrossRef] [PubMed]
- Falconi, M.; Eriksson, B.; Kaltsas, G.; Bartsch, D.K.; Capdevila, J.; Caplin, M.; Kos-Kudla, B.; Kwekkeboom, D.; Rindi, G.; Klöppel, G.; et al. ENETS Consensus Guidelines Update for the Management of Patients with Functional Pancreatic Neuroendocrine Tumors and Non-Functional Pancreatic Neuroendocrine Tumors. Neuroendocrinology 2016, 103, 153–171. [Google Scholar] [CrossRef] [PubMed]
- Perrier, N.D. From Initial Description by Wermer to Present-Day MEN1: What have We Learned? World J. Surg. 2018, 42, 1031–1035. [Google Scholar] [CrossRef] [PubMed]
- Kartik, A.; Armstrong, V.L.; Stucky, C.C.; Wasif, N.; Fong, Z.V. Contemporary Approaches to the Surgical Management of Pancreatic Neuroendocrine Tumors. Cancers 2024, 16, 1501. [Google Scholar] [CrossRef] [PubMed]
- El Sayed, G.; Frim, L.; Franklin, J.; McCrudden, R.; Gordon, C.; Al-Shamma, S.; Kiss, S.; Hegyi, P.; Eross, B.; Hegyi, P.J. Endoscopic ultrasound-guided ethanol and radiofrequency ablation of pancreatic insulinomas: A systematic literature review. Ther. Adv. Gastroenterol. 2021, 14, 17562848211042171. [Google Scholar] [CrossRef]
- Crino, S.F.; Napoleon, B.; Facciorusso, A.; Lakhtakia, S.; Borbath, I.; Caillol, F.; Pham, K.D.-C.; Rizzatti, G.; Forti, E.; Palazzo, L.; et al. Endoscopic Ultrasound-guided Radiofrequency Ablation Versus Surgical Resection for Treatment of Pancreatic Insulinoma. Clin. Gastroenterol. Hepatol. 2023, 21, 2834–2843.e2. [Google Scholar] [CrossRef] [PubMed]
- Faggiano, A.; Modica, R.; Calzo, F.L.; Camera, L.; Napolitano, V.; Altieri, B.; de Cicco, F.; Bottiglieri, F.; Sesti, F.; Badalamenti, G.; et al. Lanreotide Therapy vs Active Surveillance in MEN1-Related Pancreatic Neuroendocrine Tumors < 2 Centimeters. J. Clin. Endocrinol. Metab. 2020, 105, 78–84. [Google Scholar]
- Boharoon, H.; Grossman, A. A New Medical Therapy for Multiple Endocrine Neoplasia Type 1? touchREV. Endocrinol. 2022, 18, 86–88. [Google Scholar] [CrossRef]
- Nell, S.; Verkooijen, H.M.; Pieterman, C.R.C.; de Herder, W.W.; Hermus, A.R.; Dekkers, O.M.; van der Horst-Schrivers, A.N.; Drent, M.L.; Bisschop, P.H.; Havekes, B.; et al. Management of MEN1 Related Nonfunctioning Pancreatic NETs: A Shifting Paradigm: Results from the DutchMEN1 Study Group. Ann. Surg. 2018, 267, 1155–1160. [Google Scholar] [CrossRef] [PubMed]
- van Beek, D.J.; Nell, S.; Pieterman, C.R.C.; de Herder, W.W.; van de Ven, A.C.; Dekkers, O.M.; van der Horst-Schrivers, A.N.; Drent, M.L.; Bisschop, P.H.; Havekes, B.; et al. Prognostic factors and survival in MEN1 patients with gastrinomas: Results from the DutchMEN study group (DMSG). J. Surg. Oncol. 2019, 120, 966–975. [Google Scholar] [CrossRef]
- Kassi, E.; Kaltsas, G. Plasma Polyamines as an Additional to Imaging Biomarker in MEN1 Patients with Duodenopancreatic Neuroendocrine Tumors. J. Clin. Endocrinol. Metab. 2022, 107, e880–e882. [Google Scholar] [CrossRef] [PubMed]
- Fahrmann, J.F.; Wasylishen, A.R.; Pieterman, C.R.; Irajizad, E.; Vykoukal, J.; Murage, E.; Wu, R.; Dennison, J.B.; Krishna, H.; Peterson, C.B.; et al. A Blood-based Polyamine Signature Associated with MEN1 Duodenopancreatic Neuroendocrine Tumor Progression. J. Clin. Endocrinol. Metab. 2021, 106, e4969–e4980. [Google Scholar] [CrossRef]
- Bartsch, D.K.; Albers, M.B.; Lopez, C.L.; Apitzsch, J.C.; Walthers, E.M.; Fink, L.; Fendrich, V.; Slater, E.P.; Waldmann, J.; Anlauf, M. Bronchopulmonary Neuroendocrine Neoplasms and Their Precursor Lesions in Multiple Endocrine Neoplasia Type 1. Neuroendocrinology 2016, 103, 240–247. [Google Scholar] [CrossRef] [PubMed]
- van den Broek, M.F.M.; de Laat, J.M.; van Leeuwaarde, R.S.; van de Ven, A.C.; de Herder, W.W.; Dekkers, O.M.; Drent, M.L.; Kerstens, M.N.; Bisschop, P.H.; Havekes, B.; et al. Well-Differentiated Bronchopulmonary Neuroendocrine Tumors: More Than One Entity. J. Thorac. Oncol. 2021, 16, 1810–1820. [Google Scholar] [CrossRef] [PubMed]
- Yliaska, I.; Tokola, H.; Ebeling, T.; Kuismin, O.; Ukkola, O.; Koivikko, M.L.; Lesonen, T.; Rimpiläinen, J.; Felin, T.; Ryhänen, E.; et al. Thymic neuroendocrine tumors in patients with multiple endocrine neoplasia type 1. Endocrine 2022, 77, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Simonds, W.F. Expressions of Cushing’s syndrome in multiple endocrine neoplasia type 1. Front. Endocrinol. 2023, 14, 1183297. [Google Scholar] [CrossRef] [PubMed]
- Laks, S.; van Leeuwaarde, R.; Patel, D.; Keutgen, X.M.; Hammel, P.; Nilubol, N.; Links, T.P.; Halfdanarson, T.R.; Daniels, A.B.; Tirosh, A.; et al. Management recommendations for pancreatic manifestations of von Hippel-Lindau disease. Cancer 2022, 128, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Halperin, R.; Tirosh, A. Non-Interventional Management of Advanced Pancreatic Neuroendocrine Neoplasms in Patients with von Hippel-Lindau Disease. Cancers 2023, 15, 1739. [Google Scholar] [CrossRef]
- Halperin, R.; Arnon, L.; Eden-Friedman, Y.; Tirosh, A. Unique Characteristics of Patients with Von Hippel-Lindau Disease Defined by Various Diagnostic Criteria. Cancers 2023, 15, 1657. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwaarde, R.S.; Ahmad, S.; van Nesselrooij, B.; Zandee, W.; Giles, R.H. Von Hippel-Lindau Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [Google Scholar]
- Launbjerg, K.; Bache, I.; Galanakis, M.; Bisgaard, M.L.; Binderup, M.L.M. von Hippel-Lindau development in children and adolescents. Am. J. Med. Genet. A 2017, 173, 2381–2394. [Google Scholar] [CrossRef] [PubMed]
- Falconi, M.; Bartsch, D.K.; Eriksson, B.; Kloppel, G.; Lopes, J.M.; O’Connor, J.M.; Salazar, R.; Taal, B.G.; Vullierme, M.P.; O’Toole, D.; et al. ENETS Consensus Guidelines for the management of patients with digestive neuroendocrine neoplasms of the digestive system: Well-differentiated pancreatic non-functioning tumors. Neuroendocrinology 2012, 95, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Krauss, T.; Ferrara, A.M.; Links, T.P.; Wellner, U.; Bancos, I.; Kvachenyuk, A.; de Las Heras, K.V.G.; Yukina, M.Y.; Petrov, R.; Bullivant, G.; et al. Preventive medicine of von Hippel-Lindau disease-associated pancreatic neuroendocrine tumors. Endocr. Relat. Cancer 2018, 25, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Tirosh, A.; Sadowski, S.M.; Linehan, W.M.; Libutti, S.K.; Patel, D.; Nilubol, N.; Kebebew, E. Association of VHL Genotype with Pancreatic Neuroendocrine Tumor Phenotype in Patients With von Hippel-Lindau Disease. JAMA Oncol. 2018, 4, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Jonasch, E.; McCutcheon, I.E.; Gombos, D.S.; Ahrar, K.; Perrier, N.D.; Liu, D.; Robichaux, C.C.; Villarreal, M.F.; Weldon, J.A.; Woodson, A.H.; et al. Pazopanib in patients with von Hippel-Lindau disease: A single-arm, single-centre, phase 2 trial. Lancet Oncol. 2018, 19, 1351–1359. [Google Scholar] [CrossRef]
- Jonasch, E.; Donskov, F.; Iliopoulos, O.; Rathmell, W.K.; Narayan, V.K.; Maughan, B.L.; Oudard, S.; Else, T.; Maranchie, J.K.; Welsh, S.J.; et al. Belzutifan for Renal Cell Carcinoma in von Hippel-Lindau Disease. N. Engl. J. Med. 2021, 385, 2036–2046. [Google Scholar] [CrossRef] [PubMed]
- Pelle, E.; Al-Toubah, T.; Morse, B.; Strosberg, J. Belzutifan in a Patient with VHL-Associated Metastatic Pancreatic Neuroendocrine Tumor. J. Natl. Compr. Cancer Netw. 2022, 20, 1285–1287. [Google Scholar]
- Orlova, K.A.; Crino, P.B. The tuberous sclerosis complex. Ann. N. Y. Acad. Sci. 2010, 1184, 87–105. [Google Scholar] [CrossRef]
- Mowrey, K.; Northrup, H.; Rougeau, P.; Hashmi, S.S.; Krueger, D.A.; Ebrahimi-Fakhari, D.; Towbin, A.J.; Trout, A.T.; Capal, J.K.; Franz, D.N.; et al. Frequency, Progression, and Current Management: Report of 16 New Cases of Nonfunctional Pancreatic Neuroendocrine Tumors in Tuberous Sclerosis Complex and Comparison with Previous Reports. Front. Neurol. 2021, 12, 627672. [Google Scholar] [CrossRef]
- Northrup, H.; Aronow, M.E.; Bebin, E.M.; Bissler, J.; Darling, T.N.; de Vries, P.J.; Frost, M.D.; Fuchs, Z.; Gosnell, E.S.; Gupta, N.; et al. Updated International Tuberous Sclerosis Complex Diagnostic Criteria and Surveillance and Management Recommendations. Pediatr. Neurol. 2021, 123, 50–66. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.M.; Geenen, K.R.; O’Shea, A.; Hedgire, S.S.; Ferrone, C.R.; Thiele, E.A. Tuberous sclerosis complex-associated nonfunctional pancreatic neuroendocrine tumors: Management and surgical outcomes. Am. J. Med. Genet. A 2022, 188, 2666–2671. [Google Scholar] [CrossRef] [PubMed]
- Gutman, A.; Leffkowitz, M. Tuberous sclerosis associated with spontaneous hypoglycaemia. Br. Med. J. 1959, 2, 1065–1068. [Google Scholar] [CrossRef] [PubMed]
- Davoren, P.M.; Epstein, M.T. Insulinoma complicating tuberous sclerosis. J. Neurol. Neurosurg. Psychiatry 1992, 55, 1209. [Google Scholar] [CrossRef] [PubMed]
- Schwarzkopf, G.; Pfisterer, J. Metastasierendes Gastrinom und der Tuberöse-Sklerose-Komplex. Assoziation oder Koinzidenz? [Metastasizing gastrinoma and tuberous sclerosis complex. Association or coincidence?]. Zentralbl. Pathol. 1994, 139, 477–481. (In German) [Google Scholar] [PubMed]
- Kim, H.; Kerr, A.; Morehouse, H. The association between tuberous sclerosis and insulinoma. AJNR Am. J. Neuroradiol. 1995, 16, 1543–1544. [Google Scholar] [PubMed]
- Boubaddi, N.E.; Imbert, Y.; Tissot, B.; Chapus, J.J.; Dupont, E.; Gallouin, D.; Masson, B.; De Mascarel, A. Insulinome sécrétant et sclérose tubéreuse de Bourneville [Secreting insulinoma and Bourneville’s tuberous sclerosis]. Gastroenterol. Clin. Biol. 1997, 21, 343. [Google Scholar]
- Verhoef, S.; van Diemen-Steenvoorde, R.; Akkersdijk, W.L.; Bax, N.M.; Ariyurek, Y.; Hermans, C.J.; van Nieuwenhuizen, O.; Nikkels, P.G.; Lindhout, D.; Halley, D.J.; et al. Malignant pancreatic tumour within the spectrum of tuberous sclerosis complex in childhood. Eur. J. Pediatr. 1999, 158, 284–287. [Google Scholar] [CrossRef]
- Eledrisi, M.S.; Stuart, C.A.; Alshanti, M. Insulinoma in a patient with tuberous sclerosis: Is there an association? Endocr. Pract. 2002, 8, 109–112. [Google Scholar] [CrossRef]
- Francalanci, P.; Diomedi-Camassei, F.; Purificato, C.; Santorelli, F.M.; Giannotti, A.; Dominici, C.; Inserra, A.; Boldrini, R. Malignant pancreatic endocrine tumor in a child with tuberous sclerosis. Am. J. Surg. Pathol. 2003, 27, 1386–1389. [Google Scholar] [CrossRef]
- Merritt, J.L., 2nd; Davis, D.M.; Pittelkow, M.R.; Babovic-Vuksanovic, D. Extensive acrochordons and pancreatic islet-cell tumors in tuberous sclerosis associated with TSC2 mutations. Am. J. Med. Genet. A 2006, 140, 1669–1672. [Google Scholar] [CrossRef]
- Arva, N.C.; Pappas, J.G.; Bhatla, T.; Raetz, E.A.; Macari, M.; Ginsburg, H.B.; Hajdu, C.H. Well-differentiated pancreatic neuroendocrine carcinoma in tuberous sclerosis—Case report and review of the literature. Am. J. Surg. Pathol. 2012, 36, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Koc, G.; Sugimoto, S.; Kuperman, R.; Kammen, B.F.; Karakas, S.P. Pancreatic tumors in children and young adults with tuberous sclerosis complex. Pediatr. Radiol. 2017, 47, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Bombardieri, R.; Moavero, R.; Roberto, D.; Cerminara, C.; Curatolo, P. Pancreatic neuroendocrine tumor in a child with a tuberous sclerosis complex 2 (TSC2) mutation. Endocr. Pract. 2013, 19, e124–e128. [Google Scholar] [CrossRef] [PubMed]
- Mortaji, P.; Morris, K.T.; Samedi, V.; Eberhardt, S.; Ryan, S. Pancreatic neuroendocrine tumor in a patient with a TSC1 variant: Case report and review of the literature. Fam. Cancer 2018, 17, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Rusyn, L.; Ginsburg, H.; Hajdu, C.; Kohn, B. Pancreatic Neuroendocrine Tumor in a Young Child With Tuberous Sclerosis Complex 1. J. Endocr. Soc. 2019, 3, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Ly, K.I.; Blakeley, J.O. The Diagnosis and Management of Neurofibromatosis Type 1. Med. Clin. N. Am. 2019, 103, 1035–1054. [Google Scholar] [CrossRef] [PubMed]
- Jett, K.; Friedman, J. Clinical and genetic aspects of neurofibromatosis 1. Genet. Med. 2010, 12, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Mao, C.; Shah, A.; Hanson, D.J.; Howard, J.M. Von Recklinghausen’s disease associated with duodenal somatostatinoma: Contrast of duodenal versus pancreatic somatostatinomas. J. Surg. Oncol. 1995, 59, 67–73. [Google Scholar] [CrossRef]
- Gauci, J.; Azzopardi, N.; Babic, D.; Cortis, K.; Axisa, B. Neurofibromatosis Type 1: A Rare Predisposition for Gastrinomas and Other Neuroendocrine Tumors. Pancreas 2022, 51, 559–562. [Google Scholar] [CrossRef]
- Singeisen, H.; Renzulli, M.M.; Pavlicek, V.; Probst, P.; Hauswirth, F.; Muller, M.K.; Adamczyk, M.; Weber, A.; Kaderli, R.M.; Renzulli, P. Multiple endocrine neoplasia type 4: A new member of the MEN family. Endocr. Connect. 2023, 12, e220411. [Google Scholar] [CrossRef] [PubMed]
- Lagarde, A.; Le Collen, L.; Boulagnon, C.; Brixi, H.; Durlach, A.; Mougel, G.; Cuny, T.; Delemer, B.; Barlier, A.; Romanet, P. Early Detection of Relapse by ctDNA Sequencing in a Patient with Metastatic Thymic Tumor and MEN1 Mosaicism. J. Clin. Endocrinol. Metab. 2022, 107, e4154–e4158. [Google Scholar] [CrossRef]
- Sumiyoshi, T.; Yamasaki, T.; Takeda, M.; Mizuno, K.; Utsunomiya, N.; Sakamoto, H.; Nakamura, E.; Ogawa, O.; Akamatsu, S. Detection of von Hippel-Lindau gene mutation in circulating cell-free DNA for clear cell renal cell carcinoma. Cancer Sci. 2021, 112, 3363–3374. [Google Scholar] [CrossRef] [PubMed]
- van Treijen, M.J.C.; Korse, C.M.; Verbeek, W.H.; Tesselaar, M.E.T.; Valk, G.D. NETest: Serial liquid biopsies in gastroenteropancreatic NET surveillance. Endocr. Connect. 2022, 11, e220146. [Google Scholar] [CrossRef]
- Peipert, B.J.; Goswami, S.; Yount, S.E.; Sturgeon, C. Health-related quality of life in MEN1 patients compared with other chronic conditions and the United States general population. Surgery 2018, 163, 205–211. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwaarde, R.S.; Pieterman, C.R.C.; May, A.M.; Dekkers, O.M.; van der Horst-Schrivers, A.N.; Hermus, A.R.; de Herder, W.W.; Drent, M.L.; Bisschop, P.H.; Havekes, B.; et al. Health-Related Quality of Life in Patients with Multiple En-docrine Neoplasia Type 1. Neuroendocrinology 2021, 111, 288–296. [Google Scholar] [CrossRef]
- Giusti, F.; Cioppi, F.; Fossi, C.; Marini, F.; Masi, L.; Tonelli, F.; Brandi, M.L. Quality of life in Italian patients with Multiple endocrine neoplasia type 1 (MEN 1): Results of an extensive survey. Orphanet J. Rare Dis. 2021, 16, 16. [Google Scholar] [CrossRef]

| Syndrome | Type of NET | Other Malignant Tumors | Benign Manifestations | Frequency |
|---|---|---|---|---|
| Multiple endocrine neoplasia type 1 (MEN1) | PanNET Duodenal NET LNET TNET Gastric NET | Adrenocortical cancer Breast cancer | Primary hyperparathyroidism Pituitary adenoma Adrenal adenoma Angiofibroma Collagenoma Meningioma Lipoma | Prevalence 1–10 in 100,000 |
| von Hippel–Lindau (VHL) | PanNET | Clear cell renal carcinoma Pheochromocytoma Endolymphatic sac tumor | Hemangioblastoma Renal cyst Pancreatic serous cystadenoma Epididymis cystadenoma | 1 in 36,000 |
| Tuberous sclerosis complex (TSC) | PanNET | Renal-cell carcinoma Astrocytoma Angiomyolipoma | Angiofibroma Shagreen patch Fibroma Retinal hamartoma Ash leaf macules | 1 in 12,000–14,000 |
| Neurofibromatosis type 1 (NF1) | PanNET Duodenal NET | Gastrointestinal Stromal Tumor (GIST) Optic glioma Meningioma Astrocytoma Neurofibrosarcoma Pheochromocytoma Breast cancer | Café au lait macule Neurofibroma Axillary/inguinal freckling Lisch nodules Bone abnormalities | Prevalence 1 in 3000 |
| Multiple endocrine neoplasia type 4 (MEN4) | PanNET Duodenal NET LNET Gastric NET Small intestinal NET | Primary hyperparathyroidism Pituitary adenoma | Prevalence 1 in 1,000,000 |
| Type 1 | Renal cell carcinoma (RCC), retinal hemangioblastoma, CNS hemangioblastoma, low risk for a pheochromocytoma |
| Type 2 | Retinal hemangioblastoma, CNS hemangioblastoma, high risk for a pheochromocytoma |
| Type 2A | Low risk for RCC |
| Type 2B | High risk for RCC |
| Type 2C | Risk for pheochromocytoma only |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papadopoulou-Marketou, N.; Tsoli, M.; Chatzellis, E.; Alexandraki, K.I.; Kaltsas, G. Hereditary Syndromes Associated with Pancreatic and Lung Neuroendocrine Tumors. Cancers 2024, 16, 2075. https://doi.org/10.3390/cancers16112075
Papadopoulou-Marketou N, Tsoli M, Chatzellis E, Alexandraki KI, Kaltsas G. Hereditary Syndromes Associated with Pancreatic and Lung Neuroendocrine Tumors. Cancers. 2024; 16(11):2075. https://doi.org/10.3390/cancers16112075
Chicago/Turabian StylePapadopoulou-Marketou, Nektaria, Marina Tsoli, Eleftherios Chatzellis, Krystallenia I. Alexandraki, and Gregory Kaltsas. 2024. "Hereditary Syndromes Associated with Pancreatic and Lung Neuroendocrine Tumors" Cancers 16, no. 11: 2075. https://doi.org/10.3390/cancers16112075
APA StylePapadopoulou-Marketou, N., Tsoli, M., Chatzellis, E., Alexandraki, K. I., & Kaltsas, G. (2024). Hereditary Syndromes Associated with Pancreatic and Lung Neuroendocrine Tumors. Cancers, 16(11), 2075. https://doi.org/10.3390/cancers16112075








