Skin Malignancies Due to Anti-Cancer Therapies
Abstract
Simple Summary
Abstract
1. Introduction
2. Classic Immunosuppressants
2.1. Methotrexate
2.1.1. Clinical Indications and Mechanism of Action of Methotrexate
2.1.2. Oncogenic Mechanism of Methotrexate
2.2. mTOR Inhibitors
2.2.1. Clinical Indications and Mechanism of Action of mTOR Inhibitors
2.2.2. Oncogenic Mechanism of mTOR Inhibitors
3. Chemotherapeutic Agents
3.1. Fludarabine
3.1.1. Clinical Indications and Mechanism of Action of Fludarabine
3.1.2. Oncogenic Mechanism of Fludarabine
3.2. Hydroxyurea (HU)
3.2.1. Clinical Indications and Mechanism of Action of Hydroxyurea
3.2.2. Oncogenic Mechanism of Hydroxyurea
3.2.3. Management of Patients in Therapy with Hydroxyurea
4. Targeted Therapies
4.1. Ibrutinib
4.1.1. Clinical Indications and Mechanism of Action of Ibrutinib
4.1.2. Oncogenic Mechanism of Hydroxyurea
4.2. JAKi
4.2.1. Mechanism of Action of JAKi
4.2.2. Clinical Indications of JAKi
4.2.3. Oncogenic Mechanism of JAKi
4.2.4. Management of Patients in Therapy with JAKi
4.3. MAPKP Inhibitors
4.3.1. Clinical Indications of MAPKP Inhibitors
4.3.2. Oncogenic Mechanism of MAPKP Inhibitors
4.3.3. Incidence of NMSC in Patients Treated with MAPKP Inhibitors
4.3.4. Incidence of SPMs in Patients Treated with MAPKP Inhibitors
4.3.5. Management of Patients in Therapy with MAPKP Inhibitors
4.4. SSHPi
4.4.1. Clinical Indications and Mechanism of Action of SSHPi
4.4.2. Oncogenic Mechanism of SSHPi
4.4.3. Management of Patients in Therapy with SSHPi
5. Radiotherapy
5.1. Incidence of NMSC in Patients Treated with Radiotherapy
5.2. Oncogenic Mechanism of Radiotherapy
5.3. Angiosarcomas Post-Radiotherapy
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kreher, M.A.; Noland, M.M.B.; Konda, S.; Longo, M.I.; Valdes-Rodriguez, R. Risk of melanoma and nonmelanoma skin cancer with immunosuppressants, part I: Calcineurin inhibitors, thiopurines, IMDH inhibitors, mTOR inhibitors, and corticosteroids. J. Am. Acad. Dermatol. 2023, 88, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Ansary, T.M.; Hossain, M.R.; Komine, M.; Ohtsuki, M. Immunotherapy for the Treatment of Squamous Cell Carcinoma: Potential Benefits and Challenges. Int. J. Mol. Sci. 2022, 23, 8530. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.M.; Prickett, K.A.; Phillips, M.A. Systemic medications linked to an increased risk for skin malignancy. Cutis 2019, 104, 32–36. [Google Scholar]
- Crow, L.D.; Kaizer-Salk, K.A.; Juszczak, H.M.; Arron, S.T. Medications Associated with Increased Risk of Keratinocyte Carcinoma. Dermatol. Clin. 2019, 37, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Wang, B.; Lowe, L.; Dlugosz, A.; Bichakjian, C.K. Metastatic same-site squamous cell carcinoma arising during vismodegib therapy for basal cell carcinoma. JAAD Case Rep. 2022, 28, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Morison, W.L.; Momtaz, K.; Parrish, J.A.; Fitzpatrick, T.B. Combined methotrexate-PUVA therapy in the treatment of psoriasis. J. Am. Acad. Dermatol. 1982, 6, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Chahidi, C.; Morliere, P.; Aubailly, M.; Dubertret, L.; Santus, R. Photosensitization by methotrexate photoproducts. Photochem. Photobiol. 1983, 38, 317–322. [Google Scholar] [CrossRef]
- Polesie, S.; Gillstedt, M.; Schmidt, S.A.J.; Egeberg, A.; Pottegård, A.; Kristensen, K. Use of methotrexate and risk of skin cancer: A nationwide case-control study. Br. J. Cancer 2023, 128, 1311–1319. [Google Scholar] [CrossRef] [PubMed]
- Kreher, M.A.; Konda, S.; Noland, M.M.B.; Longo, M.I.; Valdes-Rodriguez, R. Risk of melanoma and nonmelanoma skin cancer with immunosuppressants, part II: Methotrexate, alkylating agents, biologics, and small molecule inhibitors. J. Am. Acad. Dermatol. 2023, 88, 534–542. [Google Scholar] [CrossRef]
- Lange, E.; Blizzard, L.; Venn, A.; Francis, H.; Jones, G. Disease-modifying anti-rheumatic drugs and non-melanoma skin cancer in inflammatory arthritis patients: A retrospective cohort study. Rheumatology 2016, 55, 1594–1600. [Google Scholar] [CrossRef]
- Vanni, K.M.M.; Berliner, N.; Paynter, N.P.; Glynn, R.J.; MacFadyen, J.; Colls, J.; Lu, F.; Xu, C.; Ridker, P.M.; Solomon, D.H. Adverse Effects of Low-Dose Methotrexate in a Randomized Double-Blind Placebo-Controlled Trial: Adjudicated Hematologic and Skin Cancer Outcomes in the Cardiovascular Inflammation Reduction Trial. ACR Open Rheumatol. 2020, 2, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Buchbinder, R.; Barber, M.; Heuzenroeder, L. Incidence of melanoma and other malignancies among rheumatoid arthritis patients treated with methotrexate. Arthritis Rheum. 2008, 59, 794–799. [Google Scholar] [CrossRef]
- Yan, M.K.; Wang, C.; Wolfe, R.; Mar, V.J.; Wluka, A.E. Association between low-dose methotrexate exposure and melanoma: A systematic review and meta-analysis. JAMA Dermatol. 2022, 158, 1157–1166. [Google Scholar] [CrossRef] [PubMed]
- McMahon, G.; Weir, M.R.; Li, X.C.; Mandelbrot, D.A. The evolving role of mTOR inhibition in transplantation tolerance. J. Am. Soc. Nephrol. JASN 2011, 22, 408–415. [Google Scholar] [CrossRef]
- Limson, M.V.; Sweder, K.S. Rapamycin inhibits yeast nucleotide excision repair independently of tor kinases. Toxicol. Sci. Off. J. Soc. Toxicol. 2010, 113, 77–84. [Google Scholar] [CrossRef]
- Thoms, K.M.; Kuschal, C.; Emmert, S. Lessons learned from DNA repair defective syndromes. Exp. Dermatol. 2007, 16, 532–544. [Google Scholar] [CrossRef] [PubMed]
- Kuschal, C.; Thoms, K.M.; Schubert, S.; Schäfer, A.; Boeckmann, L.; Schön, M.P.; Emmert, S. Skin cancer in organ transplant recipients: Effects of immunosuppressive medications on DNA repair. Exp. Dermatol. 2012, 21, 2–6. [Google Scholar] [CrossRef]
- Keating, M.J.; O’Brien, S.; Lerner, S.; Koller, C.; Beran, M.; Robertson, L.E.; Freireich, E.J.; Estey, E.; Kantarjian, H. Long-term follow-up of patients with chronic lymphocytic leukemia (CLL) receiving fludarabine regimens as initial therapy. Blood 1998, 92, 1165–1171. [Google Scholar] [CrossRef]
- Lukenbill, J.; Kalaycio, M. Fludarabine: A review of the clear benefits and potential harms. Leuk. Res. 2013, 37, 986–994. [Google Scholar] [CrossRef]
- Robak, T.; Lech-Maranda, E.; Korycka, A.; Robak, E. Purine nucleoside analogs as immunosuppressive and antineoplastic agents: Mechanism of action and clinical activity. Curr. Med. Chem. 2006, 13, 3165–3189. [Google Scholar] [CrossRef]
- Lam, C.J.; Curtis, R.E.; Dores, G.M.; Engels, E.A.; Caporaso, N.E.; Polliack, A.; Warren, J.L.; Young, H.A.; Levine, P.H.; Elmi, A.F.; et al. Risk Factors for Melanoma Among Survivors of Non-Hodgkin Lymphoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 3096–3104. [Google Scholar] [CrossRef] [PubMed]
- Gavini, D.R.; Salvi, D.J.; Shah, P.H.; Uma, D.; Lee, J.H.; Hamid, P. Non-melanoma Skin Cancers in Patients on Hydroxyurea for Philadelphia Chromosome-Negative Myeloproliferative Neoplasms: A systematic review. Cureus 2021, 13, 16978. [Google Scholar] [CrossRef]
- Erixon, K.; Ahnström, G. Single-strand breaks in DNA during repair of UV-induced damage in normal human and xeroderma pigmentosum cells as determined by alkaline DNA unwinding and hydroxylapatite chromatography: Effects of hydroxyurea, 5-fluorodeoxyuridine and 1-beta-D-arabinofuranosylcytosine on the kinetics of repair. Mutat. Res. 1979, 59, 257–271. [Google Scholar]
- Brash, D.E.; Ziegler, A.; Jonason, A.S.; Simon, J.A.; Kunala, S.; Leffell, D.J. Sunlight and sunburn in human skin cancer: p53, apoptosis, and tumor promotion. J. Investig. Dermatol. Symp. Proc. 1996, 1, 136–142. [Google Scholar] [PubMed]
- Bulte, C.A.; Hoegler, K.M.; Kutlu, Ö.; Khachemoune, A. Hydroxyurea: A reappraisal of its cutaneous side effects and their management. Int. J. Dermatol. 2021, 60, 810–817. [Google Scholar] [CrossRef]
- Cantisani, C.; Kiss, N.; Naqeshbandi, A.F. Nonmelanoma skin cancer associated with Hydroxyurea treatment: Overview of the literature and our own experience. Dermatol. Ther. 2019, 32, e13043. [Google Scholar] [CrossRef]
- Malato, A.; Rossi, E.; Palumbo, G.A.; Guglielmelli, P.; Pugliese, N. Drug-Related Cutaneous Adverse Events in Philadelphia Chromosome-Negative Myeloproliferative Neoplasms: A Literature Review. Int. J. Mol. Sci. 2020, 21, 3900. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Palacios, C.; Guitart, J. Hydroxyurea-associated squamous dysplasia. J. Am. Acad. Dermatol. 2004, 51, 293–300. [Google Scholar] [CrossRef]
- Sun, X.; Ma, Z.; Guo, Q.; Zhao, Z.; Liu, L. Ibrutinib-related skin cancer: A pharmacovigilance study from the Food and Drug Administration Adverse Event Reporting System. Eur. J. Cancer 2022, 160, 277–278. [Google Scholar] [CrossRef]
- March-Rodriguez, Á.; Bellosillo, B.; Álvarez-Larrán, A.; Besses, C.; Pujol, R.M.; Toll, A. Rapidly Growing and Aggressive Cutaneous Squamous Cell Carcinomas in a Patient Treated with Ruxolitinib. Ann. Dermatol. 2019, 31, 204–208. [Google Scholar] [CrossRef]
- Harrison, C.N.; Vannucchi, A.M.; Kiladjian, J.J.; Al-Ali, H.K.; Gisslinger, H.; Knoops, L.; Cervantes, F.; Jones, M.M.; Sun, K.; McQuitty, M.; et al. Long-term findings from COMFORT-II, a phase 3 study of ruxolitinib vs best available therapy for myelofibrosis. Leukemia 2016, 30, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Verstovsek, S.; Vannucchi, A.M.; Griesshammer, M.; Masszi, T.; Durrant, S.; Passamonti, F.; Harrison, C.N.; Pane, F.; Zachee, P.; Kirito, K.; et al. Ruxolitinib versus best available therapy in patients with polycythemia vera: 80-week follow-up from the RESPONSE trial. Haematologica 2016, 101, 821–829. [Google Scholar] [CrossRef]
- Ytterberg, S.R.; Bhatt, D.L.; Mikuls, T.R.; Koch, G.G.; Fleischmann, R.; Rivas, J.L.; Germino, R.; Menon, S.; Sun, Y.; Wang, C.; et al. Cardiovascular and Cancer Risk with Tofacitinib in Rheumatoid Arthritis. N. Engl. J. Med. 2022, 386, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.B.; van Vollenhoven, R.F.; Winthrop, K.L.; Zerbini, C.A.F.; Tanaka, Y.; Bessette, L.; Zhang, Y.; Khan, N.; Hendrickson, B.; Enejosa, J.V.; et al. Safety profile of upadacitinib in rheumatoid arthritis: Integrated analysis from the SELECT phase III clinical programme. Ann. Rheum. Dis. 2021, 80, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Polverelli, N.; Elli, E.M.; Abruzzese, E.; Palumbo, G.A.; Benevolo, G.; Tiribelli, M.; Bonifacio, M.; Tieghi, A.; Caocci, G.; D’Adda, M.; et al. Second primary malignancy in myelofibrosis patients treated with ruxolitinib. Br. J. Haematol. 2021, 193, 356–368. [Google Scholar] [CrossRef]
- Moutel, M.; Noel, V.; Jary, A.; Le, Q.H.; Lier, C.; Viguier, M.; Lebbe, C.; Azzouz, B.; Bani-Sadr, F. Iatrogenic Kaposi’s sarcoma in a myelofibrosis patient treated with ruxolitinib: Case-report, literature review, and French pharmacovigilance data. Am. J. Hematol. 2022, 97, E31–E34. [Google Scholar] [CrossRef] [PubMed]
- Wetwittayakhlang, P.; Golovics, P.A.; Afif, W.; Bessissow, T.; Lakatos, P.L. Tofacitinib-Associated Iatrogenic Kaposi Sarcoma in a Patient with Ulcerative Colitis. ACG Case Rep. J. 2021, 8, e00678. [Google Scholar] [CrossRef]
- King, A.J.; Arnone, M.R.; Bleam, M.R.; Moss, K.G.; Yang, J.; Fedorowicz, K.E.; Smitheman, K.N.; Erhardt, J.A.; Hughes-Earle, A.; Kane-Carson, L.S.; et al. Dabrafenib; preclinical characterization, increased efficacy when combined with trametinib, while BRAF/MEK tool combination reduced skin lesions. PLoS ONE 2013, 8, e67583. [Google Scholar] [CrossRef] [PubMed]
- Poulikakos, P.I.; Zhang, C.; Bollag, G.; Shokat, K.M.; Rosen, N. RAF inhibitors transactivate RAF dimers and ERK signalling in cells with wild-type BRAF. Nature 2010, 464, 427–430. [Google Scholar] [CrossRef]
- Heidorn, S.J.; Milagre, C.; Whittaker, S.; Nourry, A.; Niculescu-Duvas, I.; Dhomen, N.; Hussain, J.; Reis-Filho, J.S.; Springer, C.J.; Pritchardet, C.; et al. Kinase-dead BRAF and oncogenic RAS cooperate to drive tumor progression through CRAF. Cell 2010, 140, 209–221. [Google Scholar] [CrossRef]
- Flaherty, K.T.; Puzanov, I.; Kim, K.B.; Ribas, A.; McArthur, G.A.; Sosman, J.A.; O’Dwyer, P.J.; Lee, R.J.; Grippo, J.F.; Nolop, K.; et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N. Engl. J. Med. 2010, 363, 809–819. [Google Scholar] [CrossRef]
- McArthur, G.A.; Chapman, P.B.; Robert, C.; Larkin, J.; Haanen, J.B.; Dummer, R.; Ribas, A.; Hogg, D.; Hamid, O.; Ascierto, P.A.; et al. Safety and efficacy of vemurafenib in BRAF(V600E) and BRAF(V600K) mutation-positive melanoma (BRIM-3): Extended follow-up of a phase 3, randomised, open-label study. Lancet Oncol. 2014, 15, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Su, F.; Viros, A.; Milagre, C.; Trunzer, K.; Bollag, G.; Spleiss, O.; Reis-Filho, J.S.; Kong, X.; Koya, R.C.; Flaherty, K.T.; et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. N. Engl. J. Med. 2012, 366, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Wang, Y.; Hong, Y.; Ye, X.; Shi, P.; Zhang, J.; Zhao, Q. Incidence and relative risk of cutaneous squamous cell carcinoma with single-agent BRAF inhibitor and dual BRAF/MEK inhibitors in cancer patients: A meta-analysis. Oncotarget 2017, 8, 83280–83291. [Google Scholar] [CrossRef] [PubMed]
- Williams, V.L.; Cohen, P.R.; Stewart, D.J. Sorafenib-induced premalignant and malignant skin lesions. Int. J. Dermatol. 2011, 50, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Arnault, J.P.; Wechsler, J.; Escudier, B.; Spatz, A.; Tomasic, G.; Sibaud, V.; Aractingi, S.; Grange, J.D.; Poirier-Colame, V.; Malka, D.; et al. Keratoacanthomas and Squamous Cell Carcinomas in Patients Receiving Sorafenib. J. Clin. Oncol. 2009, 27, e59–e61. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.J.; Haley, H.; Hamza, S.; Skelton, H.G. Eruptive keratoacanthoma-type squamous cell carcinomas in patients taking sorafenib for the treatment of solid tumors. Dermatol. Surg. 2009, 35, 1766–1770. [Google Scholar] [CrossRef] [PubMed]
- Long, G.V.; Menzies, A.M.; Nagrial, A.M.; Haydu, L.E.; Hamilton, A.L.; Mann, G.J.; Hughes, T.M.; Thompson, J.F.; Scolyer, R.A.; Kefford, R.F. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2011, 29, 1239–1246. [Google Scholar] [CrossRef] [PubMed]
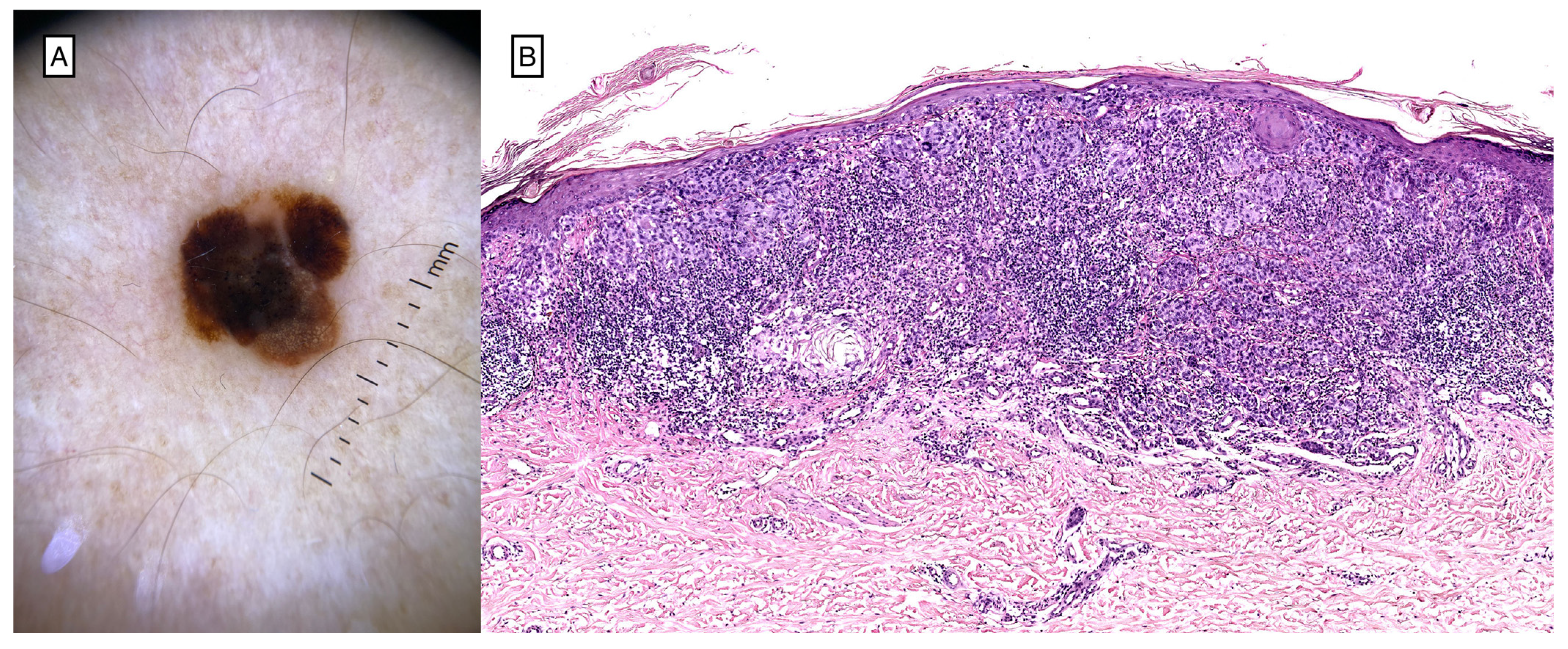
- Zimmer, L.; Hillen, U.; Livingstone, E.; Lacouture, M.E.; Busam, K.; Carvajal, R.D.; Egberts, F.; Hauschild, A.; Kashani-Sabet, M.; Goldinger, S.M.; et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2012, 30, 2375–2383. [Google Scholar] [CrossRef]
- Dalle, S.; Poulalhon, N.; Debarbieux, S. Tracking of second primary melanomas in vemurafenib-treated patients. JAMA Dermatol. 2013, 149, 488–490. [Google Scholar] [CrossRef]
- Mohan, S.V.; Chang, J.; Li, S.; Henry, A.S.; Wood, D.J.; Chang, A.L.S. Increased Risk of Cutaneous Squamous Cell Carcinoma After Vismodegib Therapy for Basal Cell Carcinoma. JAMA Dermatol. 2016, 152, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Kuonen, F.; Huskey, N.E.; Shankar, G.; Jaju, P.; Whitson, R.J.; Rieger, K.E.; Atwood, S.X.; Sarin, K.Y.; Oro, A.E. Loss of Primary Cilia Drives Switching from Hedgehog to Ras/MAPK Pathway in Resistant Basal Cell Carcinoma. J. Invest. Dermatol. 2019, 139, 1439–1448. [Google Scholar] [CrossRef] [PubMed]
- Leisenring, W.; Friedman, D.L.; Flowers, M.E.; Schwartz, J.L.; Deeg, H.J. Nonmelanoma skin and mucosal cancers after hematopoietic cell transplantation. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2006, 24, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Teepen, J.C.; Kok, J.L.; Kremer, L.C.; Tissing, W.J.E.; Heuvel-Eibrink, M.M.; Loonen, J.J.; Bresters, D.; Pal, H.J.; Versluys, B.; Dulmen-den Broeder, E.; et al. Long-Term Risk of Skin Cancer Among Childhood Cancer Survivors: A DCOG-LATER Cohort Study. J. Natl. Cancer Inst. 2019, 111, 845–853. [Google Scholar] [CrossRef]
- Ron, E.; Modan, B.; Preston, D.; Alfandary, E.; Stovall, M.; Boice, J.D., Jr. Radiation-induced skin carcinomas of the head and neck. Radiat. Res. 1991, 125, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Shore, R.E.; Moseson, M.; Xue, X.; Tse, Y.; Harley, N.; Pasternack, B.S. Skin cancer after X-ray treatment for scalp ringworm. Radiat. Res. 2002, 157, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Neglia, J.P.; Friedman, D.L.; Yasui, Y.; Mertens, A.C.; Hammond, S.; Stovall, M.; Donaldson, S.S.; Meadows, A.T.; Robison, L.L. Second malignant neoplasms in five-year survivors of childhood cancer: Childhood cancer survivor study. J. Natl. Cancer Inst. 2001, 93, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Goldust, M.; Giulini, M.; Weidenthaler-Barth, B.; Gupta, M.; Grabbe, S.; Schepler, H. Increased risk of angiosarcoma secondary to cancer radiotherapy: Case series and review of the treatment options. Dermatol. Ther. 2020, 33, e13234. [Google Scholar] [CrossRef]
- UpToDate. Methotrexate: Drug information. In UpToDate PTW; UpToDate: Waltham, MA, USA, 2024. [Google Scholar]
- Thoms, K.M.; Kuschal, C.; Oetjen, E.; Mori, T.; Kobayashi, N.; Laspe, P.; Boeckmann, L.; Schön, M.P.; Emmert, S. Cyclosporin A, but not everolimus, inhibits DNA repair mediated by calcineurin: Implications for tumorigenesis under immunosuppression. Exp. Dermatol. 2011, 20, 232–236. [Google Scholar] [CrossRef]
- Chen, H.; Ma, Z.; Vanderwaal, R.P.; Feng, Z.; Gonzalez-Suarez, I.; Wang, S.; Zhang, J.; Roti Roti, J.L.; Gonzalo, S.; Zhang, J. The mTOR inhibitor rapamycin suppresses DNA double-strand break repair. Radiat. Res. 2011, 175, 214–224. [Google Scholar] [CrossRef]
- Ricci, F.; Tedeschi, A.; Morra, E.; Montillo, M. Fludarabine in the treatment of chronic lymphocytic leukemia: A review. Ther. Clin. Risk Manag. 2009, 5, 187–207. [Google Scholar] [PubMed]
- Donehower, R.C. An overview of the clinical experience with hydroxyurea. Semin. Oncol. 1992, 19 (Suppl. 9), 11–19. [Google Scholar]
- Spivak, J.L.; Hasselbalch, H. Hydroxycarbamide: A user’s guide for chronic myeloproliferative disorders. Expert Rev. Anticancer. Ther. 2011, 11, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Simeonovski, V.; Breshkovska, H.; Duma, S.; Dohcheva-Karajovanov, I.; Damevska, K.; Nikolovska, S. Hydroxyurea Associated Cutaneous Lesions: A Case Report. Open Access Maced. J. Med. Sci. 2018, 6, 1458–1461. [Google Scholar] [CrossRef]
- Radaelli, F.; Onida, F.; Rossi, F.G. Second malignancies in essential thrombocythemia (ET): A retrospective analysis of 331 patients with long-term follow-up from a single institution. Hematology 2008, 13, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Verner, E.; Forsyth, C.; Grigg, A. Cyclical thrombocytosis, acquired von Willebrand syndrome and aggressive non-melanoma skin cancers are common in patients with Philadelphia-negative myeloproliferative neoplasms treated with hydroxyurea. Leuk. Lymphoma 2014, 55, 1139–1143. [Google Scholar] [CrossRef] [PubMed]
- Santoro, C.; Sperduti, I.; Latagliata, R. Role of treatment on the development of secondary malignancies in patients with essential thrombocythemia. Cancer Med. 2017, 6, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Damsky, W.; King, B.A. JAK inhibitors in dermatology: The promise of a new drug class. J. Am. Acad. Dermatol. 2017, 76, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.Q.; Li, S.Q.; Li, S.; Kiamanesh, E.F.; Aasi, S.Z.; Kwong, B.Y.; Chang, A.L.S. A 10-year retrospective cohort study of ruxolitinib and association with nonmelanoma skin cancer in patients with polycythemia vera and myelofibrosis. J. Am. Acad. Dermatol. 2022, 86, 339–344. [Google Scholar] [CrossRef]
- Papp, K.A.; Menter, M.A.; Abe, M.; Elewski, B.; Feldman, S.R.; Gottlieb, A.B.; Langley, R.; Luger, T.; Thaci, D.; Buonanno, M.; et al. Tofacitinib, an oral Janus kinase inhibitor, for the treatment of chronic plaque psoriasis: Results from two randomized, placebo-controlled, phase III trials. Br. J. Dermatol. 2015, 173, 949–961. [Google Scholar] [CrossRef]
- Olivera, P.A.; Lasa, J.S.; Bonovas, S.; Danese, S.; Peyrin-Biroulet, L. Safety of Janus Kinase Inhibitors in Patients with Inflammatory Bowel Diseases or Other Immune-mediated Diseases: A Systematic Review and Meta-Analysis. Gastroenterology 2020, 158, 1554–1573.e12. [Google Scholar] [CrossRef] [PubMed]
- Verstovsek, S.; Mesa, R.A.; Gotlib, J.; Gupta, V.; DiPersio, J.F.; Catalano, J.V.; Deininger, M.W.; Miller, C.B.; Silver, R.T.; Talpaz, M.; et al. Long-term treatment with ruxolitinib for patients with myelofibrosis: 5-year update from the randomized, double-blind, placebo-controlled, phase 3 COMFORT-I trial. J. Hematol. Oncol. 2017, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- Sekhri, R.; Sadjadian, P.; Becker, T.; Kolatzki, V.; Huenerbein, K.; Meixner, R.; Marchi, H.; Wallmann, R.; Fuchs, C.; Griesshammer, M.; et al. Ruxolitinib-treated polycythemia vera patients and their risk of secondary malignancies. Ann. Hematol. 2021, 100, 2707–2716. [Google Scholar] [CrossRef] [PubMed]
- Mora, B.; Rumi, E.; Guglielmelli, P.; Barraco, D.; Maffioli, M.; Rambaldi, A.; Caramella, M.; Komrokji, R.; Gotlib, J.; Kiladjian, J.J.; et al. Second primary malignancies in postpolycythemia vera and postessential thrombocythemia myelofibrosis: A study on 2233 patients. Cancer Med. 2019, 8, 4089–4092. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, T.; Hidaka, T.; Kambayashi, Y.; Aiba, S. BRAF kinase inhibitors for treatment of melanoma: Developments from early-stage animal studies to Phase II clinical trials. Expert Opin. Investig. Drugs 2019, 28, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Xie, P.; Lefrançois, P. Efficacy, safety, and comparison of sonic hedgehog inhibitors in basal cell carcinomas: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2018, 79, 1089–1100.e17. [Google Scholar] [CrossRef] [PubMed]
- Bhutani, T.; Abrouk, M.; Sima, C.S.; Sadetsky, N.; Hou, J.; Caro, I.; Chren, M.M.; Arron, S.T. Risk of cutaneous squamous cell carcinoma after treatment of basal cell carcinoma with vismodegib. J. Am. Acad. Dermatol. 2017, 77, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Hegemann, N.S.; Schlesinger-Raab, A.; Ganswindt, U.; Hörl, C.; Combs, S.E.; Hölzel, D.; Gschwend, J.E.; Stief, C.; Belka, C.; Engel, J. Risk of second cancer following radiotherapy for prostate cancer: A population-based analysis. Radiat. Oncol. 2017, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Vloten, W.A.; Hermans, J.; Daal, W.A. Radiation-induced skin cancer and radiodermatitis of the head and neck. Cancer 1987, 59, 411–414. [Google Scholar] [CrossRef]
- Little, M.P. Comparison of the risks of cancer incidence and mortality following radiation therapy for benign and malignant disease with the cancer risks observed in the Japanese A-bomb survivors. Int. J. Radiat. Biol. 2001, 77, 431–464. [Google Scholar] [CrossRef]
- Karagas, M.R.; McDonald, J.A.; Greenberg, E.R.; Stukel, T.A.; Weiss, J.E.; Baron, J.A.; Stevens, M.M. Risk of basal cell and squamous cell skin cancers after ionizing radiation therapy. For The Skin Cancer Prevention Study Group. J. Natl. Cancer Inst. 1996, 88, 1848–1853. [Google Scholar] [CrossRef] [PubMed]
- Shore, R.E. Overview of Radiation-induced Skin Cancer in Humans. Int. J. Radiat. Biol. 1990, 57, 809–827. [Google Scholar] [CrossRef] [PubMed]
- Zelefsky, M.J.; Housman, D.M.; Pei, X.; Alicikus, Z.; Magsanoc, J.M.; Dauer, L.T.; Germain, J.S.; Yamada, Y.; Kollmeier, M.; Cox, B.; et al. Incidence of Secondary Cancer Development After High-Dose Intensity-Modulated Radiotherapy and Image-Guided Brachytherapy for the Treatment of Localized Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, 953–959. [Google Scholar] [CrossRef]
- Kim, D.W.; Chung, K.; Chung, W.K.; Bae, S.H.; Shin, D.O.; Hong, S.; Park, S.H.; Park, S.Y.; Hong, C.S.; Lim, Y.K.; et al. Risk of secondary cancers from scattered radiation during intensity-modulated radiotherapies for hepatocellular carcinoma. Radiat. Oncol. 2014, 9, 109. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, B.K.; Kricker, A. The epidemiology of UV induced skin cancer. J. Photochem. Photobiol. B Biol. 2001, 63, 8–18. [Google Scholar] [CrossRef]
- Tucker, M.A.; Jones, P.H.; Boice, J.D., Jr.; Robison, L.L.; Stone, B.J.; Stovall, M.; Jenkin, R.D.; Lubin, J.H.; Baum, E.S.; Siegel, S.E.; et al. Therapeutic radiation at a young age is linked to secondary thyroid cancer. Cancer Res. 1991, 51, 2885–2888. [Google Scholar]


| Drugs | Oncogenic Mechanism | Associated Skin Malignancies |
|---|---|---|
| MTX | Immunosuppressive and photosensitizing action [6,7,8,9]. | BCC [8,10] cSCC [8,10,11] CM [8,12,13] |
| mTOR inhibitors | Suppression of the immune system [14]. Mutagenesis in normal tissues [15]. Unsure whether to prevent the onset of skin cancer [1]. | BCC [16,17] cSCC [1,16,17] CM [1,16,17] Mucosae melanoma [16] |
| Fludarabine | Inherent predisposition to malignancy, immunosuppressive and DNA-damaging effects [18,19,20]. | CM [21] |
| HU | Inhibition of DNA synthesis and repair in cutaneous cells, inducing mutations [22,23,24]. | BCC [25,26] cSCC [22,25,26,27,28] CM [22,27] MCC [22,25,27] AK [22,25,26,27,28] Bowen’s disease [25,28] Keratoacanthoma [25] |
| Ibrutinib | Increased photosensitivity [29]. | NMSC [9,29] MC [9,29] |
| JAKi | Inhibition of immune function leads to the promotion of tumor growth [30]. | BCC [31,32,33,34,35] cSCC [30,31,32,33,34,35] CM [35] Kaposi sarcoma [36,37] |
| MAPKPi | Proliferation in wild-type BRAF cells [2,3,38,39,40]. | cSCC [2,3,38,39,40,41,42,43,44,45,46,47] Keratoacanthoma [41,43,45,46] SPM [48,49,50] |
| SSHPi | Inhibition of the hedgehog pathway activates the RAS/MAPK pathway, thus avoiding dependence on the hedgehog pathway for tumor growth [51,52]. | cSCC [3,4,5,51] Keratoacanthoma [3,4,5] |
| Radiotherapy | Increased sensitivity of the basal layer of the epidermis to radiation [53,54]. | BCC [53,54,55,56,57] Angiosarcoma [58] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starace, M.; Rapparini, L.; Cedirian, S. Skin Malignancies Due to Anti-Cancer Therapies. Cancers 2024, 16, 1960. https://doi.org/10.3390/cancers16111960
Starace M, Rapparini L, Cedirian S. Skin Malignancies Due to Anti-Cancer Therapies. Cancers. 2024; 16(11):1960. https://doi.org/10.3390/cancers16111960
Chicago/Turabian StyleStarace, Michela, Luca Rapparini, and Stephano Cedirian. 2024. "Skin Malignancies Due to Anti-Cancer Therapies" Cancers 16, no. 11: 1960. https://doi.org/10.3390/cancers16111960
APA StyleStarace, M., Rapparini, L., & Cedirian, S. (2024). Skin Malignancies Due to Anti-Cancer Therapies. Cancers, 16(11), 1960. https://doi.org/10.3390/cancers16111960








