Cholangiocarcinoma: The Current Status of Surgical Options including Liver Transplantation
Abstract
Simple Summary
Abstract
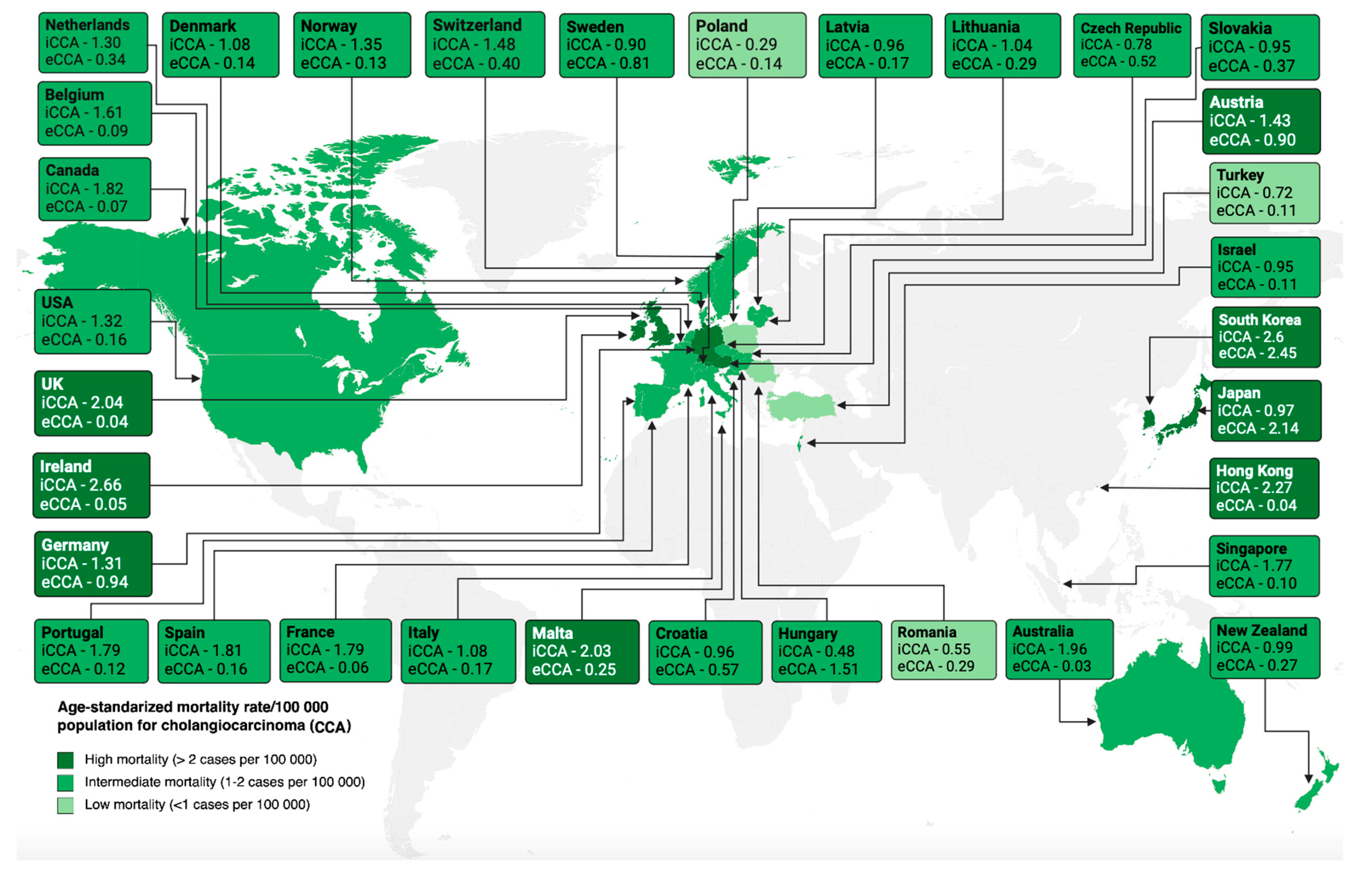
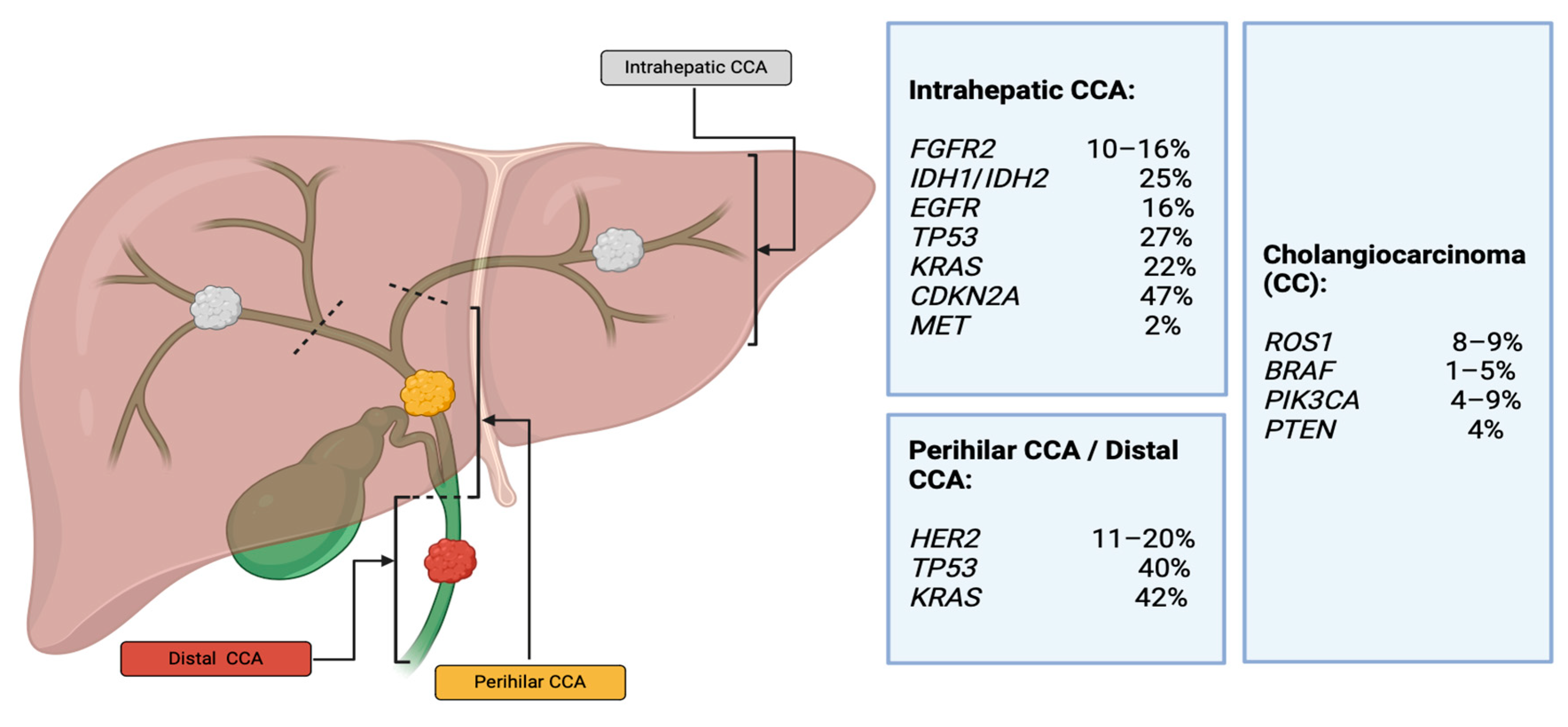
1. Introduction
2. Diagnostic Evaluation
| Technique | Sensitivity | Specificity | Advantages | Limitations |
|---|---|---|---|---|
| Ultrasound | 87–96% [39] | - |
|
|
| CT scan | 61% [41] | 88% [41] |
|
|
| MRI | 90–97% [43] | 60–81% [43] |
|
|
| Direct Cholangiography (ERCP/PTC) | 46–73% [47,48] | 100% (with tissue sampling) [47,48] |
|
|
| Direct single operator cholangioscopy combined with (DSOC) | 85–86% [47,48,50] | 100% (with tissue sampling) [47,48,50] |
|
|
| Linear endoscopic ultrasound with fine needle aspiration(EUS-FNA) | 43–89% (Better for dCCA than pCCA) [51,52,53]. | 79–100% [53] |
|
|
| Intraductal sonography(IDUS) | 89–91% [55]. | 80–92% [55] |
|
|
| Confocal laser endomicroscopy(CLE) | 88% [56] | 79% [56] |
|
3. Surgical Management
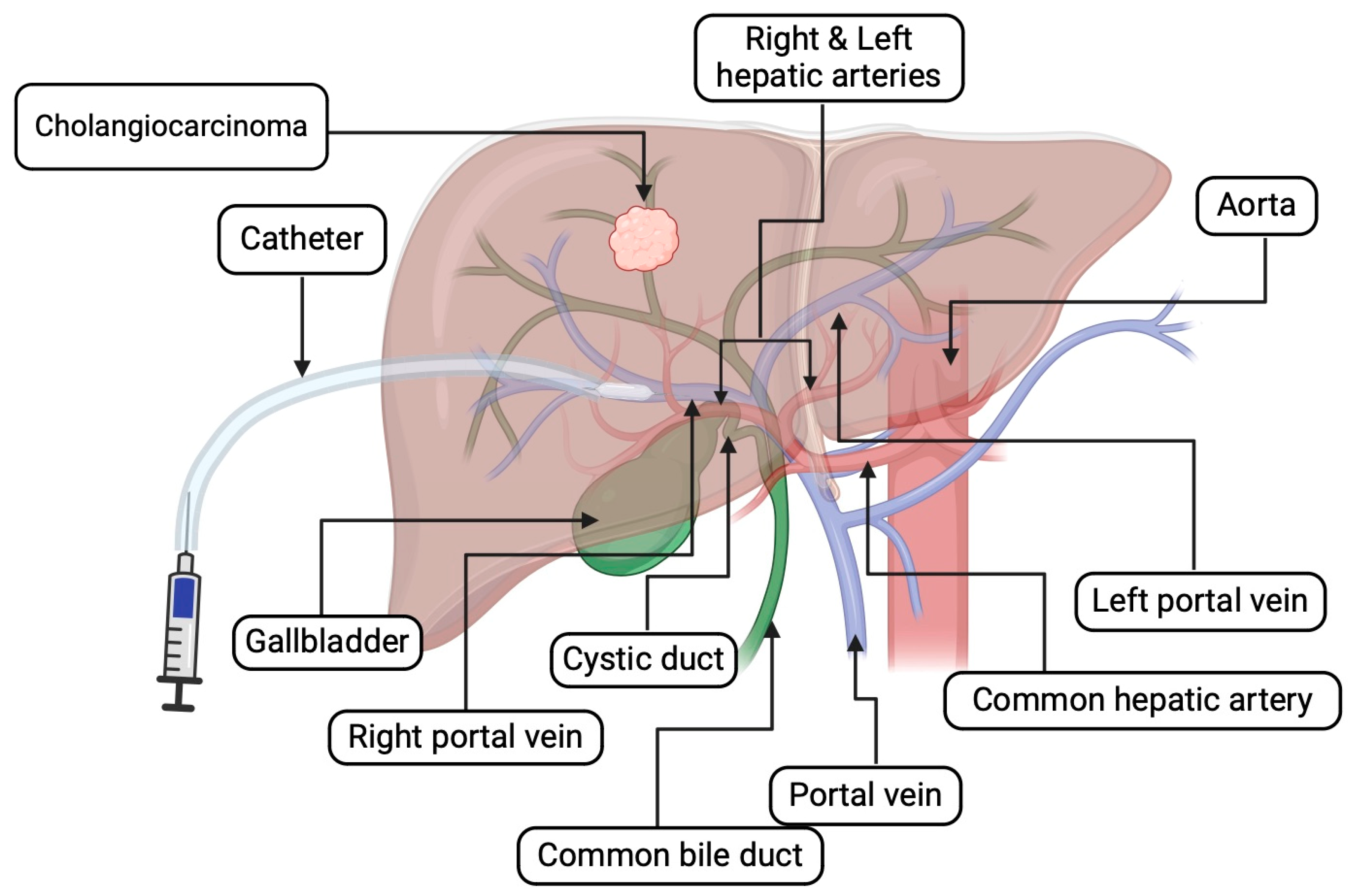
3.1. Preoperative Intervention
3.1.1. Staging Laparoscopy
3.1.2. Preoperative Biliary Decompression
3.1.3. Preoperative Portal Vein Embolization (PVE)
3.2. Hepatic Resection
3.2.1. General Considerations in Hepatic Resection
- a
- Criteria of resectability
- b
- Future liver remnant (FLR)
- c
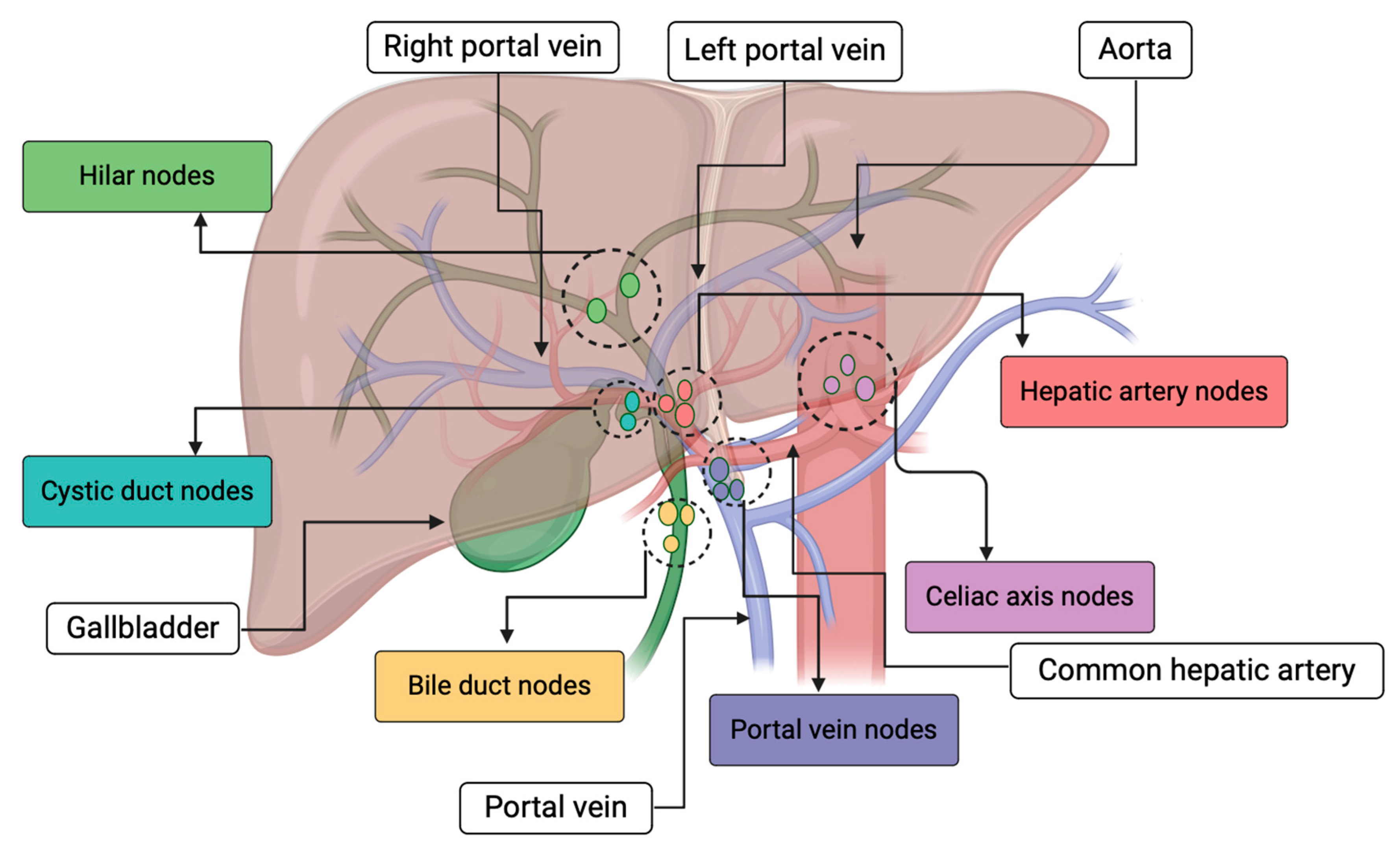
- Lymphadenectomy
3.2.2. Intrahepatic CCA
3.2.3. Peri-Hilar CCA
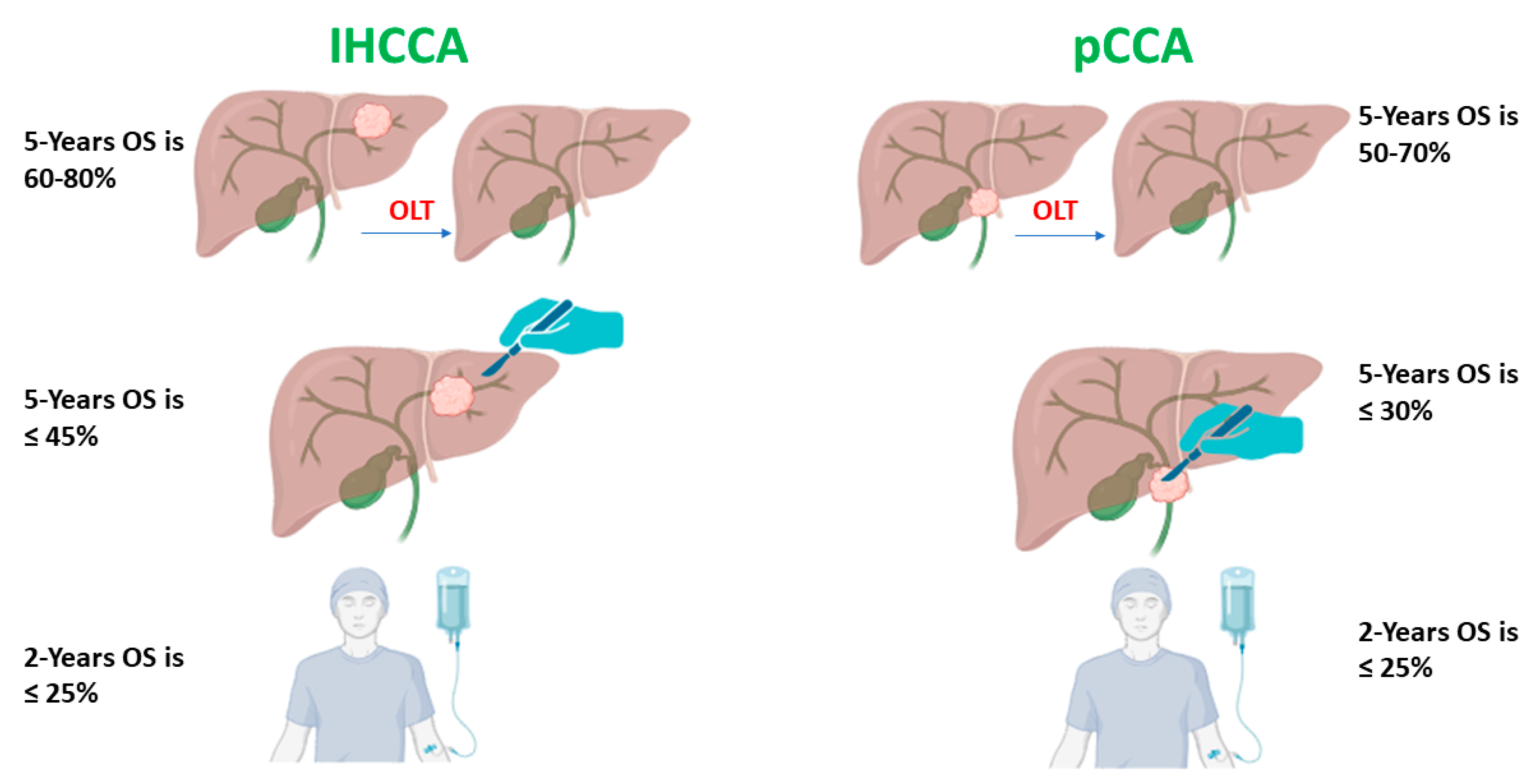
3.3. Orthotopic Liver Transplantation (OLT)
3.3.1. OLT Eligibility
3.3.2. Intrahepatic CCA
| Reference | Design | Total Patients | Treatments | 5-Year OS (%) |
|---|---|---|---|---|
| Robles et al. [150], Spain, 2004 | Retrospective, multi-center | 36 | LT | 30 |
| Sapisochin et al. [151], Spain, 2014 | Retrospective, multi-center | 27 | Neoadjuvant ethanol inj./TACE/RFA and LT | 51 |
| Sapisochin et al. [152], International, 2016 | Retrospective, multi-center | Early:15 Adv.: 33 | Neoadjuvant ethanol inj./TACE/RFA and LT | Early-65 Adv.-45 |
| Lee et al. [153], United States, 2018 | Retrospective, single center | 17 | Neoadjuvant TARE/TACE/RFA and LT | 51.9 |
| Lunsford et al. [146], United States, 2018 | Prospective, single center | 6 | Neoadjuvant chemotherapy and LT | 83.3 |
| Wong et al. [154], United States, 2019 | Prospective, single | 5 | Neoadjuvant chemotherapy and TACE and LT | 80 |
| Krasnodebski et al. [155], Poland, 2020 | Retrospective, multi-center | 8 | LT | 25 |
| Hue et al. [156], United States, 2021 | Retrospective, multi-center | 74 | Neoadjuvant chemo-radiation and LT | 33 KM |
| Abdelrahim et al. [16]. United States, 2022. | Retrospective, single center | 10 | Neoadjuvant chemotherapy and LT | 75 |
3.3.3. Peri-Hilar CCA
| Reference | Design | Total Patients | Treatments | 5-Year OS (%) |
|---|---|---|---|---|
| Robles et al., [150], Spain, 2004 | Retrospective, multi-center | 23 | LT | 42 |
| Hidalgo et al., [161], United Kingdom, 2008 | Retrospective, single center | 12 | LT | 64 |
| Darwish Murad et al., [138], United States, 2012 | Retrospective, multi-center | 287 | Neoadjuvant chemo-radiotherapy and LT | 53 KM |
| Ethun et al. [160], United States, 2018 | Retrospective, multi-center | 70 | Neoadjuvant chemo-adjuvant and LT | 64 KM |
| Azad et al. [162], United States, 2020 | Retrospective, single center | De novo: 148, PSC:228 | Neoadjuvant chemo-adjuvant and LT | De novo: 58 KM, PSC: 74 KM |
3.3.4. Limitation of OLT
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Banales, J.M.; Cardinale, V.; Carpino, G.; Marzioni, M.; Andersen, J.B.; Invernizzi, P.; Lind, G.E.; Folseraas, T.; Forbes, S.J.; Fouassier, L.; et al. Expert consensus document: Cholangiocarcinoma: Current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 261–280. [Google Scholar] [CrossRef] [PubMed]
- Bergquist, A.; von Seth, E. Epidemiology of cholangiocarcinoma. Best. Pract. Res. Clin. Gastroenterol. 2015, 29, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Qurashi, M.; Vithayathil, M.; Khan, S.A. Epidemiology of cholangiocarcinoma. Eur. J. Surg. Oncol. 2023, 9, 107064. [Google Scholar] [CrossRef] [PubMed]
- Altekruse, S.F.; Petrick, J.L.; Rolin, A.I.; Cuccinelli, J.E.; Zou, Z.; Tatalovich, Z.; McGlynn, K.A. Geographic variation of intrahepatic cholangiocarcinoma, extrahepatic cholangiocarcinoma, and hepatocellular carcinoma in the United States. PLoS ONE 2015, 10, e0120574. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Endo, I.; Gonen, M.; Yopp, A.C.; Dalal, K.M.; Zhou, Q.; Klimstra, D.; D’Angelica, M.; DeMatteo, R.P.; Fong, Y.; Schwartz, L.; et al. Intrahepatic cholangiocarcinoma: Rising frequency, improved survival, and determinants of outcome after resection. Ann. Surg. 2008, 248, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Spolverato, G.; Kim, Y.; Ejaz, A.; Alexandrescu, S.; Marques, H.; Aldrighetti, L.; Gamblin, T.C.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Conditional Probability of Long-term Survival After Liver Resection for Intrahepatic Cholangiocarcinoma: A Multi-institutional Analysis of 535 Patients. JAMA Surg. 2015, 150, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Benson, A.B., 3rd; Abrams, T.A.; Ben-Josef, E.; Bloomston, P.M.; Botha, J.F.; Clary, B.M.; Covey, A.; Curley, S.A.; D’Angelica, M.I.; Davila, R.; et al. NCCN clinical practice guidelines in oncology: Hepatobiliary cancers. J. Natl. Compr. Cancer Netw. 2009, 7, 350–391. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tabrizian, P.; Jibara, G.; Hechtman, J.F.; Franssen, B.; Labow, D.M.; Schwartz, M.E.; Thung, S.N.; Sarpel, U. Outcomes following resection of intrahepatic cholangiocarcinoma. HPB 2015, 17, 344–351. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Li, J.; Xia, Y.; Gong, R.; Wang, K.; Yan, Z.; Wan, X.; Liu, G.; Wu, D.; Shi, L.; et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J. Clin. Oncol. 2013, 31, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Hyder, O.; Hatzaras, I.; Sotiropoulos, G.C.; Paul, A.; Alexandrescu, S.; Marques, H.; Pulitano, C.; Barroso, E.; Clary, B.M.; Aldrighetti, L.; et al. Recurrence after operative management of intrahepatic cholangiocarcinoma. Surgery 2013, 153, 811–818. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aklan, H.M.; Esmail, A.; Al-Sadeq, A.A.; Eissa, G.A.; Hassan, O.A.; Al-Mikhlafy, A.A.; Al-Goshae, H.A.A. Frequency of Gallbladder Stones Among Patients Underwent Abdominal Ultrasound in a Tertiary Hospital in Sana’a City, Yemen. Malays. J. Med. Health Sci. 2020, 16, 36–39. [Google Scholar]
- Bertuccio, P.; Malvezzi, M.; Carioli, G.; Hashim, D.; Boffetta, P.; El-Serag, H.B.; La Vecchia, C.; Negri, E. Global trends in mortality from intrahepatic and extrahepatic cholangiocarcinoma. J. Hepatol. 2019, 71, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Moris, D. Surgical Management of Intrahepatic Cholangiocarcinoma: Quo Vadis. Cancers 2023, 15, 4691. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferro, V.; Regalia, E.; Doci, R.; Andreola, S.; Pulvirenti, A.; Bozzetti, F.; Montalto, F.; Ammatuna, M.; Morabito, A.; Gennari, L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N. Engl. J. Med. 1996, 334, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Abboud, K.; Umoru, G.; Esmail, A.; Abudayyeh, A.; Murakami, N.; Al-Shamsi, H.O.; Javle, M.; Saharia, A.; Connor, A.A.; Kodali, S. Immune checkpoint inhibitors for solid tumors in the adjuvant setting: Current progress, future directions, and role in transplant oncology. Cancers 2023, 15, 1433. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahim, M.; Al-Rawi, H.; Esmail, A.; Xu, J.; Umoru, G.; Ibnshamsah, F.; Abudayyeh, A.; Victor, D.; Saharia, A.; McMillan, R.; et al. Gemcitabine and Cisplatin as Neo-Adjuvant for Cholangiocarcinoma Patients Prior to Liver Transplantation: Case-Series. Curr. Oncol. 2022, 29, 3585–3594. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahim, M.; Esmail, A.; Abudayyeh, A.; Murakami, N.; Saharia, A.; McMillan, R.; Victor, D.; Kodali, S.; Shetty, A.; Nolte Fong, J.V.; et al. Transplant Oncology: An Evolving Field in Cancer Care. Cancers 2021, 13, 4911. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abdelrahim, M.; Esmail, A.; Abudayyeh, A.; Murakami, N.; Victor, D.; Kodali, S.; Cheah, Y.L.; Simon, C.J.; Noureddin, M.; Connor, A.; et al. Transplant Oncology: An Emerging Discipline of Cancer Treatment. Cancers 2023, 15, 5337. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahim, M.; Esmail, A.; Saharia, A.; Abudayyeh, A.; Abdel-Wahab, N.; Diab, A.; Murakami, N.; Kaseb, A.O.; Chang, J.C.; Gaber, A.O. Utilization of Immunotherapy for the Treatment of Hepatocellular Carcinoma in the Peri-Transplant Setting: Transplant Oncology View. Cancers 2022, 14, 1760. [Google Scholar] [CrossRef]
- Abdelrahim, M.; Esmail, A.; Umoru, G.; Westhart, K.; Abudayyeh, A.; Saharia, A.; Ghobrial, R.M. Immunotherapy as a neoadjuvant therapy for a patient with hepatocellular carcinoma in the pretransplant setting: A case report. Curr. Oncol. 2022, 29, 4267–4273. [Google Scholar] [CrossRef]
- Abdelrahim, M.; Esmail, A.; Xu, J.; Umoru, G.; Al-Rawi, H.; Saharia, A.; Abudayyeh, A.; Victor, D.; McMillan, R.; Kodali, S. Gemcitabine Plus Cisplatin Versus Non-Gemcitabine and Cisplatin Regimens as Neo-adjuvant Treatment for Cholangiocarcinoma Patients Prior to Liver Transplantation: An Institution Experience. Front. Oncol. 2022, 12, 908687. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Esmail, A.; Mazzaferro, V.; Abdelrahim, M. Newest Therapies for Cholangiocarcinoma: An Updated Overview of Approved Treatments with Transplant Oncology Vision. Cancers 2022, 14, 5074. [Google Scholar] [CrossRef] [PubMed]
- Aloia, T.A.; Charnsangavej, C.; Faria, S.; Ribero, D.; Abdalla, E.K.; Vauthey, J.N.; Curley, S.A. High-resolution computed tomography accurately predicts resectability in hilar cholangiocarcinoma. Am. J. Surg. 2007, 193, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Mansour, J.C.; Aloia, T.A.; Crane, C.H.; Heimbach, J.K.; Nagino, M.; Vauthey, J.N. Hilar cholangiocarcinoma: Expert consensus statement. HPB 2015, 17, 691–699. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anderson, C.D.; Pinson, C.W.; Berlin, J.; Chari, R.S. Diagnosis and treatment of cholangiocarcinoma. Oncologist 2004, 9, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.H.; Harnois, D.M.; Klee, G.G.; LaRusso, N.F.; Gores, G.J. The utility of CA 19-9 in the diagnoses of cholangiocarcinoma in patients without primary sclerosing cholangitis. Am. J. Gastroenterol. 2000, 95, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo-Sanchez, L.; Lamarca, A.; La Casta, A.; Buettner, S.; Utpatel, K.; Klümpen, H.J.; Adeva, J.; Vogel, A.; Lleo, A.; Fabris, L.; et al. Cholangiocarcinoma landscape in Europe: Diagnostic, prognostic and therapeutic insights from the ENSCCA Registry. J. Hepatol. 2022, 76, 1109–1121. [Google Scholar] [CrossRef] [PubMed]
- Moro, A.; Mehta, R.; Sahara, K.; Tsilimigras, D.I.; Paredes, A.Z.; Farooq, A.; Hyer, J.M.; Endo, I.; Shen, F.; Guglielmi, A.; et al. The Impact of Preoperative CA19-9 and CEA on Outcomes of Patients with Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2020, 27, 2888–2901. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.Y.; Cai, L.; He, X.D.; Liu, W.; Qu, Q. Comparison of serum tumor markers for intrahepatic cholangiocarcinoma and hepatocellular carcinoma. Am. Surg. 2010, 76, 1210–1213. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.J.; Wang, W.; Lu, M.D.; Xie, X.Y.; Xu, H.X.; Xu, Z.F.; Chen, L.D.; Wang, Z.; Liang, J.Y.; Huang, Y.; et al. Contrast-Enhanced Ultrasound for the Characterization of Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. Liver Cancer 2015, 4, 241–252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kovač, J.D.; Janković, A.; Đikić-Rom, A.; Grubor, N.; Antić, A.; Dugalić, V. Imaging Spectrum of Intrahepatic Mass-Forming Cholangiocarcinoma and Its Mimickers: How to Differentiate Them Using MRI. Curr. Oncol. 2022, 29, 698–723. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saluja, S.S.; Sharma, R.; Pal, S.; Sahni, P.; Chattopadhyay, T.K. Differentiation between benign and malignant hilar obstructions using laboratory and radiological investigations: A prospective study. HPB 2007, 9, 373–382. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Trikudanathan, G.; Navaneethan, U.; Njei, B.; Vargo, J.J.; Parsi, M.A. Diagnostic yield of bile duct brushings for cholangiocarcinoma in primary sclerosing cholangitis: A systematic review and meta-analysis. Gastrointest. Endosc. 2014, 79, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Fritcher, E.G.B.; Voss, J.S.; Brankley, S.M.; Campion, M.B.; Jenkins, S.M.; Keeney, M.E.; Henry, M.R.; Kerr, S.M.; Chaiteerakij, R.; Pestova, E.V.; et al. An Optimized Set of Fluorescence In Situ Hybridization Probes for Detection of Pancreatobiliary Tract Cancer in Cytology Brush Samples. Gastroenterology 2015, 149, 1813–1824.e1. [Google Scholar] [CrossRef]
- Larribère, L.; Martens, U.M. Advantages and Challenges of Using ctDNA NGS to Assess the Presence of Minimal Residual Disease (MRD) in Solid Tumors. Cancers 2021, 13, 5698. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, C.; Wang, T.; Yang, M.; Song, J.; Huang, M.; Bai, Y.; Su, H. Genomic Profiling of Blood-Derived Circulating Tumor DNA from Patients with Advanced Biliary Tract Cancer. Pathol. Oncol. Res. 2021, 27, 1609879. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Csoma, S.L.; Bedekovics, J.; Veres, G.; Árokszállási, A.; András, C.; Méhes, G.; Mokánszki, A. Circulating Cell-Free DNA-Based Comprehensive Molecular Analysis of Biliary Tract Cancers Using Next-Generation Sequencing. Cancers 2022, 14, 233. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pellino, A.; Loupakis, F.; Cadamuro, M.; Dadduzio, V.; Fassan, M.; Guido, M.; Cillo, U.; Indraccolo, S.; Fabris, L. Precision medicine in cholangiocarcinoma. Transl. Gastroenterol. Hepatol. 2018, 3, 40. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hann, L.E.; Greatrex, K.V.; Bach, A.M.; Fong, Y.; Blumgart, L.H. Cholangiocarcinoma at the hepatic hilus: Sonographic findings. AJR Am. J. Roentgenol. 1997, 168, 985–989. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.J.; Heimbach, J.K.; Gores, G.J. Endoscopic ultrasound staging of cholangiocarcinoma. Curr. Opin. Gastroenterol. 2012, 28, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.S.; Park, M.S.; Yu, J.S.; Kim, M.J.; Kim, K.W. Biliary ductal involvement of hilar cholangiocarcinoma: Multidetector computed tomography versus magnetic resonance cholangiography. J. Comput. Assist. Tomogr. 2007, 31, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Nagino, M. Perihilar cholangiocarcinoma: A surgeon’s viewpoint on current topics. J. Gastroenterol. 2012, 47, 1165–1176. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhu, J.; Ke, F.; Weng, M.; Wu, X.; Li, M.; Quan, Z.; Liu, Y.; Zhang, Y.; Gong, W. Radiological Imaging for Assessing the Respectability of Hilar Cholangiocarcinoma: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2015, 2015, 497942. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jhaveri, K.S.; Hosseini-Nik, H. MRI of cholangiocarcinoma. J. Magn. Reson. Imaging 2015, 42, 1165–1179. [Google Scholar] [CrossRef] [PubMed]
- Ayuso, J.R.; Pagés, M.; Darnell, A. Imaging bile duct tumors: Staging. Abdom. Imaging 2013, 38, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Ringe, K.I.; Wacker, F. Radiological diagnosis in cholangiocarcinoma: Application of computed tomography, magnetic resonance imaging, and positron emission tomography. Best. Pract. Res. Clin. Gastroenterol. 2015, 29, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, E.; Schoen, R.E.; Silverman, W.; Martin, J.; Rabinovitz, M.; Weissfeld, J.L.; Abu-Elmaagd, K.; Madariaga, J.R.; Slivka, A. Detecting cholangiocarcinoma in patients with primary sclerosing cholangitis. Gastrointest. Endosc. 2002, 56, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Boberg, K.M.; Jebsen, P.; Clausen, O.P.; Foss, A.; Aabakken, L.; Schrumpf, E. Diagnostic benefit of biliary brush cytology in cholangiocarcinoma in primary sclerosing cholangitis. J. Hepatol. 2006, 45, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, M.J.; Lee, J.M.; Kim, K.W.; Lee, J.Y.; Han, J.K.; Choi, B.I. Hilar cholangiocarcinoma: Role of preoperative imaging with sonography, MDCT, MRI, and direct cholangiography. AJR Am. J. Roentgenol. 2008, 191, 1448–1457. [Google Scholar] [CrossRef] [PubMed]
- Varadarajulu, S.; Bang, J.Y.; Hasan, M.K.; Navaneethan, U.; Hawes, R.; Hebert-Magee, S. Improving the diagnostic yield of single-operator cholangioscopy-guided biopsy of indeterminate biliary strictures: ROSE to the rescue?(with video). Gastrointest. Endosc. 2016, 84, 681–687. [Google Scholar] [CrossRef] [PubMed]
- De Moura, D.T.H.; De Moura, E.G.H.; Bernardo, W.M.; De Moura, E.T.H.; Baracat, F.I.; Kondo, A.; Matuguma, S.E.; Artifon, E.L.A. Endoscopic retrograde cholangiopancreatography versus endoscopic ultrasound for tissue diagnosis of malignant biliary stricture: Systematic review and meta-analysis. Endosc. Ultrasound 2018, 7, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Mohamadnejad, M.; DeWitt, J.M.; Sherman, S.; LeBlanc, J.K.; Pitt, H.A.; House, M.G.; Jones, K.J.; Fogel, E.L.; McHenry, L.; Watkins, J.L. Role of EUS for preoperative evaluation of cholangiocarcinoma: A large single-center experience. Gastrointest. Endosc. 2011, 73, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Rösch, T.; Hofrichter, K.; Frimberger, E.; Meining, A.; Born, P.; Weigert, N.; Allescher, H.-D.; Classen, M.; Barbur, M.; Schenck, U. ERCP or EUS for tissue diagnosis of biliary strictures? A prospective comparative study. Gastrointest. Endosc. 2004, 60, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Sanchez, W.; Rosen, C.B.; Gores, G.J. Trans-peritoneal fine needle aspiration biopsy of hilar cholangiocarcinoma is associated with disease dissemination. HPB 2011, 13, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Sequeiros, E.; Baron, T.H.; Clain, J.E.; Gostout, C.J.; Norton, I.D.; Petersen, B.T.; Levy, M.J.; Jondal, M.L.; Wiersema, M.J. Evaluation of indeterminate bile duct strictures by intraductal US. Gastrointest. Endosc. 2002, 56, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Mi, J.; Han, X.; Wang, R.; Ma, R.; Zhao, D. Diagnostic accuracy of probe-based confocal laser endomicroscopy and tissue sampling by endoscopic retrograde cholangiopancreatography in indeterminate biliary strictures: A meta-analysis. Sci. Rep. 2022, 12, 7257. [Google Scholar] [CrossRef] [PubMed]
- Taunk, P.; Singh, S.; Lichtenstein, D.; Joshi, V.; Gold, J.; Sharma, A. Improved classification of indeterminate biliary strictures by probe-based confocal laser endomicroscopy using the Paris Criteria following biliary stenting. J. Gastroenterol. Hepatol. 2017, 32, 1778–1783. [Google Scholar] [CrossRef]
- Moris, D.; Palta, M.; Kim, C.; Allen, P.J.; Morse, M.A.; Lidsky, M.E. Advances in the treatment of intrahepatic cholangiocarcinoma: An overview of the current and future therapeutic landscape for clinicians. CA Cancer J. Clin. 2023, 73, 198–222. [Google Scholar] [CrossRef] [PubMed]
- D’Angelica, M.; Fong, Y.; Weber, S.; Gonen, M.; DeMatteo, R.P.; Conlon, K.; Blumgart, L.H.; Jarnagin, W.R. The role of staging laparoscopy in hepatobiliary malignancy: Prospective analysis of 401 cases. Ann. Surg. Oncol. 2003, 10, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Goere, D.; Wagholikar, G.D.; Pessaux, P.; Carrère, N.; Sibert, A.; Vilgrain, V.; Sauvanet, A.; Belghiti, J. Utility of staging laparoscopy in subsets of biliary cancers. Surg. Endosc. Other Interv. Tech. 2006, 20, 721–725. [Google Scholar] [CrossRef]
- Laurent, A.; Tayar, C.; Cherqui, D. Cholangiocarcinoma: Preoperative biliary drainage (Con). HPB 2008, 10, 126–129. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nimura, Y. Preoperative biliary drainage before resection for cholangiocarcinoma (Pro). HPB 2008, 10, 130–133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Walter, T.; Ho, C.S.; Horgan, A.M.; Warkentin, A.; Gallinger, S.; Greig, P.D.; Kortan, P.; Knox, J.J. Endoscopic or percutaneous biliary drainage for Klatskin tumors? J. Vasc. Interv. Radiol. JVIR 2013, 24, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Kloek, J.J.; van der Gaag, N.A.; Aziz, Y.; Rauws, E.A.; van Delden, O.M.; Lameris, J.S.; Busch, O.R.; Gouma, D.J.; van Gulik, T.M. Endoscopic and percutaneous preoperative biliary drainage in patients with suspected hilar cholangiocarcinoma. J. Gastrointest. Surg. 2010, 14, 119–125. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, K.M.; Park, J.W.; Lee, J.K.; Lee, K.H.; Lee, K.T.; Shim, S.G. A Comparison of Preoperative Biliary Drainage Methods for Perihilar Cholangiocarcinoma: Endoscopic versus Percutaneous Transhepatic Biliary Drainage. Gut Liver 2015, 9, 791–799. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maguchi, H.; Takahashi, K.; Katanuma, A.; Osanai, M.; Nakahara, K.; Matuzaki, S.; Urata, T.; Iwano, H. Preoperative biliary drainage for hilar cholangiocarcinoma. J. Hepatobiliary Pancreat. Surg. 2007, 14, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, T.J.; Yopp, A.; Qin, Y.; Zhao, B.; Guo, P.; Liu, F.; Schwartz, L.H.; Allen, P.; D’Angelica, M.; Fong, Y.; et al. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB 2009, 11, 445–451. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, F.; Li, Y.; Wei, Y.; Li, B. Preoperative biliary drainage before resection for hilar cholangiocarcinoma: Whether or not? A systematic review. Dig. Dis. Sci. 2011, 56, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Ribero, D.; Zimmitti, G.; Aloia, T.A.; Shindoh, J.; Fabio, F.; Amisano, M.; Passot, G.; Ferrero, A.; Vauthey, J.N. Preoperative Cholangitis and Future Liver Remnant Volume Determine the Risk of Liver Failure in Patients Undergoing Resection for Hilar Cholangiocarcinoma. J. Am. Coll. Surg. 2016, 223, 87–97. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Paik, W.H.; Loganathan, N.; Hwang, J.H. Preoperative biliary drainage in hilar cholangiocarcinoma: When and how? World J. Gastrointest. Endosc. 2014, 6, 68–73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Madoff, D.C.; Hicks, M.E.; Abdalla, E.K.; Morris, J.S.; Vauthey, J.N. Portal vein embolization with polyvinyl alcohol particles and coils in preparation for major liver resection for hepatobiliary malignancy: Safety and effectiveness—Study in 26 patients. Radiology 2003, 227, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Hemming, A.W.; Reed, A.I.; Howard, R.J.; Fujita, S.; Hochwald, S.N.; Caridi, J.G.; Hawkins, I.F.; Vauthey, J.N. Preoperative portal vein embolization for extended hepatectomy. Ann. Surg. 2003, 237, 686–691. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nagino, M.; Kamiya, J.; Nishio, H.; Ebata, T.; Arai, T.; Nimura, Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: Surgical outcome and long-term follow-up. Ann. Surg. 2006, 243, 364–372. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Franken, L.C.; Rassam, F.; van Lienden, K.P.; Bennink, R.J.; Besselink, M.G.; Busch, O.R.; Erdmann, J.I.; van Gulik, T.M.; Olthof, P.B. Effect of structured use of preoperative portal vein embolization on outcomes after liver resection of perihilar cholangiocarcinoma. BJS Open 2020, 4, 449–455. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- van Lienden, K.P.; van den Esschert, J.W.; de Graaf, W.; Bipat, S.; Lameris, J.S.; van Gulik, T.M.; van Delden, O.M. Portal vein embolization before liver resection: A systematic review. Cardiovasc. Interv. Radiol. 2013, 36, 25–34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nathan, H.; Pawlik, T.M.; Wolfgang, C.L.; Choti, M.A.; Cameron, J.L.; Schulick, R.D. Trends in survival after surgery for cholangiocarcinoma: A 30-year population-based SEER database analysis. J. Gastrointest. Surg. 2007, 11, 1488–1496. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.K.; Davidson, B.R.; Manas, D.M. Surgical management, including the role of transplantation, for intrahepatic and peri-hilar cholangiocarcinoma. Eur. J. Surg. Oncol. 2024, 108248. [Google Scholar] [CrossRef] [PubMed]
- Brolese, A.; Rigoni, M.; Pasquale, A.; Viel, G.; Brolese, M.; Ciarleglio, F.A. The role of robotic surgery for the treatment of hilar cholangiocarcinoma: A systematic review. Front. Oncol. 2022, 12, 1001838. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Turgeon, M.K.; Maithel, S.K. Cholangiocarcinoma: A site-specific update on the current state of surgical management and multi-modality therapy. Chin. Clin. Oncol. 2020, 9, 4. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cherqui, D.; Tantawi, B.; Alon, R.; Piedbois, P.; Rahmouni, A.; Dhumeaux, D.; Julien, M.; Fagniez, P.L. Intrahepatic cholangiocarcinoma. Results of aggressive surgical management. Arch. Surg. 1995, 130, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- Angelico, R.; Sensi, B.; Parente, A.; Siragusa, L.; Gazia, C.; Tisone, G.; Manzia, T.M. Vascular Involvements in Cholangiocarcinoma: Tips and Tricks. Cancers 2021, 13, 3735. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beal, E.W.; Cloyd, J.M.; Pawlik, T.M. Surgical Treatment of Intrahepatic Cholangiocarcinoma: Current and Emerging Principles. J. Clin. Med. 2020, 10, 104. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khan, S.A.; Davidson, B.R.; Goldin, R.D.; Heaton, N.; Karani, J.; Pereira, S.P.; Rosenberg, W.M.; Tait, P.; Taylor-Robinson, S.D.; Thillainayagam, A.V.; et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: An update. Gut 2012, 61, 1657–1669. [Google Scholar] [CrossRef] [PubMed]
- Zaydfudim, V.M.; Rosen, C.B.; Nagorney, D.M. Hilar cholangiocarcinoma. Surg. Oncol. Clin. N. Am. 2014, 23, 247–263. [Google Scholar] [CrossRef] [PubMed]
- NCCN. NCCN Practice Guidelines in Oncology. Hepatobiliary Cancers; NCCN: Plymouth Meeting, PA, USA, 2020. [Google Scholar]
- Schulick, R.D. Criteria of unresectability and the decision-making process. HPB 2008, 10, 122–125. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Tsao, J.I.; Nimura, Y.; Kamiya, J.; Hayakawa, N.; Kondo, S.; Nagino, M.; Miyachi, M.; Kanai, M.; Uesaka, K.; Oda, K.; et al. Management of hilar cholangiocarcinoma: Comparison of an American and a Japanese experience. Ann. Surg. 2000, 232, 166–174. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rajagopalan, V.; Daines, W.P.; Grossbard, M.L.; Kozuch, P. Gallbladder and biliary tract carcinoma: A comprehensive update, Part 1. Oncology 2004, 18, 889–896. [Google Scholar] [PubMed]
- Hemming, A.W.; Reed, A.I.; Fujita, S.; Foley, D.P.; Howard, R.J. Surgical management of hilar cholangiocarcinoma. Ann. Surg. 2005, 241, 693–699. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ebata, T.; Nagino, M.; Kamiya, J.; Uesaka, K.; Nagasaka, T.; Nimura, Y. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: Audit of 52 consecutive cases. Ann. Surg. 2003, 238, 720–727. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weber, S.M.; Ribero, D.; O’Reilly, E.M.; Kokudo, N.; Miyazaki, M.; Pawlik, T.M. Intrahepatic cholangiocarcinoma: Expert consensus statement. HPB 2015, 17, 669–680. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rassam, F.; Olthof, P.B.; van Lienden, K.P.; Bennink, R.J.; Erdmann, J.I.; Swijnenburg, R.J.; Busch, O.R.; Besselink, M.G.; van Gulik, T.M. Comparison of functional and volumetric increase of the future remnant liver and postoperative outcomes after portal vein embolization and complete or partial associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Ann. Transl. Med. 2020, 8, 436. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, M.; Wang, J.; Song, J.; Shen, F.; Song, L.; Ni, X.; Suo, T.; Liu, H.; Zhong, M.; Liu, H. Preoperative ICG Test to Predict Posthepatectomy Liver Failure and Postoperative Outcomes in Hilar Cholangiocarcinoma. BioMed Res. Int. 2021, 2021, 8298737. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pan, Y.J.; Wu, S.J.; Zeng, Y.; Cao, Z.R.; Shan, Y.; Lin, J.; Xu, P.J. Intra-and Peri-tumoral Radiomics Based on Dynamic Contrast Enhanced-MRI to Identify Lymph Node Metastasis and Prognosis in Intrahepatic Cholangiocarcinoma. J. Magn. Reson. Imaging 2024. [Google Scholar] [CrossRef] [PubMed]
- Lluís, N.; Asbun, D.; Wang, J.J.; Cao, H.S.T.; Jimenez, R.E.; Alseidi, A.; Asbun, H. Lymph Node Dissection in Intrahepatic Cholangiocarcinoma: A Critical and Updated Review of the Literature. J. Gastrointest. Surg. 2023, 27, 3001–3013. [Google Scholar] [CrossRef] [PubMed]
- Sposito, C.; Droz Dit Busset, M.; Virdis, M.; Citterio, D.; Flores, M.; Bongini, M.; Niger, M.; Mazzaferro, V. The role of lymphadenectomy in the surgical treatment of intrahepatic cholangiocarcinoma: A review. Eur. J. Surg. Oncol. 2022, 48, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Kizy, S.; Altman, A.M.; Marmor, S.; Wirth, K.; Ching Hui, J.Y.; Tuttle, T.M.; Denbo, J.W.; Jensen, E.H. Surgical resection of lymph node positive intrahepatic cholangiocarcinoma may not improve survival. HPB 2019, 21, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Sposito, C.; Ratti, F.; Cucchetti, A.; Ardito, F.; Ruzzenente, A.; Di Sandro, S.; Maspero, M.; Ercolani, G.; Di Benedetto, F.; Guglielmi, A.; et al. Survival benefit of adequate lymphadenectomy in patients undergoing liver resection for clinically node-negative intrahepatic cholangiocarcinoma. J. Hepatol. 2023, 78, 356–363. [Google Scholar] [CrossRef] [PubMed]
- NCCN Guidelines Version: Hepatobiliary Cancers. Available online: https://www.nccn.org/professionals/physician_gls/pdf/btc.pdf (accessed on 17 May 2024).
- Cloyd, J.M.; Ejaz, A.; Pawlik, T.M. The Landmark Series: Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2020, 27, 2859–2865. [Google Scholar] [CrossRef] [PubMed]
- Gavriilidis, P.; Bath, N.M.; Pawlik, T.M. The impact of lymphadenectomy on intrahepatic cholangiocarcinoma management and prognosis: A comprehensive review. Hepatoma Res. 2023, 9, 24. [Google Scholar] [CrossRef]
- Barlow, A.D.; Garcea, G.; Berry, D.P.; Rajesh, A.; Patel, R.; Metcalfe, M.S.; Dennison, A.R. Staging laparoscopy for hilar cholangiocarcinoma in 100 patients. Langenbecks Arch. Surg. 2013, 398, 983–988. [Google Scholar] [CrossRef] [PubMed]
- Bird, N.; Elmasry, M.; Jones, R.; Elniel, M.; Kelly, M.; Palmer, D.; Fenwick, S.; Poston, G.; Malik, H. Role of staging laparoscopy in the stratification of patients with perihilar cholangiocarcinoma. Br. J. Surg. 2017, 104, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Dodson, R.M.; Weiss, M.J.; Cosgrove, D.; Herman, J.M.; Kamel, I.; Anders, R.; Geschwind, J.F.; Pawlik, T.M. Intrahepatic cholangiocarcinoma: Management options and emerging therapies. J. Am. Coll. Surg. 2013, 217, 736–750.e4. [Google Scholar] [CrossRef] [PubMed]
- Ribero, D.; Pinna, A.D.; Guglielmi, A.; Ponti, A.; Nuzzo, G.; Giulini, S.M.; Aldrighetti, L.; Calise, F.; Gerunda, G.E.; Tomatis, M.; et al. Surgical Approach for Long-term Survival of Patients with Intrahepatic Cholangiocarcinoma: A Multi-institutional Analysis of 434 Patients. Arch. Surg. 2012, 147, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Murakami, Y.; Uemura, K.; Sudo, T.; Hashimoto, Y.; Nakashima, A.; Kondo, N.; Sakabe, R.; Ohge, H.; Sueda, T. Prognostic factors after surgical resection for intrahepatic, hilar, and distal cholangiocarcinoma. Ann. Surg. Oncol. 2011, 18, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Farges, O.; Fuks, D.; Boleslawski, E.; Le Treut, Y.P.; Castaing, D.; Laurent, A.; Ducerf, C.; Rivoire, M.; Bachellier, P.; Chiche, L.; et al. Influence of surgical margins on outcome in patients with intrahepatic cholangiocarcinoma: A multicenter study by the AFC-IHCC-2009 study group. Ann. Surg. 2011, 254, 824–829. [Google Scholar] [CrossRef] [PubMed]
- Tamandl, D.; Herberger, B.; Gruenberger, B.; Puhalla, H.; Klinger, M.; Gruenberger, T. Influence of hepatic resection margin on recurrence and survival in intrahepatic cholangiocarcinoma. Ann. Surg. Oncol. 2008, 15, 2787–2794. [Google Scholar] [CrossRef] [PubMed]
- Lang, H.; Sotiropoulos, G.C.; Sgourakis, G.; Schmitz, K.J.; Paul, A.; Hilgard, P.; Zöpf, T.; Trarbach, T.; Malagó, M.; Baba, H.A.; et al. Operations for intrahepatic cholangiocarcinoma: Single-institution experience of 158 patients. J. Am. Coll. Surg. 2009, 208, 218–228. [Google Scholar] [CrossRef] [PubMed]
- Spolverato, G.; Kim, Y.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; Clark Gamblin, T.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; et al. Management and Outcomes of Patients with Recurrent Intrahepatic Cholangiocarcinoma Following Previous Curative-Intent Surgical Resection. Ann. Surg. Oncol. 2016, 23, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, F.; Paschold, M.; Baumgart, J.; Hoppe-Lotichius, M.; Heinrich, S.; Lang, H. Surgical Resection for Recurrent Intrahepatic Cholangiocarcinoma. World J. Surg. 2019, 43, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- Bridgewater, J.; Galle, P.R.; Khan, S.A.; Llovet, J.M.; Park, J.W.; Patel, T.; Pawlik, T.M.; Gores, G.J. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J. Hepatol. 2014, 60, 1268–1289. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, F.; Eberhard, J.; Rückert, F.; Schmelzle, M.; Lehwald-Tywuschik, N.; Fichtner-Feigl, S.; Gaedcke, J.; Oldhafer, K.J.; Oldhafer, F.; Diener, M.; et al. Repeated resection for recurrent intrahepatic cholangiocarcinoma: A retrospective German multicentre study. Liver Int. 2021, 41, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Tsilimigras, D.I.; Sahara, K.; Wu, L.; Moris, D.; Bagante, F.; Guglielmi, A.; Aldrighetti, L.; Weiss, M.; Bauer, T.W.; Alexandrescu, S.; et al. Very Early Recurrence After Liver Resection for Intrahepatic Cholangiocarcinoma: Considering Alternative Treatment Approaches. JAMA Surg. 2020, 155, 823–831. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hu, L.S.; Zhang, X.F.; Weiss, M.; Popescu, I.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Recurrence Patterns and Timing Courses Following Curative-Intent Resection for Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2019, 26, 2549–2557. [Google Scholar] [CrossRef] [PubMed]
- Yoh, T.; Hatano, E.; Seo, S.; Okuda, Y.; Fuji, H.; Ikeno, Y.; Taura, K.; Yasuchika, K.; Okajima, H.; Kaido, T.; et al. Long-Term Survival of Recurrent Intrahepatic Cholangiocarcinoma: The Impact and Selection of Repeat Surgery. World J. Surg. 2018, 42, 1848–1856. [Google Scholar] [CrossRef] [PubMed]
- Reames, B.N.; Ejaz, A.; Koerkamp, B.G.; Alexandrescu, S.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Impact of major vascular resection on outcomes and survival in patients with intrahepatic cholangiocarcinoma: A multi-institutional analysis. J. Surg. Oncol. 2017, 116, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Li, W.W.; Chen, J.H.; Cui, M.H.; Liu, J.L. The value of caudate lobectomy in hilar cholangiocarcinoma treatment: A meta-analysis. Medicine 2021, 100, e24727. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nimura, Y.; Kamiya, J.; Nagino, M.; Kanai, M.; Uesaka, K.; Kondo, S.; Hayakawa, N. Aggressive surgical treatment of hilar cholangiocarcinoma. J. Hepatobiliary Pancreat. Surg. 1998, 5, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, M.; Ito, H.; Nakagawa, K.; Ambiru, S.; Shimizu, H.; Shimizu, Y.; Kato, A.; Nakamura, S.; Omoto, H.; Nakajima, N.; et al. Aggressive surgical approaches to hilar cholangiocarcinoma: Hepatic or local resection? Surgery 1998, 123, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Choi, G.H.; Choi, S.H.; Kim, K.S.; Choi, J.S.; Lee, W.J. Liver resection for Bismuth type I and Type II hilar cholangiocarcinoma. World J. Surg. 2013, 37, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.W.; Hu, B.S.; Chu, Y.J.; Tan, Y.C.; Ji, X.; Chen, K.; Ding, X.M.; Zhang, A.; Chen, F.; Dong, J.H. One-stage resection for Bismuth type IV hilar cholangiocarcinoma with high hilar resection and parenchyma-preserving strategies: A cohort study. World J. Surg. 2013, 37, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, I.; Shimizu, H.; Yoshidome, H.; Ohtsuka, M.; Kato, A.; Yoshitomi, H.; Miyazaki, M. Surgical strategy for hilar cholangiocarcinoma of the left-side predominance: Current role of left trisectionectomy. Ann. Surg. 2014, 259, 1178–1185. [Google Scholar] [CrossRef] [PubMed]
- Esaki, M.; Shimada, K.; Nara, S.; Kishi, Y.; Sakamoto, Y.; Kosuge, T.; Sano, T. Left hepatic trisectionectomy for advanced perihilar cholangiocarcinoma. Br. J. Surg. 2013, 100, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Neuhaus, P.; Thelen, A.; Jonas, S.; Puhl, G.; Denecke, T.; Veltzke-Schlieker, W.; Seehofer, D. Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann. Surg. Oncol. 2012, 19, 1602–1608. [Google Scholar] [CrossRef] [PubMed]
- Neuhaus, P.; Jonas, S.; Bechstein, W.O.; Lohmann, R.; Radke, C.; Kling, N.; Wex, C.; Lobeck, H.; Hintze, R. Extended resections for hilar cholangiocarcinoma. Ann. Surg. 1999, 230, 808–818; discussion 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, Y.; Zhang, Z.; Wu, L.; Li, B. A systematic review of safety and efficacy of hepatopancreatoduodenectomy for biliary and gallbladder cancers. HPB 2016, 18, 1–6. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cillo, U.; Fondevila, C.; Donadon, M.; Gringeri, E.; Mocchegiani, F.; Schlitt, H.J.; Ijzermans, J.N.M.; Vivarelli, M.; Zieniewicz, K.; Olde Damink, S.W.M.; et al. Surgery for cholangiocarcinoma. Liver Int. 2019, 39 (Suppl. S1), 143–155. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.G.; Penn, I.; James, L. Liver transplantation for cholangiocarcinoma: Results in 207 patients. Transplantation 2000, 69, 1633–1637. [Google Scholar] [CrossRef] [PubMed]
- DeOliveira, M.L. Liver transplantation for cholangiocarcinoma: Current best practice. Curr. Opin. Organ. Transpl. 2014, 19, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Gores, G.J.; Haddock, M.G.; Alberts, S.R.; Nyberg, S.L.; Ishitani, M.B.; Rosen, C.B. Liver transplantation for unresectable perihilar cholangiocarcinoma. Semin. Liver Dis. 2004, 24, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Gores, G.J.; Haddock, M.G.; Alberts, S.R.; Pedersen, R.; Kremers, W.; Nyberg, S.L.; Ishitani, M.B.; Rosen, C.B. Predictors of disease recurrence following neoadjuvant chemoradiotherapy and liver transplantation for unresectable perihilar cholangiocarcinoma. Transplantation 2006, 82, 1703–1707. [Google Scholar] [CrossRef] [PubMed]
- Rosen, C.B.; Darwish Murad, S.; Heimbach, J.K.; Nyberg, S.L.; Nagorney, D.M.; Gores, G.J. Neoadjuvant therapy and liver transplantation for hilar cholangiocarcinoma: Is pretreatment pathological confirmation of diagnosis necessary? J. Am. Coll Surg. 2012, 215, 31–38; discussion 38–40. [Google Scholar] [CrossRef] [PubMed]
- Darwish Murad, S.; Kim, W.R.; Therneau, T.; Gores, G.J.; Rosen, C.B.; Martenson, J.A.; Alberts, S.R.; Heimbach, J.K. Predictors of pretransplant dropout and posttransplant recurrence in patients with perihilar cholangiocarcinoma. Hepatology 2012, 56, 972–981. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tan, E.K.; Taner, T.; Heimbach, J.K.; Gores, G.J.; Rosen, C.B. Liver Transplantation for Peri-hilar Cholangiocarcinoma. J. Gastrointest. Surg. 2020, 24, 2679–2685. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahim, M.; Esmail, A.; Xu, J.; Umoru, G.; Al-Rawi, H.; Saharia, A. P-168 Combination of gemcitabine plus cisplatin compared to non-gemcitabine and cisplatin regimens as neo-adjuvant treatment in liver transplant recipients with cholangiocarcinoma. Ann. Oncol. 2022, 33, S309–S410. [Google Scholar] [CrossRef]
- Esmail, A.; Xu, J.; Umoru, G.; Al-Rawi, H.; Saharia, A.; Abdelrahim, M. P-169 Feasibility of gemcitabine plus cisplatin as neo-adjuvant in cholangiocarcinoma patients prior to liver transplantation. Ann. Oncol. 2022, 33, S310. [Google Scholar] [CrossRef]
- Murad, S.D.; Kim, W.R.; Harnois, D.M.; Douglas, D.D.; Burton, J.; Kulik, L.M.; Botha, J.F.; Mezrich, J.D.; Chapman, W.C.; Schwartz, J.J. Efficacy of neoadjuvant chemoradiation, followed by liver transplantation, for perihilar cholangiocarcinoma at 12 US centers. Gastroenterology 2012, 143, 88–98.e3; quiz e14. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rea, D.J.; Heimbach, J.K.; Rosen, C.B.; Haddock, M.G.; Alberts, S.R.; Kremers, W.K.; Gores, G.J.; Nagorney, D.M. Liver transplantation with neoadjuvant chemoradiation is more effective than resection for hilar cholangiocarcinoma. Ann. Surg. 2005, 242, 451–458; discussion 458–461. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liver/Intestine, U.N.f.O.S. News. Submitting Standardized MELD/PELD Exception Scores. 2010. Available online: https://unos.org/news/submitting-standardized-meldpeld-exception-scores/ (accessed on 15 October 2022).
- Grendar, J.; Grendarova, P.; Sinha, R.; Dixon, E. Neoadjuvant therapy for downstaging of locally advanced hilar cholangiocarcinoma: A systematic review. HPB 2014, 16, 297–303. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- O’Grady, J.G.; Polson, R.J.; Rolles, K.; Calne, R.Y.; Williams, R. Liver transplantation for malignant disease. Results in 93 consecutive patients. Ann. Surg. 1988, 207, 373–379. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pichlmayr, R.; Weimann, A.; Oldhafer, K.J.; Schlitt, H.J.; Klempnauer, J.; Bornscheuer, A.; Chavan, A.; Schmoll, E.; Lang, H.; Tusch, G.; et al. Role of liver transplantation in the treatment of unresectable liver cancer. World J. Surg. 1995, 19, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Sapisochin, G.; de Sevilla, E.F.; Echeverri, J.; Charco, R. Management of “very early” hepatocellular carcinoma on cirrhotic patients. World J. Hepatol. 2014, 6, 766–775. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Sapisochin, G.; Rodríguez de Lope, C.; Gastaca, M.; Ortiz de Urbina, J.; Suarez, M.A.; Santoyo, J.; Castroagudín, J.F.; Varo, E.; López-Andujar, R.; Palacios, F.; et al. “Very early” intrahepatic cholangiocarcinoma in cirrhotic patients: Should liver transplantation be reconsidered in these patients? Am. J. Transpl. 2014, 14, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Lunsford, K.E.; Javle, M.; Heyne, K.; Shroff, R.T.; Abdel-Wahab, R.; Gupta, N.; Mobley, C.M.; Saharia, A.; Victor, D.W.; Nguyen, D.T.; et al. Liver transplantation for locally advanced intrahepatic cholangiocarcinoma treated with neoadjuvant therapy: A prospective case-series. Lancet Gastroenterol. Hepatol. 2018, 3, 337–348. [Google Scholar] [CrossRef] [PubMed]
- McMillan, R.R.; Javle, M.; Kodali, S.; Saharia, A.; Mobley, C.; Heyne, K.; Hobeika, M.J.; Lunsford, K.E.; Victor, D.W., 3rd; Shetty, A.; et al. Survival following liver transplantation for locally advanced, unresectable intrahepatic cholangiocarcinoma. Am. J. Transpl. 2022, 22, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Kuriyama, N.; Usui, M.; Gyoten, K.; Hayasaki, A.; Fujii, T.; Iizawa, Y.; Kato, H.; Murata, Y.; Tanemura, A.; Kishiwada, M.; et al. Neoadjuvant chemotherapy followed by curative-intent surgery for perihilar cholangiocarcinoma based on its anatomical resectability classification and lymph node status. BMC Cancer 2020, 20, 405. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cho, S.M.; Esmail, A.; Raza, A.; Dacha, S.; Abdelrahim, M. Timeline of FDA-approved targeted therapy for cholangiocarcinoma. Cancers 2022, 14, 2641. [Google Scholar] [CrossRef] [PubMed]
- Robles, R.; Figueras, J.; Turrión, V.S.; Margarit, C.; Moya, A.; Varo, E.; Calleja, J.; Valdivieso, A.; Valdecasas, J.C.; López, P.; et al. Spanish experience in liver transplantation for hilar and peripheral cholangiocarcinoma. Ann. Surg. 2004, 239, 265–271. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sapisochin, G.; de Lope, C.R.; Gastaca, M.; de Urbina, J.O.; López-Andujar, R.; Palacios, F.; Ramos, E.; Fabregat, J.; Castroagudín, J.F.; Varo, E.; et al. Intrahepatic cholangiocarcinoma or mixed hepatocellular-cholangiocarcinoma in patients undergoing liver transplantation: A Spanish matched cohort multicenter study. Ann. Surg. 2014, 259, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Sapisochin, G.; Facciuto, M.; Rubbia-Brandt, L.; Marti, J.; Mehta, N.; Yao, F.Y.; Vibert, E.; Cherqui, D.; Grant, D.R.; Hernandez-Alejandro, R.; et al. Liver transplantation for “very early” intrahepatic cholangiocarcinoma: International retrospective study supporting a prospective assessment. Hepatology 2016, 64, 1178–1188. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.D.; Croome, K.P.; Musto, K.R.; Melendez, J.; Tranesh, G.; Nakhleh, R.; Taner, C.B.; Nguyen, J.H.; Patel, T.; Harnois, D.M. Liver transplantation for intrahepatic cholangiocarcinoma. Liver Transpl. 2018, 24, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.; Kim, J.; George, B.; Eriksen, C.; Pearson, T.; Robbins, J.; Zimmerman, M.A.; Hong, J.C. Downstaging Locally Advanced Cholangiocarcinoma Pre-Liver Transplantation: A Prospective Pilot Study. J. Surg. Res. 2019, 242, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Krasnodębski, M.; Grąt, M.; Jastrzębski, M.; Szczęśniak, M.; Morawski, M.; Zając, K.; Patkowski, W.; Zieniewicz, K. Unsatisfactory Long-term Results of Liver Transplant in Patients With Intrahepatic Cholangiocarcinoma. Transpl. Proc. 2020, 52, 2463–2467. [Google Scholar] [CrossRef] [PubMed]
- Hue, J.J.; Rocha, F.G.; Ammori, J.B.; Hardacre, J.M.; Rothermel, L.D.; Chavin, K.D.; Winter, J.M.; Ocuin, L.M. A comparison of surgical resection and liver transplantation in the treatment of intrahepatic cholangiocarcinoma in the era of modern chemotherapy: An analysis of the National Cancer Database. J. Surg. Oncol. 2021, 123, 949–956. [Google Scholar] [CrossRef] [PubMed]
- Vugts, J.J.A.; Gaspersz, M.P.; Roos, E.; Franken, L.C.; Olthof, P.B.; Coelen, R.J.S.; van Vugt, J.L.A.; Labeur, T.A.; Brouwer, L.; Besselink, M.G.H.; et al. Eligibility for Liver Transplantation in Patients with Perihilar Cholangiocarcinoma. Ann. Surg. Oncol. 2021, 28, 1483–1492. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kubal, C.; Mihaylov, P.; Holden, J. Oncologic indications of liver transplantation and deceased donor liver allocation in the United States. Curr. Opin. Organ. Transpl. 2021, 26, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Haddock, M.G.; Alberts, S.R.; Nyberg, S.L.; Ishitani, M.B.; Rosen, C.B.; Gores, G.J. Transplantation for hilar cholangiocarcinoma. Liver Transpl. 2004, 10 (Suppl. S2), S65–S68. [Google Scholar] [CrossRef] [PubMed]
- Ethun, C.G.; Lopez-Aguiar, A.G.; Anderson, D.J.; Adams, A.B.; Fields, R.C.; Doyle, M.B.; Chapman, W.C.; Krasnick, B.A.; Weber, S.M.; Mezrich, J.D.; et al. Transplantation Versus Resection for Hilar Cholangiocarcinoma: An Argument for Shifting Treatment Paradigms for Resectable Disease. Ann. Surg. 2018, 267, 797–805. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hidalgo, E.; Asthana, S.; Nishio, H.; Wyatt, J.; Toogood, G.J.; Prasad, K.R.; Lodge, J.P. Surgery for hilar cholangiocarcinoma: The Leeds experience. Eur. J. Surg. Oncol. 2008, 34, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Azad, A.I.; Rosen, C.B.; Taner, T.; Heimbach, J.K.; Gores, G.J. Selected Patients with Unresectable Perihilar Cholangiocarcinoma (pCCA) Derive Long-Term Benefit from Liver Transplantation. Cancers 2020, 12, 3157. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schaefer, B.; Zoller, H.; Schneeberger, S. Con: Liver transplantation for expanded criteria malignant diseases. Liver Transpl. 2018, 24, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Duignan, S.; Maguire, D.; Ravichand, C.S.; Geoghegan, J.; Hoti, E.; Fennelly, D.; Armstrong, J.; Rock, K.; Mohan, H.; Traynor, O. Neoadjuvant chemoradiotherapy followed by liver transplantation for unresectable cholangiocarcinoma: A single-centre national experience. HPB 2014, 16, 91–98. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sapisochin, G.; Fidelman, N.; Roberts, J.P.; Yao, F.Y. Mixed hepatocellular cholangiocarcinoma and intrahepatic cholangiocarcinoma in patients undergoing transplantation for hepatocellular carcinoma. Liver Transpl. 2011, 17, 934–942. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferro, V.; Gorgen, A.; Roayaie, S.; Droz Dit Busset, M.; Sapisochin, G. Liver resection and transplantation for intrahepatic cholangiocarcinoma. J. Hepatol. 2020, 72, 364–377. [Google Scholar] [CrossRef] [PubMed]
- Borakati, A.; Froghi, F.; Bhogal, R.H.; Mavroeidis, V.K. Liver transplantation in the management of cholangiocarcinoma: Evolution and contemporary advances. World J. Gastroenterol. 2023, 29, 1969–1981. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Castaldo, E.T.; Pinson, C.W. Liver transplantation for non-hepatocellular carcinoma malignancy. HPB 2007, 9, 98–103. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iwatsuki, S.; Gordon, R.D.; Shaw, B.W., Jr.; Starzl, T.E. Role of liver transplantation in cancer therapy. Ann. Surg. 1985, 202, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Penn, I. Hepatic transplantation for primary and metastatic cancers of the liver. Surgery 1991, 110, 726–734; discussion 34. [Google Scholar] [PubMed]
- Sapisochin, G.; Ivanics, T.; Heimbach, J. Liver transplantation for intrahepatic cholangiocarcinoma: Ready for prime time? Hepatology 2022, 75, 455–472. [Google Scholar] [CrossRef]
- Twohig, P.; Peeraphatdit, T.B.; Mukherjee, S. Current status of liver transplantation for cholangiocarcinoma. World J. Gastrointest. Surg. 2022, 14, 1. [Google Scholar] [CrossRef]
- Ziogas, I.A.; Giannis, D.; Economopoulos, K.P.; Hayat, M.H.; Montenovo, M.I.; Matsuoka, L.K.; Alexopoulos, S.P. Liver Transplantation for Intrahepatic Cholangiocarcinoma: A Meta-analysis and Meta-regression of Survival Rates. Transplantation 2021, 105, 2263–2271. [Google Scholar] [CrossRef] [PubMed]
| Type | Characteristics | Institution/Country | Date | ID | |
|---|---|---|---|---|---|
| iCCA | Early stages, cirrhotic | University Health Network, Canada | April 2018 | NCT02878473 | |
| Unresectable | Oslo University Hospital, Norway | June 2020 | NCT04556214 | ||
| pCCA | Oslo University Hospital, Norway | September 2021 | NCT04993131 | ||
| Neoadjuvant chemo-radiotherapy | Hospital Vall d’Hebron, Spain | April 2020 | NCT04378023 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esmail, A.; Badheeb, M.; Alnahar, B.; Almiqlash, B.; Sakr, Y.; Khasawneh, B.; Al-Najjar, E.; Al-Rawi, H.; Abudayyeh, A.; Rayyan, Y.; et al. Cholangiocarcinoma: The Current Status of Surgical Options including Liver Transplantation. Cancers 2024, 16, 1946. https://doi.org/10.3390/cancers16111946
Esmail A, Badheeb M, Alnahar B, Almiqlash B, Sakr Y, Khasawneh B, Al-Najjar E, Al-Rawi H, Abudayyeh A, Rayyan Y, et al. Cholangiocarcinoma: The Current Status of Surgical Options including Liver Transplantation. Cancers. 2024; 16(11):1946. https://doi.org/10.3390/cancers16111946
Chicago/Turabian StyleEsmail, Abdullah, Mohamed Badheeb, Batool Alnahar, Bushray Almiqlash, Yara Sakr, Bayan Khasawneh, Ebtesam Al-Najjar, Hadeel Al-Rawi, Ala Abudayyeh, Yaser Rayyan, and et al. 2024. "Cholangiocarcinoma: The Current Status of Surgical Options including Liver Transplantation" Cancers 16, no. 11: 1946. https://doi.org/10.3390/cancers16111946
APA StyleEsmail, A., Badheeb, M., Alnahar, B., Almiqlash, B., Sakr, Y., Khasawneh, B., Al-Najjar, E., Al-Rawi, H., Abudayyeh, A., Rayyan, Y., & Abdelrahim, M. (2024). Cholangiocarcinoma: The Current Status of Surgical Options including Liver Transplantation. Cancers, 16(11), 1946. https://doi.org/10.3390/cancers16111946