An Investigative Analysis of Therapeutic Strategies in Hepatocellular Carcinoma: A Raetrospective Examination of 23 Biopsy-Confirmed Cases Emphasizing the Significance of Histopathological Insights
Abstract
Simple Summary
Abstract
1. Background
- LR-NC, non-categorizable due to degraded images;
- LR-1, definitely benign;
- LR-2, probably benign, referring to nodules less than 2 cm, without any imagistic criteria of malignancy;
- LR-3, intermediate probability of malignancy, referring to nodules less than 2 cm with non-rim arterial hyperenhancement or nodules larger than 2 cm with arterial iso or hypo-enhancement;
- LR-4, high HCC probability, referring to nodules less than 10 mm, with arterial hyperenhancement and one other typical feature or nodules over 20 mm with arterial hyperenhancement and no other suggestive features;
- LR-5, a definite diagnosis of HCC, nodules over 10 mm with arterial hyperenhancement and portal washout, or with a 50% size increase in less than 6 months;
- LR-TIV, malignant venous thrombus, with arterial hyperenhancement regardless of the presence of a liver nodule;
- LR-M, high malignancy probability, but not HCC, referring to nodules with rim arterial enhancement, peripheral washout, targetoid aspect, or infiltrative appearance.
2. Materials and Methods
2.1. Ethical Statement
2.2. Patient Selection
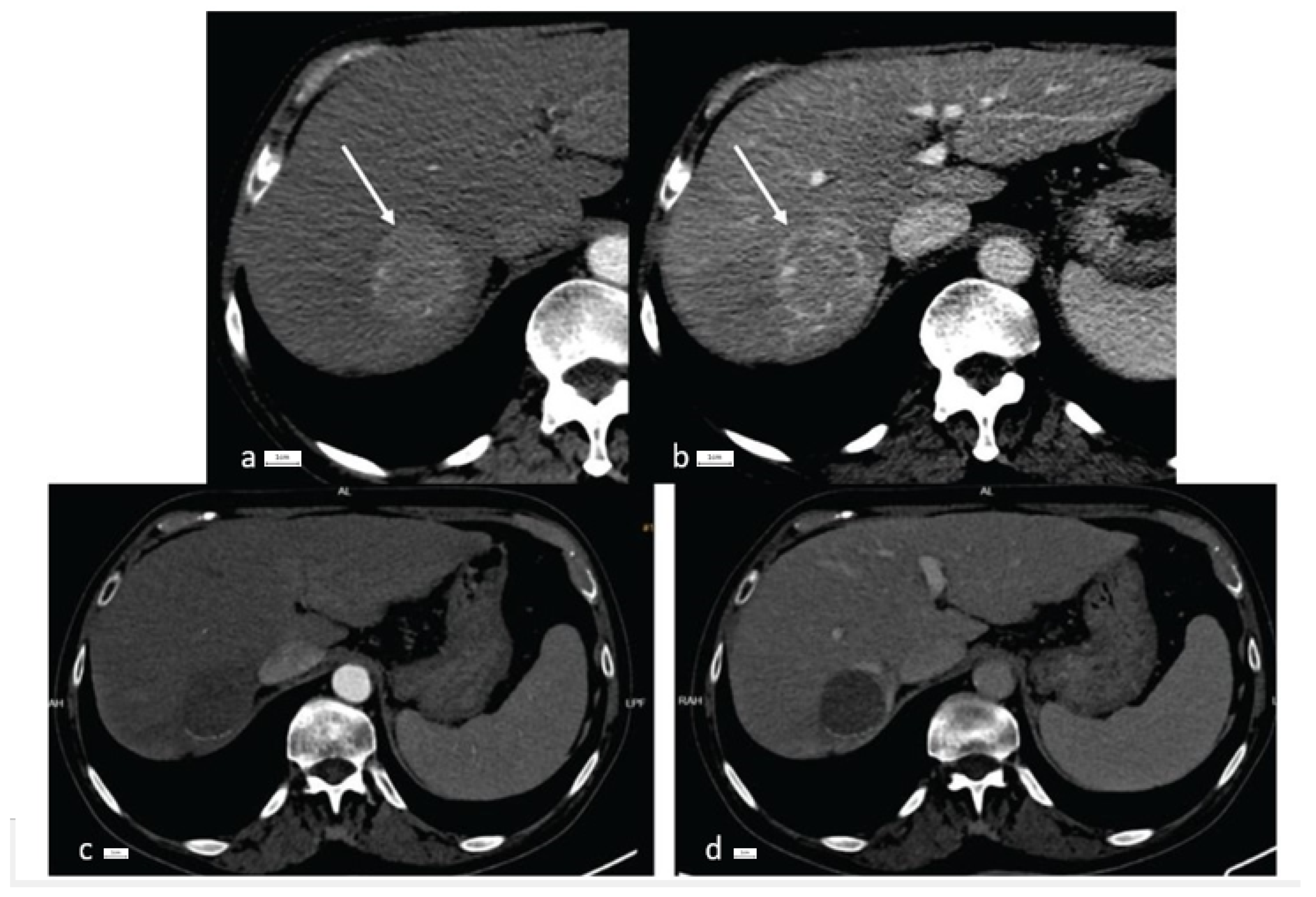
2.3. Imaging Techniques
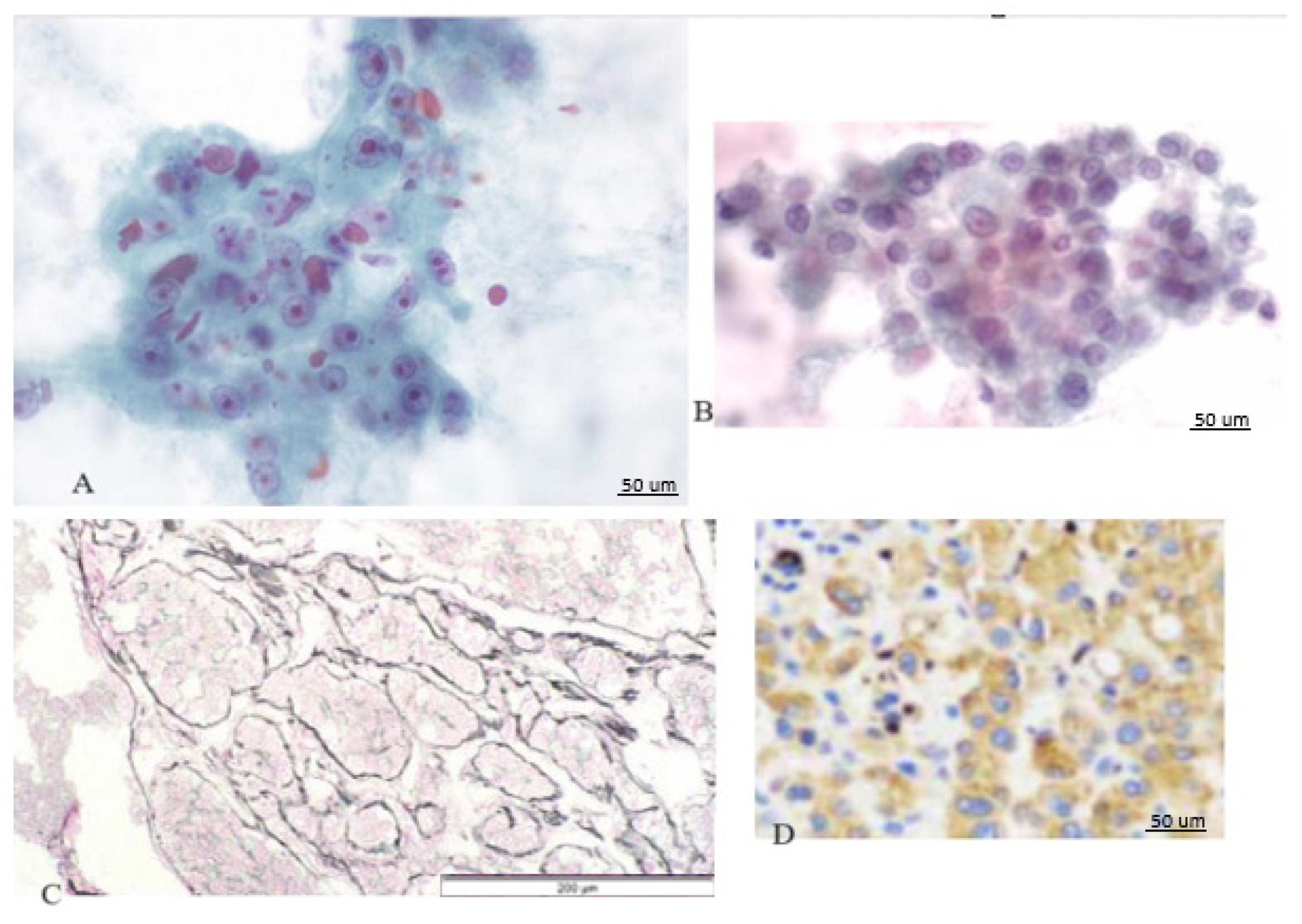
2.4. Histology Analysis
2.5. Statistical Analysis
3. Results
3.1. Descriptive Data
3.2. Liver Biopsy Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, H.M.; Lidofsky, S.D.; Taddei, T.H.; Townshend-Bulson, L.J. Attacking the public health crisis of hepatocellular carcinoma at its roots. Hepatology 2023, 77, 1456–1459. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424, Erratum in CA Cancer J. Clin. 2020, 70, 313. [Google Scholar] [CrossRef] [PubMed]
- Rumgay, H.; Arnold, M.; Ferlay, J.; Lesi, O.; Cabasag, C.J.; Vignat, J.; Laversanne, M.; McGlynn, K.A.; Soerjomataram, I. Global burden of primary liver cancer in 2020 and predictions to 2040. J. Hepatol. 2022, 77, 1598–1606. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236, Erratum in J. Hepatol. 2019, 70, 817. [Google Scholar] [CrossRef] [PubMed]
- Valery, P.C.; Laversanne, M.; Clark, P.J.; Petrick, J.L.; McGlynn, K.A.; Bray, F. Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology 2018, 67, 600–611. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singal, A.G.; Llovet, J.M.; Yarchoan, M.; Mehta, N.; Heimbach, J.K.; Dawson, L.A.; Jou, J.H.; Kulik, L.M.; Agopian, V.G.; Marrero, J.A.; et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology 2023, 22, 1922, Erratum in Hepatology 2023, 15, 1965. [Google Scholar] [CrossRef] [PubMed]
- Eisenbrey, J.R.; Gabriel, H.; Savsani, E.; Lyshchik, A. Contrast-enhanced ultrasound (CEUS) in HCC diagnosis and assessment of tumor response to locoregional therapies. Abdom. Radiol. 2021, 46, 3579–3595. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matsui, O.; Kobayashi, S.; Sanada, J.; Kouda, W.; Ryu, Y.; Kozaka, K.; Kitao, A.; Nakamura, K.; Gabata, T. Hepatocelluar nodules in liver cirrhosis: Hemodynamic evaluation (angiography-assisted CT) with special reference to multi-step hepatocarcinogenesis. Abdom. Imaging 2011, 36, 264–272. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huang, P.; Wu, F.; Hou, K.; Zhou, C.; Xiao, Y.; Wang, C.; Miao, G.; Yang, C.; Zeng, M. Diagnostic algorithm for subcentimeter hepatocellular carcinoma using alpha-fetoprotein and imaging features on gadoxetic acid-enhanced MRI. Eur. Radiol. 2023, 4, 1–12, ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.T.; Wang, J.J.; Zhu, Y.; Agopian, V.G.; Tseng, H.R.; Yang, J.D. Diagnostic Criteria and LI-RADS for Hepatocellular Carcinoma. Clin. Liver Dis. 2021, 17, 409–413. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chernyak, V.; Fowler, K.J.; Kamaya, A.; Kielar, A.Z.; Elsayes, K.M.; Bashir, M.R.; Kono, Y.; Do, R.K.; Mitchell, D.G.; Singal, A.G.; et al. Liver Imaging Reporting and Data System (LI-RADS) Version 2018: Imaging of Hepatocellular Carcinoma in At-Risk Patients. Radiology 2018, 289, 816–830. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tremosini, S.; Forner, A.; Boix, L.; Vilana, R.; Bianchi, L.; Reig, M.; Rimola, J.; Rodríguez-Lope, C.; Ayuso, C.; Solé, M.; et al. Prospective validation of an immunohistochemical panel (glypican 3, heat shock protein 70 and glutamine synthetase) in liver biopsies for diagnosis of very early hepatocellular carcinoma. Gut 2012, 61, 1481–1487. [Google Scholar] [CrossRef] [PubMed]
- Park, B.V.; Gaba, R.C.; Huang, Y.H.; Chen, Y.F.; Guzman, G.; Lokken, R.P. Histology of Hepatocellular Carcinoma: Association with Clinical Features, Radiological Findings, and Locoregional Therapy Outcomes. J. Clin. Imaging Sci. 2019, 9, 52. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bruix, J.; Chan, S.L.; Galle, P.R.; Rimassa, L.; Sangro, B. Systemic treatment of hepatocellular carcinoma: An EASL position paper. J. Hepatol. 2021, 75, 960–974. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Lu, M.; Che, J.; Chu, Q.; Zhang, P.; Chen, Y. Biomarkers and Future Perspectives for Hepatocellular Carcinoma Immunotherapy. Front. Oncol. 2021, 11, 716844. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yau, T.; Park, J.W.; Finn, R.S.; Cheng, A.L.; Mathurin, P.; Edeline, J.; Kudo, M.; Harding, J.J.; Merle, P.; Rosmorduc, O.; et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): A randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2022, 23, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Ji, J.H.; Ha, S.Y.; Lee, D.; Sankar, K.; Koltsova, E.K.; Abou-Alfa, G.K.; Yang, J.D. Predictive Biomarkers for Immune-Checkpoint Inhibitor Treatment Response in Patients with Hepatocellular Carcinoma. Int. J. Mol. Sci. 2023, 24, 7640. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Calderaro, J.; Rousseau, B.; Amaddeo, G.; Mercey, M.; Charpy, C.; Costentin, C.; Luciani, A.; Zafrani, E.S.; Laurent, A.; Azoulay, D.; et al. Programmed death ligand 1 expression in hepatocellular carcinoma: Relationship with clinical and pathological features. Hepatology 2016, 64, 2038–2046. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Lim, H.Y.; Kudo, M.; Breder, V.; Merle, P.; et al. Updated efficacy and safety data from IMbrave150: Atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J. Hepatol. 2022, 76, 862–873. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Ryoo, B.-Y.; Hsu, C.-H.; Numata, K.; Stein, S.; Verret, W.; Hack, S.P.; Spahn, J.; Liu, B.; Abdullah, H.; et al. Atezolizumab with or without Bevacizumab in Unresectable Hepatocellular Carcinoma (GO30140): An Open-Label, Multicentre, Phase 1b Study. Lancet Oncol. 2020, 21, 808–820. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M. Durvalumab plus Tremelimumab in Unresectable Hepatocellular Carcinoma. Hepatobiliary Surg. Nutr. 2022, 11, 592–596. [Google Scholar] [CrossRef] [PubMed]
- Nawaz, K. ESMO 2022: Ten Key Takeaways on Europe’s Top Oncology Event; Clarivate: London, UK, 2022. [Google Scholar]
- Formular Pentru Verificarea Respectării Criteriilor de Eligibilitate Aferente Protocolului Terapeutic Dci Atezolizumab. Available online: http://www.casan.ro/casbz/media/pageFiles/201)%20L01XC32.5-ATEZOLIZUMAB%20carcinom%20hepatocelular.pdf (accessed on 20 November 2023).
- Chiang, C.L.; Chan, A.C.Y.; Chiu, K.W.H.; Kong, F.S. Combined Stereotactic Body Radiotherapy and Checkpoint Inhibition in Unresectable Hepatocellular Carcinoma: A Potential Synergistic Treatment Strategy. Front. Oncol. 2019, 9, 1157. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Finn, R.S. The Role of Liver Biopsy in Hepatocellular Carcinoma. Gastroenterol. Hepatol. 2016, 12, 628–630. [Google Scholar] [PubMed] [PubMed Central]
- Seeff, L.B.; Everson, G.T.; Morgan, T.R.; Curto, T.M.; Lee, W.M.; Ghany, M.G.; Shiffman, M.L.; Fontana, R.J.; Di Bisceglie, A.M.; Bonkovsky, H.L.; et al. Complication rate of percutaneous liver biopsies among persons with advanced chronic liver disease in the HALT-C trial. Clin. Gastroenterol. Hepatol. 2010, 8, 877–883. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Midia, M.; Odedra, D.; Shuster, A.; Midia, R.; Muir, J. Predictors of bleeding complications following percutaneous image-guided liver biopsy: A scoping review. Diagn. Interv. Radiol. 2019, 25, 71–80. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silva, M.A.; Hegab, B.; Hyde, C.; Guo, B.; Buckels, J.A.; Mirza, D.F. Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: A systematic review and meta-analysis. Gut 2008, 57, 1592–1596. [Google Scholar] [CrossRef] [PubMed]
- Szpakowski, J.L.; Drasin, T.E.; Lyon, L.L. Rate of seeding with biopsies and ablations of hepatocellular carcinoma: A retrospective cohort study. Hepatol. Commun. 2017, 1, 841–851. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, G.J.; Wang, W.; Lu, M.D.; Xie, X.Y.; Xu, H.X.; Xu, Z.F.; Chen, L.D.; Wang, Z.; Liang, J.Y.; Huang, Y.; et al. Contrast-Enhanced Ultrasound for the Characterization of Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. Liver Cancer 2015, 4, 241–252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, G.; Zhu, S.; Li, X. Comparison of values of CT and MRI imaging in the diagnosis of hepatocellular carcinoma and analysis of prognostic factors. Oncol. Lett. 2019, 17, 1184–1188. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Semaan, S.; Vietti Violi, N.; Lewis, S.; Chatterji, M.; Song, C.; Besa, C.; Babb, J.S.; Fiel, M.I.; Schwartz, M.; Thung, S.; et al. Hepatocellular carcinoma detection in liver cirrhosis: Diagnostic performance of contrast-enhanced CT vs. MRI with extracellular contrast vs. gadoxetic acid. Eur. Radiol. 2020, 30, 1020–1030. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Zheng, J.; Yang, C.; Wang, R.; Zhou, Y.; Tao, Y.Y.; Gong, X.Q.; Wang, W.C.; Zhang, X.M.; Yang, L. Intravoxel incoherent motion diffusion-weighted imaging to differentiate hepatocellular carcinoma from intrahepatic cholangiocarcinoma. Sci. Rep. 2020, 10, 7717. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Di Tommaso, L.; Spadaccini, M.; Donadon, M.; Personeni, N.; Elamin, A.; Aghemo, A.; Lleo, A. Role of liver biopsy in hepatocellular carcinoma. World J. Gastroenterol. 2019, 25, 6041–6052. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Y.; Liang, X.; Li, H.; Yang, T.; Guo, S.; Chen, X. Nivolumab Versus Sorafenib as First-Line Therapy for Advanced Hepatocellular Carcinoma: A Cost-Effectiveness Analysis. Front Pharmacol. 2022, 13, 906956. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.X.; Finn, R.S.; Edeline, J.; Cattan, S.; Ogasawara, S.; Palmer, D.; Verslype, C.; Zagonel, V.; Fartoux, L.; Vogel, A.; et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol. 2018, 19, 940–952, Erratum in Lancet Oncol. 2018, 19, e440. [Google Scholar] [CrossRef] [PubMed]
- Powles, T.; Eder, J.P.; Fine, G.D.; Braiteh, F.S.; Loriot, Y.; Cruz, C.; Bellmunt, J.; Burris, H.A.; Petrylak, D.P.; Teng, S.L.; et al. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature 2014, 515, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Kleinovink, J.W.; van Hall, T.; Ossendorp, F.; Fransen, M.F. PD-L1 immune suppression in cancer: Tumor cells or host cells? Oncoimmunology 2017, 6, e1325982. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Von Felden, J.; Karkmann, K.; Ittrich, H.; Gil-Ibanez, I.; Fründt, T.; Krause, J.; Lohse, A.W.; Wege, H.; Schulze, K. Sequential Systemic Treatment in Advanced Hepatocellular Carcinoma Is Able to Prolong Median Survival to More than 3 Years in a Selected Real-World Cohort. Visc. Med. 2021, 37, 87–93. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pinato, D.J.; Mauri, F.A.; Spina, P.; Cain, O.; Siddique, A.; Goldin, R.; Victor, S.; Pizio, C.; Akarca, A.U.; Boldorini, R.L.; et al. Clinical implications of heterogeneity in PD-L1 immunohistochemical detection in hepatocellular carcinoma: The Blueprint-HCC study. Br. J. Cancer 2019, 120, 1033–1036. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yi, M.; Jiao, D.; Xu, H.; Liu, Q.; Zhao, W.; Han, X.; Wu, K. Biomarkers for predicting efficacy of PD-1/PD-L1 inhibitors. Mol. Cancer 2018, 17, 129. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vilain, R.E.; Menzies, A.M.; Wilmott, J.S.; Kakavand, H.; Madore, J.; Guminski, A.; Liniker, E.; Kong, B.Y.; Cooper, A.J.; Howle, J.R.; et al. Dynamic Changes in PD-L1 Expression and Immune Infiltrates Early During Treatment Predict Response to PD-1 Blockade in Melanoma. Clin. Cancer Res. 2017, 23, 5024–5033. [Google Scholar] [CrossRef] [PubMed]
- Zen, C.; Zen, Y.; Mitry, R.R.; Corbeil, D.; Karbanová, J.; O’Grady, J.; Karani, J.; Kane, P.; Heaton, N.; Portmann, B.C.; et al. Mixed phenotype hepatocellular carcinoma after transarterial chemoembolization and liver transplantation. Liver Transpl. 2011, 17, 943–954. [Google Scholar] [CrossRef] [PubMed]
- Russo, F.P.; Imondi, A.; Lynch, E.N.; Farinati, F. When and how should we perform a biopsy for HCC in patients with liver cirrhosis in 2018? A review. Dig. Liver Dis. 2018, 50, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Rallis, K.S.; Makrakis, D.; Ziogas, I.A.; Tsoulfas, G. Immunotherapy for advanced hepatocellular carcinoma: From clinical trials to real-world data and future advances. World J. Clin. Oncol. 2022, 13, 448–472. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xia, Y.; Tang, W.; Qian, X.; Li, X.; Cheng, F.; Wang, K.; Zhang, F.; Zhang, C.; Li, D.; Song, J.; et al. Efficacy and safety of camrelizumab plus apatinib during the perioperative period in resectable hepatocellular carcinoma: A single-arm, open label, phase II clinical trial. J. Immunother. Cancer 2022, 10, e004656. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maas, M.; Beets-Tan, R.; Gaubert, J.Y.; Gomez Munoz, F.; Habert, P.; Klompenhouwer, L.G.; Vilares Morgado, P.; Schaefer, N.; Cornelis, F.H.; Solomon, S.B.; et al. Follow-up after radiological intervention in oncology: ECIO-ESOI evidence and consensus-based recommendations for clinical practice. Insights Imaging 2020, 11, 83. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ciuhu, A.N.; Rahnea-Nita, G.; Popescu, M.; Rahnea-Nita, R.A. Abstract P5–15–22: Evaluation of quality of life in patients with advanced and metastatic breast cancer proposed for palliative chemotherapy and best supportive care versus best supportive care. Cancer Res. 2015, 75, P5–P15. [Google Scholar] [CrossRef]
| No Previous Interventions (N = 10 Patients) | Previous TACE (N = 9 Patients) | Previous RFA (N = 4 Patients) | |
|---|---|---|---|
| Etiology of liver disease | HCV cirrhosis: 2 patients (20%) HBV cirrhosis: 5 patients (50%) NASH cirrhosis: 1 patient (10%) HBV + HDV hepatitis: 2 patients (20%) | HCV cirrhosis: 5 patients (55.5%) HBV hepatitis: 1 patient (11.1%) HBV + HDV hepatitis: 2 patients (22.2%) NASH cirrhosis: 1 patient (11.1%) | HCV cirrhosis: 2 patients (50%) HBV hepatitis: 1 patient (25%) HBV cirrhosis: 1 patient (25%) |
| AFP (N: 0–8.1 ng/mL) | 380.52 ± 134.83 | 112.56 ± 45.24 | 135 ± 46.13 |
| LI-RADS score | LR-4: 2 patients (20%) LR-5: 8 patients (80%) | LR-4: 2 patients (22.2%) LR-5: 7 patients (77.7%) | LR-4: 1 patient (25%) LR-5: 3 patients (75%) |
| Number of nodules | 1–3: 8 patients (80%) >3: 2 patients (20%) | 1–3: 6 patients (66.6%) >3: 3 patients (33.3%) | 1–3: 3 patients (75%) >3: 1 patient (25%) |
| Size of nodule of interest | Median 3.5 cm Range 1.6–5.2 cm | Median 2.4 cm Range 1.8–3.7 | Median 2.2 cm Range 2.1–2.5 cm |
| Portal vein invasion | Yes—4 patients (40%) | Yes—2 patients (22.2%) | Yes—0 patients (0%) |
| No Previous Interventions (N = 10 Patients) | Previous TACE (N = 9 Patients) | Previous RFA (N = 4 Patients) | |
|---|---|---|---|
| Edmondson–Steiner | Grade II: 4 patients (40%) | Grade II: 3 patients (33.3%) | Grade II: 1 patient (25%) |
| Grade III: 5 patients (50%) | Grade III: 6 patients (66.6%) | Grade III: 3 patients (75%) | |
| Grade IV: 1 patient (1%) | |||
| PD-L1 expression | 11.6% | 8.7% | 9.4% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zgura, A.; Grasu, M.C.; Dumitru, R.L.; Toma, L.; Iliescu, L.; Baciu, C. An Investigative Analysis of Therapeutic Strategies in Hepatocellular Carcinoma: A Raetrospective Examination of 23 Biopsy-Confirmed Cases Emphasizing the Significance of Histopathological Insights. Cancers 2024, 16, 1916. https://doi.org/10.3390/cancers16101916
Zgura A, Grasu MC, Dumitru RL, Toma L, Iliescu L, Baciu C. An Investigative Analysis of Therapeutic Strategies in Hepatocellular Carcinoma: A Raetrospective Examination of 23 Biopsy-Confirmed Cases Emphasizing the Significance of Histopathological Insights. Cancers. 2024; 16(10):1916. https://doi.org/10.3390/cancers16101916
Chicago/Turabian StyleZgura, Anca, Mugur Cristian Grasu, Radu Lucian Dumitru, Letitia Toma, Laura Iliescu, and Cosmin Baciu. 2024. "An Investigative Analysis of Therapeutic Strategies in Hepatocellular Carcinoma: A Raetrospective Examination of 23 Biopsy-Confirmed Cases Emphasizing the Significance of Histopathological Insights" Cancers 16, no. 10: 1916. https://doi.org/10.3390/cancers16101916
APA StyleZgura, A., Grasu, M. C., Dumitru, R. L., Toma, L., Iliescu, L., & Baciu, C. (2024). An Investigative Analysis of Therapeutic Strategies in Hepatocellular Carcinoma: A Raetrospective Examination of 23 Biopsy-Confirmed Cases Emphasizing the Significance of Histopathological Insights. Cancers, 16(10), 1916. https://doi.org/10.3390/cancers16101916








