Incidence of Pediatric Cancers in French Guiana: How Does It Compare to Global Estimates?
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Background and Population
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Collected Data
2.5. Population Data
2.6. Judgement Criteria
2.7. Comparative Data
2.8. Ethical and Regulatory Aspects
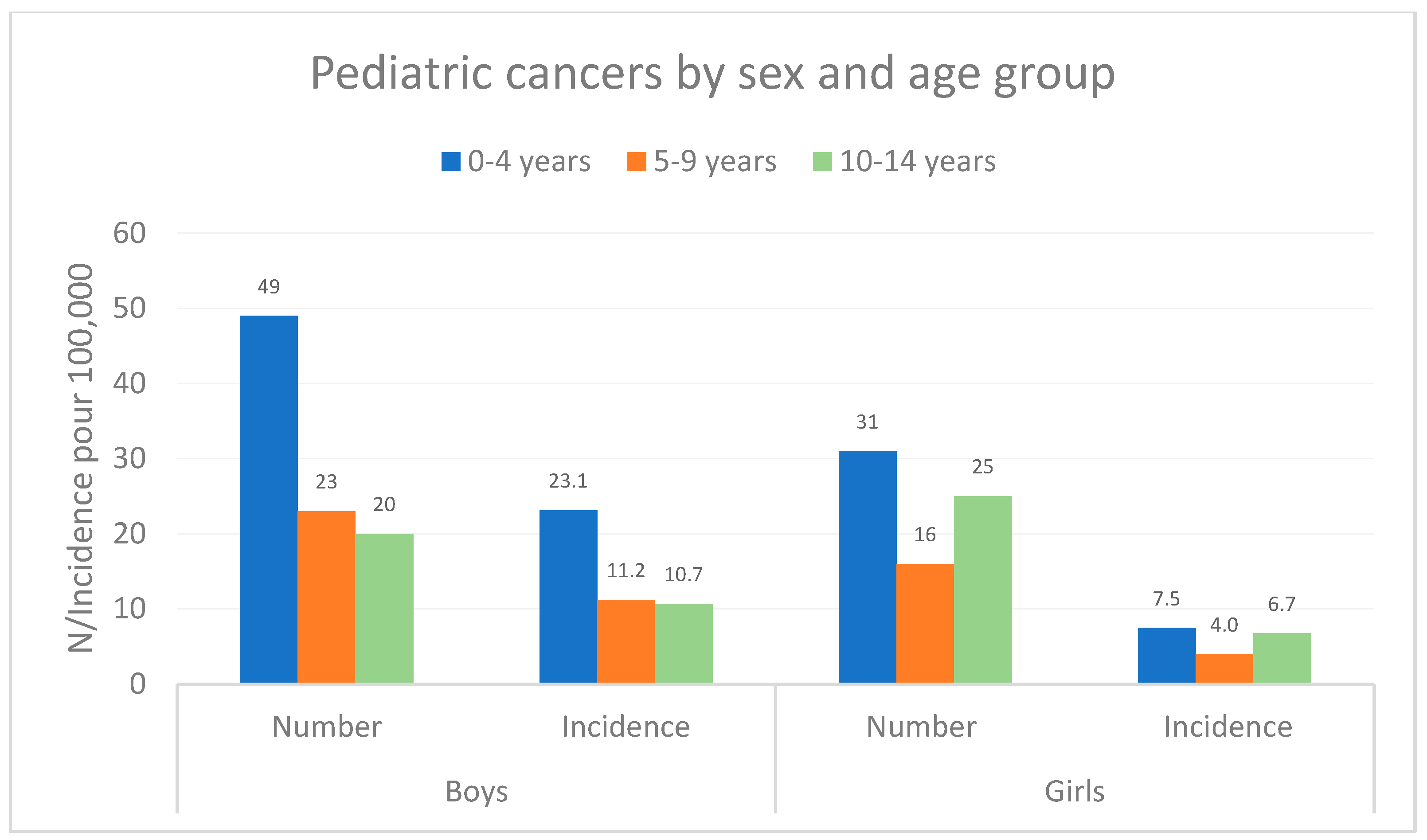
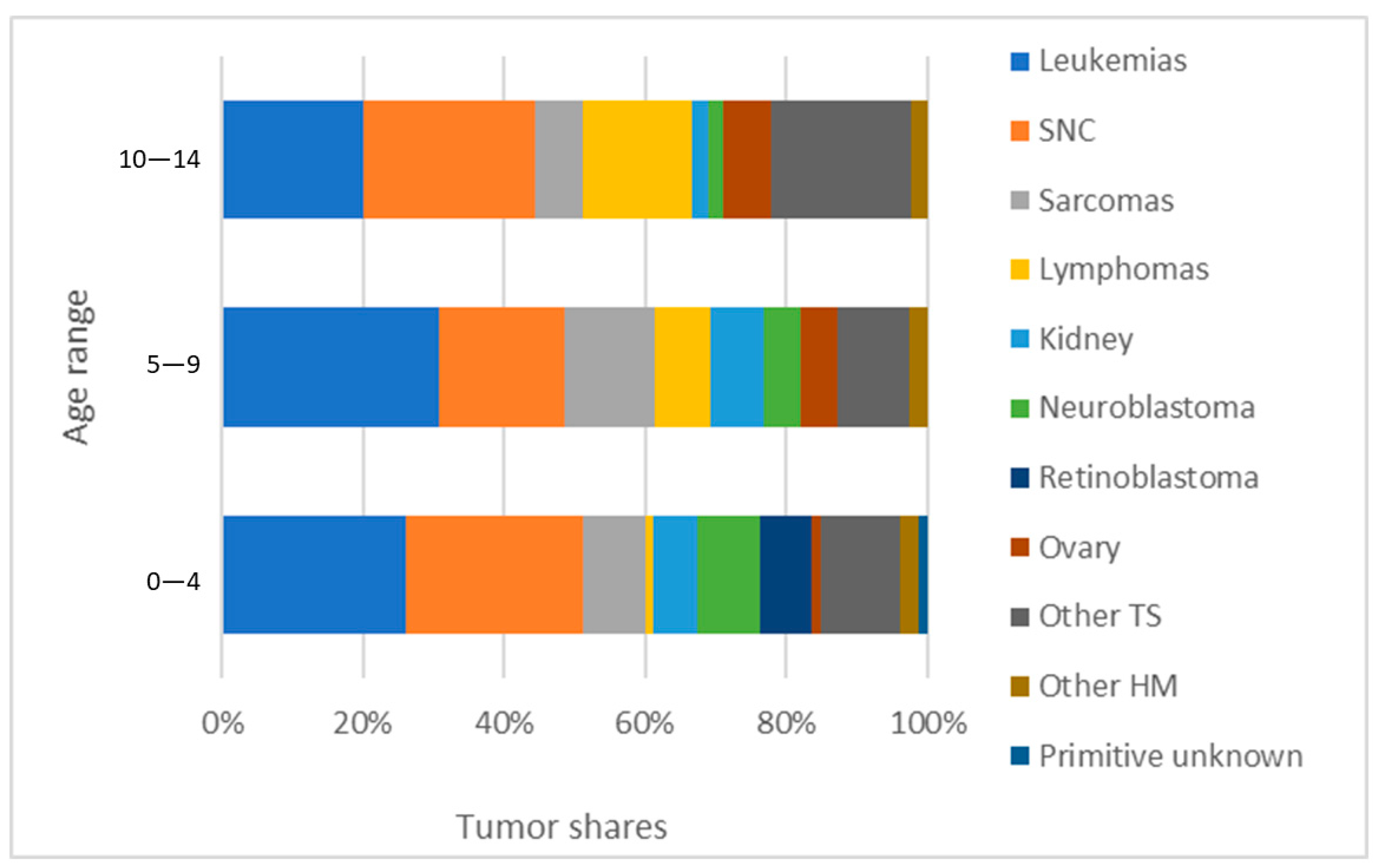
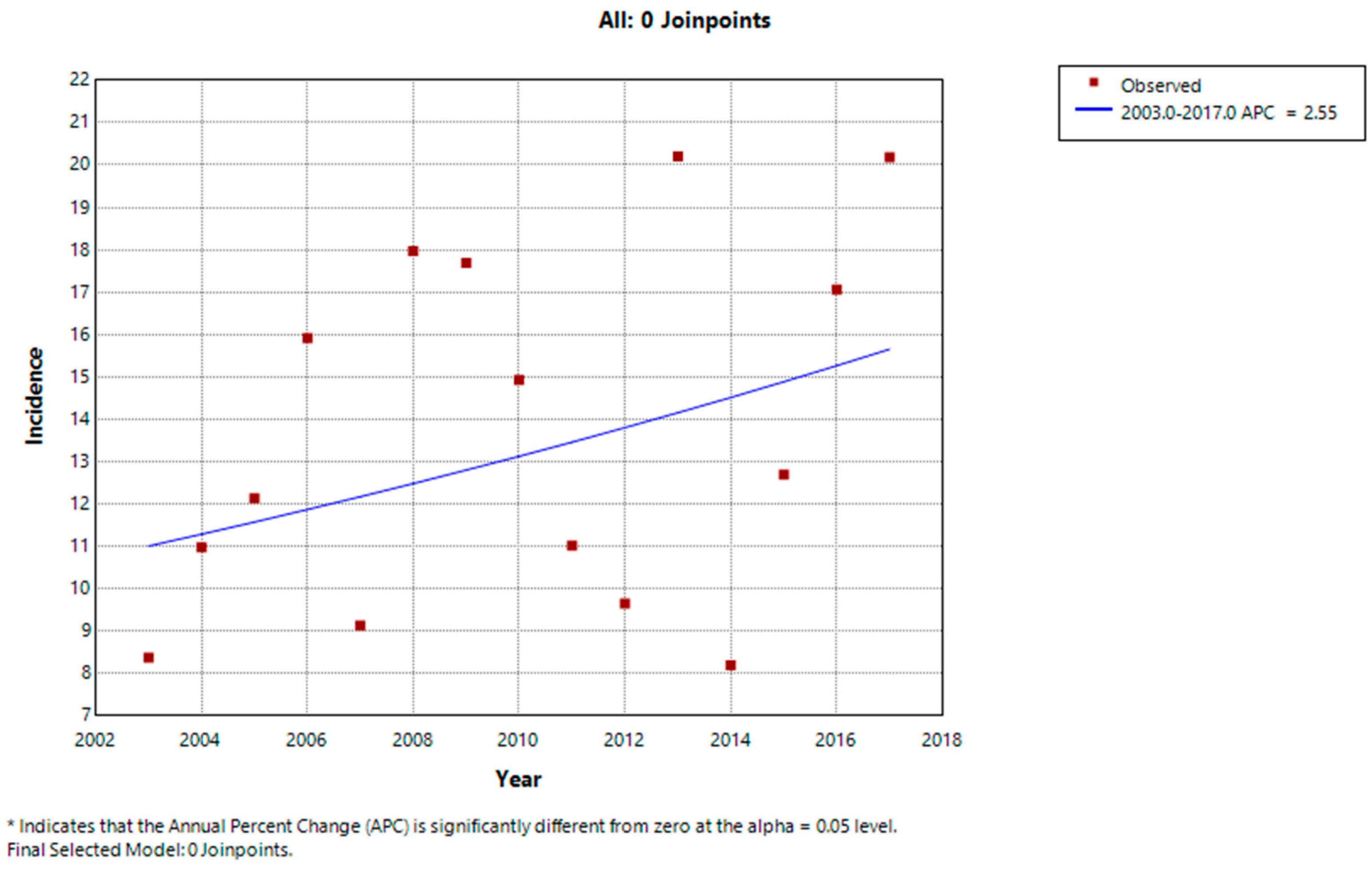
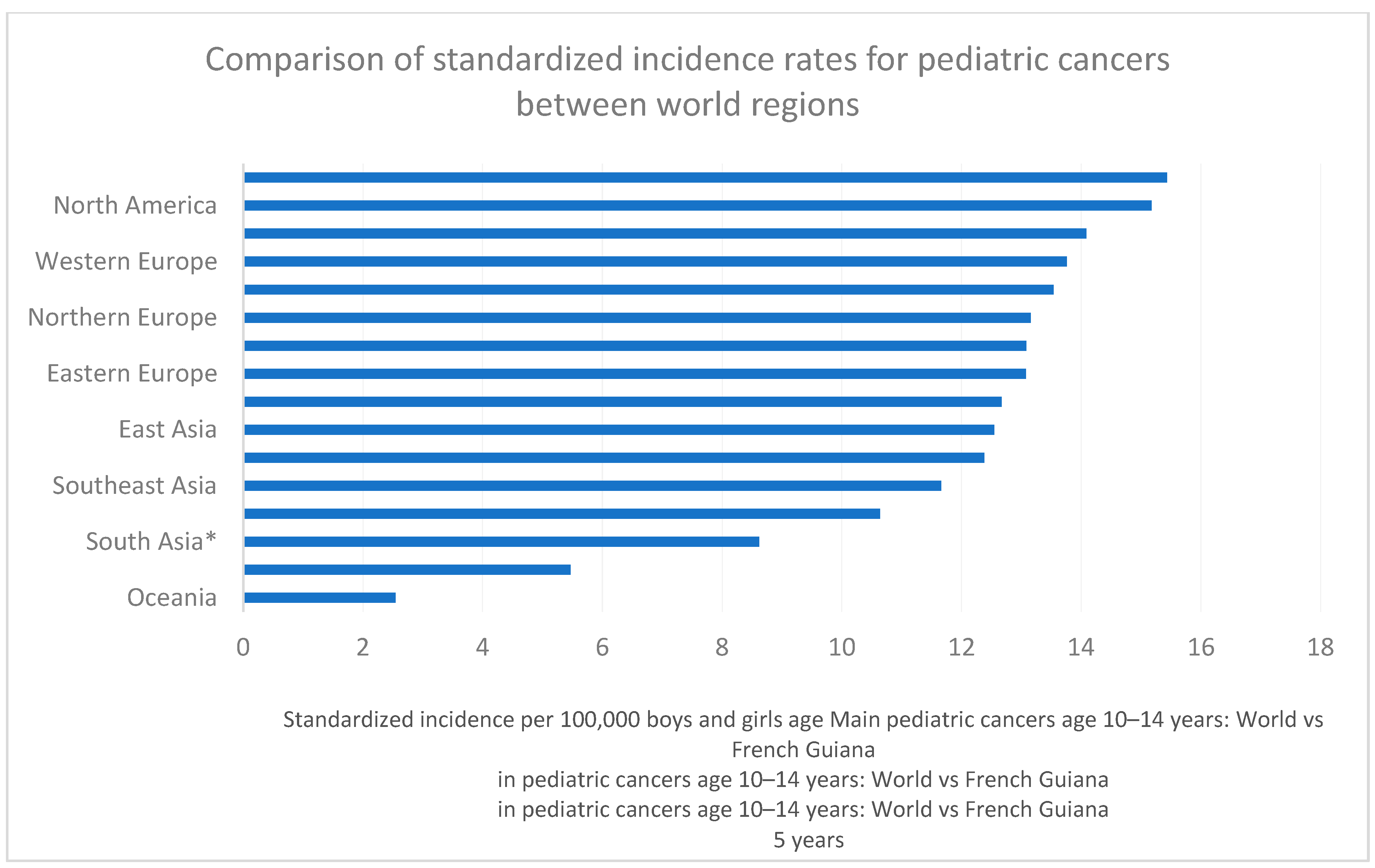
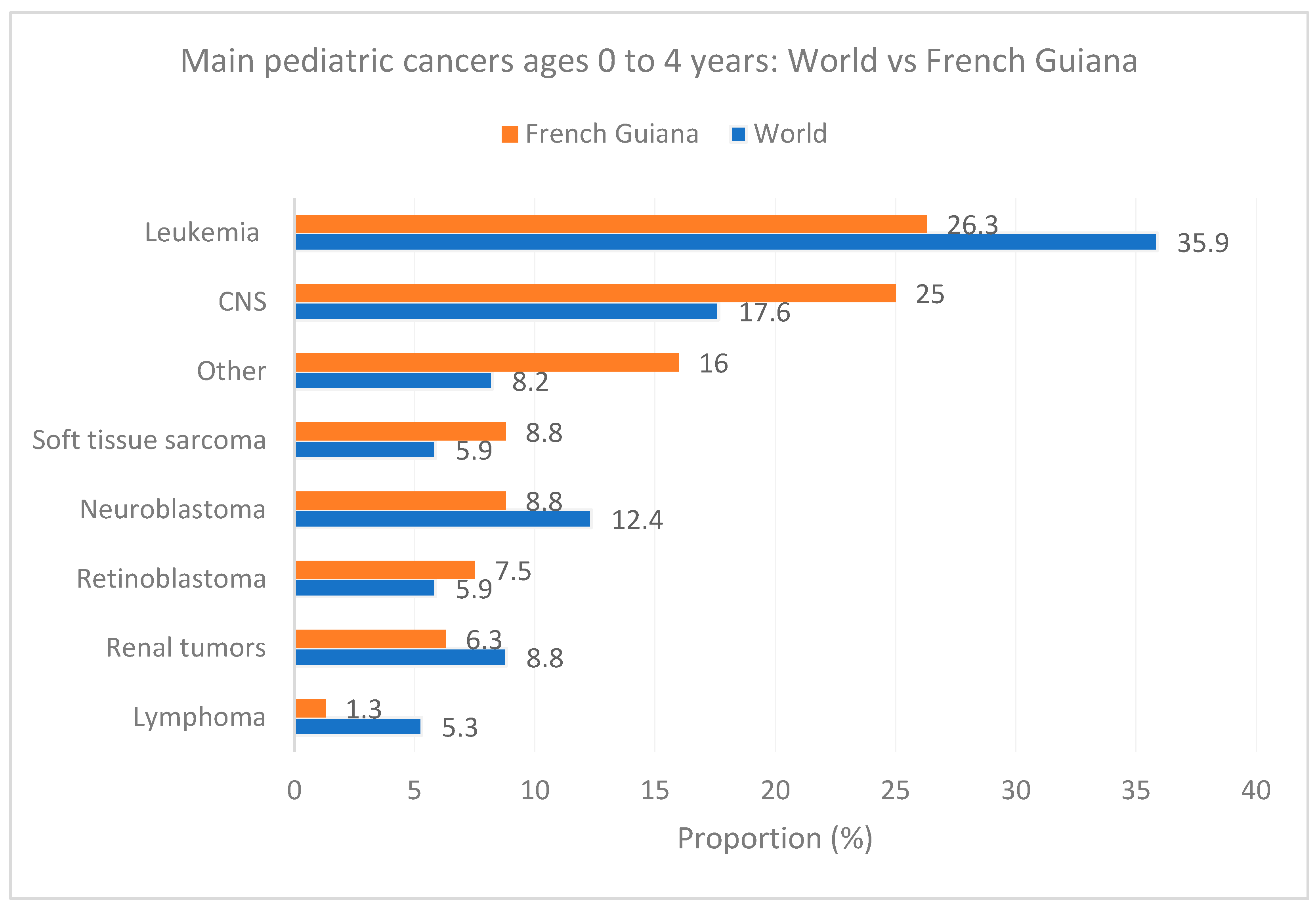
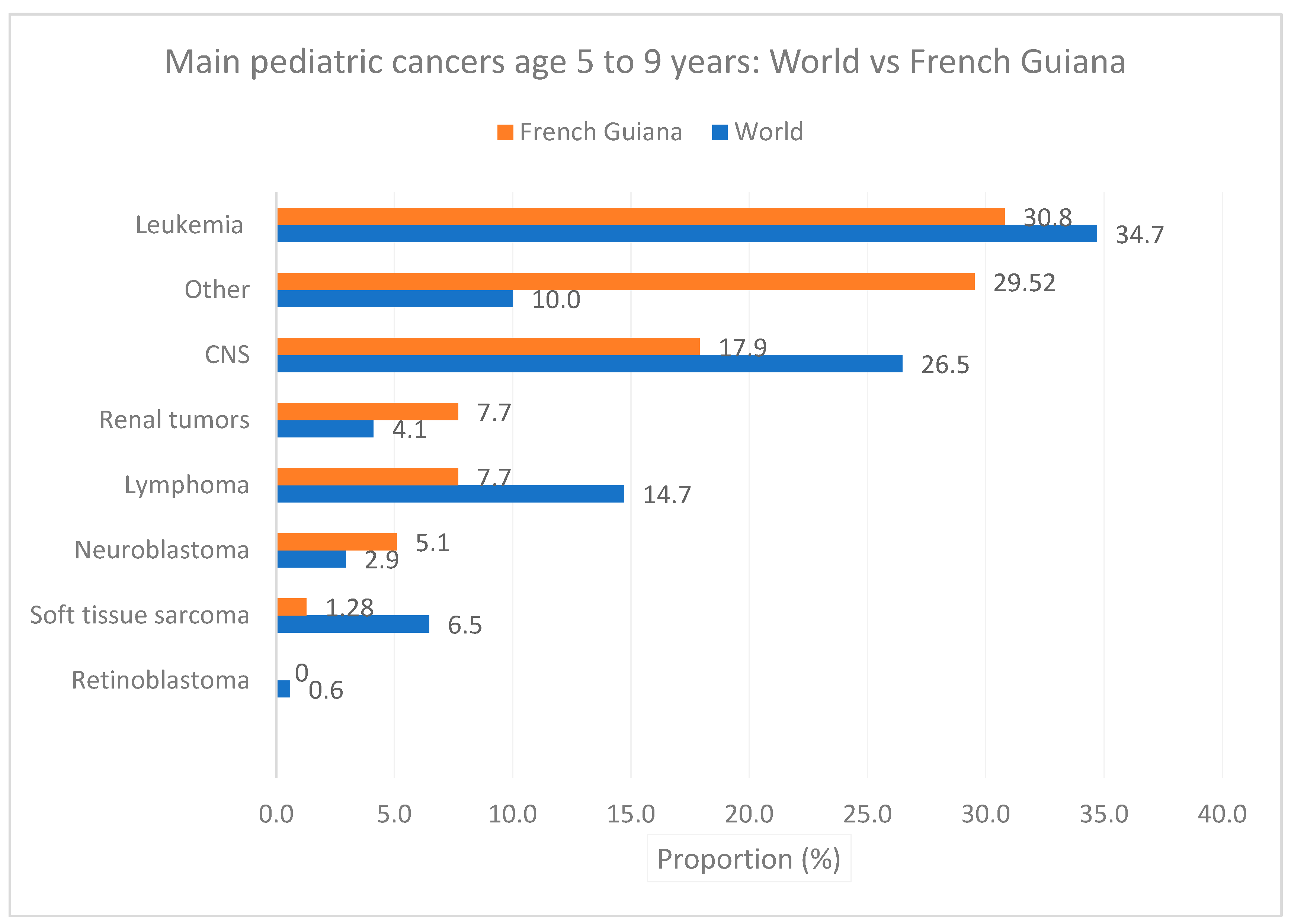
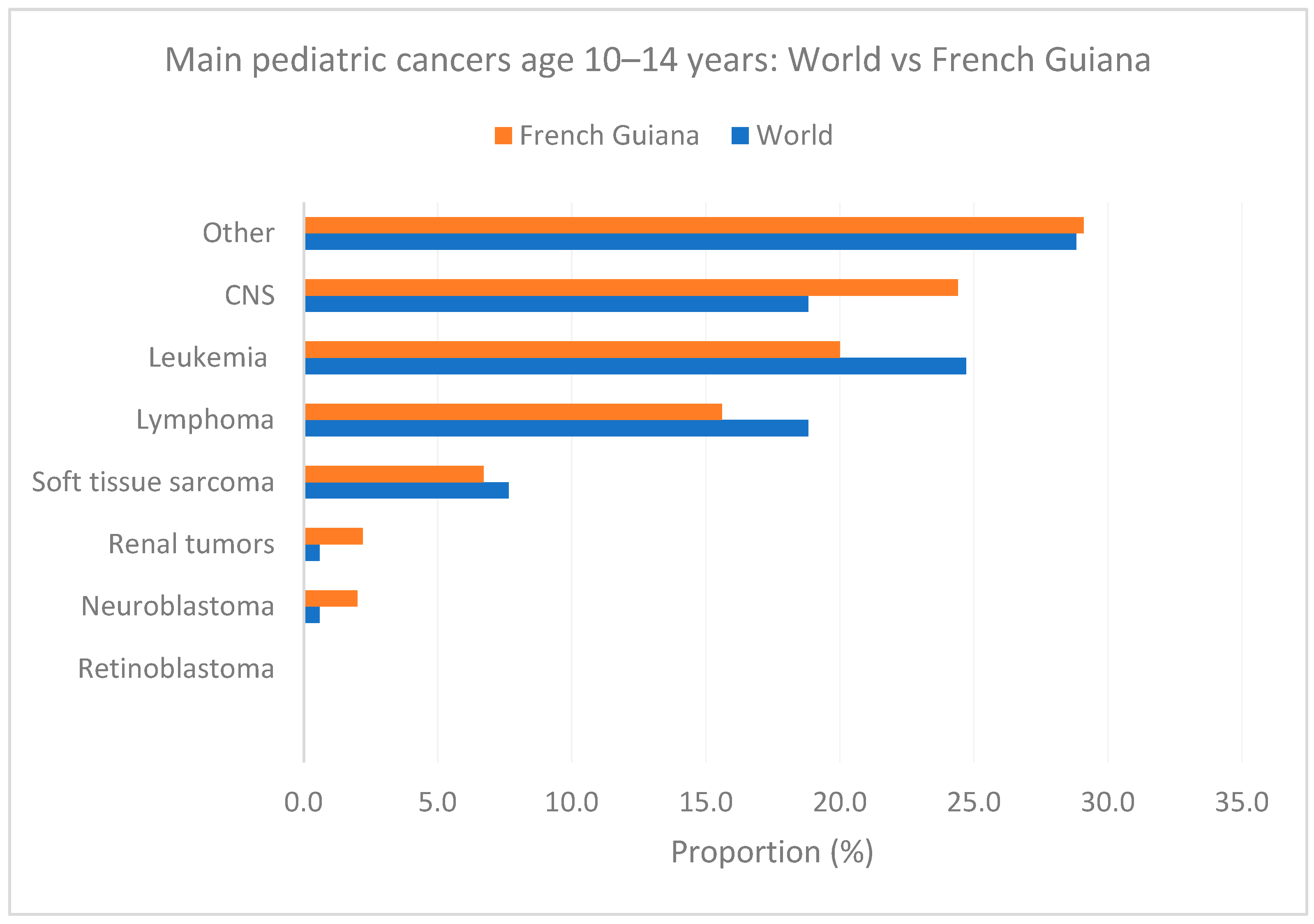
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steliarova-Foucher, E.; Colombet, M.; Ries, L.A.G.; Moreno, F.; Dolya, A.; Bray, F.; Hesseling, P.; Shin, H.Y.; Stiller, C.A.; Bouzbid, S.; et al. International Incidence of Childhood Cancer, 2001–2010: A Population-Based Registry Study. Lancet Oncol. 2017, 18, 719–731. [Google Scholar] [CrossRef] [PubMed]
- Kaatsch, P. Epidemiology of Childhood Cancer. Cancer Treat. Rev. 2010, 36, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Bhakta, N.; Force, L.M.; Allemani, C.; Atun, R.; Bray, F.; Coleman, M.P.; Steliarova-Foucher, E.; Frazier, A.L.; Robison, L.L.; Rodriguez-Galindo, C. Childhood Cancer Burden: A Review of Global Estimates. Lancet Oncol. 2019, 20, e42–e53. [Google Scholar] [CrossRef] [PubMed]
- Stiller, C.A. Epidemiology and Genetics of Childhood Cancer. Oncogene 2004, 23, 6429–6444. [Google Scholar] [CrossRef] [PubMed]
- Insee. Atlas Des Populations Immigrées En Guyane—Dossiers Régionaux. Available online: https://www.insee.fr/fr/statistiques/1290097 (accessed on 6 May 2024).
- Marie, C.-V.; Temporal, F. Les DOM: Terres de migrations. Espace Popul. Sociétés Space Popul. Soc. 2011, 3, 475–491. [Google Scholar] [CrossRef]
- Nacher, M.; Basurko, C.; Douine, M.; Lambert, Y.; Hcini, N.; Elenga, N.; Le Turnier, P.; Epelboin, L.; Djossou, F.; Couppié, P.; et al. The Epidemiologic Transition in French Guiana: Secular Trends and Setbacks, and Comparisons with Continental France and South American Countries. Trop. Med. Infect. Dis. 2023, 8, 219. [Google Scholar] [CrossRef] [PubMed]
- Imounga, L.M.; Plenet, J.; Belliardo, S.; Chine, E.C.; Adenis, A.; Gaillet, M.; Thomas, N.; Michaud, C.; Servas, V.; Couppié, P.; et al. Incidence and Mortality of Cervical Cancer in French Guiana: Temporal and Spatial Trends. Public Health Pr. 2021, 2, 100138. [Google Scholar] [CrossRef] [PubMed]
- Imounga, L.M.; Plenet, J.; Belliardo, S.; Chine, E.C.; Louvel, D.; Cenciu, B.; Couppié, P.; Alsibai, K.D.; Nacher, M. Gastric Cancer Incidence and Mortality in French Guiana: South American or French? J. Gastrointest Cancer 2022, 53, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Nacher, M.; Basurko, C.; Douine, M.; Lambert, Y.; Rousseau, C.; Michaud, C.; Garlantezec, R.; Adenis, A.; Gomes, M.M.; Alsibai, K.D.; et al. Contrasted Life Trajectories: Reconstituting the Main Population Exposomes in French Guiana. Front. Public Health 2023, 11, 1247310. [Google Scholar] [CrossRef]
- Rehman, K.; Fatima, F.; Waheed, I.; Akash, M.S.H. Prevalence of Exposure of Heavy Metals and Their Impact on Health Consequences. J. Cell. Biochem. 2018, 119, 157–184. [Google Scholar] [CrossRef]
- Skalny, A.V.; Aschner, M.; Sekacheva, M.I.; Santamaria, A.; Barbosa, F.; Ferrer, B.; Aaseth, J.; Paoliello, M.M.B.; Rocha, J.B.T.; Tinkov, A.A. Mercury and Cancer: Where Are We Now after Two Decades of Research? Food Chem. Toxicol. 2022, 164, 113001. [Google Scholar] [CrossRef] [PubMed]
- Osei, L.; Vignier, N.; Nacher, M.; Laumonnier, J.; Conan, C.; Clarke, L.; Koivogui, A.; Covis, S.; Valony, L.; Basurko, C.; et al. Small for Gestational Age Newborns in French Guiana: The Importance of Health Insurance for Prevention. Int. J. Public Health 2024, 69, 1606423. [Google Scholar] [CrossRef] [PubMed]
- Osei, L.; Basurko, C.; Nacher, M.; Vignier, N.; Elenga, N. About the Need to Address Pediatric Health Inequalities in French Guiana: A Scoping Review. Arch. Pediatr. 2022, 29, 340–346. [Google Scholar] [CrossRef] [PubMed]
- 29% Des Guyanais En Situation de Grande Pauvreté En 2018—Insee Analyses Guyane—59. Available online: https://www.insee.fr/fr/statistiques/6468775 (accessed on 15 March 2024).
- Leneuve-Dorilas, M.; Favre, A.; Carles, G.; Louis, A.; Nacher, M. Risk Factors for Premature Birth in French Guiana: The Importance of Reducing Health Inequalities. J. Matern. Fetal. Neonatal Med. 2019, 32, 1388–1396. [Google Scholar] [CrossRef] [PubMed]
- Basurko, C.; Dupart, O.; Savy, M.; Obert-Marby, C.; Mvogo, A.; Gonzalez, A.; Trepont, A.; Cann, L.; Boceno, C.; Osei, L.; et al. Hunger in French Guiana’s Vulnerable Urban Neighborhoods: A Neglected Consequence of COVID-19. Food Nutr. Bull. 2023, 44, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Rimbaud, D.; Restrepo, M.; Louison, A.; Boukhari, R.; Ardillon, V.; Carles, G.; Lambert, V.; Jolivet, A. Blood Lead Levels and Risk Factors for Lead Exposure among Pregnant Women in Western French Guiana: The Role of Manioc Consumption. J. Toxicol. Environ. Health A 2017, 80, 382–393. [Google Scholar] [CrossRef] [PubMed]
- Insee. Migrations, Famille et Vieillissement: Défis et Enjeux Pour La Guyane—AntianÉchos de Guyane. Available online: https://www.insee.fr/fr/statistiques/1291181 (accessed on 15 March 2024).
- Skidmore, M.; Sims, K.M.; Gibbs, H.; Rausch, L. Health, Climate, and Agriculture: A Case Study of Childhood Cancer in Brazil’s Amazon and Cerrado Biomes. In Proceedings of the 2021 Agricultural & Applied Economics Association Annual Meeting, Austin, TX, USA, 1–3 August 2021. [Google Scholar]
- Hurtig, A.-K.; San Sebastián, M. Geographical Differences in Cancer Incidence in the Amazon Basin of Ecuador in Relation to Residence near Oil Fields. Int. J. Epidemiol. 2002, 31, 1021–1027. [Google Scholar] [CrossRef] [PubMed][Green Version]
- World (WHO 2000-2025) Standard—Standard Populations—SEER Datasets. Available online: https://seer.cancer.gov/stdpopulations/world.who.html (accessed on 6 May 2024).
- Joinpoint Regression Program. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 6 May 2024).
- Les Registres. Available online: https://www.francim-reseau.org/les-registres (accessed on 6 May 2024).
- Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA Relevance); European Union: Maastricht, The Netherlands, 2016; Volume 119.
- Nacher, M.; Blanc, J.; Rabier, S.; Lucarelli, A.; Adenis, A.; Basurko, C.; Louis, A.; Dotou, D.; Leneuve, M.; Osei, L.; et al. Thirty Years of HIV Pregnancies in French Guiana: Prevention Successes and Remaining Obstetrical Challenges. Front. Glob. Women’s Health 2023, 4, 1264837. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A. Pesticide Use in South and South-East Asia: Environmental Public Health and Legal Concerns. Am. J. Environ. Sci. 2012, 8, 152–157. [Google Scholar] [CrossRef]
- Ward, M.H.; Colt, J.S.; Metayer, C.; Gunier, R.B.; Lubin, J.; Crouse, V.; Nishioka, M.G.; Reynolds, P.; Buffler, P.A. Residential Exposure to Polychlorinated Biphenyls and Organochlorine Pesticides and Risk of Childhood Leukemia. Environ. Health Perspect. 2009, 117, 1007–1013. [Google Scholar] [CrossRef]
- Hernández, A.F.; Menéndez, P. Linking Pesticide Exposure with Pediatric Leukemia: Potential Underlying Mechanisms. Int. J. Mol. Sci. 2016, 17, 461. [Google Scholar] [CrossRef] [PubMed]
- Valmy, L.; Gontier, B.; Parriault, M.C.; Van Melle, A.; Pavlovsky, T.; Basurko, C.; Grenier, C.; Douine, M.; Adenis, A.; Nacher, M. Prevalence and Predictive Factors for Renouncing Medical Care in Poor Populations of Cayenne, French Guiana. BMC Health Serv. Res. 2016, 16, 34. [Google Scholar] [CrossRef] [PubMed]
- Van Melle, A.; Cropet, C.; Parriault, M.-C.; Adriouch, L.; Lamaison, H.; Sasson, F.; Duplan, H.; Richard, J.-B.; Nacher, M. Renouncing Care in French Guiana: The National Health Barometer Survey. BMC Health Serv. Res. 2019, 19, 99. [Google Scholar] [CrossRef] [PubMed]
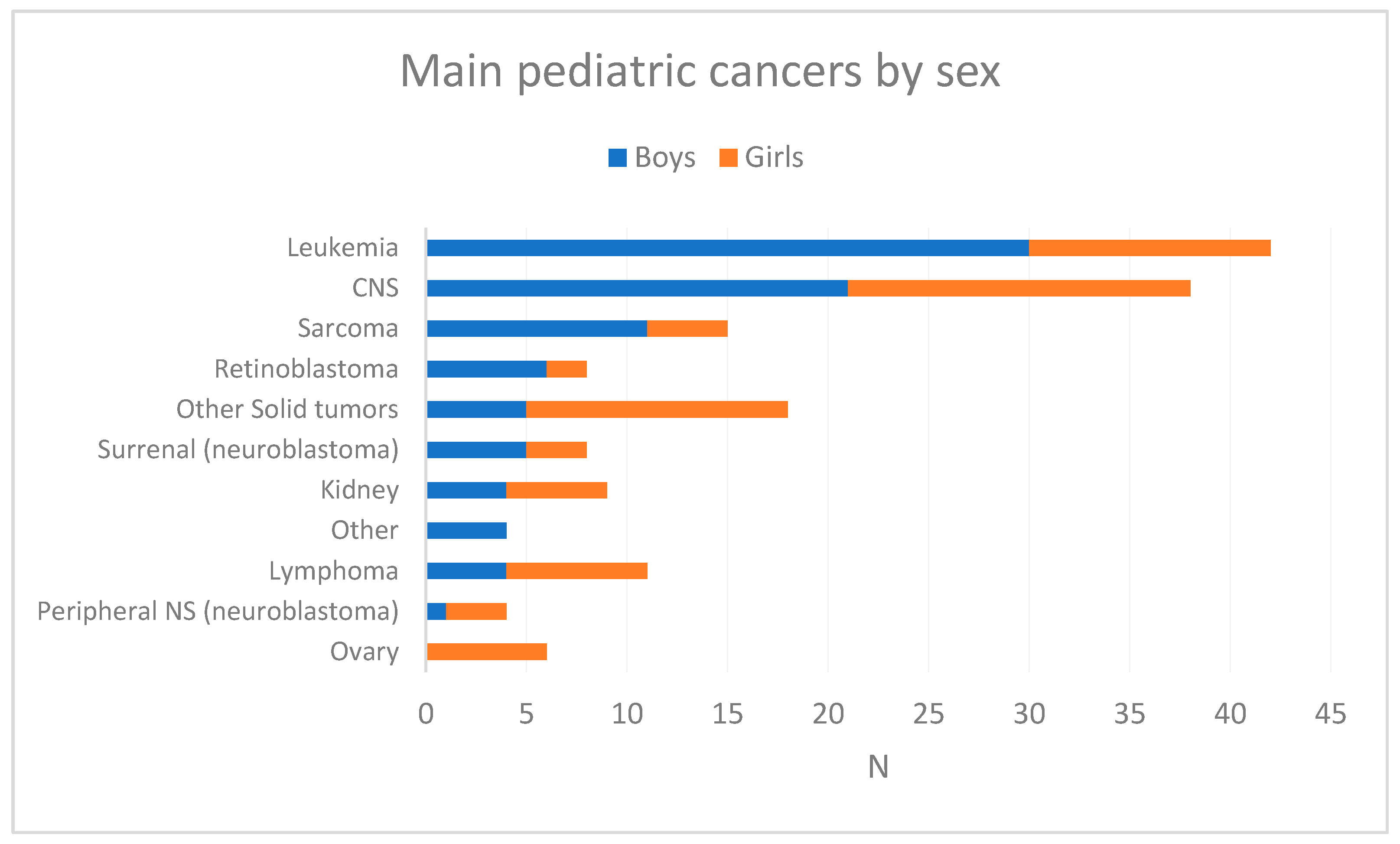
| Type of Malignancy | Number | (%) | Sex Ratio | Incidence Rate * | Median Age at Diagnosis |
|---|---|---|---|---|---|
| MALIGNANT HEMOPATHIES | 57 | 34.8 | 2.0 | 4.9 | |
| Leukemia | 42 | 25.6 | 2.5 | 3.6 | 4.5 |
| Leukemia/Precursor cell lymphoblastic lymphoma | 29 | 17.7 | 1.9 | 2.5 | 5 |
| Acute myeloid leukemia (AML) | 9 | 5.5 | 8.0 | 0.8 | 3 |
| Other leukemias | 4 | 2.4 | 3.0 | 0.3 | - |
| Lymphomas | 11 | 6.7 | 0.6 | 0.9 | 11 |
| Hodgkin’s lymphoma | 9 | 5.5 | 0.5 | 0.8 | 12 |
| Non-H. malignant lymphoma | 2 | 1.2 | 1.0 | 0.2 | - |
| Other hematological malignancies (n < 4 per location) | 4 | 2.4 | - | 0.3 | - |
| SOLID TUMORS | 106 | 64.6 | 1.0 | 9.1 | |
| Central Nervous System | 38 | 23.2 | 1.2 | 3.3 | 4 |
| Sarcomas | 15 | 9.1 | 2.8 | 1.3 | 5 |
| Kidney | 9 | 5.5 | 0.8 | 0.8 | 4 |
| Nephroblastoma | 6 | 3.7 | 0.5 | 0.5 | - |
| Adrenal gland | 8 | 4.9 | 1.7 | 0.7 | 3 |
| Neuroblastoma | 7 | 4.3 | 2.5 | 0.6 | - |
| Peripheral nerves and autonomic nervous system | 4 | 2.4 | 0.3 | 0.6 | 2 |
| Neuroblastoma | 3 | 1.8 | 0.5 | - | |
| Eye and appendages | 8 | 4.9 | 3.0 | 0.3 | 1 |
| Retinoblastoma | 6 | 3.7 | 2.0 | 0.7 | - |
| Ovary | 6 | 3.7 | - | 0.5 | 9.5 |
| Other solid tumors (ST) (n < 4 per location) | 18 | 11.0 | 0.4 | 0.5 | - |
| Unknown primitive | 1 | 0.6 | - | 0.6 | - |
| TOTAL | 164 | 100.0 | 1.3 | 14.1 | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nacher, M.; Wang, Q.; Osei, L.; Faivre, B.; Elenga, N.; Adenis, A.; Deschamps, N.; Drak Alsibai, K. Incidence of Pediatric Cancers in French Guiana: How Does It Compare to Global Estimates? Cancers 2024, 16, 1829. https://doi.org/10.3390/cancers16101829
Nacher M, Wang Q, Osei L, Faivre B, Elenga N, Adenis A, Deschamps N, Drak Alsibai K. Incidence of Pediatric Cancers in French Guiana: How Does It Compare to Global Estimates? Cancers. 2024; 16(10):1829. https://doi.org/10.3390/cancers16101829
Chicago/Turabian StyleNacher, Mathieu, Qiannan Wang, Lindsay Osei, Benjamin Faivre, Narcisse Elenga, Antoine Adenis, Nathalie Deschamps, and Kinan Drak Alsibai. 2024. "Incidence of Pediatric Cancers in French Guiana: How Does It Compare to Global Estimates?" Cancers 16, no. 10: 1829. https://doi.org/10.3390/cancers16101829
APA StyleNacher, M., Wang, Q., Osei, L., Faivre, B., Elenga, N., Adenis, A., Deschamps, N., & Drak Alsibai, K. (2024). Incidence of Pediatric Cancers in French Guiana: How Does It Compare to Global Estimates? Cancers, 16(10), 1829. https://doi.org/10.3390/cancers16101829







