Reconstruction of the Anterior Skull Base Using the Nasoseptal Flap: A Review
Abstract
Simple Summary
Abstract
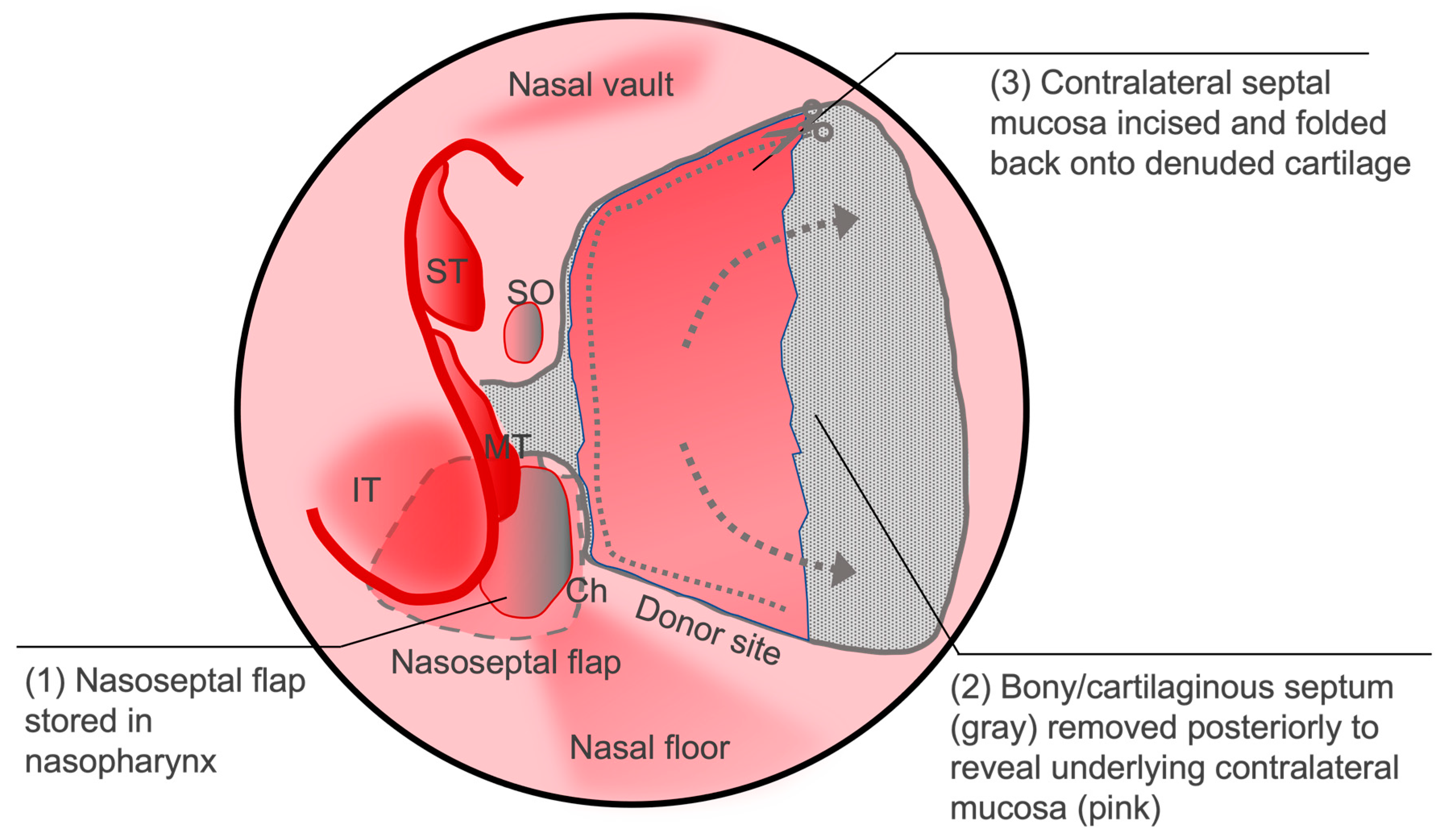
1. Introduction
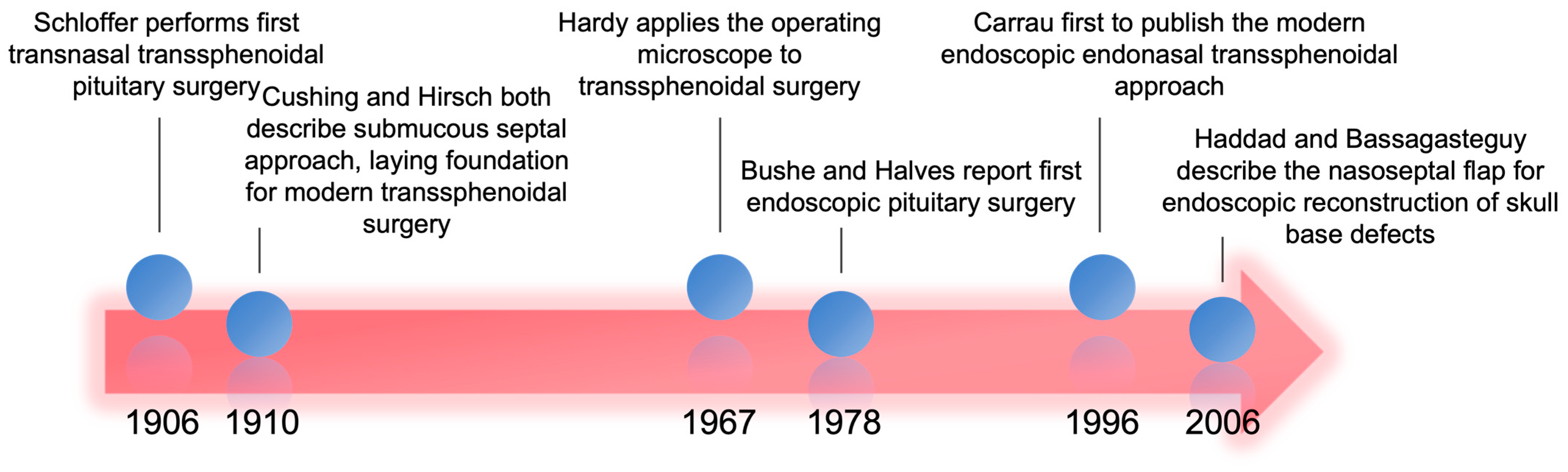
2. History of Anterior Skull Base and Cerebrospinal Fluid Leak Repairs
3. Impact of Nasoseptal Flap Closure on Postoperative CSF Leaks
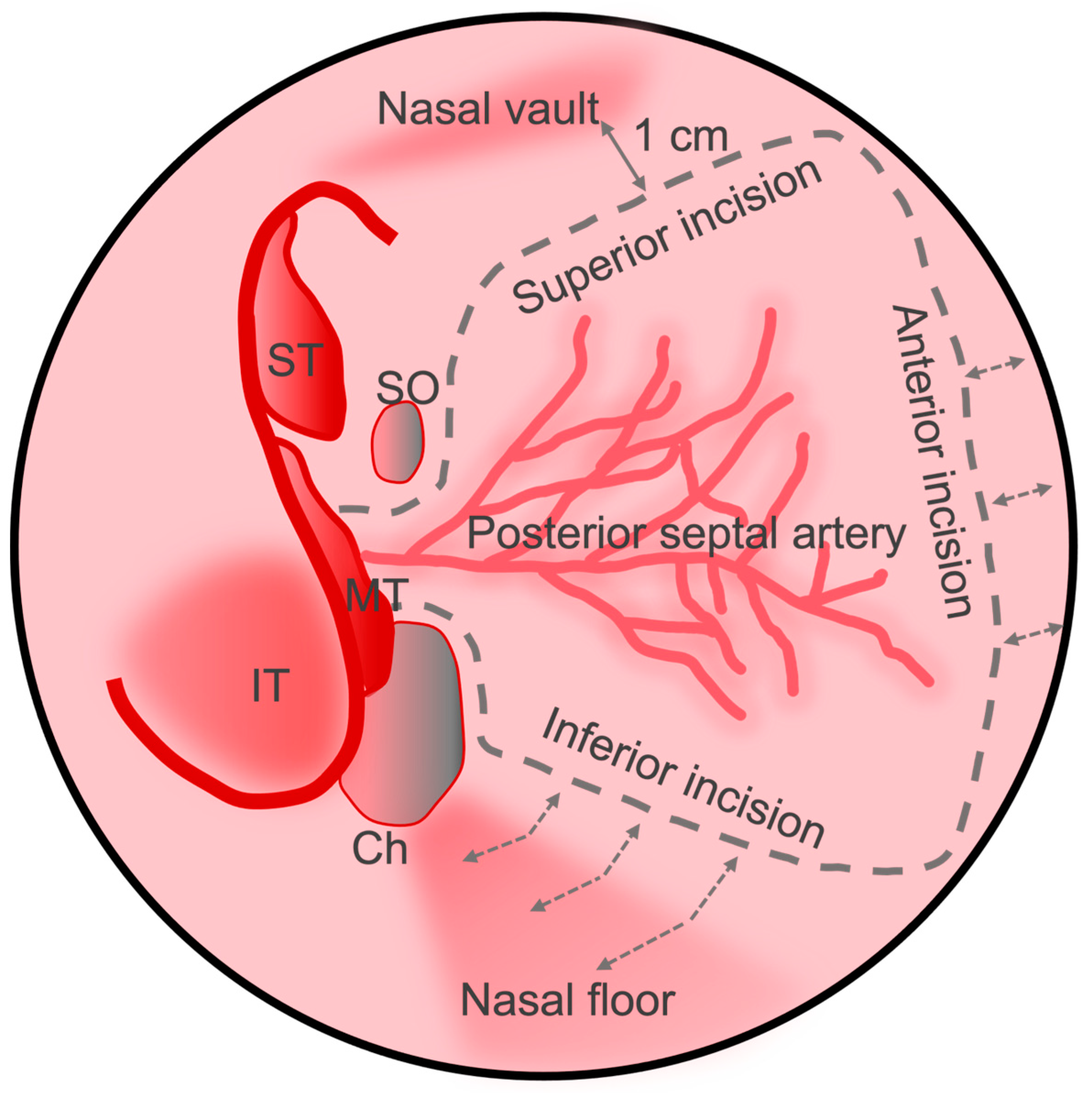
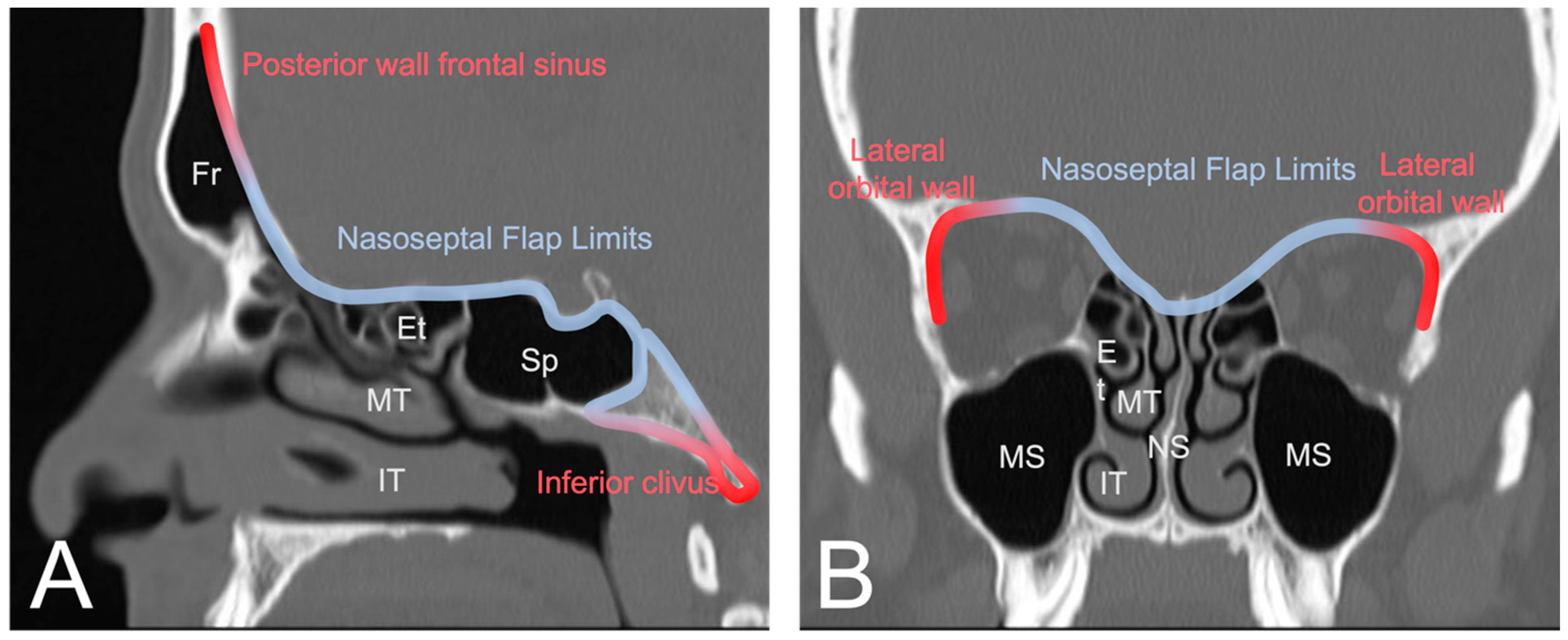
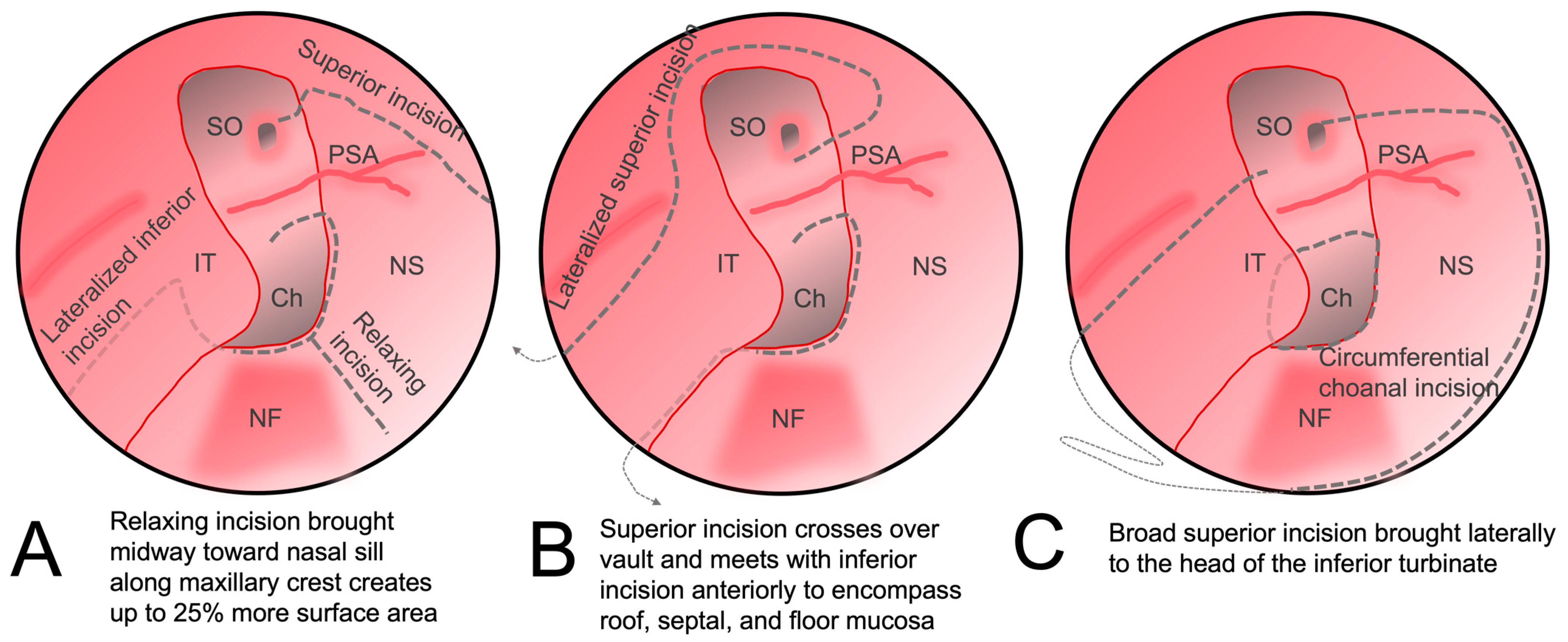
4. Indications, Modifications, and Postoperative Considerations
5. Donor Site Complications
6. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Patel, M.R.; Stadler, M.E.; Snyderman, C.H.; Carrau, R.L.; Kassam, A.B.; Germanwala, A.V.; Gardner, P.; Zanation, A.M. How to Choose? Endoscopic Skull Base Reconstructive Options and Limitations. Skull Base 2010, 20, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Zwagerman, N.T.; Wang, E.W.; Shin, S.S.; Chang, Y.; Fernandez-miranda, J.C.; Snyderman, C.H.; Gardner, P.A. Does Lumbar Drainage Reduce Postoperative Cerebrospinal Fluid Leak after Endoscopic Endonasal Skull Base Surgery? A Prospective, Randomized Controlled Trial. J. Neurosurg. 2019, 131, 1172–1178. [Google Scholar] [CrossRef] [PubMed]
- Bernal-sprekelsen, M.; Rioja, E.; Enseñat, J.; Enriquez, K.; Viscovich, L.; Agredo-lemos, F.E.; Alobid, I. Management of Anterior Skull Base Defect Depending on Its Size and Location. BioMed Res. Int. 2014, 2014, 346873. [Google Scholar] [CrossRef] [PubMed]
- Banks, C.A.; Palmer, J.N.; Chiu, A.G.; Malley, B.W.O.; Woodworth, B.A.; Kennedy, D.W. Endoscopic Closure of CSF Rhinorrhea: 193 Cases over 21 Years. Otolaryngol. Head Neck Surg. 2009, 140, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Ivan, M.E.; Bryan Iorgulescu, J.; El-Sayed, I.; McDermott, M.W.; Parsa, A.T.; Pletcher, S.D.; Jahangiri, A.; Wagner, J.; Aghi, M.K. Risk Factors for Postoperative Cerebrospinal Fluid Leak and Meningitis after Expanded Endoscopic Endonasal Surgery. J. Clin. Neurosci. 2015, 22, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Perkins, S.J.; Gao, R.; Glazer, T.A.; Zhao, C.X.; Basura, G.; Mckean, E.L. Treatment and Prognosis of Inflammatory Pseudotumor of the Skull Base. J. Neurol. Surg. Part B Skull Base 2022, 83, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Yilmazlar, S.; Arslan, E.; Kocaeli, H.; Dogan, S.; Aksoy, K.; Korfali, E.; Doygun, M. Cerebrospinal Fluid Leakage Complicating Skull Base Fractures: Analysis of 81 Cases. Neurosurg. Rev. 2006, 29, 64–71. [Google Scholar] [CrossRef]
- Gump, W.C. Endoscopic Endonasal Repair of Congenital Defects of the Anterior Skull Base: Developmental Considerations and Surgical Outcomes. J. Neurol. Surg. Part B Skull Base 2015, 76, 291–295. [Google Scholar] [CrossRef][Green Version]
- Le, C.; Strong, E.B.; Luu, Q. Management of Anterior Skull Base Cerebrospinal Fluid Leaks. J. Neurol. Surg. Part B Skull Base 2016, 77, 404–411. [Google Scholar] [CrossRef]
- Hadad, G.; Bassagasteguy, L.; Carrau, R.L.; Mataza, J.C.; Kassam, A.; Snyderman, C.H.; Mintz, A. A Novel Reconstructive Technique after Endoscopic Expanded Endonasal Approaches: Vascular Pedicle Nasoseptal Flap. Laryngoscope 2006, 116, 1882–1886. [Google Scholar] [CrossRef]
- El-Sayed, I.H. Nasal Septal Flap Repair of the Skull Base. Handb. Clin. Neurol. 2020, 170, 227–232. [Google Scholar] [PubMed]
- Cohen-Gadol, A.A.; Liu, J.K.; Laws, E.R., Jr. Cushing’s First Case of Transsphenoidal Surgery: The Launch of the Pituitary Surgery Era. J. Neurosurg. 2005, 103, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Carrau, R.L.; Jho, H.; Ko, Y. Transnasal-Transsphenoidal Endoscopic Surgery of the Pituitary Gland. Laryngoscope 1996, 106, 914–918. [Google Scholar] [CrossRef]
- Reyes, C.; Mason, E.; Solares, C.A. Panorama of Reconstruction of Skull Base Defects: From Traditional Open to Endonasal Endoscopic Approaches, from Free Grafts to Microvascular Flaps. Int. Arch. Otorhinolaryngol. 2014, 18, 179–185. [Google Scholar] [CrossRef]
- Nazim, W.M.; Elborady, M.A. Retractorless Brain Surgery: Technical Considerations. Egypt. J. Neurol. Psychiatry Neurosurg. 2021, 57, 98. [Google Scholar] [CrossRef]
- McCormack, B.; Cooper, P.R.; Persky, M.; Rothstein, S. Extracranial Repair of Cerebrospinal Fluid Fistulas: Technique and Results in 37 Patients. Neurosurgery 1990, 27, 412–417. [Google Scholar] [CrossRef]
- Cavallo, L.M.; Somma, T.; Solari, D.; Iannuzzo, G.; Frio, F.; Baiano, C.; Cappabianca, P. Endoscopic Endonasal Transsphenoidal Surgery: History and Evolution. World Neurosurg. 2019, 127, 686–694. [Google Scholar] [CrossRef]
- Liu, J.K.; Das, K.; Weiss, M.H.; Laws, E.R.; Couldwell, W.T. The History and Evolution of Transsphenoidal Surgery. J. Neurosurg. 2001, 95, 1083–1096. [Google Scholar] [CrossRef]
- Kassam, A.; Carrau, R.L.; Snyderman, C.H.; Gardner, P.; Mintz, A. Evolution of Reconstructive Techniques Following Endoscopic Expanded Endonasal Approaches. Neurosurg. Focus 2005, 19, 1–7. [Google Scholar] [CrossRef]
- Horridge, M.; Jesurasa, A.; Olubajo, F.; Mirza, S.; Sinha, S. The Use of the Nasoseptal Flap to Reduce the Rate of Post-Operative Cerebrospinal Fluid Leaks Following Endoscopic Trans-Sphenoidal Surgery for Pituitary Disease. Br. J. Neurosurg. 2013, 27, 739–741. [Google Scholar] [CrossRef]
- Najafabadi, A.H.Z.; Khan, D.Z.; Muskens, I.S. Trends in Cerebrospinal Fluid Leak Rates Following the Extended Endoscopic Endonasal Approach for Anterior Skull Base Meningioma: A Meta-Analysis over the Last 20 Years. Acta Neurochir. 2021, 163, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.J.; Parmar, P.; Sacks, R.; Zanation, A.M. Endoscopic Skull Base Reconstruction of Large Dural Defects: A Systematic Review of Published Evidence. Laryngoscope 2012, 122, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Fraser, S.; Gardner, P.A.; Koutourousiou, M.; Kubik, M.; Fernandez-miranda, J.C.; Snyderman, C.H.; Wang, E.W. Risk Factors Associated with Postoperative Cerebrospinal Fluid Leak after Endoscopic Endonasal Skull Base Surgery. J. Neurosurg. 2018, 128, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- Thorp, B.D.; Sreenath, S.B.; Ebert, C.S.; Zanation, A.M. Endoscopic Skull Base Reconstruction: A Review and Clinical Case Series of 152 Vascularized Flaps Used for Surgical Skull Base Defects in the Setting of Intraoperative Cerebrospinal Fluid Leak. Neurosurg. Focus 2014, 37, E4. [Google Scholar] [CrossRef]
- Sun, I.; Lim, J.X.; Goh, C.P.; Low, S.W.; Kirollos, R.W.; Tan, C.S.; Lwin, S.; Yeo, T.T. Body Mass Index and the Risk of Postoperative Cerebrospinal Fluid Leak Following Transsphenoidal Surgery in an Asian Population. Singap. Med. J. 2018, 59, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Nishioka, H.; Haraoka, J.; Ikeda, Y. Risk Factors of Cerebrospinal Fluid Rhinorrhea Following Transsphenoidal Surgery. Acta Neurochir. 2005, 147, 1163–1166. [Google Scholar] [CrossRef] [PubMed]
- Chabot, J.D.; Patel, C.R.; Hughes, M.A.; Wang, E.W.; Snyderman, C.H.; Gardner, P.A.; Fernandez-miranda, J.C. Nasoseptal Flap Necrosis: A Rare Complication of Endoscopic Endonasal Surgery. J. Neurosurg. 2018, 128, 1463–1472. [Google Scholar] [CrossRef]
- Soudry, E.; Psaltis, A.J.; Lee, K.H.; Vaezafshar, R.; Nayak, J.V.; Hwang, P.H. Complications Associated with the Pedicled Nasoseptal Flap for Skull Base Reconstruction. Laryngoscope 2015, 125, 80–85. [Google Scholar] [CrossRef]
- Chakravarthi, S.; Gonen, L.; Monroy-Sosa, A.; Khalili, S.; Kassam, A. Endoscopic Endonasal Reconstructive Methods to the Anterior Skull Base. Semin. Plast. Surg. 2017, 31, 203–213. [Google Scholar] [CrossRef]
- Sung, K.S.; Lim, J.; Na, M.; Lee, S.; Kim, J.S.; Hong, J.B.; Hong, C.K.; Moon, J.H. Anterior Skull Base Reconstruction Using Nasoseptal Flap: Cadaveric Feasibility Study and Clinical Implication [SevEN-001]. J. Otolaryngol. Head Neck Surg. 2020, 49. [Google Scholar] [CrossRef]
- Pinheiro-Neto, C.D.; Paluzzi, A.; Fernandez-Miranda, J.C.; Scopel, T.F.; Wang, E.W.; Gardner, P.A.; Snyderman, C.H. Extended Dissection of the Septal Flap Pedicle for Ipsilateral Endoscopic Transpterygoid Approaches. Laryngoscope 2014, 124, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro-Neto, C.D.; Peris-Celda, M.; Kenning, T. Extrapolating the Limits of the Nasoseptal Flap with Pedicle Dissection to the Internal Maxillary Artery. Oper. Neurosurg. 2019, 16, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Shastri, K.S.; Leonel, L.C.P.C.; Patel, V.; Charles-pereira, M.; Kenning, T.J.; Peris-celda, M.; Pinheiro-neto, C.D. Lengthening the Nasoseptal Flap Pedicle With Extended Dissection Into the Pterygopalatine Fossa. Laryngoscope 2020, 130, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Bassett, E.; Farag, A.; Iloreta, A.; Farrell, C.; Evans, J.; Rosen, M.; Singh, A.; Nyquist, G. The Extended Nasoseptal Flap for Coverage of Large Cranial Base Defects. Int. Forum Allergy Rhinol. 2016, 6, 1113–1116. [Google Scholar] [CrossRef] [PubMed]
- Mccormick, J.; Allen, M.; Kain, J.J.; Pena-garcia, J.A.; Cho, D.; Riley, K.O.; Woodworth, B.A. Lateral Nasal Wall Extension of the Nasoseptal Flap for Skull-Base and Medial Orbital Wall Defects. Int. Forum Allergy Rhinol. 2019, 9, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Boetto, J.; Labidi, M.; Watanabe, K.; Hanakita, S.; Bouazza, S.; Passeri, T.; Bernat, A.-L.; Froelich, S. Combined Nasoseptal and Inferior Turbinate Flap for Reconstruction of Large Skull Base Defect After Expanded Endonasal Approach: Operative Technique. Oper. Neurosurg. 2019, 16, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Alromaih, S.; Yaghmoor, F.; Alarifi, I.; Alsaleh, S. Graft-Extended Nasoseptal Flap for Endoscopic Anterior Skull Base Reconstruction: A Novel Technique. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 1344–1347. [Google Scholar] [CrossRef]
- Luginbuhl, A.J.; Campbell, P.G.; Evans, J.; Rosen, M. Endoscopic Repair of High-Flow Cranial Base Defects Using a Bilayer Button. Laryngoscope 2010, 120, 876–880. [Google Scholar] [CrossRef]
- Khatiwala, R.V.; Shastri, K.S.; Peris-Celda, M.; Kenning, T.; Pinheiro-Neto, C.D. Endoscopic Endonasal Reconstruction of High-Flow Cerebrospinal Fluid Leak with Fascia Lata “Button” Graft and Nasoseptal Flap: Surgical Technique and Case Series. J. Neurol. Surg. Part B Skull Base 2020, 81, 645–650. [Google Scholar] [CrossRef]
- Liu, J.K.; Schmidt, R.F.; Choudhry, O.J.; Shukla, P.A.; Eloy, J.A. Surgical Nuances for Nasoseptal Flap Reconstruction of Cranial Base Defects with High-Flow Cerebrospinal Fluid Leaks after Endoscopic Skull Base Surgery. Neurosurg. Focus 2012, 32, E7. [Google Scholar] [CrossRef]
- Shah, R.N.; Surowitz, J.B.; Patel, M.R.; Huang, B.Y.; Snyderman, C.H.; Carrau, R.L.; Kassam, A.B.; Germanwala, A.V.; Zanation, A.M. Endoscopic Pedicled Nasoseptal Flap Reconstruction for Pediatric Skull Base Defects. Laryngoscope 2009, 119, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Chivukula, S.; Koutourousiou, M.; Snyderman, C.H.; Fernandez-Miranda, J.C.; Gardner, P.A.; Tyler-Kabara, E.C. Endoscopic Endonasal Skull Base Surgery in the Pediatric Population. J. Neurosurg. Pediatr. 2013, 11, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Ben-Ari, O.; Wengier, A.; Ringel, B.; Carmel Neiderman, N.N.; Ram, Z.; Margalit, N.; Fliss, D.M.; Abergel, A. Nasoseptal Flap for Skull Base Reconstruction in Children. J. Neurol. Surg. Part B Skull Base 2018, 79, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Eden, J.K.; Böttcher, A.; Betz, C.S. Nasoseptal Flap for Skull Base Reconstruction in a Three-Year-Old Child With Nasofrontal Meningoencephalocele. Ear Nose Throat J. 2023, 102, NP149–NP153. [Google Scholar] [CrossRef] [PubMed]
- Kuan, E.C.; Trent, M.S.; Luu, N.N.; Kohanski, M.A.; Tong, C.C.; O’Malley, B.W., Jr.; Adappa, N.D.; Palmer, J.N. Preventing Restenosis of Marsupialized Rathke Cleft Cysts Using a Nasoseptal Flap Lining. Laryngoscope 2019, 129, 2258–2261. [Google Scholar] [CrossRef] [PubMed]
- Georgalas, C.; Kania, R.; Guichard, J.-P.; Sauvaget, E.; Tran Ba Huy, P.; Herman, P. Endoscopic Transsphenoidal Surgery for Cholesterol Granulomas Involving the Petrous Apex. Clin. Otolaryngol. 2008, 33, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Baban, M.I.; Shareef, D.J.; Hadi, S.J.; Shawkat, A.; Castelnuovo, P. Outcomes of Transnasal Endoscopic Repair of Cerebrospinal Fluid Leaks: A Prospective Cohort Study. Egypt. J. Otolaryngol. 2022, 38, 61. [Google Scholar] [CrossRef]
- Castle-Kirszbaum, M.; Wang, Y.Y.; King, J.; Uren, B.; Dixon, B.; Zhao, Y.C.; Lim, K.Z.; Goldschlager, T. Patient Wellbeing and Quality of Life after Nasoseptal Flap Closure for Endoscopic Skull Base Reconstruction. J. Clin. Neurosci. 2020, 74, 87–92. [Google Scholar] [CrossRef]
- Carmel Neiderman, N.N.; Wengier, A.; Dominsky, O.; Ringel, B.; Warshavsky, A.; Horowitz, G.; Baran, T.Z.; Ram, Z.; Grossman, R.; Fliss, D.M.; et al. A Prospective Evaluation of Quality of Life in Patients Undergoing Extended Endoscopic Endonasal Surgery for Benign Pituitary Gland Lesion. J. Neurol. Surg. Part B Skull Base 2022, 83, E386–E394. [Google Scholar] [CrossRef]
- Riley, C.A.; Tabaee, A.; Conley, L.; Amine, M.; Soneru, C.P.; Anand, V.K.; Schwartz, T.H. Long-Term Sinonasal Outcomes after Endoscopic Skull Base Surgery with Nasoseptal Flap Reconstruction. Laryngoscope 2019, 129, 1035–1040. [Google Scholar] [CrossRef]
- Awad, A.J.; Mohyeldin, A.; El-Sayed, I.H.; Aghi, M.K. Sinonasal Morbidity Following Endoscopic Endonasal Skull Base Surgery. Clin. Neurol. Neurosurg. 2015, 130, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Kimple, A.J.; Leight, W.D.; Wheless, S.A.; Zanation, A.M. Reducing Nasal Morbidity after Skull Base Reconstruction with the Nasoseptal Flap: Free Middle Turbinate Mucosal Grafts. Laryngoscope 2012, 122, 1920–1924. [Google Scholar] [CrossRef]
- Rezende, G.L.; Neto, O.R.M.; Kückelhaus, S.A.S. Morbidity in the Postoperative Follow-up of Endoscopic Anterior Skull Base Surgery. Braz. J. Otorhinolaryngol. 2021, 87, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Caicedo-Granados, E.; Carrau, R.; Snyderman, C.H.; Prevedello, D.; Fernandez-Miranda, J.; Gardner, P.; Kassam, A. Reverse Rotation Flap for Reconstruction of Donor Site after Vascular Pedicled Nasoseptal Flap in Skull Base Surgery. Laryngoscope 2010, 120, 1550–1552. [Google Scholar] [CrossRef] [PubMed]
- Kasemsiri, P.; Carrau, R.L.; Otto, B.A.; Tang, I.P.; Prevedello, D.M.; Muto, J.; Caicedo, E. Reconstruction of the Pedicled Nasoseptal Flap Donor Site with a Contralateral Reverse Rotation Flap: Technical Modifications and Outcomes. Laryngoscope 2013, 123, 2601–2604. [Google Scholar] [CrossRef] [PubMed]
- Strober, W.A.; Valappil, B.; Snyderman, C.H. Impact of Reverse Septal Flap on Morbidity of Nasoseptal Flap Reconstruction of Skull Base Defects. Am. J. Rhinol. Allergy 2023, 37, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Mccoul, E.D.; Patel, A.S.; Bedrosian, J.C.; Anand, V.K.; Schwartz, T.H. Intranasal Cross-Sectional Area and Quality of Life Changes Following Endoscopic Transsphenoidal Skull Base Surgery. Int. Forum Allergy Rhinol. 2015, 5, 1124–1128. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.Y.; Nam, D.-H.; Kong, D.-S.; Lee, S.H.; Noh, Y.; Jung, Y.G.; Kim, H.Y.; Chung, S.-K.; Lee, K.E.; Hong, S.D. Extended Apporach or Usage of Nasoseptal Flap Is a Risk Factor for Olfactory Dysfunction after Endoscopic Anterior Skullbase Surgery. Rhinology 2020, 58, 574–580. [Google Scholar]
- Harvey, R.J.; Winder, M.; Davidson, A.; Steel, T.; Nalavenkata, S.; Mrad, N.; Bokhari, A.; Barham, H.; Knisely, A. The Olfactory Strip and Its Preservation in Endoscopic Pituitary Surgery Maintains Smell and Sinonasal Function. J. Neurol. Surg. Part B Skull Base 2015, 76, 464–470. [Google Scholar] [CrossRef]
- Rowan, N.R.; Wang, E.W.; Gardner, P.A.; Fernandez-Miranda, J.C.; Snyderman, C.H. Nasal Deformities Following Nasoseptal Flap Reconstruction of Skull Base Defects. J. Neurol. Surg. Part B Skull Base 2015, 77, 14–18. [Google Scholar] [CrossRef][Green Version]
- Racette, S.; Tekumalla, S.; Agarwal, A.; Curry, J.; Beahm, D.D. Anterior Skull Base Reconstruction. Otolaryngol. Clin. N. Am. 2023, 56, 727–739. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Yang, Z.; Liu, P. Strategy of Skull Base Reconstruction after Endoscopic Transnasal Pituitary Adenoma Resection. Front. Surg. 2023, 10, 1130660. [Google Scholar] [CrossRef] [PubMed]
- Chaskes, M.B.; Khoury, T.; Chitguppi, C.; Lavergne, P.; Nyquist, G.G.; Rabinowitz, M.R.; Rosen, M.R.; Evans, J.J. A Single Layer Synthetic Dural Substitute Inlay Is an Effective Sellar Reconstruction Technique in Endoscopic Transsphenoidal Pituitary Surgery. J. Neurol. Surg. Part B Skull Base 2022, 83, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Chaskes, M.B.; Barton, B.; Bs, T.M.; Rabinowitz, M.R.; Rosen, M.R.; Flanders, A.; Farrell, C.; Evans, J.J. An Algorithm for Sellar Reconstruction Following Endoscopic Transsphenoidal Surgery for Pituitary Adenoma: A Review of 582 Cases. Int. Forum Allergy Rhinol. 2022, 12, 1120–1130. [Google Scholar] [CrossRef] [PubMed]
- Chaskes, M.B.; Fastenberg, J.H.; Vimawala, S.; Nyquist, G.F.; Rabinowitz, M.R.; Chitguppi, C.; Falls, M.; Garzon-Muvdi, T.; Rosen, M.R.; Evans, J.J. A Simple Onlay Sellar Reconstruction Does Not Increase the Risk of Postoperative Cerebrospinal Fluid Leak in Well-Selected Patients. J. Neurol. Surg. Part B Skull Base 2021, 82, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Peris-celda, M.; Chaskes, M.; Lee, D.D.; Kenning, T.J.; Pinheiro-neto, C.D. Optimizing Sellar Reconstruction After Pituitary Surgery with Free Mucosal Graft: Results from the First 50 Consecutive Patients. World Neurosurg. 2017, 101, 180–185. [Google Scholar] [CrossRef]
- Jeong, C.Y.; Cho, J.H.; Park, Y.J.; Kim, S.W.; Park, J.S.; Basurrah, M.A.; Kim, D.H.; Kim, S.W. Differences in the Predicted Nasoseptal Flap Length among Races: A Propensity Score Matching Analysis. PLoS ONE 2023, 18, e0283140. [Google Scholar] [CrossRef]
- Gu, D. Radioanatomical Study of the Skull Base and Septum in Chinese—Implications for Using the HBF for Endoscopic Skull Base Reconstruction. Oxid. Med. Cell. Longev. 2022, 2022, 9940239. [Google Scholar] [CrossRef]
- Kayastha, D.; Wiznia, D.; Manes, R.P.; Omay, S.B.; Khoury, T.; Rimmer, R. 3D Printing for Virtual Surgical Planning of Nasoseptal Flap Skull-Base Reconstruction: A Proof-of-Concept Study. Int. Forum Allergy Rhinol. 2023, 13, 2073–2075. [Google Scholar] [CrossRef]
| Location [3] | Cribriform plate | ||
| Ethmoidal roof | |||
| Sphenoid | |||
| Frontal sinus | |||
| Sella turcica | |||
| Clivus | |||
| Size [2] | <1 cm | ||
| >1 cm | |||
| Etiology [3,4,5,6,7,8,9] | Iatrogenic | Planned | |
| Accidental | Cribriform plate/fovea ethmoidalis | ||
| Frontal | |||
| Sphenoid | |||
| Neoplastic | Meningioma, olfactory fossa, planum sphenoidale, tuberculum sellae | ||
| Craniopharyngeoma | |||
| Chordoma | |||
| Esthesioneuroblastoma | |||
| Sinonasal carcinoma | |||
| Sarcoma, chondrosarcoma | |||
| Benign | Osteoma | ||
| Inverted papilloma | |||
| Infectious/ Inflammatory | Invasive fungal sinusitis | ||
| Inflammatory pseudotumor | |||
| Osteomyelitis | |||
| Mucocele | |||
| Trauma | Sphenoid | ||
| Frontal | |||
| Cribriform plate/fovea ethmoidalis | |||
| Spontaneous | Congenital | ||
| Idiopathic | Benign intracranial hypertension | ||
| Connective tissue disorder | |||
| CSF leak [1,2] | Low | Less than 1 cm dural defect, CSF weeping | |
| High | Greater than 1 cm dural defect, involvement of ventricle or cistern | ||
| After endonasal endoscopic skull base surgery [23] |
| Longer length of stay |
| Staged procedure |
| Preoperative hydrocephalus |
| Closure with graft (instead of vascularized flap) |
| Prior endoscopic skull base surgery [26] |
| Prior radiotherapy [26] |
| After closure with nasoseptal flap [5] |
| Abnormal BMI (<18.5 or >25) |
| Age > 65 |
| Intraoperative CSF leak |
| Complex closure with combined open craniofacial approach |
| Surgeon experience [1] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Werner, M.T.; Yeoh, D.; Fastenberg, J.H.; Chaskes, M.B.; Pollack, A.Z.; Boockvar, J.A.; Langer, D.J.; D’Amico, R.S.; Ellis, J.A.; Miles, B.A.; et al. Reconstruction of the Anterior Skull Base Using the Nasoseptal Flap: A Review. Cancers 2024, 16, 169. https://doi.org/10.3390/cancers16010169
Werner MT, Yeoh D, Fastenberg JH, Chaskes MB, Pollack AZ, Boockvar JA, Langer DJ, D’Amico RS, Ellis JA, Miles BA, et al. Reconstruction of the Anterior Skull Base Using the Nasoseptal Flap: A Review. Cancers. 2024; 16(1):169. https://doi.org/10.3390/cancers16010169
Chicago/Turabian StyleWerner, Michael T., Desmond Yeoh, Judd H. Fastenberg, Mark B. Chaskes, Aron Z. Pollack, John A. Boockvar, David J. Langer, Randy S. D’Amico, Jason A. Ellis, Brett A. Miles, and et al. 2024. "Reconstruction of the Anterior Skull Base Using the Nasoseptal Flap: A Review" Cancers 16, no. 1: 169. https://doi.org/10.3390/cancers16010169
APA StyleWerner, M. T., Yeoh, D., Fastenberg, J. H., Chaskes, M. B., Pollack, A. Z., Boockvar, J. A., Langer, D. J., D’Amico, R. S., Ellis, J. A., Miles, B. A., & Tong, C. C. L. (2024). Reconstruction of the Anterior Skull Base Using the Nasoseptal Flap: A Review. Cancers, 16(1), 169. https://doi.org/10.3390/cancers16010169







