Short- and Long-Term Survival among Elderly Colorectal Cancer Patients in Finland, 2006–2015: A Nationwide Population-Based Registry Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Variables
2.3. Statistical Analysis
2.4. Permissions
3. Results
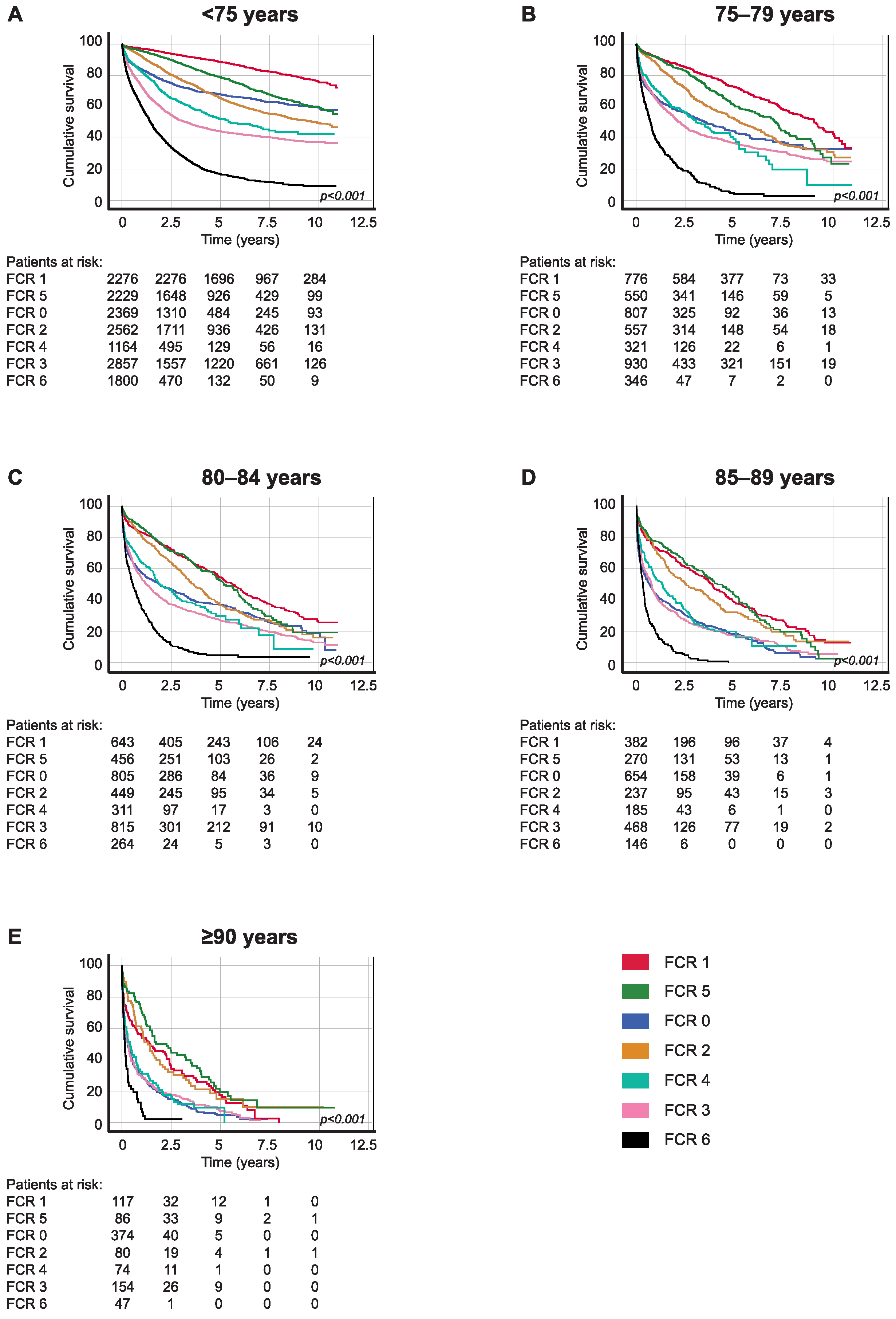
3.1. Five-Year Overall Survival Based on FCR Group
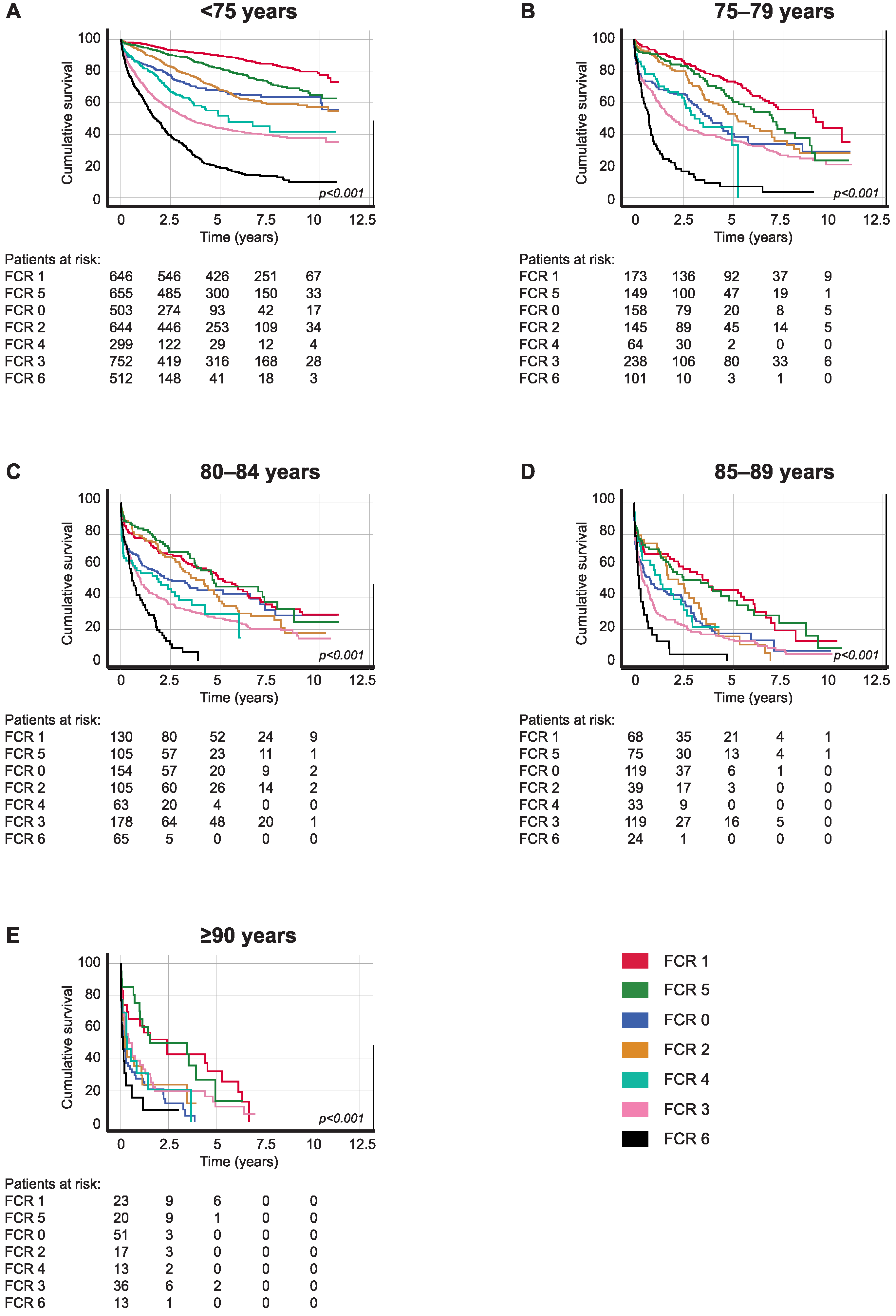
3.2. Five-Year Overall Survival Based on Tumor Location
3.3. Thirty-Day and One-Year Postoperative Overall Survival
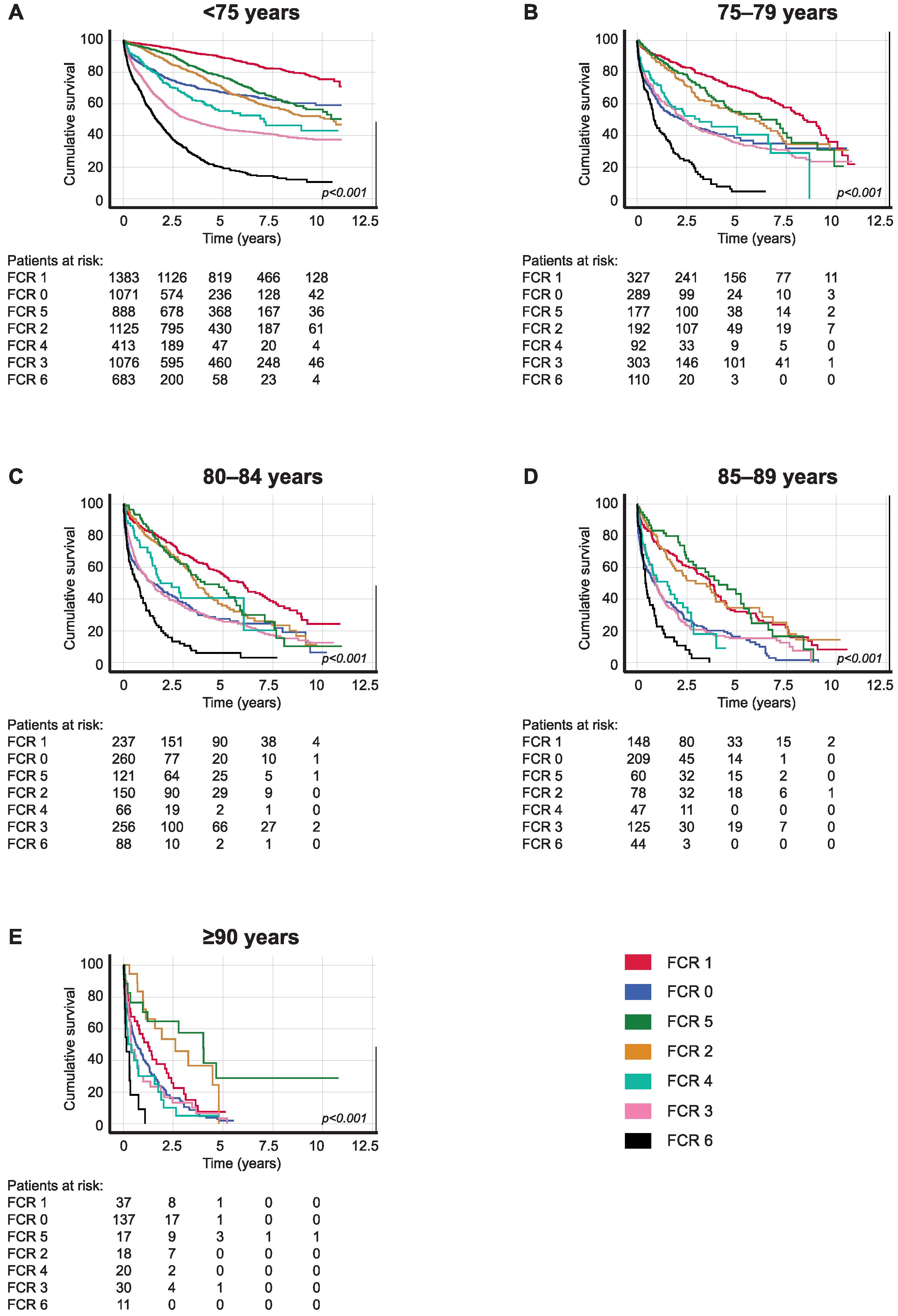
3.4. Five-Year Disease-Specific Survival Based on FCR Groups
3.5. Five-Year Disease-Specific Survival among FCR Groups Based on Tumor Location
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nordic Burden of Disease Collaborators. Life Expectancy and Disease Burden in the Nordic Countries: Results from the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet Public Health 2019, 4, e658–e669. [Google Scholar] [CrossRef] [PubMed]
- Cancer Registry. Available online: https://cancerregistry.fi/statistics/cancer-statistics/ (accessed on 26 January 2023).
- Annual Report on Cancer in Finland, Cancer in Finland 2020 Report. Available online: https://cancerregistry.fi/reports-and-publications/annual-report-on-cancer-in-finland/ (accessed on 26 January 2023).
- Dekker, J.W.T.; van den Broek, C.B.M.; Bastiaannet, E.; van de Geest, L.G.M.; Tollenaar, R.A.E.M.; Liefers, G.J. Importance of the First Postoperative Year in the Prognosis of Elderly Colorectal Cancer Patients. Ann. Surg. Oncol. 2011, 18, 1533–1539. [Google Scholar] [CrossRef] [PubMed]
- Aquina, C.T.; Mohile, S.G.; Tejani, M.A.; Becerra, A.Z.; Xu, Z.; Hensley, B.J.; Arsalani-Zadeh, R.; Boscoe, F.P.; Schymura, M.J.; Noyes, K.; et al. The Impact of Age on Complications, Survival, and Cause of Death Following Colon Cancer Surgery. Br. J. Cancer 2017, 116, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Høydahl, Ø.; Edna, T.-H.; Xanthoulis, A.; Lydersen, S.; Endreseth, B.H. Octogenarian Patients with Colon Cancer—Postoperative Morbidity and Mortality Are the Major Challenges. BMC Cancer 2022, 22, 302. [Google Scholar] [CrossRef] [PubMed]
- Nitsche, U.; Späth, C.; Müller, T.C.; Maak, M.; Janssen, K.-P.; Wilhelm, D.; Kleeff, J.; Bader, F.G. Colorectal Cancer Surgery Remains Effective with Rising Patient Age. Int. J. Color. Dis. 2014, 29, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Niemeläinen, S.; Huhtala, H.; Andersen, J.; Ehrlich, A.; Haukijärvi, E.; Koikkalainen, S.; Koskensalo, S.; Kössi, J.; Mattila, A.; Pinta, T.; et al. The Clinical Frailty Scale Is a Useful Tool for Predicting Postoperative Complications Following Elective Colon Cancer Surgery at the Age of 80 Years and above: A Prospective, Multicentre Observational Study. Color. Dis. 2021, 23, 1824–1836. [Google Scholar] [CrossRef] [PubMed]
- Olenius, T.; Koskenvuo, L.; Koskensalo, S.; Lepistö, A.; Böckelman, C. Long-Term Survival among Colorectal Cancer Patients in Finland, 1991–2015: A Nationwide Population-Based Registry Study. BMC Cancer 2022, 22, 356. [Google Scholar] [CrossRef]
- Leinonen, M.K.; Miettinen, J.; Heikkinen, S.; Pitkäniemi, J.; Malila, N. Quality Measures of the Population-Based Finnish Cancer Registry Indicate Sound Data Quality for Solid Malignant Tumours. Eur. J. Cancer 2017, 77, 31–39. [Google Scholar] [CrossRef]
- Lunkka, P.; Malila, N.; Ryynänen, H.; Heikkinen, S.; Sallinen, V.; Koskenvuo, L. Accuracy of Finnish Cancer Registry Colorectal Cancer Data: A Comparison between Registry Data and Clinical Records. Scand. J. Gastroenterol. 2021, 56, 247–251. [Google Scholar] [CrossRef]
- Zhang, L.; Li, Q.; Hu, C.; Zhang, Z.; She, J.; Shi, F. Real-World Analysis of Survival Benefit of Surgery and Adjuvant Therapy in Elderly Patients with Colorectal Cancer. Sci. Rep. 2023, 13, 14866. [Google Scholar] [CrossRef]
- Turri, G.; Caliskan, G.; Conti, C.; Martinelli, L.; De Giulio, E.; Ruzzenente, A.; Guglielmi, A.; Verlato, G.; Pedrazzani, C. Impact of Age and Comorbidities on Short- and Long-Term Outcomes of Patients Undergoing Surgery for Colorectal Cancer. Front. Oncol. 2022, 12, 959650. [Google Scholar] [CrossRef] [PubMed]
- Mege, D.; Manceau, G.; Beyer, L.; Bridoux, V.; Lakkis, Z.; Venara, A.; Voron, T.; de’Angelis, N.; Abdalla, S.; Sielezneff, I.; et al. Right-Sided vs. Left-Sided Obstructing Colonic Cancer: Results of a Multicenter Study of the French Surgical Association in 2325 Patients and Literature Review. Int. J. Color. Dis. 2019, 34, 1021–1032. [Google Scholar] [CrossRef] [PubMed]
- Jess, P.; Hansen, I.O.; Gamborg, M.; Jess, T. A Nationwide Danish Cohort Study Challenging the Categorisation into Right-Sided and Left-Sided Colon Cancer. BMJ Open 2013, 3, e002608. [Google Scholar] [CrossRef] [PubMed]
- Mangone, L.; Pinto, C.; Mancuso, P.; Ottone, M.; Bisceglia, I.; Chiaranda, G.; Michiara, M.; Vicentini, M.; Carrozzi, G.; Ferretti, S.; et al. Colon Cancer Survival Differs from Right Side to Left Side and Lymph Node Harvest Number Matter. BMC Public Health 2021, 21, 906. [Google Scholar] [CrossRef] [PubMed]
- Kasi, P.M.; Shahjehan, F.; Cochuyt, J.J.; Li, Z.; Colibaseanu, D.T.; Merchea, A. Rising Proportion of Young Individuals With Rectal and Colon Cancer. Clin. Color. Cancer 2019, 18, e87–e95. [Google Scholar] [CrossRef]
- Warschkow, R.; Sulz, M.C.; Marti, L.; Tarantino, I.; Schmied, B.M.; Cerny, T.; Güller, U. Better Survival in Right-Sided versus Left-Sided Stage I–III Colon Cancer Patients. BMC Cancer 2016, 16, 554. [Google Scholar] [CrossRef]
- Brenner, H.; Hoffmeister, M.; Arndt, V.; Haug, U. Gender Differences in Colorectal Cancer: Implications for Age at Initiation of Screening. Br. J. Cancer 2007, 96, 828–831. [Google Scholar] [CrossRef]
- Koskenvuo, L.; Malila, N.; Pitkäniemi, J.; Miettinen, J.; Heikkinen, S.; Sallinen, V. Sex Differences in Faecal Occult Blood Test Screening for Colorectal Cancer. Br. J. Surg. 2019, 106, 436–447. [Google Scholar] [CrossRef]
- Sonal, S.; Qwaider, Y.Z.; Boudreau, C.; Kunitake, H.; Goldstone, R.N.; Bordeianou, L.G.; Cauley, C.E.; Francone, T.D.; Ricciardi, R.; Berger, D.L. Association of Age with Outcomes in Locally Advanced Rectal Cancer Treated with Neoadjuvant Therapy Followed by Surgery. Am. J. Surg. 2023, 225, 1029–1035. [Google Scholar] [CrossRef]
- Duraes, L.C.; Steele, S.R.; Valente, M.A.; Lavryk, O.A.; Connelly, T.M.; Kessler, H. Right Colon, Left Colon, and Rectal Cancer Have Different Oncologic and Quality of Life Outcomes. Int. J. Color. Dis. 2022, 37, 939–948. [Google Scholar] [CrossRef]
- Devoto, L.; Celentano, V.; Cohen, R.; Khan, J.; Chand, M. Colorectal Cancer Surgery in the Very Elderly Patient: A Systematic Review of Laparoscopic versus Open Colorectal Resection. Int. J. Color. Dis. 2017, 32, 1237–1242. [Google Scholar] [CrossRef] [PubMed]
- Govaert, J.A.; Govaert, M.J.P.M.; Fiocco, M.; van Dijk, W.A.; Tollenaar, R.A.E.M.; Wouters, M.W.J.M.; Dutch Value Based Healthcare Study Group. Hospital Costs of Colorectal Cancer Surgery for the Oldest Old: A Dutch Population-Based Study. J. Surg. Oncol. 2016, 114, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Doat, S.; Thiébaut, A.; Samson, S.; Ricordeau, P.; Guillemot, D.; Mitry, E. Elderly Patients with Colorectal Cancer: Treatment Modalities and Survival in France. National Data from the ThInDiT Cohort Study. Eur. J. Cancer 2014, 50, 1276–1283. [Google Scholar] [CrossRef] [PubMed]
- Serra-Rexach, J.A.; Jimenez, A.B.; García-Alhambra, M.A.; Pla, R.; Vidán, M.; Rodríguez, P.; Ortiz, J.; García-Alfonso, P.; Martín, M. Differences in the Therapeutic Approach to Colorectal Cancer in Young and Elderly Patients. Oncologist 2012, 17, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- McGillicuddy, E.A.; Schuster, K.M.; Davis, K.A.; Longo, W.E. Factors Predicting Morbidity and Mortality in Emergency Colorectal Procedures in Elderly Patients. Arch. Surg. 2009, 144, 1157–1162. [Google Scholar] [CrossRef] [PubMed]
- Banysch, M.; Akkaya, T.; Gurenko, P.; Papadakis, M.; Heuer, T.; Kasim, E.; Tavarajah, S.; Kaiser, G.M. Surgery for Colorectal Cancer in Elderly Patients: Is There Such a Thing as Being Too Old? Il G. Chir.-J. Ital. Surg. Assoc. 2018, 39, 355–362. [Google Scholar]
- Niemeläinen, S.; Huhtala, H.; Ehrlich, A.; Kössi, J.; Jämsen, E.; Hyöty, M. Risk Factors of Short-Term Survival in the Aged in Elective Colon Cancer Surgery: A Population-Based Study. Int. J. Color. Dis. 2020, 35, 307–315. [Google Scholar] [CrossRef]
- Yukawa, N.; Aoyama, T.; Sato, T.; Oshima, T.; Yoshikawa, T.; Rino, Y.; Masuda, M. Evaluation of Safety, Feasibility and the Long-Term Outcomes of Colorectomy for Colorectal Adenocarcinoma in Patients Older than 80 Years of Age. Mol. Clin. Oncol. 2017, 7, 564–568. [Google Scholar] [CrossRef][Green Version]
- Church, S.; Rogers, E.; Rockwood, K.; Theou, O. A Scoping Review of the Clinical Frailty Scale. BMC Geriatr. 2020, 20, 393. [Google Scholar] [CrossRef]
- De Geer, L.; Fredrikson, M.; Tibblin, A.O. Frailty Predicts 30-Day Mortality in Intensive Care Patients: A Prospective Prediction Study. Eur. J. Anaesthesiol. EJA 2020, 37, 1058. [Google Scholar] [CrossRef]
- Ommundsen, N.; Wyller, T.B.; Nesbakken, A.; Jordhøy, M.S.; Bakka, A.; Skovlund, E.; Rostoft, S. Frailty Is an Independent Predictor of Survival in Older Patients with Colorectal Cancer. Oncologist 2014, 19, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Kristjansson, S.R.; Nesbakken, A.; Jordhøy, M.S.; Skovlund, E.; Audisio, R.A.; Johannessen, H.-O.; Bakka, A.; Wyller, T.B. Comprehensive Geriatric Assessment Can Predict Complications in Elderly Patients after Elective Surgery for Colorectal Cancer: A Prospective Observational Cohort Study. Crit. Rev. Oncol. Hematol. 2010, 76, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Cancer Registry. Available online: https://cancerregistry.fi/cancer-information-notification/ (accessed on 12 February 2023).

| Patient Characteristics | ||||||
|---|---|---|---|---|---|---|
| <75 Years Old | ≥75 Years Old | 75–79 Years Old | 80–84 Years Old | 85–89 Years Old | ≥90 Years Old | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| All | 15,782 | 11,306 | 4287 | 3745 | 2342 | 932 |
| Gender | ||||||
| Male | 9035 (57.2) | 5194 (45.9) | 2302 (53.7) | 1732 (46.2) | 877 (37.4) | 283 (30.4) |
| Female | 6747 (42.8) | 6112 (54.1) | 1985 (46.3) | 2013 (53.8) | 1465 (62.6) | 649 (69.6) |
| FCR classification 1 | ||||||
| 0 | 2375 (15.1) | 2641 (23.4) | 807 (18.8) | 803 (21.5) | 654 (27.9) | 374 (40.1) |
| 1 | 2782 (17.6) | 1919 (17.0) | 776 (18.1) | 644 (17.2) | 382 (16.3) | 117 (12.6) |
| 2 | 2565 (16.3) | 1321 (11.7) | 557 (13.0) | 449 (12.0) | 237 (10.1) | 80 (8.6) |
| 3 | 2859 (18.1) | 2367 (20.9) | 930 (21.7) | 815 (21.8) | 468 (20.0) | 154 (16.5) |
| 4 | 1166 (7.4) | 891 (7.9) | 321 (7.5) | 311 (8.3) | 185 (7.9) | 74 (7.9) |
| 5 | 2233 (14.1) | 1362 (12.0) | 550 (12.8) | 456 (12.2) | 270 (11.5) | 86 (9.2) |
| 6 | 1802 (11.4) | 803 (7.1) | 346 (8.1) | 264 (7.0) | 146 (6.3) | 47 (5.1) |
| Tumor location | ||||||
| Right colon | 4228 (26.8) | 4160 (36.8) | 1476 (34.4) | 1433 (38.3) | 914 (39.0) | 337 (36.1) |
| Left colon | 4016 (25.5) | 2478 (21.9) | 1028 (24.0) | 800 (21.3) | 477 (20.4) | 173 (18.6) |
| Rectum | 6651 (42.1) | 3650 (32.3) | 1490 (34.8) | 1179 (31.5) | 711 (30.4) | 270 (29.0) |
| Other | 887 (5.6) | 1018 (9.0) | 293 (6.8) | 333 (8.9) | 240 (10.2) | 152 (16.3) |
| Operative treatment | ||||||
| Resection | 6878 (43.6) | 5146 (45.5) | 2071 (48.3) | 1816 (48.5) | 971 (41.5) | 288 (30.9) |
| No resection | 738 (4.7) | 314 (2.8) | 144 (3.4) | 102 (2.7) | 54 (2.3) | 14 (1.5) |
| No information/no surgery | 8166 (51.7) | 5846 (51.7) | 2072 (48.3) | 1827 (48.8) | 1317 (56.2) | 630 (67.6) |
| Postoperative hospital stay, median in | ||||||
| days (IQR) | ||||||
| Colon cancer | 6.0 (4.0–8.0) | 7.0 (5.0–10.0) | 7.0 (5.0–9.0) | 7.0 (5.0–10.0) | 7.0 (5.0–10.0) | 7.0 (5.0–10.0) |
| Rectum cancer | 7.0 (5.0–9.0) | 7.0 (5.0–10.0) | 7.0 (5.0–10.0) | 7.0 (6.0–10.0) | 7.0 (5.0–9.5) | 7.0 (6.0–9.0) |
| Age Group | <75 Years Old | 75–79 Years Old | 80–84 Years Old | 85–89 Years Old | ≥90 Years Old |
|---|---|---|---|---|---|
| FCR 2 0 | 68.0 (65.8–70.2) | 43.9 (39.6–48.2) | 37.0 (33.3–40.7) | 18.3 (14.6–22.0) | 4.8 (2.1–7.5) |
| FCR 1 | 88.7 (87.5–89.9) | 72.7 (69.4–76.0) | 54.6 (50.5–58.7) | 38.5 (33.0–44.0) | 17.7 (9.7–25.7) |
| FCR 2 | 65.6 (63.4–67.8) | 52.2 (47.3–57.1) | 36.8 (31.7–41.9) | 32.3 (25.4–39.2) | 14.8 (4.4–25.2) |
| FCR 3 | 44.3 (42.5–46.1) | 36.7 (33.6–39.8) | 26.9 (23.8–30.0) | 17.2 (13.9–20.5) | 7.4 (3.3–11.5) |
| FCR 4 | 52.3 (48.4–56.2) | 39.1 (31.7–46.5) | 29.8 (22.7–36.9) | 19.8 (12.7–26.9) | 9.5 (2.1–16.9) |
| FCR 5 | 79.1 (77.1–81.1) | 60.4 (55.1–65.7) | 52.9 (47.2–58.6) | 42.8 (35.5–50.1) | 19.4 (9.4–29.4) |
| FCR 6 | 16.8 (14.6–19.0) | 4.1 (1.4–6.8) | 4.6 (1.5–7.7) | 0.8 (0.0–2.4) | 2.1 (0.0–6.2) |
| All patients | 61.7 (60.9–62.5) | 47.6 (46.0–49.2) | 36.6 (34.8–38.4) | 24.5 (22.5–26.5) | 9.0 (6.8–11.2) |
| Age Group | <75 Years Old | 75–79 Years Old | 80–84 Years Old | 85–89 Years Old | ≥90 Years Old |
|---|---|---|---|---|---|
| FCR 2 0 | 1.00 | 2.16 (1.91–2.44) | 2.83 (2.52–3.18) | 4.54 (4.05–5.10) | 6.77 (5.93–7.72) |
| FCR 1 | 1.00 | 2.83 (2.43–3.29) | 5.10 (4.43–5.89) | 7.69 (6.56–9.02) | 16.16 (12.88–20.28) |
| FCR 2 | 1.00 | 1.64 (1.43–1.88) | 2.31 (2.02–2.65) | 3.08 (2.61–3.65) | 5.12 (3.94–6.64) |
| FCR 3 | 1.00 | 1.32 (1.20–1.44) | 1.80 (1.64–1.97) | 2.44 (2.19–2.72) | 3.62 (3.06–4.29) |
| FCR 4 | 1.00 | 1.57 (1.32–1.87) | 2.03 (1.71–2.41) | 2.85 (2.35–3.46) | 4.95 (3.82–6.42) |
| FCR 5 | 1.00 | 2.04 (1.73–2.40) | 2.99 (2.54–3.51) | 4.18 (3.49–5.01) | 6.71 (5.15–8.73) |
| FCR 6 | 1.00 | 1.65 (1.46–1.87) | 1.96 (1.71–2.25) | 3.06 (2.57–3.64) | 4.82 (3.58–6.48) |
| All patients | 1.00 | 1.62 (1.54–1.69) | 2.23 (2.13–2.34) | 3.21 (3.04–3.38) | 5.28 (4.91–5.69) |
| Age Group | <75 Years Old | 75–79 Years Old | 80–84 Years Old | 85–89 Years Old | ≥90 Years Old |
|---|---|---|---|---|---|
| A | |||||
| FCR 2 0 | 70.1 (65.6–74.6) | 51.8 (43.8–59.8) | 43.4 (36.0–50.8) | 24.1 (16.5–31.7) | 16.8 (7.2–26.4) |
| FCR 1 | 87.4 (84.7–90.1) | 73.3 (67.2–79.4) | 55.4 (48.5–62.3) | 41.0 (32.0–50.0) | 18.9 (4.2–33.6) |
| FCR 2 | 57.7 (53.6–61.8) | 49.9 (42.3–57.5) | 37.3 (29.3–45.3) | 37.5 (27.5–47.5) | 20.9 (6.6–35.2) |
| FCR 3 | 47.2 (43.9–50.5) | 39.3 (34.3–44.4) | 29.7 (24.8–34.6) | 23.2 (17.1–29.3) | 8.5 (2.0–15.0) |
| FCR 4 | 47.6 (40.7–54.5) | 33.9 (20.8–47.0) | 27.5 (16.1–38.9) | 24.1 (13.3–34.9) | 7.9 (0.0–18.3) |
| FCR 5 | 79.9 (76.2–83.6) | 64.2 (55.6–72.8) | 59.2 (51.2–67.2) | 44.0 (32.8–55.2) | 17.9 (5.2–30.6) |
| FCR 6 | 12.2 (8.9–15.5) | 1.6 (0.0–4.7) | 5.6 (0.3–10.9) | 0.0 | 0.0 |
| All patients | 58.8 (57.2–60.4) | 49.2 (46.3–52.1) | 39.9 (37.2–42.6) | 29.1 (25.8–32.4) | 13.1 (8.8–17.4) |
| B | |||||
| FCR 2 0 | 67.4 (62.5–72.3) | 40.2 (30.0–50.4) | 44.8 (36.2–53.4) | 17.4 (9.2–25.6) | 0.0 |
| FCR 1 | 89.7 (87.2–92.2) | 73.4 (66.3–80.5) | 51.7 (42.7–60.7) | 45.1 (32.6–57.6) | 32.0 (12.0–52.0) |
| FCR 2 | 68.2 (64.1–72.3) | 53.0 (43.6–62.4) | 37.8 (27.4–48.2) | 15.5 (2.4–28.6) | 11.8 (0.0–31.0) |
| FCR 3 | 43.9 (40.4–47.4) | 36.4 (30.3–42.5) | 27.0 (20.5–33.5) | 13.4 (7.3–19.5) | 9.7 (0.0–19.9) |
| FCR 4 | 51.7 (43.5–59.9) | 33.5 (11.9–55.1) | 29.6 (14.1–45.1) | 21.4 (6.7–36.1) | 0.0 |
| FCR 5 | 81.9 (78.6–85.2) | 60.4 (50.8–70.0) | 47.0 (35.0–59.0) | 38.2 (24.9–51.5) | 13.4 (0.0–35.2) |
| FCR 6 | 18.5 (14.2–22.8) | 7.0 (0.5–13.5) | 0.0 | 0.0 | 7.7 (0.0–22.2) |
| All patients | 62.2 (60.6–63.8) | 47.6 (44.3–50.9) | 36.6 (32.9–40.3) | 22.5 (18.4–26.6) | 10.6 (5.1–16.1) |
| C | |||||
| FCR 2 0 | 67.3 (64.0–70.6) | 38.4 (31.5–45.3) | 27.6 (20.9–34.3) | 16.4 (10.5–22.3) | 1.9 (0.0–4.4) |
| FCR 1 | 89.1 (87.3–90.9) | 70.3 (65.0–75.6) | 55.9 (49.0–62.8) | 32.0 (23.6–40.4) | 7.5 (0.0–17.1) |
| FCR 2 | 70.1 (67.0–73.2) | 54.1 (45.9–62.3) | 35.9 (27.1–44.7) | 34.5 (22.5–46.5) | 0.0 |
| FCR 3 | 44.3 (41.4–47.2) | 35.4 (29.9–40.9) | 25.8 (20.5–31.1) | 15.2 (8.9–21.5) | 3.3 (0.0–9.8) |
| FCR 4 | 55.4 (48.9–61.9) | 45.5 (33.5–57.5) | 40.7 (26.6–54.8) | 9.0 (0.0–23.3) | 5.0 (0.0–14.6) |
| FCR 5 | 77.2 (74.1–80.3) | 55.0 (45.6–64.4) | 47.6 (37.0–58.2) | 43.4 (28.7–58.1) | 28.8 (2.7–54.9) |
| FCR 6 | 19.7 (16.2–23.2) | 4.6 (0.0–9.5) | 6.0 (0.5–11.5) | 0.0 | 0.0 |
| All patients | 64.3 (63.1–65.5) | 46.7 (44.0–49.4) | 34.7 (31.6–37.8) | 22.5 (19.0–26.0) | 5.0 (1.9–8.1) |
| Age Group | <75 Years Old | 75–79 Years Old | 80–84 Years Old | 85–89 Years Old | ≥90 Years Old |
|---|---|---|---|---|---|
| FCR 2 0 | 97.8 (96.8–98.8) | 96.6 (94.4–98.8) | 93.1 (90.2–96.0) | 93.9 (90.2–97.6) | 89.4 (80.6–98.2) |
| FCR 1 | 99.4 (99.0–99.8) | 97.2 (95.6–98.8) | 93.4 (90.7–96.1) | 93.1 (89.4–96.8) | 85.0 (74.0–96.0) |
| FCR 2 | 98.9 (98.3–99.5) | 97.5 (95.9–99.1) | 94.5 (92.0–97.0) | 93.4 (89.5–97.3) | 95.7 (90.0–100.0) |
| FCR 3 | 97.4 (96.6–98.2) | 94.4 (92.4–96.4) | 91.5 (88.8–94.2) | 85.8 (81.1–90.5) | 81.8 (72.6–91.0) |
| FCR 4 | 97.9 (96.7–99.1) | 93.9 (90.4–97.4) | 91.3 (87.2–95.4) | 87.2 (80.5–93.9) | 85.2 (71.9–98.5) |
| FCR 5 | 98.5 (97.9–99.1) | 96.9 (95.1–98.7) | 95.7 (93.5–97.9) | 90.4 (86.3–94.5) | 90.3 (82.9–97.7) |
| All patients | 98.4 (98.0–98.8) | 96.1 (95.3–96.9) | 93.2 (92.0–94.4) | 90.6 (88.8–92.4) | 87.9 (84.2–91.6) |
| Age Group | <75 Years Old | 75–79 Years Old | 80–84 Years Old | 85–89 Years Old | ≥90 Years Old |
|---|---|---|---|---|---|
| FCR 2 0 | 94.6 (93.0–96.2) | 89.5 (86.0–93.0) | 84.4 (80.3–88.5) | 79.7 (73.6–85.8) | 70.2 (57.1–83.3) |
| FCR 1 | 97.9 (97.1–98.7) | 92.9 (90.4–95.4) | 88.0 (84.5–91.5) | 84.9 (79.6–90.2) | 72.5 (58.6–86.4) |
| FCR 2 | 91.3 (89.9–92.7) | 89.3 (86.2–92.4) | 81.4 (76.9–85.9) | 76.1 (69.2–83.0) | 61.7 (47.8–75.6) |
| FCR 3 | 82.5 (80.5–84.5) | 75.0 (71.3–78.7) | 68.2 (63.7–72.7) | 59.3 (52.6–66.0) | 51.5 (39.3–63.7) |
| FCR 4 | 88.2 (85.7–90.7) | 80.1 (74.2–86.0) | 75.4 (69.1–81.7) | 70.2 (61.0–79.4) | 51.9 (33.1–70.7) |
| FCR 5 | 95.9 (94.9–96.9) | 92.6 (89.9–95.3) | 86.5 (82.8–90.2) | 80.9 (75.2–86.6) | 69.4 (57.8–81.0) |
| All patients | 91.7 (91.1–92.3) | 86.3 (84.7–87.9) | 80.5 (78.7–82.3) | 75.1 (72.4–77.8) | 62.9 (57.4–68.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hukkinen, T.; Olenius, T.; Koskensalo, S.; Lepistö, A.; Koskenvuo, L.; Böckelman, C. Short- and Long-Term Survival among Elderly Colorectal Cancer Patients in Finland, 2006–2015: A Nationwide Population-Based Registry Study. Cancers 2024, 16, 135. https://doi.org/10.3390/cancers16010135
Hukkinen T, Olenius T, Koskensalo S, Lepistö A, Koskenvuo L, Böckelman C. Short- and Long-Term Survival among Elderly Colorectal Cancer Patients in Finland, 2006–2015: A Nationwide Population-Based Registry Study. Cancers. 2024; 16(1):135. https://doi.org/10.3390/cancers16010135
Chicago/Turabian StyleHukkinen, Tanja, Tobias Olenius, Selja Koskensalo, Anna Lepistö, Laura Koskenvuo, and Camilla Böckelman. 2024. "Short- and Long-Term Survival among Elderly Colorectal Cancer Patients in Finland, 2006–2015: A Nationwide Population-Based Registry Study" Cancers 16, no. 1: 135. https://doi.org/10.3390/cancers16010135
APA StyleHukkinen, T., Olenius, T., Koskensalo, S., Lepistö, A., Koskenvuo, L., & Böckelman, C. (2024). Short- and Long-Term Survival among Elderly Colorectal Cancer Patients in Finland, 2006–2015: A Nationwide Population-Based Registry Study. Cancers, 16(1), 135. https://doi.org/10.3390/cancers16010135





