Multidisciplinary Treatment of Patients with Progressive Biliary Tract Cancer after First-Line Gemcitabine and Cisplatin: A Single-Center Experience
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Interventions
2.2.1. Systemic First- and Second-Line
2.2.2. Minimal Invasive Therapies (MIT)
Interstitial Brachytherapy (iBT)
Transarterial Radioembolization (TARE)
Transarterial Chemoembolization (TACE)
Stereotactic Body Radiotherapy (SBRT)
Radiofrequency Ablation (RFA)
Photodynamic Therapy (PDT)
2.3. Response and Toxicity Assessment
2.4. Statistical Analyses
3. Results
3.1. First-Line Treatment
3.2. Post-Progression Treatment
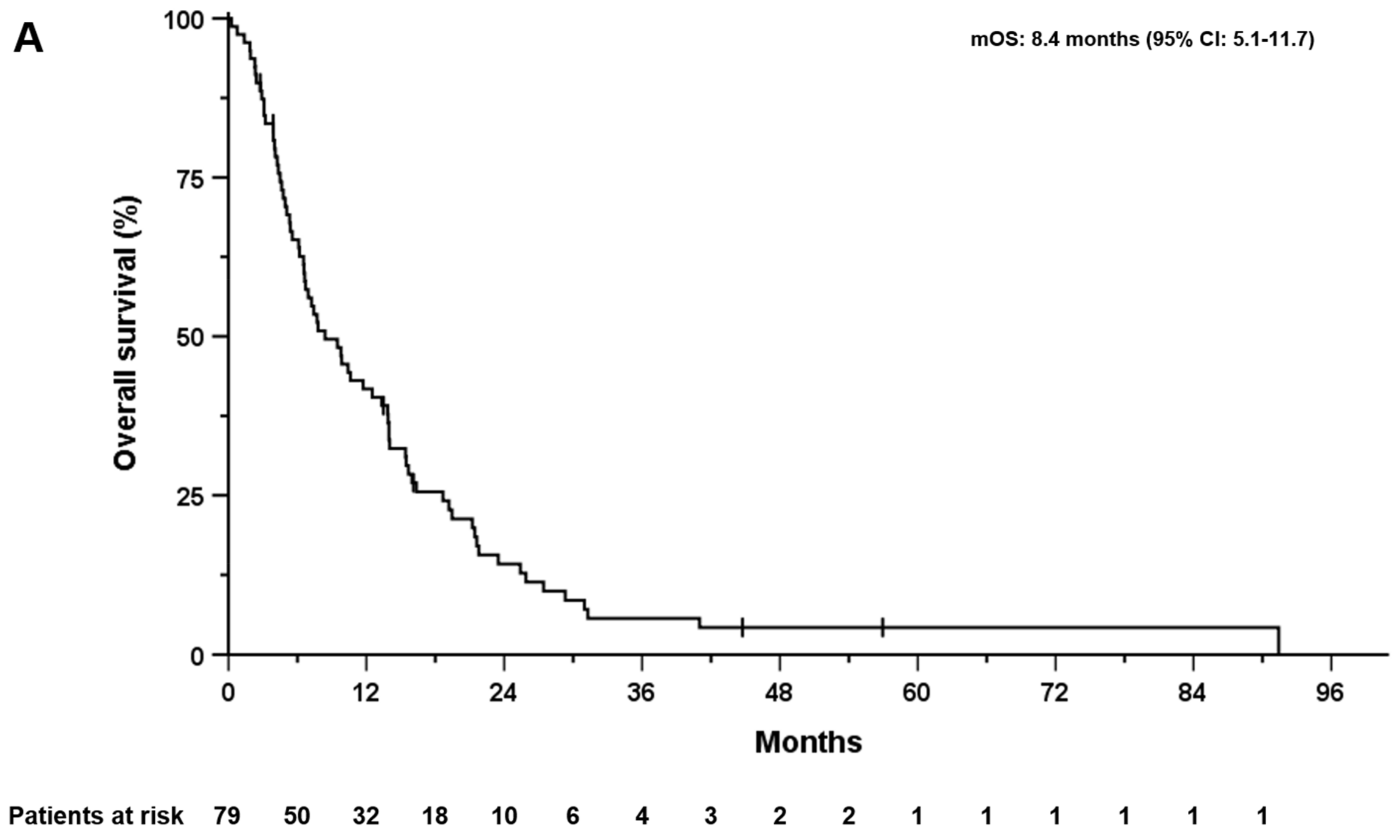
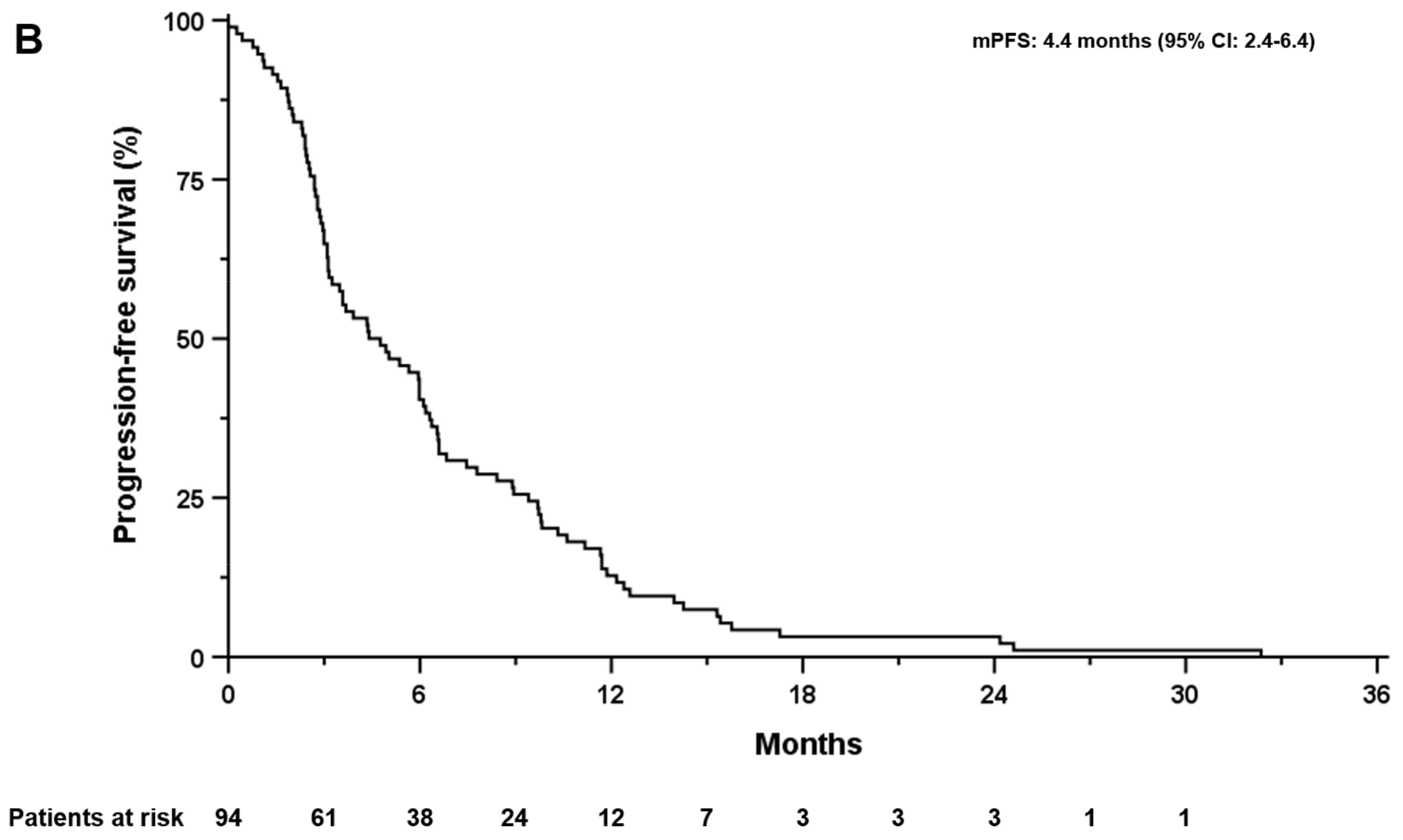
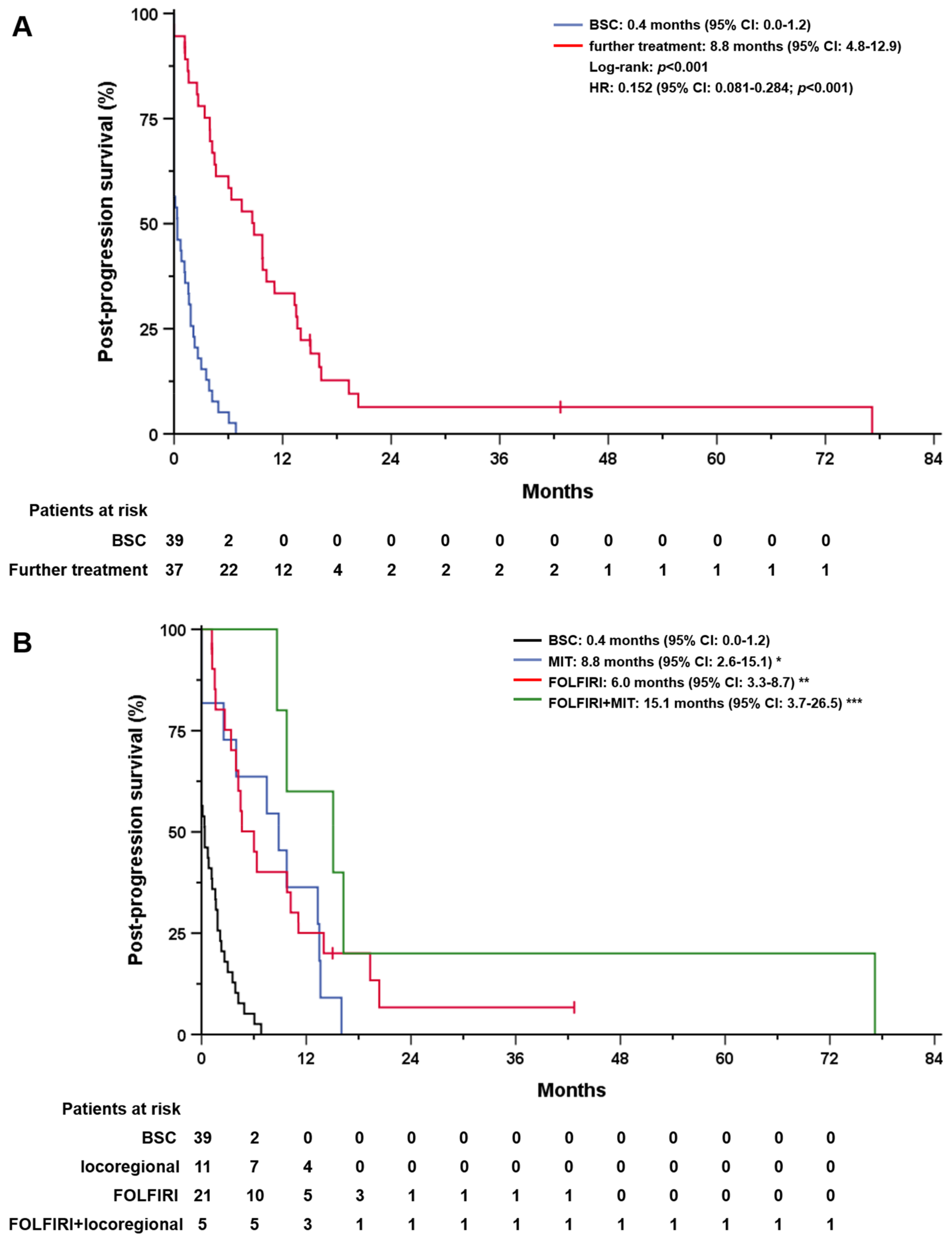
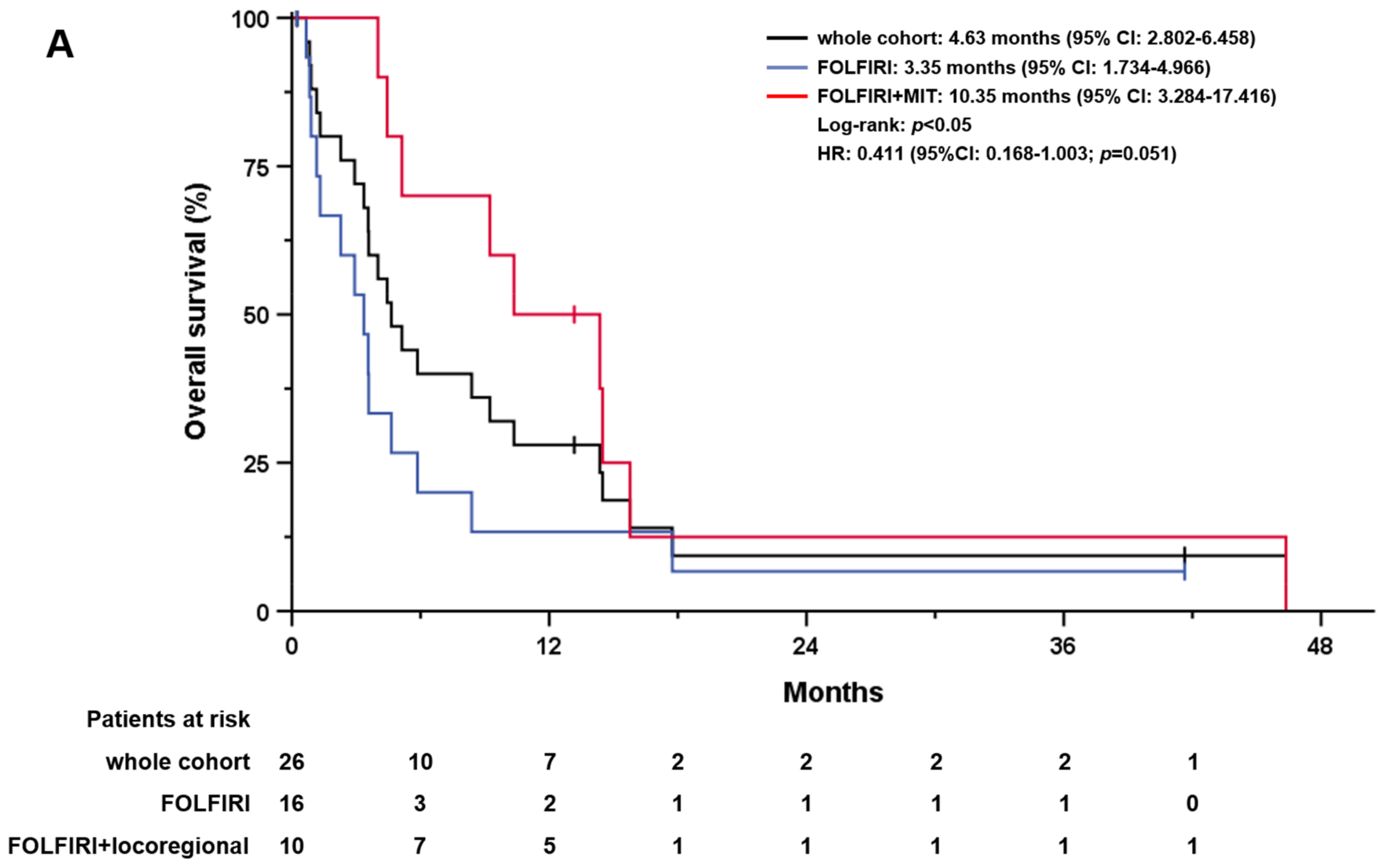
3.3. Overall Survival, Progression-Free Survival, and Post-Progression Survival
3.4. Toxicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Lamarca, A.; Edeline, J.; Goyal, L. How I Treat Biliary Tract Cancer. ESMO Open 2022, 7, 100378. [Google Scholar] [CrossRef] [PubMed]
- Banales, J.M.; Cardinale, V.; Carpino, G.; Marzioni, M.; Andersen, J.B.; Invernizzi, P.; Lind, G.E.; Folseraas, T.; Forbes, S.J.; Fouassier, L.; et al. Expert Consensus Document: Cholangiocarcinoma: Current Knowledge and Future Perspectives Consensus Statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 261–280. [Google Scholar] [CrossRef] [PubMed]
- DeOliveira, M.L.; Cunningham, S.C.; Cameron, J.L.; Kamangar, F.; Winter, J.M.; Lillemoe, K.D.; Choti, M.A.; Yeo, C.J.; Schulick, R.D. Cholangiocarcinoma: Thirty-One-Year Experience with 564 Patients at a Single Institution. Ann. Surg. 2007, 245, 755–762. [Google Scholar] [CrossRef]
- Nakeeb, A.; Pitt, H.A.; Sohn, T.A.; Coleman, J.; Abrams, R.A.; Piantadosi, S.; Hruban, R.H.; Lillemoe, K.D.; Yeo, C.J.; Cameron, J.L. Cholangiocarcinoma. A Spectrum of Intrahepatic, Perihilar, and Distal Tumors. Ann. Surg. 1996, 224, 463–475. [Google Scholar] [CrossRef]
- Nathan, H.; Pawlik, T.M.; Wolfgang, C.L.; Choti, M.A.; Cameron, J.L.; Schulick, R.D. Trends in Survival after Surgery for Cholangiocarcinoma: A 30-Year Population-Based SEER Database Analysis. J. Gastrointest. Surg. 2007, 11, 1488–1497. [Google Scholar] [CrossRef]
- Endo, I.; Gonen, M.; Yopp, A.C.; Dalal, K.M.; Zhou, Q.; Klimstra, D.; D’Angelica, M.; DeMatteo, R.P.; Fong, Y.; Schwartz, L.; et al. Intrahepatic Cholangiocarcinoma: Rising Frequency, Improved Survival, and Determinants of Outcome after Resection. Ann. Surg. 2008, 248, 84–96. [Google Scholar] [CrossRef]
- Choi, S.-B.; Kim, K.-S.; Choi, J.-Y.; Park, S.-W.; Choi, J.-S.; Lee, W.-J.; Chung, J.-B. The Prognosis and Survival Outcome of Intrahepatic Cholangiocarcinoma Following Surgical Resection: Association of Lymph Node Metastasis and Lymph Node Dissection with Survival. Ann. Surg. Oncol. 2009, 16, 3048–3056. [Google Scholar] [CrossRef]
- Brown, K.M.; Parmar, A.D.; Geller, D.A. Intrahepatic Cholangiocarcinoma. Surg. Oncol. Clin. N. Am. 2014, 23, 231–246. [Google Scholar] [CrossRef]
- Bridgewater, J.; Galle, P.R.; Khan, S.A.; Llovet, J.M.; Park, J.-W.; Patel, T.; Pawlik, T.M.; Gores, G.J. Guidelines for the Diagnosis and Management of Intrahepatic Cholangiocarcinoma. J. Hepatol. 2014, 60, 1268–1289. [Google Scholar] [CrossRef]
- Buettner, S.; ten Cate, D.W.G.; Bagante, F.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; Gamblin, T.C.; Maithel, S.K.; Pulitano, C.; et al. Survival after Resection of Multiple Tumor Foci of Intrahepatic Cholangiocarcinoma. J. Gastrointest. Surg. 2019, 23, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Sano, T.; Shimada, K.; Sakamoto, Y.; Yamamoto, J.; Yamasaki, S.; Kosuge, T. One Hundred Two Consecutive Hepatobiliary Resections for Perihilar Cholangiocarcinoma with Zero Mortality. Ann. Surg. 2006, 244, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, G.; Giuliante, F.; Ardito, F.; de Rose, A.M.; Vellone, M.; Clemente, G.; Chiarla, C.; Giovannini, I. Intrahepatic Cholangiocarcinoma: Prognostic Factors after Liver Resection. Updates Surg. 2010, 62, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Davidson, B.R.; Goldin, R.D.; Heaton, N.; Karani, J.; Pereira, S.P.; Rosenberg, W.M.C.; Tait, P.; Taylor-Robinson, S.D.; Thillainayagam, A.V.; et al. Guidelines for the Diagnosis and Treatment of Cholangiocarcinoma: An Update. Gut 2012, 61, 1657–1669. [Google Scholar] [CrossRef] [PubMed]
- Primrose, J.N.; Fox, R.P.; Palmer, D.H.; Malik, H.Z.; Prasad, R.; Mirza, D.; Anthony, A.; Corrie, P.; Falk, S.; Finch-Jones, M.; et al. Capecitabine Compared with Observation in Resected Biliary Tract Cancer (BILCAP): A Randomised, Controlled, Multicentre, Phase 3 Study. Lancet Oncol. 2019, 20, 663–673. [Google Scholar] [CrossRef]
- Bridgewater, J.; Fletcher, P.; Palmer, D.H.; Malik, H.Z.; Prasad, R.; Mirza, D.; Anthony, A.; Corrie, P.; Falk, S.; Finch-Jones, M.; et al. Long-Term Outcomes and Exploratory Analyses of the Randomized Phase III BILCAP Study. J. Clin. Oncol. 2022, 40, 2048–2057. [Google Scholar] [CrossRef]
- Valle, J.; Wasan, H.; Palmer, D.H.; Cunningham, D.; Anthoney, A.; Maraveyas, A.; Madhusudan, S.; Iveson, T.; Hughes, S.; Pereira, S.P.; et al. Cisplatin plus Gemcitabine versus Gemcitabine for Biliary Tract Cancer. N. Engl. J. Med. 2010, 362, 1273–1281. [Google Scholar] [CrossRef]
- Okusaka, T.; Nakachi, K.; Fukutomi, A.; Mizuno, N.; Ohkawa, S.; Funakoshi, A.; Nagino, M.; Kondo, S.; Nagaoka, S.; Funai, J.; et al. Gemcitabine Alone or in Combination with Cisplatin in Patients with Biliary Tract Cancer: A Comparative Multicentre Study in Japan. Br. J. Cancer 2010, 103, 469–474. [Google Scholar] [CrossRef]
- Oh, D.-Y.; Ruth He, A.; Qin, S.; Chen, L.-T.; Okusaka, T.; Vogel, A.; Kim, J.W.; Suksombooncharoen, T.; Ah Lee, M.; Kitano, M.; et al. Durvalumab plus Gemcitabine and Cisplatin in Advanced Biliary Tract Cancer. NEJM Evid. 2022, 1, EVIDoa2200015. [Google Scholar] [CrossRef]
- Lamarca, A.; Palmer, D.H.; Wasan, H.S.; Ross, P.J.; Ma, Y.T.; Arora, A.; Falk, S.; Gillmore, R.; Wadsley, J.; Patel, K.; et al. Second-Line FOLFOX Chemotherapy versus Active Symptom Control for Advanced Biliary Tract Cancer (ABC-06): A Phase 3, Open-Label, Randomised, Controlled Trial. Lancet Oncol. 2021, 22, 690–701. [Google Scholar] [CrossRef]
- Vogel, A.; Bridgewater, J.; Edeline, J.; Kelley, R.K.; Klümpen, H.J.; Malka, D.; Primrose, J.N.; Rimassa, L.; Stenzinger, A.; Valle, J.W.; et al. Biliary Tract Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2023, 34, 127–140. [Google Scholar] [CrossRef]
- Sebbagh, S.; Roux, J.; Dreyer, C.; Neuzillet, C.; de Gramont, A.; Orbegoso, C.; Hentic, O.; Hammel, P.; de Gramont, A.; Raymond, E.; et al. Efficacy of a Sequential Treatment Strategy with GEMOX-Based Followed by FOLFIRI-Based Chemotherapy in Advanced Biliary Tract Cancers. Acta Oncol. 2016, 55, 1168–1174. [Google Scholar] [CrossRef]
- Caparica, R.; Lengelé, A.; Bekolo, W.; Hendlisz, A. FOLFIRI as Second-Line Treatment of Metastatic Biliary Tract Cancer Patients. Autops. Case Rep. 2019, 9, e2019087. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, J.D.; Gunchick, V.; Mody, K.; Xiao, L.; Surapaneni, P.; Shroff, R.T.; Sahai, V. Multi-Institutional Retrospective Analysis of FOLFIRI in Patients with Advanced Biliary Tract Cancers. World J. Gastrointest. Oncol. 2020, 12, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Yoo, C.; Kim, K.-P.; Jeong, J.H.; Kim, I.; Kang, M.J.; Cheon, J.; Kang, B.W.; Ryu, H.; Lee, J.S.; Kim, K.W.; et al. Liposomal Irinotecan plus Fluorouracil and Leucovorin versus Fluorouracil and Leucovorin for Metastatic Biliary Tract Cancer after Progression on Gemcitabine plus Cisplatin (NIFTY): A Multicentre, Open-Label, Randomised, Phase 2b Study. Lancet Oncol. 2021, 22, 1560–1572. [Google Scholar] [CrossRef] [PubMed]
- Vogel, A.; Wenzel, P.; Folprecht, G.; Schütt, P.; Wege, H.; Kretzschmar, A.; Jacobasch, L.; Ziegenhagen, N.; Boeck, S.; Kanzler, S.; et al. 53MO Nal-IRI and 5-FU/LV Compared to 5-FU/LV in Patients with Cholangio- and Gallbladder Carcinoma Previously Treated with Gemcitabine-Based Therapies (NALIRICC–AIO-HEP-0116). Ann. Oncol. 2022, 33, S563–S564. [Google Scholar] [CrossRef]
- Benson, A.B.; D’Angelica, M.I.; Abbott, D.E.; Anaya, D.A.; Anders, R.; Are, C.; Bachini, M.; Borad, M.; Brown, D.; Burgoyne, A.; et al. Hepatobiliary Cancers, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 541–565. [Google Scholar] [CrossRef] [PubMed]
- Voesch, S.; Bitzer, M.; Blödt, S.; Follmann, M.; Freudenberger, P.; Langer, T.; Lorenz, P.; Jansen, P.L.; Steubesand, N.; Galle, P.; et al. S3-Leitlinie: Diagnostik und Therapie des hepatozellulären Karzinoms und biliärer Karzinome–Version 2.0–Juni 2021, AWMF-Registernummer: 032-053OL. Z. Gastroenterol. 2022, 60, e131–e185. [Google Scholar] [CrossRef] [PubMed]
- Ricke, J.; Wust, P. Computed Tomography-Guided Brachytherapy for Liver Cancer. Semin. Radiat. Oncol. 2011, 21, 287–293. [Google Scholar] [CrossRef]
- Filippi, L.; di Costanzo, G.G.; Tortora, R.; Pelle, G.; Cianni, R.; Schillaci, O.; Bagni, O. Repeated Treatment with 90Y-Microspheres in Intrahepatic Cholangiocarcinoma Relapsed After the First Radioembolization. Cancer Biother. Radiopharm. 2019, 34, 231–237. [Google Scholar] [CrossRef]
- Venturini, M.; Sallemi, C.; Agostini, G.; Marra, P.; Cereda, S.; Reni, M.; Aldrighetti, L.; de Cobelli, F.; del Maschio, A. Chemoembolization with Drug Eluting Beads Preloaded with Irinotecan (DEBIRI) vs Doxorubicin (DEBDOX) as a Second Line Treatment for Liver Metastases from Cholangiocarcinoma: A Preliminary Study. Br. J. Radiol. 2016, 89, 20160247. [Google Scholar] [CrossRef]
- Gkika, E.; Hallauer, L.; Kirste, S.; Adebahr, S.; Bartl, N.; Neeff, H.P.; Fritsch, R.; Brass, V.; Nestle, U.; Grosu, A.L.; et al. Stereotactic Body Radiotherapy (SBRT) for Locally Advanced Intrahepatic and Extrahepatic Cholangiocarcinoma. BMC Cancer 2017, 17, 781. [Google Scholar] [CrossRef] [PubMed]
- Steel, A.W.; Postgate, A.J.; Khorsandi, S.; Nicholls, J.; Jiao, L.; Vlavianos, P.; Habib, N.; Westaby, D. Endoscopically Applied Radiofrequency Ablation Appears to Be Safe in the Treatment of Malignant Biliary Obstruction. Gastrointest. Endosc. 2011, 73, 149–153. [Google Scholar] [CrossRef]
- Huang, B.-Y.; Zhou, J.-J.; Yu, Z.-Q.; Song, X.-Y.; Lin, Y.; Li, X.-M.; Li, L. Long-Term Observation of CT-Guided Radiofrequency Ablation of Lung Neoplasm in 476 Consecutive Patients by a Thoracic Surgical Service: A Single-Institutional Experience. Acad. Radiol. 2017, 24, 1517–1525. [Google Scholar] [CrossRef]
- Strand, D.S.; Cosgrove, N.D.; Patrie, J.T.; Cox, D.G.; Bauer, T.W.; Adams, R.B.; Mann, J.A.; Sauer, B.G.; Shami, V.M.; Wang, A.Y. ERCP-Directed Radiofrequency Ablation and Photodynamic Therapy Are Associated with Comparable Survival in the Treatment of Unresectable Cholangiocarcinoma. Gastrointest. Endosc. 2014, 80, 794–804. [Google Scholar] [CrossRef]
- Lamarca, A.; Hubner, R.A.; David Ryder, W.; Valle, J.W. Second-Line Chemotherapy in Advanced Biliary Cancer: A Systematic Review. Ann. Oncol. 2014, 25, 2328–2338. [Google Scholar] [CrossRef] [PubMed]
- Brieau, B.; Dahan, L.; de Rycke, Y.; Boussaha, T.; Vasseur, P.; Tougeron, D.; Lecomte, T.; Coriat, R.; Bachet, J.-B.; Claudez, P.; et al. Second-Line Chemotherapy for Advanced Biliary Tract Cancer after Failure of the Gemcitabine-Platinum Combination: A Large Multicenter Study by the Association Des Gastro-Entérologues Oncologues. Cancer 2015, 121, 3290–3297. [Google Scholar] [CrossRef]
- Schweitzer, N.; Kirstein, M.M.; Kratzel, A.-M.; Mederacke, Y.-S.; Fischer, M.; Manns, M.P.; Vogel, A. Second-Line Chemotherapy in Biliary Tract Cancer: Outcome and Prognostic Factors. Liver Int. 2019, 39, 914–923. [Google Scholar] [CrossRef]
- Möhring, C.; Feder, J.; Mohr, R.U.; Sadeghlar, F.; Bartels, A.; Mahn, R.; Zhou, T.; Marinova, M.; Feldmann, G.; Brossart, P.; et al. First Line and Second Line Chemotherapy in Advanced Cholangiocarcinoma and Impact of Dose Reduction of Chemotherapy: A Retrospective Analysis. Front. Oncol. 2021, 11, 717397. [Google Scholar] [CrossRef]
- Choi, I.S.; Kim, K.H.; Lee, J.H.; Suh, K.J.; Kim, J.W.; Park, J.H.; Kim, Y.J.; Kim, J.S.; Kim, J.H.; Kim, J.W. A Randomised Phase II Study of Oxaliplatin/5-FU (mFOLFOX) versus Irinotecan/5-FU (mFOLFIRI) Chemotherapy in Locally Advanced or Metastatic Biliary Tract Cancer Refractory to First-Line Gemcitabine/Cisplatin Chemotherapy. Eur. J. Cancer 2021, 154, 288–295. [Google Scholar] [CrossRef]
- Kim, I.-H. 81P Final Results from the NIFTY Trial, a Phase IIb, Randomized, Open-Label Study of Liposomal Irinotecan (Nal-IRI) plus Fluorouracil (5-FU)/Leucovorin (LV) in Patients (Pts) with Previously Treated Metastatic Biliary Tract Cancer (BTC). Ann. Oncol. 2022, 33, S1464. [Google Scholar] [CrossRef]
- Jia, Z.; Paz-Fumagalli, R.; Frey, G.; Sella, D.M.; McKinney, J.M.; Wang, W. Resin-Based Yttrium-90 Microspheres for Unresectable and Failed First-Line Chemotherapy Intrahepatic Cholangiocarcinoma: Preliminary Results. J. Cancer Res. Clin. Oncol. 2017, 143, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Gangi, A.; Shah, J.; Hatfield, N.; Smith, J.; Sweeney, J.; Choi, J.; El-Haddad, G.; Biebel, B.; Parikh, N.; Arslan, B.; et al. Intrahepatic Cholangiocarcinoma Treated with Transarterial Yttrium-90 Glass Microsphere Radioembolization: Results of a Single Institution Retrospective Study. J. Vasc. Interv. Radiol. 2018, 29, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Levillain, H.; Duran Derijckere, I.; Ameye, L.; Guiot, T.; Braat, A.; Meyer, C.; Vanderlinden, B.; Reynaert, N.; Hendlisz, A.; Lam, M.; et al. Personalised Radioembolization Improves Outcomes in Refractory Intra-Hepatic Cholangiocarcinoma: A Multicenter Study. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2270–2279. [Google Scholar] [CrossRef]
- White, J.; Carolan-Rees, G.; Dale, M.; Patrick, H.E.; See, T.C.; Bell, J.K.; Manas, D.M.; Crellin, A.; Slevin, N.J.; Sharma, R.A. Yttrium-90 Transarterial Radioembolization for Chemotherapy-Refractory Intrahepatic Cholangiocarcinoma: A Prospective, Observational Study. J. Vasc. Interv. Radiol. 2019, 30, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Buettner, S.; Braat, A.J.A.T.; Margonis, G.A.; Brown, D.B.; Taylor, K.B.; Borgmann, A.J.; Kappadath, S.C.; Mahvash, A.; IJzermans, J.N.M.; Weiss, M.J.; et al. Yttrium-90 Radioembolization in Intrahepatic Cholangiocarcinoma: A Multicenter Retrospective Analysis. J. Vasc. Interv. Radiol. 2020, 31, 1035–1043.e2. [Google Scholar] [CrossRef]
- Schnapauff, D.; Denecke, T.; Grieser, C.; Collettini, F.; Seehofer, D.; Sinn, M.; Banzer, J.; Lopez-Hänninen, E.; Hamm, B.; Wust, P.; et al. Computed Tomography-Guided Interstitial HDR Brachytherapy (CT-HDRBT) of the Liver in Patients with Irresectable Intrahepatic Cholangiocarcinoma. Cardiovasc. Interv. Radiol. 2012, 35, 581–587. [Google Scholar] [CrossRef]
- Kamphues, C.; Seehofer, D.; Collettini, F.; Bahra, M.; Neuhaus, P.; Wust, P.; Denecke, T.; Gebauer, B.; Schnapauff, D. Preliminary Experience with CT-Guided High-Dose Rate Brachytherapy as an Alternative Treatment for Hepatic Recurrence of Cholangiocarcinoma. HPB 2012, 14, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Jonczyk, M.; Collettini, F.; Schnapauff, D.; Geisel, D.; Böning, G.; Feldhaus, F.; Denecke, T.; Wieners, G.; Hamm, B.; Gebauer, B. Cholangiocarcinoma: CT-Guided High-Dose Rate Brachytherapy (CT-HDRBT) for Limited (<4 cm) and Large (>4 cm) Tumors. Anticancer Res. 2018, 38, 5843–5852. [Google Scholar] [CrossRef]
- Zheng, Y.; Tu, X.; Zhao, P.; Jiang, W.; Liu, L.; Tong, Z.; Zhang, H.; Yan, C.; Fang, W.; Wang, W. A Randomised Phase II Study of Second-Line XELIRI Regimen versus Irinotecan Monotherapy in Advanced Biliary Tract Cancer Patients Progressed on Gemcitabine and Cisplatin. Br. J. Cancer 2018, 119, 291–295. [Google Scholar] [CrossRef]

| Total (n = 97) | BSC (n = 50) | Further Treatment (n = 47) | |||||
|---|---|---|---|---|---|---|---|
| Gender | n | % or Range | n | % or Range | n | % or Range | |
| Male | 51 | 53 | 30 | 60 | 21 | 45 | |
| Female | 46 | 47 | 20 | 40 | 26 | 55 | |
| Age | |||||||
| median age (range) | 68.1 | 23.4–85.9 | 68.1 | 42.5–85.9 | 68.0 | 23.4–81.3 | |
| <65 years | 42 | 43 | 19 | 38.0 | 23 | 49 | |
| ≥65 years | 55 | 57 | 31 | 62.0 | 24 | 51 | |
| ECOG | |||||||
| 0 | 49 | 51 | 17 | 34 | 32 | 68 | |
| 1 | 43 | 44 | 28 | 56 | 15 | 32 | |
| 2 | 5 | 5 | 5 | 10 | 0 | 0 | |
| Primary tumor location | |||||||
| Intrahepatic | 50 | 52 | 26 | 52 | 24 | 51 | |
| Hilar | 18 | 19 | 11 | 22 | 7 | 15 | |
| Distal | 9 | 9 | 5 | 10 | 4 | 9 | |
| Gallbladder | 18 | 19 | 8 | 16 | 10 | 21 | |
| Ampulla vateri | 2 | 2 | 0 | 0 | 2 | 4 | |
| Tumor stage at diagnosis | |||||||
| locally advanced | 46 | 47 | 25 | 50 | 21 | 45 | |
| metastatic | 51 | 53 | 25 | 50 | 26 | 55 | |
| Tumor grading | |||||||
| G1 | 6 | 6 | 3 | 6 | 3 | 6 | |
| G2 | 66 | 68 | 33 | 66 | 33 | 70 | |
| G3 | 24 | 25 | 13 | 26 | 11 | 23 | |
| not available (%) | 1 | 1 | 1 | 2 | 0 | 0 | |
| prior resection | |||||||
| yes | 23 | 24 | 9 | 18 | 14 | 30 | |
| no | 74 | 76 | 41 | 82 | 33 | 70 | |
| prior loco-regional therapies | |||||||
| Yes * | 32 | 33 | 19 | 38 | 13 | 28 | |
| no | 65 | 67 | 31 | 62 | 34 | 72 | |
| serological tumour markers | |||||||
| CA19-9 (U/mL; normal value: <27 U/mL) | 194.7 | 0.6–31, 498 | 314.1 | 24.6–31, 498 | 126.7 | 0.6–9341 | |
| CEA (ng/mL; normal value: <5 ng/mL) | 3.3 | 0.4–200, 4 | 2.6 | 1.16–115 | 3.71 | 0.8–107 | |
| First-line gemcitabine/cisplatin | |||||||
| Median number of cycles | 4 | 3 | 5 | ||||
| Median duration of treatment (weeks) | 13 | 10 | 15 | ||||
| Dose reduction | 59 | 61 | 32 | 64 | 27 | 57 | |
| MIT (n = 14) | Before FOLFIRI (n = 4) | After FOLFIRI (n = 7) | Both (n = 3) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| iBT | 3 | 21 | 2 | 50 | 2 | 29 | 1 | 33 | |
| TARE | 4 | 29 | 1 | 25 | 4 | 57 | 0 | 0 | |
| SBRT | 2 | 14 | 0 | 0 | 1 | 14 | 0 | 0 | |
| RFA | 1 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | |
| PDT | 1 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | |
| iBT + TARE | 1 | 7 | 0 | 0 | 0 | 0 | 1 * | 33 | |
| SBRT + TARE | 1 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | |
| TARE + TACE | 1 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | |
| iBT + TACE | 0 | 0 | 1 | 25 | 0 | 0 | 0 | 0 | |
| multiple | 0 | 0 | 0 | 0 | 0 | 0 | 1 ** | 33 | |
| All Grades | Grade III–IV | Grade V | |||||
|---|---|---|---|---|---|---|---|
| Hematologic | n | % | n | % | n | % | |
| Anemia | 43 | 92 | 12 | 26 | 0 | 0 | |
| Thrombocytopenia | 30 | 64 | 5 | 11 | 0 | 0 | |
| Neutropenia | 13 | 28 | 3 | 6 | 0 | 0 | |
| Non-hematologic | |||||||
| AST increased | 32 | 68 | 2 | 4 | 0 | 0 | |
| ALT increased | 17 | 36 | 2 | 4 | 0 | 0 | |
| Bilirubin increased | 18 | 38 | 6 | 13 | 0 | 0 | |
| Creatinine increased | 13 | 28 | 0 | 0 | 0 | 0 | |
| Nausea | 8 | 17 | 0 | 0 | 0 | 0 | |
| Vomiting | 5 | 11 | 1 | 2 | 0 | 0 | |
| Diarrhea | 2 | 4 | 0 | 0 | 0 | 0 | |
| Stomatitis | 0 | 0 | 0 | 0 | 0 | 0 | |
| Fatigue | 8 | 17 | 0 | 0 | 0 | 0 | |
| Neuropathy | 0 | 0 | 0 | 0 | 0 | 0 | |
| Febrile neutropenia | 0 | 0 | 0 | 0 | 0 | 0 | |
| Ascites | 11 | 23 | 4 | 9 | 0 | 0 | |
| Pneumonia | 0 | 0 | 0 | 0 | 0 | 0 | |
| Hepatic failure | 1 | 2 | 0 | 0 | 1 | 2 | |
| Sepsis | 4 | 9 | 2 | 4 | 2 | 4 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, C.; Omari, J.; Mohnike, K.; Bär, C.; Pech, M.; Keitel, V.; Venerito, M. Multidisciplinary Treatment of Patients with Progressive Biliary Tract Cancer after First-Line Gemcitabine and Cisplatin: A Single-Center Experience. Cancers 2023, 15, 2598. https://doi.org/10.3390/cancers15092598
Müller C, Omari J, Mohnike K, Bär C, Pech M, Keitel V, Venerito M. Multidisciplinary Treatment of Patients with Progressive Biliary Tract Cancer after First-Line Gemcitabine and Cisplatin: A Single-Center Experience. Cancers. 2023; 15(9):2598. https://doi.org/10.3390/cancers15092598
Chicago/Turabian StyleMüller, Christian, Jazan Omari, Konrad Mohnike, Caroline Bär, Maciej Pech, Verena Keitel, and Marino Venerito. 2023. "Multidisciplinary Treatment of Patients with Progressive Biliary Tract Cancer after First-Line Gemcitabine and Cisplatin: A Single-Center Experience" Cancers 15, no. 9: 2598. https://doi.org/10.3390/cancers15092598
APA StyleMüller, C., Omari, J., Mohnike, K., Bär, C., Pech, M., Keitel, V., & Venerito, M. (2023). Multidisciplinary Treatment of Patients with Progressive Biliary Tract Cancer after First-Line Gemcitabine and Cisplatin: A Single-Center Experience. Cancers, 15(9), 2598. https://doi.org/10.3390/cancers15092598








