Update on Locoregional Therapies for Cholangiocellular Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Percutaneous Tumorablation
3. Transarterial (Chemo-)Embolization (TAE and TACE)
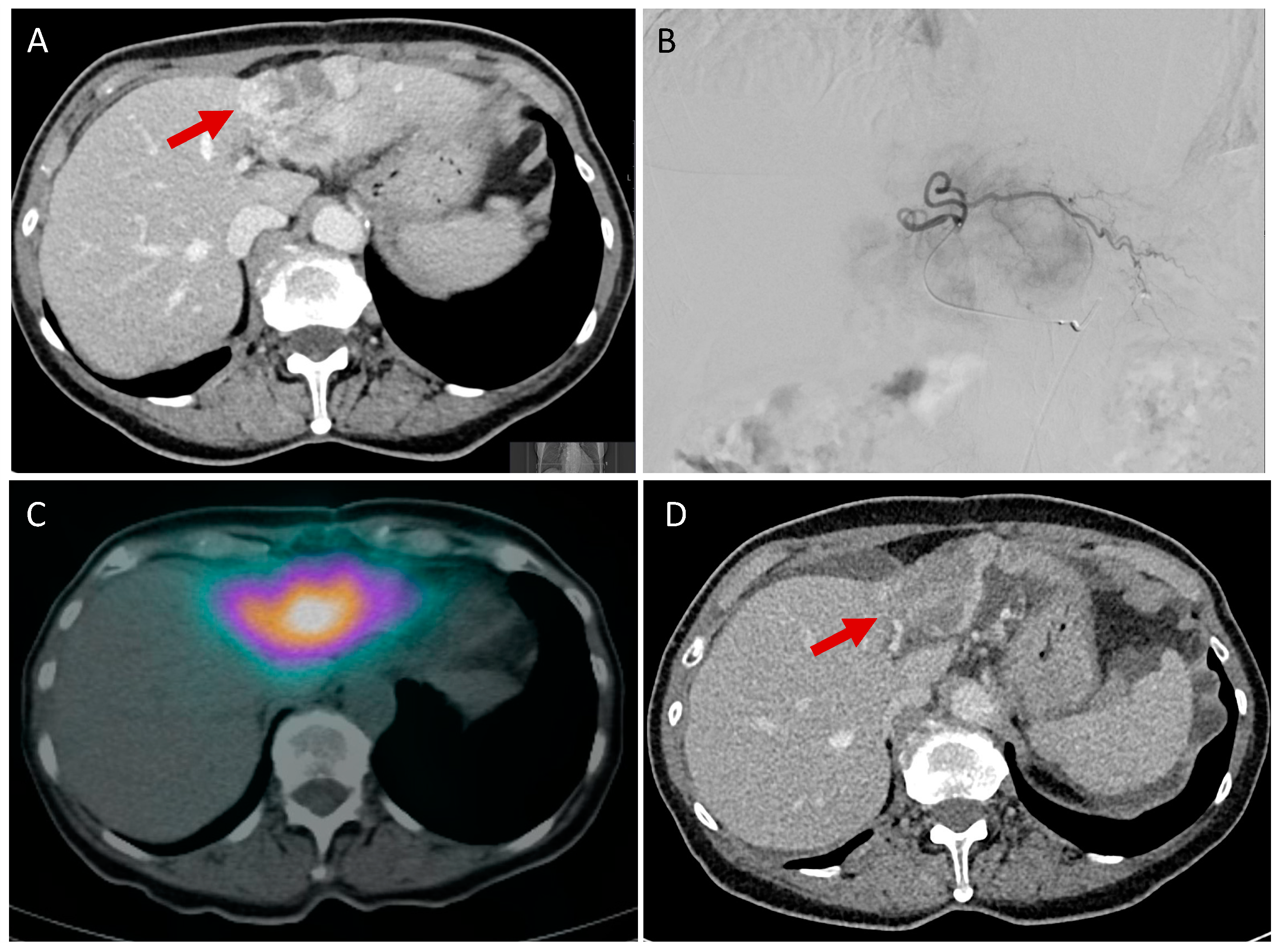
4. Selective Internal Radiotherapy (SIRT)
5. Hepatic Artery Infusion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Saha, S.K.; Zhu, A.X.; Fuchs, C.S.; Brooks, G.A. Forty-Year Trends in Cholangiocarcinoma Incidence in the U.S.: Intrahepatic Disease on the Rise. Oncologist 2016, 21, 594–599. [Google Scholar] [CrossRef]
- Patel, T. Increasing Incidence and Mortality of Primary Intrahepatic Cholangiocarcinoma in the United States. Hepatology 2001, 33, 1353–1357. [Google Scholar] [CrossRef]
- Everhart, J.E.; Ruhl, C.E. Burden of Digestive Diseases in the United States Part III: Liver, Biliary Tract, and Pancreas. Gastroenterology 2009, 136, 1134–1144. [Google Scholar] [CrossRef] [PubMed]
- Jarnagin, W.R.; Fong, Y.; DeMatteo, R.P.; Gonen, M.; Burke, E.C.; BS, J.B.; BA, M.Y.; Klimstra, D.; Blumgart, L.H. Staging, Resectability, and Outcome in 225 Patients with Hilar Cholangiocarcinoma. Ann. Surg. 2001, 234, 507–519. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Tsilimigras, D.I.; Paredes, A.Z.; Mehta, R.; Hyer, J.M.; Merath, K.; Sahara, K.; Bagante, F.; Beal, E.W.; Shen, F.; et al. Trends in the Incidence, Treatment and Outcomes of Patients with Intrahepatic Cholangiocarcinoma in the USA: Facility Type Is Associated with Margin Status, Use of Lymphadenectomy and Overall Survival. World J. Surg. 2019, 43, 1777–1787. [Google Scholar] [CrossRef] [PubMed]
- Spolverato, G.; Kim, Y.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; Gamblin, T.C.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; et al. Management and Outcomes of Patients with Recurrent Intrahepatic Cholangiocarcinoma Following Previous Curative-Intent Surgical Resection. Ann. Surg. Oncol. 2016, 23, 235–243. [Google Scholar] [CrossRef]
- Nguyen, C.L.; Scott, W.J.; Goldberg, M. Radiofrequency Ablation of Lung Malignancies. Ann. Thorac. Surg. 2006, 82, 365–371. [Google Scholar] [CrossRef]
- Třeška, V.; Brůha, J.; Skalický, T.; Liška, V.; Fichtl, J.; Mírka, H.; Korčáková, E. Radiofrequency Ablation of Colorectal Liver Metastases. Rozhl. V Chir. Mesic. Ceskoslovenske Chir. Spol. 2019, 98, 399–403. [Google Scholar]
- Slabaugh, T.K.; Ogan, K. Renal Tumor Radiofrequency Ablation. Ital. J. Urol. Nephrol. 2005, 57, 261–269. [Google Scholar]
- Slakey, D.P. Radiofrequency Ablation of Recurrent Cholangiocarcinoma. Am. Surg. 2002, 68, 395–397. [Google Scholar] [CrossRef]
- Fu, Y.; Yang, W.; Wu, W.; Yan, K.; Xing, B.C.; Chen, M.H. Radiofrequency Ablation in the Management of Unresectable Intrahepatic Cholangiocarcinoma. J. Vasc. Interv. Radiol. 2012, 23, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Haidu, M.; Dobrozemsky, G.; Schullian, P.; Widmann, G.; Klaus, A.; Weiss, H.; Margreiter, R.; Bale, R. Stereotactic Radiofrequency Ablation of Unresectable Intrahepatic Cholangiocarcinomas: A Retrospective Study. Cardiovasc. Interv. Radiol. 2012, 35, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Kamphues, C.; Seehofer, D.; Eisele, R.M.; Denecke, T.; Pratschke, J.; Neumann, U.P.; Neuhaus, P. Recurrent Intrahepatic Cholangiocarcinoma: Single-center Experience Using Repeated Hepatectomy and Radiofrequency Ablation. J. Hepato-Biliary-Pancreat. Sci. 2010, 17, 509–515. [Google Scholar] [CrossRef]
- Kim, J.H.; Won, H.J.; Shin, Y.M.; Kim, P.N.; Lee, S.-G.; Hwang, S. Radiofrequency Ablation for Recurrent Intrahepatic Cholangiocarcinoma after Curative Resection. Eur. J. Radiol. 2011, 80, e221–e225. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Won, H.J.; Shin, Y.M.; Kim, K.-A.; Kim, P.N. Radiofrequency Ablation for the Treatment of Primary Intrahepatic Cholangiocarcinoma. Am. J. Roentgenol. 2011, 196, W205–W209. [Google Scholar] [CrossRef]
- Giorgio, A.; Calisti, G.; Stefano, G.D.; Farella, N.; Sarno, A.D.; Amendola, F.; Scognamiglio, U.; Giorgio, V. Radiofrequency Ablation for Intrahepatic Cholangiocarcinoma: Retrospective Analysis of a Single Centre Experience. Anticancer. Res. 2011, 31, 4575–4580. [Google Scholar]
- Fukuda, K.; Mori, K.; Hasegawa, N.; Nasu, K.; Ishige, K.; Okamoto, Y.; Shiigai, M.; Abei, M.; Minami, M.; Hyodo, I. Safety Margin of Radiofrequency Ablation for Hepatocellular Carcinoma: A Prospective Study Using Magnetic Resonance Imaging with Superparamagnetic Iron Oxide. Jpn. J. Radiol. 2019, 37, 555–563. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, W.J.; Rhim, H.; Lim, H.K.; Choi, D.; Lee, J.Y. The Minimal Ablative Margin of Radiofrequency Ablation of Hepatocellular Carcinoma (>2 and <5 Cm) Needed to Prevent Local Tumor Progression: 3D Quantitative Assessment Using CT Image Fusion. Am. J. Roentgenol. 2010, 195, 758–765. [Google Scholar] [CrossRef]
- Han, K.; Ko, H.K.; Kim, K.W.; Won, H.J.; Shin, Y.M.; Kim, P.N. Radiofrequency Ablation in the Treatment of Unresectable Intrahepatic Cholangiocarcinoma: Systematic Review and Meta-Analysis. J. Vasc. Interv. Radiol. 2015, 26, 943–948. [Google Scholar] [CrossRef]
- Shindoh, J. Ablative Therapies for Intrahepatic Cholangiocarcinoma. Hepatobiliary Surg. Nutr. 2016, 6, 2–6. [Google Scholar] [CrossRef]
- Chu, H.H.; Kim, J.H.; Shin, Y.M.; Won, H.J.; Kim, P.-N. Percutaneous Radiofrequency Ablation for Recurrent Intrahepatic Cholangiocarcinoma After Curative Resection: Multivariable Analysis of Factors Predicting Survival Outcomes. Am. J. Roentgenol. 2021, 217, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Yousaf, A.; Kim, J.U.; Eliahoo, J.; Taylor-Robinson, S.D.; Khan, S.A. Ablative Therapy for Unresectable Intrahepatic Cholangiocarcinoma: A Systematic Review and Meta-Analysis. J. Clin. Exp. Hepatol. 2019, 9, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Chen, G.; Wang, H.; Li, H.; Xiao, J.; Duan, X.; He, J.; He, K.; Xiang, G. Increased Survival in Hepatocellular Carcinoma with Iodine-125 Implantation plus Radiofrequency Ablation: A Prospective Randomized Controlled Trial. J. Hepatol. 2014, 61, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.-W.; Zhang, Y.-J.; Chen, M.-S.; Xu, L.; Liang, H.-H.; Lin, X.-J.; Guo, R.-P.; Zhang, Y.-Q.; Lau, W.Y. Radiofrequency Ablation with or Without Transcatheter Arterial Chemoembolization in the Treatment of Hepatocellular Carcinoma: A Prospective Randomized Trial. J. Clin. Oncol. 2012, 31, 426–432. [Google Scholar] [CrossRef]
- Yu, M.-A.; Liang, P.; Yu, X.-L.; Cheng, Z.-G.; Han, Z.-Y.; Liu, F.-Y.; Yu, J. Sonography-Guided Percutaneous Microwave Ablation of Intrahepatic Primary Cholangiocarcinoma. Eur. J. Radiol. 2011, 80, 548–552. [Google Scholar] [CrossRef]
- Zhang, K.; Yu, J.; Yu, X.; Han, Z.; Cheng, Z.; Liu, F.; Liang, P. Clinical and Survival Outcomes of Percutaneous Microwave Ablation for Intrahepatic Cholangiocarcinoma. Int. J. Hyperther. 2018, 34, 292–297. [Google Scholar] [CrossRef]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef]
- Wu, S.; Hou, J.; Ding, Y.; Wu, F.; Hu, Y.; Jiang, Q.; Mao, P.; Yang, Y. Cryoablation Versus Radiofrequency Ablation for Hepatic Malignancies. Medicine 2015, 94, e2252. [Google Scholar] [CrossRef]
- Mafeld, S.; Wong, J.J.; Kibriya, N.; Stenberg, B.; Manas, D.; Bassett, P.; Aslam, T.; Evans, J.; Littler, P. Percutaneous Irreversible Electroporation (IRE) of Hepatic Malignancy: A Bi-Institutional Analysis of Safety and Outcomes. Cardiovasc. Interv. Radiol. 2019, 42, 577–583. [Google Scholar] [CrossRef]
- Kiefer, M.V.; Albert, M.; McNally, M.; Robertson, M.; Sun, W.; Fraker, D.; Olthoff, K.; Christians, K.; Pappas, S.; Rilling, W.; et al. Chemoembolization of Intrahepatic Cholangiocarcinoma with Cisplatinum, Doxorubicin, Mitomycin C, Ethiodol, and Polyvinyl Alcohol. Cancer 2011, 117, 1498–1505. [Google Scholar] [CrossRef]
- Goerg, F.; Zimmermann, M.; Bruners, P.; Neumann, U.; Luedde, T.; Kuhl, C. Chemoembolization with Degradable Starch Microspheres for Treatment of Patients with Primary or Recurrent Unresectable, Locally Advanced Intrahepatic Cholangiocarcinoma: A Pilot Study. Cardiovasc. Interv. Radiol. 2019, 42, 1709–1717. [Google Scholar] [CrossRef] [PubMed]
- Mondaca, S.; Yarmohammadi, H.; Kemeny, N.E. Regional Chemotherapy for Biliary Tract Tumors and Hepatocellular Carcinoma. Surg. Oncol. Clin. N. Am. 2019, 28, 717–729. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C.G.; Simo, K.A.; Hansen, P.; Rocha, F.; Philips, P.; McMasters, K.M.; Tatum, C.M.; Kelly, L.R.; Driscoll, M.; Sharma, V.R.; et al. Drug-Eluting Bead, Irinotecan Therapy of Unresectable Intrahepatic Cholangiocarcinoma (DELTIC) with Concomitant Systemic Gemcitabine and Cisplatin. Ann. Surg. Oncol. 2022, 29, 5462–5473. [Google Scholar] [CrossRef] [PubMed]
- Yuan, P.; Song, J.; Wang, F.; Zhu, G.; Chen, B. Combination of TACE and Lenvatinib as a Promising Option for Downstaging to Surgery of Initially Unresectable Intrahepatic Cholangiocarcinoma. Investig. New Drug. 2022, 40, 1125–1132. [Google Scholar] [CrossRef]
- Kudo, M.; Ueshima, K.; Ikeda, M.; Torimura, T.; Tanabe, N.; Aikata, H.; Izumi, N.; Yamasaki, T.; Nojiri, S.; Hino, K.; et al. Randomised, Multicentre Prospective Trial of Transarterial Chemoembolisation (TACE) plus Sorafenib as Compared with TACE Alone in Patients with Hepatocellular Carcinoma: TACTICS Trial. Gut 2020, 69, 1492–1501. [Google Scholar] [CrossRef]
- Kloeckner, R.; Ruckes, C.; Kronfeld, K.; Wörns, M.A.; Weinmann, A.; Galle, P.R.; Lang, H.; Otto, G.; Eichhorn, W.; Schreckenberger, M.; et al. Selective Internal Radiotherapy (SIRT) versus Transarterial Chemoembolization (TACE) for the Treatment of Intrahepatic Cholangiocellular Carcinoma (CCC): Study Protocol for a Randomized Controlled Trial. Trials 2014, 15, 311. [Google Scholar] [CrossRef]
- Edeline, J.; Touchefeu, Y.; Guiu, B.; Farge, O.; Tougeron, D.; Baumgaertner, I.; Ayav, A.; Campillo-Gimenez, B.; Beuzit, L.; Pracht, M.; et al. Radioembolization Plus Chemotherapy for First-Line Treatment of Locally Advanced Intrahepatic Cholangiocarcinoma. JAMA Oncol. 2020, 6, 51–59. [Google Scholar] [CrossRef]
- Mouli, S.; Memon, K.; Baker, T.; Benson, A.B.; Mulcahy, M.F.; Gupta, R.; Ryu, R.K.; Salem, R.; Lewandowski, R.J. Yttrium-90 Radioembolization for Intrahepatic Cholangiocarcinoma: Safety, Response, and Survival Analysis. J. Vasc. Interv. Radiol. 2013, 24, 1227–1234. [Google Scholar] [CrossRef]
- Edeline, J.; Du, F.L.; Rayar, M.; Rolland, Y.; Beuzit, L.; Boudjema, K.; Rohou, T.; Latournerie, M.; Campillo-Gimenez, B.; Garin, E.; et al. Glass Microspheres 90Y Selective Internal Radiation Therapy and Chemotherapy as First-Line Treatment of Intrahepatic Cholangiocarcinoma. Clin. Nucl. Med. 2015, 40, 851–855. [Google Scholar] [CrossRef]
- Levillain, H.; Derijckere, I.D.; Ameye, L.; Guiot, T.; Braat, A.; Meyer, C.; Vanderlinden, B.; Reynaert, N.; Hendlisz, A.; Lam, M.; et al. Personalised Radioembolization Improves Outcomes in Refractory Intra-Hepatic Cholangiocarcinoma: A Multicenter Study. Eur. J. Nucl. Med. Mol. I 2019, 46, 2270–2279. [Google Scholar] [CrossRef]
- Levillain, H.; Derijckere, I.D.; Marin, G.; Guiot, T.; Vouche, M.; Reynaert, N.; Hendlisz, A.; Vanderlinden, B.; Flamen, P. 90Y-PET/CT-Based Dosimetry after Selective Internal Radiation Therapy Predicts Outcome in Patients with Liver Metastases from Colorectal Cancer. Ejnmmi Res. 2018, 8, 60. [Google Scholar] [CrossRef]
- Dieudonné, A.; Garin, E.; Laffont, S.; Rolland, Y.; Lebtahi, R.; Leguludec, D.; Gardin, I. Clinical Feasibility of Fast 3-Dimensional Dosimetry of the Liver for Treatment Planning of Hepatocellular Carcinoma with 90Y-Microspheres. J. Nucl. Med. 2011, 52, 1930–1937. [Google Scholar] [CrossRef] [PubMed]
- Dewaraja, Y.K.; Devasia, T.; Kaza, R.K.; Mikell, J.K.; Owen, D.; Roberson, P.L.; Schipper, M. Prediction of Tumor Control in 90Y Radioembolization by Logit Models with PET/CT Based Dose Metrics. J. Nucl. Med. 2019, 61, jnumed.119.226472. [Google Scholar] [CrossRef]
- Cremonesi, M.; Chiesa, C.; Strigari, L.; Ferrari, M.; Botta, F.; Guerriero, F.; Cicco, C.D.; Bonomo, G.; Orsi, F.; Bodei, L.; et al. Radioembolization of Hepatic Lesions from a Radiobiology and Dosimetric Perspective. Front. Oncol. 2014, 4, 210. [Google Scholar] [CrossRef] [PubMed]
- Levillain, H.; Bagni, O.; Deroose, C.M.; Dieudonné, A.; Gnesin, S.; Grosser, O.S.; Kappadath, S.C.; Kennedy, A.; Kokabi, N.; Liu, D.M.; et al. International Recommendations for Personalised Selective Internal Radiation Therapy of Primary and Metastatic Liver Diseases with Yttrium-90 Resin Microspheres. Eur. J. Nucl. Med. Mol. I 2021, 48, 1570–1584. [Google Scholar] [CrossRef]
- Leal, J.N.; Kingham, T.P. Hepatic Artery Infusion Chemotherapy for Liver Malignancy. Surg. Oncol. Clin. N. Am. 2015, 24, 121–148. [Google Scholar] [CrossRef]
- Ensminger, W.D. Regional Chemotherapy. Semin. Oncol. 1993, 20, 3–11. [Google Scholar] [PubMed]
- Konstantinidis, I.T.; Koerkamp, B.G.; Do, R.K.G.; Gönen, M.; Fong, Y.; Allen, P.J.; D’Angelica, M.I.; Kingham, T.P.; DeMatteo, R.P.; Klimstra, D.S.; et al. Unresectable Intrahepatic Cholangiocarcinoma: Systemic plus Hepatic Arterial Infusion Chemotherapy Is Associated with Longer Survival in Comparison with Systemic Chemotherapy Alone. Cancer 2016, 122, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.-J.; He, M.-K.; Chen, H.-W.; Fang, W.-Q.; Zhou, Y.-M.; Xu, L.; Wei, W.; Zhang, Y.-J.; Guo, Y.; Guo, R.-P.; et al. Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin Versus Transarterial Chemoembolization for Large Hepatocellular Carcinoma: A Randomized Phase III Trial. J. Clin. Oncol. 2022, 40, 150–160. [Google Scholar] [CrossRef]
- Mei, J.; Tang, Y.-H.; Wei, W.; Shi, M.; Zheng, L.; Li, S.-H.; Guo, R.-P. Hepatic Arterial Infusion Chemotherapy Combined With PD-1 Inhibitors Plus Lenvatinib Versus PD-1 Inhibitors Plus Lenvatinib for Advanced Hepatocellular Carcinoma. Front. Oncol. 2021, 11, 618206. [Google Scholar] [CrossRef]
- Zhang, Q.; Liu, X.; Wei, S.; Zhang, L.; Tian, Y.; Gao, Z.; Jin, M.; Yan, S. Lenvatinib Plus PD-1 Inhibitors as First-Line Treatment in Patients with Unresectable Biliary Tract Cancer: A Single-Arm, Open-Label, Phase II Study. Front. Oncol. 2021, 11, 751391. [Google Scholar] [CrossRef] [PubMed]
- Cercek, A.; Boerner, T.; Tan, B.R.; Chou, J.F.; Gönen, M.; Boucher, T.M.; Hauser, H.F.; Do, R.K.G.; Lowery, M.A.; Harding, J.J.; et al. Assessment of Hepatic Arterial Infusion of Floxuridine in Combination with Systemic Gemcitabine and Oxaliplatin in Patients with Unresectable Intrahepatic Cholangiocarcinoma. JAMA Oncol. 2020, 6, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, N.; Yamakado, K.; Nakatsuka, A.; Fujii, A.; Matsumura, K.; Takeda, K. Arterial Chemoinfusion Therapy through an Implanted Port System for Patients with Unresectable Intrahepatic Cholangiocarcinoma—Initial Experience. Eur. J. Radiol. 2002, 41, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Cantore, M.; Mambrini, A.; Fiorentini, G.; Rabbi, C.; Zamagni, D.; Caudana, R.; Pennucci, C.; Sanguinetti, F.; Lombardi, M.; Nicoli, N. Phase II Study of Hepatic Intraarterial Epirubicin and Cisplatin, with Systemic 5-fluorouracil in Patients with Unresectable Biliary Tract Tumors. Cancer 2005, 103, 1402–1407. [Google Scholar] [CrossRef]
- Mambrini, A.; Guglielmi, A.; Pacetti, P.; Iacono, C.; Torri, T.; Auci, A.; Nicoli, N.; Orlandi, M.; Guadagni, S.; Fiorentini, G.; et al. Capecitabine plus Hepatic Intra-Arterial Epirubicin and Cisplatin in Unresectable Biliary Cancer: A Phase II Study. Anticancer. Res. 2007, 27, 3009–3013. [Google Scholar]
- Sinn, M.; Nicolaou, A.; Gebauer, B.; Podrabsky, P.; Seehofer, D.; Ricke, J.; Dörken, B.; Riess, H.; Hildebrandt, B. Hepatic Arterial Infusion with Oxaliplatin and 5-FU/Folinic Acid for Advanced Biliary Tract Cancer: A Phase II Study. Digest. Dis. Sci. 2013, 58, 2399–2405. [Google Scholar] [CrossRef]
- Ray, C.E.; Edwards, A.; Smith, M.T.; Leong, S.; Kondo, K.; Gipson, M.; Rochon, P.J.; Gupta, R.; Messersmith, W.; Purcell, T.; et al. Metaanalysis of Survival, Complications, and Imaging Response Following Chemotherapy-Based Transarterial Therapy in Patients with Unresectable Intrahepatic Cholangiocarcinoma. J. Vasc. Interv. Radiol. 2013, 24, 1218–1226. [Google Scholar] [CrossRef]
- Edeline, J.; Lamarca, A.; McNamara, M.G.; Jacobs, T.; Hubner, R.A.; Palmer, D.; Koerkamp, B.G.; Johnson, P.; Guiu, B.; Valle, J.W. Locoregional Therapies in Patients with Intrahepatic Cholangiocarcinoma: A Systematic Review and Pooled Analysis. Cancer Treat. Rev. 2021, 99, 102258. [Google Scholar] [CrossRef]
| Procedure | Official Title (ClinicalTrials.Gov Identifier) | Study Design | Arm (s) | Recruitment Status |
|---|---|---|---|---|
| Ablation | Phase III Study of Radiofrequency Ablation Combined with Cytokine-Induced Killer Cells for the Patients with Cholangiocarcinoma (NCT02482454) | Interventional (Clinical Trial) (50 participants) | RFA alone vs. RFA + CIK | Active, not recruiting |
| Ablation | Clinical Effect and Safety of Photodynamic Therapy Versus Radiofrequency Ablation Versus Photodynamic Therapy Plus Radiofrequency Ablation for Unresectable Extrahepatic Cholangiocarcinoma (NCT05519319) | Interventional (Clinical Trial) (70 participants) | Photodynamic therapy (PDT) vs. radiofrequency ablation (RFA) vs. RFA + PDT | Recruiting |
| Ablation | A Combined Endoscopy and Radiology-guided Radiofrequency Ablation Therapy Protocol for Inoperable Perihilar Cholangiocarcinoma (NCT05563870) | Interventional (Clinical Trial) (30 participants) | Endoscopic drainage arm vs. COMBO-RFA arm | Recruiting |
| Ablation | A Phase II Study of Cryoablation Combined with Sintilimab Plus Lenvatinib in Patients with Advanced Intrahepatic Cholangiocarcinoma (CASTLE-01) (NCT05010668) | Interventional (Clinical Trial) (25 participants) | Cryoablation in combination with sintilimab plus lenvatinib | Recruiting |
| Ablation | A Phase II Study of Cryoablation Combined with Anti-PD-1 Antibody (SHR-1210) in Patients with Advanced Intrahepatic Cholangiocarcinoma (NCT04299581) | Interventional (Clinical Trial) (25 participants) | Cryoablation in combination with camrelizumab | Recruiting |
| Ablation | Endobiliary Radiofrequency Ablation for Malignant Biliary Obstruction Due to Perihilar Cholangiocarcinoma: A Randomized Controlled Trial (NCT05546372) | Interventional (Clinical Trial) (98 participants) | Endobiliary RFA + stent placement vs. stent placement only | Recruiting |
| Ablation | Prospective Evaluation of the Ablation Therapy with Bipolar Radio Frequency for Nonresectable Bile Duct Cancer (NCT03679338) | Interventional (Clinical Trial) (20 participants) | Ablation therapy with bipolar radio frequency | Active, not recruiting |
| TACE | TACE Combined with “Target Immune” Therapy for First-Line Treatment Compared with Intravenous Chemotherapy in the Treatment of Unresectable Intrahepatic Cholangiocarcinoma: A Prospective, Multicenter, Open, Real-World Clinical Study (NCT05247996) | Interventional (Clinical Trial) (98 participants) | Transcatheter arterial chemoembolization combined with “target immune” therapy | Not yet recruiting |
| TACE | A Phase II Study of Transcatheter Arterial Chemoembolization (TACE) Combined with Tislelizumab in Patients with Advanced Intrahepatic Cholangiocarcinoma (NCT04954781) | Interventional (Clinical Trial) (25 participants) | TACE in combination with tislelizumab | Recruiting |
| TACE | A Single-Arm, Open-Label, Multicenter Phase II Clinical Study to Evaluate the Safety and Efficacy of Toripalimab Injection Combined with TACE in the Treatment of Extrahepatic Cholangiocarcinoma (NCT05448183) | Interventional (Clinical Trial) (45 participants) | Toripalimab combined with TACE | Recruiting |
| TACE | Combined Therapy Using D-TACE, Gemcitabine and Cisplatin Chemotherapy, and PD1 Antibody for Patients with Advanced and Unresectable Intrahepatic Cholangiocarcinoma: A Single-Center, Single-Arm Trial (NCT05738057) | Interventional (Clinical Trial) (22 participants) | Combined therapy using D-TACE, gemcitabine and cisplatin, and camrelizumab | Not yet recruiting |
| TACE | Single-Arm, Multicenter II Phase Clinical Study of DEB-TACE Combined with Surufatinib and Camrelizumab in the Treatment of Inoperable or Metastatic Intrahepatic Cholangiocarcinoma (NCT05236699) | Interventional (Clinical Trial) (18 participants) | DEB-TACE combined with surufatinib and camrelizumab | Not yet recruiting |
| TACE | Drug-Eluting Beads Transarterial Chemoembolization Combined with Apatinib and PD-1 Antibody for the Treatment of Intrahepatic Cholangiocarcinoma That Has Progressed after Standard First-Line Chemotherapy (NCT04834674) | Interventional (Clinical Trial) (20 participants) | DEB-TACE combined with apatinib and PD-1 antibody | Not yet recruiting |
| SIRT/TACE | Selective Internal Radiotherapy Is Superior to Transarterial Chemoembolization for the Treatment of Intrahepatic Cholangiocellular Carcinoma (CCC) (NCT01798147) | Interventional (Clinical Trial) (24 participants) | DEB-TACE (doxorubicin) vs. Y90-SIRT | Status unknown |
| SIRT | A Traditional Feasibility Study of Gemcitabine, Cisplatin, and 90Y TARE for Unresectable Intrahepatic Cholangiocarcinoma (NCT02512692) | Interventional (Clinical Trial) (6 participants) | 90Y TARE with gemcitabine and cisplatin | Active, not recruiting |
| SIRT | Prospective, Multicenter, Randomized, Controlled Study Evaluating SIR-Spheres Y-90 Resin Microspheres Preceding Cisplatin-Gemcitabine (CIS-GEM) Chemotherapy Versus CIS-GEM Chemotherapy Alone as First-line Treatment of Patients with Unresectable Intrahepatic Cholangiocarcinoma (NCT02807181) | Interventional (Clinical Trial) (89 participants) | Chemotherapy (cisplatin-gemcitabine) vs. radiation: SIRT + chemotherapy (cisplatin-gemcitabine) | Active, not recruiting |
| SIRT | A Phase II Trial of Induction Gemcitabine, Cisplatin and Nab-Paclitaxel Triplet Chemotherapy Followed by Gemcitabine, Cisplatin, and Radioembolization for the Treatment of Locally Advanced Unresectable Intrahepatic Cholangiocarcinoma (NCT05422690) | Interventional (Clinical Trial) (16 participants) | Gemcitabine, cisplatin and nab-paclitaxel chemotherapy with Yittrium-90 | Not yet recruiting |
| SIRT | Phase II Study of Immunotherapy With Durvalumab (MEDI4736) or Durvalumab and Tremelimumab, Both Combined with Y-90 SIRT Therapy in Advanced Stage Intrahepatic Biliary Tract Cancer (BTC) (NCT04238637) | Interventional (Clinical Trial) (50 participants) | Durvalumab vs. durvalumab in combination with tremelimumab | Recruiting |
| SIRT | A Single-Arm Phase 2 Study of Y-90 SIRT in Combination with Durvalumab (MEDI 4736) and Gemcitabine/Cisplatin in Locally Advanced, Unresectable or Metastatic Intrahepatic Cholangiocarcinoma (NCT05655949) | Interventional (Clinical Trial) (30 participants) | Gemcitabine + cisplatin + durvalumab + Yttrium-90 selective internal radiation therapy | Not yet recruiting |
| Hepatic Artery Infusion | Recombinant Human Adenovirus Type 5 Combined With Hepatic Artery Infusion Chemotherapy of FOLFOX in Patients With Intrahepatic Mass-forming Cholangiocarcinoma: a Single-site, Single-arm, Prospective Study (NCT05124002) | Interventional (Clinical Trial) (66 participants) | Recombinant human adenovirus type 5 (H101) + HAIC (FOLFOX) | Not yet recruiting |
| Hepatic Artery Infusion | Hepatic Arterial Infusion Chemotherapy Combined with Sintilimab and Bevacizumab in the Treatment of Unresectable Intrahepatic Cholangiocarcinoma: A Prospective, Single-Center, Phase II Study (NCT05400902) | Interventional (Clinical Trial) (17 participants) | HAIC combined with sintilimab and bevacizumab | Recruiting |
| Hepatic Artery Infusion | Hepatic Arterial Infusion Chemotherapy Combined with Tislelizumab and Apatinib in the Treatment of Unresectable Intrahepatic Cholangiocarcinoma: A Prospective, Single-Center, Phase II Study (NCT05290116) | Interventional (Clinical Trial) (17 participants) | HAIC combined with tislelizumab and apatinib | Recruiting |
| Hepatic Artery Infusion | Randomized, Controlled Study to Compare the Efficacy, Safety and Pharmacokinetics of Melphalan/HDS Treatment Given Sequentially Following Cisplatin/Gemcitabine Versus Cisplatin/Gemcitabine in Patients with Intrahepatic Cholangiocarcinoma (NCT03086993) | Interventional (Clinical Trial) (295 participants) | Melphalan/PHP vs. cisplatin and gemcitabine | Active, not recruiting |
| Hepatic Artery Infusion | Hepatic Arterial Infusion of Gemcitabine-oxaliplatin for Second-line Therapy in Non-metastatic Unresectable Intra-hepatic Cholangiocarcinoma: a Multicentric Single-Arm Phase II Study (NCT03364530) | Interventional (Clinical Trial) (40 participants) | Gemcitabine-oxaliplatin regimen | Status unknown |
| Hepatic Artery Infusion | Hepatic Arterial Infusion Chemotherapy (HAIC) Combined with Donafenib and Sintilimab in First-Line Treatment of Unresectable Intrahepatic Cholangiocarcinoma (ICC): A Prospective, Open-Label, Phase II Study (NCT05348811) | Interventional (Clinical Trial) (32 participants) | HAIC combined with donafenib and sintilimab | Recruiting |
| Hepatic Artery Infusion | Hepatic Arterial Infusion Chemotherapy of Oxaliplatin, 5-Fluorouracil, and Leucovorin Versus Systemic Chemotherapy of Gemcitabine and Cisplatin for Unresectable Intrahepatic Cholangiocarcinoma (NCT04961970) | Interventional (Clinical Trial) (188 participants) | Hepatic artery infusion chemotherapy vs. systemic chemotherapy | Recruiting |
| Hepatic Artery Infusion | Hepatic Arterial Infusion Chemotherapy of Irinotecan, Oxaliplatin, 5-Fluorouracil, and Leucovorin Versus Systemic Chemotherapy of Gemcitabine and Oxaliplatin for Unresectable Intrahepatic Cholangiocarcinoma (NCT03771846) | Interventional (Clinical Trial) (188 participants) | Hepatic artery infusion chemotherapy vs. systemic chemotherapy | Status unknown |
| Hepatic Artery Infusion | A Phase II Study of Hepatic Arterial Infusion (HAI) with Floxuridine (FUDR) and Dexamethasone (Dex) Combined with Systemic Gemcitabine and Oxaliplatin in Patients with Unresectable Intrahepatic Cholangiocarcinoma (ICC) (NCT01862315) | Interventional (Clinical Trial) (55 participants) | No prior chemo or responded/stable with prior chemo vs. patients who have failed systemic therapy vs. patients who have had prior oxaliplatin and have existing neuropathy | Active, not recruiting |
| Hepatic Artery Infusion | Prospective Multicenter Trial of Biliary Drainage Plus Hepatic Arterial Infusion Chemotherapy Versus Biliary Drainage Plus Best Supportive Care in Locally Advanced Perihilar Cholangiocarcinomas (NCT05024513) | Interventional (Clinical Trial) (127 participants) | BD-HAIC (biliary drainage and HAIC) vs. BD-BSC (biliary drainage and best supportive care) | Recruiting |
| Hepatic Artery Infusion | A Phase II Study of Induction Systemic mFOLFIRINOX Followed by Hepatic Arterial Infusion of Floxuridine and Dexamethasone Given Concurrently With Systemic mFOLFIRI as a First-Line Therapy in Patients with Unresectable Liver-Dominant Intrahepatic Cholangiocarcinoma (NCT04251715) | Interventional (Clinical Trial) (30 participants) | mFOLFIRINOX, floxuridine-DEX, mFOLFIRI | Recruiting |
| Hepatic Artery Infusion | Phase II Study Evaluating the Efficacy of M9241 in Combination with Hepatic Artery Infusion Pump (HAIP) and Systemic Therapy for Subjects with Metastatic Colorectal Cancer or Intrahepatic Cholangiocarcinoma (NCT05286814) | Interventional (Clinical Trial) (48 participants) | M9241 + HAIP FUDR and dexamethasone chemotherapy in combination with FOLFOX or FOLFIRI vs. M9241 + HAIP FUDR and dexamethasone chemotherapy in combination with GemOx | Recruiting |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morawitz, J.; Bruckmann, N.-M.; Jannusch, K.; Kirchner, J.; Antoch, G.; Loosen, S.; Luedde, T.; Roderburg, C.; Minko, P. Update on Locoregional Therapies for Cholangiocellular Carcinoma. Cancers 2023, 15, 2368. https://doi.org/10.3390/cancers15082368
Morawitz J, Bruckmann N-M, Jannusch K, Kirchner J, Antoch G, Loosen S, Luedde T, Roderburg C, Minko P. Update on Locoregional Therapies for Cholangiocellular Carcinoma. Cancers. 2023; 15(8):2368. https://doi.org/10.3390/cancers15082368
Chicago/Turabian StyleMorawitz, Janna, Nils-Martin Bruckmann, Kai Jannusch, Julian Kirchner, Gerald Antoch, Sven Loosen, Tom Luedde, Christoph Roderburg, and Peter Minko. 2023. "Update on Locoregional Therapies for Cholangiocellular Carcinoma" Cancers 15, no. 8: 2368. https://doi.org/10.3390/cancers15082368
APA StyleMorawitz, J., Bruckmann, N.-M., Jannusch, K., Kirchner, J., Antoch, G., Loosen, S., Luedde, T., Roderburg, C., & Minko, P. (2023). Update on Locoregional Therapies for Cholangiocellular Carcinoma. Cancers, 15(8), 2368. https://doi.org/10.3390/cancers15082368








