A Novel Score Using Lymphocyte-to-Monocyte Ratio in Blood and Malignant Body Fluid for Predicting Prognosis of Patients with Advanced Ovarian Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. A New Score Using LMRs of Peripheral Blood and Malignant Body Fluid (bmLMR Score)
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
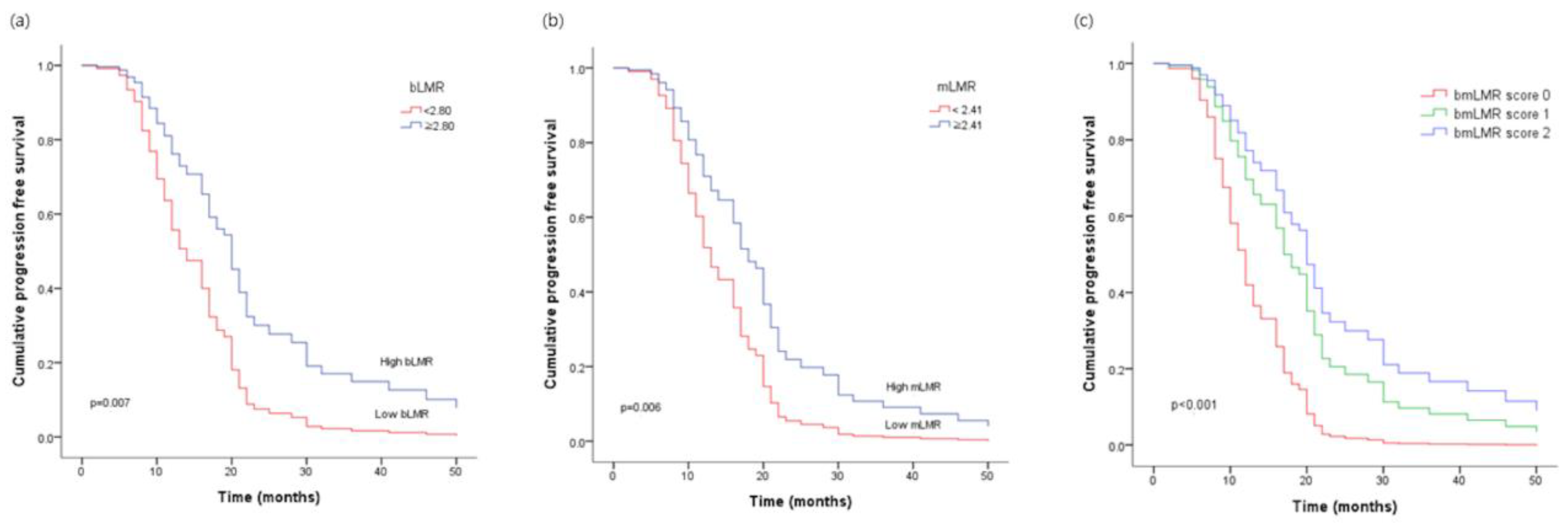
3.2. Univariate and Multivariate Analyses of Prognostic Factors for Progression-Free Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Sun, H.; Yang, L.; Deng, Y.; Yan, Y.; Wang, S.; Yang, G.; Ma, H. Improved survival in ovarian cancer, with widening survival gaps of races and socioeconomic status: A period analysis, 1983–2012. J. Cancer 2018, 9, 3548–3556. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Jiang, H.; Shu, C.; Hu, M.Q.; Huang, Y.; Liu, Q.; Li, R.F. Prognostic value of lymphocyte-to-monocyte ratio in ovarian cancer: A meta-analysis. J. Ovarian Res. 2019, 12, 51. [Google Scholar] [CrossRef]
- Nishijima, T.F.; Muss, H.B.; Shachar, S.S.; Tamura, K.; Takamatsu, Y. Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: A systematic review and meta-analysis. Cancer Treat. Rev. 2015, 41, 971–978. [Google Scholar] [CrossRef]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef]
- Zhu, J.Y.; Liu, C.C.; Wang, L.; Zhong, M.; Tang, H.L.; Wang, H. Peripheral blood lymphocyte-to-monocyte ratio as a prognostic factor in advanced epithelial ovarian cancer: A multicenter retrospective study. J. Cancer 2017, 8, 737–743. [Google Scholar] [CrossRef]
- Eo, W.K.; Chang, H.J.; Kwon, S.H.; Koh, S.B.; Kim, Y.O.; Ji, Y.I.; Kim, H.B.; Lee, J.Y.; Suh, D.S.; Kim, K.H.; et al. The Lymphocyte-Monocyte Ratio Predicts Patient Survival and Aggressiveness of Ovarian Cancer. J. Cancer 2016, 7, 289–296. [Google Scholar] [CrossRef]
- Jelovac, D.; Armstrong, D.K. Recent progress in the diagnosis and treatment of ovarian cancer. CA Cancer J. Clin. 2011, 61, 183–203. [Google Scholar] [CrossRef]
- Porcel, J.M.; Murata, P.; Porcel, L.; Bielsa, S.; Pardina, M.; Salud, A. Prevalence, clinical characteristics, and outcome of pleural effusions in ovarian cancer. Pleura Peritoneum 2021, 6, 75–81. [Google Scholar] [CrossRef]
- Rickard, B.P.; Conrad, C.; Sorrin, A.J.; Ruhi, M.K.; Reader, J.C.; Huang, S.A.; Franco, W.; Scarcelli, G.; Polacheck, W.J.; Roque, D.M.; et al. Malignant Ascites in Ovarian Cancer: Cellular, Acellular, and Biophysical Determinants of Molecular Characteristics and Therapy Response. Cancers 2021, 13, 4318. [Google Scholar] [CrossRef] [PubMed]
- Siravegna, G.; Marsoni, S.; Siena, S.; Bardelli, A. Integrating liquid biopsies into the management of cancer. Nat. Rev. Clin. Oncol. 2017, 14, 531–548. [Google Scholar] [CrossRef] [PubMed]
- Ryu, W.K.; Moon, Y.; Park, M.H.; Lim, J.H.; Kim, Y.S.; Lee, K.H.; Kwak, S.M.; Kim, C.; Nam, H.S. A Preliminary Study on the Prognostic Impact of Neutrophil to Lymphocyte Ratio of the Bronchoalveolar Lavage Fluid in Patients with Lung Cancer. Diagnostics 2021, 11, 2201. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Nam, H.S.; Lim, J.H.; Kim, J.S.; Moon, Y.; Cho, J.H.; Ryu, J.S.; Kwak, S.M.; Lee, H.L. Prognostic impact of a new score using neutrophil-to-lymphocyte ratios in the serum and malignant pleural effusion in lung cancer patients. BMC Cancer 2017, 17, 557. [Google Scholar] [CrossRef]
- Chan, J.C.; Chan, D.L.; Diakos, C.I.; Engel, A.; Pavlakis, N.; Gill, A.; Clarke, S.J. The Lymphocyte-to-Monocyte Ratio is a Superior Predictor of Overall Survival in Comparison to Established Biomarkers of Resectable Colorectal Cancer. Ann. Surg. 2017, 265, 539–546. [Google Scholar] [CrossRef]
- Kano, S.; Homma, A.; Hatakeyama, H.; Mizumachi, T.; Sakashita, T.; Kakizaki, T.; Fukuda, S. Pretreatment lymphocyte-to-monocyte ratio as an independent prognostic factor for head and neck cancer. Head Neck 2017, 39, 247–253. [Google Scholar] [CrossRef]
- Onoe, S.; Maeda, A.; Takayama, Y.; Fukami, Y.; Takahashi, T.; Uji, M.; Kaneoka, Y. The Prognostic Impact of the Lymphocyte-to-Monocyte Ratio in Resected Pancreatic Head Adenocarcinoma. Med. Princ. Pract. 2019, 28, 517–525. [Google Scholar] [CrossRef]
- Cho, H.E.; Kim, Y.J.; Cho, S.Y.; Park, T.S.; Park, K.S. Clinical application of an algorithm to screen for malignant cells in body fluids using an automated hematology analyzer. Int. J. Lab. Hematol. 2022, 44, 483–489. [Google Scholar] [CrossRef]
- Hothorn, T.; Zeileis, A. Generalized maximally selected statistics. Biometrics 2008, 64, 1263–1269. [Google Scholar] [CrossRef]
- Ezzati, M.; Abdullah, A.; Shariftabrizi, A.; Hou, J.; Kopf, M.; Stedman, J.K.; Samuelson, R.; Shahabi, S. Recent Advancements in Prognostic Factors of Epithelial Ovarian Carcinoma. Int. Sch. Res. Notices 2014, 2014, 953509. [Google Scholar] [CrossRef]
- Skírnisdóttir, I.; Sorbe, B. Prognostic factors for surgical outcome and survival in 447 women treated for advanced (FIGO-stages III-IV) epithelial ovarian carcinoma. Int. J. Oncol. 2007, 30, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Diakos, C.I.; Charles, K.A.; McMillan, D.C.; Clarke, S.J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014, 15, e493–e503. [Google Scholar] [CrossRef]
- Kitamura, T.; Qian, B.Z.; Pollard, J.W. Immune cell promotion of metastasis. Nat. Rev. Immunol. 2015, 15, 73–86. [Google Scholar] [CrossRef]
- Chanmee, T.; Ontong, P.; Konno, K.; Itano, N. Tumor-associated macrophages as major players in the tumor microenvironment. Cancers 2014, 6, 1670–1690. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.; Klink, M. The Role of Tumor-Associated Macrophages in the Progression and Chemoresistance of Ovarian Cancer. Cells 2020, 9, 1299. [Google Scholar] [CrossRef]
- Wang, H.; Tian, T.; Zhang, J. Tumor-Associated Macrophages (TAMs) in Colorectal Cancer (CRC): From Mechanism to Therapy and Prognosis. Int. J. Mol. Sci. 2021, 22, 8470. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Hu, H.Q.; Tang, F.X.; Lin, D.; Shen, R.; Deng, L.; Tang, Y.L.; Deng, L.H.; Zhou, M.; Li, J.; et al. Combined Preoperative LMR and CA125 for Prognostic Assessment of Ovarian Cancer. J. Cancer 2020, 11, 3165–3171. [Google Scholar] [CrossRef]
- Sangisetty, S.L.; Miner, T.J. Malignant ascites: A review of prognostic factors, pathophysiology and therapeutic measures. World J. Gastrointest. Surg. 2012, 4, 87–95. [Google Scholar] [CrossRef]
- Ford, C.E.; Werner, B.; Hacker, N.F.; Warton, K. The untapped potential of ascites in ovarian cancer research and treatment. Br. J. Cancer 2020, 123, 9–16. [Google Scholar] [CrossRef]
- Giarnieri, E.; Bellipanni, G.; Macaluso, M.; Mancini, R.; Holstein, A.C.; Milanese, C.; Giovagnoli, M.R.; Giordano, A.; Russo, G. Review: Cell Dynamics in Malignant Pleural Effusions. J. Cell. Physiol. 2015, 230, 272–277. [Google Scholar] [CrossRef]
- Lane, D.; Matte, I.; Garde-Granger, P.; Laplante, C.; Carignan, A.; Rancourt, C.; Piché, A. Inflammation-regulating factors in ascites as predictive biomarkers of drug resistance and progression-free survival in serous epithelial ovarian cancers. BMC Cancer 2015, 15, 492. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Cheng, W.F.; Chang, M.C.; Lin, H.W.; Huang, C.T.; Chien, C.L.; Chen, C.A. Interferon-gamma in ascites could be a predictive biomarker of outcome in ovarian carcinoma. Gynecol. Oncol. 2013, 131, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; He, T.; Yin, Z.; Shang, C.; Xue, L.; Guo, H. Ascitic Senescent T Cells Are Linked to Chemoresistance in Patients with Advanced High-Grade Serous Ovarian Cancer. Front. Oncol. 2022, 12, 864021. [Google Scholar] [CrossRef]
- Shen, Y.; Li, L. Serum HE4 superior to CA125 in predicting poorer surgical outcome of epithelial ovarian cancer. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2016, 37, 14765–14772. [Google Scholar] [CrossRef] [PubMed]
| Clinical Characteristic | Measure, n (%) | |
|---|---|---|
| Age (years) | ≥65 | 27 (29.3) 1 |
| <60 | 65 (70.7) | |
| BMI (kg/m2) | Normal 18.5–22.9 | 34 (36.9) |
| Overweight ≥ 23 | 58 (63.1) | |
| Hypertension | Yes | 31 (33.7) |
| No | 61 (66.3) | |
| Diabetes | Yes | 11 (11.9) |
| No | 81 (88.1) | |
| Histologic type | Serous | 78 (84.8) |
| Non-serous | 14 (15.2) | |
| Stage (FIGO) | III | 50 (54.3) |
| IV | 42 (45.7) | |
| Histological grade | G1 | 2 (2.2) |
| G2 | 37 (40.2) | |
| G3 | 53 (57.6) | |
| Optimal debulking | Yes | 61 (66.3) |
| No | 31 (33.7) | |
| Neoadjuvant CTx | Yes | 17 (18.5) |
| No | 75 (81.5) | |
| Body fluid | Ascitic fluid | 55 (59.8) |
| Pleural fluid | 37 (40.2) | |
| mNLR | High ≥ 0.03 | 76 (82.6) |
| Low < 0.03 | 16 (17.4) | |
| bNLR | High ≥ 5.90 | 22 (23.9) |
| Low < 5.90 | 70 (76.1) | |
| mLMR | High ≥ 2.41 | 47 (51.1) |
| Low < 2.41 | 45 (48.9) | |
| bLMR | High ≥ 2.80 | 26 (28.3) |
| Low < 2.80 | 66 (71.7) | |
| bmLMR score | 0 | 34 (35.8) |
| 1 | 42 (44.2) | |
| 2 | 16 (16.8) | |
| State | Survival | 23 (25) |
| Died | 69 (75) | |
| Recurrence | Yes | 75 (81.5) |
| No | 17 (18.5) | |
| CA-125 (U/mL) 2 | High | 89 (96.7) |
| Normal | 3 (96.7) | |
| LDH (U/L) 2 | High | 84 (97.7) |
| Normal | 2 (2.3) | |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% Cl) | p-Value | Adjusted HR (95% Cl) | p-Value | |
| Age (years) | 0.371 | |||
| ≥65 | 1.26 (0.75–2.13) 1 | |||
| <65 | 1.00 (Ref.) | |||
| BMI | 0.034 | |||
| normal =< 23 | 0.76 (0.60–0.98) | |||
| overweight > 23 | 1.00 (Ref.) | |||
| Histological grade | <0.001 | 0.001 | ||
| G3 | 1.58 (1.24–2.01) | 2.40 (1.44–4.01) | ||
| G1/G2 | 1.00 (Ref.) | 1.00 (Ref.) | ||
| Optimal debulking | <0.001 | <0.001 | ||
| yes | 0.55 (0.42–0.71) | 0.34 (0.20–0.58) | ||
| no | 1.00 (Ref.) | 1.00 (Ref.) | ||
| Histological subtype | 0.044 | |||
| serous | 2.06 (1.01–4.17) | |||
| others | 1.00 (Ref.) | |||
| Neoadjuvant CTx. | 0.596 | |||
| yes | 1.16 (0.66–2.05) | |||
| no | 1.00 (Ref.) | |||
| bLMR | 0.013 | |||
| ≥2.80 | 0.51 (0.30–0.87) | |||
| <2.80 | 1.00 (Ref.) | |||
| bNLR | 0.008 | |||
| ≥5.90 | 2.03 (1.20–3.45) | |||
| <5.90 | 1.00 (Ref.) | |||
| mLMR | 0.006 | |||
| ≥2.41 | 0.52 (0.33–0.83) | |||
| <2.41 | 1.00 (Ref.) | |||
| mNLR | 0.012 | |||
| ≥0.03 | 2.46 (1.22–4.98) | |||
| <0.03 | 1.00 (Ref.) | |||
| LDH (U/L) | 0.549 | |||
| ≥271 | 1.00 (Ref.) | |||
| <271 | 0.64 (0.15–2.67) | |||
| CA-125 (U/mL) | 0.386 | |||
| ≥35 | 1.86 (0.45–7.62) | |||
| <35 | 1.00 (Ref.) | |||
| CRP (mg/dL) | 0.952 | |||
| ≥0.5 | 1.02 (0.40–2.59) | |||
| <0.5 | 1.00 (Ref.) | |||
| albumin (g/dL) | 0.897 | |||
| ≥3.5 | 1.00 (Ref.) | |||
| <3.5 | 1.03 (0.63–1.68) | |||
| bmLMR score | 0.001 | <0.001 | ||
| 0 | 1.00 (Ref.) | 1.00 (Ref.) | ||
| 1 | 0.32 (0.16–1.64) | 1.40 (0.71–2.75) | ||
| 2 | 0.43 (0.26–0.72) | 3.36 (0.67–6.75) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, M.J.; Yoon, Y.N.; Kang, Y.K.; Kim, C.J.; Nam, H.S.; Lee, Y.S. A Novel Score Using Lymphocyte-to-Monocyte Ratio in Blood and Malignant Body Fluid for Predicting Prognosis of Patients with Advanced Ovarian Cancer. Cancers 2023, 15, 2328. https://doi.org/10.3390/cancers15082328
Jeong MJ, Yoon YN, Kang YK, Kim CJ, Nam HS, Lee YS. A Novel Score Using Lymphocyte-to-Monocyte Ratio in Blood and Malignant Body Fluid for Predicting Prognosis of Patients with Advanced Ovarian Cancer. Cancers. 2023; 15(8):2328. https://doi.org/10.3390/cancers15082328
Chicago/Turabian StyleJeong, Min Jin, Yeo Nyeong Yoon, Yeon Kyung Kang, Chan Joo Kim, Hae Seong Nam, and Yong Seok Lee. 2023. "A Novel Score Using Lymphocyte-to-Monocyte Ratio in Blood and Malignant Body Fluid for Predicting Prognosis of Patients with Advanced Ovarian Cancer" Cancers 15, no. 8: 2328. https://doi.org/10.3390/cancers15082328
APA StyleJeong, M. J., Yoon, Y. N., Kang, Y. K., Kim, C. J., Nam, H. S., & Lee, Y. S. (2023). A Novel Score Using Lymphocyte-to-Monocyte Ratio in Blood and Malignant Body Fluid for Predicting Prognosis of Patients with Advanced Ovarian Cancer. Cancers, 15(8), 2328. https://doi.org/10.3390/cancers15082328






