Comparison of Four Albumin-Based Liver Reserve Models (ALBI/EZ-ALBI/PALBI/PAL) against MELD for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Diagnosis and Definition
2.3. Treatments
2.4. Statistics
3. Results
3.1. Patient Characteristics
3.2. Survival Analysis
3.3. Multivariate Cox Analysis
3.4. Prognostic Performance of the Five Non-Invasive Liver Reserve Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Villanueva, A. Hepatocellular Carcinoma. N. Engl. J. Med. 2019, 380, 1450–1462. [Google Scholar] [CrossRef]
- Singal, A.G.; Zhang, E.; Narasimman, M.; Rich, N.E.; Waljee, A.K.; Hoshida, Y.; Yang, J.D.; Reig, M.; Cabibbo, G.; Nahon, P.; et al. HCC surveillance improves early detection, curative treatment receipt, and survival in patients with cirrhosis: A meta-analysis. J. Hepatol. 2022, 77, 128–139. [Google Scholar] [CrossRef]
- EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [CrossRef]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef]
- Kaneko, S.; Tsuchiya, K.; Yasui, Y.; Inada, K.; Kirino, S.; Yamashita, K.; Osawa, L.; Hayakawa, Y.; Sekiguchi, S.; Higuchi, M.; et al. Strategy for advanced hepatocellular carcinoma based on liver function and portal vein tumor thrombosis. Hepatol. Res. 2020, 50, 1375–1385. [Google Scholar] [CrossRef]
- Cucarull, B.; Tutusaus, A.; Rider, P.; Hernáez-Alsina, T.; Cuño, C.; de Frutos, P.G.; Colell, A.; Marí, M.; Morales, A. Hepatocellular Carcinoma: Molecular Pathogenesis and Therapeutic Advances. Cancers 2022, 14, 621. [Google Scholar] [CrossRef]
- Raoul, J.L.; Forner, A.; Bolondi, L.; Cheung, T.T.; Kloeckner, R.; de Baere, T. Updated use of TACE for hepatocellular carcinoma treatment: How and when to use it based on clinical evidence. Cancer Treat. Rev. 2019, 72, 28–36. [Google Scholar] [CrossRef]
- Bargellini, I.; Sacco, R.; Bozzi, E.; Bertini, M.; Ginanni, B.; Romano, A.; Cicorelli, A.; Tumino, E.; Federici, G.; Cioni, R.; et al. Transarterial chemoembolization in very early and early-stage hepatocellular carcinoma patients excluded from curative treatment: A prospective cohort study. Eur. J. Radiol. 2012, 81, 1173–1178. [Google Scholar] [CrossRef]
- Manini, M.A.; Sangiovanni, A.; Martinetti, L.; Viganò, D.; La Mura, V.; Aghemo, A.; Iavarone, M.; Crespi, S.; Nicolini, A.; Colombo, M. Transarterial chemoembolization with drug-eluting beads is effective for the maintenance of the Milan-in status in patients with a small hepatocellular carcinoma. Liver Transplant. 2015, 21, 1259–1269. [Google Scholar] [CrossRef]
- Golfieri, R.; Cappelli, A.; Cucchetti, A.; Piscaglia, F.; Carpenzano, M.; Peri, E.; Ravaioli, M.; D’Errico-Grigioni, A.; Pinna, A.D.; Bolondi, L. Efficacy of selective transarterial chemoembolization in inducing tumor necrosis in small (<5 cm) hepatocellular carcinomas. Hepatology 2011, 53, 1580–1589. [Google Scholar]
- Durand, F.; Valla, D. Assessment of prognosis of cirrhosis. Semin. Liver Dis. 2008, 28, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Huo, T.I.; Lin, H.C.; Hsia, C.Y.; Wu, J.C.; Lee, P.C.; Chi, C.W.; Lee, S.D. The model for end-stage liver disease based cancer staging systems are better prognostic models for hepatocellular carcinoma: A prospective sequential survey. Am. J. Gastroenterol. 2007, 102, 1920–1930. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Pinato, D.J.; Sharma, R.; Allara, E.; Yen, C.; Arizumi, T.; Kubota, K.; Bettinger, D.; Jang, J.W.; Smirne, C.; Kim, Y.W.; et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J. Hepatol. 2017, 66, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.Y.; Liu, P.H.; Hsu, C.Y.; Huang, Y.H.; Liao, J.I.; Su, C.W.; Hou, M.C.; Huo, T.I. A New Tumor Burden Score and Albumin-Bilirubin Grade-Based Prognostic Model for Hepatocellular Carcinoma. Cancers 2022, 14, 649. [Google Scholar] [CrossRef]
- Kim, T.H.; Kim, B.H.; Park, J.W.; Cho, Y.R.; Koh, Y.H.; Chun, J.W.; Oh, E.S.; Lee, D.Y.; Lee, S.U.; Suh, Y.G.; et al. Proton Beam Therapy for Treatment-Naïve Hepatocellular Carcinoma and Prognostic Significance of Albumin-Bilirubin (ALBI) Grade. Cancers 2022, 14, 4445. [Google Scholar] [CrossRef]
- Kariyama, K.; Nouso, K.; Hiraoka, A.; Wakuta, A.; Oonishi, A.; Kuzuya, T.; Toyoda, H.; Tada, T.; Tsuji, K.; Itobayashi, E.; et al. EZ-ALBI Score for Predicting Hepatocellular Carcinoma Prognosis. Liver Cancer 2020, 9, 734–743. [Google Scholar] [CrossRef]
- Ho, S.Y.; Liu, P.H.; Hsu, C.Y.; Ko, C.C.; Huang, Y.H.; Su, C.W.; Hsia, C.Y.; Tsai, P.H.; Chou, S.J.; Lee, R.C.; et al. Easy albumin-bilirubin score as a new prognostic predictor in hepatocellular carcinoma. Hepatol. Res. 2021, 51, 1129–1138. [Google Scholar] [CrossRef]
- Desai, A.; Sandhu, S.; Lai, J.P.; Sandhu, D.S. Hepatocellular carcinoma in non-cirrhotic liver: A comprehensive review. World J. Hepatol. 2019, 11, 1–18. [Google Scholar] [CrossRef]
- Tomimaru, Y.; Eguchi, H.; Gotoh, K.; Kawamoto, K.; Wada, H.; Asaoka, T.; Noda, T.; Yamada, D.; Ogawa, H.; Umeshita, K.; et al. Platelet count is more useful for predicting posthepatectomy liver failure at surgery for hepatocellular carcinoma than indocyanine green clearance test. J. Surg. Oncol. 2016, 113, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.H.; Hsu, C.Y.; Su, C.W.; Huang, Y.H.; Hou, M.C.; Rich, N.E.; Fujiwara, N.; Hoshida, Y.; Singal, A.G.; Huo, T.I. Thrombocytosis is associated with worse survival in patients with hepatocellular carcinoma. Liver Int. 2020, 40, 2522–2534. [Google Scholar] [CrossRef]
- Lu, S.N.; Wang, J.H.; Liu, S.L.; Hung, C.H.; Chen, C.H.; Tung, H.D.; Chen, T.M.; Huang, W.S.; Lee, C.M.; Chen, C.C.; et al. Thrombocytopenia as a surrogate for cirrhosis and a marker for the identification of patients at high-risk for hepatocellular carcinoma. Cancer 2006, 107, 2212–2222. [Google Scholar] [CrossRef]
- Hansmann, J.; Evers, M.J.; Bui, J.T.; Lokken, R.P.; Lipnik, A.J.; Gaba, R.C.; Ray, C.E., Jr. Albumin-Bilirubin and Platelet-Albumin-Bilirubin Grades Accurately Predict Overall Survival in High-Risk Patients Undergoing Conventional Transarterial Chemoembolization for Hepatocellular Carcinoma. J. Vasc. Interv. Radiol. 2017, 28, 1224–1231. [Google Scholar] [CrossRef]
- Liu, P.H.; Hsu, C.Y.; Hsia, C.Y.; Lee, Y.H.; Chiou, Y.Y.; Huang, Y.H.; Lee, F.Y.; Lin, H.C.; Hou, M.C.; Huo, T.I. ALBI and PALBI Grade Predict Survival for HCC across Treatment Modalities and BCLC Stages in the MELD Era. J. Gastroenterol. Hepatol. 2017, 32, 879–886. [Google Scholar] [CrossRef]
- Huo, T.I.; Liu, P.H.; Hsu, C.Y. Comment on ‘Transarterial chemo-embolisation of hepatocellular carcinoma: Impact of liver function and vascular invasion’. Br. J. Cancer. 2017, 117, e5. [Google Scholar] [CrossRef]
- Shindoh, J.; Kawamura, Y.; Kobayashi, Y.; Kiya, Y.; Sugawara, T.; Akuta, N.; Kobayashi, M.; Suzuki, Y.; Ikeda, K.; Hashimoto, M. Platelet-Albumin Score as a Sensitive Measure for Surgical Risk Prediction and Survival Outcomes of Patients with Hepatocellular Carcinoma. J. Gastrointest. Surg. 2019, 23, 76–83. [Google Scholar] [CrossRef]
- Meira Júnior, J.D.; Fonseca, G.M.; Carvalho Neto, F.N.; Jeismann, V.B.; Kruger, J.A.P.; Silva, J.P.M.; Coelho, F.F.; Herman, P. Platelet-albumin (PAL) score as a predictor of perioperative outcomes and survival in patients with hepatocellular carcinoma undergoing liver resection in a Western center. Surg. Oncol. 2022, 42, 101752. [Google Scholar] [CrossRef] [PubMed]
- Hsu, M.C.-Y.; Lee, M.Y.-H.; Hsia, M.C.-Y.; Huang, M.Y.-H.; Su, M.C.-W.; Lin, M.H.-C.; Chiou, M.Y.-Y.; Lee, M.F.-Y.; Huo, M.T.-I. Performance Status Enhances the Selection of Treatment for Patients with Hepatocellular Carcinoma Within the Milan Criteria. Ann. Surg. Oncol. 2013, 20, 2035–2042. [Google Scholar] [CrossRef]
- Huo, T.I.; Lin, H.C.; Huang, Y.H.; Wu, J.C.; Chiang, J.H.; Lee, P.C.; Lee, S.D. The model for end-stage liver disease-based Japan Integrated Scoring system may have a better predictive ability for patients with hepatocellular carcinoma undergoing locoregional therapy. Cancer 2006, 107, 141–148. [Google Scholar] [CrossRef]
- Hsu, C.Y.; Liu, P.H.; Hsia, C.Y.; Lee, Y.H.; Nagaria, T.S.; Lee, R.C.; Lin, H.C.; Huo, T.I. Surgical Resection is Better than Transarterial Chemoembolization for Patients with Hepatocellular Carcinoma Beyond the Milan Criteria: A Prognostic Nomogram Study. Ann. Surg. Oncol. 2016, 23, 994–1002. [Google Scholar] [CrossRef]
- Hsu, C.Y.; Huang, Y.H.; Su, C.W.; Chiang, J.H.; Lin, H.C.; Lee, P.C.; Lee, F.Y.; Huo, T.I.; Lee, S.D. Transarterial chemoembolization in patients with hepatocellular carcinoma and renal insufficiency. J. Clin. Gastroenterol. 2010, 44, e171–e177. [Google Scholar] [CrossRef]
- Liu, P.H.; Lee, Y.H.; Hsu, C.Y.; Hsia, C.Y.; Huang, Y.H.; Chiou, Y.Y.; Lin, H.C.; Huo, T.I. Surgical resection is better than transarterial chemoembolization for hepatocellular carcinoma beyond Milan criteria independent of performance status. J. Gastrointest. Surg. 2014, 18, 1623–1631. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Hosmer, T.; Le Cessie, S.; Lemeshow, S. A comparison of goodness-of-fit tests for the logistic regression model. Stat. Med. 1997, 16, 965–980. [Google Scholar] [CrossRef]
- Feinstein, A.R. Clinical biostatistics. XVI. The process of prognostic stratification. 2. Clin. Pharmacol. Ther. 1972, 13, 609–624. [Google Scholar] [CrossRef] [PubMed]
- Huo, T.I. ALBI grade as a new player in hepatocellular carcinoma. J. Chin. Med. Assoc. 2019, 82, 1. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.Y.; Hsu, C.Y.; Liu, P.H.; Lee, R.C.; Ko, C.C.; Huang, Y.H.; Su, C.W.; Hou, M.C.; Huo, T.I. Albumin-Bilirubin (ALBI) Grade-Based Nomogram for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization. Dig. Dis. Sci. 2021, 66, 1730–1738. [Google Scholar] [CrossRef]
- Hiraoka, A.; Kumada, T.; Tsuji, K.; Takaguchi, K.; Itobayashi, E.; Kariyama, K.; Ochi, H.; Tajiri, K.; Hirooka, M.; Shimada, N.; et al. Validation of Modified ALBI Grade for More Detailed Assessment of Hepatic Function in Hepatocellular Carcinoma Patients: A Multicenter Analysis. Liver Cancer 2019, 8, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.Y.; Hsu, C.Y.; Liu, P.H.; Hsia, C.Y.; Su, C.W.; Huang, Y.H.; Hou, M.C.; Huo, T.I. Albumin-bilirubin (ALBI) grade-based nomogram to predict tumor recurrence in patients with hepatocellular carcinoma. Eur. J. Surg. Oncol. 2019, 45, 776–781. [Google Scholar] [CrossRef]
- Liao, J.I.; Ho, S.Y.; Liu, P.H.; Hsu, C.Y.; Huang, Y.H.; Su, C.W.; Hou, M.C.; Huo, T.I. Prognostic Prediction for Patients with Hepatocellular Carcinoma and Ascites: Role of Albumin-Bilirubin (ALBI) Grade and Easy (EZ)-ALBI Grade. Cancers 2023, 15, 753. [Google Scholar] [CrossRef]

| Variables | n = 1038 |
|---|---|
| Age (years, mean ± SD) | 67 ± 13 |
| Male/female, n (%) | 786/252 (76/24) |
| Etiologies of liver disease | |
| HBV, n (%) | 438 (42) |
| HCV, n (%) | 309 (30) |
| HBV + HCV, n (%) | 49 (5) |
| Others, n (%) | 242 (23) |
| Performance status (0/1/2), n (%) | 644/235/159 (62/23/15) |
| Tumor nodules (single/multiple) | 547/491 (53/47) |
| Maximal tumor diameter ≥ 5 cm, n (%) | 506 (49) |
| Tumor diameter, mean ± SD | 6.3 ± 4.3 |
| Vascular invasion, n (%) | 185 (18) |
| Serum AFP (ng/mL), mean ± SD | 18366 ± 131500 |
| Serum AFP ≥ 200 ng/mL, n (%) | 345 (33) |
| Ascites, n (%) | 183 (18) |
| Laboratory values, mean ± SD | |
| Alanine transaminase (U/L) | 65 ± 65 |
| Albumin (g/dL) | 3.7 ± 0.5 |
| Total bilirubin (mg/dL) | 1.1 ± 1.3 |
| Platelets (104/μL) | 16.2 ± 9.4 |
| INR of prothrombin time | 1.08 ± 0.1 |
| Creatinine (mg/dL) | 1.1 ± 0.9 |
| CTP score, mean ± SD | 5.8 ± 1.0 |
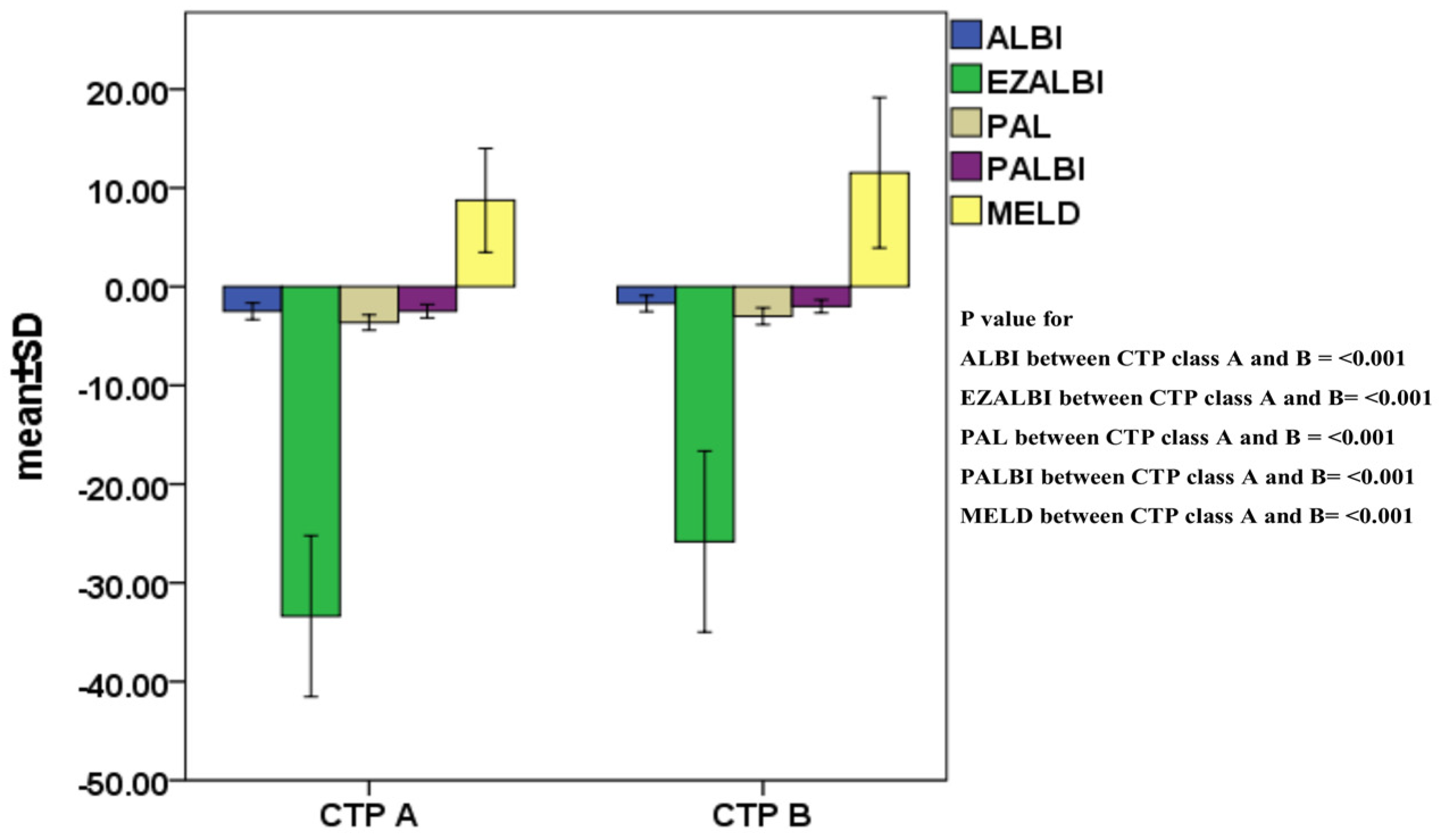
| CTP class (A/B), n (%) | 823/215 (79/21) |
| ALBI score, mean ± SD | −2.33 ± 0.52 |
| ALBI grade (1/2/3), n (%) | 350/647/41 (34/62/4) |
| EZ-ALBI score, mean ± SD | −31.8 ± 5.2 |
| EZ-ALBI grade (1/2/3), n (%) | 352/646/40 (34/62/4) |
| MELD score, mean ± SD | 9.1 ± 3.0 |
| MELD score ≤8/>8, n (%) | 420/618 (38/62) |
| PALBI score, mean ± SD | −2.38 ± 0.39 |
| PALBI grade (1/2/3), n (%) | 367/433/238 (35/42/23) |
| PAL score, mean ± SD | −3.5 ± 0.5 |
| PAL grade (1/2/3), n (%) | 317/537/184 (31/52/17) |
| BCLC stage (0/A/B/C), n (%) | 32/196/288/552 (3/19/28/50) |
| Noninvasive Liver Reserve Models | Formula |
|---|---|
| ALBI grade 1/2/3 (≤−2.6/>−2.6 and ≤−1.39/>−1.39) | (log10 (Bilirubin (μmol/L)) × 0.66) + (Albumin (g/L) × (−0.085)) |
| EZ-ALBI grade 1/2/3 (≤−34.4, >−34.4 and ≤−22.2, >−22.2) | Bilirubin (mg/dL) − (9 × Albumin (g/dL)) |
| PALBI grade 1/2/3 (≤−2.53), score > −2.53 and ≤−2.09)/(score > −2.09) | 2.02 × log10 Bilirubin (μmol/L) level − 0.37 × (log10 Bilirubin level)2 − 0.04 × Albumin level − 3.48 × log10 Platelet count (1000/μL) + 1.01 × (log10 Platelet count)2 |
| PAL grade 1/2/3 (score ≤ −3.77, score > −3.77 and ≤−3.04, score > −3.04 | 0.777 × Albumin (g/dL) − 0.575 × (log10 Platelet count) (104/μL) |
| MELD, grade 1/2 (≤8/>8) | 10 × (0.957 × ln(Creatinine)) + (0.378 × ln(Bilirubin (mg/dL))) + (1.12 × ln(INR)) + 6.43 |
| Overall Survival | Number | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||
| Age (≤67/>67 years) | 494/544 | 0.887 | 0.776–1.104 | 0.079 | |||
| Sex (male/female) | 786/252 | 0.932 | 0.798–1.088 | 0.372 | |||
| HBV (negative/positive) | 551/487 | 0.955 | 0.836–1.090 | 0.493 | |||
| HCV (negative/positive) | 680/358 | 1.177 | 1.023–1.354 | 0.023 | |||
| Platelet (≥15/<15, 104/μL) | 555/483 | 1.309 | 1.146–1.495 | 0.004 | |||
| Albumin (≥3.5/<3.5 g/dL) | 682/356 | 1.414 | 1.230–1.626 | <0.001 | |||
| Bilirubin (≤1.1/1.1 mg/dL) | 707/331 | 0.935 | 0.811–1.078 | 0.355 | |||
| Creatinine (≤1.2/>1.2 mg/dL) | 798/240 | 1.342 | 1.148–1.569 | <0.001 | 1.267 | 1.082–1.483 | 0.003 |
| Ascites (absent/present) | 855/183 | 1.482 | 1.247–1.762 | <0.001 | 1.262 | 1.055–1.510 | 0.011 |
| Serum AFP (≤200/>200 ng/mL) | 693/345 | 2.016 | 1.751–2.321 | <0.001 | 1.745 | 1.507–2.020 | <0.001 |
| Vascular invasion (no/yes) | 853/185 | 2.344 | 1.978–2.779 | <0.001 | 1.621 | 1.354–1.941 | <0.001 |
| Tumor size (≤5 cm/>5 cm) | 532/506 | 2.201 | 1.923–2.519 | <0.001 | 1.863 | 1.610–2.155 | <0.001 |
| Tumor number (single/multiple) | 547/491 | 0.965 | 0.844–1.102 | 0.595 | |||
| Performance status (0–1/2) | 879/159 | 1.677 | 1.399–2.009 | <0.001 | 1.227 | 1.015–1.484 | 0.034 |
| ALBI grade 1/grade 2–3 | 352/686 | 1.556 | 1.349–1.796 | <0.001 | 1.541 | 1.332–1.784 | <0.001 |
| Overall Survival | Number | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||
| Age (≤67/>67 years) | 494/544 | 0.887 | 0.776–1.104 | 0.079 | |||
| Sex (male/female) | 786/252 | 0.932 | 0.798–1.088 | 0.372 | |||
| HBV (negative/positive) | 551/487 | 0.955 | 0.836–1.090 | 0.493 | |||
| HCV (negative/positive) | 680/358 | 1.177 | 1.023–1.354 | 0.023 | |||
| Platelet (≥15/<15, 104/μL) | 555/483 | 1.309 | 1.146–1.495 | 0.004 | |||
| Albumin (≥3.5/<3.5 g/dL) | 682/356 | 1.414 | 1.230–1.626 | <0.001 | |||
| Bilirubin (≤1.1/1.1 mg/dL) | 707/331 | 0.935 | 0.811–1.078 | 0.355 | |||
| Creatinine (≤1.2/>1.2 mg/dL) | 798/240 | 1.342 | 1.148–1.569 | <0.001 | 1.260 | 1.076–1.475 | 0.004 |
| Ascites (absent/present) | 855/183 | 1.482 | 1.247–1.762 | <0.001 | |||
| Serum AFP (≤200/>200 ng/mL) | 693/345 | 2.016 | 1.751–2.321 | <0.001 | 1.729 | 1.493–2.002 | <0.001 |
| Vascular invasion (no/yes) | 853/185 | 2.344 | 1.978–2.779 | <0.001 | 1.613 | 1.347–1.931 | <0.001 |
| Tumor size (≤5 cm/>5 cm) | 532/506 | 2.201 | 1.923–2.519 | <0.001 | 1.853 | 1.602–2.143 | <0.001 |
| Tumor number (single/multiple) | 547/491 | 0.965 | 0.844–1.102 | 0.595 | |||
| Performance status (0–1/2) | 879/159 | 1.677 | 1.399–2.009 | <0.001 | |||
| EZ-ALBI grade 1/grade 2–3 | 352/686 | 1.556 | 1.349–1.796 | <0.001 | 1.563 | 1.350–1.810 | <0.001 |
| Overall Survival | Number | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||
| Age (≤67/>67 years) | 494/544 | 0.887 | 0.776–1.104 | 0.079 | |||
| Sex (male/female) | 786/252 | 0.932 | 0.798–1.088 | 0.372 | |||
| HBV (negative/positive) | 551/487 | 0.955 | 0.836–1.090 | 0.493 | |||
| HCV (negative/positive) | 680/358 | 1.177 | 1.023–1.354 | 0.023 | |||
| Platelet (≥150/<150, 1000/μL) | 555/483 | 1.309 | 1.146–1.495 | 0.004 | |||
| Albumin (≥3.5/<3.5 g/dL) | 682/356 | 1.414 | 1.230–1.626 | <0.001 | |||
| Bilirubin (≤1.1/1.1 mg/dL) | 707/331 | 0.935 | 0.811–1.078 | 0.355 | |||
| Creatinine (≤1.2/>1.2 mg/dL) | 798/240 | 1.342 | 1.148–1.569 | <0.001 | 1.338 | 1.142–1.567 | <0.001 |
| Ascites (absence/present) | 855/183 | 1.482 | 1.247–1.762 | <0.001 | |||
| Serum AFP (≤200/>200 ng/mL) | 693/345 | 2.016 | 1.751–2.321 | <0.001 | 1.694 | 1.460–1.964 | <0.001 |
| Vascular invasion (no/yes) | 853/185 | 2.344 | 1.978–2.779 | <0.001 | 1.596 | 1.331–1.913 | <0.001 |
| Tumor size (≤5 cm/>5 cm) | 532/506 | 2.201 | 1.923–2.519 | <0.001 | 1.790 | 1.546–2.073 | <0.001 |
| Tumor number (single/multiple) | 547/491 | 0.965 | 0.844–1.102 | 0.595 | |||
| Performance status (0–1/2) | 879/159 | 1.677 | 1.399–2.009 | <0.001 | |||
| PALBI grade 1/2–3 | 317/721 | 1.593 | 1.383–1.834 | <0.001 | 1.358 | 1.163–1.584 | <0.001 |
| Overall Survival | Number | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||
| Age (≤67/>67 years) | 494/544 | 0.887 | 0.776–1.104 | 0.079 | |||
| Sex (male/female) | 786/252 | 0.932 | 0.798–1.088 | 0.372 | |||
| HBV (negative/positive) | 551/487 | 0.955 | 0.836–1.090 | 0.493 | |||
| HCV (negative/positive) | 680/358 | 1.177 | 1.023–1.354 | 0.023 | |||
| Platelet (≥15/<15, 104/μL) | 555/483 | 1.309 | 1.146–1.495 | 0.004 | |||
| Albumin (≥3.5/<3.5 g/dL) | 682/356 | 1.414 | 1.230–1.626 | <0.001 | |||
| Bilirubin (≤1.1/1.1 mg/dL) | 707/331 | 0.935 | 0.811–1.078 | 0.355 | |||
| Creatinine (≤1.2/>1.2 mg/dL) | 798/240 | 1.342 | 1.148–1.569 | <0.001 | 1.261 | 1.077–1.477 | 0.004 |
| Ascites (absence/present) | 855/183 | 1.482 | 1.247–1.762 | <0.001 | |||
| Serum AFP (≤200/>200 ng/mL) | 693/345 | 2.016 | 1.751–2.321 | <0.001 | 1.732 | 1.496–2.005 | <0.001 |
| Vascular invasion (no/yes) | 853/185 | 2.344 | 1.978–2.779 | <0.001 | 1.663 | 1.389–1.991 | <0.001 |
| Tumor size (≤5 cm/>5 cm) | 532/506 | 2.201 | 1.923–2.519 | <0.001 | 1.949 | 1.683–2.257 | <0.001 |
| Tumor number (single/multiple) | 547/491 | 0.965 | 0.844–1.102 | 0.595 | |||
| Performance status (0–1/2) | 879/159 | 1.677 | 1.399–2.009 | <0.001 | |||
| PAL grade 1/grade 2–3 | 352/686 | 1.556 | 1.349–1.796 | <0.001 | 1.541 | 1.332–1.784 | <0.001 |
| Overall Survival | Number | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||
| Age (≤67/>67 years) | 494/544 | 0.887 | 0.776–1.104 | 0.079 | |||
| Sex (male/female) | 786/252 | 0.932 | 0.798–1.088 | 0.372 | |||
| HBV (negative/positive) | 551/487 | 0.955 | 0.836–1.090 | 0.493 | |||
| HCV (negative/positive) | 680/358 | 1.177 | 1.023–1.354 | 0.023 | |||
| Platelet (≥15/<15, 104/μL) | 555/483 | 1.309 | 1.146–1.495 | 0.004 | |||
| Albumin (≥3.5/<3.5 g/dL) | 682/356 | 1.414 | 1.230–1.626 | <0.001 | 1.451 | 1.256–1.677 | <0.001 |
| Bilirubin (≤1.1/1.1 mg/dL) | 707/331 | 0.935 | 0.811–1.078 | 0.355 | |||
| Creatinine (≤1.2/>1.2 mg/dL) | 798/240 | 1.342 | 1.148–1.569 | <0.001 | 1.270 | 1.085–1.487 | 0.003 |
| Ascites (absence/present) | 855/183 | 1.482 | 1.247–1.762 | <0.001 | |||
| Serum AFP (≤200/>200 ng/mL) | 693/345 | 2.016 | 1.751–2.321 | <0.001 | 1.709 | 1.476–1.979 | <0.001 |
| Vascular invasion (no/yes) | 853/185 | 2.344 | 1.978–2.779 | <0.001 | 1.673 | 1.397–2.003 | <0.001 |
| Tumor size (≤5/>5 cm) | 532/506 | 2.201 | 1.923–2.519 | <0.001 | 1.855 | 1.603–2.146 | <0.001 |
| Tumor number (single/multiple) | 547/491 | 0.965 | 0.844–1.102 | 0.595 | |||
| Performance status (0–1/2) | 879/159 | 1.677 | 1.399–2.009 | <0.001 | |||
| MELD score ≤8/>8 | 420/618 | 1.176 | 1.027–1.346 | 0.019 | |||
| Non-Invasive Liver Reserve Model | Homogeneity (Wald χ2) | AICc |
|---|---|---|
| ALBI | 26.009 | 10,782.486 |
| EZ-ALBI | 34.862 | 10,773.633 |
| PALBI | 55.041 | 10,753.453 |
| PAL | 31.427 | 10,777.061 |
| MELD | 5.550 | 10,802.944 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, S.-Y.; Liu, P.-H.; Hsu, C.-Y.; Huang, Y.-H.; Liao, J.-I.; Su, C.-W.; Hou, M.-C.; Huo, T.-I. Comparison of Four Albumin-Based Liver Reserve Models (ALBI/EZ-ALBI/PALBI/PAL) against MELD for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization. Cancers 2023, 15, 1925. https://doi.org/10.3390/cancers15071925
Ho S-Y, Liu P-H, Hsu C-Y, Huang Y-H, Liao J-I, Su C-W, Hou M-C, Huo T-I. Comparison of Four Albumin-Based Liver Reserve Models (ALBI/EZ-ALBI/PALBI/PAL) against MELD for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization. Cancers. 2023; 15(7):1925. https://doi.org/10.3390/cancers15071925
Chicago/Turabian StyleHo, Shu-Yein, Po-Hong Liu, Chia-Yang Hsu, Yi-Hsiang Huang, Jia-I Liao, Chien-Wei Su, Ming-Chih Hou, and Teh-Ia Huo. 2023. "Comparison of Four Albumin-Based Liver Reserve Models (ALBI/EZ-ALBI/PALBI/PAL) against MELD for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization" Cancers 15, no. 7: 1925. https://doi.org/10.3390/cancers15071925
APA StyleHo, S.-Y., Liu, P.-H., Hsu, C.-Y., Huang, Y.-H., Liao, J.-I., Su, C.-W., Hou, M.-C., & Huo, T.-I. (2023). Comparison of Four Albumin-Based Liver Reserve Models (ALBI/EZ-ALBI/PALBI/PAL) against MELD for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization. Cancers, 15(7), 1925. https://doi.org/10.3390/cancers15071925






