Impact of a Training Program on Oncology Nurses’ Confidence in the Provision of Self-Management Support and 5As Behavioral Counseling Skills
Abstract
Simple Summary
Abstract
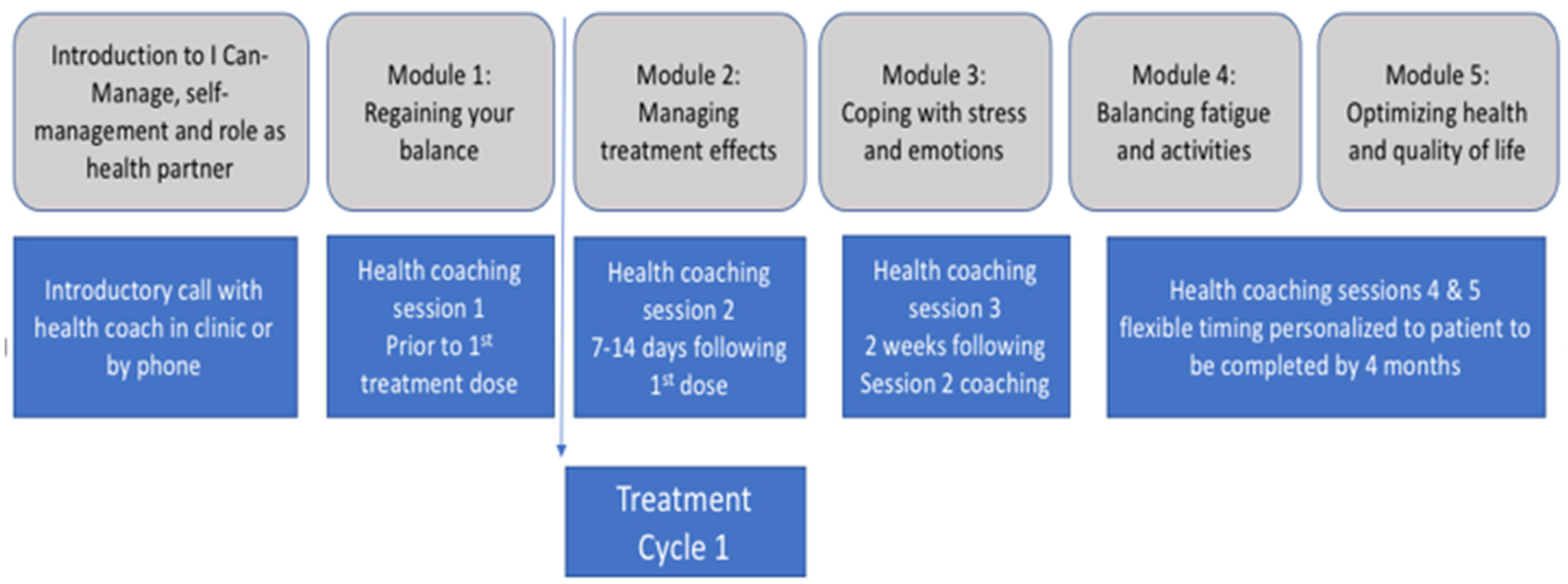
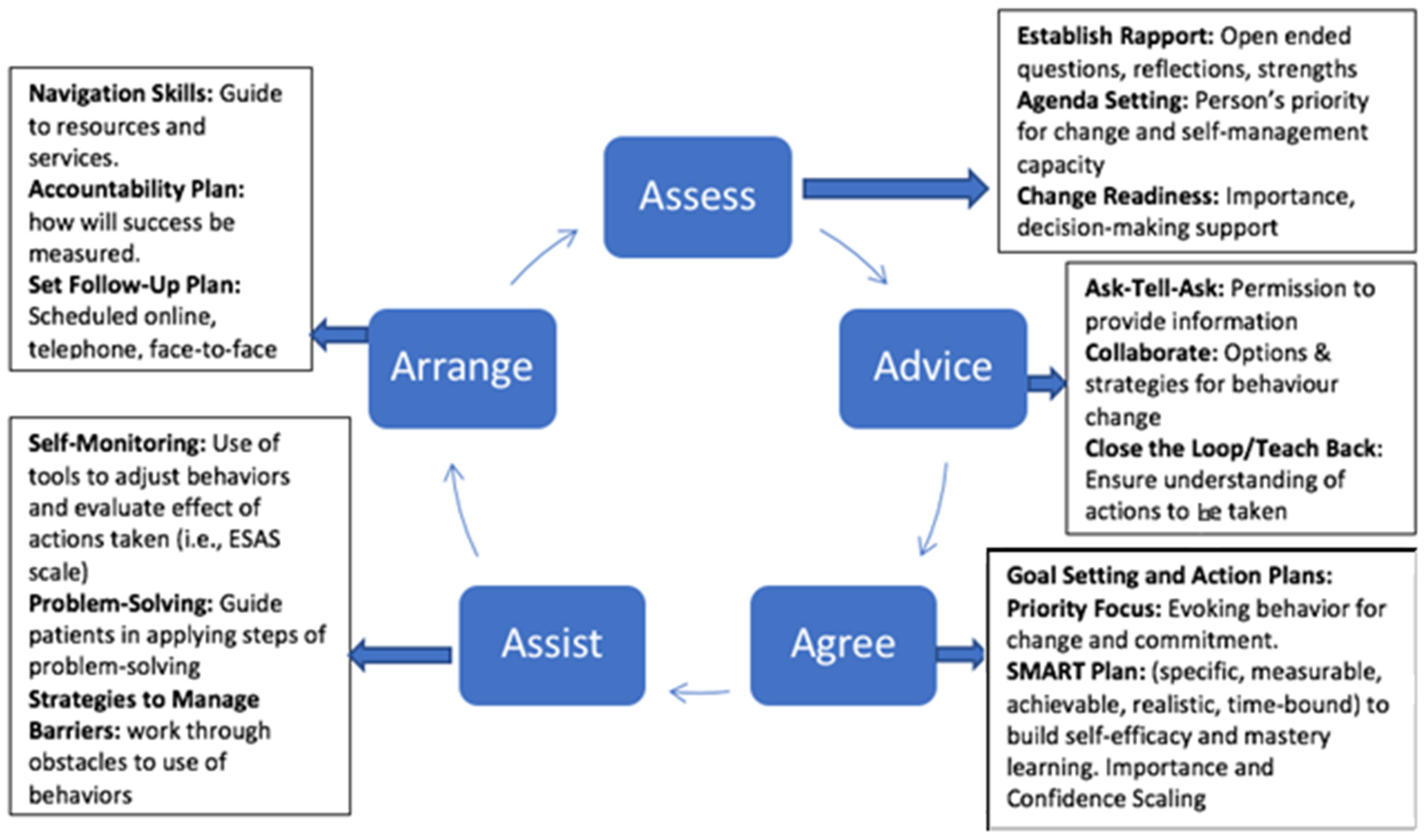
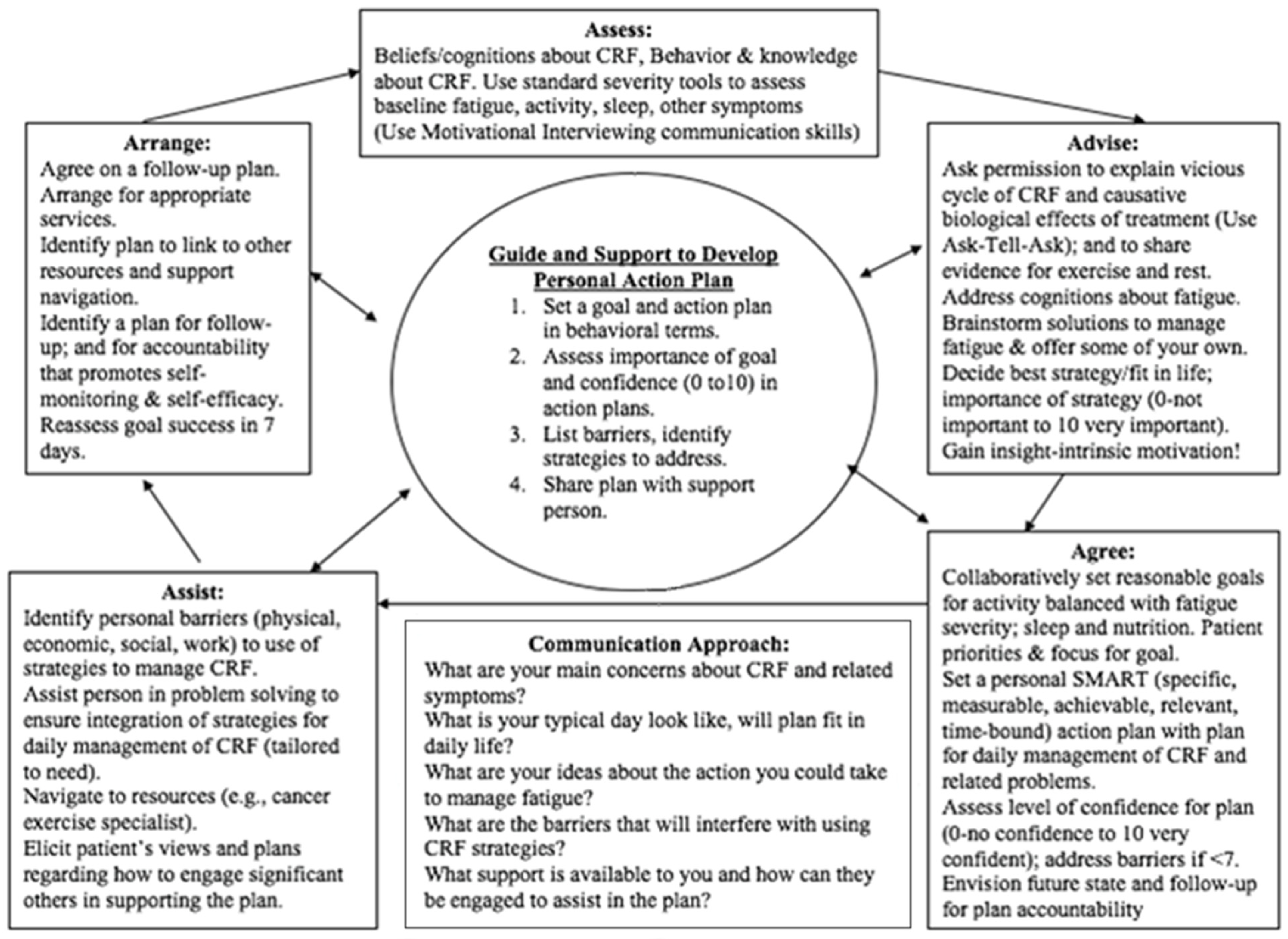
1. Background
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coolbrandt, A.; Wildiers, H.; Aertgeerts, B.; de Casterle, B.D.; Achterberg, T.V.; Millisen, K. Systematic development of CHEMO-SUPPORT, a nursing intervention to support adult patients with cancer in dealing with chemotherapy-related symptoms at home. BMC Nurs. 2018, 17, 28. [Google Scholar] [CrossRef] [PubMed]
- Foster, C. Survivorship and self-management in cancer care. In Cancer and Cancer Care; Wyatt, D., Hubert-Williams, N., Eds.; SAGE: London, UK, 2015. [Google Scholar]
- Barlow, J.H.; Wright, C.; Sheasby, J.; Turner, A.; Hainsworth, J. Self-management approaches for people with chronic conditions: A review. Patient Educ. Counsel. 2002, 48, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.R.; Holman, H. Self-management education: History, definition, outcomes, and mechanisms. Ann. Behav. Med. 2003, 26, 1–7. [Google Scholar] [CrossRef]
- Hammer, M.J.; Ercolano, E.A.; Wright, F.; Dickson, V.V.; Chyun, D.; Melkus, G.D. Self-management for Adult Patients with Cancer: An Integrative Review. Cancer Nurs. 2015, 38, E10–E26. [Google Scholar] [CrossRef] [PubMed]
- Howell, D. Supported self-management for cancer survivors to address long-term biopsychosocial consequences of cancer and treatment to optimize living well. Curr. Opin. Support. Palliat. Care 2018, 12, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Stein, K.D.; Syrjala, K.L.; Andrykowski, M.A. Physical and psychological long-term and late effects of cancer. Cancer 2008, 112 (Suppl. 11), 2577–2592. [Google Scholar] [CrossRef]
- Grimmett, C.; Corbett, T.; Brunet, J.; Shepherd, J.; Pinto, B.M.; May, C.R.; Foster, C. Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 37. [Google Scholar] [CrossRef]
- Haase, K.R.; Avery, J.; Bryant-Lukosius, D.; Kryzanowska, M.; Kukretti, V.; Liu, G.; Mayo, S.J.; Jones, J.; Howell, D. Patient and clinician perspectives of desired features for a web-based self-management program (icanmanage.ca): Exposing patients “hard work” of managing acute cancer. Support. Care Cancer 2020, 29, 1989–1998. [Google Scholar] [CrossRef]
- Ose, D.; Winkler, E.C.; Berger, S.; Baudendistel, I.; Kamradt, M.; Eckrich, F.; Szecsenyi, J. Complexity of care and strategies of self-management in patients with colorectal cancer. Patient Prefer. Adherence 2017, 11, 731–742. [Google Scholar] [CrossRef]
- Adams, K.; Greiner, A.C.; Corrigan, J.M. Report of a summit. In The First Annual Crossing the Quality Chasm Summit: A Focus on Communities; National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- McCorkle, R.; Ercolano, E.; Lazenby, M.; Schulman-Green, D.; Schilling, L.S.; Lorig, K.; Wagner, E.H. Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA Cancer J. Clin. 2011, 61, 50–62. [Google Scholar] [CrossRef]
- Chan, R.J.; Mayer, D.; Koczwara, B.; Loerzel, V.; Charalambous, A.; Agbejule, O.A.; Howell, D. Building capacity in cancer nurses to deliver self-management support: A call for action paper. Cancer Nurs. 2020, 43, 341–342. [Google Scholar] [CrossRef]
- Eagen, L.; Levesque, J. Transforming community cancer care: The Ottawa Regional Cancer Foundation’s cancer coaching practice. Univ. Ott. J. Med. 2017, 7, 15. [Google Scholar] [CrossRef]
- Taylor, S.J.C.; Pinnock, H.; Epiphaniou, E.; Pearce, G.; Parke, H. A rapid synthesis of the evidence on interventions supporting self-management for people with long- term conditions. (PRISMS Practical Systematic Review of Self-Management Support for long-term conditions). Health Serv. Deliv. Res. 2014, 2, 54. [Google Scholar] [CrossRef]
- Greene, J.; Hibbard, J. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Intern. Med. 2012, 27, 520–526. [Google Scholar] [CrossRef]
- Howell, D.; Harth, T.; Brown, J.A.; Bennet, C.; Boyco, S. Self-management education interventions for patients with cancer: A systematic review. Support Care Cancer 2017, 25, 1323–1355. [Google Scholar] [CrossRef]
- Cuthbert, C.A.; Farragher, J.F.; Hemmelgarn, B.R.; Ding, Q.; McKinnon, G.P.; Cheung, W.Y. Self-management interventions for cancer survivors: A systematic review and evaluation of intervention content and theories. Psycho-Oncology 2019, 28, 2119–2140. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, K.; Mayer, D.K. Self-management interventions for adult cancer survivors after treatment: A systematic review and meta-analysis. Oncol. Nurs. Forum. 2017, 44, 719–728. [Google Scholar] [CrossRef]
- Kantilal, K.; Hardeman, W.; Whiteside, H.; Karapanagiotou, E.; Small, M.; Bhattacharya, D. Facilitating healthcare practitioners to deliver self-management support in adult cancer survivors: A realist review. Res. Soc. Admin. Pharm. 2022, 18, 3870–3883. [Google Scholar] [CrossRef] [PubMed]
- Creer, T.L.; Holroyd, K.A. Self-management of chronic conditions. In Cambridge Handbook of Psychology, Health and Medicine; Baum, A., Newman, S., Weinman, J., West, R., McManus, C., Eds.; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Dinh, H.; Thuy, T.; Bonner, A.; Clark, R.; Ramsbotham, J.; Hines, S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Evid. Synth. 2016, 14, 210–247. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.; Pond, G.; Bryant Lukosius, D.; Powis, M.; McGowan, P.; Tutsirai, M.; Kukretti, V.; Rask, S.; Hack, S.; Krzyzanowska, M.K. Feasibility and effectiveness of self-management online education and telephone coaching on patient activation in managing cancer treatment toxicities. J. Natl. Compr. Cancer Netw. 2023, 21, 247–255. [Google Scholar] [CrossRef]
- McGowan, P.; Lynch, S.; Hensen, F. The role and effectiveness of telephone peer coaching for adult patients with Type 2 Diabetes. Can. J. Diabetes 2019, 43, 399–405. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Davis, C.L.; Funnell, M.M.; Beck, A. Implementing practical interventions to support chronic illness self-management. Jt. Comm. J. Qual. Saf. 2003, 29, 563–574. [Google Scholar] [CrossRef] [PubMed]
- Registered Nurses’ Association of Ontario. Strategies to Support Self-Management in Chronic Conditions: Collaboration with Clients; Registered Nurses’ Association of Ontario: Toronto, ON, Canada, 2010. [Google Scholar]
- Hudon, C.; Chouinard, M.C.; Diadiou, F.; Bouliane, D.; Lambert, M.; Hudon, É. The Chronic Disease Self-Management Program: The experience of frequent users of health care services and peer leaders. Fam. Pract. 2016, 33, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Wolever, R.Q.; Simmons, L.A.; Sforzo, G.A.; Dill, D.; Kaye, M.; Bechard, E.M.; Southard, M.E.; Kennedy, M.; Vosloo, J.; Yang, N. A systematic review of the literature on health and wellness coaching: Defining a key behavioral intervention in healthcare. Glob. Adv. Health Med. 2013, 2, 38–57. [Google Scholar] [CrossRef]
- Tharani, A.; Van Hecke, A.; Ali, T.S.; Duprez, V. Factors influencing nurses’ provision of self-management support for patients with chronic illnesses: A systematic mixed studies review. Int. J. Nurs. Stud. 2021, 120, 103983. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.; Doran, G.; Patton, P.; Fitsgerald, R.; Rochfort, A. Does education of primary care professionals promote self-management and improve outcomes in chronic disease? An updated review. BJGP Open 2021, 5, BJGPO.2020.0186. [Google Scholar] [CrossRef] [PubMed]
- Franklin, M.; Lewis, S.; Willis, K.; Bourke-Taylor, H.; Smith, L. Patients’ and healthcare professionals’ perceptions of self-management support interactions: Systematic review and qualitative synthesis. Chronic Illn. 2018, 14, 79–103. [Google Scholar] [CrossRef]
- Roy, D.; Mahony, F.; Horsburgh, M.; Bycroft, J. Partnering in primary care in New Zealand: Client’ and nurses’ experience of the Flinders Program ™ in the management of long term conditions. J. Nurs. Healthc. Chronic Illn. 2011, 3, 140–149. [Google Scholar] [CrossRef]
- Duprez, V.; Vandecasteele, T.; Verhaeghe, S.; Beeckman, D.; Van Hecke, A. The effectiveness of interventions to enhance self-management support competencies in the nursing profession: A systematic review. J. Adv. Nurs. 2016, 73, 1807–1824. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.J.; Oluvaseyifunmsi, A.; Crawford-Williams, F.; Yates, P.; Koczwara, B.; Erikson, J.; So, W.K.; Howell, D. Development of an international competency framework for nurses in the provision of self-management support to cancer populations. Cancer Nurs. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Howell, D.; Mayer, D.K.; Fielding, R.; Eicher, M.; Verdonck-de Leeuw, I.M.; Johansen, C.; Soto-Perez-de-Celis, E.; Foster, C.; Chan, R.; Alfano, C.M.; et al. Management of Cancer and Health After the Clinic Visit: A Call to Action for Self-Management in Cancer Care. JNCI 2020, 113, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Lawn, S.; Zhi, X.; Morellow, A. An integrative review of e-learning in the delivery of self-management support training for health professionals. BMC Med. Educ. 2017, 17, 183. [Google Scholar] [CrossRef] [PubMed]
- Self-Management in Cancer. In Quality Standards; Cancer Care Ontario: Toronto, ON, Canada, 2018; Available online: https://www.cancercareontario.ca/en/guidelines-advice/typesofcancer/57371 (accessed on 1 June 2018).
- Wagner, E.H.; Austin, B.T.; Von Korff, M. Organizing care for patients with chronic illness. Milbank Q 1996, 74, 511–544. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Funnell, M.M.; Bonomi, A.E.; Davis, C.; Beckham, V.; Wagner, E.H. Self-Management aspects of improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Ann. Behav. Med. 2002, 24, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Medland, M. Self-Management Support: A Study and Implementation Guide for Health Care Professionals; Fraser Health Authority: Abbotsford, BC, Canada, 2009; Available online: https:www.yumpu.com/en/document/view/32930119/self-management-support-a-study-and-implementation-guide (accessed on 10 May 2020).
- South West Self-Management Program. Self-Management Toolkit. A Resource for Health Care Providers. 2018. Available online: www.self-management.ca (accessed on 10 May 2020).
- Whitelock, E.P.; Orleans, C.T.; Pender, N.; Allan, J. Evaluating primary care behavioral counselling interventions: An evidence-based approach. Am. J. Prev. Med. 2002, 22, 267–284. [Google Scholar] [CrossRef]

| Question | Center 1 | Center 2 | Center 3 | Coaches |
|---|---|---|---|---|
| n = 11 | n = 14 | n = 15 | n = 8 | |
| Years working as a registered nurse, µ (σ) | 22.45 (9.88) | 29.18 (8.53) | 16.8 (11.53) | 21.5 (9.24) |
| Years working in oncology, µ (σ) | 17.45 (9.48) | 19.46 (8.95) | 13.87 (10.13) | 18.63 (10.42) |
| Current area of work, n (%) Ambulatory clinics Other | 11 1 | 13 1 | 14 1 | 7 1 |
| Highest level of nursing education, n (%) * Diploma Bachelor’s Master’s | 7 4 - | 8 5 1 | 3 10 2 | 4 2 2 |
| Completion of professional certifications, n (%) * CNA certification in oncology CNA certification in palliative care The de Souza Institute certification Other certifications | 10 2 1 2 | 11 - - 2 | 12 1 3 2 | 6 1 2 |
| Previously received professional education/training addressing the principles/practices of SMS, n (%) No Yes, within last 2 years Yes, over 2 years ago | 8 - 3 | 10 - 4 | 11 2 2 | 6 2 |
| Concept | Center 1 | Center 2 | Center 3 | Coaches |
|---|---|---|---|---|
| n = 11 | n = 14 | n = 15 | n = 8 | |
| Patient activation, µ (σ) | 2.45 (0.93) | 3.00 (0.96) | 1.73 (1.03) | 3.25 (0.71) |
| Self-management support, µ (σ) | 3.55 (0.93) | 2.93 (0.92) | 2.20 (0.86) | 3.50 (0.53) |
| Self-management, µ (σ) | 3.45 (0.93) | 3.14 (0.86) | 2.33 (0.82) | 3.38 (0.52) |
| Cancer as a chronic condition, µ (σ) | 4.09 (0.94) | 4.00 (0.78) | 3.07 (1.22) | 4.00 (0.53) |
| Question | Center 1 | Center 2 | Center 3 | Coaches | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 11 | n = 14 | n = 16 | n = 15 | n = 8 | ||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||
| a—Defining SMS, µ (σ) | 3.6 (0.97) | 4.09 (0.83) | 3.21 (1.12) | 4.19 (0.75) | 2.07 (0.8) | 4.53 (0.52) | 3.5 (0.76) | 4.25 (0.71) | ||
| b—Supporting patients in making difficult decisions, µ (σ) | 3.82 (0.6) | 3.82 (1.08) | 4 (0.78) | 4.13 (0.72) | 2.73 (0.88) | 4.20 (0.56) | 3.25 (0.71) | 3.75 (0.71) | ||
| c—Using 5As model in providing SMS, µ (σ) | Assess | Establish rapport | 4.09 (0.54) | 4.55 (0.69) | 4.07 (1) | 4.5 (0.63) | 3.38 (0.52) | 4.47 (0.64) | 3.88 (0.83) | 4.13 (0.64) |
| Setting visit agenda | 3.09 (1.04) | 4.27 (0.79) | 3.57 (1.09) | 4.06 (0.68) | 4.00 (0.53) | 4.20 (0.56) | 3.5 (1.07) | 4 (0.76) | ||
| Assess client readiness | 3.27 (0.9) | 4.45 (0.69) | 3.5 (1.02) | 4.19 (0.66) | 2.67 (0.9) | 4.33 (0.49) | 3.38 (0.74) | 3.75 (0.71) | ||
| Goal setting | 3.45 (0.82) | 4.3 (0.67) | 3.43 (1.02) | 4.19 (0.66) | 2.60 (0.91) | 4.33 (0.49) | 3.38 (0.74) | 3.50 (0.53) | ||
| Advise | Tailoring strategies | 2.73 (1.01) | 4.18 (0.6) | 3.14 (1.17) | 4.06 (0.68) | 2.13 (0.92) | 4.20 (0.68) | 2.88 (0.35) | 3.63 (0.52) | |
| Ask–tell–ask | 2.64 (0.92) | 4.09 (0.54) | 3.14 (1) | 4.44 (0.63 | 2.33 (1.05) | 4.33 (0.49) | 3.00 (0.53) | 3.88 (0.83) | ||
| Closing the loop | 3.09 (0.83) | 4.18 (0.6) | 3.00 (1.18) | 4.31 (0.7) | 2.33 (1.18) | 4.47 (0.52) | 3.00 (0.53) | 4 (0.76) | ||
| Agree | Action plans and follow-up | 3.82 (0.6) | 4.55 (0.52) | 3.43 (1.09) | 4.19 (0.66) | 2.60 (1.06) | 4.27 (0.46) | 3.25 (0.89) | 4 (0.76) | |
| Assist | Problem solving | 3.91 (0.54) | 4.36 (0.5) | 3.50 (0.94) | 4.31 (0.7) | 2.80 (0.86) | 4.20 (0.68) | 3.25 (0.71) | 3.63 (0.74) | |
| Linking to community resources | 4.00 (0.45) | 4.27 (0.47) | 3.64 (0.84) | 4.00 (0.73) | 3.00 (0.93) | 4.33 (0.49) | 3.38 (0.52) | 3.63 (0.52) | ||
| Teaching self-monitoring skills | 3.55 (0.82) | 4.27 (0.47) | 3.07 (1.07) | 3.94 (0.77) | 2.73 (0.8) | 4.13 (0.64) | 3.25 (0.71) | 3.63 (0.92) | ||
| Review goal and action plan | 3.36 (0.67) | 4.36 (0.5) | 3.43 (0.94) | 4.19 (0.54) | 2.73 (0.7) | 4.33 (0.62) | 3.25 (0.71) | 3.88 (0.64) | ||
| Arrange | Follow-up | 3.91 (0.7) | 4.5 (0.53) | 3.93 (0.92) | 4.31 (0.6) | 3.07 (0.88) | 4.33 (0.62) | 3.75 (0.46) | 4.00 (0.76) | |
| t-Test Results | Mean Diff 0.79 t = 7.18 p ≤ 0.00001 | Mean Diff 0.73 t = 8.48 p ≤ 0.00001 | Mean Diff 1.57 t = 11.45 p ≤ 0.00001 | Mean Diff 0.52 t = 7.6 <0.00001 | ||||||
| Question | Center 1 | Center 2 | Center 3 | Coaches | |
|---|---|---|---|---|---|
| n = 11 | n = 16 | n = 15 | n = 8 | ||
| Overall, µ (σ) | Valuable use of time | 3.10 (0.99) | 4.00 (0.63) | 4.47 (0.64) | 4.38 (0.52) |
| Relevant to professional practice | 4.00 (0.89) | 4.44 (0.63) | 4.73 (0.46) | 4.50 (0.53) | |
| Taught skills that can be implemented in practice | 3.82 (0.4) | 4.19 (0.66) | 4.67 (0.49) | 4.75 (0.46) | |
| Recommend to friend/colleague | 3.4 (1.07) | 3.94 (0.77) | 4.6 (0.51) | 4.38 (0.52) | |
| Taught skills that enhance ability to educate patients to manage cancer & treatment | 3.64 (1.03) | 4.19 (0.66) | 4.73 (0.46) | 4.75 (0.46) | |
| Satisfaction, µ (σ) | Overall course | 3.44 (1.24) | 4.06 (0.77) | 4.6 (0.51) | 4.63 (0.52) |
| Location | 4.73 (0.65) | 3.50 (1.03) | 4.27 (0.88) | 4.13 (0.99) | |
| Time spent/duration of course | 3.4 (1.43) | 3.94 (0.93) | 4.53 (0.52) | 4.25 (0.46) | |
| Teaching methods used: | |||||
| Reading materials | 3.64 (1.12) | 4.00 (0.82) | 4.53 (0.52) | 4.5 (0.53) | |
| Learning activities | 3.64 (1.12) | 4.19 (0.66) | 4.53 (0.52) | 4.5 (0.53) | |
| Opportunities for skills practice | 3.7 (1.16) | 4.19 (0.75) | 4.53 (0.52) | 4.5 (0.53) | |
| Opportunities to exchange ideas | 4.09 (0.54) | 4.44 (0.73) | 4.6 (0.51) | 4.5 (0.53) | |
| Opportunities to build collegial relationships | 3.9 (0.57) | 3.94 (0.85) | 4.73 (0.46) | 4 (0.53) | |
| Facilitator, µ (σ) | Ability to foster a safe, supportive learning environment | 4.36 (0.5) | 4.19 (0.66) | 4.87 (0.35) | 4.75 (0.46) |
| Ability to provide helpful feedback | 3.91 (0.83) | 4.25 (0.58) | 4.73 (0.46) | 4.75 (0.46) | |
| Ability to model skills taught while interacting | 3.82 (0.75) | 4.00 (0.82) | 4.80 (0.41) | 4.75 (0.46) | |
| Knowledge of content | 4.09 (0.83) | 4.19 (0.66) | 4.8 (0.41) | 4.63 (0.52) | |
| Clarity of presentation | 3.50 (1.27) | 4.13 (0.72) | 4.73 (0.46) | 4.63 (0.52) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Howell, D.; McGowan, P.; Bryant-Lukosius, D.; Kirkby, R.; Powis, M.; Sherifali, D.; Kukreti, V.; Rask, S.; Krzyzanowska, M.K. Impact of a Training Program on Oncology Nurses’ Confidence in the Provision of Self-Management Support and 5As Behavioral Counseling Skills. Cancers 2023, 15, 1811. https://doi.org/10.3390/cancers15061811
Howell D, McGowan P, Bryant-Lukosius D, Kirkby R, Powis M, Sherifali D, Kukreti V, Rask S, Krzyzanowska MK. Impact of a Training Program on Oncology Nurses’ Confidence in the Provision of Self-Management Support and 5As Behavioral Counseling Skills. Cancers. 2023; 15(6):1811. https://doi.org/10.3390/cancers15061811
Chicago/Turabian StyleHowell, Doris, Patrick McGowan, Denise Bryant-Lukosius, Ryan Kirkby, Melanie Powis, Diana Sherifali, Vishal Kukreti, Sara Rask, and Monica K. Krzyzanowska. 2023. "Impact of a Training Program on Oncology Nurses’ Confidence in the Provision of Self-Management Support and 5As Behavioral Counseling Skills" Cancers 15, no. 6: 1811. https://doi.org/10.3390/cancers15061811
APA StyleHowell, D., McGowan, P., Bryant-Lukosius, D., Kirkby, R., Powis, M., Sherifali, D., Kukreti, V., Rask, S., & Krzyzanowska, M. K. (2023). Impact of a Training Program on Oncology Nurses’ Confidence in the Provision of Self-Management Support and 5As Behavioral Counseling Skills. Cancers, 15(6), 1811. https://doi.org/10.3390/cancers15061811







