Surgical Approach in Metastatic Renal Cell Carcinoma: A Literature Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
- (a)
- articles published after 2016;
- (b)
- based on a screening of the references of the included articles, papers published before 2016 and relevant to the topic of this review were also included (25 articles);
- (c)
- articles including keywords such as: RCC, surgery, metastasis, vena cava invasion, mRCC, nephrectomy, metastatectomy, cytoreductive nephrectomy, partial nephrectomy, RARN, renal surgery using search term database = specific-medical subject headings terms in various combinations appropriate to the purpose of the study.
- (a)
- articles on animals, tissues, cell lines;
- (b)
- involving more than one cancer, e.g., semi-occurrence of kidney and prostate or bladder cancer;
- (c)
- papers focusing on the technical feasibility and specification of measurement methods rather than method and clinical utility;
- (d)
- publications based on small cohorts (less than 5 patients).
3. Results
3.1. Nephrectomy
3.2. IVC Thrombus
3.3. Metastectomy (MS)
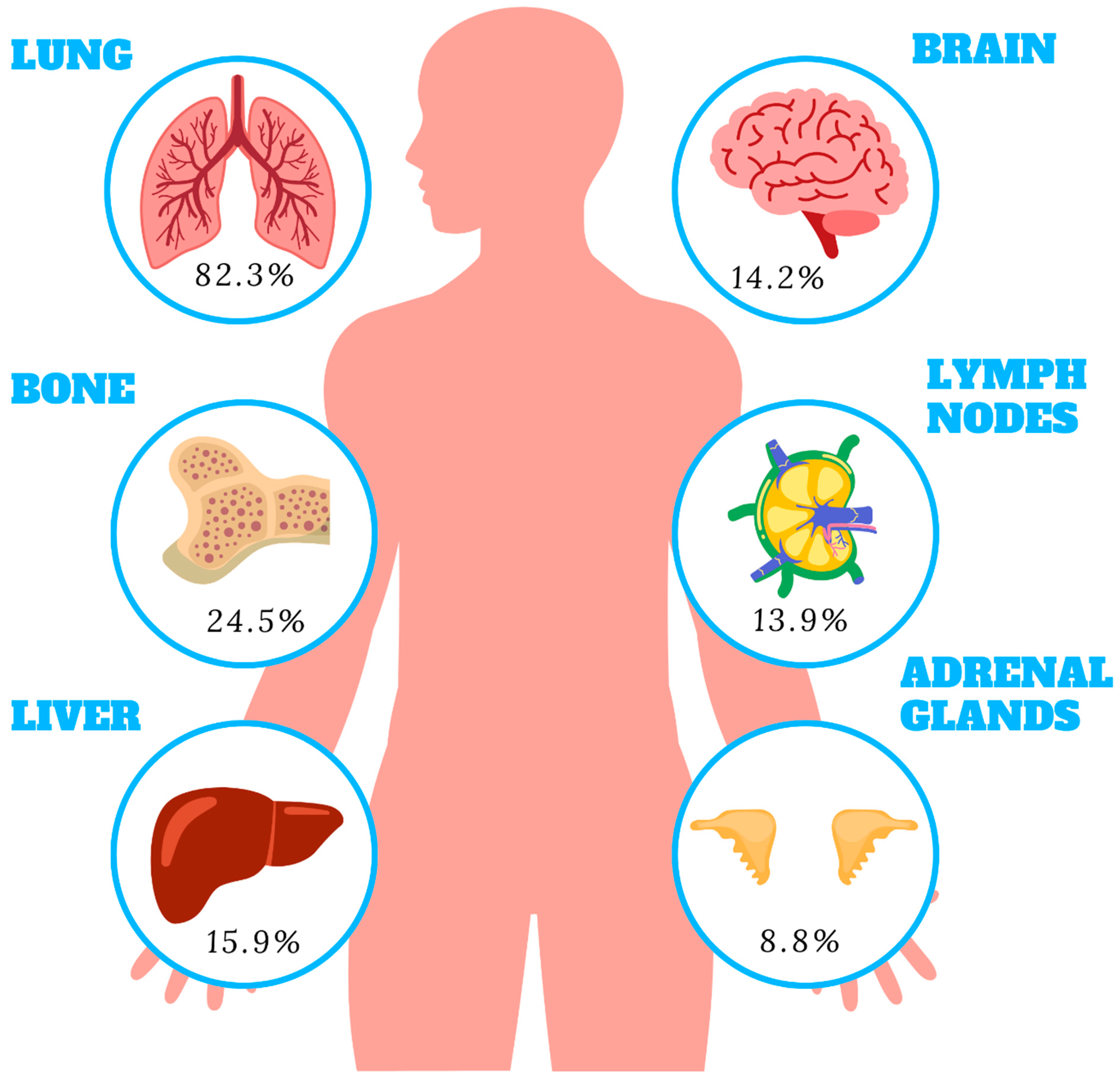
3.3.1. Lung Metastases
3.3.2. Adrenal Metastases
3.3.3. Liver Metastases
3.3.4. Pancreatic Metastases
3.3.5. Other Metastases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| cMS | Complete metastatectomy |
| CN | Cytoreductive nephrectomy |
| CPB | Cardiopulmonary bypass |
| CSM | Cancer specific mortality |
| CSS | Cancer specific survival |
| DFI | Disease free interval |
| DHCA | Deep hypothermic circulatory arrest |
| ECC | Extracorporeal circulation |
| ECOG | Eastern cooperative oncology group |
| ICI | Immune checkpoint inhibitors |
| icMS | Incomplete metastatectomy |
| IMDC | International Metastatic Database Consortium |
| IVC | Inferior vena cava |
| LC | Local control |
| LTB | Low tumor burden |
| mRCC | Metastatic renal cell carcinoma |
| MS | Metastatectomy |
| MSK | Memorial Sloan Kettering |
| mTOR | Mammalian target of rapamycin |
| NLR | Neutrocyte to lymphocyte ratio |
| NSS | Nephron sparing surgery |
| OM | Overall mortality |
| O-RNTT | Open radical nephrectomy with tumor thrombus |
| OS | Overall survival |
| PM | Pulmonary metastasectomy |
| PN | Partial nephrectomy |
| RAPN | Robot assisted partian nephrectomy |
| RA-RNTT | Robot assisted radical nephrectomy with tumor thrombus |
| RCC | Renal cell carcinoma |
| RN | Complete nephrectomy |
| TT | Targeted therapy |
| VEGF | Vascular endothelial growth factor |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.-M. Surgical treatment of renal cell carcinoma with inferior vena cava tumor thrombus. Surg. Today 2022, 52, 1125–1133. [Google Scholar] [CrossRef] [PubMed]
- Benhaim, R.; Oussoultzoglou, E.; Saeedi, Y.; Mouracade, P.; Bachellier, P.; Lang, H. Pancreatic Metastasis from Clear Cell Renal Cell Carcinoma: Outcome of an Aggressive Approach. Urology 2015, 85, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Pantuck, A.J.; Zisman, A.; Belldegrun, A.S. The changing natural history of renal cell carcinoma. J. Urol. 2001, 166, 1611–1623. [Google Scholar] [CrossRef]
- Motzer, R.J.; Bacik, J.; Schwartz, L.H.; Reuter, V.; Russo, P.; Marion, S.; Mazumdar, M. Prognostic Factors for Survival in Previously Treated Patients with Metastatic Renal Cell Carcinoma. J. Clin. Oncol. 2004, 22, 454–463. [Google Scholar] [CrossRef]
- Matuszczak, M.; Kiljańczyk, A.; Salagierski, M. The Role of Focal Therapy and Active Surveillance for Small Renal Mass Therapy. Biomedicines 2022, 10, 2583. [Google Scholar] [CrossRef]
- Palumbo, C.; Pecoraro, A.; Knipper, S.; Rosiello, G.; Tian, Z.; Shariat, S.F.; Simeone, C.; Briganti, A.; Saad, F.; Berruti, A.; et al. Survival and Complication Rates of Metastasectomy in Patients With Metastatic Renal Cell Carcinoma Treated Exclusively With Targeted Therapy: A Combined Population-based Analysis. Anticancer. Res. 2019, 39, 4357–4361. [Google Scholar] [CrossRef]
- Ficarra, V.; Novara, G.; Martignoni, G. The Use of Simplified Versions of the Fuhrman Nuclear Grading System in Clinical Practice Requires the Agreement of a Multidisciplinary Panel of Experts. Eur. Urol. 2009, 56, 782–784. [Google Scholar] [CrossRef]
- Motzer, R.J.; Jonasch, E.; Agarwal, N.; Alva, A.; Baine, M.; Beckermann, K.; Carlo, M.I.; Choueiri, T.K.; Costello, B.A.; Derweesh, I.H.; et al. Kidney Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 71–90. [Google Scholar] [CrossRef]
- Peyton, C.C.; Abel, E.J.; Chipollini, J.; Boulware, D.C.; Azizi, M.; Karam, J.A.; Margulis, V.; Master, V.A.; Matin, S.F.; Raman, J.D.; et al. The Value of Neutrophil to Lymphocyte Ratio in Patients Undergoing Cytoreductive Nephrectomy with Thrombectomy. Eur. Urol. Focus 2018, 6, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Rose, K.M.; Navaratnam, A.K.; Faraj, K.S.; Abdul-Muhsin, H.M.; Syal, A.; Elias, L.; Moss, A.A.; Eversman, W.G.; Stone, W.M.; Money, S.R.; et al. Comparison of Open and Robot Assisted Radical Nephrectomy With Level I and II Inferior Vena Cava Tumor Thrombus: The Mayo Clinic Experience. Urology 2019, 136, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Hanna, N.; Sun, M.; Meyer, C.P.; Nguyen, P.L.; Pal, S.K.; Chang, S.L.; de Velasco, G.; Trinh, Q.-D.; Choueiri, T.K. Survival Analyses of Patients With Metastatic Renal Cancer Treated With Targeted Therapy With or Without Cytoreductive Nephrectomy: A National Cancer Data Base Study. J. Clin. Oncol. 2016, 34, 3267–3275. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.; Wells, J.C.; Donskov, F.; Lee, J.L.; Fraccon, A.; Pasini, F.; Porta, C.; Bowman, I.A.; Bjarnason, G.A.; Ernst, D.S.; et al. Cytoreductive Nephrectomy in Metastatic Papillary Renal Cell Carcinoma: Results from the International Metastatic Renal Cell Carcinoma Database Consortium. Eur. Urol. Oncol. 2019, 2, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, R.; Pignot, G.; Ingles, A.; Crepel, M.; Bigot, P.; Bernhard, J.-C.; Joly, F.; Guy, L.; Ravaud, A.; Azzouzi, A.R.; et al. Nephrectomy improves overall survival in patients with metastatic renal cell carcinoma in cases of favorable MSKCC or ECOG prognostic features. Urol. Oncol. Semin. Orig. Investig. 2015, 33, 339.e9–339.e15. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Wu, W.; Duan, X.; Zeng, G.; Liu, Y. The value of cytoreductive nephrectomy on the survival of metastatic renal carcinoma patients based on the number of site-specific metastases. PLoS ONE 2019, 14, e0215861. [Google Scholar] [CrossRef] [PubMed]
- Lenis, A.T.; Burton, C.S.; Golla, V.; Pooli, A.; Faiena, I.; Johnson, D.C.; Salmasi, A.; Drakaki, A.; Gollapudi, K.; Blumberg, J.; et al. Cytoreductive nephrectomy in patients with metastatic renal cell carcinoma and venous thrombus—Trends and effect on overall survival. Urol. Oncol. Semin. Orig. Investig. 2019, 37, 577.e9–577.e16. [Google Scholar] [CrossRef] [PubMed]
- Lenis, A.T.; Salmasi, A.H.; Donin, N.M.; Faiena, I.; Johnson, D.C.; Drakaki, A.; Gollapudi, K.; Blumberg, J.; Belldegrun, A.S.; Pantuck, A.J.; et al. Trends in usage of cytoreductive partial nephrectomy and effect on overall survival in patients with metastatic renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 78.e21–78.e28. [Google Scholar] [CrossRef] [PubMed]
- DiNatale, R.G.; Xie, W.; Becerra, M.F.; Silagy, A.W.; Attalla, K.; Sanchez, A.; Mano, R.; Marcon, J.; Blum, K.A.; Benfante, N.E.; et al. The Association Between Small Primary Tumor Size and Prognosis in Metastatic Renal Cell Carcinoma: Insights from Two Independent Cohorts of Patients Who Underwent Cytoreductive Nephrectomy. Eur. Urol. Oncol. 2019, 3, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Nini, A.; Capitanio, U.; Larcher, A.; Dell’Oglio, P.; Dehò, F.; Suardi, N.; Muttin, F.; Carenzi, C.; Freschi, M.; Lucianò, R.; et al. Perioperative and Oncologic Outcomes of Nephrectomy and Caval Thrombectomy Using Extracorporeal Circulation and Deep Hypothermic Circulatory Arrest for Renal Cell Carcinoma Invading the Supradiaphragmatic Inferior Vena Cava and/or Right Atrium. Eur. Urol. 2018, 73, 793–799. [Google Scholar] [CrossRef] [PubMed]
- You, D.; Lee, C.; Jeong, I.G.; Song, C.; Lee, J.-L.; Hong, B.; Hong, J.H.; Ahn, H.; Kim, C.-S. Impact of metastasectomy on prognosis in patients treated with targeted therapy for metastatic renal cell carcinoma. J. Cancer Res. Clin. Oncol. 2016, 142, 2331–2338. [Google Scholar] [CrossRef] [PubMed]
- Tornberg, S.V.; Visapää, H.; Kilpeläinen, T.P.; Taari, K.; Järvinen, R.; Erkkilä, K.; Nisen, H.; Järvinen, P. Surgery for metastases of renal cell carcinoma: Outcome of treatments and preliminary assessment of Leuven-Udine prognostic groups in the targeted therapy era. Scand. J. Urol. 2018, 52, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.C.; Flanigan, R.C.; Clark, J.I. Nephrectomy in metastatic renal cell carcinoma. Curr. Treat. Options Oncol. 2003, 4, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Trinh, Q.-D.; Sukumar, S.; Schmitges, J.; Bianchi, M.; Sun, M.; Shariat, S.F.; Sammon, J.D.; Jeldres, C.; Zorn, K.C.; Perrotte, P.; et al. Effect of Nodal Metastases on Cancer-specific Mortality After Cytoreductive Nephrectomy. Ann. Surg. Oncol. 2012, 20, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- Patard, J.-J.; Pignot, G.; Escudier, B.; Eisen, T.; Bex, A.; Sternberg, C.; Rini, B.; Roigas, J.; Choueiri, T.; Bukowski, R.; et al. ICUD-EAU International Consultation on Kidney Cancer 2010: Treatment of Metastatic Disease. Eur. Urol. 2011, 60, 684–690. [Google Scholar] [CrossRef]
- Psutka, S.P.; Chang, S.L.; Cahn, D.; Uzzo, R.G.; McGregor, B.A. Reassessing the Role of Cytoreductive Nephrectomy for Metastatic Renal Cell Carcinoma in 2019. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 276–283. [Google Scholar] [CrossRef]
- Méjean, A.; Ravaud, A.; Thezenas, S.; Colas, S.; Beauval, J.-B.; Bensalah, K.; Geoffrois, L.; Thiery-Vuillemin, A.; Cormier, L.; Lang, H.; et al. Sunitinib Alone or after Nephrectomy in Metastatic Renal-Cell Carcinoma. N. Engl. J. Med. 2018, 379, 417–427. [Google Scholar] [CrossRef]
- Bex, A.; Mulders, P.; Jewett, M.; Wagstaff, J.; Van Thienen, J.V.; Blank, C.U.; Van Velthoven, R.; Del Pilar Laguna, M.; Wood, L.; Van Melick, H.H.E.; et al. Comparison of Immediate vs Deferred Cytoreductive Nephrectomy in Patients With Synchronous Metastatic Renal Cell Carcinoma Receiving Sunitinib: The SURTIME Randomized Clinical Trial. JAMA Oncol. 2019, 5, 164–170. [Google Scholar] [CrossRef]
- Noguchi, K.; Hori, D.; Nomura, Y.; Tanaka, H. Renal Cell Carcinoma with Tumor^|^ndash;Thrombus Extension into the Right Ventricle. Ann. Vasc. Dis. 2012, 5, 376–380. [Google Scholar] [CrossRef]
- Yuan, S.M. Innovations of surgical techniques for the management of inferior vena cava tumor thrombus of renal cell car-cinoma. Minerva Urol. Nefrol. 2014, 66, 189–200. [Google Scholar]
- Campbell, S.C.; Clark, P.E.; Chang, S.S.; Karam, J.A.; Souter, L.; Uzzo, R.G. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-Up: AUA Guideline: Part I. J. Urol. 2021, 206, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.C.; Uzzo, R.G.; Karam, J.A.; Chang, S.S.; Clark, P.E.; Souter, L. Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-up: AUA Guideline: Part II. J. Urol. 2021, 206, 209–218. [Google Scholar] [CrossRef]
- Adibi, M.; Thomas, A.Z.; Borregales, L.D.; Matin, S.F.; Wood, C.G.; Karam, J.A. Surgical considerations for patients with metastatic renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2015, 33, 528–537. [Google Scholar] [CrossRef] [PubMed]
- Ciancio, G.; Vaidya, A.; Savoie, M.; Soloway, M. Management of renal cell carcinoma with level III thrombus in the inferior vena cava. J. Urol. 2002, 168, 1374–1377. [Google Scholar] [CrossRef] [PubMed]
- Cinar, O.; Gunseren, K.O.; Cicek, C.; Vuruskan, B.A.; Vuruskan, H. Laparoscopic Transperitoneal Radical Nephrectomy for Renal Masses with Level I and II Thrombus. J. Laparoendosc. Adv. Surg. Tech. 2019, 29, 35–39. [Google Scholar] [CrossRef]
- Shao, P.; Li, J.; Qin, C.; Lv, Q.; Ju, X.; Li, P.; Shao, Y.; Ni, B.; Yin, C. Laparoscopic Radical Nephrectomy and Inferior Vena Cava Thrombectomy in the Treatment of Renal Cell Carcinoma. Eur. Urol. 2015, 68, 115–122. [Google Scholar] [CrossRef]
- Ishihara, H.; Takagi, T.; Kondo, T.; Fukuda, H.; Tachibana, H.; Yoshida, K.; Iizuka, J.; Kobayashi, H.; Ishida, H.; Tanabe, K. Prognostic impact of metastasectomy in renal cell carcinoma in the postcytokine therapy era. Urol. Oncol. Semin. Orig. Investig. 2020, 39, 77.e17–77.e25. [Google Scholar] [CrossRef]
- Seitlinger, J.; Prieto, M.; Siat, J.; Renaud, S. Pulmonary metastasectomy in renal cell carcinoma: A mainstay of multidisciplinary treatment. J. Thorac. Dis. 2021, 13, 2636–2642. [Google Scholar] [CrossRef]
- Ljungberg, B.; Albiges, L.; Abu-Ghanem, Y.; Bedke, J.; Capitanio, U.; Dabestani, S.; Fernández-Pello, S.; Giles, R.H.; Hofmann, F.; Hora, M.; et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Eur. Urol. 2022, 82, 399–410. [Google Scholar] [CrossRef]
- Pastorino, U.; Buyse, M.; Friedel, G.; Ginsberg, R.J.; Girard, P.; Goldstraw, P.; Johnston, M.; McCormack, P.; Pass, H.; Putnam, J.B., Jr.; et al. Long-term results of lung metastasectomy: Prognostic analyses based on 5206 cases. J. Thorac. Cardiovasc. Surg. 1997, 113, 37–49. [Google Scholar] [CrossRef]
- Meimarakis, G.; Angele, M.; Staehler, M.; Clevert, D.-A.; Crispin, A.; Rüttinger, D.; Löhe, F.; Preissler, G.; Hatz, R.A.; Winter, H. Evaluation of a new prognostic score (Munich score) to predict long-term survival after resection of pulmonary renal cell carcinoma metastases. Am. J. Surg. 2011, 202, 158–167. [Google Scholar] [CrossRef]
- Ouzaid, I.; Capitanio, U.; Staehler, M.; Wood, C.G.; Leibovich, B.C.; Ljungberg, B.; Van Poppel, H.; Bensalah, K. Surgical Metastasectomy in Renal Cell Carcinoma: A Systematic Review. Eur. Urol. Oncol. 2018, 2, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Amiraliev, A.; Pikin, O.; Alekseev, B.Y.; Kalpinksiy, A. Treatment strategy in patients with pulmonary metastases of renal cell cancer. Interact. CardioVasc. Thorac. Surg. 2012, 15, SXIII-F068. [Google Scholar]
- Procházková, K.; Vodička, J.; Fichtl, J.; Krákorová, G.; Šebek, J.; Roušarová, M.; Hosek, P.; May, S.D.B.; Hes, O.; Hora, M.; et al. Outcomes for Patients after Resection of Pulmonary Metastases from Clear Cell Renal Cell Carcinoma: 18 Years of Experience. Urol. Int. 2019, 103, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Meacci, E.; Nachira, D.; Congedo, M.T.; Porziella, V.; Chiappetta, M.; Ferretti, G.; Iaffaldano, A.; Ciavarella, L.P.; Margaritora, S. Lung metastasectomy following kidney tumors: Outcomes and prognostic factors from a single-center experience. J. Thorac. Dis. 2017, 9, S1267–S1272. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, A.; Cozzoli, A.; Simeone, C.; Zani, D.; Zanotelli, T.; Portesi, E.; Cunico, S.C. Surgical treatment of adrenal metastasis from renal cell carcinoma: A single-centre experience of 45 patients. BJU Int. 2006, 97, 505–508. [Google Scholar] [CrossRef] [PubMed]
- Hatzaras, I.; Gleisner, A.L.; Pulitano, C.; Sandroussi, C.; Hirose, K.; Hyder, O.; Wolfgang, C.L.; Aldrighetti, L.; Crawford, M.; Choti, M.A.; et al. A multi-institution analysis of outcomes of liver-directed surgery for metastatic renal cell cancer. HPB 2012, 14, 532–538. [Google Scholar] [CrossRef]
- Staehler, M.D.; Kruse, J.; Haseke, N.; Stadler, T.; Roosen, A.; Karl, A.; Stief, C.G.; Jauch, K.W.; Bruns, C.J. Liver resection for metastatic disease prolongs survival in renal cell carcinoma: 12-year results from a retrospective comparative analysis. World J. Urol. 2010, 28, 543–547. [Google Scholar] [CrossRef]
- Ballarin, R.; Spaggiari, M.; Cautero, N.; De Ruvo, N.; Montalti, R.; Longo, C.; Pecchi, A.; Giacobazzi, P.; De Marco, G.; D’Amico, G.; et al. Pancreatic metastases from renal cell carcinoma: The state of the art. World J. Gastroenterol. 2011, 17, 4747–4756. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis, I.T.; Dursun, A.; Zheng, H.; Wargo, J.A.; Thayer, S.P.; Castillo, C.F.-D.; Warshaw, A.L.; Ferrone, C.R. Metastatic Tumors in the Pancreas in the Modern Era. J. Am. Coll. Surg. 2010, 211, 749–753. [Google Scholar] [CrossRef]
- Tanis, P.J.; van der Gaag, N.A.; Busch, O.R.C.; van Gulik, T.M.; Gouma, D.J. Systematic review of pancreatic surgery for metastatic renal cell carcinoma. Br. J. Surg. 2009, 96, 579–592. [Google Scholar] [CrossRef] [PubMed]
- Zerbi, A.; Ortolano, E.; Balzano, G.; Borri, A.; Beneduce, A.A.; Di Carlo, V. Pancreatic Metastasis From Renal Cell Carcinoma: Which Patients Benefit From Surgical Resection? Ann. Surg. Oncol. 2008, 15, 1161–1168. [Google Scholar] [CrossRef]
- Fikatas, P.; Klein, F.; Andreou, A.; Schmuck, R.B.; Pratschke, J.; Bahra, M. Long-term Survival After Surgical Treatment of Renal Cell Carcinoma Metastasis Within the Pancreas. Anticancer Res. 2016, 36, 4273–4278. [Google Scholar] [PubMed]
- Faiena, I.; Salmasi, A.; Lenis, A.T.; Donin, N.M.; Johnson, D.C.; Bachour, K.; Drakaki, A.; Belldegrun, A.S.; Pantuck, A.J.; Chamie, K. Overall survival in patients with metastatic renal cell carcinoma and clinical N1 disease undergoing cytoreductive nephrectomy and lymph node dissection. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 79.e19–79.e26. [Google Scholar] [CrossRef] [PubMed]
- Leibovich, B.C.; Cheville, J.C.; Lohse, C.M.; Zincke, H.; Frank, I.; Kwon, E.D.; Merchan, J.R.; Blute, M.L. A scoring algorithm to predict survival for patients with metastatic clear cell renal cell carcinoma: A stratification tool for prospective clinical trials. J. Urol. 2005, 174, 1759–1763. [Google Scholar] [CrossRef] [PubMed]
- Alt, A.L.; Boorjian, S.A.; Lohse, C.M.; Costello, B.A.; Leibovich, B.C.; Blute, M.L. Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer 2011, 117, 2873–2882. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, P.-Y.; Hung, S.-C.; Li, J.-R.; Wang, S.-S.; Yang, C.-K.; Chen, C.-S.; Lu, K.; Cheng, C.-L.; Chiu, K.-Y. The effect of metastasectomy on overall survival in metastatic renal cell carcinoma: A systematic review and meta-analysis. Urol. Oncol. Semin. Orig. Investig. 2021, 39, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-R.; Ou, Y.-C.; Yang, C.-K.; Wang, S.-S.; Chen, C.-S.; Ho, H.-C.; Cheng, C.-L.; Yang, C.-R.; Chen, C.-C.; Wang, S.-C.; et al. The Impact of Local Intervention Combined with Targeted Therapy on Metastatic Renal Cell Carcinoma. Anticancer Res. 2018, 38, 5339–5345. [Google Scholar] [CrossRef]
- Kato, S.; Murakami, H.; Demura, S.; Nambu, K.; Fujimaki, Y.; Yoshioka, K.; Kawahara, N.; Tomita, K.; Tsuchiya, H. Spinal metastasectomy of renal cell carcinoma: A 16-year single center experience with a minimum 3-year follow-up. J. Surg. Oncol. 2016, 113, 587–592. [Google Scholar] [CrossRef]
- Jakubowski, C.D.; Vertosick, E.A.; Untch, B.R.; Sjoberg, D.; Wei, E.; Palmer, F.L.; Patel, S.G.; Downey, R.J.; Strong, V.E.; Russo, P. Complete metastasectomy for renal cell carcinoma: Comparison of five solid organ sites. J. Surg. Oncol. 2016, 114, 375–379. [Google Scholar] [CrossRef]

| Study | Study Group | Study Goal | Results | ||
|---|---|---|---|---|---|
| Palumbo et al. [8] | n = 3654 | MS vs. no MS comparison | MS (n = 437) Median OS = 11 months | No MS (n = 3217) Median OS = 9 months | |
| Peyton et al. [11] | n = 447 | Utility of NLR in mRCC with tumor thrombus undergoing CN | Median follow-up = 24 months Mean OS = 50.6 months | ||
| Rose et al. [12] | n = 75 | O-RNTT vs. RA-RNTT (level I, II) comparison | O-RNTT (n = 27) Median follow-up = 79 months Mean OS = 48.7 months | RA-RNTT (n = 24) Median follow-up = 24 months Mean OS = 50.6 months | |
| Hanna et al. [13] | n = 15,390 | CN vs. non-CN survival analysis | CN (n = 5374) 1 yr OS = 62.7% 2 yr OS = 39.1% 3 yr OS = 27.7% | Non-CN (n = 10,016) 1 yr OS = 34.7% 2 yr OS = 17.1% 3 yr OS = 9.8% | |
| Graham et al. [14] | n = 353 | CN vs. non-CN survival analysis | CN (n = 109) Median OS = 16.3 months PFS = 5.1 months | Non-CN (n = 244) Median OS = 8.6 months PFS = 3.4 months | |
| Mathieu et al. [15] | n = 351 | CN vs. non-CN survival analysis | CN (n = 298) Median OS = 38.1 months | Non-CN (n = 53) Median OS = 16.4 months | |
| Zhao et al. [16] | n = 1113 | CN vs. no surgery comparison | CN (n = 618) Median OS = 26 months 1 yr OS = 70.7% 1 yr CSM = 27.9% | No surgery (n = 495) Median OS = 9 months 1 yr OS = 43.6% 1 yr CSM = 60.3% | |
| Lenis et al. [17] | n = 4962 | CN vs. non-CN survival analysis | CN (n = 2460) 1 yr OS = 66.65% 2 yr OS = 39.16% 5 yr OS = 2.25% | Non-CN (n = 1502) 1 yr OS = 40.75% 2 yr OS = 19.04% 5 yr OS = 0.4% | |
| n = 2056 | CN vs. non-CN survival analysis (with IVC thrombus) | Renal vein thrombus CN median OS = 24.0 months Non-CN median OS = 9.2 months | Infradiaphragmic thrombus CN median OS = 22.3 months Non-CN median OS = 11.5 months | Supradiaphragmic thrombus CN median OS = 13.1 months Non-CN median OS = 10.3 months | |
| Lenis et al. [18] | n = 1047 | PN vs. RN comparison | PN (n = 381) 1 yr OS = 76% 2 yr OS = 49.61% 5 yr OS = 13.12% Median follow-up = 23.7 months | RN (n = 666) 1 yr OS = 64.7% 2 yr OS = 42.04% 5 yr OS = 9.46% Median follow-up = 17.4 months | |
| DiNatale et al. [19] | n = 1082 | Assessing tumor size on survival of PN patients | MSK cohort (n = 304) Median follow-up = 44.2 months 2 yr OS = 65.8% 5 yr OS = 31.2% | IMDC cohort (n = 778) Median follow-up = 28.7 months 2 yr OS = 65.3% 5 yr OS = 28.3% | |
| Nini et al. [20] | n = 46 | Comparison of OS in cM0 vs. cM1 RN with ECC and DHCA cohort | cM1 (n = 15) 1 yr OS = 46% 2 yr OS = 23% 3 yr OS = 23% | cM0 (n = 31) 1 yr OS = 89% 2 yr OS = 75% 3 yr OS = 63% | |
| You et al. [21] | n = 325 | cMS vs. icMS vs. no-MS comparison | cMS (n = 33) 2 yr OS = 81.82% 4 yr OS = 51.52% | icMS (n = 29) 2 yr OS = 51.72% 4 yr OS = 13.79% | No-MS (n = 263) 2 yr OS = 22.05% 4 yr OS = 4.94% |
| Tornberg et al. [22] | n = 97 | cMS vs. icMS comparison | cMS (n = 46) 5 yr OS = 59% 1 yr RFS = 29.79% 5 yr RFS = 4.26% | icMS (n = 51) 5 yr OS = 45% | |
| Tumor Thrombus Level | Clinical Description |
|---|---|
| I | Extension to the renal vein only |
| II | Infrahepatic IVC extension |
| III | Intrahepatic IVC extension |
| IIIa | Intrahepatic IVC extension (above the liver edge, below the level of hepatic veins) |
| IIIb | Hepatic IVC extension |
| IIIc | Suprahepatic, infradiaphragmatic extension |
| IIId | Suprahepatic, supradiaphragmatic, infraatrial extension |
| IV | Atrial extension |
| Parameter | Prognostic Group | |||
|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 4 | |
| Resectability | resectable | resectable | resectable | unresectable |
| Risk factors: | 0 | 1 | 2 | N/A |
| Disease-free interval (DFI) | >36 mo | <36 mo | <36 | N/A |
| Number of metastases | and | or | and | N/A |
| single | multiple | multiple | N/A | |
| Prognostic Factors | Groups |
|---|---|
| Pleural infiltration | I—low risk: no risk factors, R0 |
| Synchronous manifestation of primary RCC and pulmonary metastases | II—intermediate risk: ≥1 risk factor, R0 |
| Nodal status of the primary tumor | III—high risk: R1 or R2 |
| Metastasis size > 3 cm | |
| Mediastinal and/or hilar lymph node metastases | |
| Completeness of metastatectomy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matuszczak, M.; Kiljańczyk, A.; Salagierski, M. Surgical Approach in Metastatic Renal Cell Carcinoma: A Literature Review. Cancers 2023, 15, 1804. https://doi.org/10.3390/cancers15061804
Matuszczak M, Kiljańczyk A, Salagierski M. Surgical Approach in Metastatic Renal Cell Carcinoma: A Literature Review. Cancers. 2023; 15(6):1804. https://doi.org/10.3390/cancers15061804
Chicago/Turabian StyleMatuszczak, Milena, Adam Kiljańczyk, and Maciej Salagierski. 2023. "Surgical Approach in Metastatic Renal Cell Carcinoma: A Literature Review" Cancers 15, no. 6: 1804. https://doi.org/10.3390/cancers15061804
APA StyleMatuszczak, M., Kiljańczyk, A., & Salagierski, M. (2023). Surgical Approach in Metastatic Renal Cell Carcinoma: A Literature Review. Cancers, 15(6), 1804. https://doi.org/10.3390/cancers15061804






