Melanoma Brain Metastases: A Retrospective Analysis of Prognostic Factors and Efficacy of Multimodal Therapies
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Statistical Analysis
2.3. Ethics Approval and Consent to Participate
3. Results
3.1. Baseline Demographic Features
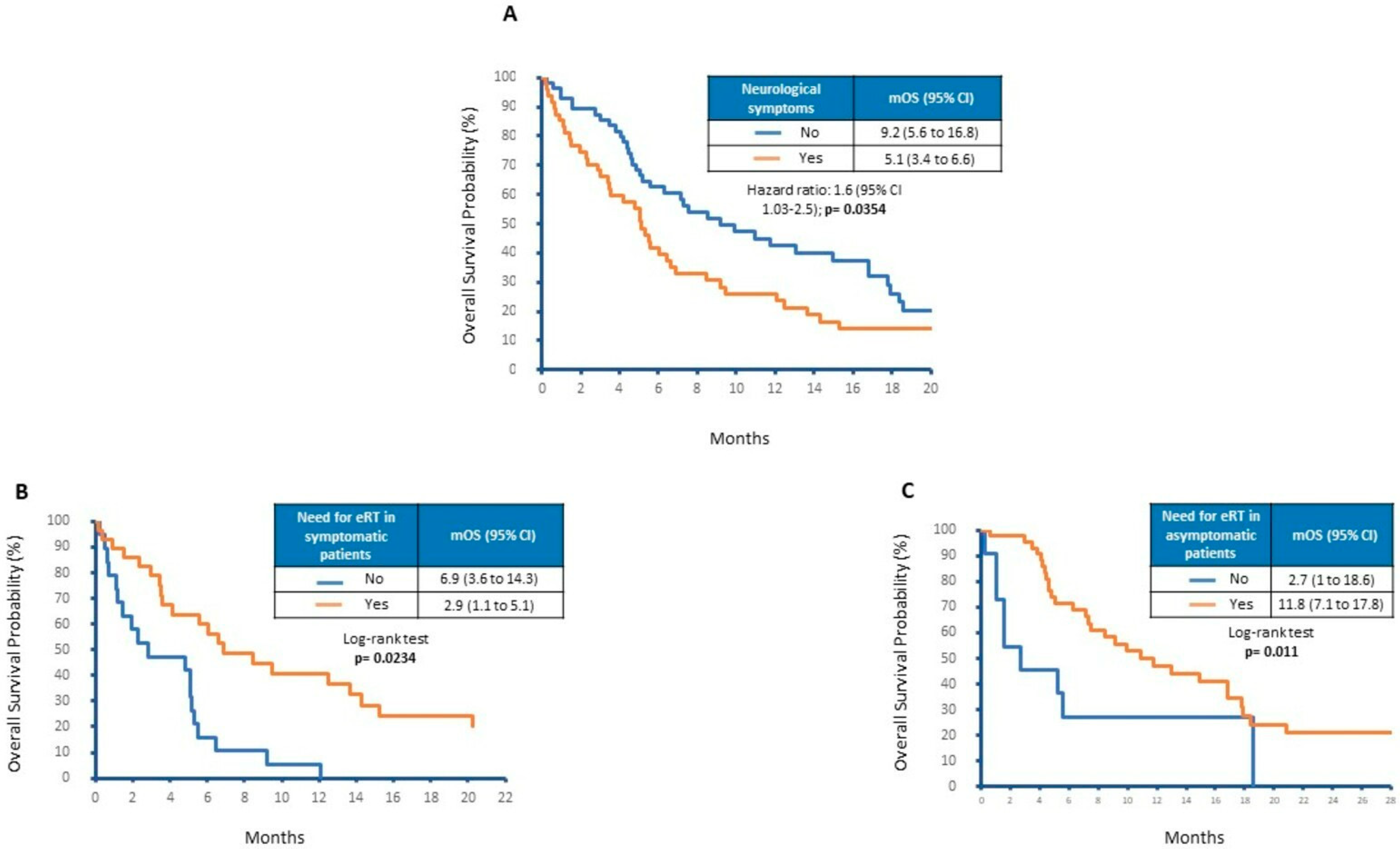
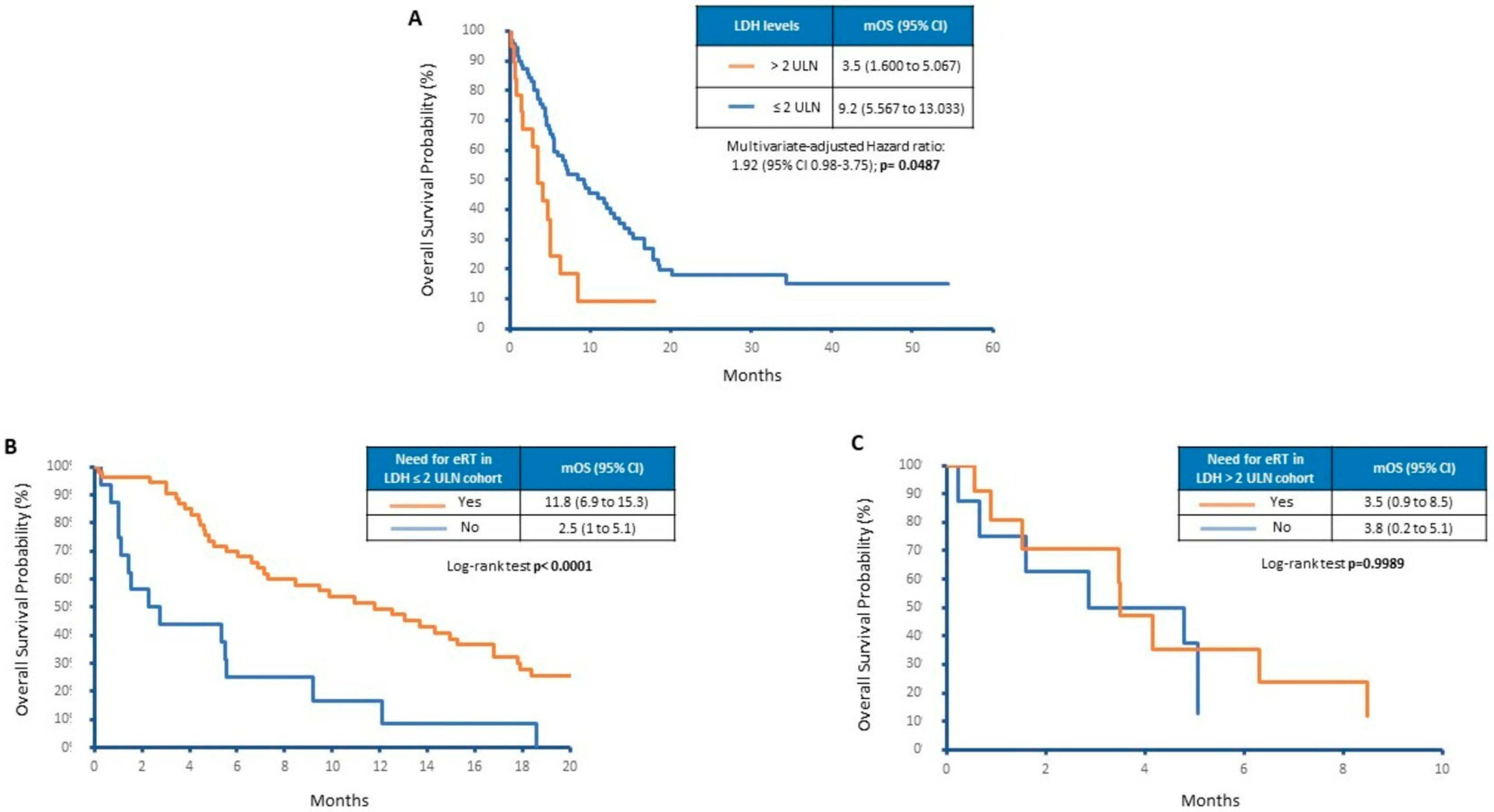
3.2. Neurological Symptoms and Factors Associated with Overall Survival
3.3. Impact of Treatments on Overall Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lamba, N.; Wen, P.Y.; Aizer, A.A. Epidemiology of brain metastases and leptomeningeal disease. Neuro Oncol. 2021, 23, 1447–1456. [Google Scholar] [CrossRef] [PubMed]
- Tadros, S.; Ray-Chaudhury, A. Pathological Features of Brain Metastases. Neurosurg. Clin. N. Am. 2020, 31, 549–564. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, M.R.S.; Chiang, V.L.; Tran, T.; Yu, J.B.; Weiss, S.A.; Goldberg, S.B.; Aboian, M.S.; Kluger, H.M.; Mahajan, A. Incidence and characteristics of metastatic intracranial lesions in stage III and IV melanoma: A single institute retrospective analysis. J. Neuro-Oncol. 2021, 154, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Bander, E.D.; Yuan, M.; Carnevale, J.A.; Reiner, A.S.; Panageas, K.S.; Postow, M.A.; Tabar, V.; Moss, N.S. Melanoma brain metastasis presentation, treatment, and outcomes in the age of targeted and immunotherapies. Cancer 2021, 127, 2062–2073. [Google Scholar] [CrossRef]
- Sperduto, P.W.; Mesko, S.; Li, J.; Cagney, D.; Aizer, A.; Lin, N.U.; Nesbit, E.; Kruser, T.J.; Chan, J.; Braunstein, S.; et al. Survival in Patients With Brain Metastases: Summary Report on the Updated Diagnosis-Specific Graded Prognostic Assessment and Definition of the Eligibility Quotient. J. Clin. Oncol. 2020, 38, 3773–3784. [Google Scholar] [CrossRef]
- Davies, M.A.; Liu, P.; McIntyre, S.; Kim, K.B.; Papadopoulos, N.; Hwu, W.J.; Hwu, P.; Bedikian, A. Prognostic factors for survival in melanoma patients with brain metastases. Cancer 2011, 117, 1687–1696. [Google Scholar] [CrossRef]
- Sacks, P.; Rahman, M. Epidemiology of Brain Metastases. Neurosurg. Clin. N. Am. 2020, 31, 481–488. [Google Scholar] [CrossRef]
- Chaung, K.V.; Sloan, A.E.; Choi, S. Limited brain metastases: A narrative review. Ann. Pall. Med. 2021, 10, 6016–6027. [Google Scholar] [CrossRef]
- Phillips, W.J.; Baghai, T.; Ong, M.; Lo, B.; Ibrahim, A.M.; Smith, T.K.T.; Song, X. A Contemporary Report of Clinical Outcomes in Patients with Melanoma Brain Metastases. Curr. Oncol. 2021, 28, 428–439. [Google Scholar] [CrossRef]
- Keung, E.Z.; Gershenwald, J.E. The eighth edition American Joint Committee on Cancer (AJCC) melanoma staging system: Implications for melanoma treatment and care. Exp. Rev. Anticanc. 2018, 18, 775–784. [Google Scholar] [CrossRef]
- Tawbi, H.; To, T.M.; Bartley, K.; Sadetsky, N.; Burton, E.; Haydu, L.; McKenna, E. Treatment patterns and clinical outcomes for patients with melanoma and central nervous system metastases: A real-world study. Cancer Med. 2022, 11, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Gutzmer, R.; Vordermark, D.; Hassel, J.C.; Krex, D.; Wendl, C.; Schadendorf, D.; Sickmann, T.; Rieken, S.; Pukrop, T.; Höller, C.; et al. Melanoma brain metastases-Interdisciplinary management recommendations 2020. Cancer Treat Rev. 2020, 89, 102083. [Google Scholar] [CrossRef] [PubMed]
- Becco, P.; Gallo, S.; Poletto, S.; Frascione, M.P.M.; Crotto, L.; Zaccagna, A.; Paruzzo, L.; Caravelli, D.; Carnevale-Schianca, F.; Aglietta, M. Melanoma Brain Metastases in the Era of Target Therapies: An Overview. Cancers 2020, 12, 1640. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.A.; Saiag, P.; Robert, C.; Grob, J.J.; Flaherty, K.T.; Arance, A.; Chiarion-Sileni, V.; Thomas, L.; Lesimple, T.; Mortier, L.; et al. Dabrafenib plus trametinib in patients with BRAFV600-mutant melanoma brain metastases (COMBI-MB): A multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 2017, 18, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Grob, J.J.; Stroyakovskiy, D.; Karaszewska, B.; Hauschild, A.; Levchenko, E.; Chiarion Sileni, V.; Schachter, J.; Garbe, C.; Bondarenko, I.; et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N Eng. J. Med. 2019, 381, 626–636. [Google Scholar] [CrossRef]
- Grob, J.J.; Amonkar, M.M.; Karaszewska, B.; Schachter, J.; Dummer, R.; Mackiewicz, A.; Stroyakovskiy, D.; Drucis, K.; Grange, F.; Chiarion-Sileni, V.; et al. Comparison of dabrafenib and trametinib combination therapy with vemurafenib monotherapy on health-related quality of life in patients with unresectable or metastatic cutaneous BRAF Val600-mutation-positive melanoma (COMBI-v): Results of a phase 3, open-label, randomised trial. Lancet Oncol. 2015, 16, 1389–1398. [Google Scholar]
- Goldberg, S.B.; Gettinger, S.N.; Mahajan, A.; Chiang, A.C.; Herbst, R.S.; Sznol, M.; Tsiouris, A.J.; Cohen, J.; Vortmeyer, A.; Jilaveanu, L.; et al. Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: Early analysis of a non-randomised, open-label, phase 2 trial. Lancet. Oncol. 2016, 17, 976–983. [Google Scholar] [CrossRef]
- Larkin, J.; Minor, D.; D’Angelo, S.; Neyns, B.; Smylie, M.; Miller, W.H., Jr.; Gutzmer, R.; Linette, G.; Chmielowski, B.; Lao, C.D.; et al. Overall Survival in Patients With Advanced Melanoma Who Received Nivolumab Versus Investigator’s Choice Chemotherapy in CheckMate 037: A Randomized, Controlled, Open-Label Phase III Trial. J. Clin. Oncol. 2018, 36, 383–390. [Google Scholar] [CrossRef]
- Patel, K.R.; Lawson, D.H.; Kudchadkar, R.R.; Carthon, B.C.; Oliver, D.E.; Okwan-Duodu, D.; Ahmed, R.; Khan, M.K. Two heads better than one? Ipilimumab immunotherapy and radiation therapy for melanoma brain metastases. Neuro-Oncol. 2015, 17, 1312–1321. [Google Scholar] [CrossRef]
- Long, G.V.; Atkinson, V.; Lo, S.; Sandhu, S.; Guminski, A.D.; Brown, M.P.; Wilmott, J.S.; Edwards, J.; Gonzalez, M.; Scolyer, R.A.; et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: A multicentre randomised phase 2 study. Lancet Oncol. 2018, 19, 672–681. [Google Scholar] [CrossRef]
- Tawbi, H.A.; Forsyth, P.A.; Hodi, F.S.; Lao, C.D.; Moschos, S.J.; Hamid, O.; Atkins, M.B.; Lewis, K.; Thomas, R.P.; Glaspy, J.A.; et al. Safety and efficacy of the combination of nivolumab plus ipilimumab in patients with melanoma and asymptomatic or symptomatic brain metastases (CheckMate 204). Neuro-Oncol. 2021, 23, 1961–1973. [Google Scholar] [CrossRef] [PubMed]
- Dummer, R.; Queirolo, P.; Abajo Guijarro, A.M.; Hu, Y.; Wang, D.; Azevedo, S.J.; Robert, C.; Ascierto, P.A.; Chiarion -Sileni, V.; Pronzato, P.; et al. Atezolizumab (A), cobimetinib (C), and vemurafenib (V) in patients (pts) with BRAFV600 mutation–positive melanoma with central nervous system (CNS) metastases (mets): Primary results from phase 2 Tricotel study. J. Clin. Oncol. 2022, 40 (Suppl. 16), 9515. [Google Scholar] [CrossRef]
- Lau, P.K.H.; Feran, B.; Smith, L.; Lasocki, A.; Molania, R.; Smith, K.; Weppler, A.; Angel, C.; Kee, D.; Bhave, P.; et al. Melanoma brain metastases that progress on BRAF-MEK inhibitors demonstrate resistance to ipilimumab-nivolumab that is associated with the Innate PD-1 Resistance Signature (IPRES). J. Immunother. Cancer 2021, 9, e002995. [Google Scholar] [CrossRef] [PubMed]
- Wegner, R.E.; Abel, S.; D’Amico, R.S.; Mehta, G.U.; Sheehan, J. Time from stereotactic radiosurgery to immunotherapy in patients with melanoma brain metastases and impact on outcome. J. Neuro-Oncol. 2021, 152, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Kim, P.H.; Suh, C.H.; Kim, H.S.; Kim, K.W.; Kim, D.Y.; Lee, E.Q.; Aizer, A.A.; Guenette, J.P.; Huang, R.Y. Immune Checkpoint Inhibitor with or without Radiotherapy in Melanoma Patients with Brain Metastases: A Systematic Review and Meta-Analysis. K. J. Radiol. 2021, 22, 584–595. [Google Scholar] [CrossRef]
- Moyers, J.T.; Chong, E.G.; Peng, J.; Tsai, H.H.C.; Sufficool, D.; Shavlik, D.; Nagaraj, G. Real world outcomes of combination and timing of immunotherapy with radiotherapy for melanoma with brain metastases. Cancer Med. 2021, 10, 1201–1211. [Google Scholar] [CrossRef]
- Lamba, N.; Aizer, A.A. The evolving role of systemic therapy and local, brain-directed treatment in patients with melanoma and brain metastases. Neuro-Oncol. 2021, 23, 1816–1817. [Google Scholar] [CrossRef]
- White, R.J.; Abel, S.; Horne, Z.D.; Lee, J.; Edington, H.; Greenberg, L.; Younes, H.; Hilton, C.; Wegner, R.E. Melanoma brain metastases: Is it time to eliminate radiotherapy? J. Neuro-Oncol. 2020, 149, 27–33. [Google Scholar] [CrossRef]
- Cortellini, A.; Tucci, M.; Adamo, V.; Stucci, L.S.; Russo, A.; Tanda, E.T.; Spagnolo, F.; Rastelli, F.; Bisonni, R.; Santini, D.; et al. Integrated analysis of concomitant medications and oncological outcomes from PD-1/PD-L1 checkpoint inhibitors in clinical practice. J. Immunother. Cancer 2020, 8, e001361. [Google Scholar] [CrossRef]
- Frinton, E.; Tong, D.; Tan, J.; Read, G.; Kumar, V.; Kennedy, S.; Lim, C.; Board, R.E. Metastatic melanoma: Prognostic factors and survival in patients with brain metastases. J. Neuro-Oncol. 2017, 135, 507–512. [Google Scholar] [CrossRef]
- Weide, B.; Elsässer, M.; Büttner, P.; Pflugfelder, A.; Leiter, U.; Eigentler, T.K.; Bauer, J.; Witte, M.; Meier, F.; Garbe, C. Serum markers lactate dehydrogenase and S100B predict independently disease outcome in melanoma patients with distant metastasis. Br. J. Cancer 2012, 107, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Marcus, D.M.; Lowe, M.; Khan, M.K.; Lawson, D.H.; Crocker, I.R.; Shelton, J.W.; Melton, A.; Maynard, N.; Delman, K.A.; Carlson, G.W.; et al. Prognostic factors for overall survival after radiosurgery for brain metastases from melanoma. Am. J. Clin. Oncol. 2014, 37, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Neal, M.T.; Chan, M.D.; Lucas, J.T., Jr.; Loganathan, A.; Dillingham, C.; Pan, E.; Stewart, J.H., 4th; Bourland, J.D.; Shaw, E.G.; Tatter, S.B.; et al. Predictors of survival, neurologic death, local failure, and distant failure after gamma knife radiosurgery for melanoma brain metastases. World Neurosurg. 2014, 82, 1250–1255. [Google Scholar] [CrossRef] [PubMed]
- Rishi, A.; Yu, H.M. Current Treatment of Melanoma Brain Metastasis. Curr. Treat. Opt. Oncol. 2020, 21, 45. [Google Scholar] [CrossRef]
- Shibahara, I.; Kanamori, M.; Watanabe, T.; Utsunomiya, A.; Suzuki, H.; Saito, R.; Sonoda, Y.; Jokura, H.; Uenohara, H.; Tominaga, T. Clinical Features of Precocious, Synchronous, and Metachronous Brain Metastases and the Role of Tumor Resection. World Neurosurg. 2018, 113, e1–e9. [Google Scholar] [CrossRef]
- Anvari, A.; Sasanpour, P.; Kheradmardi, M.R. Radiotherapy and Immunotherapy in Melanoma Brain Metastases. Hematol Oncol Stem Cell Ther. 2023, 16, 1–20. [Google Scholar] [CrossRef]
- Raizer, J.J.; Hwu, W.J.; Panageas, K.S.; Wilton, A.; Baldwin, D.E.; Bailey, E.; von Althann, C.; Lamb, L.A.; Alvarado, G.; Bilsky, M.H.; et al. Brain and leptomeningeal metastases from cutaneous melanoma: Survival outcomes based on clinical features. Neur.-Oncol. 2008, 10, 199–207. [Google Scholar] [CrossRef]
- Wagner, N.B.; Forschner, A.; Leiter, U.; Garbe, C.; Eigentler, T.K. S100B and LDH as early prognostic markers for response and overall survival in melanoma patients treated with anti-PD-1 or combined anti-PD-1 plus anti-CTLA-4 antibodies. Br. J. Cancer 2018, 119, 339–346. [Google Scholar] [CrossRef]
- Placzke, J.; Teterycz, P.; Quaglino, P.; Cybulska-Stopa, B.; Tucci, M.; Rubatto, M.; Skora, T.; Interno, V.; Rosinska, M.; Borkowska, A.; et al. The Analysis of Trends in Survival for Patients with Melanoma Brain Metastases with Introduction of Novel Therapeutic Options before the Era of Combined Immunotherapy-Multicenter Italian-Polish Report. Cancers 2022, 14, 5763. [Google Scholar] [CrossRef]
- Knispel, S.; Gassenmaier, M.; Menzies, A.M.; Loquai, C.; Johnson, D.B.; Franklin, C.; Gutzmer, R.; Hassel, J.C.; Weishaupt, C.; Eigentler, T.; et al. Outcome of melanoma patients with elevated LDH treated with first-line targeted therapy or PD-1-based immune checkpoint inhibition. Eur. J. Cancer 2021, 148, 61–75. [Google Scholar] [CrossRef]
- Scott, K.E.; Cleveland, J.L. Lactate Wreaks Havoc on Tumor-Infiltrating T and NK Cells. Cell Metab. 2016, 24, 649–650. [Google Scholar] [CrossRef] [PubMed]
- Daneshmandi, S.; Wegiel, B.; Seth, P. Blockade of Lactate Dehydrogenase-A (LDH-A) Improves Efficacy of Anti-Programmed Cell Death-1 (PD-1) Therapy in Melanoma. Cancers 2019, 11, 450. [Google Scholar] [CrossRef] [PubMed]

| Number | % | ||
|---|---|---|---|
| Sex | Male | 61 | 58 |
| Female | 44 | 42 | |
| Primary site | Limbs | 36 | 34 |
| Head and neck | 9 | 9 | |
| Trunk | 53 | 50 | |
| Other sites | 7 | 7 | |
| Histology | SSM | 39 | 38 |
| Nodular | 49 | 47 | |
| Animal type | 6 | 7 | |
| Unknown | 11 | 8 | |
| Breslow depth | ≤1 mm | 10 | 10 |
| >1–2 mm | 11 | 11 | |
| >2–4 mm | 35 | 33 | |
| >4 mm | 34 | 32 | |
| Unknown | 15 | 14 | |
| Ulceration | Present | 46 | 43 |
| Absent | 50 | 48 | |
| Unknown | 9 | 9 | |
| Mitosis | ≤1 | 38 | 36 |
| >1 | 67 | 64 | |
| BRAF status | Mutated | 58 | 55 |
| Wild-type | 47 | 45 | |
| NRAS status | Mutated | 7 | 12 |
| Wild-type | 53 | 88 | |
| LDH at melanoma diagnosis | ≤2 × ULN | 67 | 64 |
| >2 × ULN | 5 | 5 | |
| Unknown | 33 | 31 |
| Number | % | ||
|---|---|---|---|
| Extracranial metastases | Yes | 95 | 90 |
| No | 10 | 10 | |
| Number of extracranial metastatic sites | ≤2 | 52 | 50 |
| >2 | 37 | 35 | |
| Unknown | 16 | 15 | |
| Timing of BMs from melanoma diagnosis | Synchronous | 3 | 3 |
| Metachronous | 102 | 97 | |
| Timing of BMs from extracranial progression | Synchronous | 38 | 36 |
| Subsequent | 64 | 61 | |
| Unknown | 3 | 3 | |
| Site of BMs | Supra-tentorial | 54 | 51 |
| Infra-tentorial | 6 | 6 | |
| Supra- and infra-tentorial | 25 | 24 | |
| Unknown | 20 | 19 | |
| Number of BMs | ≤3 | 62 | 59 |
| >3 | 39 | 37 | |
| Unknown | 20 | 19 | |
| LDH levels at BM diagnosis | ≤2 × ULN | 71 | 68 |
| >2 × ULN | 19 | 18 | |
| Unknown | 15 | 14 | |
| Symptomatic BMs | Yes | 47 | 45 |
| No | 58 | 55 | |
| Neurosurgery | Yes | 13 | 12 |
| No | 92 | 88 | |
| Encephalic radiotherapy | Yes | 75 | 71 |
| No | 30 | 29 | |
| Type of encephalic radiotherapy | Stereotactic radiotherapy | 49 | 65 |
| Whole brain radiotherapy | 26 | 35 | |
| First-line systemic treatment | Targeted therapy with anti-BRAF + anti-MEK | 43 | 41 |
| Immunotherapy | 44 | 42 | |
| Chemotherapy | 3 | 3 | |
| None | 15 | 14 |
| Number | % | ||
|---|---|---|---|
| Sex | Male | 27 | 57 |
| Female | 20 | 43 | |
| BRAF status | Mutated | 26 | 55 |
| Wild-type | 21 | 45 | |
| LDH at BM diagnosis | ≤2 × ULN | 31 | 67 |
| >2 × ULN | 10 | 21 | |
| Unknown | 6 | 12 | |
| Site of BMs | Supra-tentorial | 27 | 57 |
| Infra-tentorial | 1 | 2 | |
| Supra- and infra-tentorial | 8 | 17 | |
| Unknown | 11 | 24 | |
| Number of BMs | ≤3 | 25 | 53 |
| >3 | 22 | 47 | |
| Steroid therapy | Yes | 47 | 100 |
| No | 0 | 0 |
| Factors | Effect Tested | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||
| Sex | Male vs. female | 0.79 | 0.51–1.25 | 0.3161 | 0.92 | 0.54–0.57 | 0.7624 |
| Age (years) | 56–65 vs. ≤55 | 2.03 | 1.11–3.71 | 0.0215 | 1.68 | 0.88–3.22 | 0.1174 |
| 66–75 vs. ≤55 | 1.59 | 0.86–2.92 | 0.1373 | 1.55 | 0.78–3.06 | 0.2070 | |
| >75 vs. ≤55 | 2.28 | 1.1–4.7 | 0.0264 | 1.97 | 0.86–4.49 | 0.1080 | |
| Radiotherapy | Yes vs. no | 0.3 | 0.18–0.49 | <0.0001 | 0.37 | 0.21–0.67 | 0.0009 |
| Neurological symptoms | Yes vs. no | 1.6 | 1.03–2.49 | 0.0374 | 1.20 | 0.71–2.01 | 0.5020 |
| Number of BM | ≥3 vs. <3 | 1.45 | 0.93–2.28 | 0.571 | 1.78 | 1.04–3.06 | 0.0363 |
| Liver metastasis | Yes vs. no | 1.44 | 0.89–2.34 | 0.1375 | 1.05 | 0.59–1.85 | 0.8763 |
| LDH levels > 2 times the ULN | Yes vs. no | 2.58 | 1.41–4.74 | 0.0021 | 1.85 | 0.96–3.56 | 0.0452 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Internò, V.; Sergi, M.C.; Metta, M.E.; Guida, M.; Trerotoli, P.; Strippoli, S.; Circelli, S.; Porta, C.; Tucci, M. Melanoma Brain Metastases: A Retrospective Analysis of Prognostic Factors and Efficacy of Multimodal Therapies. Cancers 2023, 15, 1542. https://doi.org/10.3390/cancers15051542
Internò V, Sergi MC, Metta ME, Guida M, Trerotoli P, Strippoli S, Circelli S, Porta C, Tucci M. Melanoma Brain Metastases: A Retrospective Analysis of Prognostic Factors and Efficacy of Multimodal Therapies. Cancers. 2023; 15(5):1542. https://doi.org/10.3390/cancers15051542
Chicago/Turabian StyleInternò, Valeria, Maria Chiara Sergi, Maria Elvira Metta, Michele Guida, Paolo Trerotoli, Sabino Strippoli, Salvatore Circelli, Camillo Porta, and Marco Tucci. 2023. "Melanoma Brain Metastases: A Retrospective Analysis of Prognostic Factors and Efficacy of Multimodal Therapies" Cancers 15, no. 5: 1542. https://doi.org/10.3390/cancers15051542
APA StyleInternò, V., Sergi, M. C., Metta, M. E., Guida, M., Trerotoli, P., Strippoli, S., Circelli, S., Porta, C., & Tucci, M. (2023). Melanoma Brain Metastases: A Retrospective Analysis of Prognostic Factors and Efficacy of Multimodal Therapies. Cancers, 15(5), 1542. https://doi.org/10.3390/cancers15051542






