Urine CA125 and HE4 for the Detection of Ovarian Cancer in Symptomatic Women
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Laboratory Assay Testing
2.3. Statistical Analysis
3. Results
3.1. Population Characteristics
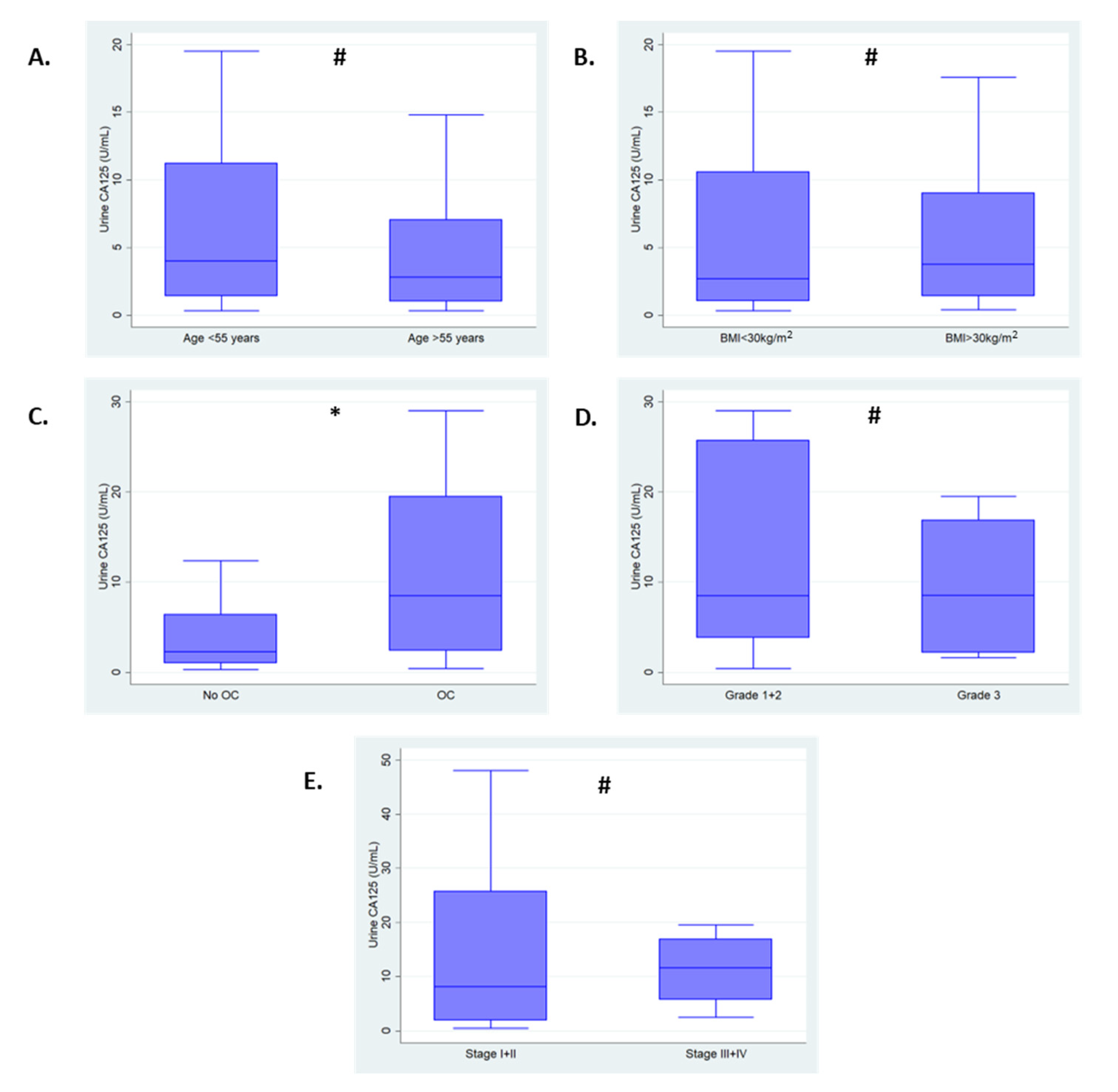
3.2. Summary of Urine CA125 Levels
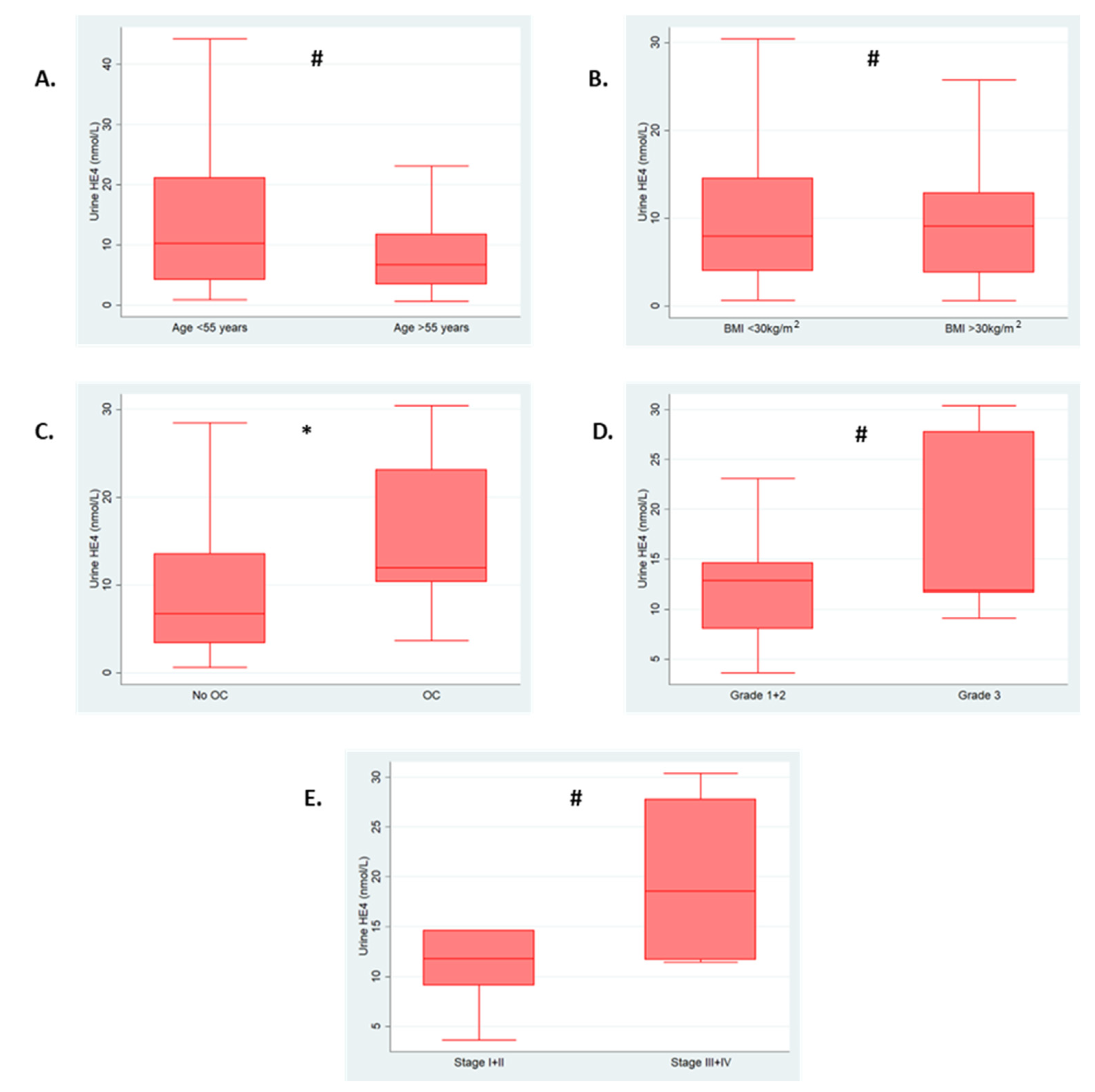
3.3. Summary of Urine HE4 Levels
3.4. Summary of Serum CA125 and HE4
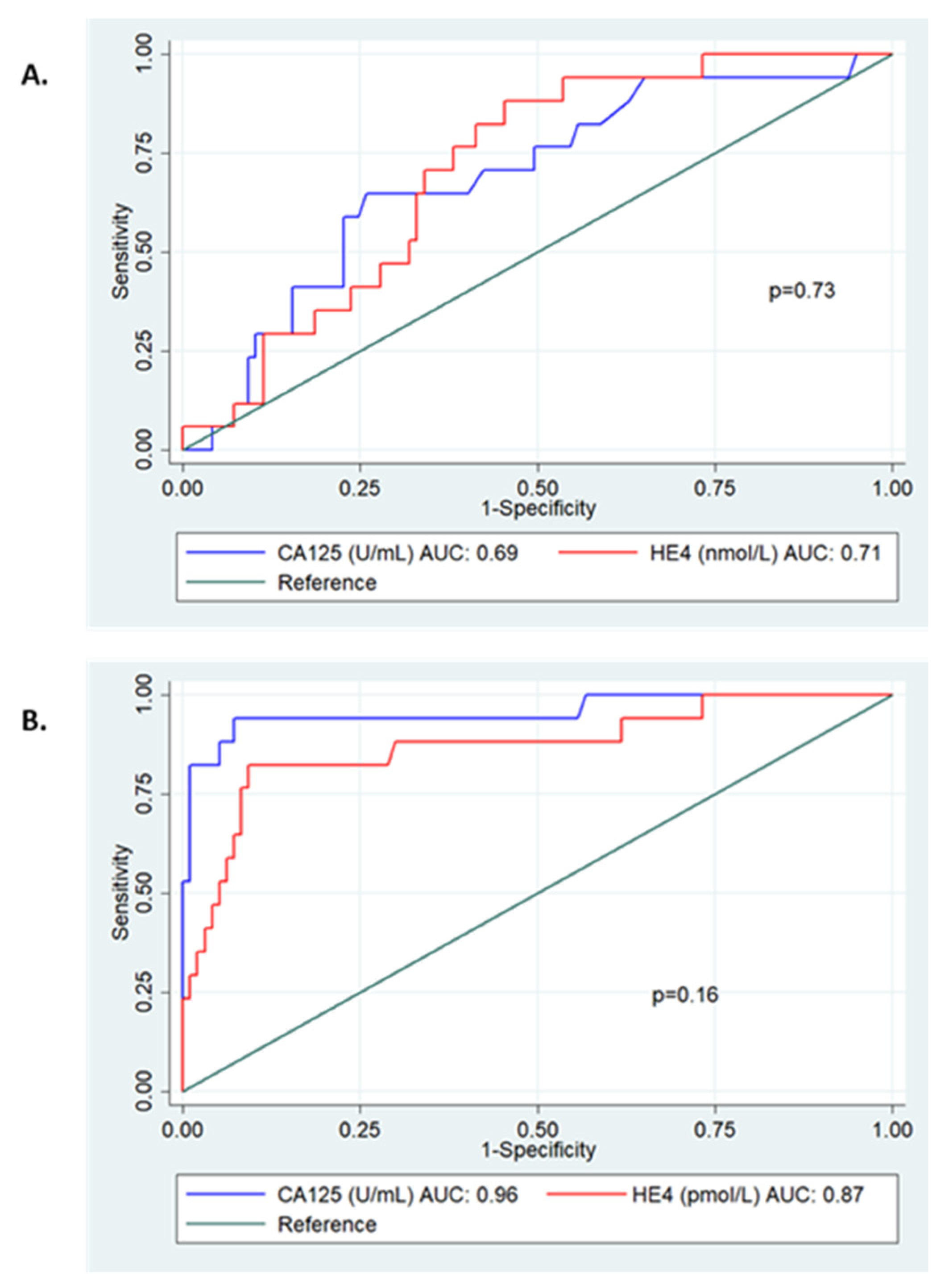
3.5. Diagnostic Accuracy of Urine CA125 and HE4
4. Discussion
4.1. Main Finding
4.2. Strengths and Limitations
4.3. Comparison with the Current Literature
4.4. Clinical and Research Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cancer Research UK (CRUK). Ovarian Cancer Mortality. Available online: https://cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer (accessed on 11 May 2022).
- Reid, B.M.; Permuth, J.B.; Sellers, T.A. Epidemiology of ovarian cancer: A review. Cancer Biol. Med. 2017, 14, 9–32. [Google Scholar] [PubMed]
- Cancer Research UK (CRUK). Ovarian Cancer Survival. Available online: https://cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer/survival#heading-three (accessed on 11 May 2022).
- Gilbert, L.; Basso, O.; Sampalis, J.; Karp, I.; Martins, C.; Feng, J.; Piedimonte, S.; Quintal, L.; Ramanakumar, A.V.; Takefman, J.; et al. Assessment of symptomatic women for early diagnosis of ovarian cancer: Results from the prospective DOvE pilot project. Lancet Oncol. 2012, 13, 285–291. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health and Care Excellence (NICE). Ovarian Cancer: Recognition and Initial Management Clinical Guideline 122. Available online: https://www.nice.org.uk/Guidance/CG1222011 (accessed on 11 May 2022).
- Goff, B.; Mandel, L.; Muntz, H.G.; Melancon, C.H. Ovarian carcinoma diagnosis. Cancer 2000, 89, 2068–2075. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Ziebland, S.; McPherson, A. Minimizing delays in ovarian cancer diagnosis: An expansion of Andersen’s model of ‘total patient delay’. Fam Pract. 2007, 24, 48–55. [Google Scholar] [CrossRef]
- Duffy, M.; Bonfrer, J.; Kulpa, J.; Rustin, G.; Söletormos, G.; Torre, G.; Tuxen, M.; Zwirner, M. CA125 in ovarian cancer: European Group on Tumor Markers guidelines for clinical use. Int. J. Gynecol. Cancer 2005, 15, 679–691. [Google Scholar] [CrossRef]
- Barr, C.E.; Funston, G.; Jeevan, D.; Sundar, S.; Mounce, L.T.A.; Crosbie, E.J. The Performance of HE4 Alone and in Combination with CA125 for the Detection of Ovarian Cancer in an Enriched Primary Care Population. Cancers 2022, 14, 2124. [Google Scholar] [CrossRef]
- Dayyani, F.; Uhlig, S.; Colson, B.; Simon, K.; Rolny, V.; Morgenstern, D.; Schlumbrecht, M. Diagnostic Performance of Risk of Ovarian Malignancy Algorithm Against CA125 and HE4 in Connection With Ovarian Cancer: A Meta-analysis. Int. J. Gynecol. Cancer 2016, 26, 1586–1593. [Google Scholar] [CrossRef]
- Scaletta, G.; Plotti, F.; Luvero, D.; Capriglione, S.; Montera, R.; Miranda, A.; Lopez, S.; Terranova, C.; Nardone, C.D.C.; Angioli, R. The role of novel biomarker HE4 in the diagnosis, prognosis and follow-up of ovarian cancer: A systematic review. Expert Rev. Anticancer. Ther. 2017, 17, 827–839. [Google Scholar] [CrossRef]
- Jing, J.; Gao, Y. Urine biomarkers in the early stages of diseases: Current status and perspective. Discov. Med. 2018, 25, 57–65. [Google Scholar]
- Liao, J.B.; Yip, Y.Y.; Swisher, E.M.; Agnew, K.; Hellstrom, K.E.; Hellstrom, I. Detection of the HE4 protein in urine as a biomarker for ovarian neoplasms: Clinical correlates. Gynecol. Oncol. 2015, 137, 430–435. [Google Scholar] [CrossRef]
- Moore, R.G.; Brown, A.K.; Miller, M.C.; Skates, S.; Allard, W.J.; Verch, T.; Steinhoff, M.; Messerlian, G.; DiSilvestro, P.; Granai, C.; et al. The use of multiple novel tumor biomarkers for the detection of ovarian carcinoma in patients with a pelvic mass. Gynecol. Oncol. 2008, 108, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Jia, M.-M.; Deng, J.; Cheng, X.-L.; Yan, Z.; Li, Q.-C.; Xing, Y.-Y.; Fan, D.-M.; Tian, X.-Y. Diagnostic accuracy of urine HE4 in patients with ovarian cancer: A meta-analysis. Oncotarget 2017, 8, 9660–9671. [Google Scholar] [CrossRef] [PubMed]
- Fotopoulou, C.; Hall, M.; Cruickshank, D.; Gabra, H.; Ganesan, R.; Hughes, C.; Kehoe, S.; Ledermann, J.; Morrison, J.; Naik, R.; et al. British Gynaecological Cancer Society (BGCS) epithelial ovarian/fallopian tube/primary peritoneal cancer guidelines: Recommendations for practice. Eur. J. Obs. Gynecol. Reprod. Biol. 2017, 213, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Liu, X. Classification accuracy and cut point selection. Stat. Med. 2012, 31, 2676–2686. [Google Scholar] [CrossRef] [PubMed]
- Barr, C.E.; Funston, G.; Mounce, L.T.A.; Pemberton, P.W.; Howe, J.D.; Crosbie, E.J. Comparison of two immunoassays for the meas-urement of serum HE4 for ovarian cancer. Pract. Lab Med. 2021, 26, e00235. [Google Scholar]
- Davenport, C.F.; Rai, N.; Sharma, P.; Deeks, J.; Berhane, S.; Mallett, S.; Saha, P.; Solanki, R.; Bayliss, S.; Snell, K.; et al. Diagnostic Models Combining Clinical Information, Ultrasound and Biochemical Markers for Ovarian Cancer: Cochrane Systematic Review and Meta-Analysis. Cancers 2022, 14, 3621. [Google Scholar] [CrossRef]
- Rai, N.; Nevin, J.; Downey, G.; Abedin, P.; Balogun, M.; Kehoe, S.; Sundar, S. Outcomes following implementation of symptom triggered diagnostic testing for ovarian cancer. Eur. J. Obs. Gynecol. Reprod. Biol. 2015, 187, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Usher-Smith, J.A.; Sharp, S.J.; Griffin, S.J. The spectrum effect in tests for risk prediction, screening, and diagnosis. BMJ 2016, 353, i3139. [Google Scholar] [CrossRef]
- Tay, S.K.; Chua, E.K. Correlation of serum, urinary and salivary CA 125 levels in patients with adnexal masses. Ann. Acad. Med. Singap. 1994, 23, 311–314. [Google Scholar]
- Sandow, J.J.; Rainczuk, A.; Infusini, G.; Makanji, M.; Bilandzic, M.; Wilson, A.L.; Fairweather, N.; Stanton, P.G.; Garama, D.; Gough, D.; et al. Discovery and Validation of Novel Protein Biomarkers in Ovarian Cancer Patient Urine. Proteom. Clin. Appl. 2018, 12, 1700135. [Google Scholar] [CrossRef]
- Lee, S.-W.; Lee, H.-Y.; Bang, H.J.; Song, H.-J.; Kong, S.W.; Kim, Y.-M. An Improved Prediction Model for Ovarian Cancer Using Urinary Biomarkers and a Novel Validation Strategy. Int. J. Mol. Sci. 2019, 20, 4938. [Google Scholar] [CrossRef] [PubMed]
- Owens, G.L.; E Barr, C.; White, H.; Njoku, K.; Crosbie, E.J. Urinary biomarkers for the detection of ovarian cancer: A systematic review. Carcinogenesis 2022, 43, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Steenbeek, M.P.; Harmsen, M.G.; Hoogerbrugge, N.; De Jong, M.A.; Maas, A.H.; Prins, J.B.; Bulten, J.; Teerenstra, S.; van Bommel, M.H.D.; van Doorn, H.C.; et al. Association of Salpingectomy With Delayed Oophorectomy Versus Salpingo-oophorectomy With Quality of Life in BRCA1/2 Pathogenic Variant Carriers: A Nonrandomized Controlled Trial. Jama Oncol. 2021, 7, 1203–1212. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, A.N.; Fraser, L.S.M.; Philpott, S.; Manchanda, R.; Burnell, M.; Badman, P.; Hadwin, R.; Rizzuto, I.; Benjamin, E.; Singh, N.; et al. Evidence of Stage Shift in Women Diagnosed With Ovarian Cancer During Phase II of the United Kingdom Familial Ovarian Cancer Screening Study. Obs. Gynecol. Surv. 2017, 72, 338–340. [Google Scholar] [CrossRef]
- A Trial Using Novel Markers to Predict Malignancy in Elevated-Risk Women. Available online: https://clinicaltrials.gov/ct2/show/NCT01121640 (accessed on 22 September 2022).
- Badrick, E.; Cresswell, K.; Ellis, P.; Detecting Cancer Early Priority Setting Partnership Steering Group (Appendix); Renehan, A.G.; Crosbie, E.J. Top ten research priorities for detecting cancer early. Lancet Public Health 2019, 4, e551. [Google Scholar] [CrossRef]
- Chornokur, G.; Amankwah, E.K.; Schildkraut, J.M.; Phelan, C.M. Global ovarian cancer health disparities. Gynecol. Oncol. 2013, 129, 258–264. [Google Scholar] [CrossRef]
- Goss, E.; Lopez, A.M.; Brown, C.L.; Wollins, D.S.; Brawley, O.W.; Raghavan, D. American Society of Clinical Oncology Policy Statement: Disparities in Cancer Care. J. Clin. Oncol. 2009, 27, 2881–2885. [Google Scholar] [CrossRef]
- Morris, C.R.; Sands, M.T.; Smith, L.H. Ovarian cancer: Predictors of early-stage diagnosis. Cancer Causes Control. 2010, 21, 1203–1211. [Google Scholar] [CrossRef]
- Pepe, M.S.; Janes, H.; Li, C.I.; Bossuyt, P.M.; Feng, Z.; Hilden, J. Early-Phase Studies of Biomarkers: What Target Sensitivity and Specificity Values Might Confer Clinical Utility? Clin. Chem. 2016, 62, 737–742. [Google Scholar] [CrossRef]
- Ferraro, S.; Borille, S.; Carnevale, A.; Frusciante, E.; Bassani, N.; Panteghini, M. Verification of the harmonization of human epi-didymis protein 4 assays. Clin. Chem. Lab. Med. 2016, 54, 1635–1643. [Google Scholar] [CrossRef]
- Bingle, L.; Singleton, V.; Bingle, C.D. The putative ovarian tumour marker gene HE4 (WFDC2), is expressed in normal tissues and undergoes complex alternative splicing to yield multiple protein isoforms. Oncogene 2002, 21, 2768–2773. [Google Scholar] [CrossRef] [PubMed]
- Hellstrom, I.; Yip, Y.Y.; Darvas, M.; Swisher, E.; Hellstrom, K.E. Ovarian carcinomas express HE4 epitopes independently of each other. Cancer Treat. Res. Commun. 2019, 21, 100152. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Number (%) |
|---|---|
| a. OC, n = 17 (15%) | |
| Age (years) | |
| Median (IQR) | 58 (52–68) |
| BMI (kg/m2) | |
| Median (IQR) | 29 (24–31) |
| Histological subtype (n,%) | |
| Serous | 6 (35) |
| Mucinous | 4 (24) |
| Endometrioid | 4 (24) |
| Clear Cell | 2 (12) |
| Carcinosarcoma | 0 (0) |
| Mixed | 1 (6) |
| Grade (n,%) | |
| 1 | 6 (35) |
| 2 | 3 (18) |
| 3 | 8 (47) |
| FIGO Stage (n,%) | |
| I | 10 (59) |
| II | 3 (18) |
| III | 3 (18) |
| IV | 1 (5) |
| Complete cytoreduction (n,%) | |
| Yes | 13 (76) |
| No | 2 (12) |
| Missing | 2 (12) |
| Adjuvant Therapy (n,%) | |
| No | 4 (23) |
| Yes | 10 (59) |
| Unknown | 3 (18) |
| b. No OC, n = 97 (85%) | |
| Age (years) | |
| Median (IQR) | 54 (51–58) |
| BMI (kg/m2) | |
| Median (IQR) | 27 (24–33) |
| Final diagnosis | |
| No demonstrable pathology | 46 (47) |
| Benign | 51 (53) |
| Atrophy | 13 (25) |
| Simple cyst | 1 (2) |
| Serous cystadenoma | 5 (10) |
| Mucinous cystadenoma | 2 (4) |
| Fibroma | 1 (2) |
| Dermoid | 1 (2) |
| Angioleiomayata | 1 (2) |
| Other benign cyst | 2 (4) |
| Fibroid | 9 (19) |
| Endo-cervical polyp | 14 (28) |
| Prolapse | 1 (2) |
| No OC, n (%) | OC, n (%) | p-Value | |
|---|---|---|---|
| Urine CA125 (U/mL) | |||
| <6.2 | 72 (74) | 6 (35) | 0.001 |
| ≥6.2 | 25 (26) | 11 (65) | |
| Urine HE4 (nmol/L) | |||
| <9.1 | 57 (59) | 5 (29) | 0.03 |
| ≥9.1 | 40 (41) | 12 (71) | |
| Urine Combined | |||
| Negative | 44 (45) | 3 (18) | 0.03 |
| Positive * | 53 (55) | 14 (82) | |
| Serum CA125 (U/mL) | |||
| <35 | 91 (94) | 2 (12) | <0.001 |
| ≥35 | 6 (6) | 15 (88) | |
| Serum HE4 (pmol/L) | 0.002 | ||
| <77 | 51 (53) | 2 (12) | |
| ≥77 | 46 (47) | 15 (88) |
| Biomarker | Sensitivity, % (95%CI) | Specificity, % (95%CI) | PPV, % (95%CI) | NPV, % (95%CI) | Positive LR, % (95%CI) | Negative LR, % (95%CI) |
|---|---|---|---|---|---|---|
| Urine CA125 (≥6.2 U/mL) | 64.7 (38.2–85.8) | 74.2 (64.3–82.6) | 30.6 (16.3–48.1) | 92.3 (84.0–97.1) | 2.51 (1.54–4.09) | 0.48 (0.25–0.92) |
| Urine HE4 (≥9.1 nmol/L) | 70.6 (44.0–89.7) | 58.8 (48.3–68.7) | 23.1 (12.5–36.8) | 91.9 (82.2–97.3) | 1.71 (1.16–2.52) | 0.50 (0.24–1.06) |
| Urine Combined * | 82.4 (56.6–96.2) | 40.2 (30.4–50.7) | 19.4 (11.1–30.5) | 92.9 (80.5–98.5) | 1.51 (1.13–2.00) | 0.39 (0.14–1.11) |
| Serum CA125 (≥35 U/mL) | 88.2 (63.6–98.5) | 93.8 (87.0–97.7) | 71.4 (47.8–88.7) | 97.8 (92.4–99.7) | 14.3 (6.45–31.6) | 0.13 (0.03–0.46) |
| Serum HE4 (≥77 pmol/L) | 88.2 (63.6–98.5) | 52.6 (42.2–62.8) | 24.6 (14.5–37.3) | 96.2 (87.0–99.5) | 1.86 (1.42–2.44) | 0.22 (0.06–0.83) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barr, C.E.; Njoku, K.; Owens, G.L.; Crosbie, E.J. Urine CA125 and HE4 for the Detection of Ovarian Cancer in Symptomatic Women. Cancers 2023, 15, 1256. https://doi.org/10.3390/cancers15041256
Barr CE, Njoku K, Owens GL, Crosbie EJ. Urine CA125 and HE4 for the Detection of Ovarian Cancer in Symptomatic Women. Cancers. 2023; 15(4):1256. https://doi.org/10.3390/cancers15041256
Chicago/Turabian StyleBarr, Chloe E., Kelechi Njoku, Gemma L. Owens, and Emma J. Crosbie. 2023. "Urine CA125 and HE4 for the Detection of Ovarian Cancer in Symptomatic Women" Cancers 15, no. 4: 1256. https://doi.org/10.3390/cancers15041256
APA StyleBarr, C. E., Njoku, K., Owens, G. L., & Crosbie, E. J. (2023). Urine CA125 and HE4 for the Detection of Ovarian Cancer in Symptomatic Women. Cancers, 15(4), 1256. https://doi.org/10.3390/cancers15041256






