Robot-Assisted Radical Prostatectomy by Lateral Approach: Technique, Reproducibility and Outcomes
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
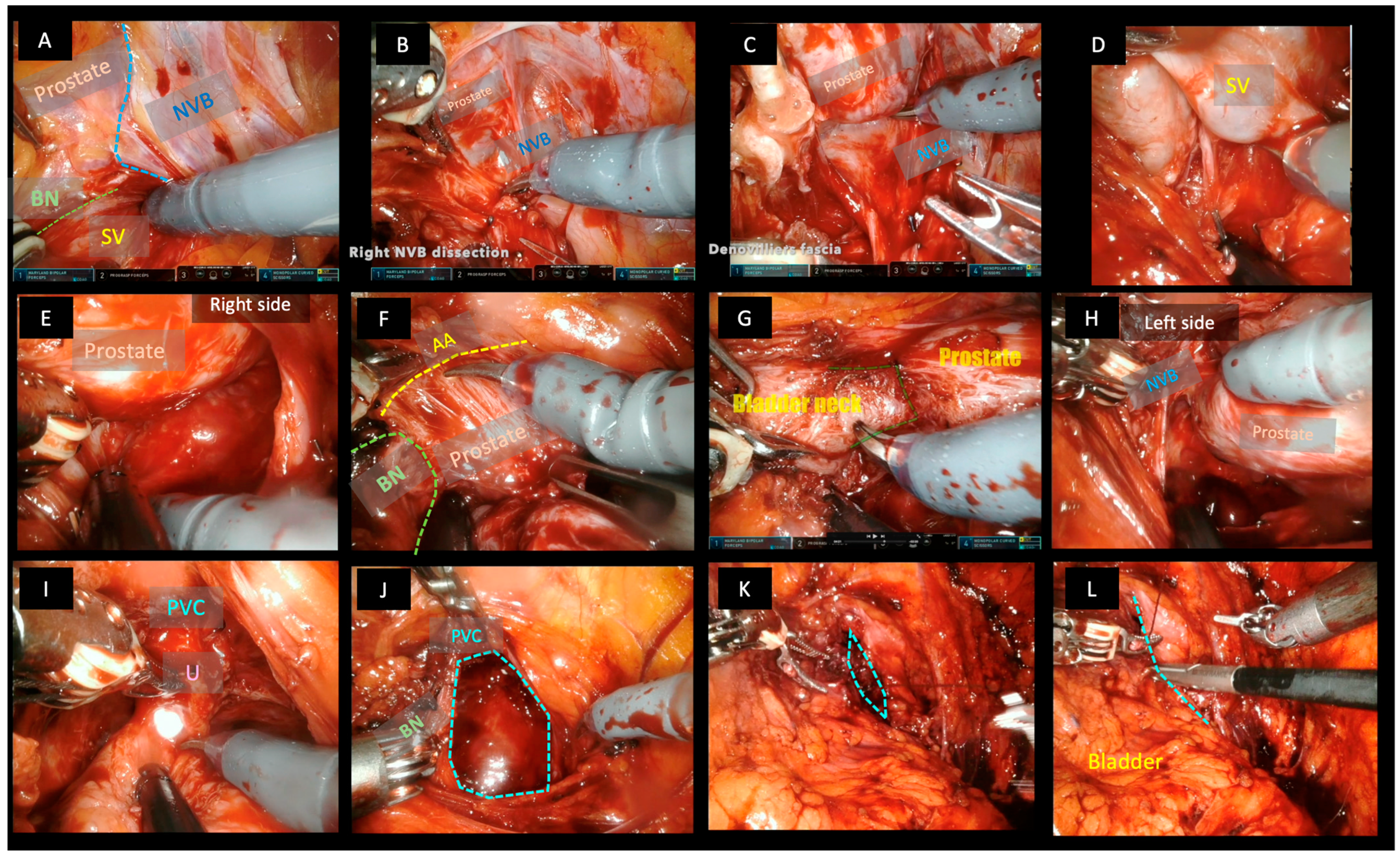
2.1. Surgical Technique
2.2. Postoperative Management and Follow-Up
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martini, A.; Falagario, U.G.; Villers, A.; Dell’oglio, P.; Mazzone, E.; Autorino, R.; Moschovas, M.C.; Buscarini, M.; Bravi, C.A.; Briganti, A.; et al. Contemporary Techniques of Prostate Dissection for Robot-assisted Prostatectomy. Eur. Urol. 2020, 78, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, V.; Reimold, P.; Goertz, M.; Hofer, L.; Dieffenbacher, S.; Nyarangi-Dix, J.; Duensing, S.; Hohenfellner, M.; Hatiboglu, G. Evolution of Salvage Radical Prostatectomy from Open to Robotic and Further to Retzius Sparing Surgery. J. Clin. Med. 2021, 11, 202. [Google Scholar] [CrossRef] [PubMed]
- Cochetti, G.; Del Zingaro, M.; Ciarletti, S.; Paladini, A.; Felici, G.; Stivalini, D.; Cellini, V.; Mearini, E. New Evolution of Robotic Radical Prostatectomy: A Single Center Experience with PERUSIA Technique. Appl. Sci. 2021, 11, 1513. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Annino, F.; D’Orazio, A.; Pereira, C.F.T.; Mugnier, C.; Hoepffner, J.-L.; Piechaud, T.; Gaston, R. Complete Periprostatic Anatomy Preservation During Robot-Assisted Laparoscopic Radical Prostatectomy (RALP): The New Pubovesical Complex-Sparing Technique. Eur. Urol. 2010, 58, 407–417. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Montes, V.E.C.; Gaston, R. Robot-Assisted Laparoscopic Radical Prostatectomy with Intrafascial Dissection of the Neurovascular Bundles and Preservation of the Pubovesical Complex: A Step-By-Step Description of the Technique. J. Endourol. 2012, 26, 1578–1585. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Miano, R.; Galfano, A.; Bocciardi, A.M.; Vespasiani, G.; Spera, E.; Gaston, R. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: Critical appraisal of the anatomic landmarks for a complete intrafascial approach: Retzius-Sparing Robot-Assisted Laparoscopic Radical Prostatectomy. Clin. Anat. 2015, 28, 896–902. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Annino, F.; Colalillo, G.; Gaston, R.; Piechaud, T.; Mauriello, A.; Anceschi, U.; Borri, F. “Urethral-Sparing” Robotic Radical Prostatectomy: Critical Appraisal of the Safety of the Technique Based on the Histologic Characteristics of the Prostatic Urethra. Curr. Oncol. 2023, 30, 1065–1076. [Google Scholar] [CrossRef]
- Oderda, M.; Calleris, G.; D’agate, D.; Falcone, M.; Faletti, R.; Gatti, M.; Marra, G.; Marquis, A.; Gontero, P. Intraoperative 3D-US-mpMRI Elastic Fusion Imaging-Guided Robotic Radical Prostatectomy: A Pilot Study. Curr. Oncol. 2022, 30, 110–117. [Google Scholar] [CrossRef]
- Socarrás, M.E.R.; Rivas, J.G.; Rivera, V.C.; Elbers, J.R.; González, L.L.; Mercado, I.M.; del Alamo, J.F.; del Dago, P.J.; Sancha, F.G. Prostate Mapping for Cancer Diagnosis: The Madrid Protocol. Transperineal Prostate Biopsies Using Multiparametric Magnetic Resonance Imaging Fusion and Micro-Ultrasound Guided Biopsies. J. Urol. 2020, 204, 726–733. [Google Scholar] [CrossRef]
- Bravi, C.A.; Tin, A.; Vertosick, E.; Mazzone, E.; Martini, A.; Dell’Oglio, P.; Stabile, A.; Gandaglia, G.; Fossati, N.; Suardi, N.; et al. The Impact of Experience on the Risk of Surgical Margins and Biochemical Recurrence after Robot-Assisted Radical Prostatectomy: A Learning Curve Study. J. Urol. 2019, 202, 108–113. [Google Scholar] [CrossRef]
- Gandi, C.; Totaro, A.; Bientinesi, R.; Marino, F.; Pierconti, F.; Martini, M.; Russo, A.; Racioppi, M.; Bassi, P.; Sacco, E. A multi-surgeon learning curve analysis of overall and site-specific positive surgical margins after RARP and implications for training. J. Robot. Surg. 2022, 16, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- Esperto, F.; Cacciatore, L.; Tedesco, F.; Testa, A.; Callè, P.; Ragusa, A.; Deanesi, N.; Minore, A.; Prata, F.; Brassetti, A.; et al. Impact of Robotic Technologies on Prostate Cancer Patients’ Choice for Radical Treatment. J. Pers. Med. 2023, 13, 794. [Google Scholar] [CrossRef] [PubMed]
- Carbonell, E.; Matheu, R.; Muní, M.; Sureda, J.; García-Sorroche, M.; Ribal, M.J.; Alcaraz, A.; Vilaseca, A. The Effect of Adverse Surgical Margins on the Risk of Biochemical Recurrence after Robotic-Assisted Radical Prostatectomy. Biomedicines 2022, 10, 1911. [Google Scholar] [CrossRef] [PubMed]
- Luan, Y.; Ding, X.-F.; Lu, S.-M.; Huang, T.-B.; Chen, J.; Xiao, Q.; Wang, L.-P.; Chen, H.-P.; Han, Y.-X. The Efficacy of Urinary Continence in Patients Undergoing Robot-Assisted Radical Prostatectomy with Bladder-Prostatic Muscle Reconstruction and Bladder Neck Eversion Anastomosis. Medicina 2022, 58, 1821. [Google Scholar] [CrossRef]
- Checcucci, E.; Veccia, A.; Fiori, C.; Amparore, D.; Manfredi, M.; Di Dio, M.; Morra, I.; Galfano, A.; Autorino, R.; Bocciardi, A.M.; et al. Retzius-sparing robot-assisted radical prostatectomy vs the standard approach: A systematic review and analysis of comparative outcomes. BJU Int. 2020, 125, 8–16. [Google Scholar] [CrossRef]
- Shikanov, S.; Song, J.; Royce, C.; Al-Ahmadie, H.; Zorn, K.; Steinberg, G.; Zagaja, G.; Shalhav, A.; Eggener, S. Length of Positive Surgical Margin After Radical Prostatectomy as a Predictor of Biochemical Recurrence. J. Urol. 2009, 182, 139–144. [Google Scholar] [CrossRef]
- John, A.; Lim, A.; Catterwell, R.; Selth, L.; O’callaghan, M. Length of positive surgical margins after radical prostatectomy: Does size matter?—A systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2023, 1–8. [Google Scholar] [CrossRef]
- Gacci, M.; De Nunzio, C.; Sakalis, V.; Rieken, M.; Cornu, J.-N.; Gravas, S. Latest Evidence on Post-Prostatectomy Urinary Incontinence. J. Clin. Med. 2023, 12, 1190. [Google Scholar] [CrossRef]
- Eichelberg, C.; Erbersdobler, A.; Michl, U.; Schlomm, T.; Salomon, G.; Graefen, M.; Huland, H. Nerve Distribution along the Prostatic Capsule. Eur. Urol. 2007, 51, 105–111. [Google Scholar] [CrossRef]
- Galfano, A.; Di Trapani, D.; Sozzi, F.; Strada, E.; Petralia, G.; Bramerio, M.; Ascione, A.; Gambacorta, M.; Bocciardi, A.M. Beyond the Learning Curve of the Retzius-sparing Approach for Robot-assisted Laparoscopic Radical Prostatectomy: Oncologic and Functional Results of the First 200 Patients with ≥1 Year of Follow-up. Eur. Urol. 2013, 64, 974–980. [Google Scholar] [CrossRef]
- de Carvalho, P.A.; Barbosa, J.A.; Guglielmetti, G.B.; Cordeiro, M.D.; Rocco, B.; Nahas, W.C.; Patel, V.; Coelho, R.F. Retrograde Release of the Neurovascular Bundle with Preservation of Dorsal Venous Complex During Robot-assisted Radical Prostatectomy: Optimizing Functional Outcomes. Eur. Urol. 2020, 77, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Lambert, E.; Allaeys, C.; Berquin, C.; De Visschere, P.; Verbeke, S.; Vanneste, B.; Fonteyne, V.; Van Praet, C.; Lumen, N. Is It Safe to Switch from a Standard Anterior to Retzius-Sparing Approach in Robot-Assisted Radical Prostatectomy? Curr. Oncol. 2023, 30, 3447–3460. [Google Scholar] [CrossRef]
- Flammia, R.S.; Bologna, E.; Anceschi, U.; Tufano, A.; Licari, L.C.; Antonelli, L.; Proietti, F.; Alviani, F.; Gallucci, M.; Simone, G.; et al. “Single Knot–Single Running Suture” Vesicourethral Anastomosis with Posterior Musculofascial Reconstruction during Robot-Assisted Radical Prostatectomy: A Step-by-Step Guide of Surgical Technique. J. Pers. Med. 2023, 13, 1072. [Google Scholar] [CrossRef]
- Olivero, A.; Tappero, S.; Maltzman, O.; Vecchio, E.; Granelli, G.; Secco, S.; Caviglia, A.; Bocciardi, A.M.M.; Galfano, A.; Dell’oglio, P. Urinary Continence Recovery after Retzius-Sparing Robot Assisted Radical Prostatectomy and Adjuvant Radiation Therapy. Cancers 2023, 15, 4390. [Google Scholar] [CrossRef]
- Montorsi, F.; Gandaglia, G.; Würnschimmel, C.; Graefen, M.; Briganti, A.; Huland, H. Re: Paolo Afonso de Carvalho, Joāo ABA Barbosa, Giuliano B. Guglielmetti, et al. Retrograde Release of the Neurovascular Bundle with Preservation of Dorsal Venous Complex During Robot-assisted Radical Prostatectomy: Optimizing Functional Outcomes. Eur Urol 2020;77:628-35: Incredible Results for Robot-assisted Nerve-sparing Radical Prostatectomy in Prostate Cancer Patients. Eur. Urol. 2021, 79, e44–e46. [Google Scholar] [CrossRef]
- Yang, C.-H.; Chen, L.-H.; Lin, Y.-S.; Hsu, C.-Y.; Tung, M.-C.; Huang, S.-W.; Wu, C.-H.; Ou, Y.-C. Incorporating VR-RENDER Fusion Software in Robot-Assisted Partial Prostatectomy: The First Case Report. Curr. Oncol. 2023, 30, 1699–1707. [Google Scholar] [CrossRef] [PubMed]
- Rodler, S.; Kidess, M.A.; Westhofen, T.; Kowalewski, K.-F.; Belenchon, I.R.; Taratkin, M.; Puliatti, S.; Rivas, J.G.; Veccia, A.; Piazza, P.; et al. A Systematic Review of New Imaging Technologies for Robotic Prostatectomy: From Molecular Imaging to Augmented Reality. J. Clin. Med. 2023, 12, 5425. [Google Scholar] [CrossRef]
- Rud, E.; Baco, E.; Klotz, D.; Rennesund, K.; Svindland, A.; Berge, V.; Lundeby, E.; Wessel, N.; Hoff, J.-R.; Berg, R.E.; et al. Does Preoperative Magnetic Resonance Imaging Reduce the Rate of Positive Surgical Margins at Radical Prostatectomy in a Randomised Clinical Trial? Eur. Urol. 2015, 68, 487–496. [Google Scholar] [CrossRef]
- Kozikowski, M.; Malewski, W.; Michalak, W.; Dobruch, J. Clinical utility of MRI in the decision-making process before radical prostatectomy: Systematic review and meta-analysis. PLoS ONE 2019, 14, e0210194. [Google Scholar] [CrossRef]
- Kim, S.H.; Cho, S.H.; Kim, W.H.; Kim, H.J.; Park, J.M.; Kim, G.C.; Ryeom, H.K.; Yoon, Y.S.; Cha, J.G. Predictors of Extraprostatic Extension in Patients with Prostate Cancer. J. Clin. Med. 2023, 12, 5321. [Google Scholar] [CrossRef]
- Pedraza, A.M.; Parekh, S.; Joshi, H.; Grauer, R.; Wagaskar, V.; Zuluaga, L.; Gupta, R.; Barthe, F.; Nasri, J.; Pandav, K.; et al. Side-specific, Microultrasound-based Nomogram for the Prediction of Extracapsular Extension in Prostate Cancer. Eur. Urol. Open Sci. 2023, 48, 72–81. [Google Scholar] [CrossRef] [PubMed]
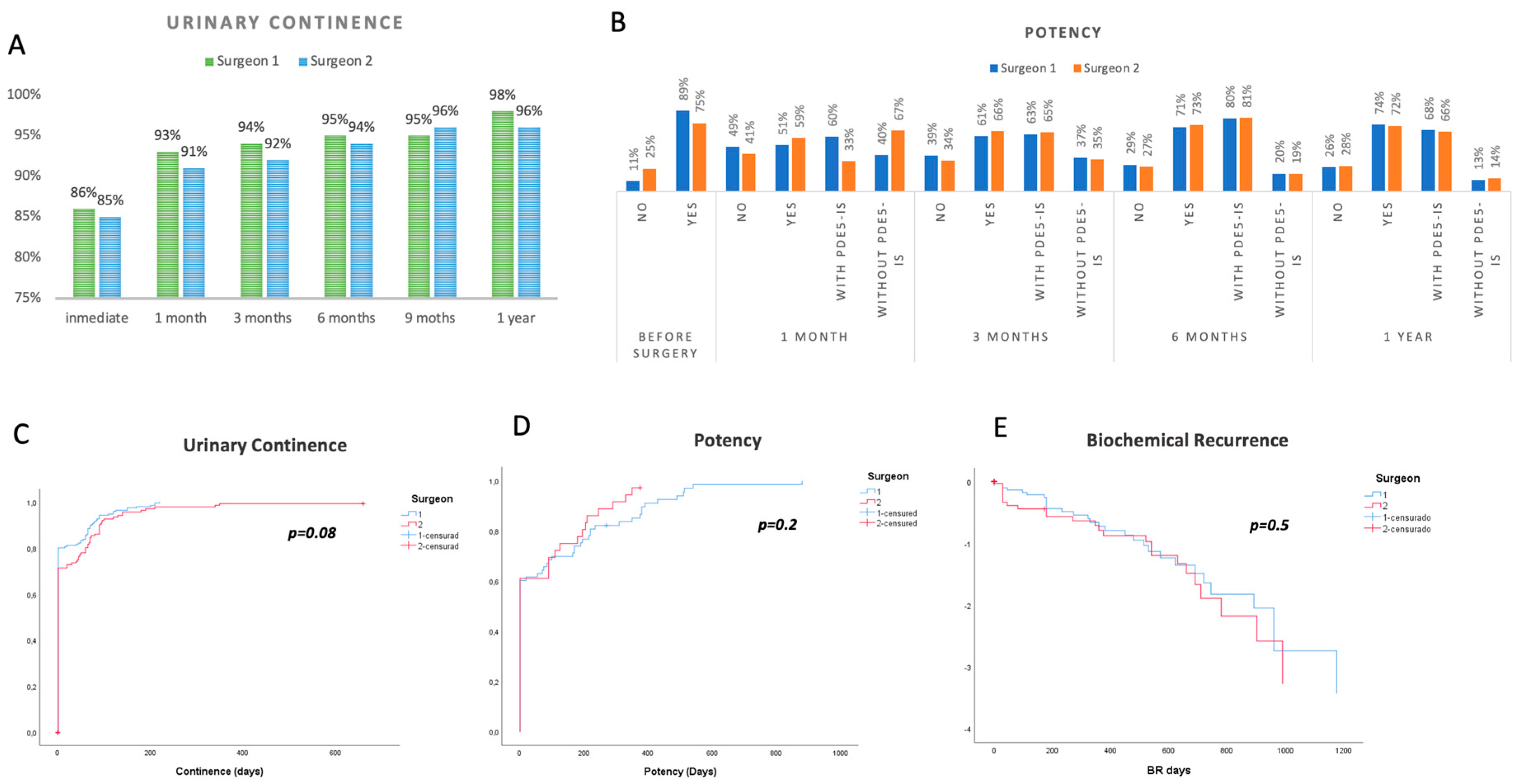
| Surgeon 1 (n = 289) | Surgeon 2 (n = 224) | p | |
|---|---|---|---|
| Baseline characteristics: | |||
| Age, mean ± SD, IQR | 62.12 ± 7.498 (56–68) | 63.23 ± 6.512 (58–64) | 0.84 |
| PSA ng/mL, ± SD, IQR | 7.98 ± 5.89 (5.01–8.21) | 7.41 ± 3.47 (5.00–8.21) | 0.283 |
| Prostate volume gr, ± SD, IQR | 42.30 ± 21.66 (28–50.5) | 47.27 ± 27.7 (28–50) | 0.077 |
| ED, n% | 11.10% | 25.00% | 0.001 |
| csPCa (ISUP ≥ 2), n% | 199 (69%) | 159 (71%) | 0.121 |
| TRUS /Fusion Bx/Mapeo (MRI + MicroUS) | 117/80/90 | 38/82/103 | <0.001 |
| Postoperative Outcomes: | |||
| Surgical Time min ± SD, IQR | 126.28 ± 36.652 | 180.56 ± 57.427 | <0.001 |
| Lateral approach, n% | 273 (94.5%) | 201 (90.5%) | 0.650 |
| Lymphadenectomy; Yes, n% | 117 (42.23%) | 73 (43.19%) | 0.84 |
| NVB preservation; No/Unilateral/Bilateral, n% | 25 (8.66%)/76 (26.35%)/188 (64.98%) | 32 (14.2%)/29 (13.01%)/163 (72.78%) | <0.001 |
| Intraoperative Bleeding ml ± SD, IQR | 266.08 ± 125.16 | 372.45 ± 135 mL | <0.001 |
| Conversion to open/laparoscopy, Yes/No, n% | 0 | 1 | - |
| Hospital stay days, mean ± SD(IQR) | 2.84 ± 0.744 (2–3) | 3.34 ± 1.022 (3–4) | 0.90 |
| Blood Transfusion, Yes/No, n% | 9 (3.11%) | 5 (2.23%) | 0.170 |
| csPCa (ISUP ≥ 2), n% | 271 (93.1%) | 207 (92.4%) | 0.681 |
| Extracapsular extension, n% | 62 (21.4%) | 61 (27.23%) | 0.273 |
| Positive lymp nodes, n% | 13 (4.49%) | 12 (4.9%) | 0.533 |
| PSM focal/significant, n%. | 95 (32.87%)/17 (5.88%) | 85 (37.9%)/17 (7.58%) | 0.262 |
| BR: Persistence/BR | 9 (3.11%)/34 (11.7%) | 8 (3.57%)/27 (12.05%) | 0.815 |
| Complications (Clavien III/IV), n%. | 11 (3.8%) | 5 (2.23%) | 0.763 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez Socarrás, M.; Gómez Rivas, J.; Reinoso Elbers, J.; Espósito, F.; Llanes Gonzalez, L.; Monsalve, D.M.C.; Fernandez Del Alamo, J.; Ruiz Graña, S.; Juarez Varela, J.; Coria, D.; et al. Robot-Assisted Radical Prostatectomy by Lateral Approach: Technique, Reproducibility and Outcomes. Cancers 2023, 15, 5442. https://doi.org/10.3390/cancers15225442
Rodríguez Socarrás M, Gómez Rivas J, Reinoso Elbers J, Espósito F, Llanes Gonzalez L, Monsalve DMC, Fernandez Del Alamo J, Ruiz Graña S, Juarez Varela J, Coria D, et al. Robot-Assisted Radical Prostatectomy by Lateral Approach: Technique, Reproducibility and Outcomes. Cancers. 2023; 15(22):5442. https://doi.org/10.3390/cancers15225442
Chicago/Turabian StyleRodríguez Socarrás, Moisés, Juan Gómez Rivas, Javier Reinoso Elbers, Fabio Espósito, Luis Llanes Gonzalez, Diego M. Carrion Monsalve, Julio Fernandez Del Alamo, Sonia Ruiz Graña, Jorge Juarez Varela, Daniel Coria, and et al. 2023. "Robot-Assisted Radical Prostatectomy by Lateral Approach: Technique, Reproducibility and Outcomes" Cancers 15, no. 22: 5442. https://doi.org/10.3390/cancers15225442
APA StyleRodríguez Socarrás, M., Gómez Rivas, J., Reinoso Elbers, J., Espósito, F., Llanes Gonzalez, L., Monsalve, D. M. C., Fernandez Del Alamo, J., Ruiz Graña, S., Juarez Varela, J., Coria, D., Cuadros Rivera, V., Gastón, R., & Gómez Sancha, F. (2023). Robot-Assisted Radical Prostatectomy by Lateral Approach: Technique, Reproducibility and Outcomes. Cancers, 15(22), 5442. https://doi.org/10.3390/cancers15225442






