Urethral Injury in Rectal Cancer Surgery: A Comprehensive Study Using Cadaveric Dissection, Imaging Analyses, and Clinical Series
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
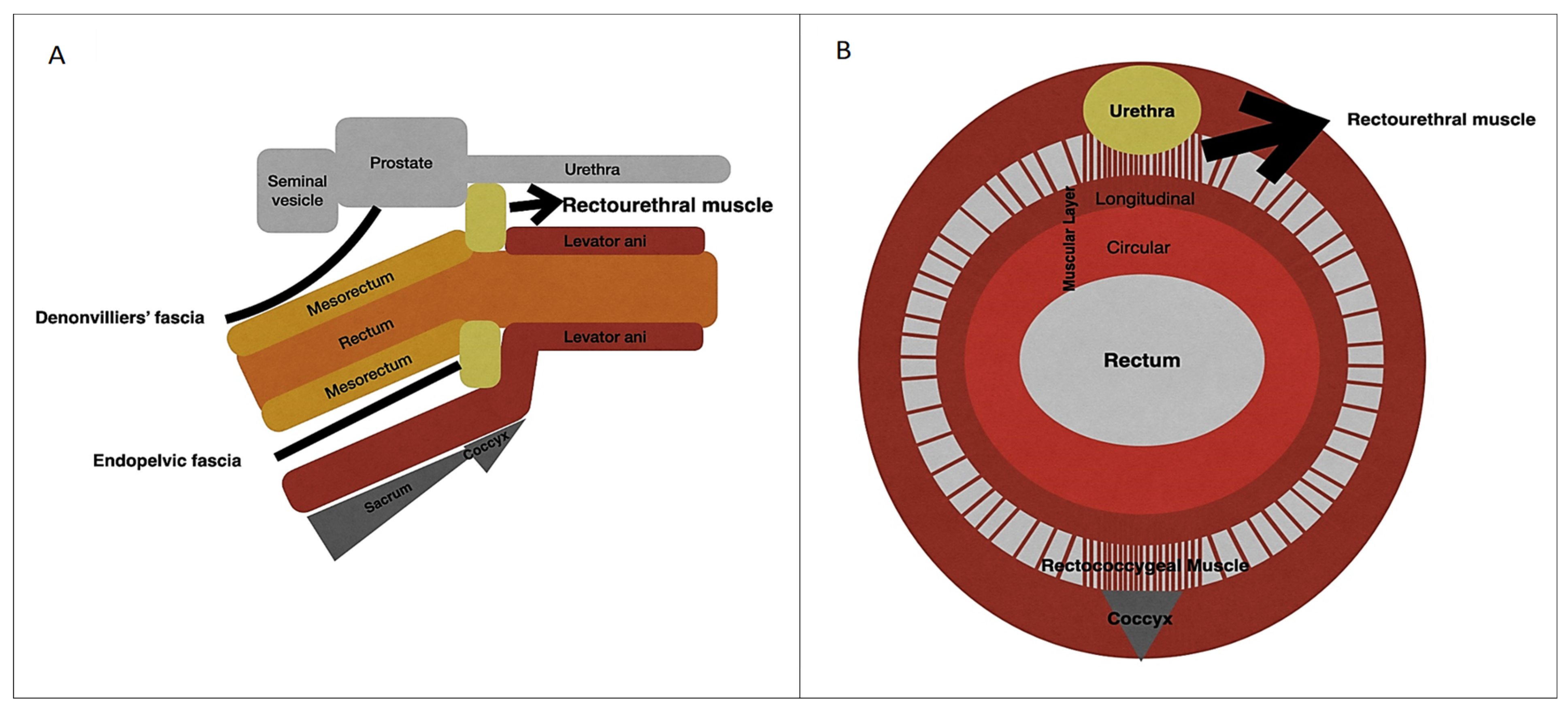
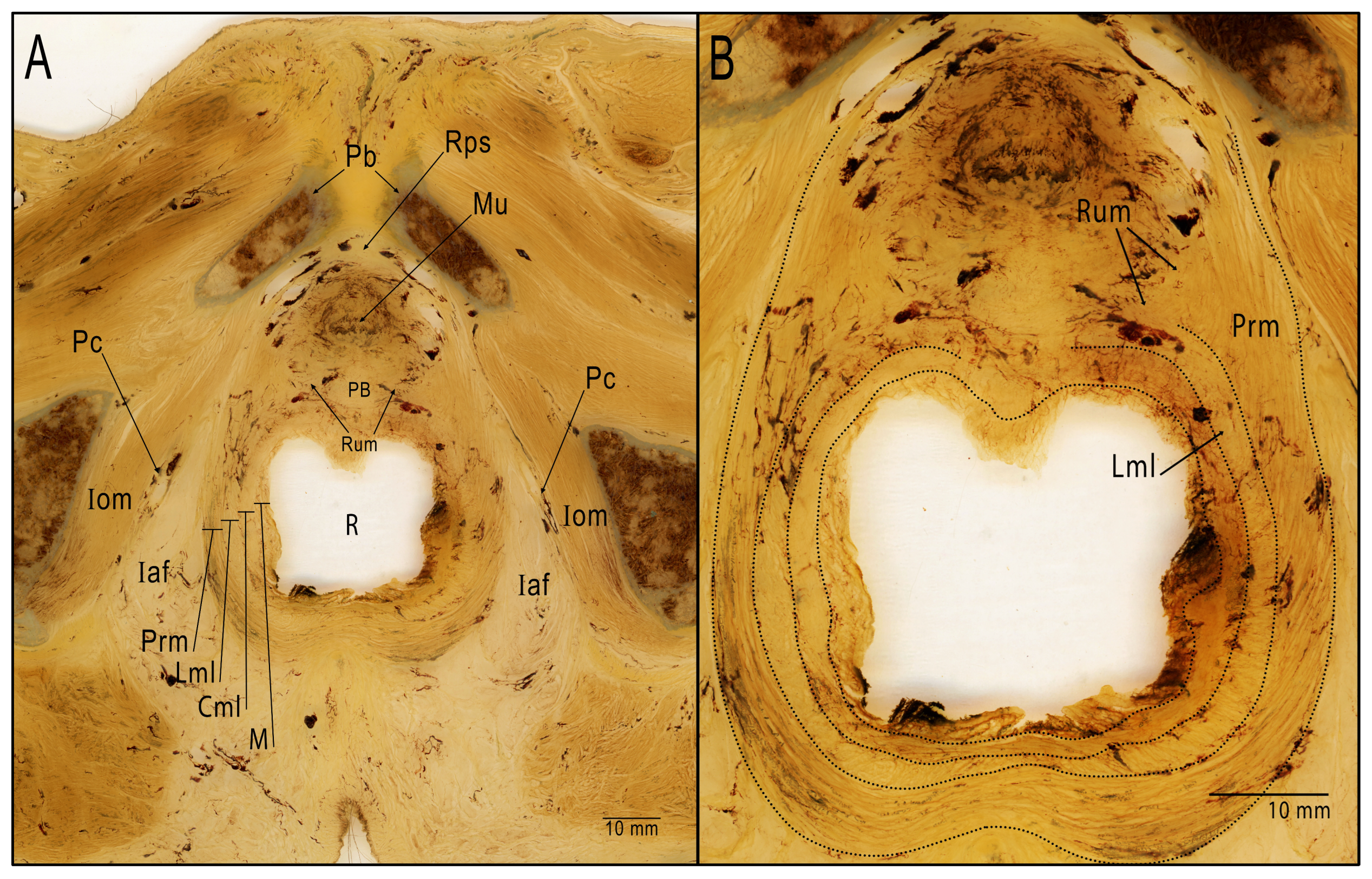
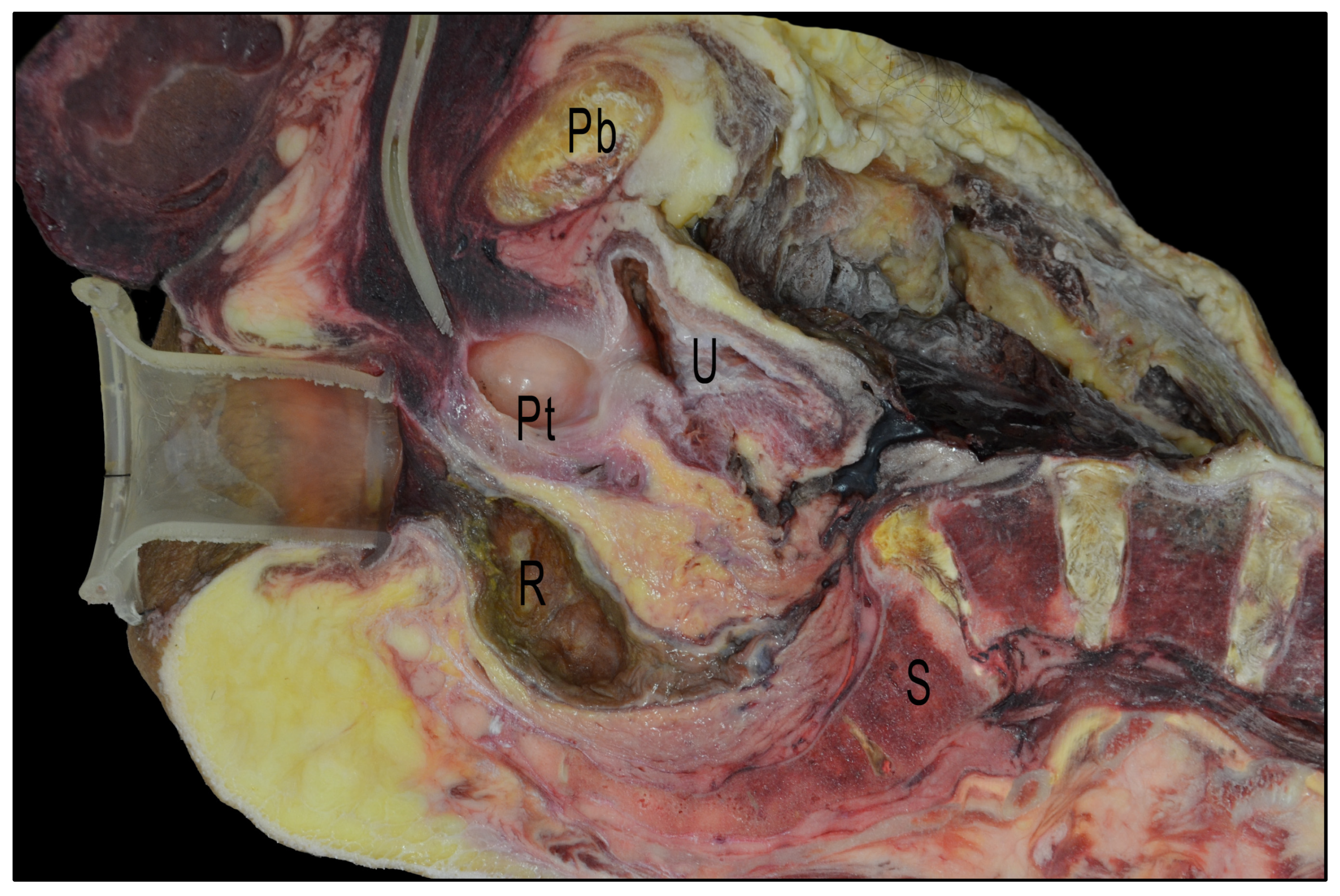
2.2. Anatomical Critical Point Description
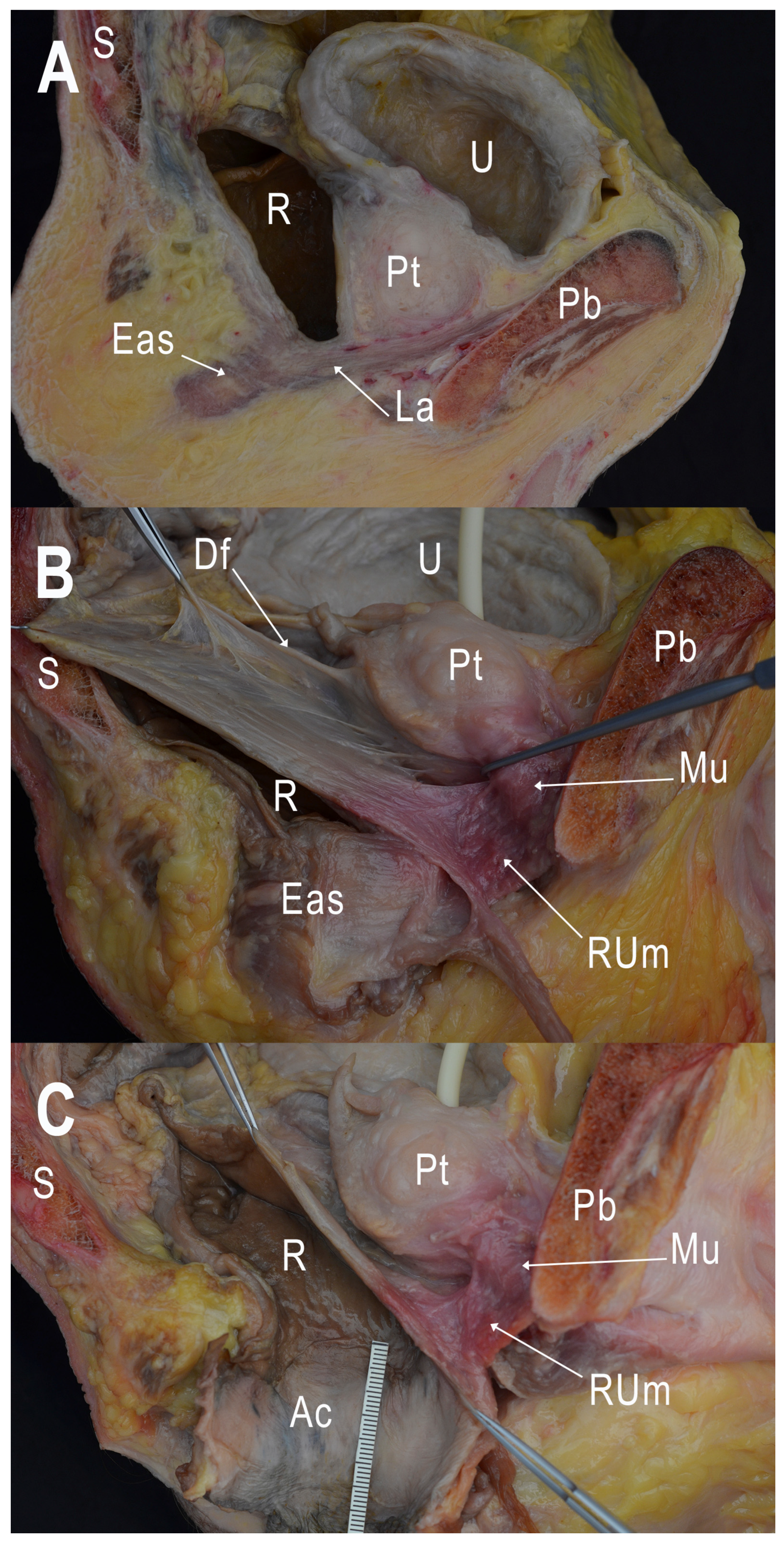
2.3. Cadaveric Dissection
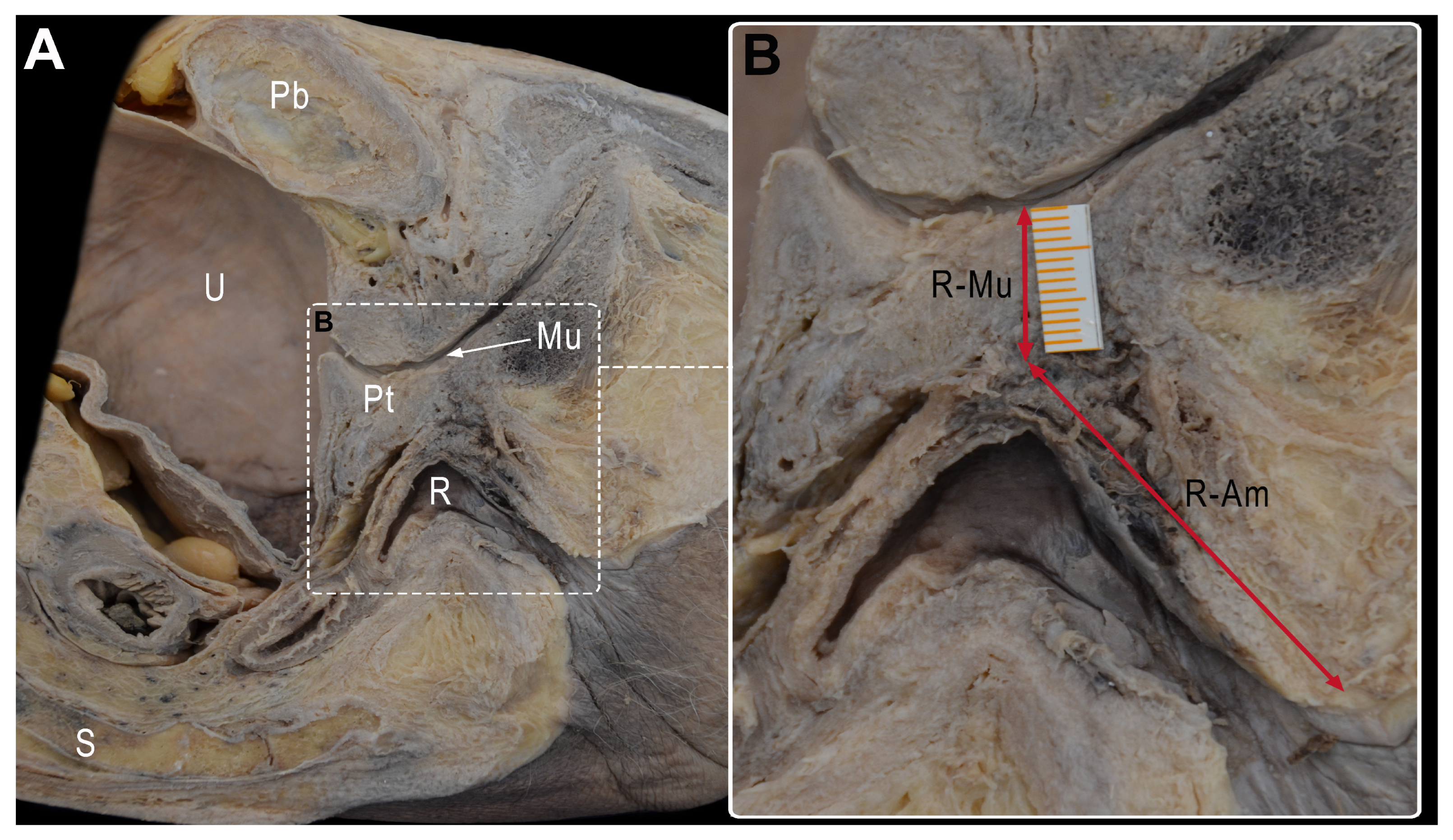
- -
- The shortest distance between the anterior surface of the rectum and the membranous urethra (R-Mu distance);
- -
- The distance between the point on the anterior wall of the rectum closest to the membranous urethra and the anal margin (R-Am distance);
- -
- The angle formed by the intersection of the axis of the anal canal and the axis of the rectum (anorectal angle).
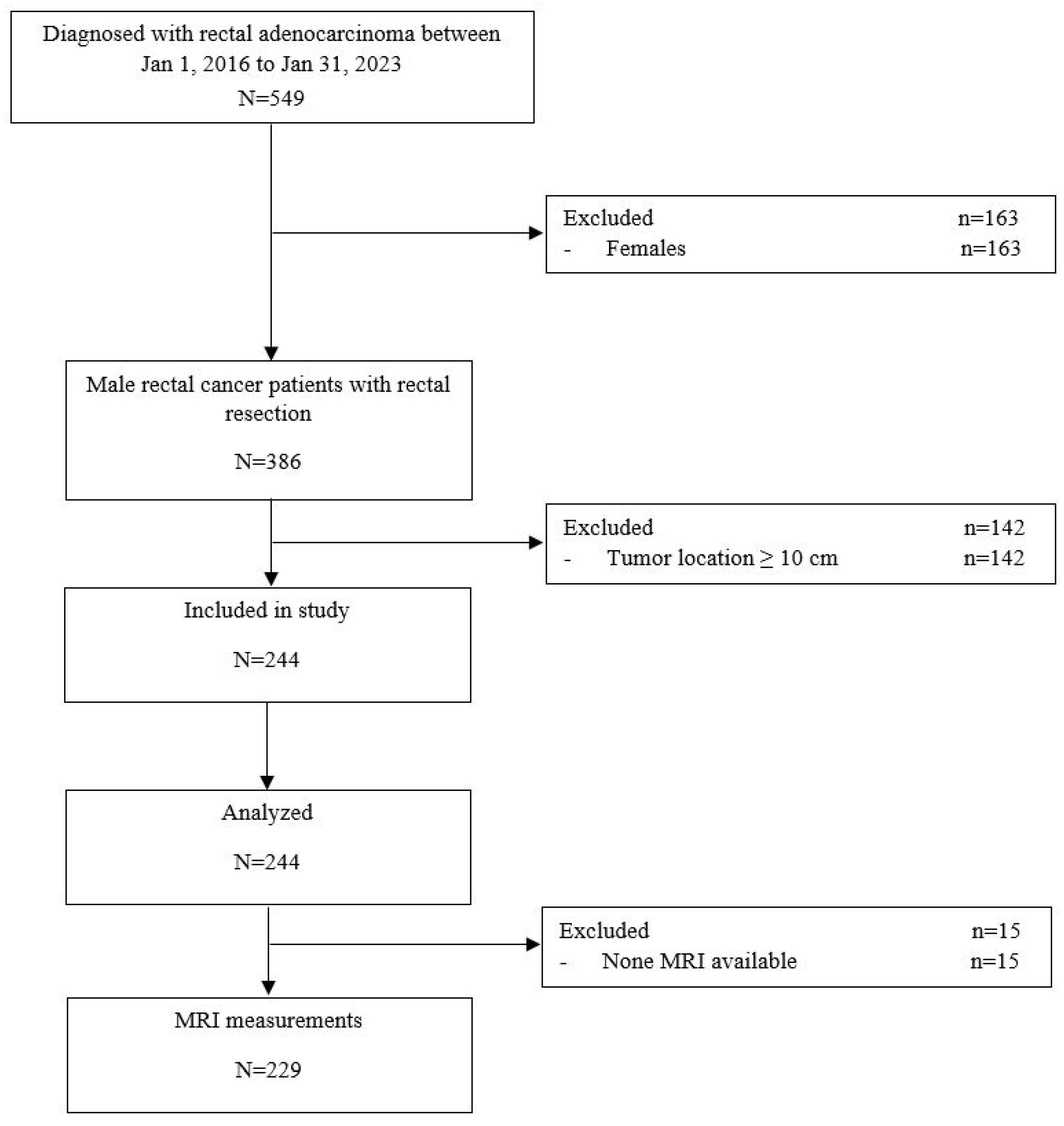
2.4. Analysis of Imaging Studies and Clinical Cases
2.5. Statistical Analysis
3. Results
3.1. Cadaveric Dissection
3.2. Analysis of Imaging Studies
3.3. Analysis of Clinical Cases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Paun, B.C.; Cassie, S.; MacLean, A.R.; Dixon, E.; Buie, W.D. Postoperative complications following surgery for rectal cancer. Ann. Surg. 2010, 251, 807–818. [Google Scholar] [CrossRef]
- Sylla, P.; Knol, J.J.; D’Andrea, A.P.; Perez, R.O.; Atallah, S.B.; Penna, M.; Hompes, R.; Wolthuis, A.; Rouanet, P.; Fingerhut, A.; et al. Urethral Injury and Other Urologic Injuries During Transanal Total Mesorectal Excision: An International Collaborative Study. Ann. Surg. 2021, 274, e115–e125. [Google Scholar] [CrossRef]
- Andersson, A.; Bergdahl, L. Urologic Complications Following Abdominoperineal Resection of the Rectum. Arch. Surg. 1976, 111, 969. [Google Scholar] [CrossRef] [PubMed]
- Sawkar, H.P.; Kim, D.Y.; Thum, D.J.; Zhao, L.; Cashy, J.; Bjurlin, M.; Bhalani, V.; Boller, A.M.; Kundu, S. Frequency of lower urinary tract injury after gastrointestinal surgery in the nationwide inpatient sample database. Am. Surg. 2014, 80, 1216–1221. [Google Scholar] [CrossRef]
- Penna, M.; Hompes, R.; Arnold, S.; Wynn, G.; Austin, R.; Warusavitarne, J.; Moran, B.; Hanna, G.B.; Mortensen, N.J.; Tekkis, P.P.; et al. Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision results from the international TATME registry. Ann. Surg. 2019, 269, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, M.; Kann, B.R. Urological Injuries during Colorectal Surgery. Clin. Colon Rectal Surg. 2019, 32, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Imai, S.; Ito, M. A novel surgical training simulator for transanal total mesorectal excision. Tech. Coloproctol. 2020, 24, 1163–1168. [Google Scholar] [CrossRef]
- Kraima, A.C.; West, N.P.; Treanor, D.; Magee, D.; Roberts, N.; van de Velde, C.J.; DeRuiter, M.C.; Quirke, P.; Rutten, H.J. The anatomy of the perineal body in relation to abdominoperineal excision for low rectal cancer. Color. Dis. 2016, 18, 688–695. [Google Scholar] [CrossRef]
- Brooks, J.D.; Eggener, S.E.; Chao, W.M. Anatomy of the rectourethralis muscle. Eur. Urol. 2002, 41, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, J.; Singh, V.; Takeda, S.; Ogeng’o, J.; Kim, H.J.; Moryś, J.; Ravi, K.S.; Ribatti, D.; Trainor, P.A.; Sañudo, J.R.; et al. Standardized statement for the ethical use of human cadaveric tissues in anatomy research papers: Recommendations from Anatomical Journal Editors-in-Chief. Clin. Anat. 2022, 35, 526–528. [Google Scholar] [CrossRef]
- Henry, R.W.; Latorre, R. Polyester Plastination of Biological Tissue: P40 Technique for Brain Slices. J. Int. Soc. Plast. 2007, 22, 59–68. [Google Scholar]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of surgical complications. Ann Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Delacroix, S.E.; Winters, J.C. Urinary tract injures: Recognition and management. Clin. Colon Rectal Surg. 2010, 23, 104–112. [Google Scholar] [CrossRef]
- Stitt, L.; Flores, F.A.; Dhalla, S.S. Urethral injury in laparoscopic-assisted abdominoperineal resection. J. Can. Urol. Assoc. 2015, 9, E900-2. [Google Scholar] [CrossRef] [PubMed]
- Renzulli, P.; Laffer, U.T. Learning curve: The surgeon as a prognostic factor in colorectal cancer surgery. Recent Results Cancer Res. 2005, 165, 86–104. [Google Scholar] [CrossRef]
- Xu, F.; Zhang, Y.; Yan, J.; Xu, B.; Wu, G.; Yang, Z.; Sun, L.; Zhang, X.; Yao, H.; Zhang, Z. The taTME learning curve for mid-low rectal cancer: A single-center experience in China. World J. Surg. Oncol. 2022, 20, 305. [Google Scholar] [CrossRef]
- Planellas, P.; Cornejo, L.; Pigem, A.; Gómez-Romeu, N.; Julià-Bergkvist, D.; Ortega, N.; Rodríguez-Hermosa, J.I.; Farrés, R. Challenges and Learning Curves in Adopting TaTME and Robotic Surgery for Rectal Cancer: A Cusum Analysis. Cancers 2022, 14, 5089. [Google Scholar] [CrossRef] [PubMed]
- Ohta, S.; Nishi, M.; Tokunaga, T.; Yoshikawa, K.; Higashijima, J.; Miyatani, T.; Kashihara, H.; Takasu, C.; Ishikawa, D.; Shimada, M. Usefulness of an ICG fluorescence catheter system in TaTME for avoiding intraoperative urethral injury. J. Med. Investig. 2020, 67, 285–288. [Google Scholar] [CrossRef]
- Peltrini, R.; Podda, M.; Castiglioni, S.; Di Nuzzo, M.M.; D’Ambra, M.; Lionetti, R.; Sodo, M.; Luglio, G.; Mucilli, F.; Di Saverio, S.; et al. Intraoperative use of indocyanine green fluorescence imaging in rectal cancer surgery: The state of the art. World J. Gastroenterol. 2021, 27, 6374–6386. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, D.A.; Zinman, L.N.; Buckley, J.C.; Marcello, P.; Browne, B.M.; Vanni, A.J. Short- and Long-term Complications and Outcomes of Radiation and Surgically Induced Rectourethral Fistula Repair with Buccal Mucosa Graft and Muscle Interposition Flap. Urology 2016, 98, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Martins, F.E.; Felicio, J.; Oliveira, T.R.; Martins, N.; Oliveira, V.; Palmas, A. Adverse features of rectourethral fistula requiring extirpative surgery and permanent dual diversion: Our experience and recommendations. J. Clin. Med. 2021, 10, 4014. [Google Scholar] [CrossRef] [PubMed]
- Phitayakorn, R.; Lachman, N. Getting back together after a break-up: Relationship advice for anatomists and surgeons. Clin. Anat. 2015, 28, 931–934. [Google Scholar] [CrossRef]

| Anatomic Pelvic Measurements | ||||||
|---|---|---|---|---|---|---|
| Cadaveric Pelvises (N = 8) | R-Mu Distance (cm) | R-Am Distance (cm) | Anorectal Angle (°) | |||
| Formalin-fixed (N = 3) | ||||||
| Case 1 | 2 | 3 | 116 | |||
| Case 2 | NA | NA | NA | |||
| Case 3 | NA | NA | NA | |||
| Cryopreserved (N = 5) | ||||||
| Case 4 | 0.8 | 3 | 116 | |||
| Case 5 | NA | NA | NA | |||
| Case 6 (Foley catheter + GP) | 0.9 | 2.7 | 120 | |||
| Case 7 (Foley catheter + GP) | 1.2 | 2.1 | 130 | |||
| Case 8 (Foley catheter + GP) | 1 | 2.4 | 150 | |||
| NA; not available, GP: GelPOINT ® Path Transanal Access Platform | ||||||
| MRI pelvic measurements | ||||||
| R-Mu distance (cm) | R-Am distance (cm) | Anorectal angle (°) | ||||
| Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | |
| MRI (N = 229) | 1 (0.7–1.2) | 1 ± 0.44 | 4.3 (3.8–5) | 4.39 ± 0.96 | 128 (121–137) | 128 ± 12.3 |
| Observational Study | |
|---|---|
| Variables | N = 244 |
| BMI, (kg/m2) | |
| <30 | 190 (77.9%) |
| ≥30 | 54 (22.1%) |
| Age (years) | |
| <70 | 141 (57.8%) |
| ≥70 | 103 (42.2%) |
| ASA | |
| I or II | 28 (11.5%) |
| III or IV | 216 (88.5%) |
| Tumor height, (cm) | |
| >10–15 | - |
| ≥5–10 | 131 (53.7%) |
| 0–5 | 113 (46.3%) |
| cT- MRI | |
| cT1 | 3 (1.3%) |
| cT2 | 36 (15.3%) |
| cT3 | 163 (69.4%) |
| cT4 | 33 (14.0%) |
| cN- MRI | |
| cN0 | 40 (17.0%) |
| cN1 | 83 (35.3%) |
| cN2 | 112 (47.7%) |
| Synchronous metastases | |
| No | 210 (86.1%) |
| Yes | 34 (13.9%) |
| Neoadjuvant treatment | |
| No | 33 (13.5%) |
| Yes | 211 (86.5%) |
| Observational Study | |
|---|---|
| Variables | N = 244 |
| Surgical approach | |
| Laparoscopy | 99 (40.6%) |
| Robot-assisted | 9 (3.7%) |
| TaTME | 63 (25.8%) |
| Open | 73 (29.9%) |
| Conversion to open surgery | |
| No | 218 (92.8%) |
| Yes | 17 (7.2%) |
| Ureteral injury | |
| No | 240 (98.4%) |
| Yes | 4 (1.6%) |
| Duration of surgery, in min, median (IQR) | 248 (200–300) |
| Hospitalization, in days, median (IQR) | 7 (5–10.8) |
| Morbidity (Clavien–Dindo) | |
| None | 156 (63.9%) |
| <IIIb | 67 (27.5%) |
| ≥IIIb | 21 (8.6%) |
| Age | Tumor Location (cm) | BMI (kg/m2) | Tumor Stage | Neoadjuvant Therapy | Time Interval (Weeks) | Intervention | |
|---|---|---|---|---|---|---|---|
| Patient 1 | 53 | 9.3 | 18.42 | T3N1M0 | Yes | 6.1 | APR |
| Patient 2 | 57 | 5 | 31.43 | T3N2M0 | Yes | 5.7 | APR |
| Patient 3 | 57 | 5.5 | 22.04 | T3N1M0 | Yes | 7.1 | TaTME |
| Patient 4 | 63 | 3.1 | 26.84 | T3N1M0 | Yes | 5.4 | TaTME |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Planellas, P.; Cornejo, L.; Ehsan, A.; Reina, F.; Ortega-Torrecilla, N.; Maldonado, E.; Codina-Cazador, A.; Osorio, M.; Farrés, R.; Carrera, A. Urethral Injury in Rectal Cancer Surgery: A Comprehensive Study Using Cadaveric Dissection, Imaging Analyses, and Clinical Series. Cancers 2023, 15, 4955. https://doi.org/10.3390/cancers15204955
Planellas P, Cornejo L, Ehsan A, Reina F, Ortega-Torrecilla N, Maldonado E, Codina-Cazador A, Osorio M, Farrés R, Carrera A. Urethral Injury in Rectal Cancer Surgery: A Comprehensive Study Using Cadaveric Dissection, Imaging Analyses, and Clinical Series. Cancers. 2023; 15(20):4955. https://doi.org/10.3390/cancers15204955
Chicago/Turabian StylePlanellas, Pere, Lídia Cornejo, Aram Ehsan, Francisco Reina, Nuria Ortega-Torrecilla, Eloy Maldonado, Antoni Codina-Cazador, Margarita Osorio, Ramon Farrés, and Anna Carrera. 2023. "Urethral Injury in Rectal Cancer Surgery: A Comprehensive Study Using Cadaveric Dissection, Imaging Analyses, and Clinical Series" Cancers 15, no. 20: 4955. https://doi.org/10.3390/cancers15204955
APA StylePlanellas, P., Cornejo, L., Ehsan, A., Reina, F., Ortega-Torrecilla, N., Maldonado, E., Codina-Cazador, A., Osorio, M., Farrés, R., & Carrera, A. (2023). Urethral Injury in Rectal Cancer Surgery: A Comprehensive Study Using Cadaveric Dissection, Imaging Analyses, and Clinical Series. Cancers, 15(20), 4955. https://doi.org/10.3390/cancers15204955





