A Comprehensive Primer on Radiation Oncology for Non-Radiation Oncologists
Abstract
Simple Summary
Abstract
1. Introduction
2. Fundamental Aspects
2.1. Basics of Radiobiology—Radiation Effects on DNA, Fractionation
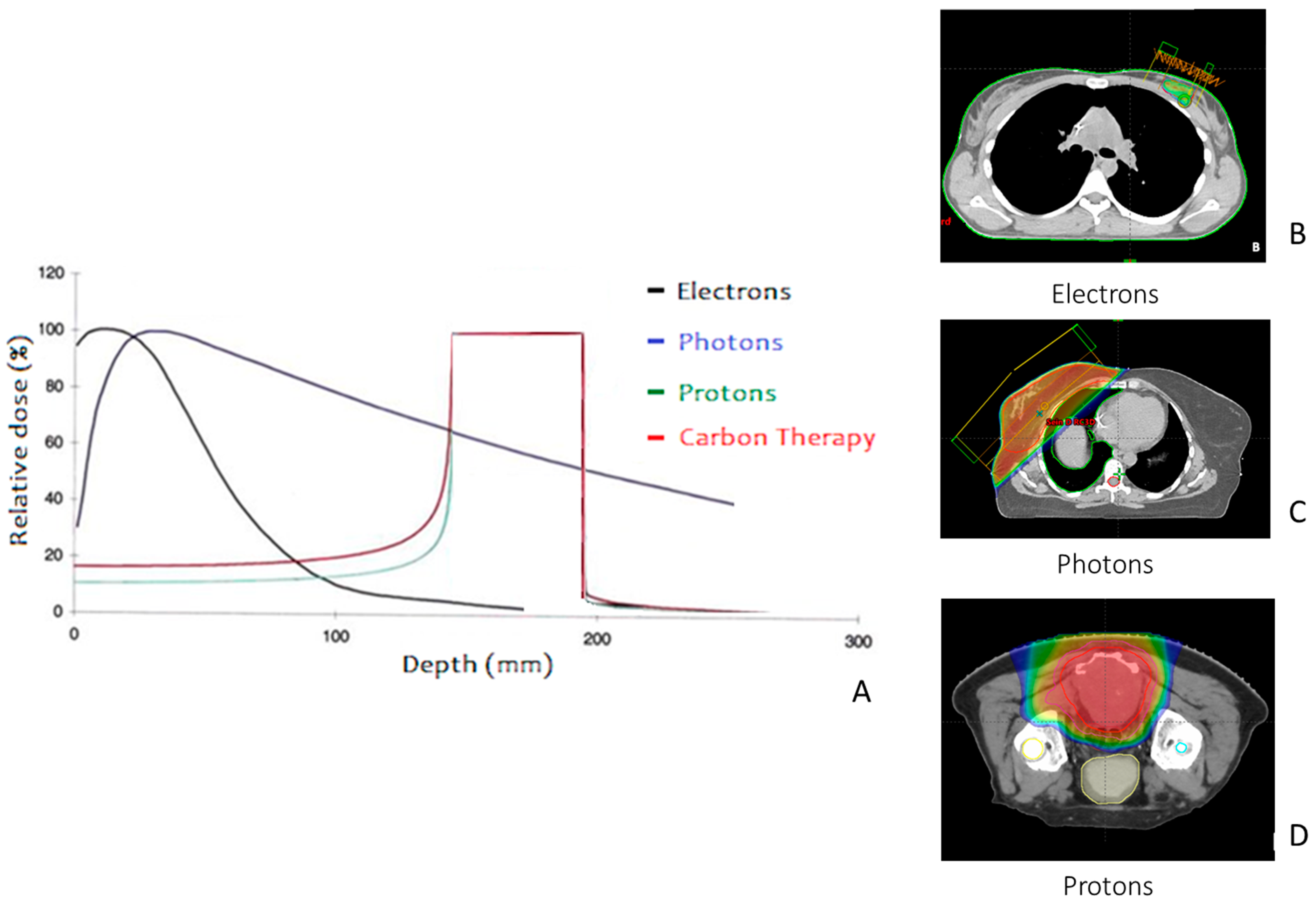
2.2. Basics of Medical Physics—Radiation Modalities
3. Main Indications of Radiation Therapy
3.1. Irradiation with Curative Intent
3.1.1. Exclusive Radiation Therapy
3.1.2. Post-Operative Radiation Therapy
3.1.3. Pre-Operative Radiation Therapy
3.2. Ablative Treatments: Stereotactic Options
3.3. Irradiation with Palliative Intent
3.4. Personalized Indications in Radiation Therapy: Balancing Risk and Life Expectancy
4. Treatment Planning
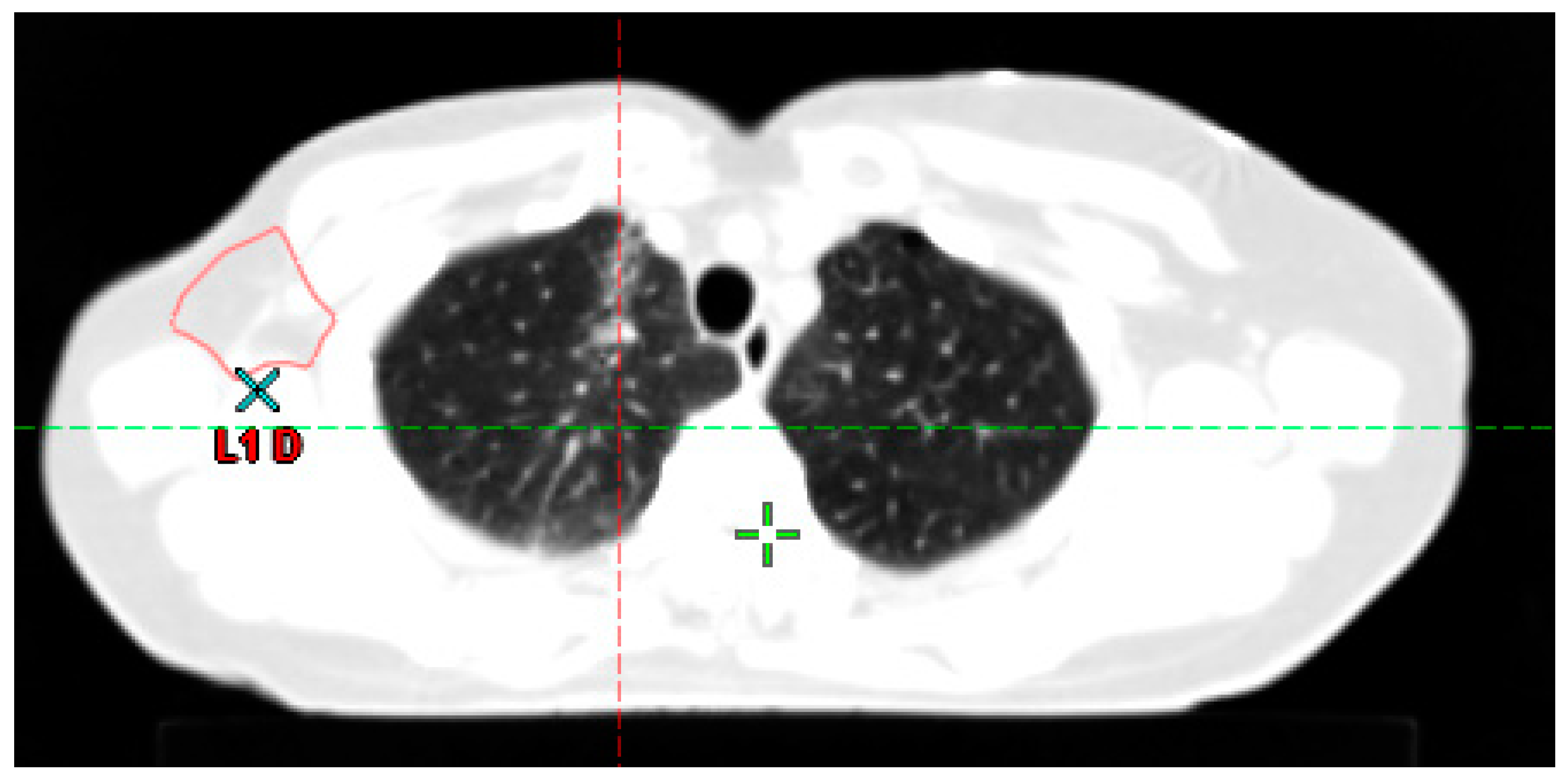
4.1. Step 1: Simulation CT
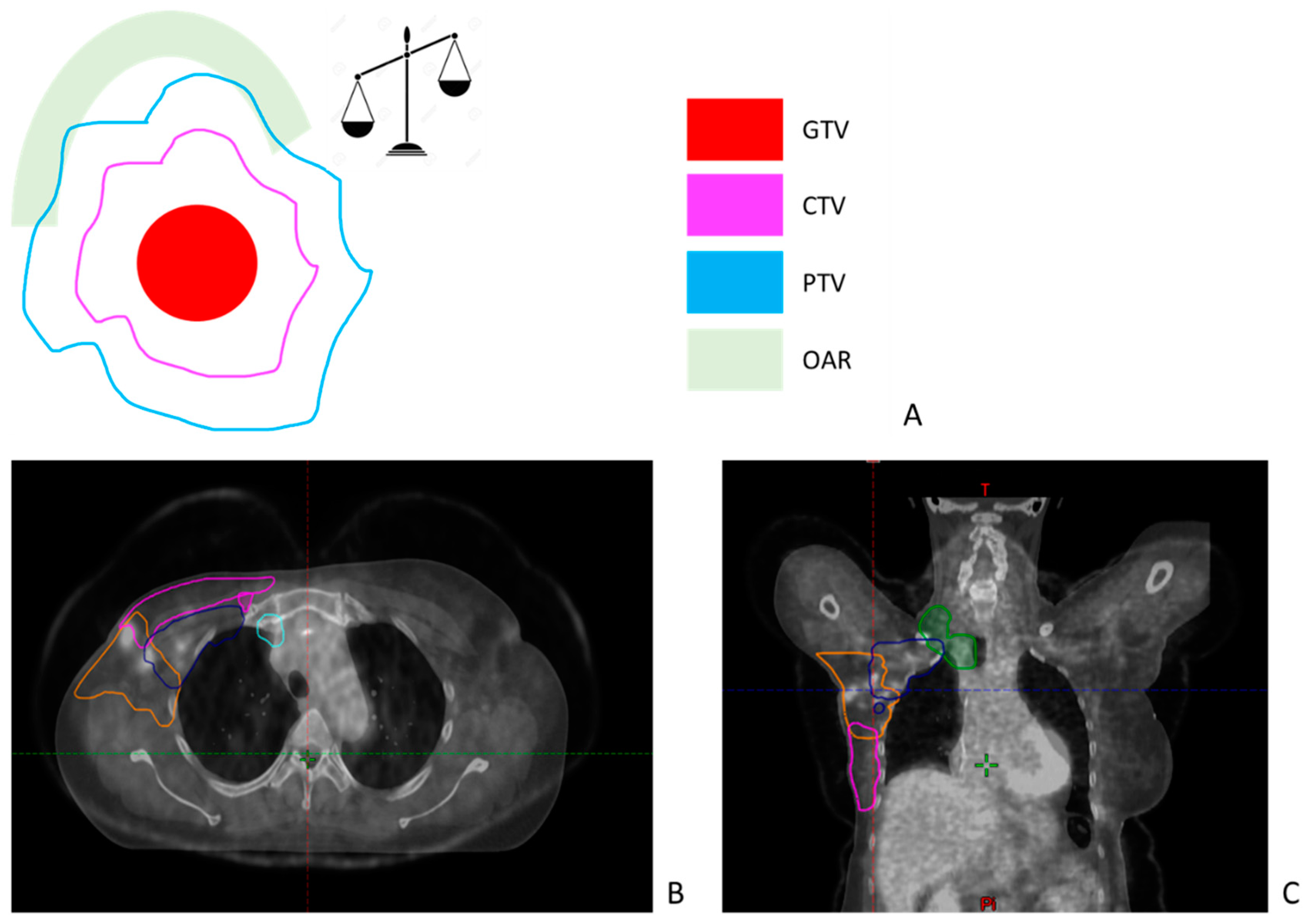
4.2. Step 2: Target Volumes and Organ at Risk Delineation
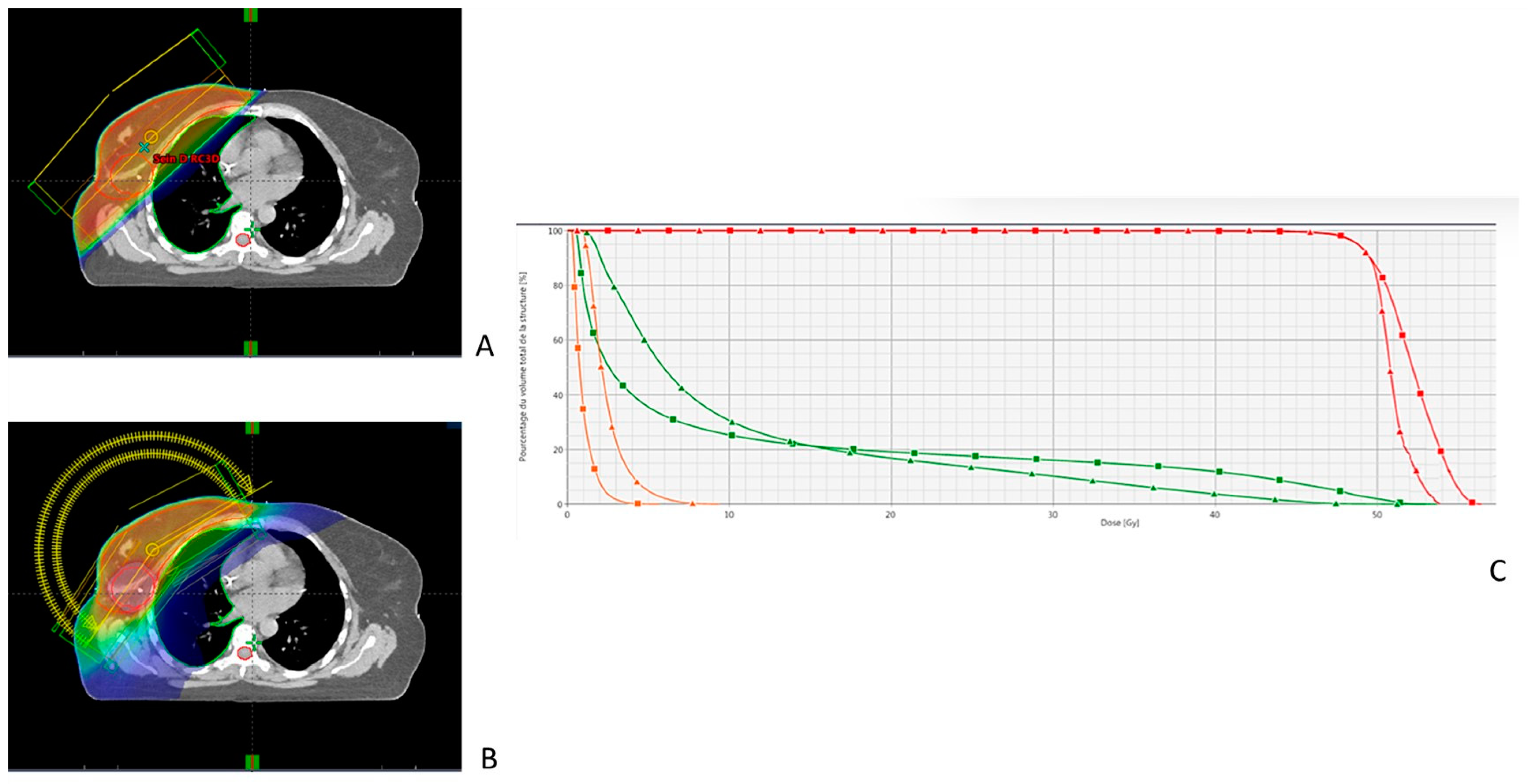
4.3. Step 3: Definition and Validation of the Radiation Therapy Plan
4.3.1. Selection of the RT Technique
4.3.2. Selection of the Fractionation
4.4. Step 4: Medical Validation of the Treatment Plan
5. Treatment Delivery and Follow-Up
5.1. Image-Guided Radiation Therapy
5.2. The Role of Radiation Therapists in Treatment Delivery
5.3. Management of Acute Toxicity
5.4. Follow-Up in Radiation Oncology
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.D.; Nogueira, L.; Devasia, T.; Mariotto, A.B.; Yabroff, K.R.; Jemal, A.; Kramer, J.; Siegel, R.L. Cancer Treatment and Survivorship Statistics, 2022. CA Cancer J. Clin. 2022, 72, 409–436. [Google Scholar] [CrossRef] [PubMed]
- Early Breast Cancer Trialists’ Collaborative Group. EBCTCG Effect of Radiotherapy after Breast-Conserving Surgery on 10-Year Recurrence and 15-Year Breast Cancer Death: Meta-Analysis of Individual Patient Data for 10,801 Women in 17 Randomised Trials. Lancet 2011, 378, 1707–1716. [Google Scholar] [CrossRef] [PubMed]
- Hayman, J.A. Treatment Summaries in Radiation Oncology and Their Role in Improving Patients’ Quality of Care: Past, Present, and Future. J. Oncol. Pract. 2009, 5, 108–109. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Siau, E.; Salazar, H.; Livergant, J.; Klein, J. Non-Oncologist Physician Knowledge of Radiation Therapy at an Urban Community Hospital. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2021, 36, 199–206. [Google Scholar] [CrossRef]
- Gillan, C.; Briggs, K.; Goytisolo Pazos, A.; Maurus, M.; Harnett, N.; Catton, P.; Wiljer, D. Barriers to Accessing Radiation Therapy in Canada: A Systematic Review. Radiat. Oncol. Lond. Engl. 2012, 7, 167. [Google Scholar] [CrossRef]
- Barnes, E.A.; Chow, E.; Danjoux, C.; Tsao, M. Collaboration between Primary Care Physicians and Radiation Oncologists. Ann. Palliat. Med. 2017, 6, 81–86. [Google Scholar] [CrossRef]
- Huang, R.; Zhou, P.-K. DNA Damage Repair: Historical Perspectives, Mechanistic Pathways and Clinical Translation for Targeted Cancer Therapy. Signal Transduct. Target. Ther. 2021, 6, 254. [Google Scholar] [CrossRef]
- Zeman, E.M. Chapter 1—The Biological Basis of Radiation Oncology. In Clinical Radiation Oncology, 4th ed.; Gunderson, L.L., Tepper, J.E., Eds.; Elsevier: Philadelphia, PA, USA, 2016; pp. 2–40.e5. ISBN 978-0-323-24098-7. [Google Scholar]
- Desouky, O.; Ding, N.; Zhou, G. Targeted and Non-Targeted Effects of Ionizing Radiation. J. Radiat. Res. Appl. Sci. 2015, 8, 247–254. [Google Scholar] [CrossRef]
- Li, L.; Guan, Y.; Chen, X.; Yang, J.; Cheng, Y. DNA Repair Pathways in Cancer Therapy and Resistance. Front. Pharmacol. 2021, 11, 629266. [Google Scholar] [CrossRef]
- Sia, J.; Szmyd, R.; Hau, E.; Gee, H.E. Molecular Mechanisms of Radiation-Induced Cancer Cell Death: A Primer. Front. Cell Dev. Biol. 2020, 8, 41. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; Tannock, I.F. Repopulation of Cancer Cells during Therapy: An Important Cause of Treatment Failure. Nat. Rev. Cancer 2005, 5, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Halperin, E.C.; Brady, L.W.; Perez, C.A.; Wazer, D.E. Perez and Brady’s Principles and Practice of Radiation Oncology, 6th ed.; Lippincott Williams&Wilkins: Philadephia, PA, USA, 2013. [Google Scholar]
- Donmez Kesen, N.; Cakir, A.; Okutan, M.; Bilge, H. A Comparison of TPS and Different Measurement Techniques in Small-Field Electron Beams. Med. Dosim. Off. J. Am. Assoc. Med. Dosim. 2015, 40, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Paganetti, H.; Beltran, C.; Both, S.; Dong, L.; Flanz, J.; Furutani, K.; Grassberger, C.; Grosshans, D.R.; Knopf, A.-C.; Langendijk, J.A.; et al. Roadmap: Proton Therapy Physics and Biology. Phys. Med. Biol. 2021, 66, 05RM01. [Google Scholar] [CrossRef]
- Durante, M.; Loeffler, J.S. Charged Particles in Radiation Oncology. Nat. Rev. Clin. Oncol. 2010, 7, 37–43. [Google Scholar] [CrossRef]
- Park, S.H.; Kang, J.O. Basics of Particle Therapy I: Physics. Radiat. Oncol. J. 2011, 29, 135–146. [Google Scholar] [CrossRef]
- Wambersie, A. RBE, Reference RBE and Clinical RBE: Applications of These Concepts in Hadron Therapy. Strahlenther. Onkol. 1999, 175, 39–43. [Google Scholar] [CrossRef]
- Choi, J.; Kang, J.O. Basics of Particle Therapy II: Relative Biological Effectiveness. Radiat. Oncol. J. 2012, 30, 1–13. [Google Scholar] [CrossRef]
- DeLaney, T.F.; Liebsch, N.J.; Pedlow, F.X.; Adams, J.; Weyman, E.A.; Yeap, B.Y.; Depauw, N.; Nielsen, G.P.; Harmon, D.C.; Yoon, S.S.; et al. Long-Term Results of Phase II Study of High Dose Photon/Proton Radiotherapy in the Management of Spine Chordomas, Chondrosarcomas, and Other Sarcomas. J. Surg. Oncol. 2014, 110, 115–122. [Google Scholar] [CrossRef]
- Mody, M.D.; Rocco, J.W.; Yom, S.S.; Haddad, R.I.; Saba, N.F. Head and Neck Cancer. Lancet Lond. Engl. 2021, 398, 2289–2299. [Google Scholar] [CrossRef]
- Falkson, C.B.; Vella, E.T.; Yu, E.; El-Mallah, M.; Mackenzie, R.; Ellis, P.M.; Ung, Y.C. Radiotherapy With Curative Intent in Patients With Early-Stage, Medically Inoperable, Non-Small-Cell Lung Cancer: A Systematic Review. Clin. Lung Cancer 2017, 18, 105–121.e5. [Google Scholar] [CrossRef] [PubMed]
- Bartelink, H.; Maingon, P.; Poortmans, P.; Weltens, C.; Fourquet, A.; Jager, J.; Schinagl, D.; Oei, B.; Rodenhuis, C.; Horiot, J.-C.; et al. Whole-Breast Irradiation with or without a Boost for Patients Treated with Breast-Conserving Surgery for Early Breast Cancer: 20-Year Follow-up of a Randomised Phase 3 Trial. Lancet Oncol. 2015, 16, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Evers, C.; Ostheimer, C.; Sieker, F.; Vordermark, D.; Medenwald, D. Benefit from Surgery with Additional Radiotherapy in N1 Head and Neck Cancer at the Time of IMRT: A Population-Based Study on Recent Developments. PLoS ONE 2020, 15, e0229266. [Google Scholar] [CrossRef]
- Beddok, A.; Cottu, P.; Fourquet, A.; Kirova, Y. Combination of Modern Radiotherapy and New Targeted Treatments for Breast Cancer Management. Cancers 2021, 13, 6358. [Google Scholar] [CrossRef] [PubMed]
- Loap, P.; Loirat, D.; Berger, F.; Rodrigues, M.; Bazire, L.; Pierga, J.-Y.; Vincent-Salomon, A.; Laki, F.; Boudali, L.; Raizonville, L.; et al. Concurrent Olaparib and Radiotherapy in Patients With Triple-Negative Breast Cancer: The Phase 1 Olaparib and Radiation Therapy for Triple-Negative Breast Cancer Trial. JAMA Oncol. 2022, 8, 1802–1808. [Google Scholar] [CrossRef]
- Haas, R.L.M.; Miah, A.B.; LePechoux, C.; DeLaney, T.F.; Baldini, E.H.; Alektiar, K.; O’Sullivan, B. Preoperative Radiotherapy for Extremity Soft Tissue Sarcoma; Past, Present and Future Perspectives on Dose Fractionation Regimens and Combined Modality Strategies. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2016, 119, 14–21. [Google Scholar] [CrossRef]
- Shapiro, J.; van Lanschot, J.J.B.; Hulshof, M.C.C.M.; van Hagen, P.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; van Laarhoven, H.W.M.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Neoadjuvant Chemoradiotherapy plus Surgery versus Surgery Alone for Oesophageal or Junctional Cancer (CROSS): Long-Term Results of a Randomised Controlled Trial. Lancet Oncol. 2015, 16, 1090–1098. [Google Scholar] [CrossRef]
- Oronsky, B.; Reid, T.; Larson, C.; Knox, S.J. Locally Advanced Rectal Cancer: The Past, Present, and Future. Semin. Oncol. 2020, 47, 85–92. [Google Scholar] [CrossRef]
- Donati, C.M.; Macchia, G.; Siepe, G.; Zamagni, A.; Benini, A.; Cellini, F.; Buwenge, M.; Cilla, S.; Cammelli, S.; Rizzo, S.; et al. Short Course Palliative Radiotherapy in Advanced Solid Tumors: A Pooled Analysis (the SHARON Project). Sci. Rep. 2022, 12, 20978. [Google Scholar] [CrossRef]
- Gardner, K.; Laird, B.J.A.; Fallon, M.T.; Sande, T.A. A Systematic Review Examining Clinical Markers and Biomarkers of Analgesic Response to Radiotherapy for Cancer-Induced Bone Pain. Crit. Rev. Oncol. Hematol. 2019, 133, 33–44. [Google Scholar] [CrossRef]
- Tsao, M.N.; Xu, W.; Wong, R.K.; Lloyd, N.; Laperriere, N.; Sahgal, A.; Rakovitch, E.; Chow, E. Whole Brain Radiotherapy for the Treatment of Newly Diagnosed Multiple Brain Metastases. Cochrane Database Syst. Rev. 2018, 1, CD003869. [Google Scholar] [CrossRef]
- Ono, T.; Nemoto, K. Re-Whole Brain Radiotherapy May Be One of the Treatment Choices for Symptomatic Brain Metastases Patients. Cancers 2022, 14, 5293. [Google Scholar] [CrossRef]
- Guhlich, M.; Maag, T.E.; Dröge, L.H.; El Shafie, R.A.; Hille, A.; Donath, S.; Schirmer, M.A.; Knaus, O.; Nauck, F.; Overbeck, T.R.; et al. Symptom Relief, Prognostic Factors, and Outcome in Patients Receiving Urgent Radiation Therapy for Superior Vena Cava Syndrome: A Single-Center Retrospective Analysis of 21 Years’ Practice. Strahlenther. Onkol. Organ Dtsch. Rontgenges. Al 2022, 198, 1072–1081. [Google Scholar] [CrossRef]
- Kawabata, H.; Fujii, T.; Yamamoto, T.; Satake, H.; Yamaguchi, K.; Okazaki, Y.; Nakase, K.; Miyata, M.; Motoi, S. Palliative Radiotherapy for Bleeding from Unresectable Gastric Cancer Using Three-Dimensional Conformal Technique. Biomedicines 2022, 10, 1394. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Mena, D.; Carbajal-Mendoza, R.; Matos, N.; Karki, N. Superior Vena Cava Syndrome: A Medical Emergency? Int. J. Angiol. Off. Publ. Int. Coll. Angiol. Inc 2008, 17, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Mitera, G.; Swaminath, A.; Wong, S.; Goh, P.; Robson, S.; Sinclair, E.; Danjoux, C.; Chow, E. Radiotherapy for Oncologic Emergencies on Weekends: Examining Reasons for Treatment and Patterns of Practice at a Canadian Cancer Centre. Curr. Oncol. Tor. Ont 2009, 16, 55–60. [Google Scholar] [CrossRef]
- Bronsart, E.; Dureau, S.; Xu, H.P.; Bazire, L.; Chilles, A.; Costa, E.; Logerot, C.; Falcou, M.-C.; Campana, F.; Berger, F.; et al. Whole Breast Radiotherapy in the Lateral Isocentric Lateral Decubitus Position: Long-Term Efficacy and Toxicity Results. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2017, 124, 214–219. [Google Scholar] [CrossRef]
- Lai, J.; Zhong, F.; Deng, J.; Hu, S.; Shen, R.; Luo, H.; Luo, Y. Prone Position versus Supine Position in Postoperative Radiotherapy for Breast Cancer: A Meta-Analysis. Medicine 2021, 100, e26000. [Google Scholar] [CrossRef] [PubMed]
- Svestad, J.G.; Heydari, M.; Mikalsen, S.G.; Flote, V.G.; Nordby, F.; Hellebust, T.P. Surface-Guided Positioning Eliminates the Need for Skin Markers in Radiotherapy of Right Sided Breast Cancer: A Single Center Randomized Crossover Trial. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2022, 177, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Contesini, M.; Guberti, M.; Saccani, R.; Braglia, L.; Iotti, C.; Botti, A.; Abbati, E.; Iemmi, M. Setup Errors in Patients with Head-Neck Cancer (HNC), Treated Using the Intensity Modulated Radiation Therapy (IMRT) Technique: How It Influences the Customised Immobilisation Systems, Patient’s Pain and Anxiety. Radiat. Oncol. Lond. Engl. 2017, 12, 72. [Google Scholar] [CrossRef]
- Dieterich, S.; Green, O.; Booth, J. SBRT Targets That Move with Respiration. Phys. Medica PM Int. J. Devoted Appl. Phys. Med. Biol. Off. J. Ital. Assoc. Biomed. Phys. AIFB 2018, 56, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Bergom, C.; Currey, A.; Desai, N.; Tai, A.; Strauss, J.B. Deep Inspiration Breath Hold: Techniques and Advantages for Cardiac Sparing During Breast Cancer Irradiation. Front. Oncol. 2018, 8, 87. [Google Scholar] [CrossRef] [PubMed]
- Guzene, L.; Beddok, A.; Nioche, C.; Modzelewski, R.; Loiseau, C.; Salleron, J.; Thariat, J. Assessing Interobserver Variability in the Delineation of Structures in Radiation Oncology: A Systematic Review. Int. J. Radiat. Oncol. Biol. Phys. 2022, 115, 1047–1060. [Google Scholar] [CrossRef] [PubMed]
- Landberg, T.; Chavaudra, J.; Dobbs, J.; Hanks, G.; Johansson, K.-A.; Möller, T.; Purdy, J. ICRU 50. Rep. Int. Comm. Radiat. Units Meas. 1993, os-26, v–vi. [Google Scholar] [CrossRef]
- Landberg, T.; Chavaudra, J.; Dobbs, J.; Gerard, J.-P.; Hanks, G.; Horiot, J.-C.; Johansson, K.-A.; Möller, T.; Purdy, J.; Suntharalingam, N.; et al. ICRU 62. Rep. Int. Comm. Radiat. Units Meas. 1999, os-32, viii–ix. [Google Scholar] [CrossRef]
- ICRU 83. J. ICRU 2010, 10, 5–6. [CrossRef]
- Rasch, C.; Steenbakkers, R.; van Herk, M. Target Definition in Prostate, Head, and Neck. Semin. Radiat. Oncol. 2005, 15, 136–145. [Google Scholar] [CrossRef]
- Marin, T.; Zhuo, Y.; Lahoud, R.M.; Tian, F.; Ma, X.; Xing, F.; Moteabbed, M.; Liu, X.; Grogg, K.; Shusharina, N.; et al. Deep Learning-Based GTV Contouring Modeling Inter- and Intra- Observer Variability in Sarcomas. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2022, 167, 269–276. [Google Scholar] [CrossRef]
- Hindocha, S.; Zucker, K.; Jena, R.; Banfill, K.; Mackay, K.; Price, G.; Pudney, D.; Wang, J.; Taylor, A. Artificial Intelligence for Radiotherapy Auto-Contouring: Current Use, Perceptions of and Barriers to Implementation. Clin. Oncol. 2023, 35, 219–226. [Google Scholar] [CrossRef]
- Grégoire, V.; Evans, M.; Le, Q.-T.; Bourhis, J.; Budach, V.; Chen, A.; Eisbruch, A.; Feng, M.; Giralt, J.; Gupta, T.; et al. Delineation of the Primary Tumour Clinical Target Volumes (CTV-P) in Laryngeal, Hypopharyngeal, Oropharyngeal and Oral Cavity Squamous Cell Carcinoma: AIRO, CACA, DAHANCA, EORTC, GEORCC, GORTEC, HKNPCSG, HNCIG, IAG-KHT, LPRHHT, NCIC CTG, NCRI, NRG Oncology, PHNS, SBRT, SOMERA, SRO, SSHNO, TROG Consensus Guidelines. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2018, 126, 3–24. [Google Scholar] [CrossRef]
- Kihara, S.; Koike, Y.; Takegawa, H.; Anetai, Y.; Nakamura, S.; Tanigawa, N.; Koizumi, M. Clinical Target Volume Segmentation Based on Gross Tumor Volume Using Deep Learning for Head and Neck Cancer Treatment. Med. Dosim. 2023, 48, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Kazemimoghadam, M.; Yang, Z.; Chen, M.; Rahimi, A.; Kim, N.; Alluri, P.; Nwachukwu, C.; Lu, W.; Gu, X. A Deep Learning Approach for Automatic Delineation of Clinical Target Volume in Stereotactic Partial Breast Irradiation (S-PBI). Phys. Med. Biol. 2023, 68, 105011. [Google Scholar] [CrossRef] [PubMed]
- van Herk, M. Errors and Margins in Radiotherapy. Semin. Radiat. Oncol. 2004, 14, 52–64. [Google Scholar] [CrossRef]
- Chang, J.Y.; Dong, L.; Liu, H.; Starkschall, G.; Balter, P.; Mohan, R.; Liao, Z.; Cox, J.D.; Komaki, R. Image-Guided Radiation Therapy for Non-Small Cell Lung Cancer. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2008, 3, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Gay, H.A.; Barthold, H.J.; O’Meara, E.; Bosch, W.R.; El Naqa, I.; Al-Lozi, R.; Rosenthal, S.A.; Lawton, C.; Lee, W.R.; Sandler, H.; et al. Pelvic Normal Tissue Contouring Guidelines for Radiation Therapy: A Radiation Therapy Oncology Group Consensus Panel Atlas. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, e353–e362. [Google Scholar] [CrossRef]
- Brouwer, C.L.; Steenbakkers, R.J.H.M.; Bourhis, J.; Budach, W.; Grau, C.; Grégoire, V.; van Herk, M.; Lee, A.; Maingon, P.; Nutting, C.; et al. CT-Based Delineation of Organs at Risk in the Head and Neck Region: DAHANCA, EORTC, GORTEC, HKNPCSG, NCIC CTG, NCRI, NRG Oncology and TROG Consensus Guidelines. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2015, 117, 83–90. [Google Scholar] [CrossRef]
- Beddok, A.; Faivre, J.-C.; Coutte, A.; Guévelou, J.L.; Welmant, J.; Clavier, J.-B.; Guihard, S.; Janoray, G.; Calugaru, V.; Pointreau, Y.; et al. Practical Contouring Guidelines with an MR-Based Atlas of Brainstem Structures Involved in Radiation-Induced Nausea and Vomiting. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2019, 130, 113–120. [Google Scholar] [CrossRef]
- Hong, T.S.; Ritter, M.A.; Tomé, W.A.; Harari, P.M. Intensity-Modulated Radiation Therapy: Emerging Cancer Treatment Technology. Br. J. Cancer 2005, 92, 1819–1824. [Google Scholar] [CrossRef]
- Nutting, C.M.; Morden, J.P.; Harrington, K.J.; Urbano, T.G.; Bhide, S.A.; Clark, C.; Miles, E.A.; Miah, A.B.; Newbold, K.; Tanay, M.; et al. Parotid-Sparing Intensity Modulated versus Conventional Radiotherapy in Head and Neck Cancer (PARSPORT): A Phase 3 Multicentre Randomised Controlled Trial. Lancet Oncol. 2011, 12, 127–136. [Google Scholar] [CrossRef]
- Beddok, A.; Vela, A.; Calugaru, V.; Tessonnier, T.; Kubes, J.; Dutheil, P.; Gerard, A.; Vidal, M.; Goudjil, F.; Florescu, C.; et al. Proton Therapy for Head and Neck Squamous Cell Carcinomas: A Review of the Physical and Clinical Challenges. Radiother. Oncol. 2020, 147, 30–39. [Google Scholar] [CrossRef]
- Blanchard, P.; Garden, A.S.; Gunn, G.B.; Rosenthal, D.I.; Morrison, W.H.; Hernandez, M.; Crutison, J.; Lee, J.J.; Ye, R.; Fuller, C.D.; et al. Intensity-Modulated Proton Beam Therapy (IMPT) versus Intensity-Modulated Photon Therapy (IMRT) for Patients with Oropharynx Cancer—A Case Matched Analysis. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2016, 120, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Langendijk, J.A.; Hoebers, F.J.P.; de Jong, M.A.; Doornaert, P.; Terhaard, C.H.J.; Steenbakkers, R.J.H.M.; Hamming-Vrieze, O.; van de Kamer, J.B.; Verbakel, W.F.A.R.; Keskin-Cambay, F.; et al. National Protocol for Model-Based Selection for Proton Therapy in Head and Neck Cancer. Int. J. Part. Ther. 2021, 8, 354–365. [Google Scholar] [CrossRef]
- PTCOG—Facilities in Operation. Available online: https://www.ptcog.site/index.php/facilities-in-operation-public (accessed on 17 April 2023).
- Amaldi, U.; Dosanjh, M.; Balosso, J.; Overgaard, J.; Sørensen, B. A Facility for Tumour Therapy and Biomedical Research in South-Eastern Europe; CERN: Geneva, Switzerland, 2019. [Google Scholar]
- Bentzen, S.M. 3—Fractionation Effects in Clinical Practice. In Leibel and Phillips Textbook of Radiation Oncology, 3rd ed.; Hoppe, R.T., Phillips, T.L., Roach, M., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2010; pp. 40–54. ISBN 978-1-4160-5897-7. [Google Scholar]
- Belani, C.P.; Wang, W.; Johnson, D.H.; Wagner, H.; Schiller, J.; Veeder, M.; Mehta, M.; Eastern Cooperative Oncology Group. Phase III Study of the Eastern Cooperative Oncology Group (ECOG 2597): Induction Chemotherapy Followed by Either Standard Thoracic Radiotherapy or Hyperfractionated Accelerated Radiotherapy for Patients with Unresectable Stage IIIA and B Non-Small-Cell Lung Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2005, 23, 3760–3767. [Google Scholar] [CrossRef]
- You, R.; Liu, Y.-P.; Xie, Y.-L.; Lin, C.; Duan, C.-Y.; Chen, D.-P.; Pan, Y.; Qi, B.; Zou, X.; Guo, L.; et al. Hyperfractionation Compared with Standard Fractionation in Intensity-Modulated Radiotherapy for Patients with Locally Advanced Recurrent Nasopharyngeal Carcinoma: A Multicentre, Randomised, Open-Label, Phase 3 Trial. Lancet Lond. Engl. 2023, 401, 917–927. [Google Scholar] [CrossRef]
- Haviland, J.S.; Owen, J.R.; Dewar, J.A.; Agrawal, R.K.; Barrett, J.; Barrett-Lee, P.J.; Dobbs, H.J.; Hopwood, P.; Lawton, P.A.; Magee, B.J.; et al. The UK Standardisation of Breast Radiotherapy (START) Trials of Radiotherapy Hypofractionation for Treatment of Early Breast Cancer: 10-Year Follow-up Results of Two Randomised Controlled Trials. Lancet Oncol. 2013, 14, 1086–1094. [Google Scholar] [CrossRef] [PubMed]
- Murray Brunt, A.; Haviland, J.S.; Wheatley, D.A.; Sydenham, M.A.; Alhasso, A.; Bloomfield, D.J.; Chan, C.; Churn, M.; Cleator, S.; Coles, C.E.; et al. Hypofractionated Breast Radiotherapy for 1 Week versus 3 Weeks (FAST-Forward): 5-Year Efficacy and Late Normal Tissue Effects Results from a Multicentre, Non-Inferiority, Randomised, Phase 3 Trial. Lancet Lond. Engl. 2020, 395, 1613–1626. [Google Scholar] [CrossRef] [PubMed]
- Chargari, C.; Deutsch, E.; Blanchard, P.; Gouy, S.; Martelli, H.; Guérin, F.; Dumas, I.; Bossi, A.; Morice, P.; Viswanathan, A.N.; et al. Brachytherapy: An Overview for Clinicians. CA Cancer J. Clin. 2019, 69, 386–401. [Google Scholar] [CrossRef]
- Fuller, D.B.; Naitoh, J.; Shirazi, R.; Crabtree, T.; Mardirossian, G. Prostate SBRT: Comparison the Efficacy and Toxicity of Two Different Dose Fractionation Schedules. Front. Oncol. 2020, 10, 936. [Google Scholar] [CrossRef]
- Beddok, A.; Lahaye, C.; Calugaru, V.; De Marzi, L.; Fouillade, C.; Salvador, S.; Fontbonne, J.-M.; Favaudon, V.; Thariat, J. A Comprehensive Analysis of the Relationship Between Dose Rate and Biological Effects in Preclinical and Clinical Studies, From Brachytherapy to Flattening Filter Free Radiation Therapy and FLASH Irradiation. Int. J. Radiat. Oncol. 2022, 113, 985–995. [Google Scholar] [CrossRef]
- Xia, P.; Sintay, B.J.; Colussi, V.C.; Chuang, C.; Lo, Y.-C.; Schofield, D.; Wells, M.; Zhou, S. Medical Physics Practice Guideline (MPPG) 11.a: Plan and Chart Review in External Beam Radiotherapy and Brachytherapy. J. Appl. Clin. Med. Phys. 2021, 22, 4–19. [Google Scholar] [CrossRef]
- Emami, B.; Lyman, J.; Brown, A.; Coia, L.; Goitein, M.; Munzenrider, J.E.; Shank, B.; Solin, L.J.; Wesson, M. Tolerance of Normal Tissue to Therapeutic Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1991, 21, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.B.; Yorke, E.D.; Jackson, A.; Ten Haken, R.K.; Constine, L.S.; Eisbruch, A.; Bentzen, S.M.; Nam, J.; Deasy, J.O. Use of Normal Tissue Complication Probability Models in the Clinic. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, S10–S19. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.A.; Babaiah, M.; Madhusudhan, N.; George, G.; Jain, S.; Ramalingam, K.; Kumar, S.A.; Karthikeyan, K.; Anantharaman, A. Comparative Dosimetric Analysis of IMRT and VMAT (RapidArc) in Brain, Head and Neck, Breast and Prostate Malignancies. Int. J. Cancer Ther. Oncol. 2014, 3, 03019. [Google Scholar] [CrossRef]
- Pawar, K.; Chen, Z.; Seah, J.; Law, M.; Close, T.; Egan, G. Clinical Utility of Deep Learning Motion Correction for T1 Weighted MPRAGE MR Images. Eur. J. Radiol. 2020, 133, 109384. [Google Scholar] [CrossRef]
- van Beek, S.; van Kranen, S.; Mencarelli, A.; Remeijer, P.; Rasch, C.; van Herk, M.; Sonke, J.-J. First Clinical Experience with a Multiple Region of Interest Registration and Correction Method in Radiotherapy of Head-and-Neck Cancer Patients. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2010, 94, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Vilotte, F.; Antoine, M.; Bobin, M.; Latorzeff, I.; Supiot, S.; Richaud, P.; Thomas, L.; Leduc, N.; Guérif, S.; Iriondo-Alberdi, J.; et al. Post-Prostatectomy Image-Guided Radiotherapy: The Invisible Target Concept. Front. Oncol. 2017, 7, 34. [Google Scholar] [CrossRef][Green Version]
- Lee, C.; Langen, K.M.; Lu, W.; Haimerl, J.; Schnarr, E.; Ruchala, K.J.; Olivera, G.H.; Meeks, S.L.; Kupelian, P.A.; Shellenberger, T.D.; et al. Assessment of Parotid Gland Dose Changes during Head and Neck Cancer Radiotherapy Using Daily Megavoltage Computed Tomography and Deformable Image Registration. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 1563–1571. [Google Scholar] [CrossRef]
- Raghavan, G.; Kishan, A.U.; Cao, M.; Chen, A.M. Anatomic and Dosimetric Changes in Patients with Head and Neck Cancer Treated with an Integrated MRI-Tri-60Co Teletherapy Device. Br. J. Radiol. 2016, 89, 20160624. [Google Scholar] [CrossRef]
- Yang, Y.; Cao, M.; Sheng, K.; Gao, Y.; Chen, A.; Kamrava, M.; Lee, P.; Agazaryan, N.; Lamb, J.; Thomas, D.; et al. Longitudinal Diffusion MRI for Treatment Response Assessment: Preliminary Experience Using an MRI-Guided Tri-Cobalt 60 Radiotherapy System. Med. Phys. 2016, 43, 1369–1373. [Google Scholar] [CrossRef]
- Bruijnen, T.; Stemkens, B.; Terhaard, C.H.J.; Lagendijk, J.J.W.; Raaijmakers, C.P.J.; Tijssen, R.H.N. Intrafraction Motion Quantification and Planning Target Volume Margin Determination of Head-and-Neck Tumors Using Cine Magnetic Resonance Imaging. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2019, 130, 82–88. [Google Scholar] [CrossRef]
- Pathmanathan, A.U.; van As, N.J.; Kerkmeijer, L.G.W.; Christodouleas, J.; Lawton, C.A.F.; Vesprini, D.; van der Heide, U.A.; Frank, S.J.; Nill, S.; Oelfke, U.; et al. Magnetic Resonance Imaging-Guided Adaptive Radiation Therapy: A “Game Changer” for Prostate Treatment? Int. J. Radiat. Oncol. Biol. Phys. 2018, 100, 361–373. [Google Scholar] [CrossRef] [PubMed]
- Kishan, A.U.; Ma, T.M.; Lamb, J.M.; Casado, M.; Wilhalme, H.; Low, D.A.; Sheng, K.; Sharma, S.; Nickols, N.G.; Pham, J.; et al. Magnetic Resonance Imaging-Guided vs Computed Tomography-Guided Stereotactic Body Radiotherapy for Prostate Cancer: The MIRAGE Randomized Clinical Trial. JAMA Oncol. 2023, 9, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.; Cao, M.; Hsu, S.; Lamb, J.; Mikaeilian, A.; Yang, Y.; Agazaryan, N.; Low, D.A.; Steinberg, M.L. Magnetic Resonance Imaging Guided Reirradiation of Recurrent and Second Primary Head and Neck Cancer. Adv. Radiat. Oncol. 2017, 2, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Yee, C.; Wang, K.; Asthana, R.; Drost, L.; Lam, H.; Lee, J.; Vesprini, D.; Leung, E.; DeAngelis, C.; Chow, E. Radiation-Induced Skin Toxicity in Breast Cancer Patients: A Systematic Review of Randomized Trials. Clin. Breast Cancer 2018, 18, e825–e840. [Google Scholar] [CrossRef] [PubMed]
- Zenda, S.; Ota, Y.; Tachibana, H.; Ogawa, H.; Ishii, S.; Hashiguchi, C.; Akimoto, T.; Ohe, Y.; Uchitomi, Y. A Prospective Picture Collection Study for a Grading Atlas of Radiation Dermatitis for Clinical Trials in Head-and-Neck Cancer Patients. J. Radiat. Res. 2016, 57, 301–306. [Google Scholar] [CrossRef][Green Version]
- Yao, J.-J.; Jin, Y.-N.; Wang, S.-Y.; Zhang, F.; Zhou, G.-Q.; Zhang, W.-J.; Zhi-Bin; Cheng, M.J.; Qi, Z.-Y.; Sun, Y. The Detrimental Effects of Radiotherapy Interruption on Local Control after Concurrent Chemoradiotherapy for Advanced T-Stage Nasopharyngeal Carcinoma: An Observational, Prospective Analysis. BMC Cancer 2018, 18, 740. [Google Scholar] [CrossRef]
- Schechter, N.R.; Brown, D.W.; Bovi, J.A.; Dominello, M.M.; Liu, A.K.; Mattes, M.D.; Michalski, J.M.; Shih, H.A.; Strom, E.; Wilkinson, J.B.; et al. ACR-ASTRO Practice Parameter for Communication: Radiation Oncology. Am. J. Clin. Oncol. 2020, 43, 553–558. [Google Scholar] [CrossRef]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E.; ESMO Guidelines Committee. Electronic address: Clinicalguidelines@esmo.org Early Breast Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up†. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef]
- Prades, J.; Remue, E.; van Hoof, E.; Borras, J.M. Is It Worth Reorganising Cancer Services on the Basis of Multidisciplinary Teams (MDTs)? A Systematic Review of the Objectives and Organisation of MDTs and Their Impact on Patient Outcomes. Health Policy 2015, 119, 464–474. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beddok, A.; Lim, R.; Thariat, J.; Shih, H.A.; El Fakhri, G. A Comprehensive Primer on Radiation Oncology for Non-Radiation Oncologists. Cancers 2023, 15, 4906. https://doi.org/10.3390/cancers15204906
Beddok A, Lim R, Thariat J, Shih HA, El Fakhri G. A Comprehensive Primer on Radiation Oncology for Non-Radiation Oncologists. Cancers. 2023; 15(20):4906. https://doi.org/10.3390/cancers15204906
Chicago/Turabian StyleBeddok, Arnaud, Ruth Lim, Juliette Thariat, Helen A. Shih, and Georges El Fakhri. 2023. "A Comprehensive Primer on Radiation Oncology for Non-Radiation Oncologists" Cancers 15, no. 20: 4906. https://doi.org/10.3390/cancers15204906
APA StyleBeddok, A., Lim, R., Thariat, J., Shih, H. A., & El Fakhri, G. (2023). A Comprehensive Primer on Radiation Oncology for Non-Radiation Oncologists. Cancers, 15(20), 4906. https://doi.org/10.3390/cancers15204906






